Abstract
Background
A ‘terrible triad injury of the elbow’ (TTIE) refers to an injury pattern involving posterior dislocation of the ulnohumeral joint, fracture of the radial head, and fracture of the coronoid process of the ulna. It is a complex injury to the elbow joint and can result in long-term elbow instability, pain, stiffness, and arthritis. In specific cases, it may be treated conservatively, but in most circumstances, surgical stabilization is advised.
The ‘drop sign’ is an objective static radiographically measured ulnohumeral distance of ≥4 mm seen intraoperatively and postoperatively. Although controversial, it may portend postoperative instability and arthritis. The senior author repairs these injuries in a standardized fashion through a modified Boyd rather than a lateral approach. Our aim was to assess the number of cases demonstrating an intraoperative drop sign after surgical treatment of a TTIE with this approach.
Methods
We retrospectively analyzed 22 consecutive patients with 23 acute TTIEs. These injuries were treated by a single surgeon using a modified Boyd (posterior) approach to the elbow. Intraoperative image intensifier x-rays were analyzed by the two authors to assess for a ‘drop sign’.
Results
None of the 23 cases had ‘drop signs’ on intraoperative imaging after stabilization. No patient has redislocated, underwent reoperation, or had symptoms of instability at follow-up.
Conclusion
None of our patient cohort had an intraoperative ‘drop sign’ after standardized stabilization for a TTIE injury using a modified Boyd approach.
Keywords: Elbow, Trauma, Terrible triad injury, Drop sign, Posterior approach, Boyd approach
A ‘terrible triad injury of the elbow’ (TTIE) refers to a combination of injuries which includes posterior dislocation of the ulnohumeral joint, fracture of the radial head, and fracture of the coronoid.3 It is a complex injury to the elbow joint and is associated with elbow instability, pain, stiffness, and arthritis.11 The injury can be treated conservatively, but in most circumstances, it undergoes surgical stabilization.
A number of surgical approaches have been described to the elbow for treatment of a terrible triad injury, and the best approach remains controversial. Surgical approaches are predominantly laterally based with a separate medial incision used if repair of the anterior medial collateral ligament is required to achieve stability. Examples are the posterolateral approach (Kocher) and the lateral approach (Kaplan). It is the senior author’s preference to address terrible triad injuries posteriorly, through a modified Boyd approach.12 The initial Boyd approach was described in 1940 and has undergone modification over the years. It facilitates excellent access to the radiocapitellar joint. In acute elbow instability, the anterior joint is also easily accessible. As the superficial approach is a dorsal utility skin incision, it can be combined with a medial approach without the need for a second incision. There is also minimal risk to the posterior interosseous nerve, and it can be extended more distally than the lateral approach.
Campbell’s Operative Orthopaedics states the choice of approach depends primarily on ‘fracture pattern, type of instability, soft-tissue injury, and surgeon experience’ and that ‘regardless of the approach selected, every effort should be made to operate through the traumatized planes and minimize surgical dissection’.9 The fixation strategy is usually from the inside out starting with the coronoid to the anterior capsule to the radial head to the lateral collateral ligament to the common extensor origin.4
In a study by Coonrad et al,1 the term ‘drop sign’ was first coined. The ‘drop sign’ is an objective static radiographically measured ulnohumeral distance of ≥ 4 mm. This sign is ‘likely to be associated with complete disruption or attenuation of the lateral or medial ligament complex or both’. The authors emphasized that the ‘drop sign’ was a different observation to the ulnohumeral separation or perching noted during O’Driscoll’s test for posterolateral rotatory instability,5,6 which is present only with axial compression and valgus stress. Although controversial, when present, it may portend postoperative instability and arthritis.3,11
Duckworth et al2 describe the ‘drop sign’ as a ‘residual subluxation’ and say it is ‘a type of pseudosubluxation analogous to that which is frequently observed in the shoulder’. Duckworth et al suggest that the ‘drop sign’ is related to relaxation of the muscles across the elbow joint. They suggest an active motion protocol with avoidance of varus stress to add dynamic muscular contributions to elbow stability.
Our approach follows a stepwise protocol with the patient in the supine position and the affected arm held in a leg holder. The procedure is performed under tourniquet control with general anesthesia and peripheral nerve block. A standard dorsal incision is used. After release of the forearm fascia and subperiosteal dissection of the anconeus, the incision is continued proximally, into the elbow joint and extending into the triceps tendon. The tissue is dissected laterally until the lateral ligamentous structures (and usually the common extensor origin) can be seen avulsed from their origin. The elbow is then dislocated, and a stitch is placed in the anterior capsule. This suture is shuttled through drill holes placed in the fractured coronoid base and exiting on the dorsal aspect of the ulna. The radial head is then either fixed or replaced. Any annular or distal lateral ligamentous damage is repaired to its insertion through transosseous drill holes in the ulna. The lateral structures are repaired as a single sheet of tissue with an anchor placed in the isometric point of the lateral capitellum. Both the capsular stitch and anchor are tied in 30 degrees of flexion. The elbow is then tested for stability through a range of motion both clinically and radiologically. The setup allows a variety of arm positions for radiographic analysis. It is the author’s preference to have the arm suspended by the hand with the image intensifier placed parallel to the bed in a “U” position to assess for a drop sign.
Our aim was to assess the number of cases demonstrating an intraoperative drop sign after stepwise surgical treatment of a TTIE through a modified Boyd approach.
Materials and methods
We retrospectively analyzed 22 consecutive patients with 23 TTIEs. These injuries were managed by one surgeon in one center using the Boyd (posterior) approach to the elbow. All cases were operated on within 2 weeks of the injury. Patients undergoing revision surgery and requiring anteromedial coronoid facet or olecranon fixation were excluded as were those with an associated proximal radio-ulnar joint dislocation.
Surgery is performed in the supine position with the arm supported in a Lloyd-Davies leg holder placed on the contralateral side of the patient. The posterior antebrachial cutaneous nerve is usually lateral to the initial skin incision, but one should be aware of its proximity and its branches during the superficial dissection. Anconeus is innervated proximally by a branch of the radial nerve. Its vascular supply is deep to the muscle. Therefore, sharp dissection of anconeus from its insertion to the ulna should not denervate or devascularize the muscle. In the deeper dissection, the posterior interosseous nerve runs through or deep to the supinator muscle. Therefore, dissection should be outside the muscle belly, and excessive retraction of the supinator should be avoided.
Superficial exposure
A longitudinal skin incision is made just lateral to the palpable subcutaneous border of the ulna (Fig. 1). Towards the lateral border of the triceps, full thickness flaps are raised off the deep fascia.
Figure 1.

A longitudinal skin incision is made just lateral to the palpable subcutaneous border of the ulna.
Deep exposure
The fascia covering anconeus and extensor carpi ulnaris is identified and incised longitudinally for the length of the skin incision, leaving a cuff of fascia approximately 3 to 5 mm in width attached to the ulna (Fig. 2). The anconeus and the more distal extensor carpi ulnaris are elevated subperiosteally to reveal the supinator deep to them. Supinator can also be raised subperiosteally from the ulna.
Figure 2.

The fascia covering anconeus and extensor carpi ulnaris is identified and incised longitudinally for the length of the skin incision, leaving a cuff of fascia approximately 3 to 5 mm in width attached to the ulna.
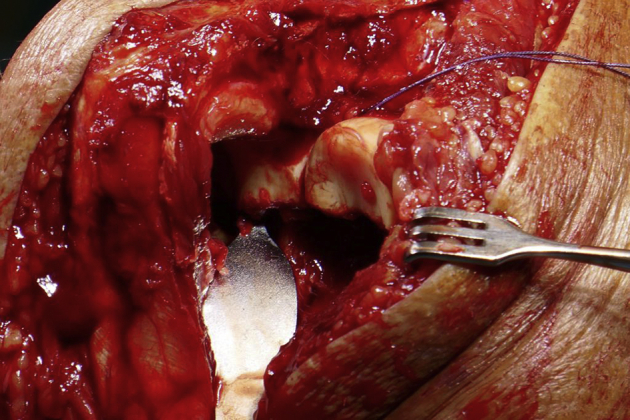
Deep to this layer, the annular ligament, the lateral ulnar collateral ligament (LUCL), and the joint capsule complex are identified. The radial head can be palpated deep to these. Attention should be paid to the insertion sites of these structures for later reference when performing an anatomic repair. The ligaments and capsule are released directly off the ulna at the supinator crest using sharp dissection (Fig. 3).
Figure 3.
The ligaments and capsule are released directly off the ulna at the supinator crest using sharp dissection.
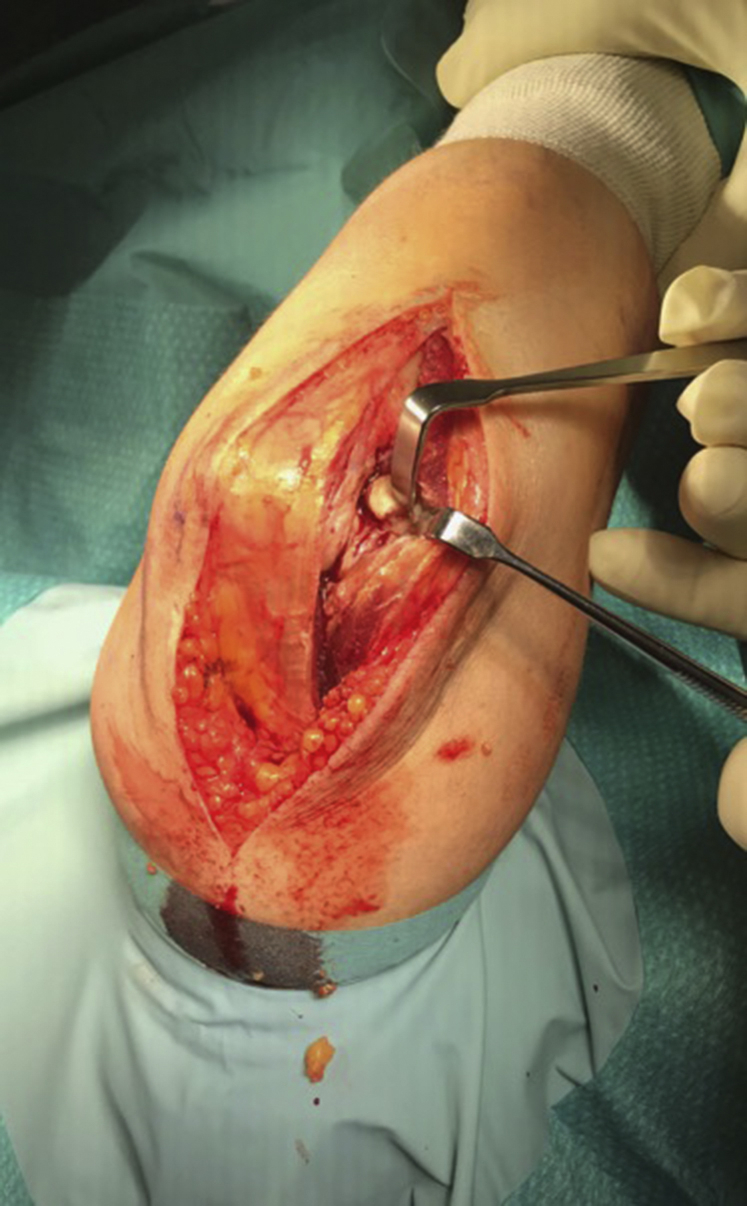
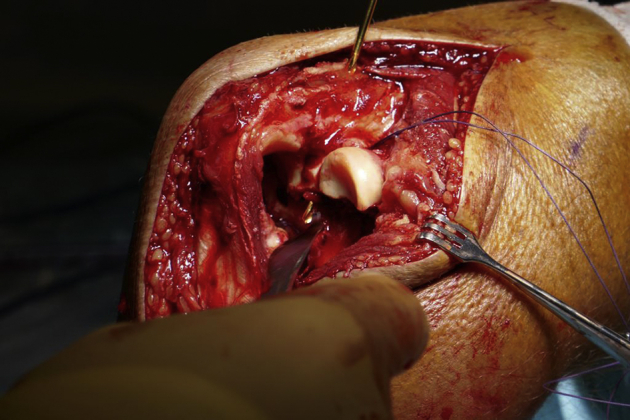
The tissue is dissected laterally until the lateral ligamentous structures (and usually the common extensor origin) can be seen avulsed from their origin. The elbow is then dislocated, and a stitch is placed in the anterior capsule (Fig. 4). This suture is shuttled through a 2.5-mm drill hole placed in the fractured coronoid base and exiting on the dorsal aspect of the ulna (Figs. 5 and 6). The radial head is then either fixed or replaced. A drill hole is created at the insertion point of the lateral collateral ligament complex, and an anchor is inserted (Fig. 7). Bone tunnels are made in the ulna using a 2.5-mm drill to allow repair of the capsule and annular ligament and insertion of the LUCL at the supinator crest. It is important that the tunnels exit at the correct site for anatomic repair of the capsuloligamentous structures to ensure elbow stability. The capsule, LUCL, and annular ligament are captured using a grasping suture configuration. These are retrieved through the bone tunnels and tied on the medial side of the ulna, ensuring that the capsule, annular ligament, and LUCL complex are all apposed to bone (Fig. 8). The lateral structures are repaired as a single sheet of tissue with an anchor placed in the lateral epicondyle (Fig. 9). The fascial layer is then repaired back to the cuff of fascia created on the ulna with a number 1 Vicryl suture (Fig. 10). From this approach, the point of avulsion (most common lateral injury) can be clearly seen. Interestingly, the lateral ligamentous footprint is broad and not always at the traditional “center point”. Both the capsular stitch and anchor are tied in 30 degrees of flexion. The elbow is then tested for stability through a range of motion both clinically and radiologically in the coronal and sagittal planes. The setup allows a variety of arm positions for radiographic analysis. It is the author’s preference to have the arm suspended by the hand with the image intensifier placed parallel to the bed in a “U” position to assess for a drop sign in the sagittal plane (Fig. 11). All intraoperative images were analyzed by the two authors to assess for a ‘drop sign’.
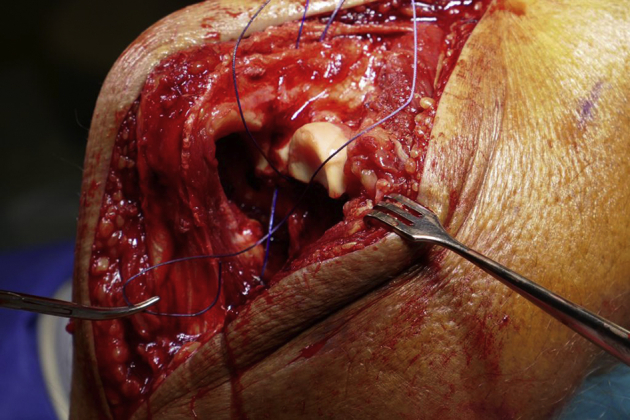
Figure 4.
A stitch is passed into the anterior capsule.
Figure 5.
The ulna is drilled at the insertion of the lateral collateral ligament complex from dorsal ulnar through the base of the coronoid process.
Figure 6.
This suture is shuttled through drill holes placed in the fractured coronoid base and exiting on the dorsal aspect of the ulna.
Figure 7.
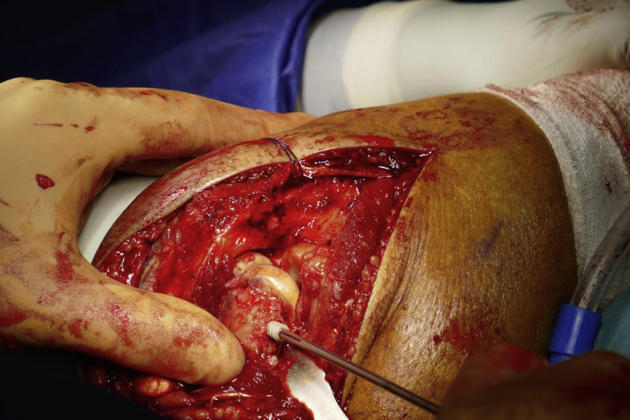
A suture anchor is inserted at the insertion point of the lateral collateral ligament complex.
Figure 8.

The lateral collateral ligament complex is then sutured from in to out with the stitches from the suture anchor.
Figure 9.
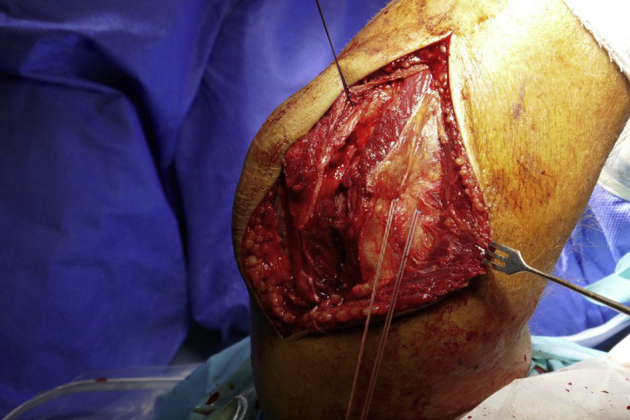
Number 5 TiCron suture is retrieved through the bone tunnels and tied on the medial side of the ulna, ensuring that the capsule, annular ligament, and LUCL complex are opposed to bone.
Figure 10.

The fascial layer is then repaired back to the cuff of fascia created on the ulna with a number 1 Vicryl suture.
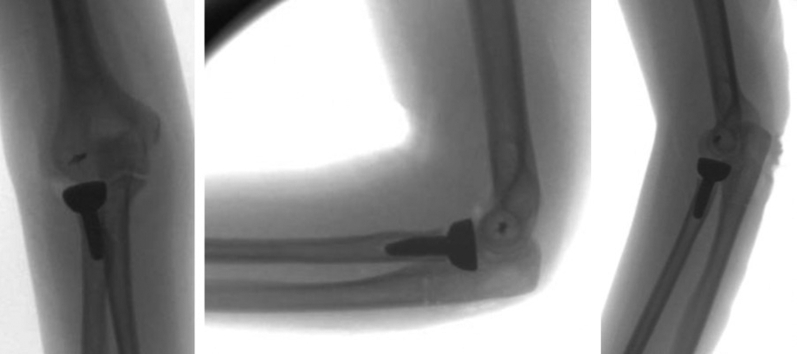
Figure 11.
Immediate postoperative images which demonstrate a negative ‘drop sign’.
Rehabilitation
Patients are immobilized in a sling only for 6 weeks. The patient is reviewed by physiotherapy postoperatively and allowed full active supination and pronation. Passive supination is not advised as it may detension the lateral structures.
In the author’s opinion, active supination will occur predominantly through the biceps which should aid stability and is allowed. Active and passive flexion and extension is advised up to the last 30 degrees of extension. Patients are reviewed at 2 weeks, checked radiologically and clinically, and referred for physiotherapy. At 6 weeks, all restrictions are removed and full return to activities commenced.
Results
None of the 23 cases demonstrated ‘drop signs’ on intraoperative imaging after surgery was performed (Table I). No patient required a medial repair or external fixator. No patient has redislocated, has undergone reoperation, or has symptoms of instability at follow-up.
Table I.
Patient characteristics.
| No. of operations | Age | DOS | Diagnosis | Treatment | Drop sign |
|---|---|---|---|---|---|
| 1 | 28 | Sep-17 | Left TT | ORIF RH, capsule + lateral repair | Neg |
| 2 | 21 | Nov-17 | Right TT | ORIF RH, capsule + lateral repair | Neg |
| 3 | 61 | Mar-18 | Left TT | ORIF RH, capsule + lateral repair | Neg |
| 4 | 61 | Mar-18 | Right TT | RHR, capsule + lateral repair | Neg |
| 5 | 56 | Jun-18 | Left TT | ORIF RH, capsule + lateral repair | Neg |
| 6 | 29 | Oct-18 | Left TT | RHR, capsule + lateral repair | Neg |
| 7 | 18 | Oct-18 | Left TT | ORIF RH, capsule + lateral repair | Neg |
| 8 | 55 | Oct-18 | Right TT | ORIF RH, capsule + lateral repair | Neg |
| 9 | 64 | Nov-18 | Left TT | ORIF RH, capsule + lateral repair | Neg |
| 10 | 25 | Jan-19 | Right TT | ORIF RH, capsule + lateral repair | Neg |
| 11 | 70 | Feb-19 | Left TT | ORIF RH, capsule + lateral repair | Neg |
| 12 | 20 | Mar-19 | Right TT | ORIF RH, capsule + lateral repair | Neg |
| 13 | 48 | Apr-19 | Left TT | ORIF RH, capsule + lateral repair | Neg |
| 14 | 74 | Aug-19 | Right TT | RHR, capsule + lateral repair | Neg |
| 15 | 55 | Sep-19 | Right TT | RHR, capsule + lateral repair | Neg |
| 16 | 75 | Sep-19 | Right TT | RHR, capsule + lateral repair | Neg |
| 17 | 58 | Oct-19 | Right TT | RHR, capsule + lateral repair | Neg |
| 18 | 25 | Dec-19 | Right TT | ORIF RH, capsule + lateral repair | Neg |
| 19 | 59 | Dec-19 | Right TT | RHR, capsule + lateral repair | Neg |
| 20 | 27 | Jan-20 | Left TT | ORIF RH, capsule + lateral repair | Neg |
| 21 | 21 | Feb-20 | Right TT | ORIF RH, capsule + lateral repair | Neg |
| 22 | 61 | Feb-20 | Right TT | ORIF RH, capsule + lateral repair | Neg |
| 23 | 65 | Mar-20 | Right TT | ORIF RH, capsule + lateral repair | Neg |
DOS, date of surgery (month-year); ORIF, open reduction and internal fixation; TT, terrible triad; RHR, radial head replacment; RH, radial head.
The average patient age was 47 years. Eleven of the 22 patients were women with one female patient suffering bilateral injuries. In this patient with bilateral elbow injuries, the right radial head was used as a bone graft for open reduction and internal fixation on the left side. Sixteen of the 23 cases underwent radial head open reduction and internal fixation, and 7 underwent radial head replacement. The average ages of patients undergoing fixation and replacement were 42 and 59, respectively.
All cases were performed by the senior author who is a fellowship-trained consultant shoulder and elbow surgeon.
Discussion
Although the ‘drop sign’ is well documented in the literature,9 the relevance has been questioned.10 In an article by Rhyou et al, a drop sign was observed in 17% of patients who underwent a surgical stabilization procedure for an unstable posterolateral elbow dislocation. The drop sign disappeared spontaneously within 1 week of the operation in all 4 cases and therefore did not signify the need for an additional stabilization procedure. A drop sign did not affect the postoperative functional outcome. The drop sign after a stabilization procedure for elbow posterolateral dislocation was felt to be caused by delayed return of muscle tone, which acts as a dynamic stabilizer under the regional block. This point was previously emphasized by Duckworth.2
Our study contradicts this concept of a regional block contributing due to a delayed return of muscle tone. All our patients had a regional block, and no patient had a drop sign. If this were the case, intraoperative radiographs of other traumatic elbow conditions performed under the regional block (ie, distal humeral fractures) would be expected to show a drop sign. We believe that it is subtle instability from a lack of static restraint rather than muscle hypotonia that causes the drop sign. Most cases will not progress to frank instability, but there is evidence that the drop sign persists and can result in secondary surgery.14 King’s group8 in London, Ontario, Canada, looked at the therapeutic implications of a ‘drop sign’ after an elbow dislocation. They state it indicates persistent instability of the elbow joint. They explain the dynamic stabilizers of the elbow undergo significant trauma after an elbow dislocation, resulting in an inhibition to produce muscle contraction. This, along with the ligamentous injury, reduces the compressive forces normally produced at the elbow which can lead to a ‘drop sign’. It is also possible that the arm position during radiographic examination may influence a drop sign. However, we have imaged the arm in different positions with the image intensifier both parallel and at 90 degrees to the floor. This has not changed the radiographic appearance. We postulate that the modified Boyd approach may be of significance. With this approach, repair of the anterior capsule is technically straightforward, and all cases in this series underwent capsular repair. Potentially, this provides improved static restraint for the ulnohumeral joint, although authors have disagreed with the routine use of capsular repair.7 It is also of interest that no patient required a medial repair. It may be that with the stepwise approach, and in particular the method of lateral ligamentous repair, the injury is fully stabilized (in the presence of an intact anterior medial collateral ligament) or converted into a medial collateral ligament injury.
Based on the work by Seki et al,13 the anterior band of the lateral collateral ligament complex has been highlighted for elbow stability in varus and external rotation. Based on their anatomical study, they suggest it is the anterior band of the lateral collateral ligament complex and not just the lateral ulnar collateral ligament that confers stability in varus and external rotation. This approach allows excellent visualization of the entire lateral ligamentous avulsion (as it is in most cases), rather than the LUCL individually. This may facilitate accurate repair of the entire lateral collateral ligament complex. This, in turn, may aid stability, precluding the need for a medial approach and guarding against a ‘drop sign’.
It must be acknowledged that the size of our present study is small and any postulations would require cadaveric testing as well as further clinical research. In addition, it is a radiographic study. Although none of the cases have required further surgery nor complained of instability symptoms, we have not assessed the functional outcomes. With that in mind, however, it calls into question the assertion that the drop sign occurs secondary to the peripheral nerve block. In addition, it may be that the visualization afforded by this approach allows a more accurate repair of the lateral structures of the elbow with improved elbow stability manifesting as an absence of the drop sign.
Conclusions
TTIE is a serious injury which can predispose to instability and arthritis even when treated surgically. It has been postulated that a ‘drop sign’ postoperatively infers instability of the elbow joint. None of our patient cohort had an intraoperative ‘drop sign’ after standardized stabilization for a TTIE injury using a modified Boyd approach. We suggest that the approach used allows better visualization of the lateral structures for repair and that it confers excellent stability to the elbow joint.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Ethical approval was granted by the Clinical Research Ethics Committee (CREC) of the Cork Teaching Hospitals (CREC review reference no: ECM 4 (a) 05/05/2020).
References
- 1.Coonrad R.W., Roush T.F., Major N.M., Basamania C.J. The drop sign, a radiographic warning sign of elbow instability. J Shoulder Elbow Surg. 2005;14:312–317. doi: 10.1016/j.jse.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Duckworth A.D., Kulijdian A., McKee M.D., Ring D. Residual subluxation of the elbow after dislocation or fracture-dislocation: treatment with active elbow exercises and avoidance of varus stress. J Shoulder Elbow Surg. 2008;17:276–280. doi: 10.1016/j.jse.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 3.Hotchkiss R.N. In: 4th ed. Rockwood C.A. Jr., Green D.P., Bucholz R.W., Heckman J.D., editors. vol 1. Lippincott-Raven; Philadelphia: 1996. Fractures and dislocations of the elbow; pp. 929–1024. (Rockwood and Green’s fractures in adults). [Google Scholar]
- 4.Mathew P.K., Athwal G.S., King G.J.W. Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg. 2009;17:137–151. doi: 10.5435/00124635-200903000-00003. [DOI] [PubMed] [Google Scholar]
- 5.O’Driscoll S.W., Morrey B.F., Korinek S., An K.N. Elbow subluxation and dislocation: a spectrum of instability. Clin Orthop. 1992;280:186–197. [PubMed] [Google Scholar]
- 6.O’Driscoll S.W., Bell D.F., Morrey B.F. Posterolateral rotary instability of the elbow. J Bone Joint Surg Am. 1991;73:440–446. [PubMed] [Google Scholar]
- 7.Papatheodorou L.K., Rubright J.H., Heim K.A., Weiser R.W., Sotereanos D.G. Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop Relat Res. 2014;472:2084–2091. doi: 10.1007/s11999-014-3471-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pipicelli J.G., Chinchalkar S.J., Grewal R., King G.J.W. Therapeutic implications of the radiographic “drop sign” following elbow dislocation. J Hand Ther. 2012;25:346–353. doi: 10.1016/j.jht.2012.03.003. quiz 354. [DOI] [PubMed] [Google Scholar]
- 9.Perez E.A. In: 13th Edition. Azar F., Beaty J., Canale S., editors. Vol. II. Elsevier; Philadelphia: 2017. Fractures of the shoulder, arm, and forearm; p. 2976. (Campbell’s Operative Orthopaedics). Chapter 57. [Google Scholar]
- 10.Rhyou I.H., Lim K.S., Kim K.C., Lee J.H., Ahn K.B., Moon S.C. Drop sign of the elbow joint after surgical stabilization of an unstable simple posterolateral dislocation: natural course and contributing factors. J Shoulder Elbow Surg. 2015;24:1081–1089. doi: 10.1016/j.jse.2015.01.018. [DOI] [PubMed] [Google Scholar]
- 11.Ring D., Jupiter J.B., Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 2002;84:547–551. doi: 10.2106/00004623-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Robinson P.M., Li Martin K.-H., Dattani R., Van Rensburg L. The Boyd interval: a modification for use in the management of elbow trauma. Tech Hand Up Extrem Surg. 2016;20:37–41. doi: 10.1097/BTH.0000000000000112. [DOI] [PubMed] [Google Scholar]
- 13.Seki A., Olsen B.S., Jensen S.L., Eygendaal D., Sojbjerg J.O. Functional anatomy of the lateral collateral ligament complex of the elbow: Configuration of Y and its role. J Shoulder Elbow Surg. 2002;11:53–59. doi: 10.1067/mse.2002.119389. [DOI] [PubMed] [Google Scholar]
- 14.Zhang D., Tarabochia M., Janssen S., Ring D., Chen N. Risk of subluxation or dislocation after operative treatment of terrible triad injuries. J Orthop Trauma. 2016;30:660–663. doi: 10.1097/BOT.0000000000000674. [DOI] [PubMed] [Google Scholar]