Abstract
Objective
To examine trends in pre-high blood pressure (BP [HBP]) and HBP among US adolescents by body weight category during 1988-2012.
Study design
We estimated pre-HBP and HBP prevalence among 14 844 participants aged 12-19 years using National Health and Nutrition Examination Surveys from 1988-1994, 1999-2002, 2003-2006, and 2007-2012. Pre-HBP and HBP were defined based on age-sex-height-specific BP percentiles. We examined the temporal trends in pre-HBP and HBP across category of body weight (normal weight vs overweight/obese), adjusted for potential explanatory factors, and estimated the number of adolescents with pre-HBP and HBP.
Results
Between 1988 and 2012, the prevalence of HBP decreased and pre-HBP did not change. Among normal weight adolescents, multivariable adjusted pre-HBP prevalence was 11.0% during 1988-2012, and 10.9% during 2007-2012 (P = .923 for trend); adjusted HBP prevalence increased from 1988-1994 (0.9%) to 1999-2002 (2.3%), then declined significantly to 1.4% during 2007-2012 (P = .049). Among overweight/obese adolescents, adjusted pre-HBP prevalence was 17.5% during 1988-2012, and 20.9% during 2007-2012 (P = .323); adjusted HBP prevalence declined significantly from 7.2% during 1988-1994 to 3.2% during 2007-2012 (P = .018). Because of population growth, estimated number of adolescents with pre-HBP or HBP increased, from 4.18 million during 1988-1994 to 5.59 million during 2007-2012.
Conclusions
Between 1988 and 2012, pre-HBP prevalence was consistently higher among overweight/obese adolescent than those of normal weight, and the pattern remain unchanged. HBP prevalence declined significantly, especially among overweight/obese adolescent that are not completely explained by sociodemographic or lifestyle characteristics.
Overweight and obesity increased significantly among US children and adolescents since the 1970s, leveling off since the mid-2000s.1-3 Overweight and obesity are important risk factors for high blood pressure (BP [HBP]) among children and adolescents.4 Childhood BP levels can continue to adulthood, and children with HBP are more likely to develop HBP as adults.5 HBP is a leading risk factor for cardiovascular disease and a significant contributor to US morbidity and mortality.6,7 Recently, attention and research have increased on the prevention of weight-associated health outcomes in children and adolescents, including HBP.4,8,9 Some investigators,10-13 but not others,8,14,15 suggest the epidemic of overweight and obesity is associated with increased average BP and HBP prevalence, and predict continuing increases in HBP prevalence with increases in overweight and obesity. A recent study examined trends in pre-HBP and HBP among US children and adolescents and found HBP prevalence declined during 1999-2012,16 though investigators indicated that the reason for this decline merits further study. The current study extends these results by examining the interaction of body mass index (BMI) status with trends in pre-HBP and HBP during 1988-2012, adjusted for potential confounding variables.
Methods
The National Health and Nutritional Examination Survey (NHANES) is designed to represent the civilian, noninstitutionalized US population. Data for NHANES were collected by household interviews and physical examinations as described elsewhere.17 Before 1999, NHANES surveys were periodic, but beginning that year, the survey became continuous. For the present study, we selected adolescents aged 12-19 years from NHANES 1988-1994, 1999-2002, 2003-2006, and 2007-2012. After excluding the pregnant adolescents, our analyses included 14 844 adolescents who had BP measurements in the NHANES mobile examination centers (MECs). NHANES III and NHANES 1999-2012 underwent institutional review board approval and included written informed consent.
Measurement and Definition of Pre-HBP and HBP
Up to 3 BP measurements were taken by the certified examiners during visits to MECs after participants rested quietly in a sitting position for at least 5 minutes. In 1988-1994, 1999-2002, 2003-2006, and 2007-2012, 99%, 89%, 78%, and 92%, respectively, of adolescents had 3 BP measurements, and 0.1%, 2.4%, 8.9%, and 2.5%, respectively, had 1 BP measurement. We used averages of 2 or 3 BP measurements for those who had multiple measurements and 1 BP reading for the remaining adolescents. We classified adolescents as having normal, pre-HBP, or HBP based on age-sex-height-specific BP percentiles and the age-sex-height-specific percentiles is determined by 2000 Centers for Disease Control and Prevention growth charts.4 For adolescents aged 12-17 years, normal was defined as systolic BP (SBP) and diastolic BP (DBP) <90th percentile for age-sex-height; pre-HBP was defined as SBP or DBP ≥90th but <95th percentile, or BP levels ≥120/80 mm Hg. HBP was defined as SBP and/or DBP ≥95th percentile. For adolescents aged 18-19 years, pre-HBP was defined as either SBP of >120 but <140 mm Hg or DBP of >80 but <90 mm Hg; HBP was defined as SBP ≥140 mm Hg, DBP ≥90 mm Hg, or taking antihypertensive medication.18 The guidelines recommend that the multiple BP measurements at different times should be used to define persistent prehypertension and hypertension in adolescents.4 To differentiate the BP measurements in the present study (up to 3 measurements at MECs in the same day) from the recommended definitions, we used the terms of pre-HBP and HBP with the same cut-off points that are used to define prehypertension and hypertension in the guidelines.4
Covariates
Age, sex, and race/ethnicity of participants were obtained from standard questionnaires. Race/ethnicity was classified as non-Hispanic white, non-Hispanic black, Mexican American, or other. BMI was calculated as measured weight (kg)/height (m2).
We compared BMI in adolescents with age-sex-specific values from 2000 Centers for Disease Control and Prevention growth charts in order to account for variability by age and sex.19 BMI-for-age of ≥85th to <95th percentiles was defined as overweight, and ≥95% percentile as obese. Waist-to-height ratio was calculated by dividing the waist (inches) by height (inches).20
For adolescents aged ≥12 years, the questions about smoking status changed substantially over time; therefore, we used the sex-race/ethnicity-specific cut-off points of cotinine concentrations to classify adolescents as current smokers vs nonsmokers.21
Questions to assess duration and intensity of physical activity varied substantially over time. Therefore, physical activity was classified at its most basic level: those reporting no activity vs some activities.22
Healthy eating index-2010 (HEI-2010) represents all major food groups, including fruits, vegetables, grains, milk, meat and beans, oils, saturated fat, sodium, and calories from solid fats, alcoholic beverages, and added sugars.23 Food components are given maximum and minimum points per 1000 calories and total score ranges from 0-100, a higher score indicating a more healthy diet.23
Total annual family income, a socioeconomic status proxy, was used to calculate the poverty-income-ratio (PIR). The PIR was derived by dividing total annual family income by the established federal poverty level for the specific family size, accounting for year and state where assessment took place.24 We defined PIR <1.0 as poor, 1.0 to <2.0 as near poor, 2.0 to <3.0 as middle income, and ≥3.0 as high income.
Statistical Analyses
We estimated the weighted prevalence and means (adjusted for age, sex, and race) of pre-HBP, HBP, BP and selected covariates by BMI status. We used linear and logistic regressions to test for temporal trends of pre-HBP and HBP prevalence, BP, and selected covariates across the 4 NHANES cycles. In the regression models, each variable of interest was the dependent variable; the independent variables included a categorical time variable corresponding to the midpoint of each survey (1991 for 1988-1994, 2001 for 1999-2002, 2005 for 2003-2006, and 2009 for 2007-2012 surveys), age, sex, and race/ethnicity. The time variable was used to assess temporal trends.
For analysis of temporal trends in prevalence, we fit logistic regression models using the Multilog procedure in SUDAAN v 10 (RTI International, Research Triangle Park, North Carolina) to estimate the adjusted pre-HBP and HBP simultaneously.25 The adjusted prevalence was estimated by taking the predicted marginal.26 In logistic regression analyses, we estimated the unadjusted prevalence (model 1); age-sex-race/ethnicity-adjusted prevalence (model 2); plus smoking status, physical activity, HEI-2010, PIR, waist-to-height ratio, and BMI as continuous variables (model 3). We conducted a 2-step trend test for each outcome, pre-HBP or HBP, by body weight categories (normal vs overweight/obese): first, we tested for linearity of the trends across all NHANES cycles; second, if the trends were linear, we presented the P values for trend during 1988-2012, and if the trends were nonlinear, with leveling off in 1999, we presented the P values from NHANES 1999-2012. To account for multiple comparisons, we calculated the adjusted P values controlling for false discovery rate (FDR) at 5.0%. The FDR represents the proportion of incorrectly rejected null hypotheses out of all rejected null hypotheses.27 We used the SAS PROC MULTTEST with the un-adjusted P values as input to calculate the FDR adjusted P values (SAS Institute, Inc, Cary, North Carolina).
We tested for interactions in logistic regression models by including a 2-way interaction term between time and each covariate adjusted for all other covariates. Because of the significant multiplicative interaction between time and BMI (P = .019), we stratified results by BMI status. We combined overweight and obese participants in a single group to stabilize our estimates. Although pre-HBP and HBP prevalence was significantly higher among males than among females, the temporal trends were consistent by sex (P = .117 for interaction between time and sex), so we combined results for males and females. We estimated the number of adolescents with pre-HBP or HBP by multiplying and summing up the BMI status-specific pre-HBP or HBP prevalence by the total number of the noninstitutionalized population derived from current population surveys for each NHANES cycle (http://www.cdc.gov/nchs/tutorials/nhanes/NHANESAnalyses/AgeStandardization/Info2.htm). We used Monte Carlo simulation to estimate the CIs for the number of adolescents with pre-HBP and HBP by taking 95% CI of BMI status-specific prevalence as a triangle distribution. @Risk v 5.0 (Palisade Corporation, Ithaca, New York) was used with 1000 draws, and the lower 2.5 and upper 97.5 percentile distributions were reported as 95% CIs.
We used weighted sequential hot deck imputation as implemented in SUDAAN v 10 (RTI International) to impute values for selected covariates with missing information.25 These covariates included smoking (N = 1363 participants with missing information), physical activity (N = 59), HEI-2010 (N = 458), PIR (N = 1214), and waist-to-height ratio (N = 190).
We conducted 2 sensitivity analyses by examining trends in pre-HBP and HBP by BMI status, excluding adolescents who had missing values for the covariates and examining trends in pre-HBP and HBP by BMI status, stratified by age (12-15 years vs 16-19 years), sex, and race/ethnicity (Tables I-III; available at www.jpeds.com).
Table I.
Adjusted prevalence of pre-HBP or HBP among adolescents aged 12-19 years with nonmissing covariates-NHANES 1988-1994,1999-2002, 2003-2006, and 2007-2012
| Pre-HBP, % (95% CI) |
HBP, % (95% CI) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI status | 1988-1994 (N = 9669) | 1999-2002 (N = 8702) | 2003-2006 (N = 8470) | 2007-2012 (N = 7780) | P value for trend* | 1988-1994 (N = 5175) | 1999-2002 (N = 4728) | 2003-2006 (N = 4262) | 2007-2012 (N = 4224) | P value for trend* |
| Normal weight | ||||||||||
| Model 1† | 11.1 (9.4-13.1) | 10.8 (9.2-12.7) | 11.5 (9.3-14.1) | 11.0 (9.2-13.1) | .9212 | 0.9 (0.5-1.5) | 2.3 (1.7-3.1) | 2.3 (1.4-4.0) | 1.4 (0.9-2.1) | .0422 |
| Model 2‡ | 11.1 (9.1-13.4) | 11.0 (9.1-13.1) | 11.5 (9.2-14.3) | 10.4 (8.5-12.7) | .7595 | 1.0 (0.5-1.7) | 2.1 (1.4-3.0) | 1.7 (1.0-3.1) | 1.2 (0.7-1.9) | .0861 |
| Overweight/obese | ||||||||||
| Model 1† | 16.7 (12.1-22.6) | 21.5 (18.8-24.5) | 21.6 (18.4-25.1) | 21.2 (18.1-24.7) | .3388 | 6.4 (3.7-10.9) | 6.6 (5.0-8.6) | 4.7 (3.0-7.4) | 3.4 (2.3-4.9) | .0078 |
| Model 2‡ | 18.6 (13.3-25.5) | 21.0 (17.9-24.4) | 20.5 (17.0-24.5) | 21.4 (18.2-25.1) | .7595 | 7.7 (4.4-13.2) | 6.0 (4.5-7.9) | 4.3 (2.7-6.9) | 3.1 (2.1-4.6) | .0152 |
P value for trends across the surveys using logistic regression models after controlling for the FDR at 5.0% for multiple comparisons. For prevalence of HBP among normal weight and overweight/obese adolescents. P values for trends during 1999-2012 were used because of the nonlinear changes in the prevalence across the surveys; all tests were 2-tailed.
Model 1 adjusted for age, sex, and race/ethnicity.
Model 2, in addition to the variables in model 1, adjusted for smoking status, physical activity, HEI-2010, PIR, waist-to-height ratio, and BMI as continuous variables.
Table III.
Adjusted prevalence and 95% CI of HBP among adolescents aged 12-19 years by age, sex, and race/ethnicity-NHANES 1988-1994, 1999-2002, 2003-2006, and 2007-2012
| HBP, % (95% CI) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Normal weight |
Overweight or obese |
|||||||||
| Characteristics | 1988-1994 | 1999-2002 | 2003-2006 | 2007-2012 | P value for trend* | 1988-1994 | 1999-2002 | 2003-2006 | 2007-2012 | P value for trend* |
| Age group | ||||||||||
| 12-15 y | ||||||||||
| Model 1† | 1.1 (0.5-2.5) | 3.0 (1.95-4.6) | 3.1 (1.7-5.8) | 1.4 (0.7-2.6) | .0381 | 7.7 (3.8-15.1) | 6.8 (4.7-9.8) | 5.0 (3.1-8.1) | 1.4 (1.2-3.6) | .0010 |
| Model 2‡ | 1.1 (0.4-2.9) | 2.4 (1.3-4.1) | 2.5 (1.4-4.6) | 1.0 (0.5-2.0) | .0749 | 10.7 (5.4-20.0) | 6.9 (4.7-10.0) | 4.7 (2.8-8.0) | 2.0 (1.1-3.6) | .0010 |
| 16-19 y | ||||||||||
| Model 1† | 0.7 (0.4-1.2) | 1.7 ((1.0-2.7) | 1.5 (0.8-2.8) | 1.4 (0.7-2.4) | .5877 | 4.7 (1.9-11.0) | 6.2 (4.4-8.7) | 4.4 (2.2-8.3) | 1.4 (2.9-8.2) | .4290 |
| Model 2‡ | 0.7 (0.5-1.2) | 1.7 (0.9-3.3) | 1.0 (0.6-1.9) | 1.4 (0.7-2.6) | .6446 | 4.7 (1.6-13.3) | 4.9 (3.5-6.7) | 3.9 (1.9-7.8) | 4.1 (2.2-7.5) | .6001 |
| Sex | ||||||||||
| Male | ||||||||||
| Model 1† | 1.0 (0.5-2.0) | 2.4 (1.5-3.7) | 2.3 (1.3-4.0) | 1.4 (1.2-3.1) | .5154 | 11.8 (6.5-20.5) | 8.7 (6.0-12.5) | 4.7 (2.7-8.0) | 1.4 (2.8-7.0) | .0282 |
| Model 2‡ | 1.1 (0.6-2.3) | 2.1 (1.5-3.1) | 1.6 (1.0-2.7) | 1.9 (1.1-3.1) | .6494 | 13.2 (7.3-22.8) | 7.3 (4.9-10.9) | 4.3 (2.4-7.5) | 3.8 (2.3-6.3) | .0516 |
| Female | ||||||||||
| Model 1† | 0.8 (0.3-2.0) | 2.3 (1.3-4.0) | 2.4 (1.1-5.0) | 1.4 (0.3-1.8) | .0369 | 0.9 (0.5-1.9) | 4.1 (2.6-6.3) | 4.9 (3.1-7.7) | 1.4 (1.2-4.2) | .1006 |
| Model 2‡ | 0.9 (0.3-3.0) | 2.0 (1.0-3.8) | 1.8 (0.8-4.2) | 1.4 (0.2-0.9) | .0246 | 0.8 (0.3-2.1) | 4.6 (2.9-7.3) | 4.0 (2.4-6.6) | 2.2 (1.1-4.5) | .0769 |
| Race/ethnicity | ||||||||||
| Non-Hispanic white | ||||||||||
| Model 1† | 0.5 (0.1-1.7) | 2.2 (1.4-3.5) | 2.9 (1.5-5.5) | 1.4 (0.3-1.9) | .0270 | 8.4 (4.3-15.6) | 6.1 (3.6-10.1) | 4.0 (2.0-7.6) | 1.4 (1.5-5.7) | .0909 |
| Model 2‡ | 0.6 (0.1-2.1) | 2.0 (1.1-3.4) | 2.2 (1.1-4.3) | 0.5 (0.2-1.3) | .0164 | 9.6 (4.8-18.4) | 5.4 (3.2-9.0) | 3.8 (1.9-7.3) | 3.1 (1.5-6.3) | .1977 |
| Non-Hispanic black | ||||||||||
| Model 1† | 3.2 (2.2-4.6) | 2.9 (2.0-4.1) | 1.9 (1.3-2.7) | 1.4 (2.0-5.8) | .6058 | 3.9 (2.1-7.2) | 7.5 (5.5-10.2) | 6.5 (4.4-9.5) | 1.4 (2.7-6.8) | .0416 |
| Model 2‡ | 3.5 (2.3-5.3) | 3.1 (2.0-4.7) | 2.1 (1.5-2.8) | 4.0 (2.3-7.1) | .4905 | 3.5 (1.6-7.5) | 7.2 (4.8-10.8) | 6.0 (3.8-9.5) | 3.1 (1.7-5.7) | .0213 |
| Mexican American | 1.9 (0.8-4.5) | 1.6 (0.9-2.9) | 1.0 (0.5-2.0) | 1.4 (0.8-5.2) | .7177 | 2.4 (1.0-5.5) | 5.5 (4.2-7.2) | 3.8 (2.8-5.3) | 1.4 (2.5-5.5) | .0493 |
| Model 1† | ||||||||||
| Model 2‡ | 1.5 (0.5-4.1) | 1.6 (0.9-3.04) | 1.1 (0.5-2.4) | 1.7 (0.5-5.4) | .9268 | 2.7 (0.9-7.5) | 5.5 (3.9-7.7) | 2.9 (1.8-4.8) | 3.8 (2.6-5.7) | .0540 |
P value for trends across the surveys using logistic regression models. For prevalence of HBP among normal and overweight/obese female adolescents, prevalence of HBP among Non-Hispanic black and Mexican American overweight/obese adolescents, P values for trends were used during 1999-2012 because of the nonlinear changes in the prevalence across the surveys; all tests were 2-tailed.
Model 1 adjusted for age, sex, and race/ethnicity.
Model 2, in addition to variables in model 1, adjusted for smoking status, physical activity, HEI-2010, PIR, waist-to-height ratio, and BMI as continuous variables.
Data were analyzed using SAS v 9.3 (SAS Institute, Inc, Cary, North Carolina) and SUDAAN v 10 (RTI International) to account for the complex sampling design.25 All tests were 2-sided, and an adjusted P value of <.05 was considered statistically significant.
Results
Current smoking declined significantly among US adolescents from 1988-2012. HEI-2010 increased, especially during 1999-2012. The percentage of adolescents living in higher PIR households significantly increased. The mean BMI remained unchanged among normal weight adolescents, and increased significantly over time among overweight/obese adolescents. Adjusted mean SBP or DBP did not change significantly during 1988-2012 (Table IV).
Table IV.
Characteristics of adolescents aged 12-19 years, NHANES 1988-2012
| Normal weight |
Overweight or obese |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | 1988-1994, N = 1985 (95% CI) | 1999-2002, N = 2844 (95% CI) | 2003-2006, N = 2629 (95% CI) | 2007-2012, N = 2211 (95% CI) | P value for trend* | 1988-1994, N = 780 (95% CI) | 1999-2002, N = 1576 (95% CI) | 2003-2006, N = 1518 (95% CI) | 2007-2012, N = 1301 (95% CI) | P value for trend* |
| Age group, % | ||||||||||
| 12-15 y | 48.1 (44.0-52.2) | 50.9 (48.2-53.5) | 50.9 (48.0-53.8) | 50.4 (47.0-53.8) | .399 | 60.0 (53.6-66.1) | 51.8 (47.6-56.0) | 52.6 (48.1-57.0) | 54.3 (50.6-57.9) | .162 |
| 16-19 y | 51.9 (47.8-56.0) | 49.1 (46.5-51.8) | 49.1 (46.2-52.0) | 49.6 (46.2-53.0) | .399 | 40.0 (33.9-46.4) | 48.2 (44.0-52.4) | 47.4 (43.0-51.9) | 45.7 (42.1-49.4) | .162 |
| Sex, % | ||||||||||
| Male | 51.3 (47.0-55.6) | 51.5 (49.4-53.7) | 50.6 (48.0-53.2) | 50.8 (48.1-53.4) | .745 | 50.0 (44.6-55.4) | 52.0 (47.9-56.0) | 52.7 (49.0-56.4) | 53.1 (49.4-56.8) | .344 |
| Female | 48.7 (44.4-53.0) | 48.5 (46.3-50.6) | 49.4 (46.8-52.0) | 49.2 (46.6-51.9) | .745 | 50.0 (44.6-55.4) | 48.0 (44.0-52.1) | 47.3 (43.6-51.0) | 46.9 (43.2-50.6) | .344 |
| Race/ethnicity, % | ||||||||||
| Non-Hispanic white | 68.6 (63.3-73.4) | 61.6 (57.1-65.8) | 65.0 (59.5-70.0) | 61.1 (56.5-65.6) | .095 | 65.5 (58.4-71.9) | 53.6 (48.4-58.7) | 62.2 (54.3-69.5) | 52.7 (46.7-58.5) | .030 |
| Non-Hispanic black | 14.5 (11.9-17.7) | 12.7 (10.1-16.0) | 13.8 (10.5-17.9) | 13.6 (11.0-16.6) | .777 | 16.3 (13.1-20.1) | 16.3 (12.6-20.8) | 16.3 (12.7-20.7) | 17.2 (13.8-21.2) | .748 |
| Mexican American | 7.5 (5.6-9.9) | 9.3 (7.1-12.1) | 10.3 (7.9-13.4) | 11.5 (9.2-14.3) | .016 | 9.8 (7.5-12.5) | 14.3 (10.9-18.5) | 12.7 (9.7-16.4) | 16.3 (12.7-20.5) | .014 |
| Other | 9.4 (6.7-13.1) | 16.4 (12.5-21.1) | 10.9 (8.9-13.4) | 13.8 (11.5-16.6) | .264 | 8.5 (4.2-16.4) | 15.8 (10.9-22.4) | 8.8 (5.9-12.8) | 13.9 (11.3-17.0) | .365 |
| Smoking status, %† | ||||||||||
| Current smoker | 21.8 (18.6-25.4) | 19.3 (16.6-22.3) | 17.2 (14.9-19.7) | 14.2 (12.3-16.3) | <.001 | 23.0 (18.2-28.5) | 21.5 (18.0-25.4) | 17.0 (14.6-19.8) | 14.5 (11.6-18.0) | .002 |
| Noncurrent smoker | 78.2 (74.6-81.4) | 80.7 (77.7-83.4) | 82.8 (80.3-85.1) | 85.8 (83.7-87.7) | <.001 | 77.0 (71.5-81.8) | 78.5 (74.6-82.0) | 83.0 (80.2-85.4) | 85.5 (82.0-88.4) | .002 |
| PIR, %‡ | ||||||||||
| <1 (poor) | 19.5 (17.0-22.3) | 21.2 (18.2-24.5) | 20.1 (17.0-23.5) | 20.9 (18.0-24.2) | .550 | 28.4 (22.2-35.5) | 28.7 (25.2-32.6) | 23.2 (19.0-28.0) | 27.3 (23.6-31.4) | .456 |
| ≥1-<2 (near poor) | 23.9 (20.0-28.2) | 24.2 (22.1-26.5) | 19.8 (17.5-22.3) | 21.0 (18.2-24.0) | .068 | 26.5 (21.4-32.3) | 22.5 (18.9-26.6) | 21.8 (19.0-24.9) | 24.0 (21.0-27.3) | .466 |
| ≥2-<3 (middle income) | 22.5 (18.5-27.1) | 15.5 (13.3-17.9) | 15.3 (12.9-18.2) | 14.6 (12.6-16.9) | .002 | 23.1 (17.6-29.7) | 16.1 (13.2-19.4) | 20.0 (17.1-23.3) | 15.2 (12.6-18.4) | .037 |
| ≥3 (high income) | 34.0 (29.6-38.7) | 39.1 (35.4-43.0) | 44.8 (40.0-49.7) | 43.5 (38.8-48.4) | <.001 | 22.0 (15.7-30.0) | 32.7 (28.9-36.8) | 35.0 (30.4-39.9) | 33.4 (29.0-38.2) | .004 |
| BMI, mean | 20.3 (20.1-20.4) | 20.4 (20.2-20.5) | 20.3 (20.1-20.5) | 20.5 (20.3-20.6) | .172 | 28.2 (27.4-28.9) | 29.4 (29.1-29.6) | 29.4 (28.9-29.9) | 29.8 (29.4-32.2) | .001 |
| Waist-to-height ratio, mean§ |
0.43 (0.43-0.44) | 0.45 (0.44-0.45) | 0.45 (0.44-0.45) | 0.45 (0.44-0.45) | <.001 | 0.55 (0.54-0.56) | 0.57 (0.57-0.58) | 0.58 (0.57-0.58) | 0.58 (0.57-0.58) | <.001 |
| HEI-2010, mean¶ | 41.0 (40.0-41.9) | 40.2 (39.4-41.0) | 41.0 (40.3-41.6) | 42.8 (42.0-43.6) | .002 | 39.9 (38.7-41.2) | 39.6 (38.8-40.3) | 40.6 (39.8-41.3) | 42.9 (42.0-43.9) | <.001 |
| SBP, mean** | 106.7 (105.9-107.5) | 107.5 (106.9-108.1) | 108.1 (107.3-109.0) | 107.5 (106.9-108.2) | .089 | 112.0 (110.9-113.0) | 113.7 (112.8-114.6) | 113.6 (112.8-114.5) | 112.5 (111.8-113.3) | .463 |
| DBP, mean** | 60.6 (59.6-61.7) | 63.0 (62.0-64.0) | 60.3 (59.5-61.1) | 60.1 (59.1-61.0) | .052 | 61.5 (59.9-63.0) | 62.2 (61.1-63.3) | 59.5 (58.7-60.4) | 60.7 (59.5-61.9) | .106 |
P value for trends across the surveys using logistic regression models. For prevalence of HBP among normal and overweight/obese adolescents, P values for trends during 1999-2012 were used because of the nonlinear changes in the prevalence across the surveys; all tests were 2-tailed.
The weighted hot-deck imputation was used to impute 1363 participants with missing information on smoking status.
The weighted hot-deck imputation was used to impute 1214 participants with missing information on PIR.
The weighted hot-deck imputation was used to impute 190 participants with missing information on waist-to-height ratio.
The weighted hot-deck imputation was used to impute 458 participants with missing information on HEI-2010.
The mean SBP and DBP was adjusted for age, sex, and race/ethnicity.
Age-sex-race/ethnicity-adjusted pre-HBP prevalence remained unchanged during 1988-2012 among normal and overweight/obese adolescents with and without adjusting for covariates. During 1988-2012, about 11%-12% of normal weight and 18%-22% of overweight/obese adolescents had pre-HBP (Table V). In contrast, age-sex-race/ethnicity-adjusted HBP prevalence appeared to double from 1984-1994 to 1999-2002 among normal weight adolescents, but not among overweight/obese adolescents and then declined significantly from 1999-2002 to 2007-2012 among both normal and overweight/obese adolescents. After further adjusting for the covariates, the prevalence was 0.9% (95% CI 0.5%-1.5%), 2.3% (95% CI 1.7%-3.2%), 2.4% (95% CI 1.4%-4.0%), and 1.4% (95% CI 0.9%-2.2%) during 1988-1994, 1999-2002, 2003-2006, and 2007-2012, respectively, among normal weight adolescents (P = .049 for trend), and 7.2% (95% CI 4.5%-11.3%), 6.6% (95% CI 5.0%-8.5%), 4.7% (95% CI 3.0%-7.3%), and 3.2% (95% CI 2.2%-4.6%) among overweight/obese adolescents (P = .018; Table V).
Table V.
Adjusted prevalence and estimated number of adolescents aged 12-19 years with HBP, NHANES 1988-2012
| Pre-HBP, % (95% CI) |
HBP, % (95% CI) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI status | 1988-1994 | 1999-2002 | 2003-2006 | 2007-2012 | P value for trend* | 1988-1994 | 1999-2002 | 2003-2006 | 2007-2012 | P-value for trend* |
| Normal weight | ||||||||||
| Model 1† | 11.4 (9.6-13.6) | 10.6 (9.2-12.3) | 11.4 (9.1-14.2) | 11.1 (9.3-13.1) | .939 | 0.9 (0.5-1.5) | 2.3 (1.7-3.1) | 2.3 (1.4-4.0) | 1.4 (0.9-2.1) | .066 |
| Model 2‡ | 11.1 (9.4-13.1) | 10.8 (9.2-12.7) | 11.5 (9.3-14.1) | 11.0 (9.2-13.1) | .921 | 0.9 (0.5-1.5) | 2.3 (1.7-3.1) | 2.3 (1.4-4.0) | 1.4 (0.9-2.1) | .042 |
| Model 3§ | 11.0 (9.3-12.9) | 10.9 (9.3-12.8) | 11.7 (9.4-14.4) | 10.9 (9.1-12.9) | .958 | 0.9 (0.5-1.5) | 2.3 (1.7-3.1) | 2.4 (1.4-4.0) | 1.4 (0.9-2.2) | .049 |
| Overweight/obese | ||||||||||
| Model 1† | 15.5 (11.1-22.3) | 21.7 (18.9-24.8) | 22.1 (18.6-26.0) | 21.4 (18.2-25.0) | .896 | 6.4 (3.6-11.0) | 6.6 (5.0-8.7) | 4.7 (3.0-7.4) | 3.4 (2.3-4.9) | .067 |
| Model 2‡ | 16.7 (12.1-22.6) | 21.5 (18.8-24.5) | 21.6 (18.4-25.1) | 21.2 (18.1-24.7) | .338 | 6.4 (3.7-10.9) | 6.6 (5.0-8.6) | 4.7 (3.0-7.4) | 3.4 (2.3-4.9) | .008 |
| Model 3§ | 17.5 (12.8-23.3) | 21.8 (19.0-24.8) | 21.1 (18.1-24.5) | 20.9 (17.9-24.4) | .646 | 7.2 (4.5-11.3) | 6.6 (5.0-8.5) | 4.7 (3.0-7.3) | 3.2 (2.2-4.6) | .018 |
| Estimated number of adolescents, 100 000 | 35.3 (32.3-40.3) | 45.1 (42.3-48.6) | 50.1 (45.9-55.2) | 49.1 (45.3-53.3) | <.001 | 6.48 (5.33-9.11) | 11.7 (10.4-13.6) | 10.5 (8.76-13.7) | 6.85 (5.96-8.60) | <.001 |
P value for trends across the surveys using logistic regression models after controlling for the FDR at 5.0% for multiple comparisons. For prevalence of pre-HBP among overweight/obese adolescents for model 1, and prevalence of HBP among normal weight adolescents, P values for trends during 1999-2012 were used because of the nonlinear changes in the prevalence across the surveys; all tests were 2-tailed.
Model 1 unadjusted prevalence.
Model 2 adjusted for age, sex, and race/ethnicity.
Model 3, in addition to the variables in Model 2, adjusted for smoking status, physical activity, HEI-2010, PIR, waist-to-height ratio and BMI as continuous variables.
The prevalence ratios (PRs) for pre-HBP by demographic characteristics did not change over time; PRs for pre-HBP were higher among males compared with females, 16- to 19-year-olds compared with 12- to 15-year-olds, and non-Hispanic blacks compared with non-Hispanic whites (Table VI).
Table VI.
Adjusted PRs of Pre-HBP and HBP among adolescents aged 12-19 years by BMI status, NHANES 1988-2012
| Normal weight* |
Overweight/obese* |
|||
|---|---|---|---|---|
| Characteristics | PR for Pre-HBP (95% CI) | PR for HBP (95% CI) | PR for Pre-HBP (95% CI) | PR for HBP (95% CI) |
| NHANES survey year | ||||
| 1988-1994 | Reference | Reference | Reference | Reference |
| 1999-2002 | 1.00 (0.76-1.33) | 2.76 (1.49-5.11) | 1.36 (0.89-2.07) | 0.98 (0.52-1.85) |
| 2003-2006 | 1.10 (0.79-1.53) | 2.86 (1.30-6.31) | 1.25 (0.76-2.05) | 0.66 (0.32-1.36) |
| 2007-2012 | 0.99 (0.74-1.32) | 1.61 (0.77-3.36) | 1.19 (0.75-1.89) | 0.43 (0.22-0.82) |
| Age group | ||||
| 12-15 y | Reference | Reference | Reference | Reference |
| 16-19y | 2.13 (1.72-2.63) | 0.62 (0.39-1.00) | 1.77 (1.36-2.31) | 0.81 (0.53-1.25) |
| Sex | ||||
| Female | Reference | Reference | Reference | Reference |
| Male | 3.31 (2.61-4.20) | 1.31 (0.82-2.12) | 3.60 (2.90-4.47) | 3.10 (2.08-4.63) |
| Race/ethnicity | ||||
| Non-Hispanic white | Reference | Reference | Reference | Reference |
| Non-Hispanic black | 1.44 (1.18-1.75) | 1.61 (1.02-2.53) | 1.19 (0.94-1.50) | 1.14 (0.76-1.69) |
| Mexican American | 0.94 (0.74-1.19) | 1.03 (0.53-2.00) | 0.94 (0.74-1.19) | 0.90 (0.60-1.36) |
PRs were adjusted for age, sex, race/ethnicity, smoking, physical activity, HEI-2010, PIR, waist-to-height ratio, and BMI.
Among normal weight adolescents, PR for HBP was 2.8 (95% CI 1.5-5.1) during 1999-2002 compared with 1988-1994, and 0.6 (95% CI 0.3-1.0) during 2007-2012 compared with 1999-2002. Among overweight/obese adolescents, PR for HBP was 0.4 (95% CI 0.2-0.8) during 2007-2012 compared with 1988-1994 (Table VI).
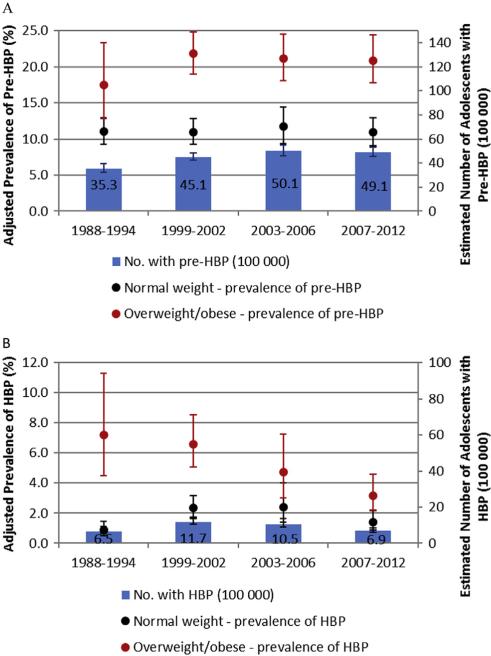
The estimated number of adolescents with pre-HBP increased from 3.53 million (95% CI 3.23-4.03) during 1988-1994 to 4.91 million (95% CI 4.53-5.33) during 2007-2012 (Figure, A and Table V). However, the estimated number of adolescents with HBP increased significantly from 0.65 million (95% CI 0.53-0.91) during 1988-1994 to 1.17 million (95% CI 1.04-1.36) during 1999-2002, then declined to 0.69 million (95% CI 0.60-0.86) during 2007-2012, mainly due to significant decline in HBP prevalence since 1999 (Figure, B and Table V). In spite of this decline, the estimated number of US adolescents with pre-HBP and HBP increased from 4.18 million (95% CI 3.99-4.81) during 1988-1994 to 5.59 million (95% CI 5.14-5.95) million during 2007-2012.
Figure.
Adjusted prevalence of A, pre-HBP and B, HBP among adolescents aged 12-19 years by BMI status, and estimated number of adolescents with pre-HBP and HBP, NHANES 1988-2012.
The trends in pre-HBP and HBP prevalence were largely unchanged when we excluded the missing covariates (Table I), and remained consistent across age group, sex, and race/ethnicity (Tables II and III).
Table II.
Adjusted prevalence and 95% CI of pre-HBP among adolescents aged 12-19 years by age, sex, and race/ethnicity-NHANES 1988-1994, 1999-2002, 2003-2006, and 2007-2012
| Pre-HBP, % (95% CI) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Normal weight |
Overweight or obese |
|||||||||
| Characteristics | 1988-1994 | 1999-2002 | 2003-2006 | 2007-2012 | P value for trend* | 1988-1994 | 1999-2002 | 2003-2006 | 2007-2012 | P value for trend* |
| Age group | ||||||||||
| 12-15 y | ||||||||||
| Model 1† | 5.9 (4.3-8.2) | 6.2 (4.7-8.2) | 6.8 (4.8-9.5) | 6.3 (4.5-8.6) | .7217 | 13.9 (9.0-20.9) | 14.9 (11.3-19.4) | 13.6 (10.2-18.0) | 15.3 (12.4-18.8) | .7911 |
| Model 2‡ | 6.0 (4.1-8.6) | 6.2 (4.5-8.6) | 7.2 (4.9-10.5) | 5.5 (3.8-8.0) | .9395 | 15.6 (9.9-23.5) | 14.8 (10.9-19.6) | 13.7 (9.9-18.6) | 15.6 (12.5-19.4) | .9455 |
| 16-19 y | ||||||||||
| Model 1† | 16.1 (13.3-19.3) | 15.4 (12.8-18.4) | 16.1 (12.8-20.2) | 16.0 (13.2-19.2) | .9612 | 18.4 (11.3-28.6) | 29.1 (24.6-34.2) | 31.1 (26.3-36.4) | 28.3 (22.6-34.8) | .0514 |
| Model 2‡ | 16.3 (13.3-19.8) | 15.8 (12.8-19.3) | 15.7 (12.2-20.0) | 15.5 (12.6-18.8) | .7242 | 22.0 (13.3-34.0) | 27.7 (22.8-33.2) | 28.3 (23.2-34.1) | 28.1 (22.3-34.7) | .2936 |
| Sex | ||||||||||
| Male | ||||||||||
| Model 1† | 18.3 (15.3-21.7) | 15.2 (13.3-17.2) | 17.2 (13.9-21.0) | 15.7 (13.1-18.8) | .3790 | 21.5 (14.3-31.0) | 31.1 (26.3-36.2) | 29.9 (25.5-34.9) | 30.2 (24.8-36.1) | .1201 |
| Model 2‡ | 18.7 (15.2-22.9) | 15.5 (13.2-18.1) | 16.9 (13.6-20.7) | 15.0 (12.2-18.3) | .1872 | 23.9 (15.7-34.7) | 32.3 (27.2-38.0) | 29.0 (24.1-34.5) | 30.5 (25.1-36.5) | .3546 |
| Female | ||||||||||
| Model 1† | 3.4 (2.1-5.3) | 6.3 (4.1-9.5) | 5.5 (3.6-8.3) | 6.3 (4.5-8.8) | .0620 | 10.9 (6.4-17.9) | 11.0 (8.2-14.5) | 12.6 (9.6-16.4) | 11.6 (8.6-15.5) | .7140 |
| Model 2‡ | 3.2 (1.9-5.4) | 6.2 (3.9-9.9) | 5.9 (3.8-9.0) | 5.6 (3.6-8.5) | .1107 | 13.2 (7.2-23.0) | 8.2 (6.0-11.2) | 11.2 (8.6-14.5) | 10.9 (7.7-15.3) | .7765 |
| Race/ethnicity | ||||||||||
| Non-Hispanic white | ||||||||||
| Model 1† | 10.7 (8.6-13.2) | 10.9 (8.5-13.9) | 11.8 (9.1-15.1) | 9.8 (7.4-12.8) | .7633 | 17.6 (11.5-26.1) | 21.6 (17.4-26.3) | 20.5 (15.9-25.9) | 22.4 (17.6-28.1) | .3635 |
| Model 2‡ | 11.5 (9.1-14.4) | 11.5 (8.9-14.7) | 11.6 (8.6-15.4) | 9.1 (6.7-12.3) | .2480 | 20.0 (12.9-29.6) | 21.1 (16.4-26.8) | 19.2 (14.3-25.1) | 22.7 (18.1-28.0) | .6814 |
| Non-Hispanic black | ||||||||||
| Model 1† | 10.9 (6.4-17.9) | 11.0 (8.2-14.5) | 12.6 (9.6-16.4) | 11.6 (8.6-15.5) | .7140 | 17.2 (12.3-23.5) | 23.7 (19.6-28.4) | 25.8 (22.2-29.8) | 22.7 (18.8-27.1) | .0840 |
| Model 2‡ | 13.7 (10.8-17.4) | 14.9 (11.9-18.5) | 16.6 (13.4-20.3) | 18.0 (15.3-21.1) | .0357 | 18.4 (12.7-26.0) | 23.2 (18.4-29.0) | 25.5 (21.6-29.9) | 23.1 (18.6-28.3) | .1985 |
| Mexican American | ||||||||||
| Model 1† | 8.7 (6.4-11.8) | 10.0 (8.2-12.1) | 10.2 (8.4-12.4) | 10.9 (7.9-14.9) | .3227 | 19.8 (16.1-24.1) | 23.1 (19.9-26.7) | 22.1 (18.5-26.2) | 16.1 (11.4-22.1) | .2322 |
| Model 2‡ | 9.1 (6.9-11.8) | 9.0 (6.8-11.9) | 10.9 (8.8-13.5) | 10.5 (6.9-15.6) | .4410 | 20.9 (15.5-27.5) | 22.3 (18.6-26.5) | 22.0 (17.3-27.5) | 16.9 (12.0-23.2) | .3332 |
P value for trends across the surveys using logistic regression models. All tests were 2-tailed.
Model 1 adjusted for age, sex, and race/ethnicity.
Model 2, in addition to variables in model 1, adjusted for smoking status, physical activity, HEI-2010, PIR, waist-to-height ratio, and BMI as continuous variables.
Discussion
Our results, derived from a series of nationally representative samples of adolescents, suggested that the adjusted pre-HBP prevalence remained largely unchanged among adolescents aged 12-19 years during 1988-2012. In contrast, the adjusted HBP prevalence was halved from 1999-2002 to 2007-2012 among overweight/obese adolescents. The observed decline in HBP prevalence could not be explained by sociodemographic changes or by selected risk factors such as age, sex, race/ethnicity, smoking status, physical activity, dietary factors, waist-to-height ratio, BMI, or income. The observed changes in pre-HBP and HBP prevalence were largely consistent across age group, sex, and race/ethnicity.
Using NHANES data, a number of studies have examined the temporal trends of BP, pre-HBP, and HBP;10-13,16 several studies indicated that the mean BP or pre-HBP and HBP prevalence rose significantly after 1999 compared with 1988-1994 and attributed the increase, at least partly, to rises in overweight and obesity.10,11,13,16 One study suggested that the HBP prevalence increased among girls and decreased among boys, comparing the results from 2003-2006 to those of 1988-1994.12 A recent study of children and adolescents aged 8-17 years suggested that HBP prevalence declined during 1999-2012.16
However, the findings of the Bogalusa Heart Study, which included 2 convenience samples of white and black children aged 7-9 years in 1973, who were followed up in 1981 and again in 1992, suggested that the levels of DBP and SBP, and the HBP prevalence did not increase despite significant rises in obesity. The study suggested potential problems with interpreting trends in BP and HBP prevalence based on only 2 time points.14 In fact, if we compare the age-sex-race/ethnicity-adjusted pre-HBP and HBP prevalence during 1988-1994 to that during 1999-2006, it increased from 14.7% (95% CI 12.9%-16.7%) to 18.0% (95% CI 16.3%-19.8%) (P = .010) among adolescents aged 12-19 years, consistent with these findings of other studies.10-13 After adjusting for the available covariates, some of which (eg, physical activity and HEI-2010) were not available in other studies, the adjusted prevalence was 16.4% (95% CI 14.2%-18.8%) vs 17.6% (95% CI 16.0%-19.4%) (P = .376). These results suggest that some of the increase in the combined pre-HBP and HBP prevalence might be explained by temporal trends in these covariates. In contrast, the findings on temporal trends in BP and HBP prevalence from other countries were inconsistent, some studies documented increased BP or HBP prevalence.28-30 Some investigators argue that the effect of changes in BMI on BP among children and adolescents is limited,30 and its association with BP declined over time.31 Still others indicate a decline in mean BP and/or HBP prevalence despite increasing levels of childhood overweight and obesity.8,15,32,33 We found significant interactions between time and BMI status on the prevalence of HBP. Our stratified results suggested that HBP, but not pre-HBP prevalence, declined significantly over time among both normal and overweight/obese US adolescents. The lack of temporal trends in pre-HBP prevalence did not imply BMI was not associated with BP. The nearly constant PR (~2.0) of pre-HBP by BMI status (Figure, A) indicated that BMI continued to be an important and consistent risk factor. Although since mid-2000 obesity among adolescents appears to be leveling off,2 continued efforts should be made to promote regular physical activity and healthy diets among adolescents to prevent overweight/obesity and reduce HBP.4,34
The reasons for the observed decline in HBP are unclear. Because the mean BMI among overweight/obese adolescents increased significantly over time, from 28.2 (95% CI 27.4-28.9) in 1988-1994 to 29.8 (29.4-32.2) in 2007-2012 (P < .001), we expected pre-HBP and HBP prevalence to increase, other things being equal, among overweight/obese adolescents because of the shifted BMI distribution toward right. NHANES used consistent methods to measure BP among adolescents during 1988-2012; detailed information about BP measurements, protocol, procedure, and quality control can be found online regarding NHANES III and NHANES 1999-2012 (http://www.cdc.gov/nchs/nhanes/survey_methods.htm). One other study documented signifi-cant decline in the prevalence of current smoking and elevated total cholesterol, and an increased prevalence of higher HEI-2010 scores during 1988-2010 among US adolescents aged 12-17 years.22 In our study, however, the results remained largely unchanged after adjusting for smoking status, HEI-2010, and other covariates.
Some investigators suggest that family history of HBP, which was not collected from adolescents in NHANES, is an independent predictor of developing HBP among adolescents.35-37 However, the HBP prevalence increased significantly among adults since 1988,38 which might not explain the significant decline in HBP prevalence among adolescents since 1999. It has been suggested that birth weight is an important determinant of childhood BP.39,40 Birth weight was not collected from adolescents in NHANES III, and NHANES only began collecting birth weight information in 1999 from adolescents aged 12-15 years; there was no evidence of any significant change in average birth weights among adolescents aged 12-15 years during 1999-2012 (results not shown). The syndrome known as “white-coat hypertension” might also present among adolescents and might affect the observed HBP prevalence.41,42 However, white-coat hypertension likely would not explain the consistent temporal decline in HBP prevalence and differences by BMI status. It is encouraging that the HBP prevalence among adolescents declined significantly since 1999, which might have significant public health consequences as adolescents mature. Further study is needed to determine the causes of the significant decline.
The main strengths of our study include the use of nationally representative data, the consistent methods used to measure BP across time, and adjustment using a comprehensive set of covariates to estimate pre-HBP and HBP prevalence.
Our analyses have some limitations. The multiple BP measurements were taken during a single visit to an MEC rather than over multiple visits as recommended by guidelines.4 Further study is needed to examine temporal trends in clinically diagnosed hypertension among overweight/obese adolescents. The observed significant decline in HBP prevalence should be interpreted with caution. Second, our adjustments included a comprehensive list of covariates, but not family history and birth weight, which might be important determinants of BP. Third, we were unable to control for confounding related to temporal changes in physical activity duration and intensity. Fourth, HEI-2010 was based on a single 24-hour dietary recall and may not reflect usual individual intake. In addition, the methodology for collecting 24-hour dietary recall in NHANES changed over time (http://www.cdc.gov/nchs/tutorials/dietary/index.htm). Fifth, multiple imputations for missing information may not accurately reflect actual values if data are not missing at random.
In summary, our findings indicate the pre-HBP prevalence among US adolescents remained largely unchanged during 1988-2012. The HBP prevalence declined significantly, among overweight/obese adolescents, though the decline cannot be explained by changes in sociodemographic and selected risk factors. Despite this significant decline in HBP prevalence, the estimated number of adolescents with pre-HBP and HBP increased during 1988-2012.
Glossary
- BMI
Body mass index
- BP
Blood pressure
- DBP
Diastolic BP
- FDR
False discovery rate
- HBP
High BP
- HEI-2010
Healthy eating index-2010
- MEC
Mobile examination center
- NHANES
National Health and Nutritional Examination Survey
- PIR
Poverty-income-ratio
- PR
Prevalence ratio
- SBP
Systolic BP
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors declare no conflicts of interest.
References
- 1.Troiano RP, Flegal KM, Kuczmarski RJ, Campbell SM, Johnson CL. Overweight prevalence and trends for children and adolescents. The National Health and Nutrition Examination Surveys, 1963 to 1991. Arch Pediatr Adolesc Med. 1995;149:1085–91. doi: 10.1001/archpedi.1995.02170230039005. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 19992010. JAMA. 2012;307:483–90. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(Suppl 4 4th Reprot):555–76. [PubMed] [Google Scholar]
- 5.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117:3171–80. doi: 10.1161/CIRCULATIONAHA.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention National Center for Health Statistics. Underlying Cause of Death 1999-2013 on CDC WONDER Online Database, released. 2015. [February 20, 2015]. http://wonder.cdc.gov/mcd.html.
- 7.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 8.Chiolero A, Bovet P, Paradis G, Paccaud F. Has blood pressure increased in children in response to the obesity epidemic? Pediatrics. 2007;119:544–53. doi: 10.1542/peds.2006-2136. [DOI] [PubMed] [Google Scholar]
- 9.McCrindle BW. Assessment and management of hypertension in children and adolescents. Nat Rev Cardiol. 2010;7:155–63. doi: 10.1038/nrcardio.2009.231. [DOI] [PubMed] [Google Scholar]
- 10.Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488–96. doi: 10.1161/CIRCULATIONAHA.106.683243. [DOI] [PubMed] [Google Scholar]
- 11.Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. Trends in blood pressure among children and adolescents. JAMA. 2004;291:2107–13. doi: 10.1001/jama.291.17.2107. [DOI] [PubMed] [Google Scholar]
- 12.Ostchega Y, Carroll M, Prineas RJ, McDowell MA, Louis T, Tilert T. Trends of elevated blood pressure among children and adolescents: data from the National Health and Nutrition Examination Survey 1988-2006. Am J Hypertens. 2009;22:59–67. doi: 10.1038/ajh.2008.312. [DOI] [PubMed] [Google Scholar]
- 13.Rosner B, Cook NR, Daniels S, Falkner B. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988-2008. Hypertension. 2013;62:247–54. doi: 10.1161/HYPERTENSIONAHA.111.00831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freedman DS, Goodman A, Contreras OA, DasMahapatra P, Srinivasan SR, Berenson GS. Secular trends in BMI and blood pressure among children and adolescents: the Bogalusa Heart Study. Pediatrics. 2012;130:e159–66. doi: 10.1542/peds.2011-3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watkins D, McCarron P, Murray L, Cran G, Boreham C, Robson P, et al. Trends in blood pressure over 10 years in adolescents: analyses of cross sectional surveys in the Northern Ireland Young Hearts project. BMJ. 2004;329:139. doi: 10.1136/bmj.38149.510139.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kit BK, Kuklina E, Carroll MD, Ostchega Y, Freedman DS, Ogden CL. Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999-2012. JAMA Pediatr. 2015;169:272–9. doi: 10.1001/jamapediatrics.2014.3216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Center for Health Statistics National Health and Nutrition Examination Survey. Questionnaires, Datasets, and Related Documentation. [January 8, 2014]. http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
- 18.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 19.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;246:1–190. [PubMed] [Google Scholar]
- 20.Kahn HS, Imperatore G, Cheng YJ. A population-based comparison of BMI percentiles and waist-to-height ratio for identifying cardiovascular risk in youth. J Pediatr. 2005;146:482–8. doi: 10.1016/j.jpeds.2004.12.028. [DOI] [PubMed] [Google Scholar]
- 21.Benowitz NL, Bernert JT, Caraballo RS, Holiday DB, Wang J. Optimal serum cotinine levels for distinguishing cigarette smokers and non-smokers within different racial/ethnic groups in the United States between 1999 and 2004. Am J Epidemiol. 2009;169:236–48. doi: 10.1093/aje/kwn301. [DOI] [PubMed] [Google Scholar]
- 22.Yang Q, Yuan K, Gregg EW, Loustalot F, Fang J, Hong Y, et al. Trends and clustering of cardiovascular health metrics among U.S. adolescents 1988-2010. J Adolesc Health. 2014;55:513–20. doi: 10.1016/j.jadohealth.2014.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HA, Kuczynski KJ, et al. Update of the healthy eating index: HEI-2010. J Acad Nutr Diet. 2013;113:569–80. doi: 10.1016/j.jand.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dalaker J, Proctor BD. Current Population Reports Series P60, No. 210. US Census Bureau; Washington, DC: 2000. [June 1, 2015]. Poverty in the United States: 1999. http://www.census.gov/hhes/www/poverty/publications/p60-210.pdf. [Google Scholar]
- 25.Research Triangle Institute . SUDAAN User's Manual, Release 10.0 Research. Research Triangle Institute; Triangle Park. NC: 2009. [Google Scholar]
- 26.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 2010;171:618–23. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- 27.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statist Soc B. 1995;57:289–300. [Google Scholar]
- 28.Kollias A, Antonodimitrakis P, Grammatikos E, Chatziantonakis N, Grammatikos EE, Stergiou GS. Trends in high blood pressure prevalence in Greek adolescents. J Hum Hypertens. 2009;23:385–90. doi: 10.1038/jhh.2008.166. [DOI] [PubMed] [Google Scholar]
- 29.Liang YJ, Xi B, Hu YH, Wang C, Liu JT, Yan YK, et al. Trends in blood pressure and hypertension among Chinese children and adolescents: China Health and Nutrition Surveys 1991-2004. Blood Press. 2011;20:45–53. doi: 10.3109/08037051.2010.524085. [DOI] [PubMed] [Google Scholar]
- 30.Peters H, Whincup PH, Cook DG, Law C, Li L. Trends in blood pressure in 9- to 11-year-old children in the United Kingdom 1980-2008: the impact of obesity. J Hypertens. 2012;30:1708–17. doi: 10.1097/HJH.0b013e3283562a6b. [DOI] [PubMed] [Google Scholar]
- 31.Clarke R, Bennett DA, Parish S, Verhoef P, Dotsch-Klerk M, Lathrop M, et al. Homocysteine and coronary heart disease: meta-analysis of MTHFR case-control studies, avoiding publication bias. PLoS Med. 2012;9:e1001177. doi: 10.1371/journal.pmed.1001177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khang YH, Lynch JW. Exploring determinants of secular decreases in childhood blood pressure and hypertension. Circulation. 2011;124:397–405. doi: 10.1161/CIRCULATIONAHA.110.014399. [DOI] [PubMed] [Google Scholar]
- 33.Chiolero A, Paradis G, Madeleine G, Hanley JA, Paccaud F, Bovet P. Discordant secular trends in elevated blood pressure and obesity in children and adolescents in a rapidly developing country. Circulation. 2009;119:558–65. doi: 10.1161/CIRCULATIONAHA.108.796276. [DOI] [PubMed] [Google Scholar]
- 34.Barlow SE, Expert C. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 35.Munger RG, Prineas RJ, Gomez-Marin O. Persistent elevation of blood pressure among children with a family history ofhypertension: the Minneapolis Children's Blood Pressure Study. J Hypertens. 1988;6:647–53. doi: 10.1097/00004872-198808000-00008. [DOI] [PubMed] [Google Scholar]
- 36.van den Elzen AP, de Ridder MA, Grobbee DE, Hofman A, Witteman JC, Uiterwaal CS. Families and the natural history of blood pressure. A 27-year follow-up study. Am J Hypertens. 2004;17:936–40. doi: 10.1016/j.amjhyper.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 37.Shear CL, Burke GL, Freedman DS, Berenson GS. Value of childhood blood pressure measurements and family history in predicting future blood pressure status: results from 8 years of follow-up in the Bogalusa Heart Study. Pediatrics. 1986;77:862–9. [PubMed] [Google Scholar]
- 38.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303:2043–50. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 39.Franco MC, Christofalo DM, Sawaya AL, Ajzen SA, Sesso R. Effects of low birth weight in 8- to 13-year-old children: implications in endothe-lial function and uric acid levels. Hypertension. 2006;48:45–50. doi: 10.1161/01.HYP.0000223446.49596.3a. [DOI] [PubMed] [Google Scholar]
- 40.Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2009;120:1011–20. doi: 10.1161/CIRCULATIONAHA.109.192627. [DOI] [PubMed] [Google Scholar]
- 41.Sorof JM, Poffenbarger T, Franco K, Portman R. Evaluation of white coat hypertension in children: importance of the definitions of normal ambulatory blood pressure and the severity of casual hypertension. Am J Hypertens. 2001;14:855–60. doi: 10.1016/s0895-7061(01)02180-x. [DOI] [PubMed] [Google Scholar]
- 42.Sorof JM, Portman RJ. White coat hypertension in children with elevated casual blood pressure. J Pediatr. 2000;137:493–7. doi: 10.1067/mpd.2000.108394. [DOI] [PubMed] [Google Scholar]