Abstract
Background:
Spinal extradural arachnoid cysts (SEDACs) are rare and are variously attributed to congenital, traumatic, or inflammatory etiologies. Here, we report a 70-year-old male who presented with a T11-T12 SEDAC and an incidental craniovertebral junction (CVJ) meningioma.
Case Description:
A 70-year-old male presented with progressive bilateral lower limb weakness and paresthesias. The thoracic MRI identified an extradural arachnoid cystic lesion at the T11-T12 level. In addition, the brain/ cervical MR documented an incidental meningioma at the CVJ. The patient underwent T11-T12 laminectomy for fenestration/removal of the extradural arachnoid cyst resulting in immediate cord decompression and neurological recovery. The histologic examination was consistent with a SEDAC who underwent successful resection of the SEDAC that resulted in symptom resolution.
Conclusion:
We presented a 71-year-old male with a thoracic SEDAC and an incidental CVJ meningioma, where resection of the SEDAC resulted in symptom resolution.
Keywords: Arachnoid cyst, Cyst resection, Extradural cyst, Thoracic spine

INTRODUCTION
Spinal extradural arachnoid cysts (SEDACs) account for <1% of all spinal lesions. They are classified as a subtype of spinal arachnoid cysts that most frequently occur in the mid-to-lower thoracic levels.[8] They typically develop when the arachnoid membrane herniates through the dura.
Neurological symptoms of SEDACs that range from radicular pain to compressive myelopathy reflect the level, size, and location of the SEDAC.[2] Here, we report a 71-year-old male who was treated for myelopathy attributed to a T11-T12 SEDAC; his symptoms/signs resolved following successful resection/marsupialization of the SEDAC. Notably, the incidental craniovertebral junction (CVJ) meningioma, unrelated to the SEDAC, was later treated with stereotactic radiosurgery.
CASE REPORT
Clinical and radiographic presentation
A 70-year-old male patient presented with 2 years but 3 weeks of marked progression of lower limb weakness/paresthesias associated with a paraparesis/and lower extremity sensory changes. The thoracic MR showed a T11-T12 CSF-like extradural compressive lesion considered to represent an extradural arachnoid cyst [Figure 1a-d]. The brain/cervical MRI documented an incidental CVJ meningioma.
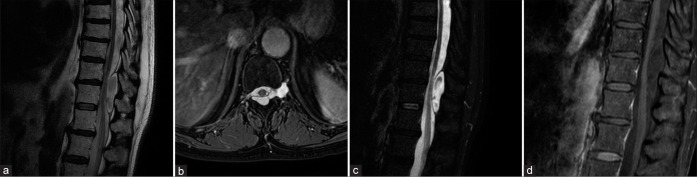
Figure 1:
MRI images at T2-WI sagittal (a) and axial (b) planes, sagittal STIR (c), and gadolinium-enhanced T1-WI (d) showing a CSF-like signal at the T11-T12 levels and an altered thoracic spine signal intensity area.
Surgical management/postoperative course/pathology
A T11-T12 laminectomy was performed, and the extradural arachnoid cyst was fenestrated, marsupialized, and removed en bloc utilizing intraoperative neurophysiological monitoring without any changes being noted [Figure 2a]. A microsurgical repair of the left T11-T12 paramedian/ foraminal dural defect (i.e., through which the arachnoid had extruded into the epidural space) was repaired/sutured using nonabsorbable Prolene sutures, collagen sponge, and dural sealant [Figure 2b and c]. The histological examination confirmed the diagnosis of a SEDAC. Immediately postoperatively, the patient’s gait progressively improved. Three months later, the follow-up thoracic MRI showed no residual cord compression and full resolution of the extradural arachnoid cyst [Figure 3a-c]. The incidental meningioma was later treated with stereotactic radiosurgery.
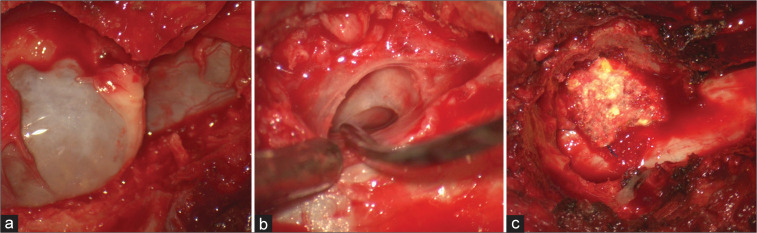
Figure 2:
Intraoperative findings after T11-T12 laminectomy: (a) identification of an extradural cystic lesion and below dural sac, (b) left T11-T12 paramedian dural defect with extension to the neuroforamen detected after cystic fenestration and en bloc removal, (c) microsurgical repair of the dural defect using nonabsorbable Prolene suture, collagen sponge and dural sealant have been performed.
Figure 3:
Postoperative MRI images at sagittal STIR (a), and T2-WI sagittal (b) and axial (c) planes showing spinal cord decompression and excluding further development of arachnoid cysts or CSF leaks.
DISCUSSION
Classification of spinal arachnoid cysts
Spinal arachnoid cysts are usually located either dorsal or ventral to the spinal cord and are mostly observed in adolescents and middle-aged men.[2] Nabors divided SEDACs into three types: extradural cysts without spinal nerve root fibers (Type I), extradural cysts with spinal nerve root fibers (Type II), and intradural cysts (Type III). According to this classification, our case is characterized as a Type I SEDAC.[6] The etiology of spinal arachnoid cysts involves congenital, traumatic, or inflammatory mechanisms.[1] The following features likely play important roles in their progressive enlargement; pulsatile CSF dynamics, differential osmotic pressures between the subarachnoid space and cyst, and the one-way valve-like mechanism that develops at the narrow communication between the cyst and dural sac.[1,2] Symptoms reflect the level, size, and site of cord/root compression.[2,5] Signs may vary from radiculopathy to major myelopathy and typically include back/leg pain, leg weakness plus urinary incontinence, and sexual dysfunction.[4,8] Diagnostic neuroimaging should typically include both CT and MRI studies to differentiate these lesions from cystic tumors (e.g., cystic meningioma) and/or rare spinal infections.[3,7] The treatment most often involves surgical decompression with obliteration of the communication between the subarachnoid space and the extradural cyst followed by cyst resection.
CONCLUSION
Here, we presented a 71-year-old male with a T11-T12 extradural arachnoid cyst who underwent successful occlusion of the communication between the subarachnoid space and cyst, followed by cyst excision, and primary dural repair without sequelae.
Footnotes
How to cite this article: Marrone S, Kharbat AF, Palmisciano P, Umana GE, Haider AS, Iacopino DG, et al. Thoracic spinal extradural arachnoid cyst: A case report and literature review. Surg Neurol Int 2022;13:55.
Contributor Information
Salvatore Marrone, Email: salvo.mr89@gmail.com.
Abdurrahman F. Kharbat, Email: ak.kharbat@yahoo.com.
Paolo Palmisciano, Email: paolo.palmisciano94@gmail.com.
Giuseppe Emmanuele Umana, Email: umana.nch@gmail.com.
Ali S. Haider, Email: aralam09@gmail.com.
Domenico Gerardo Iacopino, Email: gerardo.iacopino@gmail.com.
Giovanni Federico Nicoletti, Email: gfnicoletti@alice.it.
Gianluca Scalia, Email: gianluca.scalia@outlook.it.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cilluffo JM, Gomez MR, Reese DF, Onofrio BM, Miller RH. Idiopathic (“congenital”) spinal arachnoid diverticula. Clinical diagnosis and surgical results. Mayo Clin Proc. 1981;56:93–101. [PubMed] [Google Scholar]
- 2.Cloward RB. Congenital spinal extradural cysts: Case report with review of literature. Ann Surg. 1968;168:851–64. doi: 10.1097/00000658-196811000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Furnari M, Scalia G, Umana GE, Giuffrida M, Ponzo G, Garozzo SF, et al. Rare spondylodiscitis due to Mycobacterium mucogenicum. Surg Neurol Int. 2020;11:289. doi: 10.25259/SNI_525_2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee SW, Foo A, Tan CL, Tan T, Lwin S, Yeo TT, et al. Spinal extradural cyst: Case report and review of literature. World Neurosurg. 2018;116:343–6. doi: 10.1016/j.wneu.2018.05.199. [DOI] [PubMed] [Google Scholar]
- 5.Myles LM, Gupta N, Armstrong D, Rutka JT. Multiple extradural arachnoid cysts as a cause of spinal cord compression in a child. J Neurosurg Spine. 1999;91:116–20. doi: 10.3171/spi.1999.91.1.0116. [DOI] [PubMed] [Google Scholar]
- 6.Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI, et al. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg. 1988;68:366–77. doi: 10.3171/jns.1988.68.3.0366. [DOI] [PubMed] [Google Scholar]
- 7.Ponzo G, Umana GE, Giuffrida M, Furnari M, Nicoletti GF, Scalia G. Intramedullary craniovertebral junction metastasis leading to the diagnosis of underlying renal cell carcinoma. Surg Neurol Int. 2020;11:152. doi: 10.25259/SNI_259_2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woo JB, Son DW, Kang KT, Lee JS, Song GS, Sung SK, et al. Spinal extradural arachnoid cyst. Korean J Neurotrauma. 2016;12:185. doi: 10.13004/kjnt.2016.12.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]