Abstract
Introduction
The incidence of acute coronary syndrome is rising in step with the growth of life expectancy. An increase in the age of patients with coronary artery disease has been related to in-hospital mortality, which has seen an upsurge over a short period of time. However, there is no consensus about the percutaneous coronary angioplasty strategy to follow for older patients with multivessel coronary artery disease (MVCAD). Complete revascularisation (CR) or incomplete revascularisation (ICR) strategy depends on prognosis but this has not yet been accurately described because of geriatric conditions and comorbidities. The aim of this study is to evaluate changes of clinical and biochemical parameters in older patients with MVCAD undergoing revascularisation and to establish a prognostic stratification model for CR and ICR.
Methods and analysis
This observational, longitudinal, prospective study will include 150 patients with MVCAD and subsequent revascularisation who attend the Hospital Universitario Virgen de la Victoria (Málaga, Spain). Because of the dropout rates, 180 patients will be recruited at the beginning. Sociodemographic characteristics, clinical and angiographic parameters, and biochemical variables, such as cardiovascular, metabolic, inflammatory, stress oxidative biomarkers, will be collected in the admission for coronary revascularisation and three follow-ups at 6, 12 and 18 months. Statistical analyses will be conducted with these data using CR and ICR as the primary exposure variable. Relevant explanatory variables will be selected from a predictive model for their inclusion in a prognostic stratification model. The primary outcome measures will be major adverse cardiovascular events.
Ethics and dissemination
Protocols and patient information have been approved by the regional research ethics committee (CEIm Provincial de Málaga-PEIBA (PI0131/2020). The results will be disseminated in international peer-reviewed journals, presented at conferences in Cardiology and Gerontology, and sent to participants, medical and health service managers, clinicians and other researchers.
Keywords: myocardial infarction, ischaemic heart disease, adult cardiology, geriatric medicine, coronary intervention
Strengths and limitations of this study.
This study will collect a comprehensive range of clinical and biochemical data from older patients with multivessel coronary artery disease treated with percutaneous coronary angioplasty to compare complete revascularisation (CR) and incomplete revascularisation (ICR) strategies.
Because this prospective study will allow follow-up patients over time, relevant explanatory data will be analysed to develop predictive models for both revascularisation strategies with the objective of establishing a prognostic stratification.
Causality cannot be established between outcomes because this is an observational research and we will be unable to control for all confounding factors, only associations between outcomes will be explored.
All participants will be recruited from a single centre, which affects the sample size and restricts the extrapolation of results to other populations, but the decision-making of the clinicians for CR or ICR will be more uniform than in a multicentre study.
The COVID-19 pandemic and the health system saturation risk may produce high rates of delay and loss of follow-up in the study because older populations are more likely to develop severe illness by SARS-CoV-2.
Introduction
Ischaemic heart disease is the main cause of death globally. It is responsible for 16% of the world’s total mortality and caused 8.9 million deaths in 2019.1 The progressive increase of age of patients with coronary artery disease, such as angina, myocardial infarction and cardiac arrest, has been related to in-hospital mortality over a short period of time. In Spain, 14.2% of the population is ≥70 years old, and it is estimated that 27.4% of patients with ischaemic heart diseases are between 70 and 80 years of age.2
Despite their demographic importance, older adults are usually excluded or under-represented in most clinical trials and large studies of cardiovascular diseases because of the high prevalence of comorbidities (eg, psychiatric disorders, metabolic diseases such as diabetes mellitus, cancer and chronic inflammatory diseases) and the presence of geriatric syndromes (eg, frailty, falls, pressure ulcers, cognitive impairment, delirium, mood disorders, polypharmacy and urinary incontinence), which are related to a worse quality of life with high rates of hospitalisation, disability and mortality.3–5 Furthermore, several lines of evidence demonstrate that dysregulation of the regulation of energy metabolism occur during ageing and contribute to low-grade inflammation and oxidative stress.6 7 This systemic dysregulation in major molecular processes has adverse effects on the structure and function of the cardiovascular system, among others.7 8 Therefore, the scientific evidence for this group of the population is quite limited and the current management in clinical practice is usually carried out on the basis of studies in younger patients and the experience of the doctors, which causes a great variability in the prognosis and therapeutic approaches of ischaemic heart diseases.
There are considerable differences between older patients hospitalised for acute coronary syndrome (ST and non-ST segment elevation acute coronary syndromes (STE-ACS and NSTE-ACS)) and the general population. Thus, older patients with ischaemic heart diseases present particular clinical and electrocardiographic characteristics that affect their prognosis relative to younger patients. Specifically, there is a higher rate of all cause-mortality, stroke, myocardial infarction, bleeding and unscheduled revascularisation, atypical symptoms (eg, lower percentage of chest pain and more dyspnoea), syncope, vegetative alterations (eg, arterial hypotension and sweating), nausea and/or confusion.9 10 Regarding electrocardiographic manifestations, older patients show high prevalence of repolarisation disorders, left ventricular hypertrophy, left bundle branch block and atrial fibrillation.9 11 12
An important point is that older adults with ischaemic heart disease usually present multivessel coronary artery disease (MVCAD), which makes treatment difficult because of the complex coronary anatomy and differences in the severity and extension of the coronary artery disease in these vessels.13 14 In fact, patients with MVCAD show major adverse cardiac events (MACE) such as heart failure, reinfarction, stroke, hospitalisation for cardiovascular-related illness, unscheduled revascularisation and all-cause death and mortality. A critical step is to decide the most appropriate strategy for revascularisation through percutaneous transluminal coronary angioplasty (PTCA). While a complete revascularisation (CR) treats all haemodynamically significant coronary artery lesions, an incomplete revascularisation (ICR) treats the culprit-lesion-only when MVCAD exists, leaving any untreated lesion.13 15 16 However, the main limitation is the lack of uniformity in the definition of both revascularisation strategies because there is no consensus on relevant angiographic criteria related to the functional and anatomical relevance of the coronary lesions (eg, coronary segment diameter (≥1.5 mm–≥2.5 mm), diameter stenosis (≥50%–≥70%)).17 There is greater evidence that CR is associated with reduced risk of mortality and MACE, and this magnitude of risk relates to degree of CR.18 In contrast, these observations with CR are much more limited in older patients because comorbidities progressively reduce the revascularisation benefit.19 20 Because of the lack of consensus on angiographic criteria and clinical guidelines for the coronary revascularisation strategy in older patients, the decision-making is complex, variable and open to considerable influence from human factors.13 21
Several determining factors may participate in the prognosis of older patients with MVCAD undergoing PTCA. The present study will be focused on clinical and biochemical measures associated with the dysregulation of physiological processes that is observed during ageing, which causes declining adaptive homoeostasis, low-grade inflammation and oxidative stress.7 22 Because we hypothesise that these measures are susceptible to change over time, clinical data linked to geriatric syndromes, comorbidities and MVCAD (eg, patient health records and angiographic parameters) will be analysed in combination with cardiovascular (eg, cardiac T/I troponins, NT-proBNP, soluble ST2 and CKMB) metabolic (eg, glucose, transaminases, lipoproteins and urea), inflammatory (ie, cytokines (eg, tumour necrosis factor (TNF)-α, interleukin (IL)-1β and IL-6), chemokines (eg, IL-8/CXCL8, fractalkine/CX3CL1) and others (eg, C reactive protein)) and stress oxidative (eg, reduced glutathione (GSH), oxidised glutathione (GSSG), malondialdehyde (MDA), oxidised low-density lipoprotein (LDL) and myeloperoxidase (MPO)) biomarkers.23–25 Finally, sexual dimorphism is common in the expression of these biomarkers, mainly in proinflammatory and oxidative stress biomarkers.
This study aims to evaluate changes over time of a comprehensive range of sociodemographic/anthropometric, clinical and biochemical data from older patients with MVCAD treated with coronary revascularisation through PTCA. Subsequently, relevant explanatory variables will be selected to develop a first predictive model based on MACE as primary outcome with the objective of establishing a reliable prognostic stratification for CR and ICR strategies.
There is no consensus on which revascularisation strategy is more recommendable for older patients with MVCAD because of the lack of clinical trials addressing this question. Given that a randomised controlled trial to compare outcomes of CR and ICR presents important ethical issues related to the random distribution of patients into one or another treatment group, an observational study will be of great utility to collect parameters and evaluate their validity in the prognosis of PTCA strategies in patients with MVCAD. Furthermore, a single-centre study will allow that the decision-making procedures of clinicians are uniform.
Methods and analysis
Study design
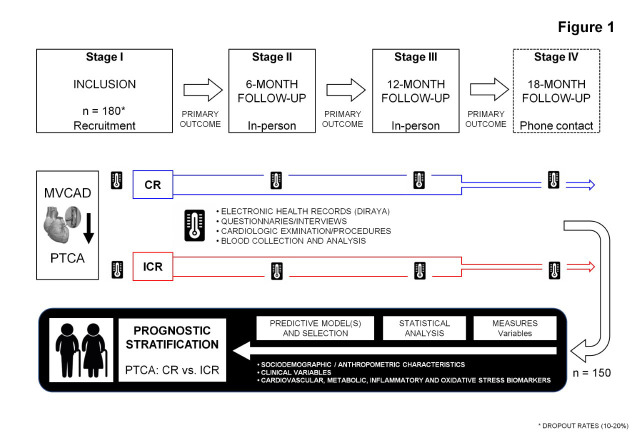
This prospective, observational, longitudinal study consists of three main in-person stages: (1) patient recruitment during the first year; (2) 6-month follow-up; and (3) 12-month follow-up. Finally, an 18-month follow-up will conclude with a phone contact to assess health status using clinical questionnaires. Participants will finish the study after a MACE or the completion of follow-ups (primary endpoints). A schematic summary is shown in figure 1.
Figure 1.
Schematic representation of the study design. CR, complete revascularisation; ICR, incomplete revascularisation; MVCAD, multivessel coronary artery disease; PTCA, percutaneous transluminal coronary angioplasty.
Participants and eligibility criteria
Participants
Eligible volunteers with MVCAD who will undergo a coronary revascularisation will be recruited from the Department of Cardiovascular Surgery and Cardiology in the Hospital Universitario Virgen de la Victoria (Málaga, Spain). The first patient was included in June 2021.
Eligibility criteria
Inclusion criteria: men and women, 70 years and older (older adults) on admission to the hospital, hospitalisation for acute coronary syndrome (NSTE-ACS and STE-ACS), diagnosis of MVACD (criteria: ≥2 coronary arteries with ≥2.0 mm segment diameter and ≥70% diameter stenosis), treatment with revascularisation using PTCA, and signed informed consent.
Exclusion criteria: life expectancy less than 1 year, refused informed consent, decisional impairment with no legally authorised representative, inability to complete questionnaires or interviews, inability to contact for follow-up or non-English/non-Spanish speaking.
Sample size and power calculation
The sample size was calculated using MACE as the primary outcome measures. Previous studies in older patients with MVCAD have revealed significant differences between CR and ICR groups in the primary outcome measures after a 12-month follow-up. Specifically, 20%–30% of MACE in the ICR group and 5%–10% of MACE in the CR group (ie, HRICR/CR=3.3).26 27 In addition, dropout rates of 10%–20% have been reported in prospective studies evaluating ischaemic heart disease.28
Considering these preceding observations, the statistical parameters that were used to calculate the sample size for two independent groups (CR and ICR) were as follows: type I error (α)=0.05, power (1−β)=0.8 and HR=3.3. The calculation revealed that the minimum number of participants for adequate study power was 138 patients, which is concordant with the historical records of older adults admitted to our hospital with coronary artery disease. Therefore, we aim to ensure a sample size of 150 older patients through the recruitment of 180 participants at the beginning of the study.
Data collection and variables
Relevant sociodemographic, anthropometric and clinical measures of the participants will be obtained through the electronic health records (DIRAYA, Servicio Andaluz de Salud—Junta de Andalucía). Clinical data related to geriatric syndromes (eg, frailty), comorbidity, disability, MVCAD and revascularisation (eg, angiographic and electrocardiographic measures) will be obtained using questionnaires, interviews and cardiological procedures. In addition, biochemical variables (eg, inflammatory biomarkers) will be obtained through different laboratory techniques such as selective ELISA and multiplex immunoassays.
Clinical questionnaires
Patients will complete various questionnaires and interviews at the baseline and follow-ups under supervision by trained and experienced staff:
The 5-item Fatigue, Resistance, Ambulation, Illness and Loss of weight scale for frailty; Charlson Comorbidity Index predicts 10-year survival in patients with multiple comorbidities; the 10-item Barthel Index measures performance in activities of daily living; the Lawton-Brody scale measures instrumental activities of daily living; the 10-item Alcohol Use Disorders Identification test for alcohol-related problems; the Pfeiffer Short Portable Mental Status Questionnaire for cognitive decline; the 36-item Short Form survey for quality of life related to health; the Global Registry of Acute Coronary Events risk score estimates admission—6-month mortality for patients with acute coronary syndrome; and the Can Rapid risk stratification of Unstable angina patients Suppress Adverse outcomes with Early implementation of the ACC/AHA guidelines bleeding score estimates major bleeding risk in patients with acute coronary syndrome.
Collection of blood samples
Blood extractions will be collected by experienced nurses at the baseline and follow-up stages. Venous blood will be extracted into two 10 mL K2 EDTA tubes (BD, Franklin Lakes, New Jersey, USA) and centrifuged at 1200×g for 10 min (4°C) to obtain plasma. Plasma samples will be aliquoted into 0.5 mL tubes and immediately encoded and stored at −80°C until biochemical determinations.
Variables
Sociodemographic and anthropometric variables (eg, age, ethnicity, sex, body mass, index, educational status, marital status, family size and socioeconomic status).
Clinical variables (eg, cardiovascular risks (eg, arterial hypertension, dyslipidaemia, smoking and chronic inflammatory diseases such as diabetes) and variables related to quality of life and geriatric syndromes (eg, frailty, comorbidity, functional and cognitive disability, polypharmacy and use of psychoactive substances)
Cardiovascular variables related to MVCAD and revascularisation (eg, acute coronary syndrome (STE-ACS and NSTE-ACS), revascularisation (CR and ICR), electrocardiographic evolution (T-waves, R-waves and ST-segment), ventricular ejection fraction, angiographic variables (eg, diameters, stenosis), SYNTAX score for evaluating the complexity of coronary artery lesions (eg, dominance, total occlusion, trifurcation, bifurcation, aorto-ostial lesion, severe tortuosity, length >20 mm, heavy calcification, thrombus and diffuse disease) and in-hospital and domiciliary care and pharmacological treatments.
Biochemical markers: (1) cardiovascular (eg, cardiac troponins (cTnT and cTnI), N-terminal prohormone of brain natriuretic peptide (NT-proBNP), soluble suppression of tumorigenicity (ST2) and creatine kinase MB isoenzyme (CKMB)); (2) metabolic (eg, glucose, transaminases, lipoproteins and urea); (3) inflammatory (ie, cytokines (eg, TNF-α, IL-1β and IL-6), chemokines (eg, IL-8/CXCL8, fractalkine/CX3CL1) and others (eg, C reactive protein)); and stress oxidative (eg, GSH and GSSG, MDA, oxidised LDL and MPO) biomarkers.
Primary outcome
The primary outcome measures will be a combination of MACE: heart failure, reinfarction, stroke, hospitalisation for cardiovascular-related illness, unscheduled revascularisation and all-cause mortality. Otherwise, older patients will complete the study to the 18-month follow-up. Severe changes in the quality of life, geriatric syndromes and disability will be examined as secondary outcome measures.
Statistical analysis
Descriptive variables will be expressed as the number and percentage of subjects (n (%)), mean and SD (mean±SD), or median and IQR. The significance of differences in categorical and continuous variables between the revascularisation groups (CR and ICR) will be determined using the χ2 test and Student’s t-test (normal distribution) or Mann-Whitney U test (non-normal distribution), respectively.
Correlation analyses between quantitative variables will be performed using the correlation coefficients of Pearson (r) and Spearman (rho) with continuous and categorical variables, respectively to determine the association and dependency between explanatory variables.
Multivariate analyses such as analyses of covariance will be performed to evaluate the main effects and interaction of dependent categorical variables (eg, revascularisation strategy and occurrence of MACE) on explanatory variables (eg, clinical and biochemical variables) while controlling covariates. Levene’s test will be used to test the homoscedasticity of the independent explanatory variables and log10-transformation will be used for positively skewed distributions.
Cox proportional-hazards models and binary logistic regression models will be constructed with independent exploratory variables as predictors of primary and secondary outcomes and/or revascularisation strategy. Receiver operating characteristics analyses will be performed to evaluate the discriminative power of these regression models through the area under the curve. A final model will include the most predictive clinical and biochemical variables to distinguish older patients with CR and ICR. The identification of these predictive variables will help with the prognostic stratification of patients with MVCAD who need a PTCA.
All statistical analyses of the database will be performed using IBM SPSS Statistics V.24 (IBM). A p value <0.05 will be considered statistically significant.
Conclusion
In summary, there have been numerous studies focused on the establishment of a prognostic stratification of patients with ischaemic heart disease who require angioplasty or percutaneous coronary revascularisation. However, these studies are inconclusive because of different factors (eg, very specific study samples, limited inclusion of parameters and exclusion of older patients with health complications). This study focuses on the elderly population, whose demand for care is increasing rapidly in parallel to the life expectancy and the high prevalence of cardiovascular diseases. This research intends to identify, characterise and integrate metabolic, inflammatory and oxidative biomarkers with clinical and cardiovascular factors in older patients taking into account sex differences. This information will contribute to improving the prognostic stratification of patients diagnosed with MVCAD who need treatment with percutaneous CR or ICR. The ultimate goal of this study is to contribute improving the welfare and quality of life of older adults in modern society.
Ethics and dissemination
Ethics
The study has been approved by the regional research ethics committee (the CEIm-Provincial de Málaga and the Portal de Ética de la Investigación Biomédica de Andalucía-PEIBA) (Id. PI0131/2020) in accordance with the Ethical Principles for Medical Research Involving Human Subjects adopted in the Declaration of Helsinki by the World Medical Association (64th WMA General Assembly, Fortaleza, Brazil, October 2013) and the Regulation (EU) 2016/679 of the European Parliament and of the Council 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data (General Data Protection Regulation). In Spain, the Law 41/2002 on regulating patient autonomy and rights and obligations regarding clinical information and documentation; and the Organic Law 3/2018 on the protection of personal data and guarantee of digital rights. Written informed consents were obtained from each participant after a complete description of the study. All the participants will have the opportunity to discuss any questions or issues. All collected data and samples will be registered and stored with alphanumeric codes in order to maintain privacy and confidentiality.
Dissemination
The proposed study is based on two issues that are of special interest to society, but also to the scientific community: Aging and Heart Disease. The results will be disseminated in international peer-reviewed journals, presented at conferences in Cardiology and Gerontology, and sent to participants, medical and health service managers, clinicians and other researchers. Additional activities will contribute to the divulgation of relevant results in social networks and education/research institution websites (Universidad de Málaga (https://www.uma.es); CIBERCV (https://www.cibercv.es); IBIMA (http://www.ibima.eu) and Hospital Universitario Virgen de la Victoria (http://www.huvv.es).
Supplementary Material
Acknowledgments
This study has received support for the statistical approaches from the Cátedra de Terapias Avanzadas en Patología Cardiovascular (The subject of Advanced Therapies in Cardiovascular Pathologies. CIF Q-2918001-E.) of the Universidad de Málaga. We thank José Herrera Jiménez for his help in the biochemical determinations.
Footnotes
Contributors: The study concept and design was conceived by FJP-M and MJ-N. Patient recruitment process and collection of clinical data are performed by ADMC-S, MVD-A, VMB-M, JR-C and AIM-R. Angiographic data are collected by FS-P, MA-G, LG-R and LP-M. Questionnaires and interviews are designed and applied by ADMC-S and MF-L. Biochemical determinations in blood samples are performed by FJP-M, MJS-Q, DM-V and REB. Statistical analyses are conducted by VMB-M, JMM-A, FJP-M and MJ-N. ADMC-S prepared the first draft of the manuscript. All authors critically read, edited and approved the final manuscript and approved the submitted version.
Funding: This study has received funding from the following grants: PI-131/2020 funded by the Consejería de Salud y Familias—Junta de Andalucía and European Regional Development Funds/European Social Fund (ERDF/ESF); and UMA-20-FEDERJA-074 funded by the Universidad de Málaga, Consejería de Economía, Conocimiento, Empresas y Universidad—Junta de Andalucía and ERDF/ESF. This study is also supported by the Servicio Andaluz de Salud (Consejería de Salud y Familias—Junta de Andalucía) and the Fundación Andaluza de Cardiología.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.World Health Organization . WHO global health estimates. leading causes of death and disability 2000-2019. Available: https://wwwwhoint/data/global-health-estimates
- 2.Instituto Nacional de Estadística . Madrid, 2020. Available: https://wwwinees/dyngs/INEbase/es/categoriahtm?c=Estadistica_P&cid=1254734710984
- 3.Murad K, Kitzman DW. Frailty and multiple comorbidities in the elderly patient with heart failure: implications for management. Heart Fail Rev 2012;17:581–8. 10.1007/s10741-011-9258-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Madhavan MV, Gersh BJ, Alexander KP, et al. Coronary Artery Disease in Patients ≥80 Years of Age. J Am Coll Cardiol 2018;71:2015–40. 10.1016/j.jacc.2017.12.068 [DOI] [PubMed] [Google Scholar]
- 5.Inouye SK, Studenski S, Tinetti ME, et al. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc 2007;55:780–91. 10.1111/j.1532-5415.2007.01156.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schöttker B, Saum K-U, Jansen EHJM, et al. Associations of metabolic, inflammatory and oxidative stress markers with total morbidity and multi-morbidity in a large cohort of older German adults. Age Ageing 2016;45:127–35. 10.1093/ageing/afv159 [DOI] [PubMed] [Google Scholar]
- 7.Wu J, Xia S, Kalionis B, et al. The role of oxidative stress and inflammation in cardiovascular aging. Biomed Res Int 2014;2014:615312. 10.1155/2014/615312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steven S, Frenis K, Oelze M, et al. Vascular inflammation and oxidative stress: major triggers for cardiovascular disease. Oxid Med Cell Longev 2019;2019:7092151. 10.1155/2019/7092151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dai X, Busby-Whitehead J, Alexander KP. Acute coronary syndrome in the older adults. J Geriatr Cardiol 2016;13:101–8. 10.11909/j.issn.1671-5411.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hwang SY, Park EH, Shin ES, et al. Comparison of factors associated with atypical symptoms in younger and older patients with acute coronary syndromes. J Korean Med Sci 2009;24:789–94. 10.3346/jkms.2009.24.5.789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tavares CAM, Samesima N, Lazar Neto F, et al. Usefulness of ECG criteria to rule out left ventricular hypertrophy in older individuals with true left bundle branch block: an observational study. BMC Cardiovasc Disord 2021;21:547. 10.1186/s12872-021-02332-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zannad F, Huvelle E, Dickstein K, et al. Left bundle branch block as a risk factor for progression to heart failure. Eur J Heart Fail 2007;9:7–14. 10.1016/j.ejheart.2006.04.011 [DOI] [PubMed] [Google Scholar]
- 13.Wang TY, McCoy LA, Bhatt DL, et al. Multivessel vs culprit-only percutaneous coronary intervention among patients 65 years or older with acute myocardial infarction. Am Heart J 2016;172:9–18. 10.1016/j.ahj.2015.10.017 [DOI] [PubMed] [Google Scholar]
- 14.Cano-García M, Millán-Gómez M, Sánchez-González C, et al. Impact of percutaneous coronary revascularization of severe coronary lesions on secondary branches. Rev Esp Cardiol 2019;72:456–65. 10.1016/j.rec.2018.04.011 [DOI] [PubMed] [Google Scholar]
- 15.Gaba P, Gersh BJ, Ali ZA, et al. Complete versus incomplete coronary revascularization: definitions, assessment and outcomes. Nat Rev Cardiol 2021;18:155–68. 10.1038/s41569-020-00457-5 [DOI] [PubMed] [Google Scholar]
- 16.Zimarino M, Calafiore AM, De Caterina R. Complete myocardial revascularization: between myth and reality. Eur Heart J 2005;26:1824–30. 10.1093/eurheartj/ehi249 [DOI] [PubMed] [Google Scholar]
- 17.Shannon J, Colombo A. Revascularization in multivessel CAD: a functional approach. Nat Rev Cardiol 2012;9:243–52. 10.1038/nrcardio.2011.213 [DOI] [PubMed] [Google Scholar]
- 18.Nagaraja V, Ooi S-Y, Nolan J, et al. Impact of incomplete percutaneous revascularization in patients with Multivessel coronary artery disease: a systematic review and meta-analysis. J Am Heart Assoc 2016;5. 10.1161/JAHA.116.004598. [Epub ahead of print: 16 12 2016]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanchis J, García Acuña JM, Raposeiras S, et al. Comorbidity burden and revascularization benefit in elderly patients with acute coronary syndrome. Rev Esp Cardiol 2021;74:765–72. 10.1016/j.rec.2020.06.015 [DOI] [PubMed] [Google Scholar]
- 20.Girerd N, Magne J, Rabilloud M, et al. The impact of complete revascularization on long-term survival is strongly dependent on age. Ann Thorac Surg 2012;94:1166–72. 10.1016/j.athoracsur.2012.05.023 [DOI] [PubMed] [Google Scholar]
- 21.Ando T, Takagi H, Grines CL. Complete versus incomplete revascularization with drug-eluting stents for multi-vessel disease in stable, unstable angina or non-ST-segment elevation myocardial infarction: a meta-analysis. J Interv Cardiol 2017;30:309–17. 10.1111/joic.12390 [DOI] [PubMed] [Google Scholar]
- 22.Pomatto LCD, Davies KJA. The role of declining adaptive homeostasis in ageing. J Physiol 2017;595:7275–309. 10.1113/JP275072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liguori I, Russo G, Curcio F, et al. Oxidative stress, aging, and diseases. Clin Interv Aging 2018;13:757–72. 10.2147/CIA.S158513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dhingra R, Vasan RS. Biomarkers in cardiovascular disease: statistical assessment and section on key novel heart failure biomarkers. Trends Cardiovasc Med 2017;27:123–33. 10.1016/j.tcm.2016.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soysal P, Stubbs B, Lucato P, et al. Inflammation and frailty in the elderly: a systematic review and meta-analysis. Ageing Res Rev 2016;31:1–8. 10.1016/j.arr.2016.08.006 [DOI] [PubMed] [Google Scholar]
- 26.Harada M, Miura T, Kobayashi T, et al. Clinical impact of complete revascularization in elderly patients with multi-vessel coronary artery disease undergoing percutaneous coronary intervention: a sub-analysis of the SHINANO registry. Int J Cardiol 2017;230:413–9. 10.1016/j.ijcard.2016.12.093 [DOI] [PubMed] [Google Scholar]
- 27.Berezhnoi K, Kokov L, Vanyukov A. Effects of complete revascularization on long-term treatment outcomes in patients with multivessel coronary artery disease over 80 years of age admitted for acute coronary syndrome. Cardiovasc Diagn Ther 2019;9:301–9. 10.21037/cdt.2018.12.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stocks NP, Broadbent JL, Lorimer MF, et al. The Heart Health Study - increasing cardiovascular risk assessment in family practice for first degree relatives of patients with premature ischaemic heart disease: a randomised controlled trial. BMC Fam Pract 2015;16:116. 10.1186/s12875-015-0328-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.