Abstract
While nightmares are known to predict the clinical course of PTSD, research on the relationship between specific nightmare characteristics and PTSD severity is sparse. This study conducted a secondary analysis to explore how five nightmare characteristics are cross-sectionally related to PTSD severity in 76 combat veterans with PTSD and at-risk alcohol use. Consistent with Emotional Processing Theory, we hypothesized that more replicative, threatening, realistic, and easily recalled nightmares would be associated with more severe PTSD while those with greater symbolism would predict lower PTSD severity. Nightmares narratives were audio-recorded and rated by multiple coders. MANOVAs explored the relationship between nightmare characteristics and PTSD clinical indicators. Most nightmares were realistic, easily recalled, and involved significant threat. Greater realism and replication were associated with greater PTSD severity. Realistic and replicative nightmares may be markers of more severe PTSD and may indicate that less emotional processing of the trauma has occurred.
Keywords: PTSD, nightmares, emotional processing theory, veterans
Nightmares are common among individuals with Posttraumatic Stress Disorder (PTSD) and are associated with other sleep disturbances, psychiatric concerns, and the severity and course of PTSD (Creamer et al., 2018; Pigeon et al., 2013). Nightmares are also independently associated with impairments in functioning and suicidality (Pigeon et al., 2012; Titus et al., 2018). Posttraumatic nightmares are “recurrent distressing dreams in which the content and/or affect of the dream are related to the traumatic event” (APA, 2013, p. 271). This definition allows characteristics such as how symbolic, repetitive, and threatening the nightmare is to vary. It is largely unknown to what extent these characteristics relate to clinical indicators of PTSD.
Posttraumatic nightmares are understood in different ways in the fields of PTSD and dream research (Phelps et al., 2008). Within the PTSD field, Emotional Processing Theory conceptualizes posttraumatic nightmares as a re-experiencing symptom (i.e., unsuccessful attempt to process the traumatic memory that are experienced as distressing and unwanted) (Foa & Kozak, 1986). Within the dream research field, dreams following trauma are thought to promote emotional adaptation. For instance, the Threat Simulation Theory proposes that dreaming functions to simulate realistic threats within the safe space of dreaming to rehearse and prepare for threats in waking life (Revonsuo, 2008).
The limited existing research exploring connections between posttraumatic nightmare characteristics and clinical indicators supports Emotional Processing Theory. References to violence in nightmares are associated with poorer treatment outcomes (Harb et al., 2012). Individuals with more detailed recall of nightmares experience worse PTSD symptoms (Mellman et al., 2001). Nightmares that closely replicate traumas are also related to greater PTSD severity while distressing but non-trauma-replicative dreams are correlated with more positive outcomes (Davis et al., 2007, de Tassel et al., 2018). Therefore, nightmares that are more realistic, threatening, recalled in greater detail, and more closely replicate trauma may indicate less emotional processing has occurred and are related to more severe PTSD. While these studies hint at the implications of varying nightmare characteristics, much remains to be discovered.
The systematic study of nightmare characteristics and how they relate to important clinical indicators is rare (de Tassel et al., 2018; Titus et al., 2018; Whitmann et al., 2007). Surveys that capture a limited number of nightmare characteristic exist (Cranston et al., 2017; Donovan et al., 2005). However, single studies have yet to evaluate a wide range of theory-based characteristics. To address this gap, we sought to describe the characteristics of PTSD nightmares in Iraq and Afghanistan combat veterans with PTSD and at-risk alcohol use and explore their relationships to PTSD severity. This a clinically relevant sample as PTSD and alcohol use commonly co-occur and individuals with PTSD report drinking to manage sleep difficulties, including nightmares (Nishith et al., 2001; Possemato et al, 2015). We hypothesized several relationships based on Emotional Processing Theory. As indicators of less emotional processing, dreams that closely replicate past traumas, are easily recalled, and have high threat and more realistic content were hypothesized to be associated with higher PTSD severity. As an indication of more emotional processing, more symbolic dreams were hypothesized to predict lower PTSD severity. Because the sample also had risky alcohol use we explored if alcohol use severity was related to dream characteristics.
Method
The is a secondary analysis of data collected from two IRB-approved studies that shared the same inclusion/exclusion criteria, recruitment procedures, and measurement (Acosta et al., 2017; Possemato et al., 2015). Participants were recruited from primary care clinics based on positive screens for PTSD and/or alcohol use. Participants were required to be 1) combat veterans of conflicts in Iraq and Afghanistan within the last 5-years from when data was collected (e.g., served in at least one conflict between 2005–2015) and 2) primary care patients in one of four Veterans Affairs facilities. Veterans needed to be at-risk drinkers (women ≥7, men ≥8 on the Alcohol Use Identification Test (AUDIT; Barbour et al., 2001) and have at least subthreshold PTSD (defined as experiencing a traumatic event, 1 re-experiencing symptom, and either 3 avoidance symptoms, or 2 hyperarousal symptoms with functional impairment; as measured by the Clinician-Administered PTSD Scale) (CAPS; Blake et al., 1995) completed at the initial assessment. The CAPS assessed the 17 DSM-IV symptoms and has excellent diagnostic utility (Blake et al., 1995) and good internal consistency in this sample (alpha= .76).
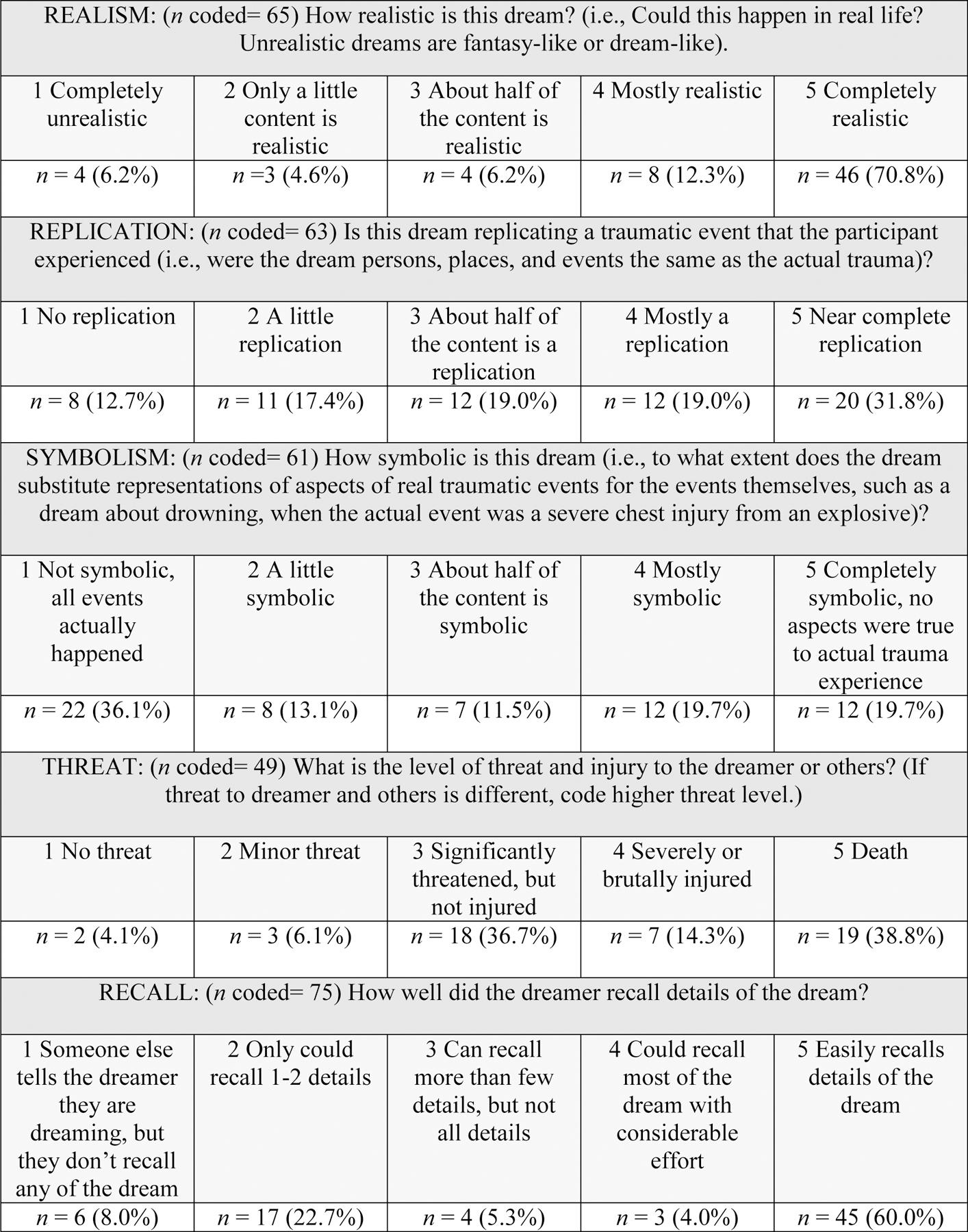
All CAPS interviews were recorded and the trauma assessment and nightmare item were reviewed and coded for nightmare characteristics. A coding template was created that rated five dream characteristics (Figure 1). Dream characteristics were chosen based on past research and the data available within the audio-recorded CAPS symptoms. Intensity and type of emotion (i.e., fear, shame, anger, sadness) were also coded, however, these data are not presented because all dreams were coded as fearful and most dream narratives did not provide enough information to code for emotional intensity. Three authors independently coded each nightmare narrative and regularly met to resolve discrepancies. In addition, a clinical psychologist provided training and supervision for coding and coded a random 25% of the dream narratives to ensure accuracy.
Figure 1:
Nightmare Coding Template with Descriptive Results
SPSS 22 was used for analyses. Dream characteristics were described with descriptive statistics. The 5-point dream characteristic scales were dichotomized and used as independent variables within MANOVAs to explore their relationship to the dependent variables of PTSD intensity, and severity of PTSD clusters (e.g., re-experiencing, avoidance, numbing and arousal). PTSD clusters were explored as outcomes because nightmare characteristics may have different relationships with different types of PTSD symptoms. The nightmare and sleep items were removed from all PTSD scales to ensure independence between nightmare characteristics and PTSD clinical indicators. In preliminary analyses dream characteristics were found to be unrelated to AUDIT scores and therefore no other analyses included alcohol severity.
Results
Nightmare narratives were coded for 76 participants. Participants were 90% (n=68) male and 82% (n=62) non-Hispanic White with an average age of 31(SD=8) years. Participants reported an average annual income of $37,000(SD=$25,000) and 38% (n=29) veterans were currently married. Fifty-seven participants (75%) were Army veterans with an average number of 1.5(SD=.7) combat deployments. Participants reported moderately severe PTSD [CAPS total M(SD)=64.8(20.0)], and severe alcohol use [AUDIT total M(SD)=18.9(6.8)]. Sixty-six veterans (87%) met full PTSD diagnostic criteria and 10 (13%) reported subthreshold symptoms.
Figure 1 includes descriptive characteristics of dream coding results. Not all the 76 narratives had sufficient detail to be coded for each dream characteristic. For instance, recall was coded for 75 narratives (99%), while threat was only coded for 49 narratives (65%). No other data for this study was missing. Most narratives were coded as completely realistic (n=46, 71%) and as easily recalled (n=45, 60%). Ratings of other dream characteristics were more evenly distributed across the rating scale with the most common codes being for dreams that were near complete replication of the trauma (n=20, 32%), not at all symbolic (n=22, 36%), and severely threatening, resulting in death (n=19, 39%).
No MANOVA assumptions were violated: PTSD indicators were correlated with each other at r ≤ .73, data was normally distributed, and variance was equal between nightmare characteristic groups. Table 1 displays means for PTSD clinical indicators for groups of participants who scored high and low on each nightmare characteristics and results from the five MANOVAs exploring the relationship between nightmare characteristics and PTSD indicators. The models for replication and realism were significant indicating that participants with highly replicating and more realistic dreams had significantly higher PTSD intensity scores than those with less replicating and less realistic dreams. The models for recall, threat, and symbolism were not significant. However, the model for threat approached significance and the between-subjects analyses indicate that this finding maybe be driven by PTSD arousal symptoms. Between-subjects analyses for the relationship between recall and PTSD indicators indicate that participants with better nightmare recall may have higher severity of re-experiencing and avoidance symptoms than those with less nightmare recall. Symbolism was unrelated to PTSD indicators. Taken together, these findings indicate that greater replication, more realistic, and possibly more threat content and better recall, are related to more severe PTSD indicators.
Table 1.
MANOVA Results for the Relationship Between Nightmare Characteristics and Clinical Indicators of PTSD
| Wilk’s Lambda | PTSD Intensity | Re-experiencing | Avoidance | Numbing | Arousal | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Value, F (df) | M (SD) | F (SS) | M (SD) | F (SS) | M (SD) | F (SS) | M (SD) | F (SS) | M (SD) | F (SS) | ||
| Replication | .08, 160.97 (58)* | High | 39 (9) | 1.74 (157)† | 17 (8) | .30 (10) | 9 (5) | 1.59 (27) | 18 (8) | .73 (34) | 27 (9) | .02 (.44) |
| Low | 33 (10) | 15 (6) | 8 (4) | 15 (8) | 25 (6) | |||||||
|
| ||||||||||||
| Recall | .92, 1.50 (70) | High | 36 (9) | 1.20 (100) | 17 (7) | 2.23 (78)†† | 9 (4) | .39 (7) | 17 (8) | 2.80 (78) † | 26 (7) | .03 (1) |
| Low | 33 (10) | 13 (6) | 8 (4) | 14 (7) | 26 (7) | |||||||
|
| ||||||||||||
| Realism | .131, 2.27 (60)* | High | 36 (11) | 2.71 (248)† | 16 (7) | .01 (.07) | 9 (4) | .12 (2) | 17 (8) | −2.78 (248)† | 26 (7) | .36 (12) |
| Low | 31 (6) | 12 (5) | 8 (4) | 13 (8) | 25 (5) | |||||||
|
| ||||||||||||
| Threat | .18, 1.68 (48)†† | High | 35 (9) | .67 (51) | 15 (6) | .01 (.41) | 8 (4) | .01 (1) | 15 (7) | .04 (2) | 27 (6) | 5.73 (213)* |
| Low | 33 (10) | 15 (8) | 8 (4) | 15 6) | 22 (7) | |||||||
|
| ||||||||||||
| Symbolism | .13, 2.11 (56) | High | 34 (10) | .27 (25) | 16 (6) | .01 (1) | 9 (4) | .05 (1) | 16 (8) | .02 (2) | 26 (6) | .05 (2) |
| Low | 36 (10) | 16 (7) | 8 (4) | 16 (8) | 26 (8) | |||||||
Notes: Wilk’s Lambda represents the omnibus F for the MANOVA for each nightmare characteristic. Other F statistics are between subjects effects. Clinician Administered PTSD Scale (CAPS) sleep and nightmare items were removed from all relevant scales. PTSD Intensity = CAPS intensity score for all items. Re-experiencing, avoidance, numbing and arousal are total CAPS severity score for each of these clusters. For all dream characteristics “high” was coded as 4 and 5 and “low” was coded as 1, 2, and 3 on the Nightmare Coding Template.
p < .05
p< .10
p<.20. SS= Sum of Squares. Post-hoc power ranged from .419-.529 for MANOVA models.
Discussion
Results are consistent with previous studies finding that more replication, higher threat, and better recall are associated with more severe PTSD (Harb et al., 2012; Mellman et al., 2001, de Tassel et al., 2018; Davis et al., 2007). Findings build upon previous research that assessed fewer than five nightmare characteristics within a study and did not sample recent combat veterans. Also, this is the first study to find that realism is associated with PTSD severity. Results are consistent with Emotional Processing Theory. Higher realism, replication, threat, and recall may suggest that little emotional processing is occurring halting adaptation and recovery. Specifically, nightmares that more accurately depict past traumas may enhance pre-existing or elicit new behavioral avoidance, such as avoidance of sleep, which in turn decreases opportunities for emotional processing and symptom resolution. The potential relationship between higher nightmare threat content and more arousal symptoms may be explained via veterans also perceiving more threat content during the day resulting in increased hyperarousal. Our results join previous research unable to find a link between symbolism and PTSD severity (Phelps et al., 2008) indicating that symbolism may not be a useful predictive characteristic. Results should be interpreted cautiously given the exploratory nature of this study and replication is larger sample is needed.
The strengths of this study include reliable, structured assessment of nightmares that resulted in a rich qualitative dataset of multiple nightmare characteristics and systematic coding of nightmare narratives by three independent coders. Limitations include lack of previous validation of the nightmare coding template, the CAPS was not designed to yield nightmare characteristics resulting in missing data, and did not include the three newer symptoms in the DSM-V. Also, our study was underpowered and replication in a larger sample may reveal more associations between nightmare characteristics and PTSD.
In conclusion, research investigating posttraumatic nightmare characteristics suffers from poorly developed parameters (Phelps et a., 2008; Titus et al., 2018). To help standardize the study of nightmare characteristics, investigators utilizing existing accounts of nightmares can use our template. Measures that assess a more limited number of nightmare characteristics are available for new data collection efforts (Cranston et al., 2017; Donovan et al, 2005). Our results are consistent with emotional processing as a mechanism of action for nightmare treatment (Rousseau & Belleville, 2018). Firstline PTSD treatments such as prolonged exposure and cognitive processing therapy can effectively treat nightmares (Colvonen et al., 2018). For individuals experiencing nightmares that are not resolved by firstline treatments, nightmare-specific interventions that facilitate emotional processing, such as Imagery Rehearsal Therapy, are efficacious (Gieselmann et al., 2019).
Acknowledgments
Source of Funding:
This research is supported by NIAAA grant R01AA020181, VA CSR&D grant 1I01CX000175, and the VA Center for Integrated Healthcare.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest.
Disclosures: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. The authors declare no conflicts of interest.
References
- Acosta MC, Possemato K, Maisto SA, Marsch LA, Barrie K, Lantinga L, Fong X, Haiyi X, Rosenblum R (2017). Web-delivered CBT reduces drinking in OEF-OIF veterans in primary care with symptomatic substance use and PTSD. Behavior Therapy, 48(2), 262–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). [Google Scholar]
- Barbour TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG (2001). The alcohol use disorders identification test guidelines for use in primary care (2nd Ed.). Geneva, Switzerland: World Health Organization. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney D, & Keane TM (1995). The development of the Clinician-Administered PTSD Scale. Journal of Traumatic Stress, 8(1), 75–90. [DOI] [PubMed] [Google Scholar]
- Colvonen PJ, Straus LD, Stepnowsky C, McCarthy MJ, Goldstein LA, Norman SB (2018). Recent Advancements in Treating Sleep Disorders in Co-Occurring PTSD. Current Psychiatry Reports, 20: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cranston CC, Miller KE, Davis JL, & Rhudy JL (2017). Preliminary validation of a brief measure of frequency and severity of nightmares: The trauma-related nightmare survey. Journal of Trauma & Dissociation, 18(1), 88–99. [DOI] [PubMed] [Google Scholar]
- Creamer JL, Brock MS, Matsangas P, Motamedi V, Mysliwiec V (2018). Nightmares in United States military personnel with sleep disturbances. Journal of Clinical Sleep Medicine, 14(3), 419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JL, Byrd P, Rhudy JL, & Wright DC (2007). Characteristics of chronic nightmares in a trauma-exposed treatment-seeking sample. Dreaming, 17(4), 187–198. [Google Scholar]
- de Dassel T, Wittmann L, Protic S, Hollmer H, Gorzka RJ (2018). Association of posttraumatic nightmares and psychopathology in a military sample. Psychological Trauma: Theory, Research, Practice, and Policy, 10, 475–481. [DOI] [PubMed] [Google Scholar]
- Donovan BS, Padin-Rivera E, Chapman H, Strass M, Murray M (2005). Development of the Nightmare Intervention and Treatment Evaluation (NITE) scale. Journal of Trauma Practice, 3, 47–68. [Google Scholar]
- Gieselmann A, Aoudia MA, Carr M…, & Petrowsky R (2019). Aetiology and treatment of nightmare disorder: State of the art and future perspectives. Journal of Sleep Research, 28, e12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20–35. [PubMed] [Google Scholar]
- Harb GC, Thompson R, Ross RJ, & Cook JM (2012). Combat-related PTSD nightmares and imagery rehearsal: Nightmare characteristics and relation to treatment outcomes. Journal of Traumatic Stress, 25(5), 511–518. [DOI] [PubMed] [Google Scholar]
- Mellman TA, David D, Bustamante V, Torres J, & Fins A (2001). Dreams in the acute aftermath of trauma and their relationship to PTSD. Journal of Traumatic Stress, 14(1), 241–247. [Google Scholar]
- Nishith P, Resick P, Mueser KT (2001). Sleep difficulties and alcohol use motives in female rape victims with PTSD. Journal of Traumatic Stress, 14, 463–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pigeon WR, Campbell CE, Possemato K, & Ouimette P (2013). Longitudinal relationships of insomnia, nightmares, and PTSD severity in recent combat veterans. Journal of Psychosomatic Research, 75(6), 546–550. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, Pinquart M, & Conner K (2012). Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. Journal of Clinical Psychiatry, 73(2), 1160–1167. [DOI] [PubMed] [Google Scholar]
- Phelps AJ, Forbes D, & Creamer M (2008). Understanding posttraumatic nightmares: An empirical and conceptual review. Clinical Psychology Review, 28(2), 338–355. [DOI] [PubMed] [Google Scholar]
- Possemato K, Maisto SA, Wade M, Barrie K, McKenzie S, Lantinga LJ, & Ouimette P (2015). Ecological momentary assessment of PTSD symptoms and alcohol use in recent combat veterans. Psychology of Addictive Behaviors, 29(4), 894–905. [DOI] [PubMed] [Google Scholar]
- Revonsuo A (2000). The reinterpretation of dreams: an evolutionary hypothesis of the function of dreaming. Behavioral Brain Science, 23(06), 877–901. [DOI] [PubMed] [Google Scholar]
- Rousseau A & Belleville G (2018) The mechanisms of action underlying the efficacy of psychological nightmare treatments: A systematic review and thematic analysis of discussed hypotheses, Sleep Medicine Reviews 39, 122–133. [DOI] [PubMed] [Google Scholar]
- Titus CE, Speed KJ, Cartwright PM, Drapeau CW, Heo Y, Nadroff MR, (2018). What role do nightmares play in suicide? A brief exploration, Current Opinion in Psychology, 22, 59–62. [DOI] [PubMed] [Google Scholar]
- Wittmann L, Schredl M, & Kramer M (2007). Dreaming in posttraumatic stress disorder: A critical review of phenomenology, psychophysiology and treatment. Psychotherapy and Psychosomatics, 76, 25–39. [DOI] [PubMed] [Google Scholar]


