Abstract
Background
Formal physical therapy (PT) traditionally has been a critical part of postoperative recovery, but recently, because of cost containment, coverage of PT has become limited. Alternatives to formal PT have been proposed, including telerehabilitation, internet-based PT (IBPT), and home-based physician-guided PT. The purpose of this study was to understand patient perceptions of PT, the benefits, perception of improvements, access to PT, and alternative forms of PT after shoulder surgery.
Methods
Eighty patients who underwent orthopedic shoulder surgery were anonymously surveyed at one institution. Demographics, PT access, number of PT sessions, insurance, copayment, patients’ perceptions of improvement, and their opinion about IBPT were collected. Answers were designed using Likert-scale or open-ended questions. Descriptive statistics were used to report survey data. Analyses were performed based on demographic variables using independent t-test, chi-square tests, and analysis of variance.
Results
Patients attended an average of 16.3 ± 13.8 PT sessions, with 65% ± 32.2 attributing average improvement to their sessions. Average copay was $18 ± 20.8 per session, which 56.1% agreed was reasonable. Almost all patients (94.8%) agreed their therapist took time to educate them. Half (52.5%) disagreed that successful PT could be achieved by IBPT, and 68.6% of patients responded they would not consider using IBPT even after a few in-person sessions.
Conclusion
Patients have a positive perception of their therapist, cost, number of sessions, and utility of PT to impact improvements after orthopedic shoulder surgery. For IBPT to be a viable alternative, it should involve close engagement of a physical therapist given patients’ perceptions of PT.
Keywords: Physical therapy, Shoulder surgery, Internet-based physical therapy, Patient perception, Survey
The use of physical therapy (PT) had been considered a critical part of the recovery after shoulder surgery. Many studies have demonstrated that PT helps guide patients through the postoperative recovery period, speeding up recovery and improving final functional outcomes.4,8,17,19,23,26 In addition, PT had also demonstrated effectiveness in the literature as a way to avoid surgery in the majority (75%) of atraumatic full-thickness rotator cuff tears.16
Even with its proven effectiveness, over the past decades, there have been substantial changes in insurance coverage of PT, even postoperatively. As health care costs rise exponentially, the trend has been for insurance companies to limit the number of formal PT sessions allotted to patients or increase costs to patients through higher copays. Restrictions on the utilization of PT sessions, limitations on location, and high copays can pose a significant barrier for patient access to PT, thus preventing optimal treatment and outcomes.3,6,7,13,15,18,22 The impact of insurance providers alone is concerning given that studies have shown a higher rate of utilization of PT for patients with private insurance than for Medicare patients after shoulder surgery.12,28 In addition, among Medicare beneficiaries, patients who had a postsurgical shoulder condition showed to be a strong predictor for a higher utilization rate of PT visits compared with lumbar, knee, and cervical conditions.11 Moreover, shoulder patients were more likely to result in an improved outcome after PT use, further highlighting the importance of unrestricted access to PT in this subpopulation.11
Formal PT has traditionally been considered essential after complex orthopedic surgeries like shoulder surgery, but recently, because of the environment of cost containment in the health care system, alternatives for formal PT have been proposed such as telerehabilitation and internet- or virtual-based PT.1,9,13,21,25 In addition, it has been proposed that a home-based physician-guided therapy program can provide similar results with lower costs, thus challenging the need for formal PT after total shoulder arthroplasty.20
As access is threatened and alternatives to formal PT are proposed, we need to better understand the patient’s perception, outcomes, and utilization of this important resource. Currently, no research has been conducted assessing patient perceptions of PT after orthopedic surgery The purpose of this study was to survey patients to understand access to PT, effectiveness of PT, perception of improvements from PT, and alternative forms of PT after shoulder surgery.
Methods
This study was an anonymous survey of patients who presented to the orthopedic surgery clinic after shoulder surgery. The survey was conducted in a single, urban, academic institution between 2018 and 2019 and was institutional review board approved. The questionnaire consisted of multiple-choice structured and open-ended questions (Appendix I). Patients included were seen in the orthopedic surgery clinic and underwent shoulder surgery.
Surveys were collected from patients who had autonomy and agreed to complete an anonymous questionnaire by themselves or with the assistance of a research team member. The survey was composed of 18 questions grouped into 4 sections: The first section collected demographic information including gender, age, race, and ethnicity. The second section assessed patient access, coverage, and utilization of PT. The questions evaluated the number of PT sessions before and after surgery, location PT was performed (whether at home, in a rehabilitation center, or both), health insurance coverage or limitations, and number of extra sessions. Patients were asked whether they were referred to PT and which provider referred them. In the third section, perception questions asked about alternatives to PT such as the internet-based PT programs. The fourth section assessed patients' overall experience with PT. Patients were asked to report a subjective percent of improvement (0%-100%) gained from PT. They were also asked whether the amount of copayment, number of covered sessions, and travel distance were reasonable. The survey also asked patients if the therapists took time to educate them about their treatment plan. A section for any additional comments was included at the end of the survey.
Statistical analysis
Descriptive statistics were reported using a 5-point Likert scale for the multiple-choice questions and open-ended questions, and numerical values were reported with regard to range, average, and standard deviation. Analyses performed included independent t-test, analysis of variance, and chi-square test with an alpha of 0.05. All analyses were performed using SPSS Software (Version 24.0; IBM, Armonk, NY, USA).
Results
Eighty patients completed surveys collected on a Redcap database with an almost equitable distribution of sex (54.4% men and 45.6% women [P = .43]). All completed questions were analyzed. The majority (90.8%) of the cohort was aged 45 years or above, and a majority (66.2%) of patients identified as Caucasian. Only 36 patients answered the question regarding their ethnicity, with a majority (68.6%) of the cohort reporting non-Hispanic and 31.4% reporting Hispanic (Table I).
Table I.
Patient demographic information (n = 80).
| Demographic | Categories | Distribution and count | P value |
|---|---|---|---|
| Sex, n | Male | 54.4% (n = 43) | P = .43 |
| Female | 45.6% (n = 36) | ||
| Age, yr | 18-24 | 2.6% (n = 2) | P < .01∗ |
| 25-34 | 2.6% (n = 2) | ||
| 35-44 | 4.0% (n = 3) | ||
| 45-54 | 18.4% (n = 14) | ||
| 55-64 | 26.3% (n = 20) | ||
| 65-74 | 22.4% (n = 17) | ||
| 75 or older | 23.7% (n = 18) | ||
| Race | Caucasian | 66.2% (n = 51) | P < .01∗ |
| Hispanic/Latino/Spanish | 18.2% (n = 14) | ||
| Black/African American | 13.0% (n = 10) | ||
| American Indian/Alaskan | 1.3% (n = 1) | ||
| Native Asian | 0% (n = 0) | ||
| Native Hawaiian/Other Pacific Islander | 1.3% (n = 1) | ||
| Other | 0% (n = 0) | ||
| Ethnicity | Hispanic or Latino | 31.4% (n = 11) | P = .019∗ |
| Not Hispanic or Latino | 68.6% (n = 25) |
Table I describes the patient demographic information of 80 patients. This includes sex, age, race, and ethnicity. Significant difference in demographics was analyzed and represented by a “∗” if statistically significant. Categories, distribution, count, and P-value for each demographic are described in the table.
Statistically significant.
There were significantly more PT sessions after surgery with an average of 10.0 ± 10.3 sessions compared with 3.4 ± 8.4 sessions before surgery (Figure 1). The total average number of sessions was 16.3 ± 13.8 sessions. Overall, the PT sessions for 20% of the patients were performed in both rehab centers and at home, 18.6% were performed just at home, and a majority of 61.4% were just in the rehab centers.
Figure 1.
PT sessions before surgery in comparison with after surgery. There is a significantly higher average of 10.0 ± 10.3 PT sessions after surgery than 3.4 ± 8.4 PT sessions before surgery. The “∗” shows that there is a significant difference with a P-value less than 0.05 (P = .0028). The orange column represents average sessions after surgery, and the blue column represents average sessions before surgery. The bars and caps over each column represent the standard deviation visually of each average. PT, physical therapy.
In terms of health care insurance coverage for PT, 64.4% of patients had private or Medicare with supplemental private medical insurance, with 95.9% reporting that their therapy was covered by insurance. Of the patients who had PT coverage, their copayment ranged from $0 to $100 with an average of $18 ± 20.8 per session. In addition, most patients (55%) were unsure if the number of sessions covered by their insurance was limited. For those who knew the number of covered PT sessions by their insurance, this was reported to be on average 19 ± 6.4 sessions (range = 7-35) for the cohort. There was no significant difference between the number of PT sessions covered between the different insurance types (P = .506). When asked if the participants exceeded the number of allotted PT sessions, 5.6% reported they had to pay additional funds, 49.3% reported they did not, 21.1% were not sure, and 23.9% stated they could request additional sessions. Regarding coverage of services provided by PT, most patients (58.7%) were unsure if it was covered, whereas 40% reported that their insurance covered all services, and 1.3% reported services were not covered by their insurance.
When patients were asked whether successful PT may be achieved with internet-based PT (IBPT), 52.5% of patients disagreed, 28.8% of patients agreed, and 18.8% of patients were undecided (Figure 2). Approximately 17% of patients responded that they prefer to start IBPT after a few sessions with a physical therapist (Figure 3). As for accessing IBPT programs through different modalities, 19.4% preferred access from a smartphone app, 19.4% preferred access from a desktop website, and 61.1% had no preference.
Figure 2.
Patient perceived success of physical therapy achieved using IBPT. The distribution of responses to whether successful physical therapy may be achieved using internet-based physical therapy (IBPT) is analyzed between responses that agreed, were undecided, or disagreed. Responses are represented as different colors on the pie graph.
Figure 3.
Patient preference for IBPT. The distribution was found on patients' responses to whether they prefer to start internet-based physical therapy (IBPT) after a few sessions with a physical therapist. Responses are represented as different colors on the pie graph including strongly agree, agree, undecided, disagree, and strongly disagree.
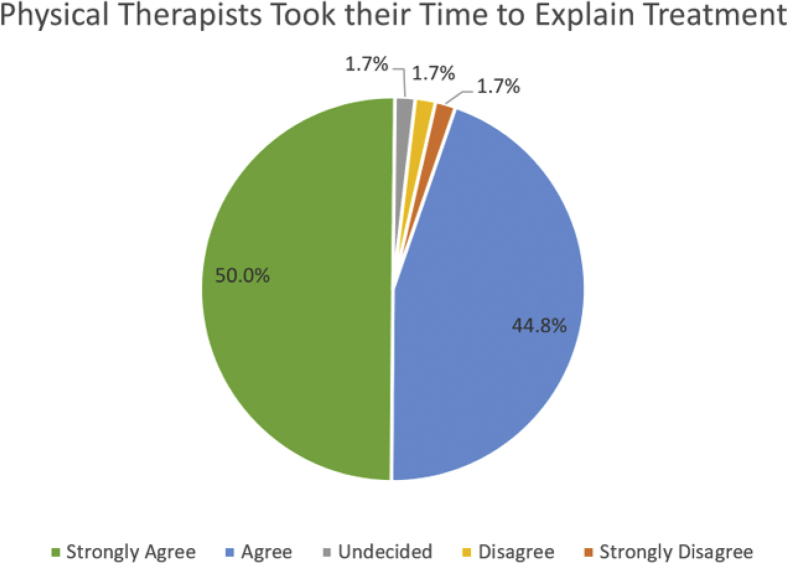
Regarding improvement in their conditions, patients attributed 65.0% ± 32.2 to their PT sessions. There was no significant difference in the location of PT sessions attended (home, rehab center, or both) and percentage improvement from PT sessions (P = .505). With regard to cost, 56.1% of patients agreed/strongly agreed that the copayments paid toward PT were reasonable. About half (50.3%) agreed/strongly agreed that the number of PT sessions covered by insurance was reasonable. Finally, when patients were asked if physical therapists took their time to educate them on their treatment plan, an overwhelming majority of 94.8% of patients agreed (50% strongly agreed and 44.8% agreed) (Figure 4).
Figure 4.
Perception of patients of whether physical therapists took their time to explain treatment. The distribution represents patients’ perception of whether physical therapists took their time to explain treatment. Responses represented as different colors in the pie graph to include strongly agree, agree, undecided, disagree, and strongly disagree.
Discussion
PT is an important component of recovery after shoulder surgery. Whether it is home-based, physician-guided, or formal outpatient PT, studies have demonstrated that PT helps guide patients through the recovery period, speeding up their recovery and improving their final functional gains and outcomes.1,2,5,14,15,20,21,25,27 In a value-based health care system, PT seems to be important because it is valued by patients. Our data suggested that patients have an overwhelmingly positive perception of their physical therapists, and they feel PT is important for improvements and outcomes. Because outcomes are an important value in a patient-centered health care system, we need to make sure we continue to provide comparable alternatives to this resource.
As cost containment and the pandemic remain a priority in health care, alternatives to formal PT have been proposed. Telerehabilitation and IBPT have been proven to be effective alternatives to formal PT. Randomized controlled trials have found no differences when comparing telerehabilitation and IBPT with conventional PT in the treatment of knee osteoarthritis and after total knee arthroplasty, respectively.1,24 However, our data emphasize that we need to be careful on how we institutionalize the use of IBPT because not all patients will be open to this as a viable option even though it increases access. Our patients also did not find that travel was a burden to access to PT, which aligns with a study by Mattson which concluded that distance and transportation variables were not found to significantly influence the total number of routine or chronic care trips made.18
Our results showed that patients perceive clear benefits from their relationship with their therapists. Whether it is home-based or formal PT, it seems that for those new PT modalities to be a viable alternative to traditional PT, they will require integration and close engagement of a physical therapist. Our data can be an avenue for future projects given that patients perceive that their relationship with the therapist adds value, regardless of copayment barriers and coverage limitations. Future efforts should be focused on integrating telerehabilitation and outpatient PT experiences into home-based PT to promote cost containment. However, our data find that patients have a perceived preference toward having PT sessions at a rehab center as well as perceiving formal PT over IBPT programs.1,10,24 Thus, education for patients on the similar efficacy of formal PT and IBPT programs should be provided.
We acknowledge several limitations in our study. First, this was a survey study which relies on full patient participation and complete answers for all questions, which did not occur in some cases. The lowest response rate was surrounding copayment and coverage questions, in which missed answers most commonly were due to patient education of their own PT coverage. We still felt that our results reflected the spectrum of insurance types and patients commonly seen in an orthopedic surgery clinic. Clearly larger cohort studies in various locations or health care systems are still needed to fully understand application of our results on a national level. Second, our sample was mainly composed of patients who had undergone orthopedic surgery, and consequently, these patients had more complex pathology which makes PT more necessary. Finally, given a single location and hospital system included in our study, further research is needed to fully characterize both a younger cohort and geographic variations that would be seen in PT coverage and usage. Future studies should analyze patient perception within different age groups, ethnicities, urban/rural settings, and geographic regions.
Conclusion
Patients have a positive perception of their therapist, the number of sessions, and utility of PT to impact improvements after shoulder surgery. In a value-based health care system, PT seems to be important because it is valued by patients. As cost containment remains a priority in health care, it seems that for IBPT programs to be a viable alternative to traditional PT, IBPT will require integration and close engagement of a physical therapist, given patients’ perceptions and values on the impact of formal PT.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: Vani J. Sabesan receives research support from Orthofix, Inc. and Wright Medical Technology, Inc. The other authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
This study was performed under approval of the Cleveland Clinic Institutional Review Board (FLA 18-039).
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jseint.2021.11.014.
Supplementary data
References
- 1.Allen K.D., Arbeeva L., Callahan L.F., Golightly Y.M., Goode A.P., Heiderscheit B.C., et al. Physical therapy vs internet based exercise training for patients with knee osteoarthritis: results of a RCT. Heal Res Alliance. 2018;26:383–396. doi: 10.1016/j.joca.2017.12.008. Physical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arndt J., Clavert P., Mielcarek P., Bouchaib J., Meyer N., Kempf J.F. Immediate passive motion versus immobilization after endoscopic supraspinatus tendon repair: a prospective randomized study. Orthop Traumatol Surg Res. 2012;98:S131–S138. doi: 10.1016/j.otsr.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Arshi A., Kabir N., Cohen J.R., Lord E.L., Wang J.C., McAllister D.R., et al. Utilization and costs of postoperative physical therapy after rotator cuff repair: a comparison of privately insured and medicare patients. Arthroscopy. 2015;31:2392–2399.e1. doi: 10.1016/j.arthro.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 4.Boudreau S., Boudreau E.D., Higgins L.D., Wilcox R.B. Rehabilitation following reverse total shoulder arthroplasty. J Orthop Sports Phys Ther. 2007;37:734–741. doi: 10.2519/jospt.2007.2562. [DOI] [PubMed] [Google Scholar]
- 5.Chen L., Peng K., Zhang D., Peng J., Xing F., Xiang Z. Rehabilitation protocol after arthroscopic rotator cuff repair: early versus delayed motion. Int J Clin Exp Med. 2015;8:8329–8338. No doi. [PMC free article] [PubMed] [Google Scholar]
- 6.Civelek M., Lusis A.J. Systems genetics approaches to understand complex traits. Nat Rev Genet. 2014;15:34–48. doi: 10.1038/nrg3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dall T.M., Gallo P., Koenig L., Gu Q., Ruiz D. Modeling the indirect economic implications of musculoskeletal disorders and treatment. Cost Eff Resour Alloc. 2013;11:1–14. doi: 10.1186/1478-7547-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Denard P.J., Lädermann A. Immediate versus delayed passive range of motion following total shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25:1918–1924. doi: 10.1016/j.jse.2016.07.032. [DOI] [PubMed] [Google Scholar]
- 9.Eriksson L., Lindström B., Gard G., Lysholm J. Physiotherapy at a distance: a controlled study of rehabilitation at home after a shoulder joint operation. J Telemed Telecare. 2009;15:215–220. doi: 10.1258/jtt.2009.081003. [DOI] [PubMed] [Google Scholar]
- 10.Ferguson C.M., Harmer L., Seymour R.B., Ellington J.K., Bosse M. Does formal vs home-based physical therapy predict outcomes after ankle fracture or ankle fracture-dislocation? OTA Int. 2019;2:e039. doi: 10.1097/oi9.0000000000000039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fritz J.M., Hunter S.J., Tracy D.M., Brennan G.P. Utilization and clinical outcomes of outpatient physical therapy for Medicare beneficiaries with musculoskeletal conditions. Phys Ther. 2011;91:330–345. doi: 10.2522/ptj.20090290. [DOI] [PubMed] [Google Scholar]
- 12.Garzon-Serrano J., Ryan C., Waak K., Hirschberg R., Tully S., Bittner E.A., et al. Early mobilization in critically ill patients: patients’ mobilization level depends on health care provider’s profession. PM&R. 2011;3:307–313. doi: 10.1016/j.pmrj.2010.12.022. [DOI] [PubMed] [Google Scholar]
- 13.Hernon M.J., Hall A.M., O’Mahony J.F., Normand C., Hurley D.A. Systematic review of costs and effects of self-management interventions for chronic musculoskeletal pain: spotlight on analytic perspective and outcomes assessment. Phys Ther. 2017;97:998–1019. doi: 10.1093/ptj/pzx073. [DOI] [PubMed] [Google Scholar]
- 14.Houck D.A., Kraeutler M.J., Schuette H.B., McCarty E.C., Bravman J.T. Early versus delayed motion after rotator cuff repair: a systematic review of overlapping meta-analyses. Am J Sports Med. 2017;45:2911–2915. doi: 10.1177/0363546517692543. [DOI] [PubMed] [Google Scholar]
- 15.Hush J.M., Cameron K., Mackey M. Patient satisfaction with musculoskeletal physical therapy care: a systematic review. Phys Ther. 2011;91:25–36. doi: 10.2522/ptj.20100061. [DOI] [PubMed] [Google Scholar]
- 16.Kuhn J.E., Dunn W.R., Sanders R., An Q., Baumgarten K.M., Bishop J.Y., et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg. 2013;22:1371–1379. doi: 10.1016/j.jse.2013.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marinko L.N., Chacko J.M., Dalton D., Chacko C.C. The effectiveness of therapeutic exercise for painful shoulder conditions: a meta-analysis. J Shoulder Elbow Surg. 2011;20:1351–1359. doi: 10.1016/j.jse.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 18.Mattson J. Transportation, distance, and health care utilization for older adults in rural and small urban areas. Transp Res Rec. 2011:192–199. doi: 10.3141/2265-22. [DOI] [Google Scholar]
- 19.Morris P.E., Herridge M.S. Early intensive care unit mobility: future directions. Crit Care Clin. 2007;23:97–110. doi: 10.1016/j.ccc.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 20.Mulieri P.J., Holcomb J.O., Dunning P., Pliner M., Bogle R.K., Pupello D., et al. Is a formal physical therapy program necessary after total shoulder arthroplasty for osteoarthritis? J Shoulder Elbow Surg. 2010;19:570–579. doi: 10.1016/j.jse.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 21.Pignato M., Arbeeva L., Schwartz T.A., Callahan L.F., Cooke J., Golightly Y.M., et al. Level of participation in physical therapy or an internet-based exercise training program: associations with outcomes for patients with knee osteoarthritis. BMC Musculoskelet Disord. 2018;19:1–11. doi: 10.1186/s12891-018-2139-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roberson T.A., Bentley J.C., Griscom J.T., Kissenberth M.J., Tolan S.J., Hawkins R.J., et al. Outcomes of total shoulder arthroplasty in patients younger than 65 years: a systematic review. J Shoulder Elbow Surg. 2017;26:1298–1306. doi: 10.1016/j.jse.2016.12.069. [DOI] [PubMed] [Google Scholar]
- 23.Romano A.M., Oliva F., Nastrucci G., Casillo P., Di Giunta A., Susanna M., et al. Reverse shoulder arthroplasty patient personalized rehabilitation protocol. preliminary results according to prognostic groups. Muscles Ligaments Tendons J. 2017;7:263–270. doi: 10.32098/mltj.02.2017.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Russell T.G., Buttrum P., Wootton R., Jull G.A. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2011;93:113–120. doi: 10.2106/JBJS.I.01375. [DOI] [PubMed] [Google Scholar]
- 25.Saltzman B.M., Zuke W.A., Go B., Mascarenhas R., Verma N.N., Cole B.J., et al. Does early motion lead to a higher failure rate or better outcomes after arthroscopic rotator cuff repair? A systematic review of overlapping meta-analyses. J Shoulder Elbow Surg. 2017;26:1681–1691. doi: 10.1016/j.jse.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 26.Thigpen C.A., Shaffer M.A., Gaunt B.W., Leggin B.G., Williams G.R., Wilcox R.B. The American Society of Shoulder and Elbow Therapists’ consensus statement on rehabilitation following arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25:521–535. doi: 10.1016/j.jse.2015.12.018. [DOI] [PubMed] [Google Scholar]
- 27.Uesugi Y., Koyanagi J., Takagi K., Yamaguchi R., Hayashi S., Nishii T. Exercise therapy interventions in patients with hip osteoarthritis: comparison of the effects of DVD and website-based interventions. J Med Internet Res. 2018;20 doi: 10.2196/rehab.8251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wagner E.R., Solberg M.J., Higgins L.D. The utilization of formal physical therapy after shoulder arthroplasty. J Orthop Sports Phys Ther. 2018;48:856–863. doi: 10.11164/jjsps.8.2_255_5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.