Abstract
Background
Hemorrhoids are one of the most common anorectal disorders. The Milligan‐Morgan open hemorrhoidectomy is the most widely practiced surgical technique used for the management of hemorrhoids and is considered the current "gold standard". Circular stapled hemorrhoidopexy was first described by Longo in 1998 as alternative to conventional excisional hemorrhoidectomy. Early, small randomized‐controlled trials comparing stapled hemorrhoidopexy with traditional excisional surgery have shown it to be less painful and that it is associated with quicker recovery. The reports also suggest a better patient acceptance and a higher compliance with day‐case procedures potentially making it more economical. A previous Cochrane Review of stapled hemorrhoidopexy and conventional excisional surgery has shown that the stapled technique is associated with a higher risk of recurrent hemorrhoids and some symptoms in long term follow‐up. Since this initial review, several more randomized controlled trials have been published that may shed more light on the differences between the novel stapled approach and conventional excisional techniques.
Objectives
This review compares the use of circular stapling devices and conventional excisional techniques in the surgical treatment of hemorrhoids. Its goal is to ascertain whether there is any difference in the outcomes of the two techniques in patients with symptomatic hemorrhoids.
Search methods
We searched all the major electronic databases (MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials (CENTRAL) from 1998 to December 2009.
Selection criteria
All randomized controlled trials comparing stapled hemorrhoidopexy to conventional excisional hemorrhoidal surgeries with a minimum follow‐up period of 6 months were included.
Data collection and analysis
Data were collected on a data sheet. When appropriate, an Odds Ratio was generated using a random effects model.
Main results
Patients with SH were significantly more likely to have recurrent hemorrhoids in long term follow up at all time points than those with CH (12 trials, 955 patients, OR 3.22, CI 1.59‐6.51, p=0.001). There were 37 recurrences out of 479 patients in the stapled group versus only 9 out of 476 patients in the conventional group. Similarly, in trials where there was follow up of one year or more, SH was associated with a greater proportion of patients with hemorrhoid recurrence (5 trials, 417 patients, OR 3.60, CI 1.24‐10.49, p=0.02). Furthermore, a significantly higher proportion of patients with SH complained of the symptom of prolapse at all time points (13 studies, 1191 patients, OR 2.65, CI 1.45‐4.85, p=0.002). In studies with follow up of greater than one year, the same significant outcome was found (7 studies, 668 patients, OR 3.14, CI 1.20‐8.22, p=0.02). Patients undergoing SH were more likely to require an additional operative procedure compared to those who underwent CH (8 papers, 553 patients, OR 2.75, CI 1.31‐5.77, p=0.008). When all symptoms were considered, patients undergoing CH surgery were more likely to be asymptomatic (12 trials, 1097 patients, OR 0.59, CI 0.40‐0.88). Non significant trends in favor of SH were seen in pain, pruritis ani, and fecal urgency. All other clinical parameters showed trends favoring CH.
Authors' conclusions
Stapled hemorrhoidopexy is associated with a higher long‐term risk of hemorrhoid recurrence and the symptom of prolapse. It is also associated with a higher likelihood of long‐term symptom recurrence and the need for additional operations compared to conventional excisional hemorrhoid surgeries. Patients should be informed of these risks when being offered the stapled hemorrhoidopexy as surgical therapy. If hemorrhoid recurrence and prolapse are the most important clinical outcomes, then conventional excisional surgery remains the "gold standard" in the surgical treatment of internal hemorrhoids.
Plain language summary
Conventional surgical hemorrhoidectomy results in fewer recurrences than stapled hemorrhoidopexy.
Hemorrhoids are one of the most common anorectal disorders. The Milligan‐Morgan open hemorrhoidectomy is the most widely practiced surgical technique used for the management of hemorrhoids and is considered the current "gold standard". Circular stapled hemorrhoidopexy was first described in 1998 as alternative to conventional excisional hemorrhoidectomy. A review of randomized control trials comparing stapled hemorrhoidopexy and conventional excisional surgery was conducted. The results show that the stapled technique is associated with a higher risk of recurrent hemorrhoids and some symptoms in long term follow‐up. Patients should be informed of these risks when being offered the stapled homorrhoidopexy as surgical therapy.
Background
Hemorrhoidal disease is one of the most common anorectal disorders, affecting more than 15 million people annually in the United States (Johanson 2002). This number is thought to underestimate the prevalence of the disease because one‐third of patients with complaints consistent with hemorrhoids never present to a physician (Johanson 1990). The prevalence of hemorrhoids is equal between men and women, but men are more likely to seek treatment (Hussain 1999); moreover, the prevalence of hemorrhoids also increases with age until the seventh decade, at which point there appears to be a slight decline (Hussain 1999; Johanson 1990).
Internal hemorrhoids (referred to as "hemorrhoids") exist due to the chronic engorgement of the submucosal venous plexus of the anal canal and originate above the dentate line (Thomson 1975). Based on the degree of the prolapse, they may be classified into four grades. Grade I hemorrhoids are non prolapsing, grade II hemorrhoids prolapse on straining but reduce spontaneously, grade III hemorrhoids require manual reduction, and grade IV hemorrhoids are non‐reducible (Sardinha 2002). Concurrent components of the disease below the dentate line are termed external hemorrhoids (Sardinha 2002). The external components of the disease, especially skin tags, may interfere with perianal hygiene resulting in dermatological symptoms such as perianal pruritus and skin excoriation in addition to painful thrombosis. Hemorrhoids are characterized by complaints of bright red bleeding per rectum, mucosal prolapse or protrusion, and pruritis ani (Thomson 1975). They do not typically cause pain because they originate from the viscerally innervated tissue above the dentate line (Johanson 2002).
Conventional surgical hemorrhoidectomy (CH) involves excision of the hemorrhoidal cushions and is generally advocated for 3rd and 4th degree hemorrhoids (Sutherland 2002). This traditional approach is effective, however it is often accompanied by a high incidence of complications like urinary retention, hemorrhage, and significant pain (Polglase 1997). Over the years, several modifications have been made to the original operation of excision of hemorrhoids using scissors, to improve the outcomes, especially the postoperative pain following the procedure. The Milligan‐Morgan open hemorrhoidectomy is the most widely practiced technique as is considered the current "gold standard" for surgical management of hemorrhoids (MacRae 1995).
Circular stapled hemorrhoidopexy (SH) was first described by Longo in 1998 as alternative to conventional excisional hemorrhoidectomy (Longo 1998). In contrast to the traditional approach, it does not remove the hemorrhoidal tissue. Alternatively, it fashions a mucosa to mucosa anastomosis by excising the submucosa proximal to the dentate line. This results in relocation of the cushions and interruption of the feeding arteries. As a result of the excision occurring above the dentate line, it avoids a painful wound in the somatically innervated anoderm (Correa‐Rovelo 2002). Early, small randomized‐controlled trials comparing stapled hemorrhoidopexy with traditional excisional surgery have shown it to be less painful and that it is associated with quicker recovery. The reports also suggest a better patient acceptance and a higher compliance with day‐case procedures potentially making it more economical. In studies with short‐term follow‐up, stapled hemorrhoidopexy appears to be equally efficient in controlling the hemorrhoidal symptoms. Furthermore, the nature and incidence of the general complications after stapled hemorrhoidopexy seems to be similar when compared to conventional excisional surgery (Mehigan 2000; Rowsell 2000). The favorable results from the early randomized‐controlled studies and prospective series have resulted in an increasing interest in stapled hemorrhoidopexy. Driven by this early success and concerns regarding pain associated with excisional surgery, stapled hemorrhoidopexy has achieved rapid popularity as an alternative surgical approach to treat hemorrhoids in many centres.
Most of the completed randomized trials are too small to definitively conclude that the stapled technique is clearly superior. Data on the long‐term functional outcome of stapled hemorrhoidopexy are still emerging and there is a paucity of evidence rationalizing its wide‐spread use. Furthermore, there have been reports of serious complications such as severe, pelvic sepsis, rectal obstruction, rectal perforation, and staple line dehiscence following the new technique (Pescatori 2002). Critics also site the inadequacy of stapled anopexy in managing concomitant external hemorrhoids, it carries a postoperative bleeding rate similar to that of conventional hemorrhoidectomy, and has an early re‐intervention rate of more than 5% (Pescatori 2002). These revelations and reports of severe post‐defecation pain syndrome and fecal urgency (Cheetham 2000) has generated some doubts about the safety of stapled hemorrhoidopexy. There is a lack of long‐term results regarding control of hemorrhoid symptoms and rates of recurrence. It is essential that evidence pertaining to long‐term efficacy are obtained before stapled hemorrhoidopexy becomes the first‐line surgical option in the treatment of hemorrhoids.
The Cochrane review published in 2006 included 12 randomized controlled trials comparing the stapled and excisional techniques. It revealed that stapled hemorrhoidopexy was associated with a significantly higher rate of hemorrhoid recurrence. In addition, patients who underwent the stapled procedure were more likely to experience hemorrhoid prolapse. Non‐significant trends favoring stapled hemorrhoidopexy were observed in postoperative pain and patient complaints of pruritis ani.
Since 2006, several additional randomized controlled trials have been published, comparing the two surgical strategies, as well as follow‐up data on some of the initial trials. As these studies may shed additional light on the long‐term therapeutic efficacy of the two techniques, an updated review is warranted.
Objectives
This review compares the use of circular stapling devices and conventional excisional techniques in the surgical treatment of hemorrhoids. Its goal is to ascertain whether there is any difference in the outcomes of the two techniques in patients with symptomatic hemorrhoids.
Methods
Criteria for considering studies for this review
Types of studies
All randomized controlled trials comparing the outcomes of circular stapled hemorrhoidopexy and conventional excisional hemorrhoidectomy techniques for the treatment of hemorrhoids were used. If desired data was unavailable in the relevant studies, the authors were contacted to provide full details. Studies comparing stapled hemorrhoidopexy with non‐operative techniques (rubber band ligation, injection sclerotherapy, cryotherapy, infrared coagulation, laser coagulation and diathermy coagulation) and studies comparing different forms of conventional excisional surgery were excluded. Studies on non‐human subjects or that are not randomized were excluded. The analysis includes papers published from 1998 and onward, this is when Longo first described the circular stapling technique in clinical use (Longo 1998).
Types of participants
Adults who received stapled hemorrhoidopexy or conventional excisional hemorrhoidectomy, either elective or emergent, for surgical treatment of their hemorrhoids. All grades of hemorrhoidal disease were eligible.
Types of interventions
Techniques using either custom designed staplers or other designs for hemorrhoidopexy were compared to excisional hemorrhoidectomy. The latter group included any method irrespective of the actual instrument used for the excision. This includes the traditional Milligan‐Morgan open hemorrhoidectomy using scissors, diathermy, lasers, harmonic scalpel and the Ligasure device. The other variants of excisional hemorrhoidectomy such as the Ferguson's closed hemorrhoidectomy and the Parks submucosal hemorrhoidectomy were eligible.
Types of outcome measures
Primary Outcomes: Post‐operative pain, post‐operative recurrence of hemorrhoid symptoms, need for repeat procedures/operations, long‐term recurrence of hemorrhoids and their symptoms.
Secondary Outcomes: stricture/stenosis, re‐operation, wound problems, return to normal activities, length of hospital stay, presence of external hemorrhoidal skin tags, soiling/incontinence/difficulty with peri‐anal hygiene and post‐operative and long‐term complications
Search methods for identification of studies
We searched for published and unpublished randomized controlled trials performed in 1998 and up to December 2009 with no restriction on language in the following electronic databases: MEDLINE, EMBASE, CENTRAL, Cochrane Database of Systematic Reviews. The following search terms were used:
Hemorrhoid/Hemorrhoid Hemorrhoidectomy/Hemorrhoidectomy Hemorrhoidopexy/Hemorrhoidopexy Anopexy Mucosectomy PPH Anus Ano‐rectal disease Benign anal disease Longo Staple Surgical staplers Trial Randomized Random allocation Randomized controlled trial
Principal authors were contacted if possible for further information relating to the study and any other studies published and unpublished. All reference lists were searched for additional studies. Hand‐searches were performed on the following journals from 1998 at beyond: Diseases of the Colon and Rectum, British Journal of Surgery, and Annals of Surgery. Abstracts presented to the following society meetings from 1998 at onward were hand‐searched: American Society of Colon and Rectal Surgeons, the Association of Coloproctology of Great Britain and Ireland, and the European Association of Coloproctology.
Data collection and analysis
The articles found in the search were screened by two independent authors (KL and SJ). Full text of the eligible studies were obtained and each reviewer independently assessed whether the studies met the inclusion and exclusion criteria. The excluded studies were documented and the reasons for exclusion stated. Any difference in opinion was arbitrated by a third‐party (RM). The methodological quality of all studies eligible for the review was assessed independently. Each included trial was read for the following criteria: concealed randomization, technique of randomization, time of randomization (pre or intra‐operatively), number of randomized patients, number of patients not randomized with explanation, exclusion of randomization, blinding of observer, blinding of outcome assessment, similarity between treatment and control group at entry, representativeness of patients, prospective data collection, documentation of drop‐outs, follow‐up, standardization of outcome assessment, and whether the intention‐to‐treat analysis was employed. This information was included in a table describing included studies. Two investigators independently extracted the results of each trial on a standard data sheet. The data were cross‐checked. Where possible, missing data was sought from the authors. Statistical Analysis The software RevMan 5 was used for statistical analysis. Where there was sufficient data, a summary statistic for each outcome was calculated, in the form of an odds ratio. If data were insufficient for statistical analysis, observational results were presented. Where appropriate, a formal meta‐analysis and investigation of heterogeneity among trials was conducted using a random effects model. For statistically significant findings, a number needed to treat, or a number needed to harm was calculated.
Results
Description of studies
A total of 22 RCTs out of 32 potentially eligible RCTs were included (Basdanis 2004; Bikhchandani 2004; Boccasanta 2001; Cheetham 2003; Chung 2005; Correa‐Rovelo 2002; Ganio 2001; Gravie 2005; Hetzer 2002; Huang 2006; Kairaluoma 2003; Mehigan 2000; Nystrom 2008; Ortiz 2002; Ortiz 2005; Palimento 2003; Racalbuto 2004; Rowsell 2000; Senagore 2004; Shalaby 2001; Thaha 2008; Van de Stadt 2005). The details of these trials are given in the table, "Characteristics of included studies." Most of the papers studied patients with grade III or IV hemorrhoids (Basdanis 2004; Bikhchandani 2004; Boccasanta 2001; Correa‐Rovelo 2002; Ganio 2001; Hetzer 2002; Kairaluoma 2003; Nystrom 2008; Ortiz 2002; Ortiz 2005; Palimento 2003; Racalbuto 2004; Rowsell 2000; Senagore 2004; Shalaby 2001; Thaha 2008; Van de Stadt 2005). Four papers included patients with grade II hemorrhoids (Hetzer 2002; Shalaby 2001; Thaha 2008; Van de Stadt 2005). Two papers looked only at grade III hemorrhoids (Chung 2005; Huang 2006). Three papers did not specify the grade of hemorrhoids being treated (Cheetham 2003; Gravie 2005; Mehigan 2000). All of the papers compared the use of stapled hemorrhoidopexy to conventional excisional hemorrhoidectomy.
Most trials assessed several different clinical outcomes with symptoms being the most common. Of all symptoms studied as a primary outcome, pain and prolapse were the most common. Follow up in most studies was by interview and only one paper specifically mentioned the routine use of proctoscopy as part of the physical exam in follow‐up (Kairaluoma 2003). Some studies were interested in outcomes not being studied in this review such as: anorectal manometry (Boccasanta 2001; Ganio 2001; Shalaby 2001; Van de Stadt 2005); operative time (Basdanis 2004; Bikhchandani 2004; Boccasanta 2001; Chung 2005; Correa‐Rovelo 2002; Gravie 2005; Hetzer 2002; Huang 2006; Kairaluoma 2003; Ortiz 2002; Ortiz 2005; Palimento 2003; Racalbuto 2004; Shalaby 2001; Van de Stadt 2005); anal electrosensitivity (Thaha 2008); and length of hospital stay (Basdanis 2004; Bikhchandani 2004; Boccasanta 2001; Chung 2005; Ganio 2001; Gravie 2005; Hetzer 2002; Huang 2006; Kairaluoma 2003; Mehigan 2000; Nystrom 2008; Rowsell 2000; Racalbuto 2004; Shalaby 2001; Thaha 2008; Van de Stadt 2005).
Four of the included trials were multi‐centre RCTs (Gravie 2005; Nystrom 2008; Senagore 2004; Thaha 2008). Three of the included trials were subsequently re‐published under different authors with long‐term follow up of the original patients in the trial. The original publication Mehigan 2000 was updated with long‐term data by Smyth in 2003 (Smyth 2003). Similarly, the original data published by Rowsell 2000 was updated by Au‐Yong in 2004 (Au‐Yong 2004). The publication by Palimento 2003 was updated by Picchio in 2006 (Picchio 2006).
One trial (Shalaby 2001) lost a large number of patients in the CH group at one year follow‐up. At one year, 95% (95 patients) were available for follow‐up in the SH group, while only 80% (80 patients) were available in the CH group. There was no explanation as to why this occurred. This trial was identified as having potential bias, however it was included because the allocation concealment was adequate.
Risk of bias in included studies
Of the 10 excluded trials, 9 were excluded because the follow‐up period was inadequate (Brown 2001; Ho 2000; Ho 2006; Khan 2009; Kraemer 2005; Krska 2003; Lau 2004; Pavlidis 2001; Wilson 2002). One trial was excluded because it compared linear stapled hemorrhoidectomy to conventional excisional techniques (Khalil 2000).
Effects of interventions
A total of 22 studies were included in the analysis. Follow‐up periods ranged from 6 to 56 months with a median follow‐up period of 12.3 months. Odds ratios were generated using a random effects model. Most of the trials had varying follow‐up periods, so when possible, the data was sub‐divided according to the length of follow‐up reported in the trials: less than 1 year (but greater than 6 months); greater than 1 year; 1 to 2 years, and greater than 2 years. Similarly, final follow‐up at the conclusion of all the trials irrespective of overall follow‐up period was reported as a comparison of data at all time points.
Asymptomatic Patients
There were fewer asymptomatic patients in the SH group versus the CH group in final follow‐up at all time points (12 trials, 1097 patients, OR 0.59, CI 0.40‐0.88). In trials with follow‐up of greater than one year, a trend showing lower numbers of asymptomatic patients in the SH group was observed, though this did not reach statistical signifigance (6 trials, 553 patients, OR 0.81, CI 0.51‐1.28, p=0.37). The study by Shalaby et al was subjected to a sensitivity analysis as is it contributed to excessive heterogeneity clinically and statistically. It had been identified as being potentially subject to bias as too many patient were lost to follow‐up in the control group and were not accounted for. When the analysis was performed with this study excluded, SH patients were significantly more likely to complain of hemorrhoidal symptoms at all times than those in the CH group (11 trials, 922 patients, OR 0.53, CI 0.38‐0.74, p=0.0002).
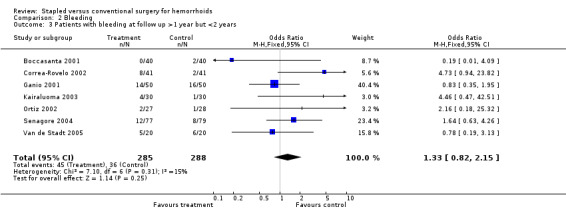
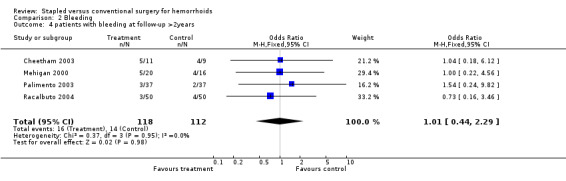
Bleeding
A trend indicating patients with SH were more likely to complain of hemorrhoidal bleeding at all time points was seen (13 trials, 1006 patients, OR 1.13, CI0.80‐1.61, p=0.48) Similarly, non‐significant trends in favor of CH were seen in papers with follow‐up of one to two years (7 trials, 573 patients, OR 1.33, CI 0.82‐2.15, p=0.25).
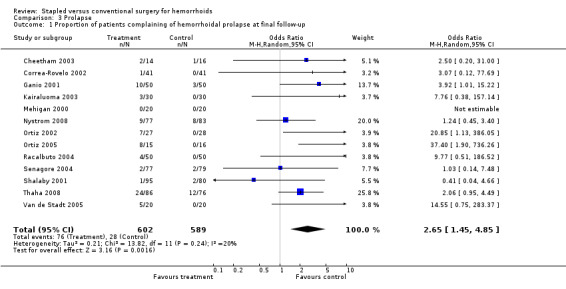
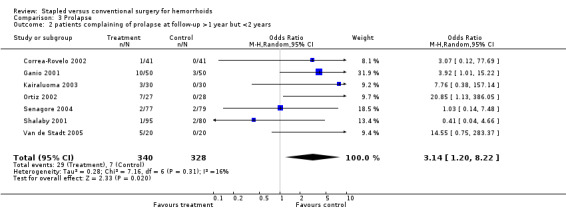
Prolapse
A significantly higher proportion of patients with SH complained of the symptom of prolapse at all time points (13 studies, 1191 patients, OR 2.65, CI 1.45‐4.85, p=0.002). In studies with follow up of greater than one year, the same significant outcome was found (7 studies, 668 patients, OR 3.14, CI 1.20‐8.22, p=0.02).
Pruritis
A non‐significant trend showed patients with CH were less likely to complain of pruritis ani at final follow‐up for all time points than those with SH (7 studies, 506 patients, OR 1.19, CI 0.75‐1.86, p=0.46). However, in studies with follow‐up of greater than two years, the trend is reversed with fewer patients in the SH group reporting pruritis than those in the CH group (2 studies, 136 patients, OR 0.75, CI 0.26‐2.18, p=0.59).
Soiling/Difficulty with Hygiene/Incontinence A non‐significant trend showing patients with SH were more likely to complain of difficulties with soiling, hygiene, or incontinence was seen at all time points (10 studies, 717 patients, OR 1.10, CI 0.67‐1.82, p=0.70).
Fecal Urgency A trend in the proportion of patients complaining of fecal urgency was seen to be higher in the SH group at final follow‐up (5 studies, 373 patients, OR 1.26, CI 0.75‐2.11, p=0.38).
Skin Tags Trends showing a higher proportion of patients with peri‐anal skin tags were seen in the SH group as compared to CH at all time points (10 studies, 782 patients OR 1.47, CI 1.00‐2.16, p=0.05), in studies with follow‐up of one to two years (5 studies, 377 patients, OR 1.36, CI 0.13‐2.53, p=0.). The trend was in favor of SH in studies with follow‐up of greater than two years (3 studies, 210 patients, OR 0.95, CI 0.34‐2.70, p=0.93).
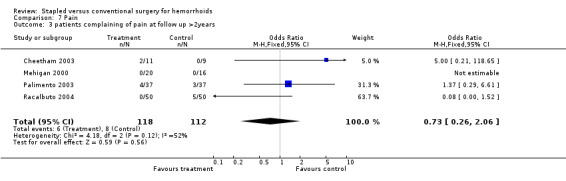
Pain There were trends showing that SH was associated improved pain compared to CH at all time points (11 studies, 823 patients, OR 0.79, CI 0.50‐1.24, p=0.31), in studies with follow‐up of greater than one year (5 studies, 337 patients, OR 0.76, CI 0.36‐1.59, p=0.46), and in studies with follow‐up of greater than two years (4 studies, 230 patients, OR 0.73, CI 0.26‐2.06, p=0.56).
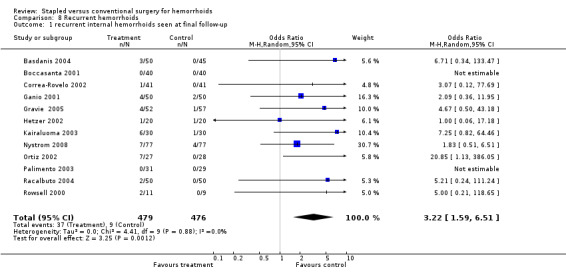
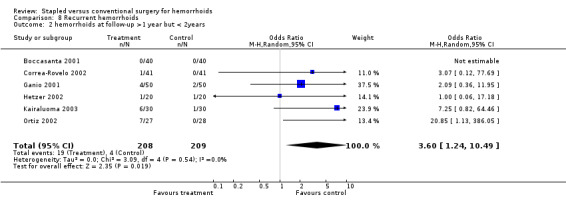
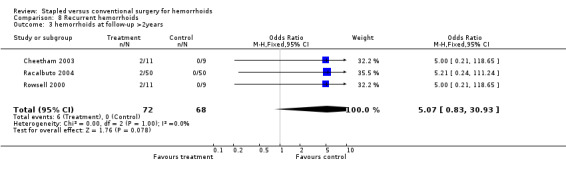
Hemorrhoid Recurrence Patients with SH were significantly more likely to have recurrent hemorrhoids in long term follow up at all time points than those with CH (12 trials, 955 patients, OR 3.22, CI 1.59‐6.51, p=0.001). There were 37 recurrences out of 479 patients in the stapled group versus only 9 out of 476 patients in the conventional group. Similarly, in trials where there was follow up of one year or more, SH was associated with a greater proportion of patients with hemorrhoid recurrence(6 trials, 417 patients, OR 3.60, CI 1.24‐10.49, p=0.02).
Anal Stenosis Trends in favor of SH were seen regarding the proportion of patients complaining of symptoms of anal stenosis at all time points (10 studies, 1536 patients, OR 0.68, CI 0.34‐1.35, p=0.27) and in studies with follow up of one year or more (3 studies, 295 patients, OR 0.44, CI 0.13‐1.49, p=0.18).
Additional Operations Patients in the SH group were more likely to require repeat operations of any nature in long‐term follow‐up for their hemorrhoids (8 papers, 553 patients, OR 2.75, CI 1.31‐5.77, p=0.008).
Cost
No study properly assessed cost formally.
Quality of Life No study utilized a validated Quality of Life grading system as part of its analysis.
Discussion
Surgical treatment for grade III and IV hemorrhoids has been a mainstay of therapy for years. The decision to pursue surgical therapy for hemorrhoids is typically based on symptom severity and the traditional classification of hemorrhoid prolapse. It has been shown to be superior to conservative treatments such as rubber band ligation in terms of remission of hemorrhoidal symptoms and need for re‐treatment (Shanmugam 2005). However, the postoperative pain associated with the procedure has been a major deterrent for patients and clinicians. Innovations in the field have focused on attempting to reduce the impact of postoperative pain as well as potential complications such as bleeding and relapse. This meta‐analysis demonstrates that the more novel stapled hemorrhoidopexy technique is associated with a higher rate of hemorrhoid recurrence and prolapse, as well as an increase in hemorrhoidal symptoms and need for re‐operation in long‐term follow‐up.
Results showing reduced postoperative pain, analgesia requirements, and shorter hospital stays have been demostrated in several systemic reviews (Tjandra 2007; Sutherland 2002). In additions, a previous meta‐analysis (Nisar 2004) demonstrated that patients had improved peri‐operative outcomes, particularly with respect to pain and return to normal activities, compared to the conventional techniques.
Two meta‐analyses comparing stapled hemorrhoidopexy to conventional hemorrhoidectomy have been published since our original review (Burch 2008; Shao 2008). These included 27 and 29 trials respectively. Both reviews concluded that SH is associated with decreased pain in the early postoperative period, increased recurrence of prolapse when compared to conventional hemorrhoidectomy, shorter hospital stay, and reduced operating time. No difference was seen in the rate of complications between the two procedures in either review. Burch 2008 also included a cost effectiveness analysis, which revealed that the two techniques were similar overall (based on the cost of the staple gun at the time and the savings in shorter hospital stay with SH).
Our meta‐analysis was designed to identify and assess clinically important parameters that prompt patients to seek therapy for their hemorrhoids. In a Cochrane Review comparing CH to rubber band ligation (RBL), the authors comment that the most important and obvious measure of success of any treatment method is the ability for long‐term control of the hemorrhoidal symptoms (Shanmugam 2005). In their review, they found that CH was associated with less symptom recurrence and significantly fewer re‐treatments and thus deemed the efficacy of CH to be superior. We have shown similar results demonstrating the long‐term efficacy of CH. Using the data obtained in this study, we have calculated numbers needed to harm for hemorrhoid recurrence and the symptom of prolapse at all time points. They are 17 and 13 respectively.
The study by Shalaby et al. was identifed as being potentially biased as a large number of patients were lost to follow‐up in the excisional hemorrhoidectomy group. We therefore conducted a sensitivity analysis to examine the implications this study had on the data sets. When this study was excluded, there was no change in the statistical significance of any parameter examined in the analysis.
Several studies included in this analysis report symptoms and outcomes that are not necessarily in keeping with our pre‐determined primary and secondary outcomes. For this reason, our analysis considers all symptoms of hemorrhoids with greater emphasis as opposed to the individual symptoms themselves. In addition, outcomes such as various quality of life measures and return to normal activities are reported differently between the papers included in this study. It is difficult to make any meaningful conclusions on this subject based on the literature available. Similarly, the studies in this analysis compared varying degrees of hemorrhoids from grade II to grade IV. Based on the manner in which the data was presented between studies, it was not possible to compare stapled hemorrhoidopexy to excision on a grade‐by‐grade basis.
Both of the techniques employed in this study are safe. Very few complications were reported in the data presented. The only major complications were those indicated in the study by Cheetham et al. which have been recently published. No other similar problems with severe ano‐rectal pain have been reported in the literature. Moreover, the reports of serious complications occurring with both techniques are very rare.
With the addition of the 10 new studies, the power of the current meta‐analysis has been increased and the results strengthened. Differences between the SH and CH techniques that reached significance in the original review remain unchanged.
Authors' conclusions
Implications for practice.
In conclusion, this systematic review demonstrates that stapled hemorrhoidopexy is associated with a higher long‐term risk of hemorrhoid recurrence and the symptom of prolapse. It is also associated with a higher likelihood of long‐term symptom recurrence and the need for additional operations compared to conventional excisional hemorrhoid surgeries. Patients should be informed of these risks when being offered the stapled hemorrhoidopexy as surgical therapy. However, there may be a sub‐set of patients for whom SH is more beneficial. If hemorrhoid recurrence and prolapse are the most important clinical outcomes, then conventional excisional surgery remains the "gold standard" in the surgical treatment of internal hemorrhoids.
Implications for research.
Several questions have yet to be addressed with respect to the choice of surgical technique for hemorrhoidectomy. Are patients willing the accept a greater likelihood of hemorrhoid recurrence and symptom recurrence if the intervention is more tolerable in the short term? How should recurrences and other complications after stapled hemorrhoidopexy be treated? Can the stapled procedure be repeated, or are other modalities required? Finally, further accurate assessments of the impact on cost and a validated measure of quality of life is needed to properly understand the implications of this novel method of treating hemorrhoids.
What's new
| Date | Event | Description |
|---|---|---|
| 21 July 2010 | New search has been performed | New searches performed and 10 new trials included in the analyses. |
History
Protocol first published: Issue 3, 2005 Review first published: Issue 4, 2006
| Date | Event | Description |
|---|---|---|
| 16 February 2009 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
Henning Keinke Andersen P.H.D., Managing Editor of the CCCG
Data and analyses
Comparison 1. Asymptomatic patients.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 patients with no hemorrhoidal symptoms | 12 | 1097 | Odds Ratio (M‐H, Random, 95% CI) | 0.59 [0.40, 0.88] |
| 2 patients with no hemorrhoidal symptoms at follow up >1year but <2 years | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.51, 1.28] |
1.1. Analysis.
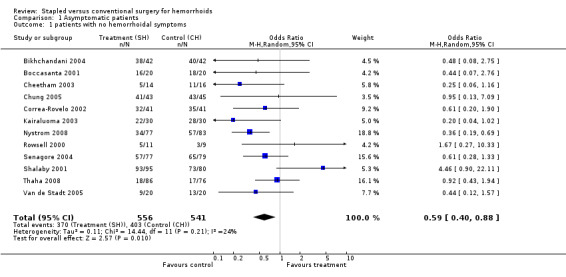
Comparison 1 Asymptomatic patients, Outcome 1 patients with no hemorrhoidal symptoms.
1.2. Analysis.
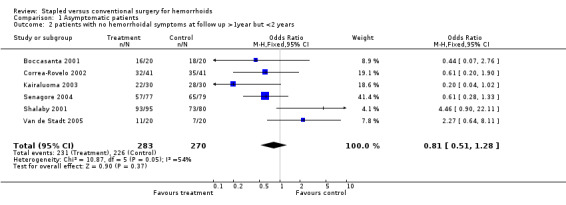
Comparison 1 Asymptomatic patients, Outcome 2 patients with no hemorrhoidal symptoms at follow up >1year but <2 years.
Comparison 2. Bleeding.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 number of patients with bleeding consistent with hemorrhoids | 1 | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Proportion of patients experiencing bleeding consistent with hemorrhoidal bleeding at final follow‐up | 13 | 1006 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.80, 1.61] |
| 3 Patients with bleeding at follow up >1 year but <2 years | 7 | 573 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.82, 2.15] |
| 4 patients with bleeding at follow‐up >2years | 4 | 230 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.44, 2.29] |
2.1. Analysis.
Comparison 2 Bleeding, Outcome 1 number of patients with bleeding consistent with hemorrhoids.
2.2. Analysis.
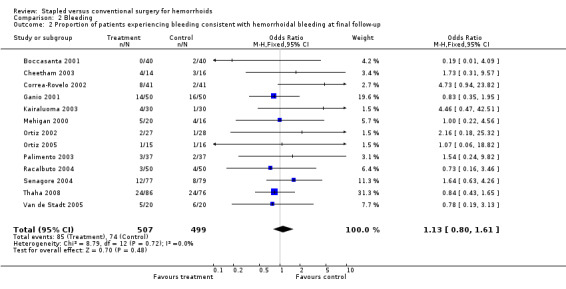
Comparison 2 Bleeding, Outcome 2 Proportion of patients experiencing bleeding consistent with hemorrhoidal bleeding at final follow‐up.
2.3. Analysis.
Comparison 2 Bleeding, Outcome 3 Patients with bleeding at follow up >1 year but <2 years.
2.4. Analysis.
Comparison 2 Bleeding, Outcome 4 patients with bleeding at follow‐up >2years.
Comparison 3. Prolapse.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion of patients complaining of hemorrhoidal prolapse at final follow‐up | 13 | 1191 | Odds Ratio (M‐H, Random, 95% CI) | 2.65 [1.45, 4.85] |
| 2 patients complaining of prolapse at follow‐up >1 year but <2 years | 7 | 668 | Odds Ratio (M‐H, Random, 95% CI) | 3.14 [1.20, 8.22] |
| 3 patients complaining of prolapse at follow‐up >2 years | 3 | 116 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.00 [0.25, 35.33] |
3.1. Analysis.
Comparison 3 Prolapse, Outcome 1 Proportion of patients complaining of hemorrhoidal prolapse at final follow‐up.
3.2. Analysis.
Comparison 3 Prolapse, Outcome 2 patients complaining of prolapse at follow‐up >1 year but <2 years.
3.3. Analysis.
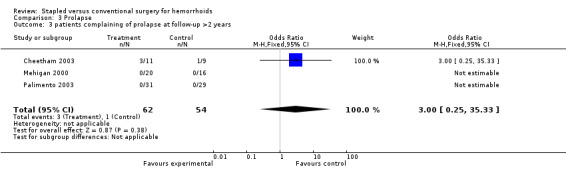
Comparison 3 Prolapse, Outcome 3 patients complaining of prolapse at follow‐up >2 years.
Comparison 4. Pruritis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion of patients complaining of pruritis ani at final follow‐up | 7 | 506 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.75, 1.86] |
| 2 patients complaining of pruritis ani at follow‐up >2years | 2 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.26, 2.18] |
4.1. Analysis.
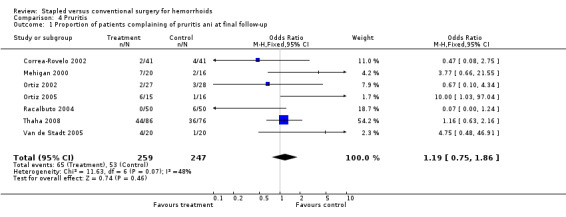
Comparison 4 Pruritis, Outcome 1 Proportion of patients complaining of pruritis ani at final follow‐up.
4.2. Analysis.
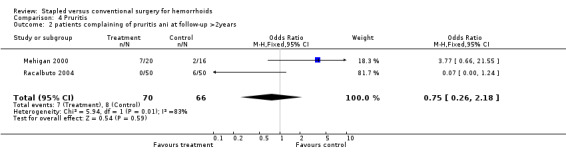
Comparison 4 Pruritis, Outcome 2 patients complaining of pruritis ani at follow‐up >2years.
Comparison 5. Soiling/Difficulty with hygiene/Incontinence.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion of patients experiencing soiling or diffiulty with hygiene or continence | 10 | 717 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.67, 1.82] |
| 2 fecal urgency | 5 | 373 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.75, 2.11] |
| 3 patients with hygiene/continence problems at follow up >1year but <2 years | 4 | 224 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.26, 3.78] |
| 4 patients with fecal urgency at follow up >2years | 4 | 176 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.57, 3.68] |
5.1. Analysis.
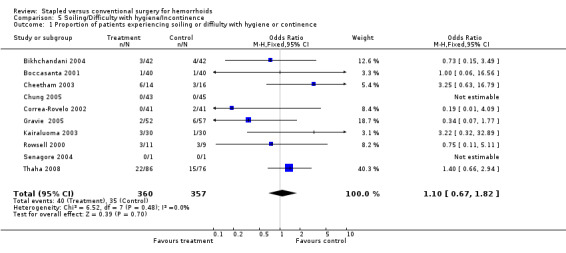
Comparison 5 Soiling/Difficulty with hygiene/Incontinence, Outcome 1 Proportion of patients experiencing soiling or diffiulty with hygiene or continence.
5.2. Analysis.
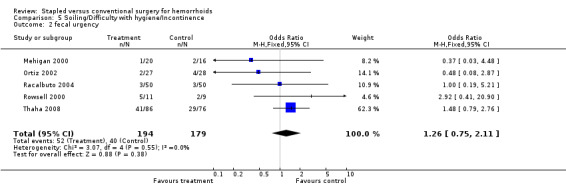
Comparison 5 Soiling/Difficulty with hygiene/Incontinence, Outcome 2 fecal urgency.
5.3. Analysis.
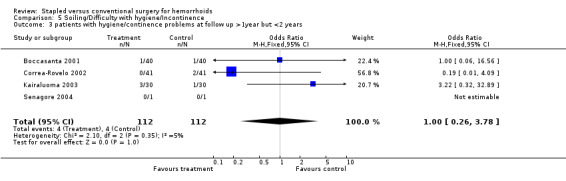
Comparison 5 Soiling/Difficulty with hygiene/Incontinence, Outcome 3 patients with hygiene/continence problems at follow up >1year but <2 years.
5.4. Analysis.
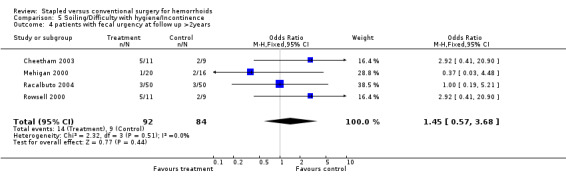
Comparison 5 Soiling/Difficulty with hygiene/Incontinence, Outcome 4 patients with fecal urgency at follow up >2years.
Comparison 6. Skin tags.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 proportion of patients with peri‐anal skin tags at final follow‐up | 10 | 782 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.47 [1.00, 2.16] |
| 2 patients with skin tags at follow up >1 year but <2years | 5 | 377 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.36 [0.73, 2.53] |
| 3 patients with skin tags at follow up >2years | 3 | 210 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.34, 2.70] |
6.1. Analysis.
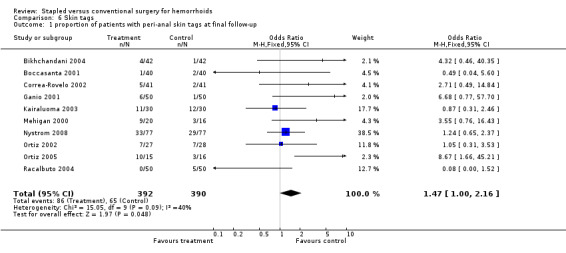
Comparison 6 Skin tags, Outcome 1 proportion of patients with peri‐anal skin tags at final follow‐up.
6.2. Analysis.
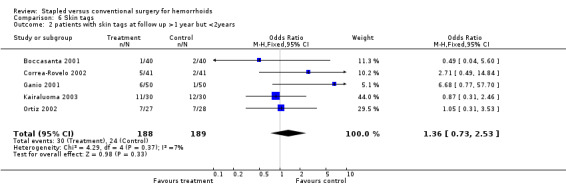
Comparison 6 Skin tags, Outcome 2 patients with skin tags at follow up >1 year but <2years.
6.3. Analysis.
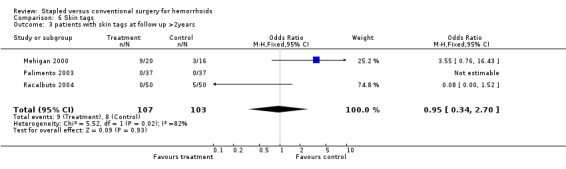
Comparison 6 Skin tags, Outcome 3 patients with skin tags at follow up >2years.
Comparison 7. Pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 proportion of patients complaining of pain related to hemorrhoids at final follow‐up | 11 | 823 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.50, 1.24] |
| 2 patients complaining of pain at follow up >1year but <2years | 5 | 337 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.36, 1.59] |
| 3 patients complaining of pain at follow up >2years | 4 | 230 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.26, 2.06] |
7.1. Analysis.
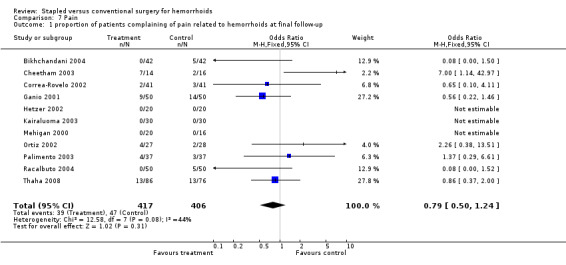
Comparison 7 Pain, Outcome 1 proportion of patients complaining of pain related to hemorrhoids at final follow‐up.
7.2. Analysis.
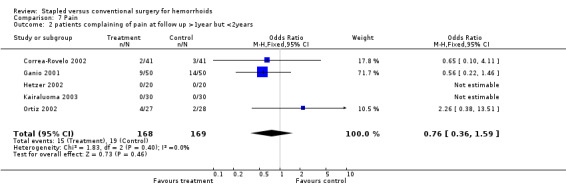
Comparison 7 Pain, Outcome 2 patients complaining of pain at follow up >1year but <2years.
7.3. Analysis.
Comparison 7 Pain, Outcome 3 patients complaining of pain at follow up >2years.
Comparison 8. Recurrent hemorrhoids.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 recurrent internal hemorrhoids seen at final follow‐up | 12 | 955 | Odds Ratio (M‐H, Random, 95% CI) | 3.22 [1.59, 6.51] |
| 2 hemorrhoids at follow‐up >1 year but < 2years | 6 | 417 | Odds Ratio (M‐H, Random, 95% CI) | 3.60 [1.24, 10.49] |
| 3 hemorrhoids at follow‐up >2years | 3 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.07 [0.83, 30.93] |
8.1. Analysis.
Comparison 8 Recurrent hemorrhoids, Outcome 1 recurrent internal hemorrhoids seen at final follow‐up.
8.2. Analysis.
Comparison 8 Recurrent hemorrhoids, Outcome 2 hemorrhoids at follow‐up >1 year but < 2years.
8.3. Analysis.
Comparison 8 Recurrent hemorrhoids, Outcome 3 hemorrhoids at follow‐up >2years.
Comparison 9. Stenosis/Outlet obstruction.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion of patients complaining of difficulty voiding due to outlet obstruction or anal stenosis | 10 | 1536 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.34, 1.35] |
| 2 stenosis/outlet obstruction at follow up >1 year but <2 years | 3 | 295 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.13, 1.49] |
| 3 stenosis/outlet obstruction at follow‐up >2years | 4 | 197 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.17, 3.92] |
9.1. Analysis.
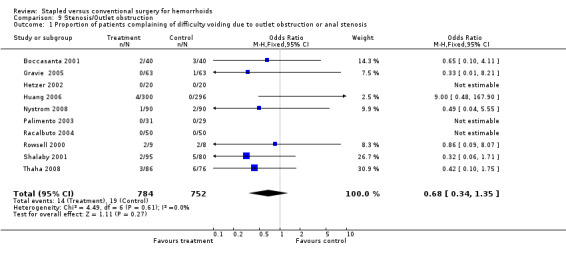
Comparison 9 Stenosis/Outlet obstruction, Outcome 1 Proportion of patients complaining of difficulty voiding due to outlet obstruction or anal stenosis.
9.2. Analysis.
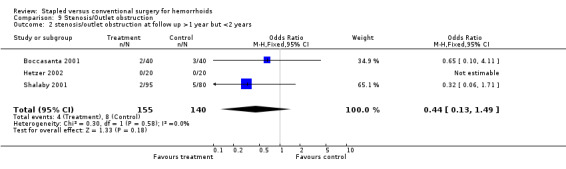
Comparison 9 Stenosis/Outlet obstruction, Outcome 2 stenosis/outlet obstruction at follow up >1 year but <2 years.
9.3. Analysis.
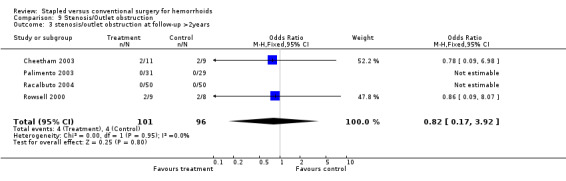
Comparison 9 Stenosis/Outlet obstruction, Outcome 3 stenosis/outlet obstruction at follow‐up >2years.
Comparison 11. Additional Operations.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Further surgeries done later as a result of their initial operation (not peri‐operative) | 8 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.75 [1.31, 5.77] |
11.1. Analysis.
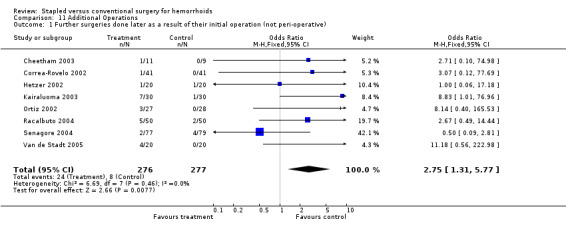
Comparison 11 Additional Operations, Outcome 1 Further surgeries done later as a result of their initial operation (not peri‐operative).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Basdanis 2004.
| Methods | RCT | |
| Participants | grade III and IV hemorrhoids | |
| Interventions | Stapled vs. Ligasure | |
| Outcomes | operative time, symptom control, postoperative pain, recurrence rate, anorectal manometry | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Bikhchandani 2004.
| Methods | RCT | |
| Participants | grade III and IV hemorrhoids | |
| Interventions | Stapled vs. Milligan‐Morgan hemorrhoidectomy | |
| Outcomes | Operative time, symptom control, complication, analgesic requirement, hospital stay, return to work, patient satisfaction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Boccasanta 2001.
| Methods | RCT | |
| Participants | grade IV hemorrhoids | |
| Interventions | Stapled vs. Hospital Leopold Bellan technique | |
| Outcomes | symptoms, anorectal manometry, pain | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Cheetham 2003.
| Methods | RCT | |
| Participants | >18 years old with symptomatic, prolapsing internal hemorrhoids +/‐ external hemorrhoids | |
| Interventions | Stapled vs. Diathermy hemorrhoidectomy | |
| Outcomes | return to work, satisfaction, pain, symptoms | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Chung 2005.
| Methods | RCT | |
| Participants | grade III hemorrhoids | |
| Interventions | Stapled vs. Harmonic Scalpel | |
| Outcomes | operative time, complication rates, analgesic requirement, postoperative pain, hospital stay, return to work, patient satisfaction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Correa‐Rovelo 2002.
| Methods | RCT | |
| Participants | patients with non‐thrombosed grade III and IV hemorrhoidal disease | |
| Interventions | Stapled vs. Ferguson hemorrhoidectomy | |
| Outcomes | pain at 2 weeks and 2 months, satisfaction, clinical response (symptoms), complications, recurrence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Ganio 2001.
| Methods | RCT | |
| Participants | patients aged 25‐78 with symptomatic grade III and IV hemorrhoids | |
| Interventions | Stapled vs. Milligan Morgan hemorrhoidectomy | |
| Outcomes | return to normal activity, anorectal manometry, symptoms, pain, continence, constipation | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Gravie 2005.
| Methods | RCT | |
| Participants | symptomatic hemorrhoidal disease | |
| Interventions | Stapled vs. Milligan Morgan hemorrhoidectomy | |
| Outcomes | postoperative pain, analgesic requirements, symptom control, re‐treatment rates, length of hospital stay, complications, return to work, patient satisfaction | |
| Notes | multicentre | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Hetzer 2002.
| Methods | RCT | |
| Participants | grade II or III hemorrhoids | |
| Interventions | Stapled vs. Ferguson hemorrhoidectomy | |
| Outcomes | pain, continence, hemorrhoid recurrence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Huang 2006.
| Methods | RCT | |
| Participants | grade III hemorrhoids | |
| Interventions | Stapled vs. Ferguson hemorrhoidectomy | |
| Outcomes | operative time, postoperative pain, return to work, patient satisfaction, symptom control, complications | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Kairaluoma 2003.
| Methods | RCT | |
| Participants | grade III or IV hemorrhoids | |
| Interventions | Stapled vs. Excisional hemorrhoidecomty (with no ligation of vascular pedicle) | |
| Outcomes | symptoms, findings at proctoscopy, continence, satisfaction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Mehigan 2000.
| Methods | RCT | |
| Participants | symptomatic prolapsing hemorrhoids | |
| Interventions | Stapled vs. Milligan‐Morgan hemorrhoidectomy | |
| Outcomes | incontinence, quality of life, satisfaction, symptoms | |
| Notes | long‐term follow‐up published by Smyth in 2003 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Nystrom 2008.
| Methods | RCT | |
| Participants | grade III and IV hemorrhoids | |
| Interventions | Stapled vs. Milligan‐Morgan hemorrhoidectiomy | |
| Outcomes | postoperative pain, symptom control, operative time, hospital stay, complications | |
| Notes | multicentre | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Ortiz 2002.
| Methods | RCT | |
| Participants | patients with grade III or IV hemorrhoids | |
| Interventions | Stapled vs. Ferguson hemorrhoidectomy | |
| Outcomes | operative time, post‐operative pain, analgesic use, return to normal activity, complications, symptoms, satisfaction, continence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Ortiz 2005.
| Methods | RCT | |
| Participants | patients with grade IV hemorrhoids | |
| Interventions | Stapled vs. diathermy excision | |
| Outcomes | postoperative pain, symptom control | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Palimento 2003.
| Methods | RCT | |
| Participants | symptomatic hemorrhoidal disease | |
| Interventions | Stapled vs. Milligan‐Morgan hemorrhoidectomy | |
| Outcomes | postoperative pain, symptom control, patient satisfaction, rigid sigmoidoscopy, recurrence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Racalbuto 2004.
| Methods | RCT | |
| Participants | grade III and IV hemorrhoids | |
| Interventions | Stapled vs. Milligan‐Morgan hemorrhoidectomy | |
| Outcomes | symptoms, recurrence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Rowsell 2000.
| Methods | RCT | |
| Participants | symptomatic grade III hemorrhoids | |
| Interventions | Stapled vs. Excisional hemorrhoidectomy | |
| Outcomes | pain, urgency with defacation, continence, anal stenosis, relief of symptoms | |
| Notes | long term results published by Au‐Yong in 2004 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Senagore 2004.
| Methods | RCT | |
| Participants | grage III internal hemorrhoids | |
| Interventions | Stapled vs. Ferguson hemorrhoidectomy | |
| Outcomes | pain, recurrence of hemorrhoid symptoms | |
| Notes | multi‐centre trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Shalaby 2001.
| Methods | RCT | |
| Participants | grade II to grade IV hemorrhoids | |
| Interventions | Stapled vs. Milligan‐Morgan hemorrhoidectomy | |
| Outcomes | pain, pain medication use, anorectal manometry, operative time, length of hospital stay, return to normal activity, wound healing, satisfaction, complications | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Thaha 2008.
| Methods | RCT | |
| Participants | grade II to grade IV hemorrhoids | |
| Interventions | Stapled vs. closed (diathermy) hemorrhoidectomy | |
| Outcomes | postoperative pain, symptom control, complications, re‐treatment rates, patient satisfaction and quality of life | |
| Notes | multicentre trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Van de Stadt 2005.
| Methods | RCT | |
| Participants | grade II or grade III hemorrhoids | |
| Interventions | Stapled vs. Milligan‐Morgan hemorrhoidectomy | |
| Outcomes | postoperative pain, analgesia requirements, number of bowel motions, ,symptom control, re‐treatment rates, patient comfort, anal manometry, anal ultrasound, surgeon and patient satisfaction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Brown 2001 | Insufficient follow‐up period |
| Ho 2000 | Insufficient follow‐up period |
| Ho 2006 | Insufficient follow‐up period |
| Khalil 2000 | Circular stapling device not used. Investigators utilized linear stapling device to staple hemorrhoid pedicles. |
| Khan 2009 | Insufficient follow‐up period |
| Kraemer 2005 | Insufficient follow‐up period |
| Krska 2003 | Insufficient follow‐up period |
| Lau 2004 | Insufficient follow‐up period |
| Pavlidis 2001 | Insufficient follow‐up period |
| Wilson 2002 | Insufficient follow‐up period |
Differences between protocol and review
The Protocol was published as 'Circular stapled anopexy versus excisional haemorrhoidectomy for haemorrhoidal disease'
Contributions of authors
As informed in the Method section
Declarations of interest
None
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Basdanis 2004 {published data only}
- Basdanis G, Papadopoulos V, Michalopoulos A, Apostolidis S, Harlaftis N. Randomized clinical trial of stapled hemorrhoidectomy vs open with Ligasure for prolapsed piles.. Surg Endosc 2005;19:235‐239. [DOI] [PubMed] [Google Scholar]
Bikhchandani 2004 {published data only}
- Bikhchandani J, Agarwal P, Kant R, Malik V. Randomized controlled trial to compare the early and mid‐term results of stapled versus open hemorrhoidectomy.. Am J Surg 2005;189:56‐60. [DOI] [PubMed] [Google Scholar]
Boccasanta 2001 {published data only}
- Boccasanta P, Capretti PG, Venturi, M, et al. Randomised controlled trial between stapled circumferential mucosectomy and conventional circular hemorrhoidectomy in advanced hemorrhoids with external mucosal prolapse. American Journal of Surgery 2001;182:64‐68. [DOI] [PubMed] [Google Scholar]
Cheetham 2003 {published data only}
- Cheetham MJ, Cohen, CRG, Kamm, MA, Phillips, RKS. A randomized controlled trial of diathermy hemorrhoidecomy vs. stapled hemorrhoidectomy in an intended day‐care setting with longer‐term follow‐up. Dis Colon and Rectum 2003;46:491‐497. [DOI] [PubMed] [Google Scholar]
Chung 2005 {published data only}
- Chung C, Cheung H, Chan E, Kwok S, Li M. Stapled hemorrhoidopexy vs. harmonic scalpel hemorrhoidectomy: a randomized trial.. Dis Colon Rectum 2005;48:1213‐1219. [DOI] [PubMed] [Google Scholar]
Correa‐Rovelo 2002 {published data only}
- Correa‐Rovelo JM, Tellez O, Obregon L, et al. Stapled rectal mucosectomy vs. Closed hemorrhoidectomy. Dis Colon and Rectum 2002;45:1367‐1376. [DOI] [PubMed] [Google Scholar]
Ganio 2001 {published data only}
- Ganio E, Altomare F, Gabrielli E, et al. Prospective randomized multicentre trial comparing stapled with open haemorrhoidectomy. Br J Surg 2001;88:669‐674. [DOI] [PubMed] [Google Scholar]
Gravie 2005 {published data only}
- Gravie J, Lehur P, Huten N, Papillon M, Fantoli M, Descottes B, Pessaux P, Arnaud J. Stapled hemorrhoidopexy versus Milligan‐Morgan hemorrhoidectomy.. Annals of Surgery 2005;242(1):29‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hetzer 2002 {published data only}
- Hetzer FH, Demartines N, Handschin AE, Clavien P‐A. Stapled vs excision hemorrhoidectomy. Arch Surg 2002;137:337‐340. [DOI] [PubMed] [Google Scholar]
Huang 2006 {published data only}
- Huang W, Chin C, Yeh C, Lin P, Wang J. Randomized comparison between stapled hemorrhoidopexy and Ferguson hemorrhoidectomy for grade 3 hemorrhoids in Taiwan: a prospective study.. Int J Colorectal Dis 2007;22:955‐961. [DOI] [PubMed] [Google Scholar]
Kairaluoma 2003 {published data only}
- Kairaluoma M, Nuorva K, Kellokumpu I. Day‐case stapled (circular) vs. diathermy hemorrhoidectomy. Dis Colon and Rectum 2003;46:93‐99. [DOI] [PubMed] [Google Scholar]
Mehigan 2000 {published data only}
- Mehigan BJ, Monson JRT, Hartley JE. Stapling procedure for haemorrhoids versus Milligan‐Morgan haemorrhoidectomy: randomised controlled trial. Lancet 2000;355:782‐785. [DOI] [PubMed] [Google Scholar]
Nystrom 2008 {unpublished data only}
Ortiz 2002 {published data only}
- Ortiz H, Marzo J, Armendariz P. Randomized clinical trial of stapled haemorrhoidopexy versus conventional diathermy haemorrhoidopexy. Br J Surg 2002;89:1376‐1381. [DOI] [PubMed] [Google Scholar]
Ortiz 2005 {published data only}
- Oritz H, Marzo J, Armendariz P, Miguel M. Stapled hemorrhoidopexy vs. diathermy excision for fourth‐degree hemorrhoids: a randomized, clinical trial and review of the literature.. Dis Colon Rectum 2005;48:809‐815. [DOI] [PubMed] [Google Scholar]
Palimento 2003 {published data only}
- Palimento D, Picchio M, Attanasio U, Lombardi A, Bambini C, Renda A. Stapled and open hemorrhoidectomy: randomized controlled trial of early results.. World J Surg. 2003;27:203‐207. [DOI] [PubMed] [Google Scholar]
Racalbuto 2004 {published data only}
- Racalbuto, A, Aliotta, I, Corsaro, G, Lanteri, R, Di Cataldo, A, Licata, A. Hemorrhoidal stapler prolapsectomy vs. Milligan Morgan hemorrhoidectomy: a long‐term randomized trial. Int. J. Colorectal Disease 2004;19:239‐244. [DOI] [PubMed] [Google Scholar]
Rowsell 2000 {published data only}
- Rowsell M, Bello M, Hemingway DM. Circumferential mucosectomy (stapled haemorrhoidectomy) versus conventional haemorrhoidectomy: randomised controlled trial. Lancet 2000;355:779‐781. [DOI] [PubMed] [Google Scholar]
Senagore 2004 {published data only}
- Senagore AJ, SInger M, Abcarian H et. al. A prospective, randomized, controlled multicenter trial comparing stapled hemorrhoidopexy and ferguson hemorrhoidectomy: perioperative and one‐year results.. Dis Colon and Rectum 2004;47:1824‐1836. [DOI] [PubMed] [Google Scholar]
Shalaby 2001 {published data only}
- Shalaby, R, Desoky, A. Randomized clinical trial of stapled versus Milligan‐Morgan haemorrhoidectomy. Br J Surg 2001;88:1049‐1053. [DOI] [PubMed] [Google Scholar]
Thaha 2008 {published data only}
- Thaha M, Campbell K, Kazmi S, Irvine L, Khalil A, Binnie N, Hendry W, Walker A, Staines H, Steele R. Prospective randomised multi‐centre trial comparing the clinical efficacy, safety and patient acceptability of circular stapled anopexy with closed diathermy haemorrhoidectomy.. Gut 2008;58(5):668‐678. [DOI] [PubMed] [Google Scholar]
Van de Stadt 2005 {published data only}
- Stadt J, D'Hoore A, Duinslaeger M, Chasse E, Penninckx F. Long‐term results after excision haemorrhoidectomy versus stapled haemorrhoidopexy for prolapsing haemorrhoids: a Belgian prospective randomized trial.. Acta Chir Belg 2005;105:44‐52. [PubMed] [Google Scholar]
References to studies excluded from this review
Brown 2001 {published data only}
- Brown Sr, Ballan K, Ho E, et. al. Stapled mucosectomy for acute thrombosed circumferentially prolapsed piles: a prospective randomized comparison with conventional haemorrhoidectomy.. Colorect Dis 2001;3:175‐8. [DOI] [PubMed] [Google Scholar]
Ho 2000 {published data only}
- Ho YH, Cheong WK, Tsang C et. al. Stapled hemorrhoidectomy‐cost and effectiveness. Randomized, controlled trial including incontinence scoring, anorectal manometry, and endoanal ultrasound assessments a up to three months.. Dis Colon and Rectum 2000;43:1666‐1675. [DOI] [PubMed] [Google Scholar]
Ho 2006 {published data only}
- Ho K, Ho Y. Prospective randomized trial comparing stapled hemorrhoidopexy versus closed Ferguson hemorrhoidectomy. Tech Coloproctol 2006;10:193‐197. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khalil 2000 {published data only}
- Khalil KH, O'Bichere A, Sellu D. Randomised clinical trial of sutured versus stapled closed haemorrhoidectomy. Br J Surg 2000;87:1352‐1355. [DOI] [PubMed] [Google Scholar]
Khan 2009 {published data only}
- Khan N, Shah SSH, Rasul S, Bokhari I, Mahboob S, Gulfam MA, Ghayasuddin M, Khan A. Outcome of stapled haemorrhoidectomy versus Milligan Morgan's haemorrhoidectomy.. J Coll Physicians Surg Pak 2009;19(9):561‐565. [PubMed] [Google Scholar]
Kraemer 2005 {published data only}
- Kraemer M, Parulava T, Roblick M, Duschka L, Muller‐Lobeck H. Prospective, randomized study: Proximate PPH stapler vs Ligasure for hemorrhoidal surgery.. Dis Colon Rectum 2005;48:1517‐1522. [DOI] [PubMed] [Google Scholar]
Krska 2003 {published data only}
- Krska Z, Kvasnieka J, Faltyn J, Schmidt D, Svab J, Kormanova K, Hubik J. Surgical treatment of haemorrhoids according to Longo and Milligan Morgan: an evaluation of postoperative tissue response.. Colorectal Dis 2003;5:573‐576. [DOI] [PubMed] [Google Scholar]
Lau 2004 {published data only}
- Lau P, Meng W, Yip A. Stapled haemorrhoidectomy in Chinese patients: a prospective randomised control study.. Hong Kong Med J 2004;10(6):373‐377. [PubMed] [Google Scholar]
Pavlidis 2001 {published data only}
- Pavlidis T, Papaziogas B, Souparis A, et al. Modern stapled Longo procedure vs. conventional Milligan‐Morgan hemorrhoidectomy: a randomized controlled trial.. Int J Colorectal Dis 2002;17:50‐53. [DOI] [PubMed] [Google Scholar]
Wilson 2002 {published data only}
- Wilson MS, Pope V, Doran HE, et. al. Objective comparison of stapled anopexy and open hemorrhoidectomy: a randomized, controlled trial.. Dis Colon and Rectum 2002;45:1437‐1444. [DOI] [PubMed] [Google Scholar]
Additional references
Au‐Yong 2004
- Au‐Yong I, Rowsell, M, Hemingway DM. Randomised controlled clinical trial of stapled haemorrhoidectomy vs conventional haemorrohoidectomy; a three and a half year follow up. Colorectal Disease 2004;6:37‐38. [DOI] [PubMed] [Google Scholar]
Burch 2008
Cheetham 2000
- Cheetham MJ, Mortensen NJ, Nystrom P‐O, et al. Persistent pain and faecal urgency after stapled haemorrhoidectomy. Lancet 2000;356:730‐733. [DOI] [PubMed] [Google Scholar]
Correa‐Rovelo 2002
- Correa‐Rovelo JM, Tellez O, Obregon L, et al. Stapled rectal mucosectomy vs. Closed hemorrhoidectomy. Dis Colon and Rectum 2002;45:1367‐1376. [DOI] [PubMed] [Google Scholar]
Hussain 1999
- Hussain JN. Hemorrhoids. Primary Care 1999;26:35‐51. [DOI] [PubMed] [Google Scholar]
Johanson 1990
- Johanson, JF, Sonnenberg, A. The prevalence of hemorrhoids and chronic constipation. An epidemilogic study.. Gastroenterology 1990;98:380‐386. [DOI] [PubMed] [Google Scholar]
Johanson 2002
- Johanson, JF. Evidence based approach to the treatment of hemorrhoidal disease. Evidence Based Gastroenterology 2002;3:26‐31. [Google Scholar]
Longo 1998
- Longo, A. Treatment of hemorrhoids disease by reduction of mucosa and hemorrhoidal prolapse with a circular suturing device: a new procedure. Proceedings of the 6th World Congress of Endoscopic Surgery. 1998.
MacRae 1995
- MacRae HM, McLeod RS. Comparison of hemorrhoidal treatment modalities: a meta‐analysis. Dis Colon Rectum 1995;38:687‐694. [DOI] [PubMed] [Google Scholar]
Mehigan 2000
- Mehigan BJ, Monson JRT, Hartley JE. Stapling procedure for haemorrhoids versus Milligan‐Morgan haemorrhoidectomy: randomised controlled trial. Lancet 2000;355:782‐785. [DOI] [PubMed] [Google Scholar]
Nisar 2004
- Nisar, PJ, Acheson, AG, Neal, KR, Scholefield JH. Stapled hemorroidopexy compared with conventional hemorrhoidectomy: systematic review of randomized controlled trials.. Dis Colon and Rectum 2004;47:1837‐1845. [DOI] [PubMed] [Google Scholar]
Pescatori 2002
- Pescatori, M. Stapled hemorrhoidectomy: a word of caution. International Journal of Colorectal Disease 2002;17:362‐363. [DOI] [PubMed] [Google Scholar]
Picchio 2006
- Picchio M, Palimento D, Attanasio U, Renda A. Stapled vs open hemorrhoidectomy: long‐term outcome of a randomized controlled trial.. Int J Colorectal Dis 2006;21:668‐669. [DOI] [PubMed] [Google Scholar]
Polglase 1997
- Polglase, A. Haemorrhoids: a clinical update. Med J Aust 1997;167:85‐88. [DOI] [PubMed] [Google Scholar]
Rowsell 2000
- Rowsell M, Bello M, Hemingway DM. Circumferential mucosectomy (stapled haemorrhoidectomy) versus conventional haemorrhoidectomy: randomised controlled trial. Lancet 2000;355:779‐781. [DOI] [PubMed] [Google Scholar]
Sardinha 2002
- Sardinha TC, Corman ML. Hemorrhoids. Surgical Clinics of North America 2002;82:1153‐1167. [DOI] [PubMed] [Google Scholar]
Shanmugam 2005
- Shanmugam V, Thaha MA, Rabindranath KS, Campbell KL, Steele RJC, Loudon MA. Rubber band ligation versus excisional haemorrhoidectomy for haemorrhoids. Cochrane Database of Systematic Reviews 2005, Issue 1. [DOI: 10.1002/14651858.CD005034.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shao 2008
- Shao W, Li G, Zhang Z, Yang B, Sun G, Chen Y. Systematic review and meta‐analysis of randomized controlled trials comparing stapled haemorrhoidopexy with conventional haemorrhoidectomy. British Journal of Surgery 2008;95(2):147‐160. [DOI] [PubMed] [Google Scholar]
Smyth 2003
- Smyth EF, Baker RP, Wilken BJ, Hartley JE, White TJ, Monson JRT. Stapled versus excision haemorrhoidectomy: long‐term follow‐up of a randomised controlled trial. Lancet 2003;361:1437‐38. [DOI] [PubMed] [Google Scholar]
Sutherland 2002
- Sutherland, LM, Burchard AK, Masuda, K, et al. A systematic review of stapled hemorrhoidectomy. Arch Surg 2002;137:1395‐1406. [DOI] [PubMed] [Google Scholar]
Thomson 1975
- Thomson, WH. The nature of haemorrhoids. Br J Surg 1975;62:542‐552. [DOI] [PubMed] [Google Scholar]
Tjandra 2007
- Tjandra JJ, Chan KY. Systematic review on the procedure for prolapse and hemorrhoids (stapled hemorrhoidopexy). Dis Colon Rectum 2007;50(6):878‐892. [DOI] [PubMed] [Google Scholar]


