Abstract
Background:
Rare soft-tissue tumors, termed desmoid fibromatosis (DF), are comprised proliferated spindle cell fibroblasts and myofibroblasts embedded in a prominent collagenous stroma. They can occur either sporadically, due to prior trauma or surgery, or may have a genetic component. Clinically, DF has a high infiltrative growth/ local recurrence rate, but does not metastasize.
Case Description:
A 58-year-old male underwent a C5-C7 laminectomy/instrumented fusion. Two years later, he presented with a large gross swelling on the right side of the neck. The lesion was removed and proved to histologically consist of DF. Within the first postoperative 12 months, tumor did not recur.
Conclusion:
Sporadic DF may follow trauma or prior surgery. Symptomatic tumors are treated by surgical en bloc resection (preferably R0). If lesions are inoperable, partially resected, or recur, different hormonal/ chemotherapeutic systematic treatment options are available (e.g., tamoxifen or tyrosine kinase inhibitors). In the future, better molecular understanding of DF likely offers additional therapeutic approaches (e.g., immune checkpoint inhibitors).
Keywords: Desmoid fibrosis, Soft-tissue tumor, Spine surgery

INTRODUCTION
Desmoid fibromatosis (DF) (also known as desmoid-type fibromatosis) is defined by the World Health Organization as a rare type of soft-tissue tumor that occurs with a frequency of 3–4 cases/ million per year. DF arises from fibroblasts/myofibroblasts of the muscle connective tissue, fascia, and aponeurosis and demonstrates infiltrative growth and a high local recurrence rate; however, they do not metastasize.[1,7] DF can be classified as extra-abdominal (trunk and limbs), located on the abdominal wall, or intra-abdominal. Sporadic DF often affects young adults between 35 and 40 years of age, with a clear female preponderance (i.e., during/after pregnancy or following trauma or surgery). Here, we present a 58-year-old male whose DF occurred 2 years after spine surgery.[7]
CASE DESCRIPTION
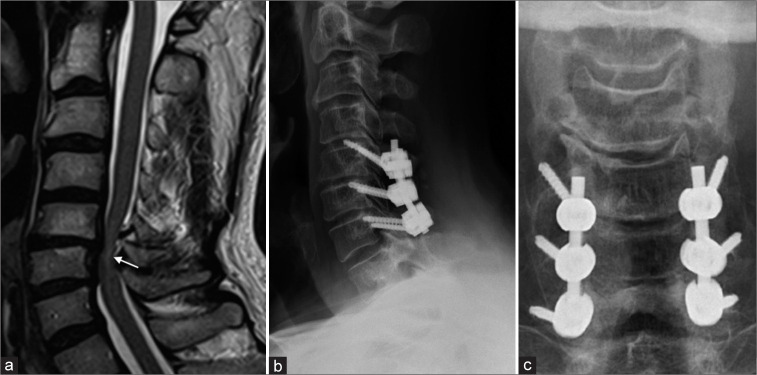
A 58-year-old male underwent a C5-C7 laminectomy/rod-screw-instrumented fusion for multilevel spondylotic cervical myelopathy [Figure 1].
Figure 1:
A sagittal T2-weighted magnetic resonance imaging (a) of cervical spondylotic myelopathy patient shows the change of spinal cord signal intensity (white arrow). Postoperative cervical spinal X-ray showing lateral (b) and anteroposterior (c) view after decompressive cervical laminectomy and C4-6 lateral mass fusion.
Two years postoperatively, the patient newly presented with a progressive right-sided painful swelling of the posterolateral neck; the lesion was fixed to the skin/deep neck structures. The MR revealed a 5.2 × 4.5 × 3.7 cm mass; the lesion on the T1 study was iso-hypointense, on the T2-weighted image showed slight hyperintensity, and inhomogeneous enhancement with contrast [Figure 2].
Figure 2:
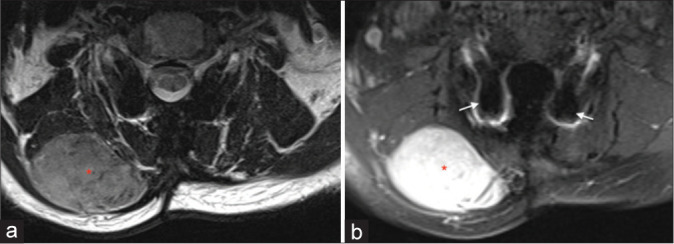
Axial T2-weighted (a) and contrast-enhanced axial T1-weighted (b) magnetic resonance imaging of the neck showing tumor mass (red asterix) anatomically located between the trapezius muscle and the splenius capitis muscle. Metal-related artifacts in MRI (b) caused by lateral mass screws (white arrow).
Surgery for DF
The patient underwent surgical en bloc resection of the mass that was located between the trapezius and splenius capitis muscles; it was well demarcated from the surrounding tissues. The 24 h postoperative MR confirmed complete tumor resection.
Histology and Immunohistochemistry of DF
Histologically, the DF showed spindle cell fibroblast proliferation embedded in a collagenous stroma with rim infiltration of the skeletal muscle. Immunohistochemistry showed a cytoplasmic and nuclear expression of β-catenin [Figure 3]. Molecular pathology revealed a CTNNB1 mutation (c.121A>G; p.T41A) typical for DF. A second histological examination by a national reference center for soft-tissue tumors confirmed the diagnosis of a DF.
Figure 3:
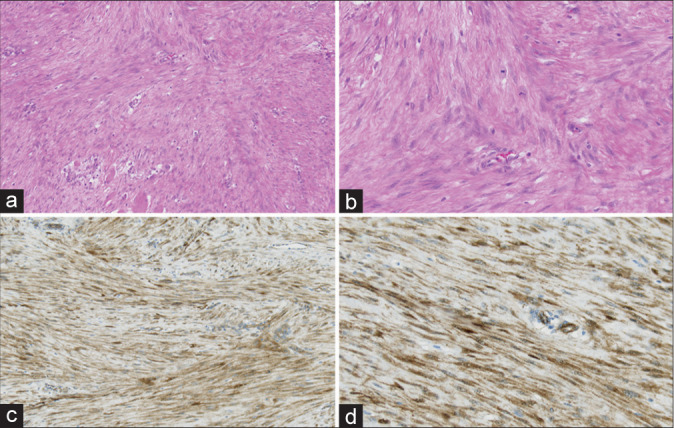
(a) Histopathologic specimen demonstrating spindle cell fibroblast proliferates embedded in a collagenous stroma network with rim infiltration of skeletal muscle (H&E, ×10) and (b) nonatypical mitotic figures in desmoid fibromatosis (H&E, ×20). (c) (×10) and (d) (×20): cytoplasmic and nuclear expression of β-catenin, which is typical for desmoid fibromatosis.
Twelve-month postoperative course
At 6 months and 12 postoperative months, the patient was clinically asymptomatic. Further, the 12-month postoperative magnetic resonance imaging (MRI) showed no tumor recurrence [Figure 4].
Figure 4:
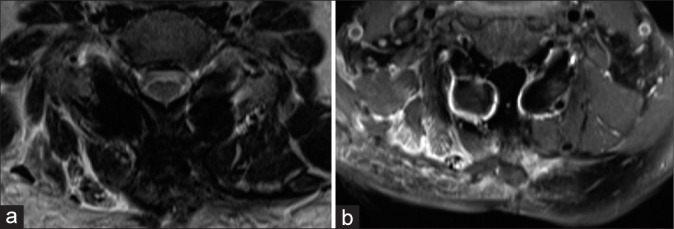
Axial T2-weighted (a) and contrast-enhanced axial T1-weighted (b) magnetic resonance imaging of the neck showed no evidence of tumor recurrence (12 months follow-up).
DISCUSSION
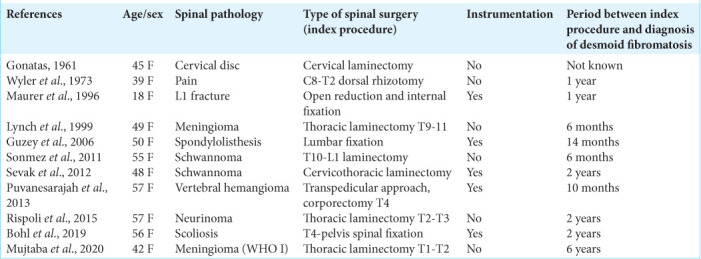
The occurrence of DF after spinal surgery has been reported sporadically and typically ranges from 10 months to 7 postoperative years[2,5,6,9-16] [Table 1]. In our case, a DF developed 23 months after dorsal surgery of the cervical spine. MRI is the study of choice to assess the size, location, and type of soft-tissue mass consistent with DF low signal intensity in T2-weighted series and moderate contrast uptake is typical for fibrotic and collagenous tumor parts. However, MRI signal patterns can change during the course of the disease.[4] The histopathological examination of DF, obtained either by surgery or needle biopsy, typically shows proliferated spindle cell fibroblasts and myofibroblasts embedded in a prominent collagenous stroma and vascular network. Further, additional immunohistochemical and molecular pathological tests are crucial for diagnostic accuracy. A locally displacing growth can lead to different symptoms by compression of the surrounding tissue. For technical, functional, or cosmetic reasons, this surgical goal (R0) is sometimes not achievable and an R1 resection is then acceptable. The evidence of adjuvant radiotherapy after R1 resection is low and can only be recommended with limitations.[3] Recurrent lesions may be surgically excised, although an alternative is radiotherapy (i.e., dose of 56 Gy distributed over 28 daily single doses a 2 Gy leads to local growth control in inoperable tumors).[8] Systemic therapy options should be used in particular if there is aggressive tumor growth which cannot be treated by surgery due to its anatomical location or if early recurrence of tumor growth occurs after surgery.[3] There are also chemotherapeutic and immunotherapeutic options for treating DF. Nevertheless, there is no standardized protocol for treating DF. Therefore, their diagnosis/treatment must be carefully assessed on a case-by-case basis.
Table 1:
Postoperative development of desmoid tumor after previous spinal surgery (n=11).
CONCLUSION
Here, we presented a 58-year-old male who, 2 years following a C5-C7 laminectomy/fusion, presented with a right posterolateral neck mass that was diagnosed as a DF. Following gross total en bloc excision, the lesion did not recur within 12 postoperative months.
Footnotes
How to cite this article: Schlag H, Neuhoff J, Castein J, Hoffmann C, Kandziora F. Sporadic desmoid fibromatosis of the neck after dorsal spondylodesis of the cervical spine. Surg Neurol Int 2022;13:64.
Contributor Information
Holger Schlag, Email: h.schlag@gmx.net.
Jonathan Neuhoff, Email: jonathan.neuhoff@bgu-frankfurt.de.
Jens Castein, Email: jens.castein@bgu-frankfurt.de.
Chirstoph Hoffmann, Email: christoph.hoffman@bgu-frankfurt.de.
Frank Kandziora, Email: frank.kandziora@bgu-frankfurt.de.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bauer BM, Williams NL, Zuckerman LM. Development of multifocal extra-abdominal desmoid fibromatosis after surgical resection. Clin Case Rep. 2019;7:2515–9. doi: 10.1002/ccr3.2551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bohl MA, Leveque JC, Bayles S, Sethi R. Postoperative development of desmoid tumor after surgical correction of adult spinal deformity: Case report and review of literature. World Neurosurg. 2019;128:4–10. doi: 10.1016/j.wneu.2019.04.201. [DOI] [PubMed] [Google Scholar]
- 3.Desmoid Tumor Working G. The management of desmoid tumours: A joint global consensus-based guideline approach for adult and paediatric patients. Eur J Cancer. 2020;127:96–107. doi: 10.1016/j.ejca.2019.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Dinauer PA, Brixey CJ, Moncur JT, Fanburg-Smith JC, Murphey MD. Pathologic and MR imaging features of benign fibrous soft-tissue tumors in adults. Radiographics. 2007;27:173–87. doi: 10.1148/rg.271065065. [DOI] [PubMed] [Google Scholar]
- 5.Gonatas NK. Extra-abdominal desmoid tumors. Report of six cases. Arch Pathol. 1961;71:214–21. [PubMed] [Google Scholar]
- 6.Guzey FK, Emel E, Bas NS, Ozkan N, Turgut H, Sel B. Aggressive postoperative lumbar fibromatosis after the placement of instrumentation for treatment of spondylolisthesis. Case report. J Neurosurg Spine. 2006;4:338–41. doi: 10.3171/spi.2006.4.4.338. [DOI] [PubMed] [Google Scholar]
- 7.Kasper B, Baumgarten C, Bonvalot S, Haas R, Haller F, Hohenberger P, et al. Management of sporadic desmoid-type fibromatosis: A European consensus approach based on patients’ and professionals’ expertise-a sarcoma patients EuroNet and European organisation for research and treatment of cancer/soft tissue and bone sarcoma group initiative. Eur J Cancer. 2015;51:127–36. doi: 10.1016/j.ejca.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Keus RB, Nout RA, Blay JY, de Jong JM, Hennig I, Saran F, et al. Results of a phase II pilot study of moderate dose radiotherapy for inoperable desmoid-type fibromatosis-an EORTC STBSG and ROG study (EORTC 62991-22998) Ann Oncol. 2013;24:2672–6. doi: 10.1093/annonc/mdt254. [DOI] [PubMed] [Google Scholar]
- 9.Lynch JJ, Parvizi J, Scheithauer BW, Krauss WE. Development of postoperative fibromatosis after resection of an intraspinal meningioma. Case report. J Neurosurg. 1999;90(Suppl 1):121–4. doi: 10.3171/spi.1999.90.1.0121. [DOI] [PubMed] [Google Scholar]
- 10.Maurer F, Horst F, Pfannenberg C, Wehrmann M. Multifocal extra-abdominal desmoid tumor-diagnostic and therapeutic problems. Arch Orthop Trauma Surg. 1996;115:359–62. doi: 10.1007/BF00420333. [DOI] [PubMed] [Google Scholar]
- 11.Mujtaba B, Call C, Rowland F, Spear RP, Amini B, Valenzuela R, et al. Desmoid fibromatosis following surgical resection of spinal meningioma. Radiol Case Rep. 2020;15:697–701. doi: 10.1016/j.radcr.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puvanesarajah V, Lina IA, Liauw JA, Hsu W, Burger PC, Witham TF. Desmoid tumor formation following posterior spinal instrumentation placement. Evid Based Spine Care J. 2013;4:137–42. doi: 10.1055/s-0033-1357356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rispoli R, di Chirico A, Tinella E, Peciarolo A, Ascani S, Caputo N, et al. Desmoid tumor following dorsal laminectomy: Case report. Clin Case Rep Rev. 2016;1:251–2. [Google Scholar]
- 14.Sevak S, Blount AL, Cottingham S, DeLano M, Woude DL, Stevenson J, et al. Fibromatosis of the cervical region following laminectomy: A case report and literature review. Spine (Phila Pa 1976) 2012;37:E456–9. doi: 10.1097/BRS.0b013e318232922a. [DOI] [PubMed] [Google Scholar]
- 15.Sonmez E, Altinors N, Gulsen S, Ozen O. Extraabdominal desmoid tumor appearing following resection of thoracolumbar schwannoma. Turk Neurosurg. 2011;21:246–8. doi: 10.5137/1019-5149.JTN.2750-09.2. [DOI] [PubMed] [Google Scholar]
- 16.Wyler AR, Harris AB. Recurrent desmoid tumor following cervical laminectomy. Case report. J Neurosurg. 1973;39:114–6. doi: 10.3171/jns.1973.39.1.0114. [DOI] [PubMed] [Google Scholar]