Abstract
Nonbacterial thrombotic endocarditis (NBTE) is relatively rare, with an identification rate of 1.6% at autopsy, and is associated with malignancy and systemic lupus erythematosus. Further, bioprosthetic valve NBTE is extremely rare, with only a few reports in the literature. To ensure appropriate treatment, it is essential to differentiate between NBTE from infective endocarditis (IE) as soon as possible, but this is difficult without information regarding underlying disease and sufficient time for careful investigation. Here, we report a case of recurrent NBTE of a bioprosthetic valve the day following surgery based on an initial diagnosis of IE.
<Learning objective: Nonbacterial thrombotic endocarditis (NBTE) is a relatively rare condition associated with some malignancies and systemic lupus erythematosus. Without information on underlying disease and sufficient time for detailed investigation, it is difficult to distinguish NBTE from infective endocarditis (IE). Unlike IE, the treatment strategy of NBTE involves initiating systemic heparinization as soon possible. This study suggests that NBTE should be considered in cases of recurrent cerebral embolism, even without information indicating underlying pathology.>
Keywords: Recurrent nonbacterial thrombotic endocarditis, Bioprosthetic valve, Malignancy
Introduction
Nonbacterial thrombotic endocarditis (NBTE) is relatively rare, identified at a rate of 1.6% at autopsy [1]. NBTE is associated with prothrombotic conditions, including advanced malignancy and systemic lupus erythematosus. Clinically, NBTE manifests as systemic embolism, commonly cerebral infarction. The fundamental treatment of NBTE involves initiation of systemic anticoagulation as early as possible. Surgical intervention is not recommended unless the patient is in acute congestive failure or in cases with large vegetations. Therefore, it is essential to differentiate NBTE from infective endocarditis (IE), but this is difficult without information regarding underlying disease and sufficient time for careful investigation. Here, we describe a case of recurrent NBTE of bioprosthetic valve the day after urgent mitral valve replacement with an initial diagnosis of IE.
Case report
A 44-year-old man with no previous relevant medical history was transferred to our hospital with right-sided hemiplegia, dysarthria, and high fever. On physical examination, the patient had fever of 38°C, with regular pulse of 98 beats/min and blood pressure of 144/102 mmHg. Oxygen saturation was 98% in room air. Laboratory tests showed elevation of inflammatory markers with white blood cell count of 12600 cells/μL and C-reactive protein level of 11.9 mg/dL. Brain magnetic resonance imaging (MRI) revealed multiple acute cerebral infarctions (Fig. 1a). Transesophageal echocardiography also revealed mobile vegetations >10 mm attached to the posterior mitral leaflet and moderate mitral regurgitation from the posterior commissure (Fig. 1b,c). Although the results of blood cultures were not available preoperatively, he was initially suspected to have IE and multiple cerebral infarction due to embolism. On the day after admission, he had a reduced level of consciousness and computed tomography (CT) revealed a newly developed hemorrhagic infarct in the middle cerebral artery. Due to ongoing vegetation growth and recurrent embolism, mitral valve replacement was urgently performed (Magna Mitral EASE 27 mm; Edwards Lifesciences, Irvine, CA, USA) on day 2 after admission. Perioperatively, fragile vegetations were seen extensively attached to both mitral leaflets on the posterior commissure side (Fig. 1d). We implanted a bioprosthetic valve (BV) to prevent hemorrhagic infarction due to postoperative anticoagulation therapy. Although he awakened promptly after surgery, his level of consciousness was again reduced on the day following surgery, and brain CT revealed global right hemispheric infarction and midline shift (Fig. 2a). On consultation with neurosurgeons in our hospital, internal decompression was performed. Transesophageal echocardiography indicated thickened BV leaflet (Fig. 2b) and its mean pressure gradient was 7.8 mmHg. Initial blood cultures showed negative findings, and histopathological examination revealed no significant inflammatory signs or bacterial colony formation in his vegetations (Fig. 2c). Laboratory tests showed elevation of fibrinogen degradation product level to 246 μg/ml and D-dimer to 51.9 μg/ml. Whole-body CT revealed multiple bone metastases. Therefore, he was re-diagnosed with NBTE associated with malignancy and acute recurrence on the mitral BV. After initiation of intravenous heparinization, leaflet thrombosis was improved (Fig. 3). However, his general condition worsened and the primary lesion could not be identified despite whole-body CT and bone marrow biopsy. The patient died from carcinomatous lymphangiomatosis 50 days after surgery.
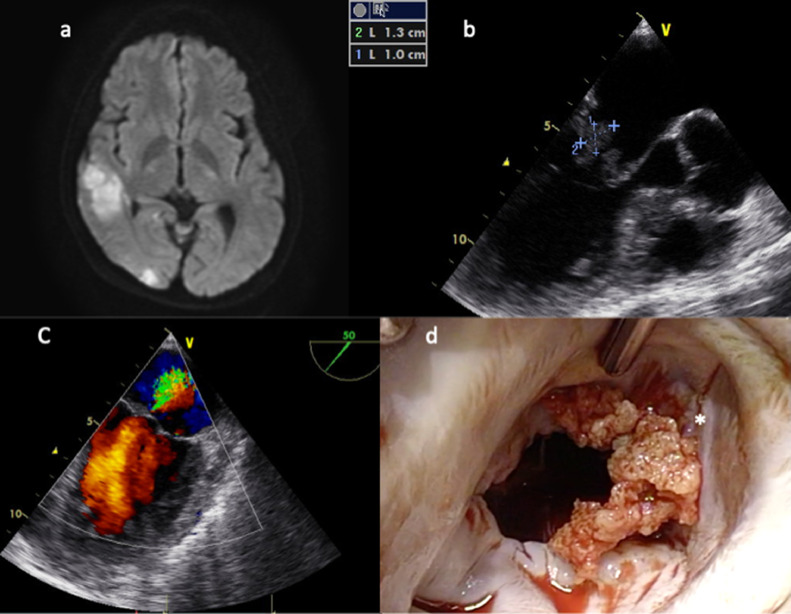
Fig. 1.
(a) Brain magnetic resonance imaging showing multiple acute cerebral infarctions. (b) Transesophageal echocardiography showing mobile vegetations >10 mm attached to the posterior mitral leaflet. (c) Moderate mitral regurgitation from the posterior commissure (commissural view). (d) Intraoperative findings (surgeon's view): fragile vegetations were seen extensively attached to the both mitral leaflets on the posterior commissure side (*).
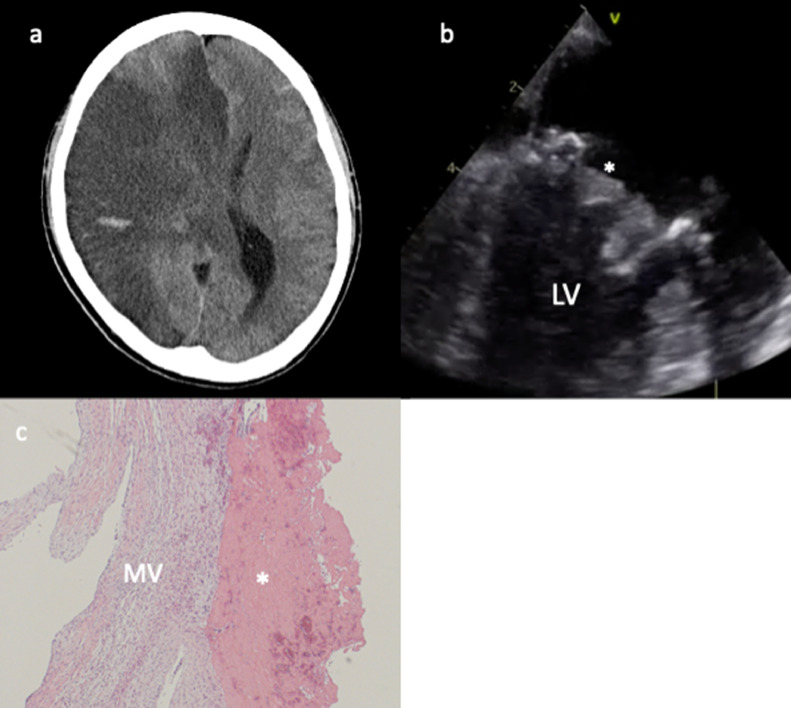
Fig. 2.
(a) Brain computed tomography the day following surgery. Global right hemispheric infarction and midline shift. (b) Transesophageal echocardiography indicating thickened leaflet of the bioprosthetic mitral valve (*) and limited mobility. (c) Histology demonstrating no significant inflammatory cells and no bacterial colonies. LV, left ventricle; MV, mitral valve; *, vegetation.
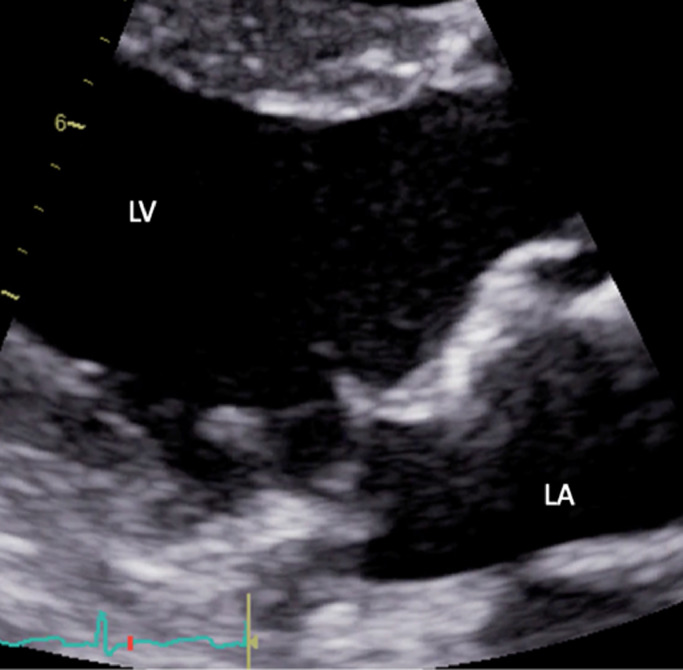
Fig. 3.
After systemic heparinization, transthoracic echocardiography (long-axis view) demonstrated improvement of leaflet thrombosis. LV, left ventricle; LA, left atrium.
Discussion
NBTE characterized by the presence of sterile vegetations on cardiac valves, consisting of fibrin and platelet aggregates, was first described by Ziegler in 1888 [1]. NBTE is a relatively uncommon disease, identified at a rate of 1.6% at autopsy, but is increasingly recognized as a condition associated with numerous diseases, especially malignancies and autoimmune diseases [2]. The cause of NBTE was thought to be hypercoagulability caused by underlying disease. Although a standard treatment for NBTE has not been formally established, many authors have recommended initiating systemic anticoagulation promptly [3]. Unlike the treatment of IE, surgical intervention is not recommended unless the patient is in acute congestive failure or has recurrent thromboembolism despite anticoagulation therapy [2]. Therefore, it is essential to distinguish NBTE from IE to allow appropriate treatment.
NBTE and IE have been reported to differ in fever, blood culture, vegetation size, and underlying disease [1]. In this case, although the results of blood cultures were not available preoperatively, he was febrile. While vegetations in NBTE are commonly smaller than 10 mm [2], the vegetations in this case were >10 mm. Importantly, he had no prior medical history indicating underlying pathology. Our team and radiologist could not detect bone metastasis on preoperative whole-body CT. Moreover, as the current guidelines recommend earlier surgery for IE if it is indicated even with cerebral infarction [3], this patient required urgent operation. Therefore, we did not have sufficient time for in-depth investigation, and it was extremely difficult to distinguish between NBTE and IE preoperatively in this case.
The cerebral hemorrhagic infarction in this patient affected our treatment strategy. Although the current guidelines recommend a 4-week wait for surgery [3], he had high risk of more recurrence of embolism. Moreover, a few reports showed that postoperative exacerbation of small hemorrhage <20-30 mm was not common, as in this case [4]. Therefore, we decided to perform surgery after careful discussion and with the patient's informed consent. We implanted a BV and did not initiate systemic heparinization on the day after surgery, which resulted in acute recurrent NBTE. NBTE of BV is extremely rare, and there are few reports in the literature [5]; this previous report described NBTE of BV 4 years after first valvular surgery. To our knowledge, there have been no reports regarding acute recurrent NBTE of BV the day after surgery, as in our case. Another report about recurrent NBTE recommended that anticoagulation should be continued even after surgery [6]. In our case, hypercoagulation and lack of anticoagulation resulted in recurrence. Unfortunately, the lack of information about malignancy and cerebral hemorrhage in our case did not allow us to select appropriate management. This report suggests that NBTE should be considered in cases of recurrent cerebral embolism, even without information indicating underlying pathology.
Conflict of interest
The authors have no conflicts of interest to report.
Acknowledgments
This report has not been presented elsewhere.
References
- 1.Lopez JA, Ross RS, Fishbein MC. Nonbacterial thrombotic endocarditis. A review. Am Heart J. 1987;113:773–784. doi: 10.1016/0002-8703(87)90719-8. [DOI] [PubMed] [Google Scholar]
- 2.Asopa S, Patel A, Khan OA, Sharma R, Ohri SK. Non-bacterial thrombotic endocarditis. Eur J Cardiothorac Surg. 2007;32:696–701. doi: 10.1016/j.ejcts.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 3.Nakatani S, Ohara T, Ashihara K, Izumi C, Iwanaga S, Eishi K, Okita Y, Daimon M, Kimura T, Toyoda K, Nakase H, Nakano K, Higashi M, Mitsutake K, Murakami T, et al. JCS 2017 guideline on prevention and treatment of infective endocarditis. Circ J. 2019;83:1767–1809. doi: 10.1253/circj.CJ-19-0549. [DOI] [PubMed] [Google Scholar]
- 4.Hosono M, Sasaki Y, Hirai H, Sakaguchi M, Nakahira A, Seo H, Morisaki A, Suehiro S. Considerations in timing of surgical intervention for infective endocarditis with cerebrovascular complications. J Heart Valve Dis. 2010;19:321–325. [PubMed] [Google Scholar]
- 5.Ram D, Armstrong G, Khanijow V, Sibal AK. Nonbacterial thrombotic endocarditis of a bioprosthetic valve: Questions to ponder before replacement of the valve. J Card Surg. 2020;35:1142–1144. doi: 10.1111/jocs.14536. [DOI] [PubMed] [Google Scholar]
- 6.Brock MA, Bleiweis MA, Reid J, Moguillanksy D. Recurrent nonbacterial thrombotic endocarditis: a novel therapeutic approach. J Cardiol Cases. 2018;17:175–177. doi: 10.1016/j.jccase.2018.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]