Abstract
Rationale
The “Berlin definition” of acute respiratory distress syndrome (ARDS) does not allow inclusion of patients receiving high-flow nasal oxygen (HFNO). However, several articles have proposed that criteria for defining ARDS should be broadened to allow inclusion of patients receiving HFNO.
Objectives
To compare the proportion of patients fulfilling ARDS criteria during HFNO and soon after intubation, and 28-day mortality between patients treated exclusively with HFNO and patients transitioned from HFNO to invasive mechanical ventilation (IMV).
Methods
From previously published studies, we analyzed patients with coronavirus disease (COVID-19) who had PaO2/FiO2 of ⩽300 while treated with ⩾40 L/min HFNO, or noninvasive ventilation (NIV) with positive end-expiratory pressure of ⩾5 cm H2O (comparator). In patients transitioned from HFNO/NIV to invasive mechanical ventilation (IMV), we compared ARDS severity during HFNO/NIV and soon after IMV. We compared 28-day mortality in patients treated exclusively with HFNO/NIV versus patients transitioned to IMV.
Measurements and Main Results
We analyzed 184 and 131 patients receiving HFNO or NIV, respectively. A total of 112 HFNO and 69 NIV patients transitioned to IMV. Of those, 104 (92.9%) patients on HFNO and 66 (95.7%) on NIV continued to have PaO2/FiO2 ⩽300 under IMV. Twenty-eight-day mortality in patients who remained on HFNO was 4.2% (3/72), whereas in patients transitioned from HFNO to IMV, it was 28.6% (32/112) (P < 0.001). Twenty-eight-day mortality in patients who remained on NIV was 1.6% (1/62), whereas in patients who transitioned from NIV to IMV, it was 44.9% (31/69) (P < 0.001). Overall mortality was 19.0% (35/184) and 24.4% (32/131) for HFNO and NIV, respectively (P = 0.2479).
Conclusions
Broadening the ARDS definition to include patients on HFNO with PaO2/FiO2 ⩽300 may identify patients at earlier stages of disease but with lower mortality.
Keywords: COVID-19, ARDS, HFNO, mechanical ventilation, noninvasive ventilation
At a Glance Commentary
Scientific Knowledge on the Subject
Currently, the Berlin oxygenation criterion requires that patients must be on invasive mechanical ventilation (IMV) with a positive end-expiratory pressure (PEEP) of ⩾5 cm H2O, with the exception of mild acute respiratory distress syndrome (ARDS), in which patients can be receiving PEEP during noninvasive ventilation (NIV) or receiving continuous positive airway pressure of ⩾5 cm H2O. To make the diagnosis of ARDS more widely applicable and independent of the need for IMV, several studies have suggested that the Berlin definition’s oxygenation criterion be broadened to include patients on high-flow nasal oxygen (HFNO), since an HFNO flow of >40 L/min generates a PEEP of ∼5 cm H2O. However, there is a paucity of empirical data to fully support this recommendation.
What This Study Adds to the Field
After institution of IMV, 7.1% of HFNO patients and 4.3% of NIV patients with PaO2/FIO2 ratio ⩽300 mm Hg and bilateral chest infiltrates lost ARDS criteria. However, mortality was substantially lower in HFNO patients than in those subsequently intubated. Thus, allowing the diagnosis of ARDS in patients on HFNO may allow identification of patients at an earlier stage of the syndrome; however, this may select a different cohort of patients with substantially lower mortality.
Acute respiratory distress syndrome (ARDS) is a severe form of acute hypoxemic respiratory failure not resulting from congestive heart failure or fluid overload (1). Although the “conceptual model” of ARDS (2) has not changed greatly since its original description (3), the formal definition of ARDS has undergone multiple modifications, occasionally with some degree of controversy (4). The most recent update in 2012, the so called “Berlin definition,” classified ARDS as “mild,” “moderate,” or “severe” when the PaO2/FiO2 was 200–300, 100–200, and <100 mm Hg, respectively (5). The definition required that the PaO2/FiO2 criteria be obtained while the patient was receiving invasive mechanical ventilation with ⩾5 cm H2O of positive end-expiratory pressure (PEEP). For mild ARDS, the definition allowed the PaO2/FiO2 criterion to be met while continuous positive airway pressure (CPAP) was delivered noninvasively (5).
One major criticism of the Berlin definition is that it does not allow inclusion of patients early in the lung injury process (6–9) and excludes patients on high-flow nasal oxygen (HFNO) (10). HFNO delivers heated and humidified oxygen via the nose at flows of ⩽60 L/min at oxygen concentrations up to 80–100% (11, 12) and is increasingly being used to support patients with hypoxemic respiratory failure (13–16). To address these concerns, a number of authors have proposed that criteria for defining ARDS should be broadened to allow inclusion of patients receiving HFNO (10, 17, 18). However, there is a paucity of empirical data to fully support this recommendation.
The present study set out to examine some of the implications of allowing patients on HFNO to be categorized as having ARDS. We analyzed data from four published studies during the coronavirus disease (COVID-19) pandemic (19–22) and focused on two major study outcomes. First, in the subset of patients who transitioned from HFNO to invasive mechanical ventilation (IMV), we compared the proportion of patients fulfilling ARDS criteria during HFNO and soon after intubation. Second, we compared 28-day mortality between patients treated exclusively with HFNO and patients who transitioned from HFNO to IMV. Patients initially treated with noninvasive ventilation (NIV) were used as a comparator group.
Methods
This study is a secondary analysis of data from four previously published studies performed in Italy from February to December 2020 that enrolled patients with acute hypoxemic respiratory failure secondary to confirmed COVID-19 (19–22). Patients were selected if all the following inclusion criteria were met: 1) worsening respiratory symptoms due to severe COVID-19 for ⩽1 week; 2) bilateral opacities on standard chest X-ray consistent with ARDS (23); 3) PaO2/FiO2 ⩽300 mm Hg; and 4) patients initially treated for ⩾12 continuous hours with HFNO using gas flows of ⩾40 L/min, or treated with NIV with PEEP of ⩾5 cm H2O. Exclusion criteria were 1) treated with IMV since the onset of respiratory failure; 2) treated with more than one mode (e.g., HFNO/NIV/CPAP) at the onset of respiratory failure; 3) underwent awake prone positioning; 4) had incomplete records for the variables of interest; or 5) had a “do not intubate/do not resuscitate” order. Details of enrollment criteria for each study are in the online supplement.
Study outcomes were 1) in the subset of patients transitioned from noninvasive ventilatory support (HFNO or NIV) to IMV, we compared the proportion of patients fulfilling ARDS criteria and the proportion of patients who fulfilled the oxygenation criteria for “mild,” “moderate,” and “severe” ARDS during HFNO or NIV, and after intubation; and 2) 28-day mortality in patients treated with HFNO or NIV who did not transition to IMV versus the 28-day mortality in patients transitioned to IMV. We examined the association between changes in PaO2/FiO2 after IMV and flow rate during HFNO, or the level of PEEP during NIV. We also examined mortality and change in PaO2/FiO2 after initiation of IMV in patients initially treated with HFNO versus NIV.
We recorded the first arterial blood gases collected within the initial 12 hours of treatment with HFNO or NIV. In patients who transitioned from noninvasive ventilatory support (HFNO or NIV) to IMV, blood gases were collected before intubation (i.e., the final blood gas before intubation), and 30–120 minutes after intubation. Chest radiographs were evaluated for pulmonary infiltrates consistent with ARDS (23). We examined changes in PaO2/FiO2 ratios after intubation, as well as 28-day mortality using different PaO2/FiO2 cutoffs (24).
Continuous variables were expressed as medians and interquartile range, categorical variables as absolute and percentage frequencies. Comparison of continuous data between samples was done using Mann-Whitney or Kruskal-Wallis test; comparison of paired continuous variables was performed with Wilcoxon signed-rank test. Comparison of categorical data was done using χ2 or Fisher’s exact test; paired categorical data was compared with McNemar test. Correlation between continuous variables was assessed with Spearman’s correlation. Logistic regression was used to compare mortality in patients undergoing HFNO and NIV and to test the effects of different variables on mortality. Multivariable logistic regression analysis was used to adjust the odds of mortality in HFNO versus NIV for relevant confounders. All statistical tests were two-sided. Significance level was set at P < 0.05, and no imputation of missing data was necessary as there were no missing data for key variables. Analyses were done using R software version 4.0.5 and GraphPad Prism version 9.1.
Results
Among the 2,358 patients with documented COVID-19 enrolled in the four studies, 184 receiving HFNO and 131 receiving NIV had bilateral radiographic opacities consistent with ARDS, respiratory symptoms occurring/worsening <1 week from study admission, and PaO2/FiO2 ⩽300. Remaining patients were excluded for the following reasons: respiratory symptoms for >1 week (n = 25); no bilateral opacities on chest X-ray (n = 101); PaO2/FiO2 >300 mm Hg (n = 28); treated with IMV since the onset of respiratory failure (n = 971); received a combination of NIV/HFNO/CPAP at the onset of respiratory failure (n = 553); received awake prone positioning (n = 50); do not intubate/do not resuscitate order in place (n = 212); and/or incomplete records for the variables of interest (n = 103) (Figure 1).
Figure 1.
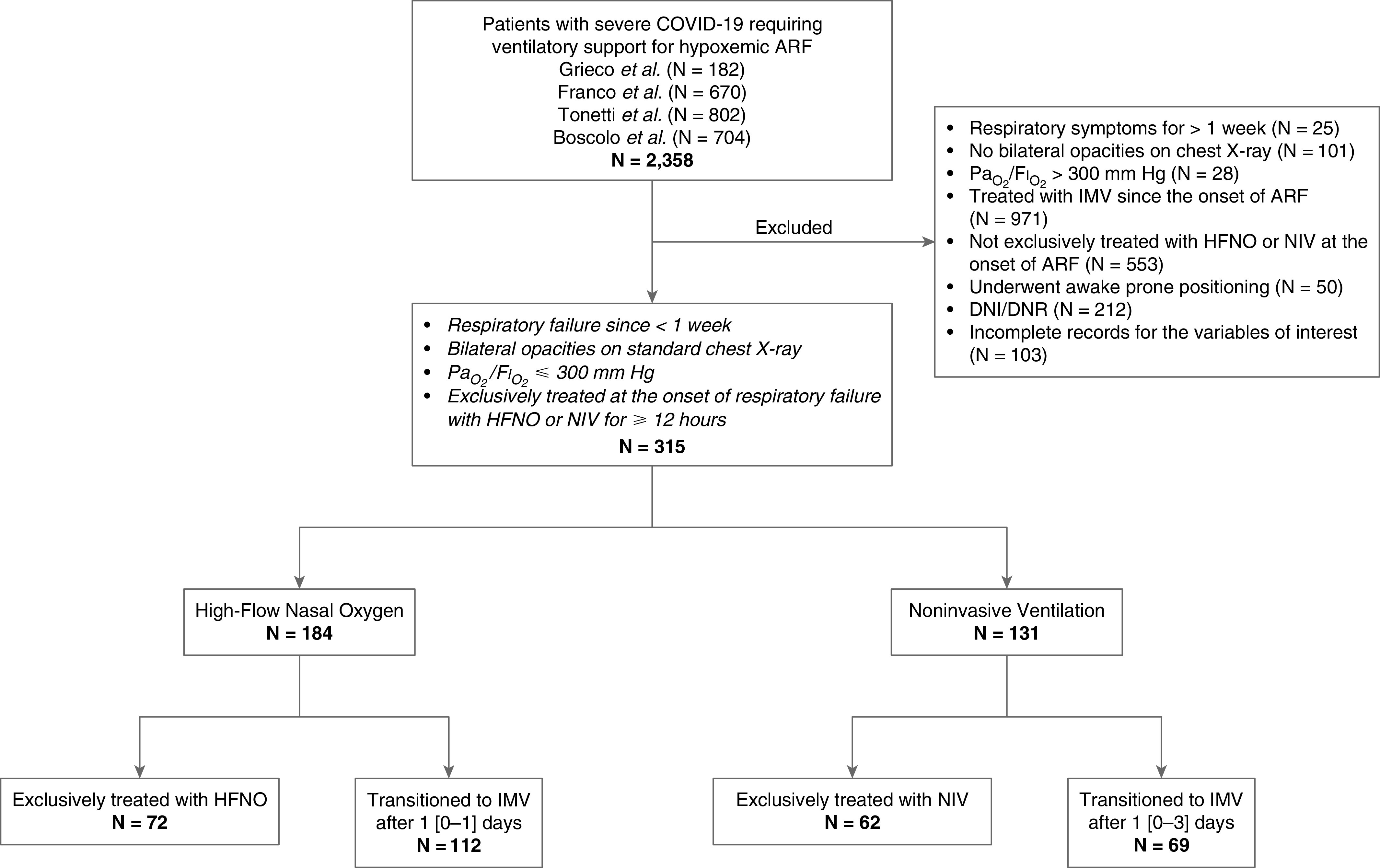
Flow chart of the study. ARF = acute respiratory failure; COVID-19 = coronavirus disease; DNI/DNR = “do not intubate/do not resuscitate” order; HFNO = high-flow nasal oxygen; IMV = invasive mechanical ventilation; NIV = noninvasive ventilation.
Table 1 presents relevant variables at study inclusion during HFNO/NIV. HFNO (flow 55 [50–60] L/min) was started 2 (1–3) days from hospital admission. NIV (pressure support level 10 [10–12] cm H2O and PEEP 10 [10–12] cm H2O) was started 2 (1–4) days from hospital admission. A total of 112 (60.9%) patients with HFNO and 69 (52.7%) with NIV were intubated and received mechanical ventilation for severe hypoxemia not responding to 1 (0–1) day and 1 (0–3) days of HFNO and NIV, respectively. Clinical and physiological variables in patients exclusively treated with HFNO or NIV and in patients transitioned from HFNO/NIV to IMV are reported in Tables E1A and E1B in the online supplement. Ventilatory settings after intubation are reported in Table E2.
Table 1.
Baseline Characteristics of the Patients Included in the Study
| HFNO (n = 184) | NIV (n = 131) | P Value | |
|---|---|---|---|
| Sex, M, n (%) | 144 (78.3) | 99 (75.6) | 0.5755 |
| Age, yr | 63 (54–71) | 67 (59–73) | 0.0122 |
| Weight, kg | 80 (74–90) | 80 (75–90) | 0.7456 |
| Height, cm | 174 (168–179) | 172 (170–177) | 0.8128 |
| BMI, kg/m2 | 27.4 (24.7–30.9) | 27.5 (25.5–29.8) | 0.8938 |
| SOFA score | 3 (2–4) | 2 (2–3) | 0.0009 |
| Time from hospital admission to HFNO/NIV start, d | 2 (1–3) | 2 (1–4) | 0.4604 |
| HFNO flow, L/min | 55 (50–60) | — | — |
| NIV PEEP, cm H2O | — | 10 (10–12) | — |
| NIV pressure support, cm H2O | — | 10 (10–12) | — |
| PaO2, mm Hg | 79 (68–89) | 79 (69–92) | 0.1728 |
| FiO2, % | 60 (60–60) | 60 (50–70) | 0.8422 |
| PaO2/FiO2 ratio, mm Hg | 128 (107–163) | 147 (121–178) | 0.0021 |
| PaCO2, mm Hg | 35 (33–37) | 35 (31–39) | 0.8265 |
| pH, units | 7.46 (7.44–7.48) | 7.45 (7.43–7.48) | 0.1320 |
Definition of abbreviations: BMI = body mass index; HFNO = high-flow nasal oxygen; NIV = noninvasive ventilation; PEEP = positive end-expiratory pressure; SOFA = sequential organ failure assessment.
Data are median (interquartile range) unless otherwise indicated.
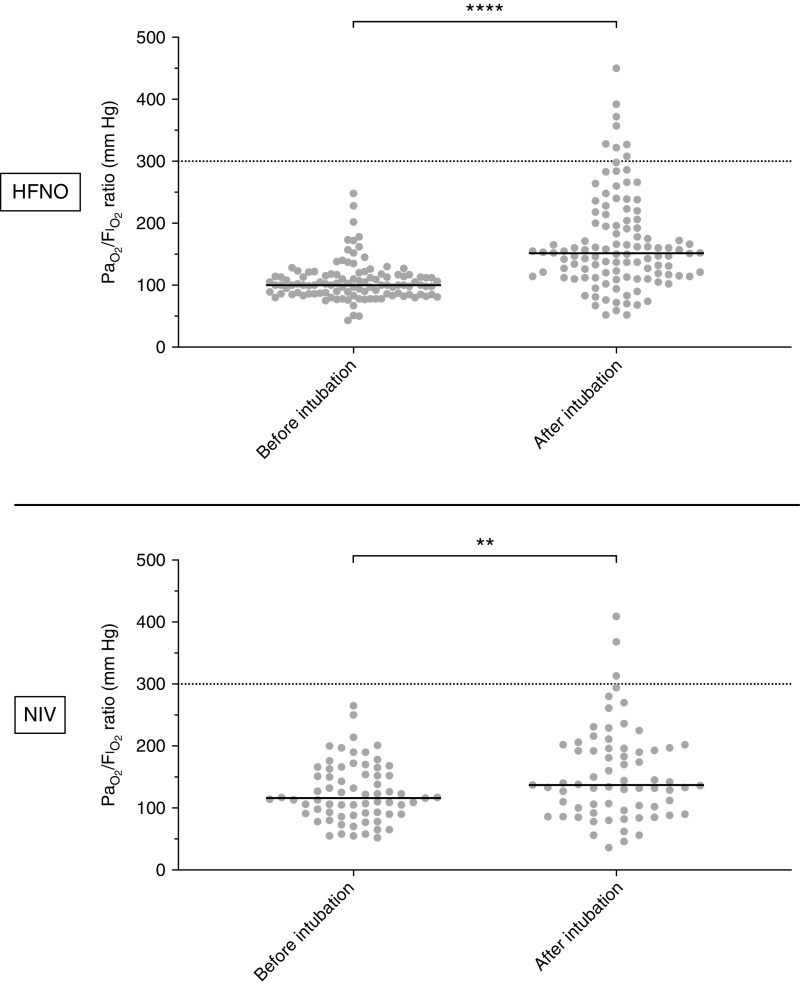
In patients who transitioned from HFNO to IMV, median PaO2/FiO2 increased from 100 (86–115) during HFNO to 152 (115–201) mm Hg after initiation of IMV (P < 0.0001) (Figure 2, top); 91 (81.3%) patients had an increase in PaO2/FiO2, and 21 (18.8%) had a decrease after IMV. In the subset who transitioned from NIV to IMV, median PaO2/FiO2 increased from 116 (91–154) to 137 (100–196) mm Hg after initiation of IMV (P = 0.0013) (Figure 2, bottom); 45 (65.2%) patients had an increase in PaO2/FiO2 and 24 (34.8%) had a decrease after IMV. Shortly after intubation, 92.9% (104/112) of patients who had PaO2/FiO2 of ⩽300 mm Hg while on HFNO, and 95.7% (66/69) on NIV, continued to have PaO2/FiO2 of ⩽300 mm Hg. The proportion of patients on HFNO who lost ARDS criteria after intubation (7.1% [8/112]) was not different from the proportion of patients on NIV who lost ARDS criteria after intubation (4.3% [3/69]; P = 0.5363].
Figure 2.
Values of PaO2/FiO2 ratio before and after intubation in patients treated with HFNO (top) and with NIV (bottom). Horizontal solid lines indicate median values of PaO2/FiO2. Horizontal dotted line indicates the cutoff value of PaO2/FiO2 (⩽300) below which patients are classified as having acute respiratory distress syndrome. Definition of abbreviations. HFNO = high-flow nasal oxygen; NIV = noninvasive ventilation. **P = 0.0013 and ****P < 0.0001.
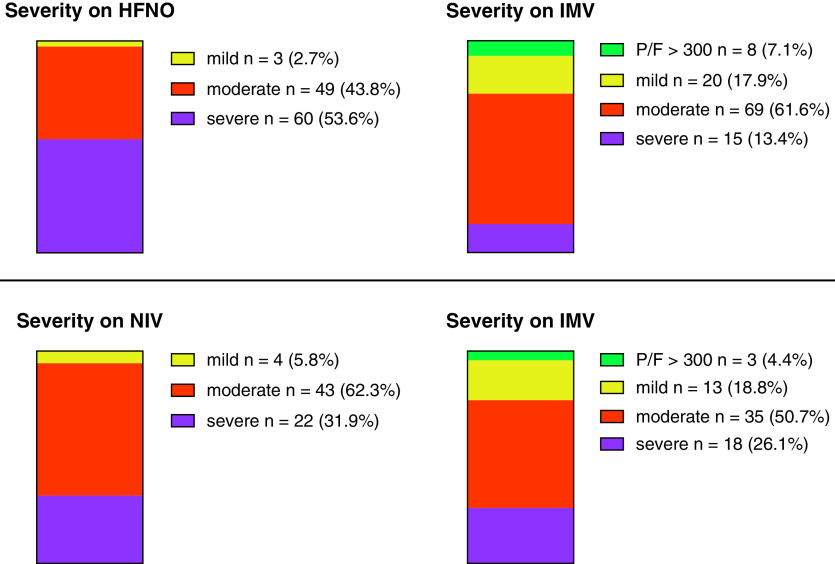
Figure 3, top, and Figure E2, top, show severity categories during HFNO and shortly after institution of IMV. Three patients with “mild” ARDS before intubation continued to have “mild” ARDS after IMV. For “moderate” ARDS, ∼10% lost ARDS criteria (PaO2/FiO2 > 300 mm Hg), ∼20% had “mild” ARDS, ∼60% had no change in severity, and ∼10% had “severe” ARDS after IMV. For “severe” ARDS, ∼20% maintained the same severity after IMV and ∼60% had “moderate” ARDS. Remaining patients lost PaO2/FiO2 criteria for ARDS or were classified as “mild” ARDS. In patients on HFNO, ARDS severity decreased significantly after intubation (Wilcoxon’s test: Z = 7.39; P < 0.001). Figure 3, bottom, and Figure E2, bottom, present patients classified by ARDS severity during NIV and shortly after institution of IMV. Among the 69 patients on NIV, 66 patients (95.7%) continued to have PaO2/FiO2 of ⩽300 mm Hg after intubation. There were only four patients with “mild” ARDS; of these, two remained “mild” and two had “moderate” ARDS after intubation. For “moderate” ARDS while on NIV , ∼60% maintained the same severity, ∼5% lost criteria, ∼20% had “mild” ARDS, and ∼15% had “severe” ARDS, after institution of IMV . For patients on NIV classified as “severe” ARDS, after intubation, ∼50% remained severe, ∼30% had “moderate” ARDS, ∼10% had “mild” ARDS, and ∼10% lost ARDS criteria. In patients on NIV, ARDS severity decreased significantly after intubation (Wilcoxon’s test: Z = 4.22; P = 0.001).
Figure 3.
Percentage distribution in the different severity classes before and after institution of IMV for patients on HFNO (top) and NIV (bottom). See text for more details. HFNO = high-flow nasal oxygen; IMV = invasive mechanical ventilation; NIV = noninvasive ventilation; P/F = PaO2/FIO2 ratio.
Figure 4 shows 28-day mortality in patients initially treated with HFNO (left) and NIV (right). Mortality in patients treated with HFNO who were not intubated was 4.2% (3/72), whereas in patients transitioned from HFNO to IMV, mortality was 28.6% (32/112) (P < 0.001). Mortality in patients treated with NIV but not intubated was 1.6% (1/62), whereas in patients who transitioned from NIV to IMV, mortality was 44.9% (31/69) (P < 0.001). Overall mortality in patients initially treated with HFNO and NIV was 19.0% (35/184) and 24.4% (32/131), respectively (P = 0.2479). Table E3 presents the comparison of mortality between HFNO and NIV patients using logistic regression and multiple logistic regression analysis. Mortality was similar in the two groups in univariate analysis (HFNO vs. NIV odds ratio = 0.727; 95% confidence interval, 0.422–1.250) and after adjusting for covariates (odds ratio = 0.603; 95% confidence interval, 0.320–1.137).
Figure 4.
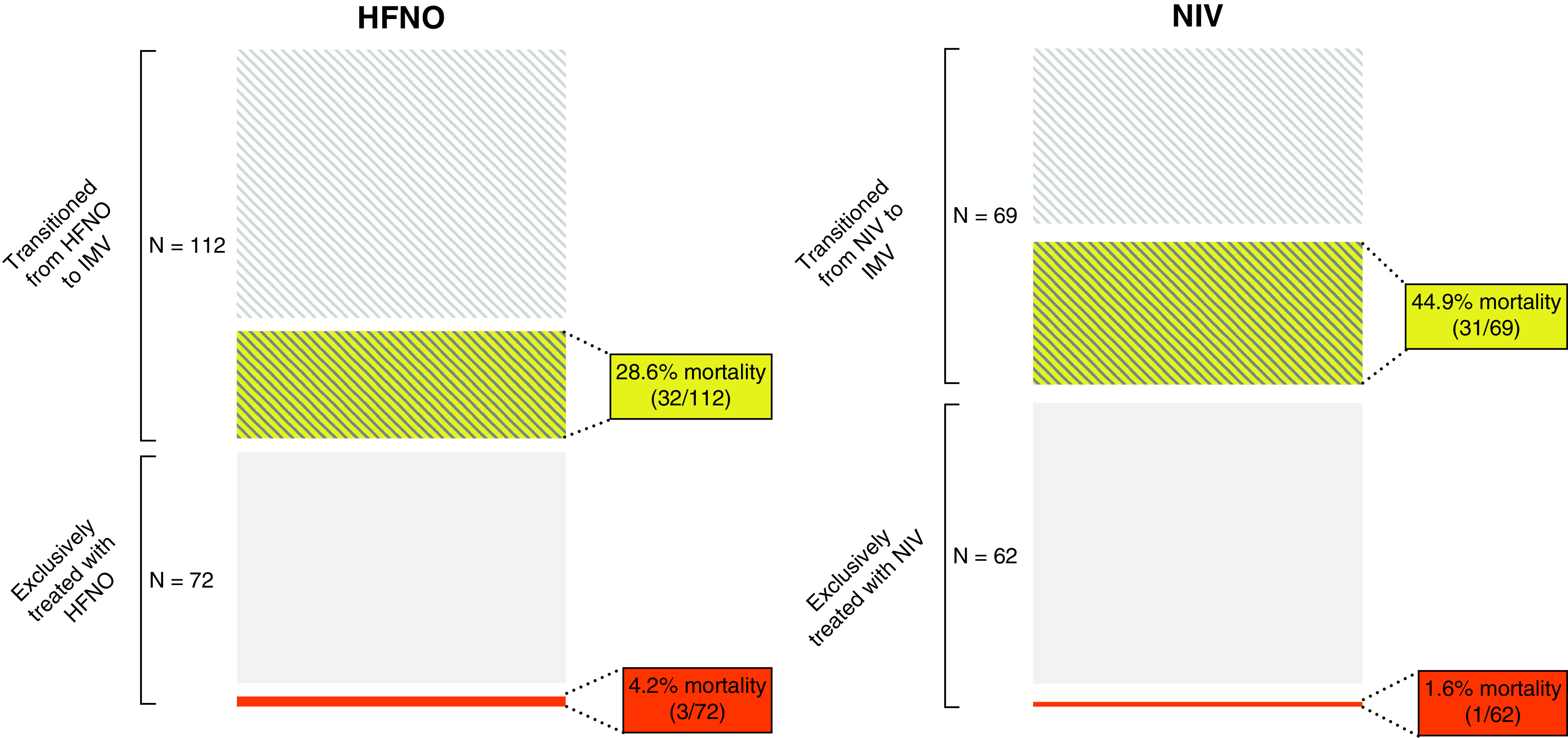
Mortality at Day 28 in the HFNO (left) and NIV (right) groups. Mortality in patients treated with HFNO who were not intubated was 4.2% (3/72), whereas in patients transitioned from HFNO to IMV, mortality was 28.6% (32/112) (P < 0.001). Mortality in patients treated with NIV but not intubated was 1.6% (1/62), whereas in patients who transitioned from NIV to IMV, mortality was 44.9% (31/69) (P < 0.001). Overall mortality in patients initially treated with HFNO and NIV was 19.0% (35/184) and 24.4% (32/131), respectively (P = 0.2479). HFNO = high-flow nasal oxygen; IMV = invasive mechanical ventilation; NIV = noninvasive ventilation.
The relationship between ARDS severity and mortality differed depending on whether patients were receiving HFNO or IMV (Table 2). Patients treated with HFNO and classified after intubation as having severe ARDS had almost double the 28-day mortality of patients who had a PaO2/FiO2 of ⩽100 before intubation (∼46.7% vs. ∼26.7%; McNemar’s test = 31.3; P < 0.001). This was not the case for patients with severe ARDS initially treated with NIV (McNemar’s test = 0.063; P = 0.804).
Table 2.
28-Day Mortality according to Severity before and after IMV
| Mild | Moderate | Severe | P Value | |
|---|---|---|---|---|
| 28-d mortality in the HFNO group | ||||
| Severity based on blood gas within first 12 h on HFNO | 7.7% (1/13) | 19.3% (27/140) | 22.6% (7/31) | 0.327 |
| Severity based on last HFNO blood gas before IMV | 0.0% (0/3) | 32.7% (16/49) | 26.7% (16/60) | 0.768 |
| Severity based on first blood gas on IMV | 25.0% (5/20) | 29.0% (20/69) | 46.7% (7/15) | 0.202 |
| 28-d mortality in the NIV group | ||||
| Severity based on blood gas within first 12 h on NIV | 10.5% (2/19) | 21.2% (21/92) | 45.0% (9/20) | 0.012 |
| Severity based on last NIV blood gas before IMV | 25.0% (1/4) | 48.8% (21/43) | 40.9% (9/22) | 0.887 |
| Severity based on first blood gas on IMV | 46.2% (6/13) | 48.6% (17/35) | 38.9% (7/18) | 0.634 |
Definition of abbreviations: HFNO = high-flow nasal oxygen; IMV = invasive mechanical ventilation; NIV = noninvasive ventilation.
Table 3 compares the 28-day mortality between patients transitioned and not transitioned to IMV using different PaO2/FiO2 cutoff values. There was a significant difference between the two groups at each cutoff, except for PaO2/FiO2 of ⩽100. The percentage of patients who lost ARDS oxygenation criteria after IMV according to different PaO2/FiO2 cutoff values is presented in Table E4.
Table 3.
28-Day Mortality according to Different PaO2/FiO2 Cutoffs
| Blood gas within First 12 h of HFNO or NIV | Exclusively Treated with HFNO | Transitioned from HFNO to IMV | P for Fisher’s Exact Test | Exclusively Treated with NIV | Transitioned from NIV to IMV | P for Fisher’s Exact Test |
|---|---|---|---|---|---|---|
| PaO2/FiO2 ⩽300 mm Hg | 3/72 (4.2%) | 32/112 (28.6%) | <0.0001 | 1/62 (1.6%) | 31/69 (44.9%) | <0.0001 |
| PaO2/FiO2 ⩽250 mm Hg | 3/71 (4.2%) | 31/111 (27.9%) | <0.0001 | 1/59 (1.7%) | 31/65 (47.7%) | <0.0001 |
| PaO2/FiO2 ⩽200 mm Hg | 3/64 (4.7%) | 31/107 (29.0%) | <0.0001 | 1/53 (1.9%) | 29/59 (49.2%) | <0.0001 |
| PaO2/FiO2 ⩽150 mm Hg | 2/41 (4.9%) | 26/84 (31.0%) | 0.001 | 1/31 (3.2%) | 20/40 (50.0%) | <0.0001 |
| PaO2/FiO2 ⩽100 mm Hg | 0/4 (0.0%) | 7/27 (25.9%) | 0.55 | 0/4 (0.0%) | 9/16 (56.3%) | 0.0941 |
For definition of abbreviations, see Table 2.
The relationship between gas flow during HFNO and changes in PaO2/ FiO2 after IMV was not significant (Spearman’s rho = 0.044; P = 0.6520). Higher PEEP levels during NIV were associated with greater increases in PaO2/FiO2 after IMV (rho = 0.361; P = 0.004) (Figure E1). Changes in PaO2/FiO2 after IMV were unrelated to PEEP (during IMV) in patients treated initially with HFNO or with NIV (rho = 0.097; P = 0.33, and rho = 0.03; P = 0.8150, for HFNO and NIV groups, respectively) (Figure E1).
Discussion
In the present study, we provide data to help address how, in patients with COVID-19 with bilateral infiltrates consistent with ARDS treated with HFNO, the assessment of severity of hypoxemia based on PaO2/FiO2 may change after transition from HFNO to IMV. Our data provide some support that the hypoxemia criterion of ARDS based on PaO2/FiO2 can be applied to patients on HFNO in that only 7.1% of patients treated with HFNO lost ARDS criteria immediately after intubation. However, our data also show that ARDS severity categories changed substantially after intubation, and 28-day mortality in patients treated exclusively with HFNO was significantly lower than in patients who transitioned from HFNO to IMV (4.2% vs. 28.6%; P < 0.001). Thus, allowing patients initially treated with HFNO to be categorized as having ARDS could lead to identification of patients with different outcomes than patients diagnosed while on invasive ventilation. This may have great implications for clinical trials.
To identify patients in the initial stages of acute lung injury, several studies have proposed allowing the diagnosis of ARDS in patients not receiving IMV (6). Coudroy and coworkers found that most patients with bilateral pulmonary infiltrates and PaO2/FiO2 of ⩽300 mm Hg under conventional oxygen therapy still fulfilled ARDS criteria after NIV was initiated, with an overall mortality rate of 31% (7). Kangelaris and coworkers reported that mortality in patients meeting ARDS criteria (other than intubation) had a hospital mortality similar to patients with ARDS who were intubated early (26% vs. 30%, respectively) (8).
The Berlin definition states that patients being managed with noninvasive respiratory support can be diagnosed as having mild ARDS if their end-expiratory airway pressure is ⩾5 cm H2O and 300 mm Hg ⩾ PaO2/FiO2 > 200 mm Hg (5). However, the definition is somewhat ambiguous with respect to other severity categories, as there is no explicit guidance given. As such, Hernu and coworkers (25) interpreted the Berlin definition as not being able to classify patients on noninvasive support as having ARDS if their PaO2/FiO2 ratio was <200 mm Hg (5). However, Bellani and coworkers (26) and Zhao and coworkers (27) categorized patients treated with noninvasive support using all degrees of ARDS severity based on the PaO2/FiO2 ratio categories for invasively ventilated patients. For the purposes of this study, we compared the change in ARDS severity before and after intubation of our two cohorts (patients on HFNO and NIV) with the patients on NIV reported by Bellani and coworkers (26) (Table E5). We found that our patients on NIV for COVID-19 ARDS behaved similarly to patients with “conventional” ARDS after intubation (26).
There are several physiological mechanisms by which HFNO may improve outcomes: decreased dead space by washout of carbon dioxide, increased secretion clearance, decreased nasal resistance, decreased entrainment of ambient air and generating positive airway pressure similar to CPAP (11, 28). Groves and colleagues demonstrated that in healthy subjects, HFNO flow rates of 40–60 L/min could pressurize the airways up to 5–7 cm H2O (29). Papazian and colleagues reported values of end-expiratory pressure of ⩾5 cm H2O with flow rates of 60 L/min (12). Parke and coworkers found that for every 10-L/min increase in flow, there was an ∼0.7-cm H2O increase in generated pressure (30). This increase in end-expiratory pressure during HFNO provides the physiological rationale underpinning the proposal that patients on HFNO with flows of ⩾30 L/min should be considered to have ARDS if they fulfill all Berlin criteria except PEEP of ⩾5 cm H2O (10). Indeed, our data demonstrate that 93% of patients who fulfilled (nonintubation) ARDS criteria on HFNO at 40–60 L/min also fulfilled these criteria after intubation and ventilation.
In our study, the percentage of HFNO patients that lost ARDS criteria after intubation was similar to the percentage of NIV patients that lost ARDS criteria (7.1% vs. 4.3%; P = 0.5363). However, applying these criteria in patients on HFNO may require the adoption of a different “conceptual model” of ARDS that includes much less severely ill patients, as 1) many patients had a change in severity after transition from HFNO to IMV (for example, only 20% of patients with PaO2/FiO2 <100 during HFNO were classified as having “severe” ARDS after IMV; 2) mortality rate based on ARDS severity changed substantially depending on whether categorization was based on PaO2/FiO2 during HFNO or during IMV; and 3) mortality rate was substantially lower in patients on HFNO who were not intubated compared with patients who were intubated. Of course, the latter observation is expected given that less sick patients would not need to be intubated, a finding that has been previously reported in patients with COVID-19 (31). However, in the context of a clinical trial that enrolled patients based on PaO2/FiO2 while on HFNO or while on IMV, this could lead to recruitment of patients with substantially different mortality rates.
Although a comparison between HFNO and NIV was not the primary focus of our study, we examined the basic pathophysiological mechanisms underlying variations in PaO2/FiO2 after institution of IMV. We hypothesized that the higher the HFNO flow, the lower would be the difference in PaO2/FiO2 after intubation. Our findings did not confirm this hypothesis. This could be owing to the fact that our sample was limited to a relatively narrow range of flow rates (40–60 L/min), and thus the “effective” PEEP on HFNO would have been similar at all the HFNO flow rates; or it could be owing to variability in PEEP, and hence in PaO2, after intubation, which was set “clinically”. We did observe a positive association between PEEP on NIV and difference in PaO2/FiO2; this observation is perhaps counterintuitive. It is possible that PEEP level on NIV is more a marker of severity of respiratory failure and more severe patients may benefit from the transition to IMV. Another possible explanation is that higher PEEP levels during NIV may be associated with higher leaks, making this mode of ventilation less effective compared with IMV.
Strengths of our study include its multicenter design and the fact that it selected patients who were exclusively treated with HFNO (19–22) and were intubated without a NIV trial (32). However, there are several important limitations that should be taken into account in interpreting our results. First, there may be issues in generalizing our results. We included only patients with COVID-19 ARDS, and this could represent a problem in generalizing to ARDS from other causes. As well, all patients included in the comparison of PaO2/FiO2 before and after intubation transitioned to IMV because of respiratory worsening. As such, these patients represent the most severe patients. In addition, our sample may have intrinsic heterogeneity as it is a post hoc analysis of data collected for observational (20–22) or interventional (19) studies. Some of the patients were treated outside ICUs (20, 21), and patients in the trial by Grieco and coworkers were randomized to HFNO or NIV before requiring higher levels of respiratory support (19). This could have modified timing for intubation and/or mortality. However, our dataset (n = 315 out of 2,385) only selected patients from the previous four studies for whom clinicians were committed to full support (Figure 1). Consistently, in Tonetti and coworkers’ study, 28-day mortality of patients receiving noninvasive ventilatory support outside the ICU was not substantially different from the 28-day mortality observed in patients treated in the ICU (52.1 vs. 47.3%; P = 0.01) (21). Second, HFNO flow rates were in a relatively narrow range between 40 and 60 L/min, and thus we cannot directly address whether patients treated with lower flow rates would have similar PaO2/FiO2 ratios before and after intubation (Figure 3). Third, we had a relatively small sample size despite starting with a relatively large cohort. This meant we had very few patients with mild ARDS before intubation, so we cannot draw any definitive conclusion on this severity group. However, based on the moderate and severe patient data (∼60-mm Hg increases in PaO2/FiO2 after intubation), it is tempting to speculate that many patients diagnosed with mild ARDS on HFNO would not meet oxygenation criteria for ARDS after intubation.
Conclusions
Our data suggest that categorizing hypoxemic patients with bilateral infiltrates who are treated with HFNO as having ARDS may permit identification of patients at an earlier stage of the natural history of acute lung injury both in the context of clinical trials and clinical management. However, this may select patients with lower mortality and thus have important implications in terms of recruitment of patients into clinical trials.
Acknowledgments
Acknowledgment
The authors thank all the ICU doctors, nurses, and personnel who strenuously fought against COVID-19 and supported this research. They also thank Cecilia Berardi, Filippo Bongiovanni, Salvatore Lucio Cutuli (Università Cattolica del Sacro Cuore, Rome, Italy Department of Anesthesiology and Intensive Care Medicine, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy), and Giulia Panzuti (Alma Mater Studiorum–Università di Bologna) for their collaboration.
Footnotes
Supported in part by Progetti di Ricerca di Interesse Nazionale, Ministero dell’Istruzione, dell’Università e della Ricerca (PRIN 2017, project J4BE7A) of the Italian Ministry of University; Ricerca Finalizzata of the Italian Ministry of Health, Ministero della Salute (project PB-0154 PROGETTO COVID-2020-12371675); and the Canadian Institutes of Health Research (grants 137772 and OV3-170344).
Author Contributions: V.M.R., T.T., and A.S.S. were responsible for study design, data analysis, data interpretation, and preparing the first draft of the manuscript. V.M.R., T.T., P.N., S.N., M.A., A.P., G.G., D.L.G., L.S.M., L.P., A.B., N.S., L.P., C.M., G.P., A.D.’O., R.D., and A.S.S. were responsible for data acquisition and data interpretation. P.R. and T.T. performed statistical analysis. V.M.R., T.T., P.R., and A.S.S. finalized the manuscript. V.M.R., T.T., and A.S.S. are responsible for study data integrity. All authors reviewed the manuscript and approved its final submitted version.
Deidentified individual participant data that underlie results reported in this article will be available. Applicant must provide: 1) a methodologically sound approach to achieve scientific aims; and 2) formal ethics committee approval of the applicant’s institution. Data will be made available pending authorization of the Policlinico di Sant’Orsola Ethics Committee, which will review the applicant’s request, and after signing an appropriate data sharing agreement. Proposals should be directed to m.ranieri@unibo.it. Data will be available after publication, no end date.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.202109-2163OC on December 3, 2021
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Thompson BT, Chambers RC, Liu KD. Acute respiratory distress syndrome. N Engl J Med . 2017;377:562–572. doi: 10.1056/NEJMra1608077. [DOI] [PubMed] [Google Scholar]
- 2. Rubenfeld GD. Epidemiology of acute lung injury. Crit Care Med . 2003;31:S276–S284. doi: 10.1097/01.CCM.0000057904.62683.2B. [DOI] [PubMed] [Google Scholar]
- 3. Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults Lancet 1967. 2 319 323 4143721 [Google Scholar]
- 4. Villar J, Blanco J, Kacmarek RM. Acute respiratory distress syndrome definition: do we need a change? Curr Opin Crit Care . 2011;17:13–17. doi: 10.1097/MCC.0b013e32834271fb. [DOI] [PubMed] [Google Scholar]
- 5. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. ARDS Definition Task Force Acute respiratory distress syndrome: the Berlin definition. JAMA . 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 6. Levitt JE, Bedi H, Calfee CS, Gould MK, Matthay MA. Identification of early acute lung injury at initial evaluation in an acute care setting prior to the onset of respiratory failure. Chest . 2009;135:936–943. doi: 10.1378/chest.08-2346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Coudroy R, Frat JP, Boissier F, Contou D, Robert R, Thille AW. early identification of acute respiratory distress syndrome in the absence of positive pressure ventilation: implications for revision of the Berlin Criteria for acute respiratory distress syndrome. Crit Care Med . 2018;46:540–546. doi: 10.1097/CCM.0000000000002929. [DOI] [PubMed] [Google Scholar]
- 8. Kangelaris KN, Ware LB, Wang CY, Janz DR, Zhuo H, Matthay MA, et al. Timing of intubation and clinical outcomes in adults with acute respiratory distress syndrome. Crit Care Med . 2016;44:120–129. doi: 10.1097/CCM.0000000000001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ranieri VM, Rubenfeld GD, Thompson BT. Defining ARDS: do we need a mandatory waiting period? Intensive Care Med . 2013;39:775–778. doi: 10.1007/s00134-013-2834-y. [DOI] [PubMed] [Google Scholar]
- 10. Matthay MA, Thompson BT, Ware LB. The Berlin definition of acute respiratory distress syndrome: should patients receiving high-flow nasal oxygen be included? Lancet Respir Med . 2021;9:933–936. doi: 10.1016/S2213-2600(21)00105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rochwerg B, Einav S, Chaudhuri D, Mancebo J, Mauri T, Helviz Y, et al. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline. Intensive Care Med . 2020;46:2226–2237. doi: 10.1007/s00134-020-06312-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Papazian L, Corley A, Hess D, Fraser JF, Frat JP, Guitton C, et al. Use of high-flow nasal cannula oxygenation in ICU adults: a narrative review. Intensive Care Med . 2016;42:1336–1349. doi: 10.1007/s00134-016-4277-8. [DOI] [PubMed] [Google Scholar]
- 13. Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, et al. FLORALI Study Group REVA Network. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med . 2015;372:2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 14. Hernández G, Vaquero C, González P, Subira C, Frutos-Vivar F, Rialp G, et al. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA . 2016;315:1354–1361. doi: 10.1001/jama.2016.2711. [DOI] [PubMed] [Google Scholar]
- 15. Demoule A, Vieillard Baron A, Darmon M, Beurton A, Géri G, Voiriot G, et al. High-flow nasal cannula in critically iii patients with severe COVID-19. Am J Respir Crit Care Med . 2020;202:1039–1042. doi: 10.1164/rccm.202005-2007LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mellado-Artigas R, Ferreyro BL, Angriman F, Hernández-Sanz M, Arruti E, Torres A, et al. COVID-19 Spanish ICU Network High-flow nasal oxygen in patients with COVID-19-associated acute respiratory failure. Crit Care . 2021;25:58. doi: 10.1186/s13054-021-03469-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chertoff J. High-flow oxygen, positive end-expiratory pressure, and the Berlin definition of acute respiratory distress syndrome: are they mutually exclusive? Am J Respir Crit Care Med . 2017;196:396–397. doi: 10.1164/rccm.201701-0005LE. [DOI] [PubMed] [Google Scholar]
- 18. Riviello ED, Kiviri W, Twagirumugabe T, Mueller A, Banner-Goodspeed VM, Officer L, et al. Hospital incidence and outcomes of the acute respiratory distress syndrome using the Kigali modification of the Berlin definition. Am J Respir Crit Care Med . 2016;193:52–59. doi: 10.1164/rccm.201503-0584OC. [DOI] [PubMed] [Google Scholar]
- 19. Grieco DL, Menga LS, Cesarano M, Rosà T, Spadaro S, Bitondo MM, et al. COVID-ICU Gemelli Study Group Effect of Helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: the HENIVOT randomized clinical trial. JAMA . 2021;325:1731–1743. doi: 10.1001/jama.2021.4682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Franco C, Facciolongo N, Tonelli R, Dongilli R, Vianello A, Pisani L, et al. Feasibility and clinical impact of out-of-ICU noninvasive respiratory support in patients with COVID-19-related pneumonia. Eur Respir J . 2020;56:2002130. doi: 10.1183/13993003.02130-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tonetti T, Grasselli G, Zanella A, Pizzilli G, Fumagalli R, Piva S, et al. COVID-19 Northern Italian ICU Network Use of critical care resources during the first 2 weeks (February 24-March 8, 2020) of the Covid-19 outbreak in Italy. Ann Intensive Care . 2020;10:133. doi: 10.1186/s13613-020-00750-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Boscolo A, Sella N, Lorenzoni G, Pettenuzzo T, Pasin L, Pretto C, et al. COVID-19 VENETO ICU Network Static compliance and driving pressure are associated with ICU mortality in intubated COVID-19 ARDS. Crit Care . 2021;25:263. doi: 10.1186/s13054-021-03667-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, et al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med . 2012;38:1573–1582. doi: 10.1007/s00134-012-2682-1. [DOI] [PubMed] [Google Scholar]
- 24. Maiolo G, Collino F, Vasques F, Rapetti F, Tonetti T, Romitti F, et al. Reclassifying acute respiratory distress syndrome. Am J Respir Crit Care Med . 2018;197:1586–1595. doi: 10.1164/rccm.201709-1804OC. [DOI] [PubMed] [Google Scholar]
- 25. Hernu R, Wallet F, Thiollière F, Martin O, Richard JC, Schmitt Z, et al. An attempt to validate the modification of the American-European consensus definition of acute lung injury/acute respiratory distress syndrome by the Berlin definition in a university hospital. Intensive Care Med . 2013;39:2161–2170. doi: 10.1007/s00134-013-3122-6. [DOI] [PubMed] [Google Scholar]
- 26. Bellani G, Laffey JG, Pham T, Madotto F, Fan E, Brochard L, et al. LUNG SAFE Investigators ESICM Trials Group. Noninvasive ventilation of patients with acute respiratory distress syndrome. Insights from the LUNG SAFE study. Am J Respir Crit Care Med . 2017;195:67–77. doi: 10.1164/rccm.201606-1306OC. [DOI] [PubMed] [Google Scholar]
- 27. Zhao X, Huang W, Li J, Liu Y, Wan M, Xue G, et al. Noninvasive positive-pressure ventilation in acute respiratory distress syndrome in patients with acute pancreatitis: a retrospective cohort study. Pancreas . 2016;45:58–63. doi: 10.1097/MPA.0000000000000377. [DOI] [PubMed] [Google Scholar]
- 28. Goligher EC, Slutsky AS. Not just oxygen? Mechanisms of benefit from high-flow nasal cannula in hypoxemic respiratory failure. Am J Respir Crit Care Med . 2017;195:1128–1131. doi: 10.1164/rccm.201701-0006ED. [DOI] [PubMed] [Google Scholar]
- 29. Groves N, Tobin A. High flow nasal oxygen generates positive airway pressure in adult volunteers. Aust Crit Care . 2007;20:126–131. doi: 10.1016/j.aucc.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 30. Parke RL, Eccleston ML, McGuinness SP. The effects of flow on airway pressure during nasal high-flow oxygen therapy. Respir Care . 2011;56:1151–1155. doi: 10.4187/respcare.01106. [DOI] [PubMed] [Google Scholar]
- 31. Calligaro GL, Lalla U, Audley G, Gina P, Miller MG, Mendelson M, et al. The utility of high-flow nasal oxygen for severe COVID-19 pneumonia in a resource-constrained setting: A multi-centre prospective observational study. EClinicalMedicine . 2020;28:100570. doi: 10.1016/j.eclinm.2020.100570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A, Acute Respiratory Distress Syndrome Network Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med . 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]