Abstract
Introduction:
Shock index (SI) and delta shock index (ΔSI) predict mortality and blood transfusion in trauma patients. This study aimed to evaluate the predictive ability of SI and ΔSI in a rural environment with prolonged transport times, and transfers from critical access hospitals or level IV trauma centers.
Methods:
We completed a retrospective database review at an ACS Level 1 trauma center over 2 years. Adult subjects analyzed sustained torso trauma. Subjects with missing data or severe head trauma were excluded. For analysis poisson regression and binomial logistic regression were utilized to study the effect of time in transport and SI/ΔSI on resource utilization and outcomes. P<0.05 was considered significant.
Results:
Complete data was available on 549 scene patients and 127 transfers. Mean ISS was 11 (IQR9.0) for scene and 13 (IQR6.5) for transfers. Initial EMS SI was the most significant predictor for blood transfusion and ICU care in both scene and transferred patients (p<0.0001) compared to trauma center arrival SI or transferring center SI. A negative ΔSI was significantly associated with the need for transfusion and the number of units transfused. Longer transport time also had a significant relationship with increasing ICU LOS. Cohorts were analyzed separately.
Conclusion:
Providers must maintain a high level of clinical suspicion for patients who had an initially elevated SI. EMS SI was the greatest predictor of injury and need for resources. Enroute SI and ΔSI were less predictive as time from injury increased. This highlights the improvements in enroute care, but does not eliminate the need for high-level trauma intervention.
Level of Evidence IV, therapeutic/care management
Keywords: blunt torso trauma, rural trauma, shock index
Media Summary:
EMS shock index outperforms SI at transferring facility or trauma center. EMS SI predicted need for blood products, total number of PRBC and mortality. Trauma surgeons shouldn’t have a false sense of security if vitals improve during transport.
Introduction:
Millions of Americans reside over an hour from definitive trauma care1,2. In a rural trauma environment, patients are frequently taken through a multiple step process before arriving at definitive surgical care. As trauma systems mature there are additional critical access and smaller trauma centers available for initial evaluation and stabilization. Patients undergo evaluation and resuscitation at every stage of this process, but at the cost of increased time to definitive care. Despite these systems, rural trauma victims have higher mortality than matched urban counterparts3–6. Optimal care and transfer pathways in rural America still require further study and development.
Shock index (SI) and delta shock index (ΔSI) predict mortality and blood transfusion in trauma patients7–9. This has been shown both during emergency medical services (EMS) transport and on hospital admission. In particular, an increase in SI that occurs from prehospital to hospital arrival is associated with worse outcomes10. However, it should be noted, these data come from an urban environment. Data on prehospital vital signs data in a rural environment is lacking in detail, quantity, and clarity. Compounding this lack of data is evidence that longer times in transport decrease the correlation between EMS vital signs and arriving ER vital signs11,12. This has made prior work on SI hard to generalize in a rural setting.
The authors hypothesized that SI on hospital arrival was less predictive in a rural environment. With total time in transport routinely over multiple hours, patients would essentially pass the test of time, or be resuscitated throughout their transport to definitive trauma care. In either case this would render hospital arrival SI less valuable as a predictor of mortality and resource need. This study aimed to evaluate the predictive ability of SI and ΔSI in a rural environment with prolonged transport times, and transfers from critical access hospitals or level IV trauma centers.
Methods:
This was a retrospective review of the trauma registry at an American College of Surgeons Verified Level 1 trauma center from January 1, 2017, through December 31, 2018. This center serves as the tertiary referral center for a large rural catchment basin, and half of patients are transferred through a level III or level IV trauma center or critical access hospital. The study included all adult subjects presenting as a trauma activation, after blunt chest or abdominal trauma (AIS>1). Subjects with transport times less than 30 minutes, severe head trauma (AIS Head>3), penetrating injuries, those that received blood products prior to arrival for definitive care, inpatient transfers, and direct from outside hospital operating room transfers were excluded. The study was conducted with approval from the West Virginia University Institutional Review Board and completed in accordance with the STROBE guidelines.
The trauma registry is prospectively maintained by trained registrars. Registry data collected included demographics, injury and transport data, vital signs (EMS, transferring facility, arrival), and hospital outcomes. Shock index was calculated as SI=Heart rate (HR) divided by systolic blood pressure (SBP) and this was calculated from registry vitals from the first set of EMS vitals (SI-EMS), transferring facilities (SI-TX), and on arrival for definitive care (SI-DC). ΔSI was calculated as a time dependent function, for example ΔSI=(SI-EMS) – (SI-DC), as a result negative values for ΔSI indicates worsening SI. Delta SI and SI were determined at each phase of transport to understand the importance of the different time periods associated with outcomes in transport. Hypotension was defined as SBP less than 90 millimeters of mercury (mmHg). Registry data was reviewed to collect data on hemorrhage control procedures through either open or endovascular techniques.
Statistical analysis was performed utilizing Poisson regression and binomial logistic regression to study the effect of time in transport and SI/ΔSI on resource utilization and outcomes. P<0.05 was considered significant.
Results:
After applying inclusion and exclusion criteria, a sample of 676 patients were analyzed. This included 549 (81.2%) scene patients, and 127 (18.8%) transferred from another facility. Of the transferred patients 61 were female (48.0%), compared to 190 females who were direct from scene (34.7%). Mean ISS was 11 (IQR9.0) for scene and 13 (IQR6.5) for transfers. The time to arrival to the trauma center from the scene differ between the two groups as expected and shows that the mean time for patients transported direct from scene was 75.63 minutes (median 58 minutes, IQR 27) and those routed through a transferring facility had a mean time of 366.5 minutes (median 341 minutes, IQR 166.5). After arrival for definitive care, blood products were transfused in 9.1% of scene patients and 15.0% of transfer patients. Hemorrhage control procedures were required in 38 (6%) of scene patients and 16 (12%) of transfers.
We investigated SI and corresponding ΔSI as a measure of injury severity. There was a weak positive correlation (r=0.34) between ISS and SI, and no correlation between ISS and ΔSI The SI-EMS for scene patients transported to the trauma center had a mean of 0.684 (standard deviation 0.213) while the patients who were routed through a transferring facility had a mean SI-EMS of 0.701 (standard deviation 0.240). This difference was not significant (p=0.450). For transferred patients, SI-TX had a mean of 0.686 (standard deviation 0.2). On arrival for definitive care, the mean SI-DC was 0.676 (standard deviation 0.191) for scene transports and 0.708 (standard deviation 0.0.248) for transfers (p=.178).
The mean ΔSI from SI-EMS to SI-DC for patients who were transported directly from the scene is −0.007 (standard deviation of 0.189), while those being transported through a transfer facility have a mean ΔSI from scene to trauma center of 0.006 (standard deviation of 0.250) (p=0.5518). For patients who were transferred, the ΔSI between SI-EMS and the SI-TX demonstrated a mean of −0.015 (standard deviation of 0.169).
The effects of SI and ΔSI were then evaluated on need for blood product transfusion, number of units of packed red blood cells (PRBC), intensive care unit length of stay (ICU LOS), and mortality. For comparison the effect of SI was evaluated both with and without accounting for the presence of hypotension in the respective models. Results show that SI-EMS (Table 1) and EMS hypotension (Table 2) are significant predictors of resource use when investigated separately, with the exception being that hypotension was not shown to be significant in mortality. Hence, we study the impact of SI-EMS when hypotension is included in the models (Table 3). SI-EMS was the most significant predictor for PRBC transfusion and ICU care in both scene and transferred patients when adjusting for the impact of SBP<90 mmHg. A 0.1 change in SI produces a 50.9% increase in odds ratio of receiving any blood and a 31% increase in the expected number of units of PRBC. Similarly, a 0.1 change in SI-EMS predicts an 13.7% increase in the expected days spent in ICU, (p<0.0001 in transferred patients) compared to SI-TX or SI-DC. A negative ΔSI was significantly associated with the need for transfusion and the number of PRBC transfused. Longer transport time also had a significant relationship with increasing ICU LOS (p<0.01) for transfer patients. Mortality was found to be associated with EMS-SI in all patients at the p<0.1 level (0.1 increase in SI predicts a 29.87% increase in the odds ratio of death, p<.1), while time, hypotension, and ΔSI were not significant at any standard level.
Table 1:
Evaluation of ICU LOS, use of blood products, and number of units PRBC based on scene vs. transfer status when considering only SI-EMS. Regression coefficients corresponding to analysis.
| Transfer Patients | Scene Patients | All Patients | |||||
|---|---|---|---|---|---|---|---|
| Days in ICU (Log Scale) | Use of any Blood product (Binomial Logistic) | Number of Units of PRBC (log scale) | Days in ICU (Log Scale) | Use of any Blood product (Binomial Logistic) | Number of Units of PRBC (log scale) | Mortality (Binomial Logistic) | |
| Intercept | 0.372 (0.219) . | −5.778 (1.543)*** | −1.349 (0.726) | 1.028 (0.110)*** | −6.083 (0.747)*** | 1.447 (0.358) | −5.844 (1.021)*** |
| Time | 0.001 (.0002)*** | 0.001 (0.002) | 0.000 (0.001) | −0.001 (.001) | 0.001 (0.001) | −0.006 (.003) | 0.001 (0.002) |
| SI-EMS | 1.058 (.220)*** | 4.875 (1.599)** | 2.167 (0.661)** | 0.623 (0.129)*** | 5.147 (0.815)*** | 0.218 (0.637) | 2.80 (1.228K)* |
| ΔSI (EMS-DC) | 0.23 (0.145) | 3.134 (0.782)*** | 0.637 (0.286)* | 0.358 (1.451) | |||
| ΔSI (EMS-TX) | −0.388 (0.343) | 2.254 (2.034) | 1.219 (0.916) | ||||
| ΔSI (Tx-DC) | 0.4445 (0.231). | 1.954 (1.216) | 1.277 (0.441)** | ||||
The significance is indicated by p-value<0.10 (.), p-value<0.05 (*), p-value <0.01 (**), p-value <0.001 (***).
Table 2:
Evaluation of ICU LOS, use of blood products, and number of units PRBC based on scene vs. transfer status when considering only EMS hypotension. EMS hypotension defined as SBP<90mmHg. Regression coefficients corresponding to analysis.
| Transfer Patients | Scene Patients | All Patients | |||||
|---|---|---|---|---|---|---|---|
| Days in ICU (Log Scale) | Use of any Blood product (Binomial Logistic) | Number of Units of PRBC (log scale) | Days in ICU (Log Scale) | Use of any Blood product (Binomial Logistic) | Number of Units of PRBC (log scale) | Mortality (Binomial Logistic) | |
| Intercept | 1.009 (0.124). | −2.250 (0.641)*** | 0.985 (0.248)*** | 1.499 (0.052)*** | −2.437 (0.266)*** | 1.601 (0.178) | −3.970 (1.021)*** |
| Time | 0.001 (0.000)*** | 0.001 (0.002) | 0.000 (0.001) | −0.000 (0.000) | 0.001 (0.001) | −0.003 (.002) | 0.001 (0.002) |
| EMS Hypotension | 1.207 (0.229)*** | 2.873 (1.117)*** | 1.424 (0.364)*** | 0.149 (0.138)*** | 4.270 (0.815)*** | −0.231 (0.637) | 1.433 (0.977) |
| ΔSI (EMS-DC) | 0.032 (0.128) | 1.331 (0.671) * | −0.581 (0.286)** | −0.547 (1.064) | |||
| ΔSI (EMS-TX) | −0.363 (0.330) | 0.901 (1.561) | 1.276 (0.523)* | ||||
| ΔSI (Tx-DC) | 0.4445 (0.231). | 1.48 (1.097) | 1.050 (0.321)** | ||||
The significance is indicated by p-value<0.10 (.), p-value<0.05 (*), p-value <0.01 (**), p-value <0.001 (***).
Table 3:
Evaluation of ICU LOS, use of blood products, and number of units PRBC based on scene vs. transfer status when considering both SI-EMS and EMS hypotension. EMS hypotension defined as SBP<90mmHg. Regression coefficients corresponding to analysis.
| Transfer Patients | Scene Patients | All Patients | |||||
|---|---|---|---|---|---|---|---|
| Days in ICU (Log Scale) | Use of any Blood product (Binomial Logistic) | Number of Units of PRBC (log scale) | Days in ICU (Log Scale) | Use of any Blood product (Binomial Logistic) | Number of Units of PRBC (log scale) | Mortality (Binomial Logistic) | |
| Intercept | 0.143 (0.236) | −5.324 (1.66)** | −1.570 (0.730)* | 1.431 (0.052)*** | −5.344 (0.266)*** | 1.325 (0.363) | −5.716 (1.114)*** |
| Time | 0.001 (0.000)*** | 0.001 (0.002) | −0.000 (0.001) | −0.000 (0.000) | 0.001 (0.004) | −0.006 (.003). | −0.002 (0.002) |
| SI-EMS | 1.284 (0.275)*** | 4.117 (1.863)* | 2.760 (0.828)*** | 0.088 (0.182) | 3.903 (0.896)*** | 0.422 (0.355) | 2.610 (1.406). |
| EMS Hypotension | −0.727 (0.372). | 1.711 (2.59) | −1.185 (0.828)*** | 0.129 (0.154) | 3.237 (0.887)*** | −0.354 (0.254) | 0.331 (1.079) |
| ΔSI (EMS-DC) | −0.060 (0.166) | 3.545 (0.818) *** | 0.606 (0.291)* | 0.391 (1.446) | |||
| ΔSI (EMS-TX) | −0.816 (0.439). | 2.846 (2.128) | 0.487 (1.154) | ||||
| ΔSI (Tx-DC) | 0.244 (0.278) | 1.987 (1.248) | 1.088 (0.487)* | ||||
The significance is indicated by p-value<0.10 (.), p-value<0.05 (*), p-value <0.01 (**), p-value <0.001 (***).
Figure 1 presents a comparison of the models for the probability of using any blood products and for the number of units of PRBC used on arrival for definitive care. These were performed for each patient type under the assumption that hypotension was present, and all other variables are set to the mean for that patient type. The results show the impact of EMS-SI in resource usage and the importance of this calculation specifically in transfer patients to do their increased number of PRBC required.
Figure 1-.
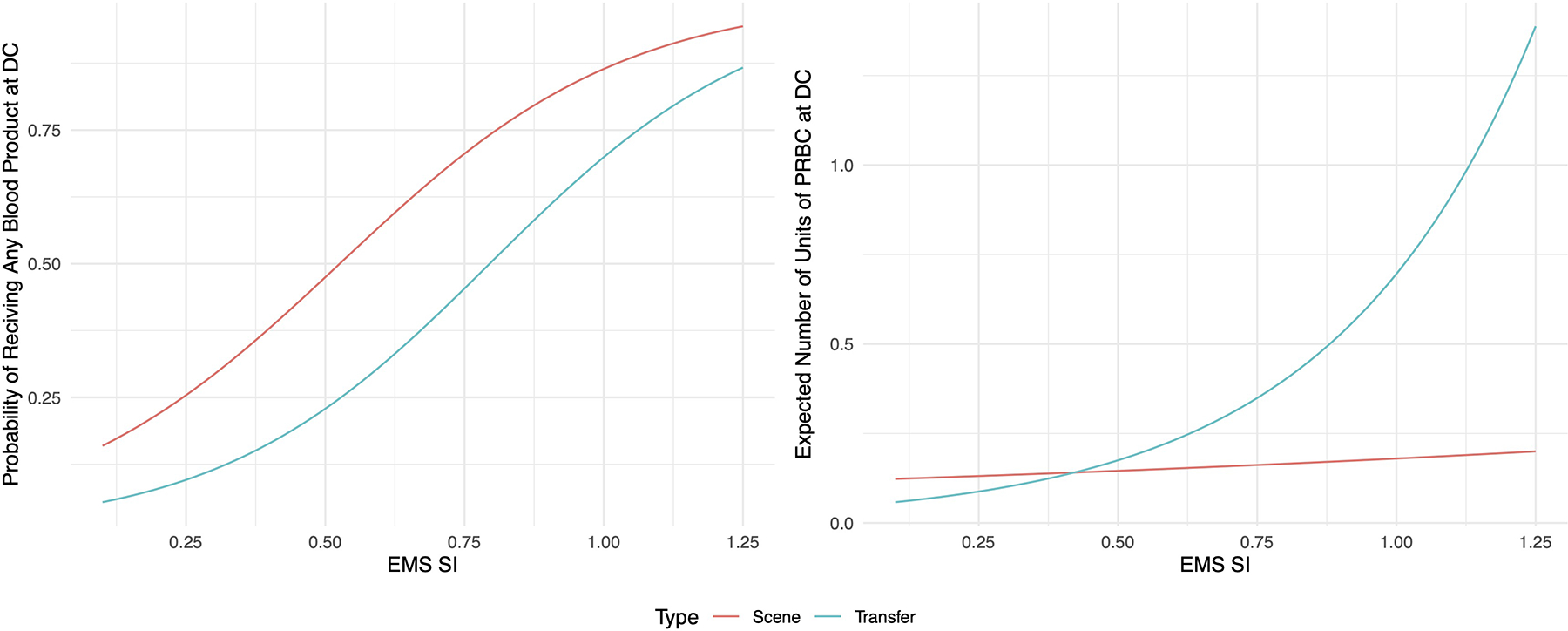
Effect plots for binomial logistic and Poisson regression models, demonstrating need for any blood product and expected number of packed red blood cells (PRBC) on arrival for definitive care (DC). Models performed under the assumption hypotension was present, and all other variables are set to the mean for that patient type.
Discussion:
Rural trauma patients face barriers in time, distance, and access to receiving surgical care. State trauma systems have developed to allow for initial triage, transport, and stabilization enroute to a definitive care center. The differences in transport time effects the applicability of some urban studies to rural locations. Due to this observation, the authors aimed to evaluate the predictive ability of shock index at multiple stages in a patients care. This study demonstrated that initial EMS-SI was the most predictive of patient outcomes and resource utilization. Our findings build upon the work by Seamon et al. demonstrating that a single episode of hypotension was predictive of severe injury, despite subsequent improvements in blood pressure13. As a result, trauma surgeons must maintain a high level of clinical suspicion for patients who had an initially elevated SI, despite improvement during transport and resuscitation. This is particularly important for the surgeon at an accepting facility, and providers should not have a false sense of security due to the time that has passed since the injury occurred if the initial SI was elevated.
Evaluating the mean SI and ΔSI at each phase of patient contact had some interesting findings. Transfer patients had a higher mean SI-EMS than did scene patients. While not statistically significant this may imply that rural patients requiring transfer are sicker, and beyond the capability of the initial facility. Similarly, the initial facility may identify a severe but not life-threatening injury, and still be able to successfully transfer the patient, leading to the increase in ICU LOS seen with increased time from injury. On average there was also a negative ΔSI during transport, indicating worsening SI as time from injury increased. For the patient with non-compressible hemorrhage this is to be expected. However, the patients that went through a transferring facility had a smaller change in SI. This is likely explained by increased resuscitation or interventions during transport, however that data was not reliable for analysis.
As expected, hypotension independently predicted increased ICU days and the need for blood products. However, SI-EMS demonstrated a larger effect size for these predictions. This study then identified the added value using SI-EMS in conjunction with the presence of hypotension. Perhaps due to long transport time, this combination demonstrated an even greater ability to predict days in ICU and use of blood products based on SI-EMS. This suggests further study be conducted on the use of SI in trauma team activation criteria after blunt torso trauma.
This study has all the usual limitations of a retrospective study. The lack of serial vital signs and timing of interventions must be mentioned. The registry routinely collects a single set of vital signs from each phase of patient transport, and resuscitation interventions performed by EMS and transferring facilities are poorly captured. Unfortunately, there was a high percentage of missing data on prehospital fluids which precluded analysis on its effects of SI over time. This practice is common place in trauma registries, and demonstrated in large national databases as well14. This could worsen the survivor bias seen in this environment. For subjects that received ongoing and progressive resuscitation enroute to definitive care, this lack of granular data could blunt the impact of ΔSI, SI-TX, and SI-DC, but the demonstrated use of SI-EMS should be preserved. Finally, the impact on SI-EMS on the need for hemorrhage control procedures is an area for further study, this cohort was limited by the small percentage of patients requiring operative intervention.
EMS-SI was the greatest predictor of need for resources and mortality. SI and ΔSI were less predictive as time from injury increased and patients stopped at transferring facilities. This highlights the improvements in enroute care but does not eliminate the need for high-level trauma intervention. Based on these results, elevated EMS-SI could also be considered a triage component for use in rural environments. Trauma surgeons in similar clinical settings should maintain a high index of suspicion for patients with an elevated EMS shock index, despite improvements in vital signs during transport.
Supplementary Material
Sources of Funding
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 5U54GM104942. This work is supported in part by funds from the National Science Foundation NSF: #1920920. Funding provided protected research time for the investigators.
Footnotes
The authors have no conflicts of interest to declare.
This work was presented as a poster during the 80th Annual Meeting of the American Association for the Surgery of Trauma, Atlanta, GA, September 30, 2021.
Reference:
- 1.Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, Blatt AJ, ReVelle CS. Access to Trauma Centers in the United States. JAMA. 2005;293(21):2626. [DOI] [PubMed] [Google Scholar]
- 2.Carr B, Bowman A, Wolff C, Mullen MT, Holena D, Branas CC, Wiebe D. Disparities in Access to Trauma Care in the United States: A Population-Based Analysis. Injury. 2017;48(2):332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jarman MP, Castillo RC, Carlini AR, Kodadek LM, Haider AH. Rural risk: Geographic disparities in trauma mortality. Surgery. 2016;160(6):1551–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grossman DC, Kim A, Macdonald SC, Klein P, Copass MK, Maier RV. Urban-rural Differences in Prehospital Care of Major Trauma. J Trauma. 1997;42(4):723–729. [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez RP, Cummings G, Mulekar M, Rodning CB. Increased Mortality in Rural Vehicular Trauma: Identifying Contributing Factors Through Data Linkage. J Trauma. 2006;61(2):404–409. [DOI] [PubMed] [Google Scholar]
- 6.Esposito TJ, Maier RV, Rivara FP, Pilcher S, Griffith J, Lazear S, Hogan S. The impact of variation in trauma care times: urban versus rural. Prehosp Disaster Med. 10(3):161–166; discussion 166–7. [DOI] [PubMed] [Google Scholar]
- 7.Cannon CM, Braxton CC, Kling-Smith M, Mahnken JD, Carlton E, Moncure M. Utility of the Shock Index in Predicting Mortality in Traumatically Injured Patients. J Trauma. 2009;67(6):1426–1430. [DOI] [PubMed] [Google Scholar]
- 8.Joseph B, Haider A, Ibraheem K, Kulvatunyou N, Tang A, Azim A, O’Keeffe T, Gries L, Vercruysse G, Rhee P. Revitalizing Vital Signs: The Role of Delta Shock Index. Shock. 2016;46(3S):50–54. [DOI] [PubMed] [Google Scholar]
- 9.Schroll R, Swift D, Tatum D, Couch S, Heaney JB, Llado-Farrulla M, Zucker S, Gill F, Brown G, Buffin N, et al. Accuracy of shock index versus ABC score to predict need for massive transfusion in trauma patients. Injury. 2018;49(1):15–19. [DOI] [PubMed] [Google Scholar]
- 10.Schellenberg M, Strumwasser A, Grabo D, Clark D, Matsushima K, Inaba K, Demetriades D. Delta Shock Index in the Emergency Department Predicts Mortality and Need for Blood Transfusion in Trauma Patients. Am Surg. 2017;83(10):1059–1062 [DOI] [PubMed] [Google Scholar]
- 11.Trust MD, Schellenberg M, Biswas S, Inaba K, Cheng V, Warriner Z, Love BE, Demetriades D. Prehospital Vital Signs Accurately Predict Initial Emergency Department Vital Signs. Prehosp Disaster Med. 2020;35(3):254–259. [DOI] [PubMed] [Google Scholar]
- 12.Schellenberg M, Biswas S, Bardes JM, Trust MD, Grabo D, Wilson A, Inaba K. Longer Prehospital Time Decreases Reliability of Vital Signs in the Field: A Dual Center Study. Am Surg. 2021;87(6):943–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seamon MJ, Feather C, Smith BP, Kulp H, Gaughan JP, Goldberg AJ. Just one drop: The significance of a single hypotensive blood pressure reading during trauma resuscitations. J Trauma. 2010;68(6):1289–1294. [DOI] [PubMed] [Google Scholar]
- 14.Zehtabchi S, Nishijima DK, McKay MP, Mann NC. Trauma Registries: History, Logistics, Limitations, and Contributions to Emergency Medicine Research. Acad Emerg Med. 2011;18(6):637–643. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


