Abstract
Takotsubo syndrome (TS) is a reversible form of cardiomyopathy characterized by transient systolic dysfunction with regional wall motion abnormalities and absence of coronary artery obstruction, which can be precipitated by severe emotional or physical stress. Its clinical presentation is similar to that of acute coronary syndrome. However, TS presenting with atrioventricular (AV) block with ventricular asystole is rarely reported. In this article, we describe the case of a postmenopausal woman who experienced near cardiac arrest due to high-degree AV block. Although transthoracic echocardiography revealed left ventricular dysfunction with severe global hypokinesia, coronary angiography and cardiac magnetic resonance imaging showed normal coronary arteries without myocardial scarring. The patient's condition improved after permanent pacemaker implantation and medical treatment for heart failure. Echocardiography and pacemaker analysis at two-month follow-up revealed normalization of heart function and cardiac rhythm, and the patient was finally diagnosed with TS.
<Learning objective: Takotsubo syndrome can present with conduction abnormalities such as a high-degree atrioventricular block in case of left ventricular basal segment involvement. Cardiac magnetic resonance imaging is useful for distinguishing stress-induced cardiomyopathy from other myocardial diseases with non-obstructive coronary arteries.>
Keywords: Takotsubo cardiomyopathy, Atrioventricular block, Ventricular asystole
Introduction
Takotsubo syndrome (TS) is induced by emotional or physical stress and it commonly occurs in postmenopausal women. Electrocardiographic abnormalities mimicking acute coronary syndrome, including ST segment elevation and T-wave inversion, are commonly seen; however, the coexistence of high-degree atrioventricular (AV) block is rare in patients with TS. Here, we describe TS presenting as high-degree AV block with ventricular asystole provoked by emotional stress.
Case report
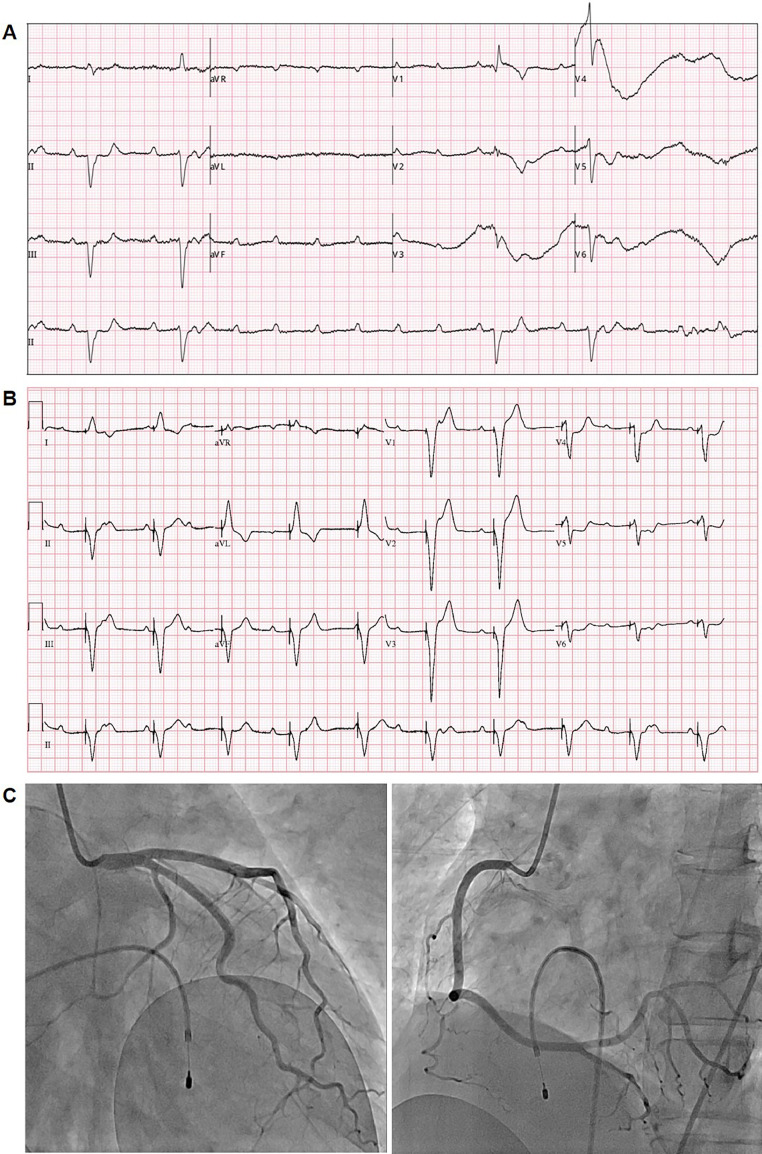
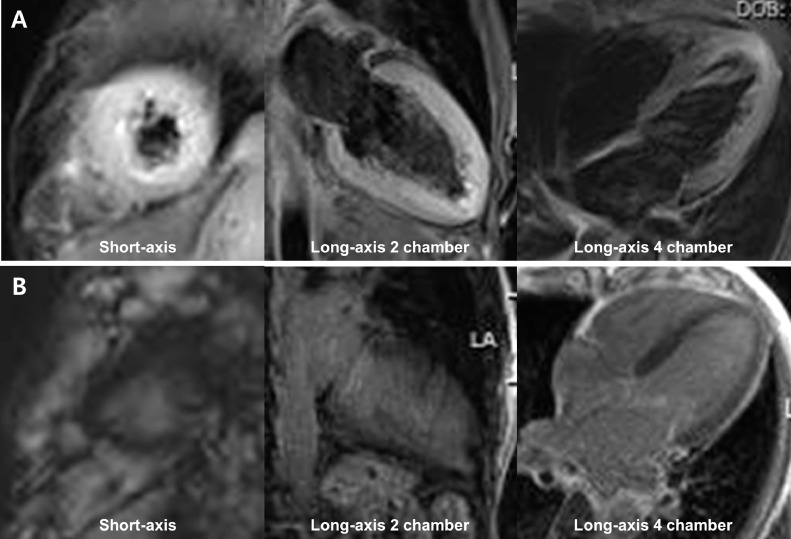
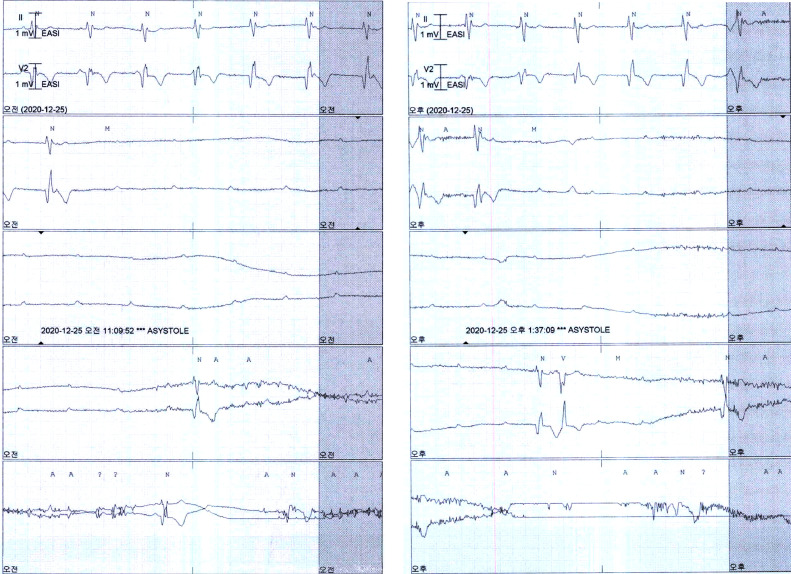
A 60-year-old female presented to the emergency room with two-day history of sudden onset squeezing chest pain. Her risk factors for cardiovascular disease included smoking and being postmenopausal. The patient stated that she had recently experienced severe psychological stress due to her husband's cancer diagnosis. Not long after she came to the emergency room, she showed signs of agitation and complained of severe chest discomfort, and suddenly developed a generalized tonic-clonic seizure. Her blood pressure was low at 77/43 mmHg and electrocardiography showed high-degree AV block with marked bradycardia (heart rate, 26 beats/minute) (Fig. 1A). With transcutaneous cardiac pacing, no further convulsion occurred. Serum cardiac enzymes (creatine kinase-MB, 73.8 ng/ml; troponin-T, 11.58 ng/ml) and brain natriuretic peptide (834 pg/mL) were both elevated. Ventricular pacing with a temporary pacemaker via the right common femoral vein was promptly performed (Fig. 1B). Acute myocardial infarction was suspected, and emergent coronary angiography was performed, which showed non-obstructive coronary arteries (Fig. 1C). Her renal function, electrolytes, and thyroid function were normal. Transthoracic echocardiography showed depressed left ventricular systolic function (ejection fraction, 28%) with severe global hypokinesia (Movies 1 and 2). With intravenous dobutamine administration, her blood pressure remained within the normal range, and her heart rate remained above 60 beats/minute without back-up temporary pacing. To determine myocardial viability and identify the presence of myocardial disease, cardiac magnetic resonance imaging (CMR) was performed on hospital day 4. Cine images of CMR revealed moderately reduced systolic function with quantitative ejection fraction of 35%, and relative hypokinesis of mid to apical septal wall (Movies 3 and 4). Anterior and septal wall edema was noted in T2 stir sequences, however delayed gadolinium enhancement was not seen (Fig. 2). Temporary pacemaker was removed on hospital day 4; however, the patient experienced recurrent episodes of near syncope during dobutamine tapering, and several episodes of high-degree AV block with ventricular asystole were documented at telemetry monitoring on hospital day 6 and 7 (Fig. 3). Therefore, the temporary pacemaker was re-implanted via the jugular vein, and a dual-chamber permanent pacemaker was implanted on hospital day 11 because the AV block had not resolved during hospitalization. Bisoprolol and valsartan were prescribed to reduce cardiac afterload, and the patient was discharged on hospital day 15 after the improvement in her symptoms and stable vital signs. After recovery from the AV block, the electrocardiography showed deep and widespread precordial T inversion (Online Fig. 1). At two-month follow-up in the outpatient clinic, echocardiography showed normalization of left ventricular systolic function (ejection fraction, 60%) without regional wall motion abnormality. Permanent pacemaker event analysis showed that the spontaneous sinus rhythm was well-maintained without AV block, and no pacing rhythm was observed. The patient was finally diagnosed with TS provoked by severe emotional stress related to her husband's health issues.
Fig. 1.
12-lead electrocardiography and coronary angiography results. (A) Electrocardiography revealed a high-degree atrioventricular block with transient asystole. (B) Ventricular pacing rhythm after temporary pacemaker insertion. (C) Coronary angiography revealed normal coronary arteries without luminal narrowing.
Fig. 2.
Cardiac magnetic resonance imaging findings. (A) T2-weighted short-tau inversion recovery sequence showed high-signal intensity in the apex and anterior wall. (B) Delayed phase showed no late gadolinium enhancement.
Fig. 3.
Recurrent episodes of high-degree atrioventricular block with ventricular asystole documented on telemetry.
Discussion
TS was first reported in Japan in 1990 and was called takotsubo cardiomyopathy due to its distinctive morphology of left ventricular apical ballooning resembling a Japanese octopus pot, takotsubo. It is predominantly seen in postmenopausal women and is frequently precipitated by a stressful event or systemic illness. Typical TS is characterized by ventricular dysfunction (hypokinesia, akinesia, or dyskinesia) of the apical and/or mid-segments of the left ventricle with apical ballooning; however, other types of ventricular dysfunction have been reported, including biventricular, basal, and focal hypokinesia [1]. Although the pathophysiology of this disorder remains unclear, it has been proposed that TS develops secondary to catecholamine-mediated myocardial stunning due to coronary artery spasm, microvascular dysfunction, dynamic mid-ventricular or outflow tract obstruction, and direct effects of catecholamines on cardiomyocytes [2, 3].
Association of TS with various arrhythmic complications, ranging from benign tachyarrhythmia to fatal ventricular fibrillation, has been previously reported [4]. In a comprehensive review of case series of TS patients regarding the arrhythmia occurrence, AV block was reported in 2.9% of total cases [4]. However, ventricular asystole due to high-degree AV block as an initial presentation in TS such as in our case is rarely reported. Unlike typical cases of TS involving the mid-segments and/or apex of the left ventricle, global involvement, including the basal segment of the left ventricle that is adjacent to the AV node, was suspected in the initial echocardiography finding in our patient. This may explain the transient conduction system impairment, which was probably caused by the neurogenic or ischemic injury of the left ventricular basal segment. Global hypokinesis type of TS is not included in the general variants of the TS, and it is not adequately represented in the international registries since catheterization is not routinely performed in this group. However, several case reports and series showed the transient severe global hypokinesia that developed over the course of noncardiac illness, which is thought to be another form of TS [5], and we strongly believe several instances of TS manifest as global left ventricular dysfunction. However, the CMR, which was taken three days later, showed a slight improvement in ejection fraction with the relative hypokinesia of mid to apical septal wall compared to initial echocardiography. In the T2 stir sequence, myocardial edema appeared in the anterior wall and septum, but not in the basal wall, which was inconsistent with our hypothesis that AV block could have been caused by basal segment involvement. As the myocardial edema indicative of acute ischemic or inflammation is a transient dynamic phenomenon, however, the global myocardial edema might have been improving during the interval between symptom onset and CMR scan. In our case, heart function and area of wall motion abnormality has changed over a few days, and myocardial edema and wall hypokinesia coincided in CMR. Some case reports, in which TS was accompanied by complete AV block, showed that the AV block persisted after complete recovery of the cardiac function [6, 7]. These reports hypothesized that the occurrence of complete AV block was probably a trigger for TS. In our patient, pacemaker interrogation two months after the index event showed complete resolution of left ventricular contractile dysfunction as well as normalization of cardiac rhythm, which suggests that the conduction abnormality was probably caused by TS.
The clinical features of TS are similar to those of acute coronary syndrome, and conduction defects are frequently observed in myocardial infarction or other myocardial diseases. Therefore, prompt diagnosis of this disorder can be challenging. If the angiographic findings are discordant with acute coronary syndrome, CMR can be useful to differentiate between TS and other forms of acute ventricular dysfunction associated with patent coronary arteries. The combination of regional wall motion abnormalities and matching reversible myocardial edema without late gadolinium enhancement may help distinguishing TS from embolism and myocarditis [8]. Since we did not conduct a biopsy of myocardium, it can be difficult to exclude acute myocarditis. However, our patient had no prior symptoms of upper respiratory infection or fever suggesting myocarditis. In addition, there were no late gadolinium enhancement on CMR or pericardial involvement which are usually seen in acute myocarditis. In our case, hence, we considered the possibility of TS and expected spontaneous resolution to sinus rhythm. However, the point in time when the improvement in heart function and rhythm can be expected to occur remains unpredictable; therefore, permanent pacemaker implantation was needed to prevent recurrent paroxysmal syncopal episodes. It has been reported in the literature that the resolution of conduction defect does not always coincide with the recovery of left ventricular function, and the reported period before the normalization of cardiac rhythm ranged from two days to two years [9, 10]. Although TS is believed to be a relatively benign condition that resolves spontaneously, the recognition of AV conduction defects, which can be potentially life-threatening is important; and timely management is necessary to improve patient outcomes.
Declaration of Competing Interest
The authors declare that there is no conflict of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jccase.2021.09.004.
Appendix. Supplementary materials
Transthoracic echocardiography, 4-chamber view.
Transthoracic echocardiography, 2-chamber view.
Cine image of cardiac magnetic resonance, 4-chamber view.
Cine image of cardiac magnetic resonance, 3 chamber view.
References
- 1.Medina de Chazal H, Del Buono MG, Keyser-Marcus L, Ma L, Moeller FG, Berrocal D, Abbate A. Stress cardiomyopathy diagnosis and treatment: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72:1955–1971. doi: 10.1016/j.jacc.2018.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roshanzamir S, Showkathali R. Takotsubo cardiomyopathy a short review. Curr Cardiol Rev. 2013;9:191–196. doi: 10.2174/1573403X11309030003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goico A, Chandrasekaran M, Herrera CJ. Novel developments in stress cardiomyopathy: From pathophysiology to prognosis. Int J Cardiol. 2016;223:1053–1058. doi: 10.1016/j.ijcard.2016.08.241. [DOI] [PubMed] [Google Scholar]
- 4.Syed FF, Asirvatham SJ, Francis J. Arrhythmia occurrence with takotsubo cardiomyopathy: a literature review. Europace. 2011;13:780–788. doi: 10.1093/europace/euq435. [DOI] [PubMed] [Google Scholar]
- 5.Win CM, Pathak A, Guglin M. Not takotsubo: a different form of stress-induced cardiomyopathy–a case series. Congest Heart Fail. 2011;17:38–41. doi: 10.1111/j.1751-7133.2010.00195.x. [DOI] [PubMed] [Google Scholar]
- 6.Rathore A, Banavalikar B, Shenthar J, Acharya D, Parvez J, Setty Srinivasa KH. An unusual case of complete atrioventricular block causing takotsubo syndrome. Indian Pacing Electrophysiol J. 2018;18:123–125. doi: 10.1016/j.ipej.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sakul NFN, Shrestha S, Balabbigari N, Talati S. Complete heart block: A rare complication of takotsubo syndrome. Case Rep Cardiol. 2019;2019 doi: 10.1155/2019/2576373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Placido R, Cunha Lopes B, Almeida AG, Rochitte CE. The role of cardiovascular magnetic resonance in takotsubo syndrome. J Cardiovasc Magn Reson. 2016;18:68. doi: 10.1186/s12968-016-0279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benouda L, Roule V, Foucault A, Dahdouh Z, Lebon A, Milliez P. Conduction disturbances in takotsubo cardiomyopathy: a cause or a consequence? Int J Cardiol. 2012;159:61–62. doi: 10.1016/j.ijcard.2012.03.164. [DOI] [PubMed] [Google Scholar]
- 10.Inayat F, Virk HUH, Ullah W, Riaz I. Takotsubo cardiomyopathy-related complete heart block and torsades de pointes. BMJ Case Rep. 2017;2017 doi: 10.1136/bcr-2016-218017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic echocardiography, 4-chamber view.
Transthoracic echocardiography, 2-chamber view.
Cine image of cardiac magnetic resonance, 4-chamber view.
Cine image of cardiac magnetic resonance, 3 chamber view.