Abstract
Background:
Patterns of food security persistently vary by race, yet limited research has examined how community-specific experiences of race and racism are associated with nutritional outcomes.
Objectives:
This analysis describes a novel approach for classifying experiences of race and racism and explores the relationship between identified classes and measures of food security and diet quality.
Methods:
Cross-sectional self-reported survey data from 306 African American adults living in two urban midwestern cities were collected in 2017–18. Measures of racialized experiences assessed consciousness of race, perceived discrimination, and health effects of perceived discrimination. Food security was measured with a 6-item screener and diet quality with the Healthy Eating Index-2010. Latent class analysis was used to generate racialized classes. Bivariate analyses were conducted to examine differences in class membership by sociodemographics and nutrition outcomes.
Results:
Participants were majority women who were receiving Supplemental Nutrition Assistance Program benefits. Three racialized classes were identified: Class 1 reported few racialized experiences (42.8% of the sample), Class 2 was racially conscious with few experiences of discrimination (45.1%), and Class 3 was both racially conscious and affected by racialized actions (12.1%). Racialized classes were significantly different in mean household income, level of education, home ownership, and job loss in the past year. Class 3 was the least represented among those that were food secure and the most represented among those that were very low food secure. There were no differences by class in Healthy Eating Index-2010 scores.
Discussion:
Findings offer an innovative method for measuring exposures to racism and for assessing its relationship to food security. Findings highlight heterogeneity of racialized experiences in similar contexts as well as potential root cause targets such as wages, education, home ownership, and employment that may be modulated to mitigate the effects of racism on food insecurity.
Keywords: Social determinant of health, Food security, Racism, Health equity
Racism is an underlying problem structuring population health in the US (Johnson-Agbakwu et al., 2020; Poteat et al., 2020) and this point has been formally recognized in statements issued by national professional organizations as well as over 150 cities, counties, and states across the country (Krisberg, 2021; Serchen et al., 2020; Trent et al., 2019) The COVID-19 pandemic beginning in 2020, further highlighted links between racialized social factors, or social determinants of health (SDH)—such as crowded housing, transportation limitations, workforce characteristics—and racial inequities in COVID-19 cases, hospitalizations, and death (Figueroa et al., 2020; Maness et al., 2021; Ogojiaku et al., 2020).
Negative experiences of race and racism have been linked to an array of physical and mental health conditions and disparities (Paradies et al., 2015). These experiences influence public health though diverse pathways that range from personal experiences of discrimination to societal-level socioeconomic deprivations associated with systemic disinvestment in schools and housing (Williams & Mohammed, 2013). These exposures may be directly associated with health or health care (e.g., poor access to high quality healthcare, violence victimization) or may indirectly affect health due to cumulative physiological short-term stress, chronic stress, and trauma (Williams & Mohammed, 2009).
Measuring experiences of racism and how they influence health is challenging due to the lack of gold standard measures. A systematic review conducted over a decade ago identified 34 racism experience measurement tools with varying lengths and degrees of specificity (Kressin et al., 2008). This plethora of tools makes it difficult to compare results across studies. Beyond this methodologic issue, the contextual nature of occurrences of racism raises the possibility that similar racialized experiences could yield differential results due to within community characteristics, even when using standardized tools. The use of a data driven approach to measurement of racialized experiences, rather than one of the available standardized questionnaires, retains comparability limitations but it may offer a more nuanced approach for understanding heterogeneity of racialized experiences within communities.
Food insecurity is an exemplar SDH with known racial inequities and a strong linkage to community context for which a data-driven approach to measuring racism could be applied. Its significance now is greater than ever given rising rates of food insecurity due to the economic downturn resulting from the COVID-19 pandemic (Wolfson & Leung, 2020). Food insecurity is defined as the disruption of food intake or eating patterns because of lack of money and other resources (Nord et al., 2005). In 2019, 10.5% of Americans experienced food insecurity, yet for non-Hispanic Blacks, this rate was nearly double (19.1%) (Coleman-Jensen et al., 2020). Food insecurity limits the opportunity for healthy eating. and is thus associated with diet-related health conditions with known racial inequities (Gundersen & Ziliak, 2015). The food environment, transportation barriers, poverty, and safety-net policies are among the underlying causes of food insecurity (Raskind, 2020), however, the fact that racial inequities continue to exist after controlling for these factors suggests that racism is also a factor. To date, research on this relationship has been limited (Koh et al., 2020).
The foundational nature of food insecurity and healthy eating structuring multiple health disparities sets it as a target for cross-cutting interventions that enhance health broadly. Understanding how community specific experiences of race are associated with food insecurity could assist with the design of responsive food security interventions in minority communities. This analysis describes a novel approach for classifying experiences of race and racism and explores the relationship between identified classes and measures of food security and diet quality among African Americans in two urban midwestern cities. Specifically, we attempt to answer two research questions: 1) Can latent classes of racialized experiences be extracted from racism-related questions included in a community-based survey of food security? and 2) If so, are these classes predictive of food security and diet quality.
Methods
Study Area and Approach
These analyses are derived from cross-sectional data collected in 2017–18 from residents living in two urban communities in Cleveland and Columbus, Ohio, USA that had comparable racial and economic composition and access to healthy food retailers. Data are part of a broader longitudinal study with baseline data collected in 2015–16 (Freedman et al., 2020). Participants were recruited from contiguous census tracts in each community. Most of the census tracts within each community (5 of 7 tracts in Cleveland, 4 of 4 tracts in Columbus) were defined as low-income and low healthy food access per U.S. Department of Agriculture guidelines (Economic Research Service, 2016), and identified as areas in Ohio in greatest need of food environment interventions (Tucker et al., 2014). Additionally, community selection focused on areas with high rates of receipt of Supplemental Nutrition Assistance Program (SNAP) benefits and non-Hispanic Black populations based on five-year (2011–2015) American Community Survey estimates (U.S. Census Bureau, 2016).
A community-based recruitment approach was used to identify, screen, and enroll potential participants from August 2015 to July 2016 using mailings, flyers, public presentations, and word-of-mouth. Eligibility criteria included: at least 18 years old, English speaking, living in targeted census tracts, plan to live in current neighborhood at least 12 months, and responsible for more than half of household food shopping. Study enrollment was limited to one person per household. At baseline a total of 516 participants enrolled in the study and 442 (85.7%) participated in 2017–18 data collection. All participants provided written or verbal (over the phone) informed consent.
Data Collection
The study was reviewed and approved by the Institutional Review Board. Data were collected using closed-ended phone-based surveys administered by trained research assistants that took about 60 minutes to complete. Data collection for each participant involved three phone surveys during a 37-day timeframe. All three calls included a 24-hour dietary recall. Additionally, the first call included a psychosocial survey. Prior to their phone surveys, each participant received materials to support data collection (e.g., food amounts booklet with standardized information about reporting portion sizes, response options for Likert scales). Participants were compensated $35 after calls 1 and 2 and $40 after call 3.
Measures of Racialized Experiences
The survey included four questions that were used to create classes of racialized experiences - consciousness of race, perceived discrimination by service providers, and health effects (physical and mental) from perceived discrimination. Three were directly from and one was adapted from the Behavioral Risk Factor Surveillance System (Center for Disease Control and Prevention, 2012).
Consciousness of Race
We assessed participants’ consciousness of race with a single item, “How often do you think about your race?” The response options were never, once a year, once a month, once a day, once an hour, constantly, don’t know/not sure. We recoded responses into three binary variables: rarely think about race (i.e., those who responded never or once a year), occasionally think about race (i.e., those who responded once a month or once a day) and often think about race (i.e., those who responded once a day, once an hour, and constantly). We included rarely think about race and often think about race in the latent class analysis.
Perceived Discrimination
We assessed participants’ experiences with discrimination for two domains related to service providers - health care and food shopping. The questions asked: “Within the past 12 months, when seeking health care [change to ‘when shopping for food for your household’], do you feel your experiences were worse than, the same as, or better than people of other races?” The response options included worse than other races; same as other races; better than some races, worse than some races; better than others; and only encountered people of the same race. We used these two items to create one variable, experienced discrimination from service providers where persons who indicated being treated “worse than other races” or “worse than some races, better than others” when seeking health care and/or food shopping were coded as 1, all other responses were coded as 0. This item was included in the latent class analysis.
Health Effects of Perceived Discrimination
Health effects of perceived discrimination were assessed using two items with response options yes, no, or don’t know. Physical health effects from perceived discrimination were assessed with the question: “Within the past 30 days, have you experienced any physical symptoms, for example, headache, an upset stomach, tensing of your muscles, or a pounding heart, as a result of how you were treated based on your race?” Mental health effects from perceived discrimination were assessed with the question: “Within the past 30 days, have you felt emotionally upset, for example angry, sad, or frustrated, as a result of how you were treated based on your race?” Persons who responded yes were coded as 1 for each of the questions, those we responded no or don’t know were coded as zero. Both variables, physical health effects and mental health effects from perceived discrimination, were included in the latent class analysis.
Nutrition Outcome Variables
Two nutritional outcomes, food security and diet quality, were examined by racialized classes. Food security status was classified based on the USDA’s Six Item Food Security Short Form (Blumberg et al., 1999). Participants were asked to answer questions based on their experiences in the last 12 months. Responses of “often” or “sometimes”; “yes”; and “almost every month” or “some months but not every month” were coded as affirmative, and the sum of affirmative responses were translated into a scaled score (0–6). A score of 0–1 represented food security, 2–4 represented low food security (LFS), and 5–6 represent very low food security (VLFS) (Blumberg et al., 1999).
Overall diet quality was assessed using the Healthy Eating Index (HEI-2010), a measure of diet quality based on conformity to 2010 dietary guidelines (Guenther et al., 2013; U.S. Department of Health and Human Services, 2010). HEI-2010 scores were calculated based on data collected and processed using the Nutrition Data System for Research software version 2014, a standardized and comprehensive 24-hour dietary recall method developed by the Nutrition Coordinating Center (NCC), University of Minnesota, Minneapolis, MN (Schakel et al., 1988; Schakel, 2001; Schakel et al., 1997). Three dietary recalls per person were collected, reflecting two nonconsecutive weekday and one weekend day within a 37-day window to limit within subject seasonal variability (Locke et al., 2009; MA et al., 2009; Ziegler et al., 1987). HEI-2010 scores were calculated based on the average of three 24-hour dietary recalls with higher average scores (maximum=100) indicating greater adherence to dietary guidelines.
Personal Characteristics
Socio-demographics were measured based on self-report using questions adapted from the Behavioral Risk Factor Surveillance System (Center for Disease Control and Prevention, 2014). Questions assessed race, sex, age, level of education, annual household income, receipt of Supplemental Nutrition Assistance Program (SNAP) benefits in the past 12 months, employment status, home ownership, and self-reported chronic disease such as high blood pressure, heart disease, diabetes, obesity, and asthma. One item assessed timing of last visit to a health care provider for a routine visit using the question: “About how long has it been since you last visited a doctor for a routine check-up? A routine check-up is a general physical exam, not an exam for a specific injury, illness, or condition” (Center for Disease Control and Prevention, 2015). Response options were within the past year, within the past 2 years, within the past 5 years, 5 or more years ago, never, or don’t know/not sure. Four self-developed items assessed negative life events over the past year including personal injury or illness, job loss or difficulty finding a job, legal troubles, and victim of a crime or witnessed violence. Participants were asked to respond yes or no if they experienced these events within the past 12 months.
Statistical Analysis
All analyses were limited to African American participants (n = 306). Missing data were examined and no patterns were noted, therefore listwise deletion was used (Cheema, 2014). Descriptive statistics were calculated for the study sample characteristics. Next, in order to examine patterns of racialized experiences, we conducted a latent class analysis (LCA) using Mplus 7. Specifically, the LCA was estimated using the five variables previously described in the measures of racialized experience section of the paper - rarely think about race, often think about race, experienced discrimination from service providers, and physical and mental health effects from perceived discrimination.
We employed LCA because unlike traditional statistical procedures that are variable-centered (e.g., t-test, ANOVA, regression) and focused on how variables, or characteristics of people are related, LCA is a person-centered analytic procedure that examines how variables group within people (i.e., LCA allows us to identify unobservable subgroups within a population). To establish the optimal number of latent classes, we will consider the following model fit criteria: Akaike information criteria (AIC), Bayesian information criterion (BIC), Sample Size-Adjusted BIC (SSABIC). the Entropy Index, and the Lo-Mendell-Rubin Likelihood Ratio Test (LMR-LRT) test. We will examine and compare improvement in model fit between the n versus n-1 models. The information criteria and the likelihood ratio test will be assessed to indicate goodness of fit of different latent class models, with the best model indicating the lowest AIC and BIC values and a p-value greater than .05 for the LMR-LRT. Practical meanings and interpretation of the identified classes were also used as criteria for model selection.
After identifying the latent classes, we conducted bivariate analyses to examine if there were socio-demographics differences in class membership and nutritional outcomes. Chi-square test of independence was used for binary variables and one-way ANOVA was used for continuous variables. To better understand the relationship between class membership and our dietary outcomes, when the results from the chi-square test of independence or one-way ANOVA revealed statistically significant differences between classes and our nutritional outcome, we conducted post-hoc pairwise comparisons. Statistical significance was established at p<.05.
Results
As shown in Table 1, the majority of the study sample were female (74.84%) with limited income. About two-thirds (62.4%) were either currently receiving SNAP benefits or received benefits in the past 12 months. About one-third (35.4%) were employed for wages and 33.0% were unable to work. Almost half of the study population had completed 12th grade or had a high school diploma. Nearly two-thirds were food secure (61.8%). Overall, participants had poor diet quality with a mean HEI-2010 score of 49.9 out of 100.
Table 1.
Sample characteristics of African American participants from two urban midwestern cities (N=306)
| % or Mean (STD, Min, Max) | |
|---|---|
| Demographics | |
| Study Community: Cleveland | 55.2 |
| Female | 74.8 |
| Age (years) | 51.4 (12.91, 21, 91) |
| Annual Household Income ($) | 18,609 (15,677, 0, 96,000) |
| Receives SNAP | 62.4 |
| Owns Home | 23.5 |
| Employment | |
| Employed for wages | 35.3 |
| Self-employed | 2.6 |
| Out of work for 1 or more years | 5.9 |
| Out of work less than 1 year | 8.2 |
| Homemaker | 3.9 |
| Retired | 11.1 |
| Unable to work | 33.0 |
| Education | |
| Grades 1 −8 | 1.6 |
| Grades 9–11 | 19.0 |
| Grade 12 or GED | 47.2 |
| College 1 year to 3 years | 24.9 |
| College 4 years or more | 6.2 |
| Post-graduate degree | 1.0 |
| Self-reported Racialized Experiences | |
| Rarely Thinks About Race | 44.1 |
| Often Thinks About Race | 38.2 |
| Experienced Discrimination by Service Provider(s) | 16.5 |
| Physical Health Effects from Perceived Discrimination | 9.5 |
| Mental Health Effects from Perceived Discrimination | 19.3 |
| Food Security and Diet Quality | |
| Food Secure | 61.8 |
| Low Food Security | 23.9 |
| Very Low Food Security | 14.4 |
| Healthy Eating Index 2010 Score | 49.9 (9.7, 24, 84) |
Racialized experiences varied among the sample population spanning from participants who rarely thought about their race to others that had experienced racial discrimination by service providers. Just under half of the sample (44.1%) indicated they rarely think about their race and 38% reported that they often think about their race. Overall, 16.5% had experienced racial discrimination from a service provider in healthcare or at a grocery store (See Table 1). Nearly one in five (19.3%) reported mental health effects and 9.5% reported experiencing physical symptoms as a result of how they were treated because of their race.
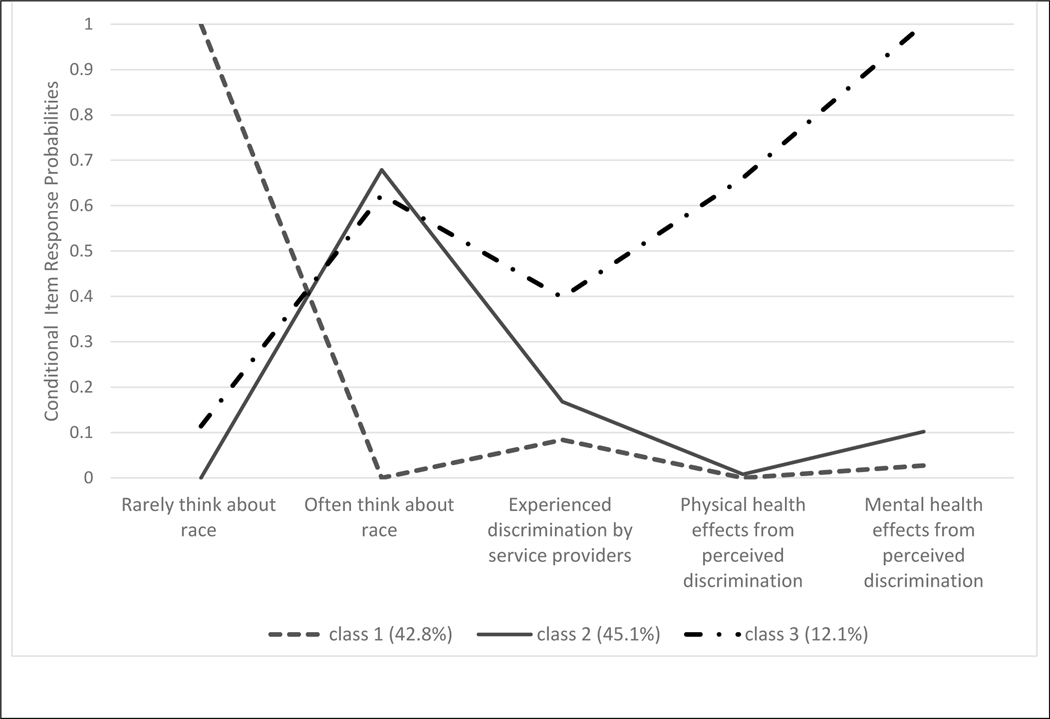
As shown in Table 2, the three-class solution was the best fitting model. Figure 1 contains details on the defining characteristics of the three classes. Class 1 represented 42.8% of the sample; it is defined as reporting few racialized experiences. This group includes African Americans who rarely report all three of the following: (a) thinking about their race, (b) experiencing physical or mental health effects based on how they are treated because of their race, and (c) experiencing discrimination from service providers. Class 2 represented 45.1% of the sample and is defined as being racially conscious. African American participants in class 2 differ from those in class 1 in terms of how often they report thinking about their race. In class 2, the majority reported they often think about their race. However, like class 1, the majority in class 2 do not report experiencing emotional and physical responses to how they are treated and most do not report experiencing discrimination from health care and retail food service providers. Class 3 is the smallest representing 12.1% of the sample and is defined as being both racially conscious and affected by racialized actions. African Americans in class 3 reported the highest levels of discrimination from a service provider and experiencing physical and mental health effects because of their race.
Table 2.
Results from latent class analysis for establishing three racialized classes among African Americans in two urban midwestern cities (N=306).
| Model (Number of latent classes)* | Loglikelihood | Best H0 replicated (Yes/No) | # of parameters | AIC | BIC | SSABIC | LMR-LRT (p) | Entropy | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | −792.4 | yes | 5 | 1594.7 | 1613.4 | 1597.5 | -- | -- | |
| 2 | −655.8 | yes | 11 | 1353.5 | 1384.5 | 1359.6 | <.0001 | .87 | |
| 3 | −627.7 | yes | 17 | 1289.4 | 1352.7 | 1298.8 | <.0001 | .94 | |
| 4 | −617.6 | yes | 23 | 1281.2 | 1366.9 | 1293.9 | .0012 | .95 |
Note: SSABIC = sample size adjusted BIC; LMR-LRT = Vuong-Lo-Mendal-Rubin Likelihood Ratio Test comparing current model with a model with one less latent profile.
Even though the measures of model fit suggest that a 4-class solution was better than a 3-class solution, we selected the 3-class model as our best model because in the 4-class model two of the classes contained less than 10% of the sample, thus making that model a less desirable solution.
Figure 1. Three classes of racialized experiences among African Americans in two urban midwestern cities.
Note: Class 1 = few racialized expereinces, Class 2 = racially concious, Class 3 = racially concious and affected.
As shown in Table 3, the classes were not significantly different based on several factors including gender, age, employment, receipt of SNAP, chronic disease status, medical checkup in the past year, and several stressful life events. Class 1, characterized as having few racialized experiences, had the lowest income and least education. Class 2, characterized as being more racially conscious, had the highest income and level of education. Class 3, characterized as being both racially conscious and affected by racialized actions, had the smallest percent of homeownership and the highest present reporting job loss in the past year.
Table 3.
Characteristics of racialized classes among African Americans in two midwestern urban neighborhoods (N=306).
| Class 1 Few Racialized Experiences (n = 131) | Class 2 Racially Conscious (n = 138) | Class 3 Racially Conscious and Affected (n = 37) | p-value | |
|---|---|---|---|---|
| Female | 82 | 69 | 73 | .0508 |
| Age (years) | 51.36 | 51.91 | 49.71 | .6522 |
| Household Income, $ | 15,782 (12,379) | 21,172 (17,952) | 19,049 (15,742) | .0186 |
| Employed for Wages | 39 | 36 | 43 | .6559 |
| Receives SNAP | 69 | 57 | 62 | .1193 |
| More than High School Education | 22 | 41 | 35 | .0048 |
| Owns Home | 23 | 28 | 8 | .0362 |
| Self-reported Chronic Disease* | 52 | 62 | 69 | .1006 |
| Had Medical Checkup in Past Year | 76 | 85 | 76 | .1827 |
| Stressful Life Events in Past Year | ||||
| Personal Injury/Illness | 27 | 33 | 49 | .0520 |
| Job Loss | 14 | 23 | 49 | .0001 |
| Legal Troubles | 6 | 7 | 16 | .1003 |
| Victim or Witness a Crime | 6 | 12 | 16 | .1023 |
| Food Secure | 47 | 47 | 6 | .0001 |
| Low Food Secure | 38 | 47 | 15 | .5506 |
| Very Low Food Secure | 32 | 34 | 34 | .0001 |
| Healthy Eating Index - 2010 | 49.48 (8.82) | 50.82 (10.36) | 47.55 (9.65) | .1591 |
Notes. Values for categorical variables represent percentages. Values for continuous variables are the mean and standard deviation. p-values for categorical variables are from Chi-Square analysis and one-way ANOVA for continuous variables. Alpha set at .05.
Self-reported high blood pressure, heart disease, diabetes, obesity, hyperlipemia, asthma, cancer, and kidney disease.
From the post-hoc pairwise comparisons for food secure persons and class membership we found that the proportion of food secure people in Class 3 (.30) was significantly lower than Class 1 (.68) and 2 (.64; Class 3 vs 1: χ2 (1, 168) = 17.48, p =.0001; Class 3 vs. 2: χ2 (1, 175) = 14.49, p =.0001; Class 2 vs. 1: χ2 (1,269) = 0.3565, p=.55041). Conversely, the proportion of very low food secure people in Class 3 (.41) was significantly greater than those in Class 1 (.11) and Class 2 (.11; Class 3 vs 1: χ2 (1,168) = 18.00, p=..0001; Class 3 vs. 2: χ2 (1,175) = 18.08, p=..0001; Class 2 vs. 1: χ2 (1,269) = 0.0023, p=.9615). Class 3 was the least represented among those that were food secure and the most represented among those that were very low food secure. There were no differences by class in HEI-2010.
Discussion
This analysis demonstrated that three distinct racialized experiences could be extracted as latent classes from survey data among African Americans living in two urban communities in the Midwest characterized as being low income with low access to stores carrying healthy foods. The classes included one with low consciousness of race and few experiences of racism and its effects (Class 1), one with high consciousness of race yet few experiences of racism and its effects (Class 2), and one with high consciousness of race and high experiences of racism and its effects (Class 3).
In addition to having different racialized experiences, these classes had different experiences of food security although no differences in diet quality. Class 3 was most affected by racialized experiences—physically, emotionally, and through routine actions—and was significantly more likely to have very low food security compared to the two other racialized classes. This finding is important because Class 3 had higher mean household income compared to Class 2, and income is one of the primary factors defining food security status (Nord et al., 2005). Class 3 was more likely to report job loss in the past year that may have created income instability. Furthermore, our findings differentiated African Americans with high (Class 2) and low consciousness (Class 1) of race. Africans who were more conscious of their race with few experiences of racism and its effects had higher income and more education compared to those less conscious of their race. This is consistent with research showing that exposure to diversity in higher education and workplaces further the development of racial identity (Neville & Cross, 2017). Experiences of food insecurity were, however, similar for these two classes.
Despite persistent racialized patterning of food insecurity in the United States (Odoms-Young, 2018), limited research has examined the role of discrimination and racism as an underlying mechanism structuring food insecurity. Our findings build on three cross-sectional studies that examined the relationship between experiences of discrimination and food insecurity. These prior studies found increasing levels of exposure to discrimination was associated with increased odds or frequency of food insecurity (Burke et al., 2018; Larson et al., 2020; Phojanakong et al., 2019).
This illuminates complexity of experiences among African Americans and the potential mechanisms by which racism structures opportunity. Notably, the racialized classes found in our study were significantly different in four SDH factors including mean household income, level of education, home ownership, and job loss in the past year. These represent potential pathways through which racism structures food security. Furthermore, we found some differences in the three racialized classes by study site indicating broader contextual factors such as historical practices and contemporary policies that may shape collective experiences of racism. Our findings affirm other research suggesting potential levers for reducing racialized patterns of food insecurity may include growth in livable-wage job security for African Americans and dismantling discrimination in educational and housing sectors (Odoms-Young, 2018). Evaluation of these types of upstream interventions, which may require long-term assessment, are warranted especially in racialized contexts that have a history of purposeful disinvestment.
Given that racism is a structuring force that influences many outcomes (Powell, 2008), future research is warranted to examine how racialized experiences help us understand variability in other health outcomes. Existing scales measure experiences of racism, perceptions of racism, and stress associated with racism (Bastos et al., 2010). Our approach attempted to identify latent classes that captured a gestalt of these factors within a specific set of communities. Additional research is needed in a larger, more heterogeneous population to determine whether the classes found in this analysis could be replicated and whether different relationships would be found. Qualitative research may be used to further unpack the meaning of racialized experiences while quantitative research may allow for comparison of responses across heterogenous groups. Methods that examine spatial and temporal patterning of experiences of racism as well as social network characteristics associated with racialized experiences will add context to these experiences. Finally, this new line of research may investigate other factors structuring diet quality among African Americans that were not captured in the current classifications of racialized experiences.
Conclusion
This research offers an example of an innovative method for measuring exposures to racism and for assessing its relationship to food security—an important SDH. We note that these results are not generalizable because of the highly localized sample. We, however, believe that this is a feature rather than a limitation. It allows for a process that accounts for the contexts in which racialized experiences occur. It recognizes the uniqueness of racial experiences and the associated outcomes in a way that allows for localized solutions.
Acknowledgement
This research was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK108184), Foundation for Food and Agriculture Research (560290), Michael & Susan Dell Foundation (no grant number), National Dairy Council (2923), The Center for Child Health Equity and Outcomes Research, Nationwide Children’s Hospital (no grant number), and National Center for Advancing Translational Science (UL1TR002548). Some of the funders were provided updates but none of the funders had a role in study design; collection, analysis, or interpretation of data; writing the report; or the decision to submit the report for publication. The views presented here do not represent those of the National Institutes of Health.
The study was reviewed and approved by the Institutional Review Board at Nationwide Children’s Hosptial.
Contributor Information
Deena J. Chisolm, Department of Pediatrics, The Ohio State University College of Medicine, Columbus, and Abigail Wexner Research Institute, Nationwide Children’s Hospital, Columbus, Ohio..
Bethany A. Bell, Department Chair, Educational Leadership, Foundations, and Policy Department, University of Virginia School of Education and Human Development, Charlottesville, VA..
Owusua Yamoah, Mary Ann Swetland Center for Environmental Health, Case Western Reserve University School of Medicine, Cleveland, Ohio..
Darcy A. Freedman, Mary Ann Swetland Center for Environmental Health and Department of Population and Quantitative Health Sciences, Case Western Reserve University School of Medicine, Cleveland, Ohio.
References
- Bastos JL, Celeste RK, Faerstein E, & Barros AJD (2010). Racial discrimination and health: A systematic review of scales with a focus on their psychometric properties. Social Science Medicine, 70, 1091–1099. 10.1016/j.socscimed.2009.12.020 [DOI] [PubMed] [Google Scholar]
- Blumberg SJ, Bialostosky K, Hamilton WL, & Briefel RR (1999). The effectiveness of a short form of the Household Food Security Scale. American Journal of Public Health, 89, 1231–1234. 10.2105/AJPH.89.8.1231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke MP, Jones SJ, Frongillo EA, Fram MS, Blake CE, & Freedman DA (2018). Severity of household food insecurity and lifetime racial discrimination among African-American households in South Carolina. Ethnicity & Health, 23, 276–292. 10.1080/13557858.2016.1263286 [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. (2012). 2013 Behavioral Risk Factor Surveillance System Questionnaire. https://www.cdc.gov/brfss/questionnaires/pdf-ques/2013-BRFSS_English.pdf
- Center for Disease Control and Prevention. (2014). 2015 Behavioral Risk Factor Surveillance System Questionnaire (p. 79). https://www.cdc.gov/brfss/questionnaires/pdf-ques/2015-brfss-questionnaire-12-29-14.pdf
- Center for Disease Control and Prevention. (2015). 2016 Behavioral Risk Factor Surveillance System Questionnaire. https://www.cdc.gov/brfss/questionnaires/pdf-ques/2015-brfss-questionnaire-12-29-14.pdf
- Cheema J. (2014). Some General Guidelines for Choosing Missing Data Handling Methods in Educational Research. Journal of Modern Applied Statistical Methods, 13(2). 10.22237/jmasm/1414814520 [DOI] [Google Scholar]
- Coleman-Jensen A, Rabbitt MP, Gregory CA, & Singh A. (2020). Household food security in the United States in 2019. United States Department of Agriculture Economic Research Services. Economic Research Report; 275. http://www.ers.usda.gov/publications/pub-details/?pubid=99281 [Google Scholar]
- Economic Research Service. (2016). Food Environment Atlas. U.S. Department of Agriculture (USDA). https://www.ers.usda.gov/data-products/food-environment-atlas/go-to-the-atlas/ [Google Scholar]
- Figueroa JF, Wadhera RK, Lee D, Yeh RW, & Sommers BD (2020). Community-level factors associated with racial and ethnic disparities in COVID-19 rates in Massachusetts. Health Affairs, 39, 1984–1992. 10.1377/hlthaff.2020.01040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman DA, Bell BA, Clark J, Ngendahimana D, Borawski E, Trapl E, Pike S, & Sehgal AR (2020). Small improvements in an urban food environment resulted in no changes in diet among residents. Journal of Community Health, 46(1), 1–12. 10.1007/s10900-020-00805-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HAB, Kuczynski KJ, Kahle LL, & Krebs-Smith SM (2013). Update of the Healthy Eating Index: HEI-2010. Journal of the Academy of Nutrition and Dietetics, 113, 569–580. 10.1016/j.jand.2012.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gundersen C, & Ziliak JP (2015). Food insecurity and health outcomes. Health Affairs, 34(11), 1830–1839. 10.1377/hlthaff.2015.0645 [DOI] [PubMed] [Google Scholar]
- Johnson-Agbakwu CE, Ali NS, Oxford CM, Wingo S, Manin E, & Coonrod DV (2020). Racism, COVID-19, and health inequity in the USA: A call to action. Journal of Racial and Ethnic Health Disparities. 10.1007/s40615-020-00928-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh K, Kaiser ML, Sweeney G, Samadi K, & Hyder A. (2020). Explaining racial inequality in food security in Columbus, Ohio: A Blinder–Oaxaca decomposition analysis. International Journal of Environmental Research and Public Health, 17(15), 5488. 10.3390/ijerph17155488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kressin NR, Raymond KL, & Manze M. (2008). Perceptions of race/ethnicity-based discrimination: A review of measures and evaluation of their usefulness for the health care setting. Journal of Health Care for the Poor and Underserved, 19, 697–730. 10.1353/hpu.0.0041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson N, Laska MN, & Neumark-Sztainer D. (2020). Food insecurity, diet quality, home food availability, and health risk behaviors among emerging adults: Findings from the EAT 2010–2018 study. American Journal of Public Health, 110, 1422–1428. 10.2105/AJPH.2020.305783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke E, Coronado GD, Thompson B, & Kuniyuki A. (2009). Seasonal variation in fruit and vegetable consumption in a rural agricultural community. Journal of the American Dietetic Association, 109, 45–51. 10.1016/j.jada.2008.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MA Y, Olendzki BC, Pagoto SL, Hurley TG, Magner RP, Ockene IS, Schneider KL, Merriam PA, & Hébert JR (2009). Number of 24-hour diet recalls needed to estimate energy intake. Annals of Epidemiology, 19, 553–559. 10.1016/j.annepidem.2009.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maness SB, Merrell L, Thompson EL, Griner SB, Kline N, & Wheldon C. (2021). Social determinants of health and health disparities: COVID-19 exposures and mortality among African American people in the United States. Public Health Reports, 136(1), 18–22. 10.1177/0033354920969169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neville HA, & Cross WE (2017). Racial awakening: Epiphanies and encounters in Black racial identity. Cultural Diversity & Ethnic Minority Psychology, 23(1), 102–108. 10.1037/cdp0000105 [DOI] [PubMed] [Google Scholar]
- Nord M, Andrews M, & Carlson S. (2005). Household food security in the United States, 2004. United States Department of Agriculture Economic Research Services. Economic Research Report 11. https://www.ers.usda.gov/webdocs/publications/44787/29607_err11_002.pdf?v=3429.6 [Google Scholar]
- Odoms-Young AM (2018). Examining the impact of structural racism on food insecurity: Implications for addressing racial/ethnic disparities. Family & Community Health, 41(Suppl 2 FOOD INSECURITY AND OBESITY), S3–S6. 10.1097/FCH.0000000000000183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogojiaku CN, Allen J, Anson-Dwamena R, Barnett KS, Adetona O, Im W, & Hood DB (2020). The Health Opportunity Index: Understanding the input to disparate health outcomes in vulnerable and high-risk census tracts. International Journal of Environmental Research and Public Health, 17(16). 10.3390/ijerph17165767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, & Gee G. (2015). Racism as a determinant of health: A systematic review and meta-analysis. PloS One, 10(9), e0138511. 10.1371/journal.pone.0138511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phojanakong P, Brown Weida E, Grimaldi G, Lê-Scherban F, & Chilton M. (2019). Experiences of racial and ethnic discrimination are associated with food insecurity and poor health. International Journal of Environmental Research and Public Health, 16(22). 10.3390/ijerph16224369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteat T, Millett GA, Nelson LE, & Beyrer C. (2020). Understanding COVID-19 risks and vulnerabilities among black communities in America: The lethal force of syndemics. Annals of Epidemiology, 47, 1–3. 10.1016/j.annepidem.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell J. (2008). Structural racism: Building upon the insights of John Calmore. North Carolina Law Review, 86(3), 791. [Google Scholar]
- Raskind IG (2020). Hunger does discriminate: Addressing structural racism and economic inequality in food insecurity research. American Journal of Public Health, 110, 1264–1265. 10.2105/AJPH.2020.305841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schakel SF, Sievert YA, & Buzzard IM (1988). Sources of data for developing and maintaining a nutrient database. Journal of the American Dietetic Association, 88, 1268–1271. [PubMed] [Google Scholar]
- Schakel Sally F. (2001). Maintaining a nutrient database in a changing marketplace: Keeping pace with changing food products—A research perspective. Journal of Food Composition and Analysis, 14, 315–322. 10.1006/jfca.2001.0992 [DOI] [Google Scholar]
- Schakel Sally F., Buzzard IM, & Gebhardt SE (1997). Procedures for estimating nutrient values for food composition databases. Journal of Food Composition and Analysis, 10, 102–114. 10.1006/jfca.1997.0527 [DOI] [Google Scholar]
- Tucker J, Waldoks R, & Treering D. (2014). Food for every child: The need for healthy food financing in Ohio. The Food Trust. [Google Scholar]
- U.S. Census Bureau. (2016). 2011–2015 American community survey 5-year estimates. [Google Scholar]
- U.S. Department of Health and Human Services. (2010). Dietary guidelines for Americans (7th ed.). U.S. Government Printing Office. [Google Scholar]
- Williams DR, & Mohammed SA (2009). Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine, 32(1), 20. 10.1007/s10865-008-9185-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Mohammed SA (2013). Racism and health I: pathways and scientific evidence. The American Behavioral Scientist, 57(8). 10.1177/0002764213487340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson JA, & Leung CW (2020). Food insecurity and COVID-19: Disparities in early effects for US Adults. Nutrients, 12(6), 1648. 10.3390/nu12061648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegler RG, Wilcox HB, Mason TJ, Bill JS, & Virgo PW (1987). Seasonal variation in intake of carotenoids and vegetables and fruits among white men in New Jersey. The American Journal of Clinical Nutrition, 45(1), 107–114. 10.1093/ajcn/45.1.107 [DOI] [PubMed] [Google Scholar]