During the first wave of the coronavirus disease 2019 (COVID-19) pandemic, there was a decline in admissions with cardiovascular disease, corresponding to social containment mandates (1, 2, 3). It is not clear whether widespread media coverage around this phenomenon during the first wave would potentially lessen the effect of any subsequent social containment mandates on cardiovascular admissions. Using data from the NHFA (National Heart Failure Audit) and MINAP (Myocardial Ischaemia National Audit Project), we examined whether the public response to the second national lockdown in the United Kingdom replicated that of the first.
We studied the daily incidence of admissions with heart failure (HF) and myocardial infarction (MI) among adults in the National Institute for Cardiovascular Outcomes Research databank between November 1, 2018, and November 17, 2020. To avoid data reporting lag bias, we only included rapid reporting hospitals (22 and 42 hospitals for NHFA and MINAP, respectively) for the analysis. We compared the daily incidence of hospital admissions for the pre–COVID-19 period (November 1, 2018, to March 22, 2020) with that of the nadir and peak following the first UK lockdown and the rates in the second UK lockdown to date of latest available data (November 17, 2020). Incidence rate ratios, estimated from an interrupted times series using a generalized linear model for a Poisson distribution fitted and adjusted for seasonality with a harmonic term, were used to compare the relative change in event rates between the periods. All datasets used in our study collect information routinely used for audit research purposes without requiring informed patient consent under section 251 of the National Health Service Act 2006, and therefore, institutional board review was not required for this study. Access to datasets required for this study has been fast-tracked by adopting a novel collaboration as part of the national drive for research related to COVID-19.
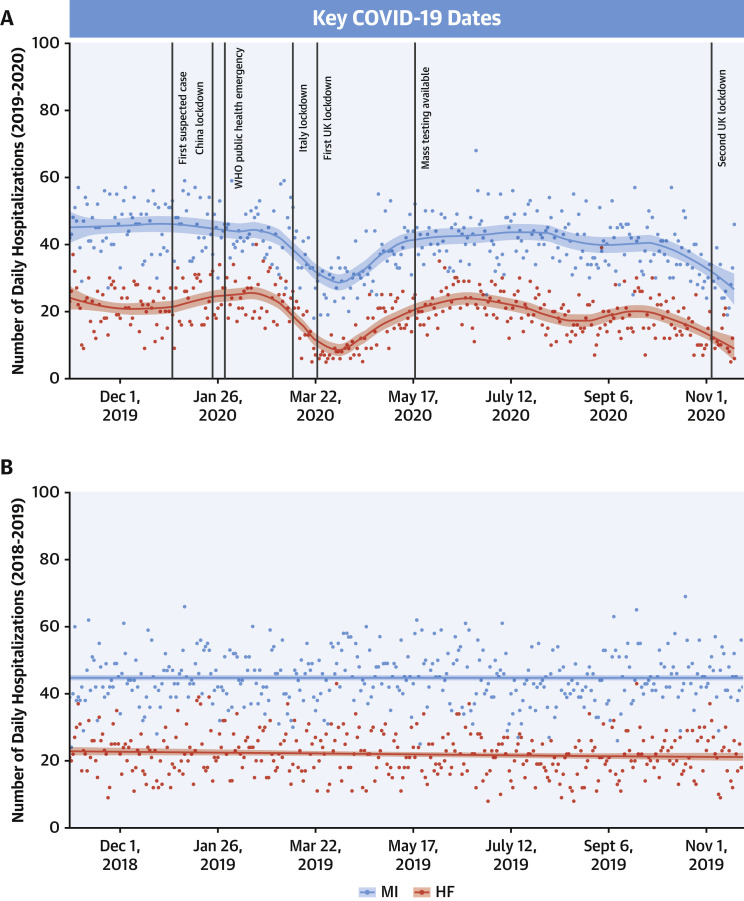
For the rapid reporting hospitals, there were 62,683 admissions with HF and MI between November 1, 2018, and November 17, 2020. From March 23, 2020 (first UK lockdown), daily HF and MI hospitalizations decreased by 54% (incident rate ratio [IRR]: 0.46; 95% confidence interval [CI]: 0.41 to 0.51) and by 32% (IRR: 0.68; 95% CI: 0.65 to 0.73) to a nadir on April 2, 2020, and April 4, 2020, respectively (Figure 1A ). For admissions with HF and MI, peak recovery occurred on June 16, 2020, and June 29, 2020, respectively, but remained at 95% (IRR: 0.95; 95% CI: 0.91 to 0.99) and 93% (IRR: 0.93; 95% CI: 0.90 to 0.95) of pre–COVID-19 rates. From the beginning of October 2020, there was a second decline in admissions by 41% for HF (IRR: 0.59; 95% CI: 0.54 to 0.64) and by 34% for MI (IRR: 0.66; 95% CI: 0.63 to 0.69) up to November 17, 2020, compared with the pre–COVID-19 period. As a comparison, there was little variation in admissions with HF and MI in the baseline year between 2018 and 2019 (Figure 1B).
Figure 1.
Times Series of Daily Admissions With HF and MI
The daily admission data were presented for heart failure (HF) and myocardial infarction (MI) from November 1, 2019, to November 17, 2020 (30,380 admissions) (A) and from November 1, 2018, to November 17, 2019 (33,831 admissions) (B). Daily hospitalizations were plotted in a scatterplot and fitted with a smooth curve using local weighted scatterplot smoothing technique for HF and acute MI, respectively. The peak and nadir of daily hospitalizations were derived from the fitted curve. (Updates of the figure will be available at the University of Leeds’s Cardiovascular Research Into the COVID-19 Virus website.) COVID-19 = coronavirus disease 2019; WHO = World Health Organization.
Despite an initial recovery in admissions with HF and MI, the latter part of 2020 has witnessed a second decline in people hospitalized with these conditions, which pre-dated the onset of the second national lockdown in the United Kingdom. The second dip appears of similar magnitude to that of the first and signals that the public are fearful of attending hospitals despite having medical emergencies, and that this varies over time—possibly relating to numbers of cases and social mandates. Given that the period cohort for this analysis cannot determine a nadir in admissions, rates of admissions may decline further. This is important because earlier work from the United Kingdom described how delays to seeking help were temporally related to an inflation in deaths from a range of acute cardiovascular diseases (4,5). Clear public messaging is necessary to prevent further unintended consequences of social distancing mandates to reduce the spread of severe acute respiratory syndrome coronavirus 2.
Footnotes
Drs. Wu and Gale have received funding from the University of Leeds. Dr. Mamas has received funding from the University of Keele. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose. The funding organizations for this study had no involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. Dr. Wu had full access to all of the data in the study and takes responsibility for the accuracy of the data analysis. The National Institute for Cardiovascular Outcomes (NICOR) provided NHS Digital with the Myocardial Ischaemia National Audit Project (MINAP) and National Heart Failure Audit (NHFA) data and has accepted responsibility for the integrity of the MINAP and NHFA data. The authors do not have authorization to share the data, but the data can be accessed through NHS Digital upon approval.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Mafham M.M., Spata E., Goldacre R., et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Solomon M.D., McNulty E.J., Rana J.S., et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 3.Wu J., Mamas M., Rashid M., et al. Patient response, treatments and mortality for acute myocardial infarction during the COVID-19 pandemic. Eur Heart J Qual Care Clin Outcomes. 2020 Jul 30 doi: 10.1093/ehjqcco/qcaa062. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu J., Mamas M.A., Mohamed M.O., et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2020 Sep 28 doi: 10.1136/heartjnl-2020-317912. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Banerjee A., Pasea L., Harris S., et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020;395:1715–1725. doi: 10.1016/S0140-6736(20)30854-0. [DOI] [PMC free article] [PubMed] [Google Scholar]