Abstract
Studies in the field of neuroscience and psychology have hypothesized that a causal association exists between atopic diseases and attention-deficit/hyperactivity disorder (ADHD). Previous systematic reviews and meta-analyses have reported a higher risk of ADHD in children with atopic diseases; however, the relationship between ADHD symptoms and atopic diseases remains unclear. We systematically reviewed observational cross-sectional and longitudinal studies to investigate the relationship between atopic diseases and ADHD symptom severity (hyperactivity/impulsivity and inattention). The majority of studies showed a statistically significant association between atopic diseases and both ADHD symptoms, with substantial heterogeneity in the outcome of hyperactivity/impulsivity. Remarkably decreased heterogeneity and statistical significance were observed in the second meta-analysis of ADHD-related behavior symptoms in atopic patients without ADHD. Our study indicated that atopic diseases not only associated with ADHD but also ADHD symptoms severity. This association was even observed in children with subthreshold ADHD, indicating that atopic diseases may play a role in the spectrum of ADHD symptom severity. Trial registration: This study was registered on PROSPERO (registration ID: CRD42020213219).
Subject terms: Immunology, Psychology, Medical research, Signs and symptoms
Introduction
In the past decade, atopic diseases have been a cause of increased concern because of their substantially high prevalence (approximately 20 to 40%) worldwide1, with more prominent increasing trend in developing countries2. Atopic march, defined as the development of atopic dermatitis in infancy and subsequent allergic rhinitis and asthma in later childhood, can cause fatigue; attention, learning, and memory deficits; and depression. Moreover, atopic diseases have been reported to considerably affect children’s sleep, school performance, development, and quality of life3,4. In addition, recent studies have reported that the parents or main caregivers of children with atopic diseases, particularly those with multiple atopic diseases, experience considerable stress and psychosocial burden4–8 Thus, increasing public attention has been focused on the management of atopic diseases8.
Attention-deficit/hyperactivity disorder (ADHD) is among the most common neuropsychiatric disorders in children and adolescents, with a prevalence of approximately 5%. ADHD is characterized by hyperactivity, impulsivity, and inattention that lead to not only functional impairment but also executive function impairment and emotional dysregulation9,10. ADHD can be caused by multiple factors (e.g., genetic, epigenetic, and environmental). Moreover, studies have indicated that ADHD occurs due to immature brain development, and it may also be accompanied by other neurobehavioral developmental delays and even intellectual disability10,11. Many studies have reported that ADHD symptoms were still observed in adulthood in a majority of patients with ADHD, even in those with adult ADHD who did not meet the criteria for ADHD in their childhood12–14. Adult patients with ADHD experience a financial burden and may even require considerable support14. These findings indicate that ADHD is a matter of considerable concern in child and adolescent psychiatry.
A previous study investigated the relationship between atopic diseases and ADHD15. A higher risk of ADHD was noted in patients with all three atopic diseases, namely atopic dermatitis, allergic rhinitis, and asthma (i.e., atopic march)16,17. In addition, children with both atopic diseases and ADHD had an increased risk of developing more severe ADHD symptoms compared with those with only ADHD18. Also, the association between atopic diseases and ADHD-related behavioral symptoms19, which some researches mentioned as subthreshold ADHD20, has been investigated recently. Although several meta-analyses and systematic reviews have strongly supported the relationship between atopic diseases and ADHD17,21,22, they still had many limitations. The heterogeneity observed in some systematic reviews might have affected their findings; for instance, some reviews did not include studies with standard inclusion and exclusion criteria, and whether the atopic and unexposed groups included patients diagnosed as having ADHD remained unclear16,21. In addition, few studies have reported a relationship between atopic diseases and subthreshold ADHD. Moreover, no systematic review and meta-analysis has examined whether atopic diseases affect the severity of both hyperactivity/impulsivity and inattention—the two main symptoms and diagnostic criteria related to ADHD.
In this systematic review and meta-analysis, we reviewed studies examining the relationship between atopic diseases and the severity of ADHD symptoms including hyperactivity/impulsivity and inattention. In addition, we explored more precise value of this relationship by defining inclusion and exclusion criteria for groups. By doing so, we could exclude some confounding effects and provide additional information regarding the relationship between atopic diseases and subthreshold ADHD; this involved examining the data of children without a previous diagnosis of ADHD but who had an association of developing more severe ADHD symptoms.
Results
Search results
Through our literature search, we identified 4722 studies (2872, 1504, 345, and 1 from PubMed + Medline, Embase, Psycinfo, and register, respectively). Fifteen additional studies were identified through other sources. Using EndNote, we found that 671 studies were duplicates and we thus excluded them. Subsequently, we screened the titles and abstract for eligibility of the remaining 4066 studies. During title and abstract screening, we removed 630 because they did not include a relevant unexposed group and were letters or replies. Additionally, we excluded 1077 studies because they were not original research. Moreover, 1222 studies were excluded because they were not relevant to our research. Subsequently, after reviewing the full texts of the remaining 1136 studies, we excluded 1098 studies, 78 of which had missing data or full texts, 811 had nonrelevance, and 210 were not case–control, cross-sectional, or cohort studies. Finally, we included the remaining 38 studies in this systematic review for qualitative synthesis, and 16 of them were included in the quantitative review and meta-analysis. The procedure for study inclusion is shown in Appendix B in the Supplementary Materials.
Qualitative systematic review
In 38 studies including 117,181,049 participants in our qualitative systemic review, the researchers examined the relationship between atopic diseases and ADHD symptoms severity by displaying prevalence of ADHD in patients with atopy, odds ratios (OR) of Attention deficit disorder (ADD)/ADHD in children with atopy, or calculating scores for hyperactivity/impulsivity, inattention, or total ADHD symptoms. Table 1 lists the characteristics of included studies. Most of the studies assessed atopic diseases by using parental questionnaires or based on their diagnosis by physicians or dermatologists according to specific diagnostic criteria, including the Global Initiative for Asthma guidelines, Allergic Rhinitis and its Impact on Asthma guidelines, and UK Working Party criteria. Seven study groups conducted an advanced additional test for atopy such as the skin-prick test and blood sampling for serum-specific IgE (MAST or Phadiatop tests). The included studies used different outcome scales including the Conners’ Parent Rating Scale; ADHD Rating Scale; Swanson, Nolan, and Pelham IV Scale; Child Behavior Checklist, Early Childhood Inventory-4, the German ADHD Rating scale (FBB-HKS), and the Strengths and Difficulties Questionnaire (SDQ). Despite the variability in outcome scales, most scales were designed on the basis of the DSM-IV criteria. Eight studies adopted the SDQ, which is not derived from the DSM-IV criteria; however, the SDQ has been reported to be relevant to the DSM-IV23–25. Most of the studies investigated the effect of confounding factors, including age, sex, multiple atopic diseases, the comorbidity with ADHD, severity of atopic diseases, persistent atopic diseases, and stressful parenting. Nineteen of the twenty studies examining the outcome of total ADHD symptoms reported a significant relationship between the severity of ADHD symptoms and atopic diseases. Furthermore, 9 of the 15 studies examining the outcome of hyperactivity and 13 of the 16 studies examining the outcome of inattention demonstrated a significant relationship between the severity of the examined ADHD symptoms and atopic diseases.
Table 1.
Studies examining the relationship between atopic diseases and hyperactivity in the qualitative analysis.
| Study name | Outcome (95% CI) | Study design | Country/City | Ethnicity | Number of participants/Exposed group/Unexposed group | Age (mean of the exposed group)/sex (male, %) | Diagnostic criteria for ADHD | Atopic disease/method used for assessing atopic diseases | Adjustment for confounding factors |
|---|---|---|---|---|---|---|---|---|---|
| Yuksel et al. 200858 | Continuous data for HI and IN* | Cross-sectional | Manisa, Turkey | Not reported | 100/62/38 | 7–12 years (9.2)/57% | DSM-IV | Asthma/Physician’s diagnosis (GINA 2006) | No |
| Camfferman et al. 201026 | Continuous data for HI* and total ADHD symptoms* | Cross-sectional | South Australia, Australia | Not reported | 107/77/30 | 6–16 years (9.9)/46.72% | Conner’s Parent Rating Scale-Revised | Atopic dermatitis/Physician’s diagnosis (Hanifin and Rajka criteria) | Yes |
| Chang et al. 201359 | Continuous data for HI and IN | Cross-sectional | Seoul and Ilsan and Gwacheon in Gyeonggi-do province in Korea | Not reported | 575 | 3–7 years (4.8)/51.3% | CBCL | Atopic dermatitis, allergic rhinitis, and asthma/Physician’s diagnosis and questionnaire (ISAAC questionnaire and SCORAD index) | No |
| Goodwin et al. 201360 | OR of ADHD in children with asthma*(different grades of severity [moderate*]/persistent [remission* and late onset*]) | Cohort | Perth, Western Australia | Not reported | 2193/390/1803 | 5, 8, 10, 14, and 17 years/62.56% | CBCL | Asthma/Physician’s diagnosis (Australian Asthma Handbook) | Yes |
| Kim et al. 201461 | Continuous data for impulsivity and inattention (divided attention task*) | Cohort | Korea | Not reported | 1036/797/239 | 3–16 years (11.4)/69.88% | Computerized comprehensive attention test | Allergic rhinitis/skin prick test | Yes |
| Lee et al. 201462 | Continuous data for HI and IN* | Cross-sectional | Seoul, Korea | Not reported | 160/87/73 | 6–13 years (8.49)/39.4% | DSM-IV | Allergic rhinitis/physician’s diagnosis (ARIA guideline) | Yes |
| Yang et al. 201463 | Continuous data for HI* and IN* | Cross-sectional | Taipei, Taiwan | Not reported | 122/93/29 | 6–14 years (10.78)/52.2% | DSM-IV-TR | Allergic rhinitis/Physician’s diagnosis (ARIA 2008) + IgE test (MAST or Phadiatop tests) | Yes |
| Catal et al. 201664 | Continuous data for total ADHD symptoms* and percentage of psychiatric disorders determined by ECI-4* | Cross-sectional | Malatya, Samsun, Aydın, Istanbul, Turkey | Not reported | 154/80/74 | 3–5 years (4.03)/51.3% | ECI-4 | Atopic dermatitis/Physician’s diagnosis (Hanifin and Rajka criteria) | No |
| Hammer-Helmich et al. 201665 | Continuous data for total ADHD symptoms *© | Cross-sectional | Copenhagen, Denmark | Not reported | 9036/2433/6603 | 3–15 years (NA)/49.5% | SDQ | Eczema, asthma, and hay fever/Questionnaire (UK Working Party Criteria) | Yes |
| Strom et al. 201666 | OR of ADD/ADHD in children with atopic dermatitis* | Cross-sectional | U.S. Bureau of Census | Not reported | 180,799/17,277/163,522 | < 18 years (NA)/49.94% | Questionnaire | Atopic dermatitis, asthma, and allergic rhinitis/questionnaire | Yes |
| Yang et al. 201667 | Continuous data for HI* and IN* | Case–control | Taipei, Taiwan | Not reported | 99/68/31 | 6–14 years (9.25)/82.4% | DSM-IV | Allergic rhinitis/physician’s diagnosis + IgE test (MAST or Phadiatop tests) | Yes |
| Feng et al. 201768 | Continuous data for HI* and IN* | Cross-sectional | Wenzhou, China | Not reported | 643/248/320 | 6–12 years (9.25)/51.9% | DSM-IV | Allergic rhinitis/physician’s diagnosis (ARIA 2008) + skin prick test | Yes |
| Lin et al. 201745 | OR of ADHD (inattentive/Hyperactive impulsive/combined) in children with atopic dermatitis, asthma, allergic rhinitis (fever/active)* | Cross-sectional | Taiwan | Han Chinese | 2896/2235/661 | 9–10 years (10)/50.5% | SNAP-IV | Atopic dermatitis, asthma, and allergic rhinitis/questionnaire (ISAAC questionnaire) | Yes |
| Abd El-Hamid et al. 201869 | Prevalence of different grades of ADHD symptoms (mild, moderate, and severe) in children with or without atopic diseases* | Case–control | Cairo, Egypt | Not reported | 160/100/60 | 6–12 years (8.54)/81.25% | DSM-IV | Allergic diseases/physician’s diagnosis, skin prick test, and total IgE enzyme immunoassay (ELISA) | No |
| Kuniyoshi et al. 201870 | Continuous data for total ADHD symptoms©* | Cross-sectional | Miyagi Prefecture, Japan | Not reported | 9954/1641/8313 | 7–14 years (10.42)/49.9% | SDQ | Eczema/ISAAC (Eczema symptom questionnaire) | Yes |
| Schmitt et al. 20186 | Continuous data for HI and IN* | Case–control | Dresden, Germany | Not reported | 89/35/45 | 6–12 years (9.9)/62.9% | ICD-10 | Atopic dermatitis/dermatologist’s diagnosis (UK Working Party Criteria) | Yes |
| Cices et al. 201971 | Continuous data for HI and IN* | Case–control | US, Chicago, Illinois | Caucasian (31.43%) African American (22.86%) Hispanic (20%) Asian (20%) Other (5.71%) | 35/17/18 | 6–16 years (11.07)/65.7% | Standardized Vanderbilt questionnaires | Atopic dermatitis/SCORAD | Yes |
| Tajdini et al. 201972 | Prevalence of ADHD in patients with asthma and controls* | Case–control | Tehran, Iran | Not reported | 171/79/92 | 5–11 years (7.54)/57% | Child Symptom Inventory-4 (CSI-4) | Asthma/respiratory function test | Yes |
| Zhou et al. 201973 | Prevalence of ADHD in patients with asthma and controls* | Cross-sectional | Guiyang, China | Han (77.59%) | 522/261/261 | 6–16 years (9.35)/61.69% | Mini-International Neuropsychiatric Interview for children and adolescents | Asthma/physician’s diagnosis (Bronchial Asthma Diagnostic and Prevention Guide for Children [2016 version]) | Yes |
| Feng et al. 202074 | Continuous data for HI* and IN* | Cross-sectional | Chongqing, China | Not reported | 273/89/184 | 6–12 years (8.3)/62.63% | SNAP-IV | Atopic dermatitis/dermatologist’s diagnosis (UK criteria) | Yes |
| Fuhrmann et al. 202075 | HR of ADD/ADHD in children with atopic dermatitis* | Cohort | Germany | Not reported | 37,235/9257/27,978 | From 0 to 7–9 years/51.7% | ICD-10 | Atopic dermatitis/ICD-10 | Yes |
| Guo et al. 202076 | Continuous data for HI (AR, AD, and asthma) and IN (AR*, AD, and asthma*) | Cohort | Kaohsiung, Taiwan | Not reported | 97 | 6 years/54.6% | SNAP-IV | Atopic dermatitis, asthma, and allergic rhinitis/ISAAC questionnaire, physician’s diagnosis (Hanifin–Rajka criteria), and IgE test | Yes |
| Huang et al. 202077 | OR of ADD/ADHD in children with atopic dermatitis* | Cross-sectional | US Northeast (17.96%) North Central (19.33%) South (45.83%) West (16.42%) Unknown (0.47%) | Not reported | 203,533/86,969/116,564 | 0–17 years (5.3)/51.74% | ICD-10-CM | Atopic dermatitis/IBM MarketScan Commercial Claims database (ICD-10-CM code for AD: L20*) | Yes |
| Jackson-Cowan et al. 202078 | OR of ADD/ADHD in children with atopic dermatitis* | Cross-sectional | US Northeast (15.73%) North Central (20.27%) South (36.21%) West (27.78%) | White (48.44%) Black (15.38%) Hispanic (27.86%) Asian (6.06%) Native American (0.97%) Other (1.29%) | 109,482/13,398/96,084 | 2–17 years/51.48% | Questionnaire | Atopic dermatitis/questionnaire | Yes |
| Kuo et al. 202041 | Continuous data for HI* and IN | Cross-sectional | Kaohsiung, Taiwan | Not reported | 191/109/92 | (6.59)/54.44% | SNAP-IV | Atopic dermatitis, asthma, and allergic rhinitis/physician’s diagnosis | Yes |
| Minatoya et al. 202079 | Continuous data for total ADHD symptoms* | Cross-sectional | Hokkaido, Japan | Not reported | 3862/799/3063 | (5.28)/49.9% | SDQ | Atopic dermatitis/ISAAC | Yes |
| Montalbano et al. 202080 | Continuous data for total ADHD symptoms * | Cross-sectional | Florence, Italy | Not reported | 141 | 6–11 years (10)/61.7% | SDQ | Asthma/GINA | Yes |
| Sollander et al. 202081 | OR of ADD/ADHD symptoms in children with atopic dermatitis* | Cross-sectional | Uppsala, Sweden | Not reported | 4451/397/4054 | 3–5 years (4.34)/50.42% | SDQ | Asthma/questionnaire | Yes |
| Wan et al. 202082 | OR of significant ADD/ADHD symptoms in children with atopic dermatitis* | Cross-sectional | US | White (66.6%)Black (20.9%)Indian (0.9%)Asian (5.3%)Multiracial (6.3%) | 57,726,856/6,807,687/50,919,169 | (10.08)/48.6% | SDQ | Atopic dermatitis/questionnaire | Yes |
| Berzosa-Grande et al. 202119 | Continuous data for IN* | Cross-sectional | Madrid, Spain | Not reported | 366/194/172 | 6–11 years (8.68)/52.7% | CBCL | Asthma, atopic dermatitis, allergic rhinitis/questionnaire | No |
| Chai et al. 202183 | OR of comorbidity of ADHD and Asthma* | Cross-sectional | Canada | Not reported | 768,460/28,729/158,064 | (8.7)/45.8% | ICD-10 | Asthma/clinical physician’s diagnosis | No |
| Galéra et al. 202184 | Continuous data for ADHD symptoms* | Cohort | Canada | Not reported | 2120 | 1.5, 2.5, 3.5, 4.5, 5, 6, 7, 8, 10, 13, 15, 17 years/50.9% | Behavioral ratings of ADHD symptoms | Asthma, eczema/Code of database (Quebec Longitudinal Study of Child Development (QLSCD)) | Yes |
| Hou et al. 202185 | OR of ADD/ADHD in children with atopic dermatitis* | Cross-sectional | US | Not reported | 228,898/23,353/205,545 | < 17 years/50.2% | database | Atopic dermatitis/questionnaire | Yes |
| Keller et al. 202186 | Association between asthma, atopic dermatitis* and ADHD symptoms | Cross-sectional | Leipzig, Germany | Not reported | 1764 | 2.53–10.49 years(6.1)/53.1% | SDQ | Asthma, atopic dermatitis/questionnaire | No |
| Özyurt et al. 202187 | Continuous data for ADHD symptoms* | Cross-sectional | Izmir, Turkey | Not reported | 121/61/60 | 12–18 years (14.27)/47.54% | SDQ | Asthma/GINA (2017) | No |
| Rajhans et al. 202188 | Continuous data for IN* | Cross-sectional | North India | Not reported | 60/30/30 | 8–15 years (11.92)/70% | M.I.N.I. KID, CBCL | Asthma/GINA (2015) | Yes |
| Vittrup et al. 202189 | HR of ADHD in children with atopic dermatitis* | Cohort | Denmark | Not reported | 157,113/14,283/142,830 | 0–18 years/57% | Codes of database | Atopic dermatitis/clinical physician’s diagnosis | Yes |
| Yüksel et al. 202190 | Continuous data for HI* and IN in ADHD children with or without asthma | Cross-sectional | Izmir, Turkey | Not reported | 355/91/264 | 2–6 years | ADHD Rating Scale-IV, K-SADS-PL | Asthma/questionnaire | Yes |
ADHD, Attention-Deficit/Hyperactivity Disorder; OR, Odds Ratio; HI, Hyperactivity/Impulsivity; IA, Inattention; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders; GINA 2006, Global Initiative for Asthma, 2006; CBCL, Child Behavior Checklist; ARIA, Allergic Rhinitis and its Impact on Asthma; MAST, multiple-antigen simultaneous test; ECI-4, The Early Childhood Inventory-4; ADD, Attention deficit disorder; SDQ, Strengths and Difficulties Questionnaire; ICD-10, International Classification of Diseases, Tenth Revision; SCORAD, SCORing Atopic Dermatitis; ISAAC, International Study of Asthma and Allergies in Childhood; M.I.N.I. KID, Mini-International Neuropsychiatric Interview for Children and Adolescents; K-SADS-PL; Schedule for Affective Disorders and Schizophrenia for School-Aged Children—Present and Lifetime Version © Calculated from the available information in the article. *Statistically significant.
Three of the four studies reported a significant association between the comorbidity of ADHD and atopic diseases in patients with ADHD. Ten studies reported a significantly positive correlation among atopic diseases, sleep disturbance, and ADHD or an increased risk of ADHD in children with atopic diseases. One research group26 performed structural equation modeling to determine interactions among eczema, asthma, rhinitis, sleep, and behavior disorders. In three studies, the computerized comprehensive attention test (CAT) was performed, a more objective and precise measurement tool, to assess attention deficit, and they obtained results similar to those of other studies, thus supporting our hypothesis that atopy increased ADHD symptoms severity. In addition, eight studies examined treatment modalities for atopic diseases; however, additional randomized controlled trials are required to obtain more consistent results and causal relationships. The included studies evaluated several confounding factors such as age, sex, and atopic disease severity. Additional detailed information is provided in Table S1 in the Supplementary Materials.
Quantitative review and meta-analysis of cross-sectional studies
Sixteen studies including 25,337 participants examined the relationship between at least one type of atopic disease and the severity of total ADHD symptoms, hyperactivity/impulsivity or inattention, by including unexposed groups consisting of participants without atopic diseases. Table 2 lists the characteristics of included studies. Of the included studies, all studies were cross-sectional designs.
Table 2.
Studies examining the relationship between atopic diseases and hyperactivity in the meta-analysis.
| Study name | Country | Study design | Number of participants/Exposed group/unexposed group | Age (mean of the exposed group)/sex (male, %) | Diagnostic criteria for ADHD | Atopic disease/method used for assessing atopic diseases | Outcome scale | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|
| Yuksel et al. 200858 | Turkey | Cross-sectional | 100/62/38 | 7–12 years (9.2)/57% | DSM-IV | Asthma/physician’s diagnosis (GINA 2006) | Conner’s Parent Rating Scale | Included |
| Camfferman et al. 201026 | Australia | Cross-sectional | 107/77/30 | 6–16 years (9.9)/46.72% | Conner’s Parent Rating Scale-Revised | Atopic dermatitis/physician’s diagnosis (Hanifin and Rajka criteria) | Conner’s Parent Rating Scale | Included |
| Lee et al. 201462 | Republic of Korea | Cross-sectional | 160/87/73 | 6–13 years (8.49)/39.4% | DSM-IV | Allergic rhinitis/physician’s diagnosis (ARIA guideline) | ARS | Included |
| Yang et al. 201463 | Taiwan | Cross-sectional | 122/93/29 | 6–14 years (10.78)/52.2% | DSM-IV-TR | Allergic rhinitis/physician’s diagnosis (ARIA 2008) + IgE test (MAST or Phadiatop tests) | SNAP-IV (parent) | Included |
| Catal et al. 201664 | Turkey | Cross-sectional | 154/80/74 | 3–5 years | ECI-4 | Atopic dermatitis/physician’s diagnosis (Hanifin and Rajka criteria) | ECI-4 | Included |
| Hammer-Helmich et al. 201665 | Denmark | Cross-sectional | 9036/2433/6603 | 3–15 years (NA)/49.5% | SDQ | Eczema, asthma, and hay fever/Questionnaire | SDQ | Included |
| Yang et al. 201667 | Taiwan | Case–control | 99/68/31 | 6–14 years (9.25)/82.4% | DSM-IV | Allergic rhinitis/Physician’s diagnosis + IgE test (MAST or Phadiatop tests) | SNAP-IV (parent) | Included |
| Feng et al. 201768 | China | Cross-sectional | 643/248/320 | 6–12 years (9.25)/51.9% | DSM-IV | Allergic rhinitis/Physician’s diagnosis (ARIA 2008) + skin prick test | SNAP-IV | Included |
| Kuniyoshi et al. 201870 | Japan | Cross-sectional | 9954/1641/8313 | 7–14 years (10.42)/49.9% | SDQ | Eczema/ISAAC Eczema Symptom questionnaire | SDQ | Included |
| Schmitt et al. 20186 | Germany | Case–control | 89/35/45 | 6–12 years (9.9)/62.9% | ICD-10 | Atopic dermatitis/Dermatologist’s diagnosis (UK Working Party Criteria) | FBB-HKS | Included |
| Feng et al. 202074 | China | Cross-sectional | 273/89/184 | 6–12 years (8.3)/62.63% | SNAP-IV | Atopic dermatitis/Dermatologist’s diagnosis (UK criteria) | SNAP-IV | Included |
| Kuo et al. 202041 | Taiwan | Cross-sectional | 191/109/92 | (6.59)/54.44% | SNAP-IV | Atopic dermatitis, asthma, and allergic rhinitis/Physician’s diagnosis | SNAP-IV | “Seek further information” |
| Minatoya et al. 202079 | Japan | Cross-sectional | 3862/799/3063 | (5.28)/49.9% | SDQ | Atopic dermatitis/ISAAC | SDQ | Included |
| Berzosa-Grande et al. 202119 | Spain | Cross-sectional | 366/194/172 | 6–11 years (8.68)/52.7% | CBCL | Asthma, atopic dermatitis, allergic rhinitis/questionnaire | CBCL | Included |
| Özyurt et al. 202187 | Turkey | Cross-sectional | 121/61/60 | 12–18 years (14.27)/47.54% | SDQ | Asthma/GINA (2017) | SDQ | Included |
| Rajhans et al. 202188 | India | Cross-sectional | 60/30/30 | 8–15 years (11.92)/70% | M.I.N.I. KID, CBCL | Asthma/GINA (2015) | CBCL | Included |
ADHD, Attention-Deficit/Hyperactivity Disorder; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders; GINA 2006, Global Initiative for Asthma, 2006; ARIA, Allergic Rhinitis and its Impact on Asthma; ARS, ADHD Rating Score; MAST, multiple-antigen simultaneous test; ECI-4, The Early Childhood Inventory-4; SNAP-IV, Swanson, Nolan, and Pelham Questionnaire; SDQ, Strengths and Difficulties Questionnaire; CBCL, Child Behavior Checklist; M.I.N.I. KID, Mini-International Neuropsychiatric Interview for Children and Adolescents; ICD-10, International Classification of Diseases, Tenth Revision; FBB-HKS, The German ADHD Rating Scale.
Overview of total ADHD symptoms through a meta-analysis
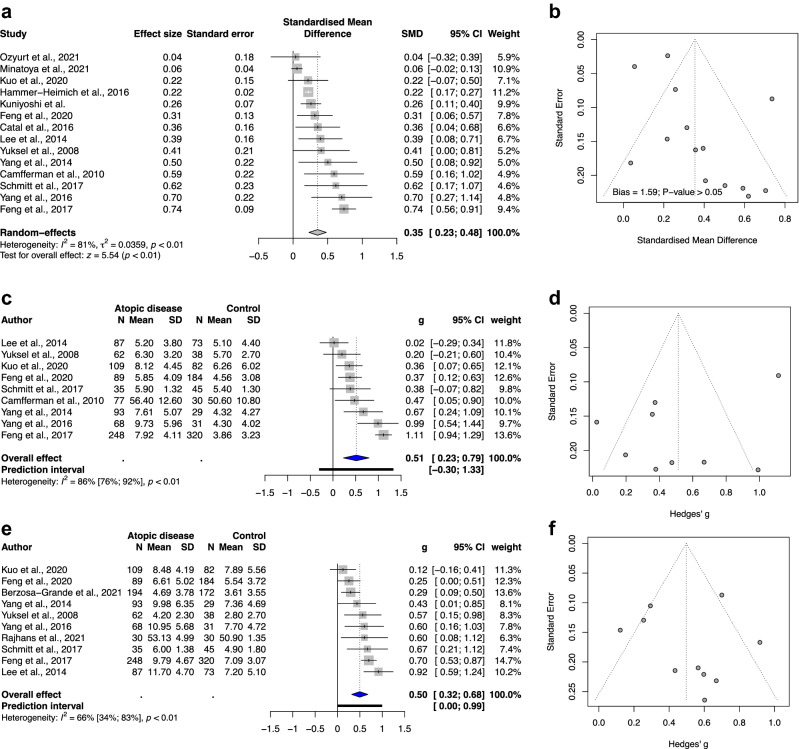
In terms of the outcome of total ADHD symptoms, the overall effect exhibited a statistically significant association with standardized mean difference (SMD) of 0.35, 95% CI of 0.23–0.48, and p value < 0.01 (Fig. 1a). We observed considerable heterogeneity among subgroups with an I2 value of 81%. The funnel plot displayed no asymmetry (p > 0.05; Fig. 1b).
Figure 1.
(a) Forest plot of the meta-analysis of the severity of total ADHD symptoms in childhood and the presence of atopic diseases. (b) Funnel plot of the meta-analysis of the severity of total ADHD symptoms in childhood and the presence of atopic diseases. (c) Forest plot of the meta-analysis of the severity of hyperactivity/impulsivity in childhood and the presence of atopic diseases. (d) Funnel plot of the meta-analysis of the severity of hyperactivity/impulsivity in childhood and the presence of atopic diseases. (e) Forest plot of the meta-analysis of the severity of inattention in childhood and the presence of atopic diseases. (f) Funnel plot of the meta-analysis of the severity of inattention in childhood and the presence of atopic diseases. Abbreviations: SD, standard deviation; CI, confidence interval; SMD, standardized mean difference.
Overview of hyperactivity/impulsivity through a meta-analysis
In terms of the outcome of hyperactivity/impulsivity, the overall effect showed a statistically significant association with atopic diseases, with SMD of 0.51, 95% CI: 0.23–0.79, and p value of 0.003 (Fig. 1c). Substantial to considerable heterogeneity was noted (I2 value: 86%). The funnel plot (Fig. 1d) and Egger’s test (Figure S1; p = 0.15) showed no significant publication bias.
Overview of inattention through a meta-analysis
The overall effect of the outcome of inattention showed a significant and positive correlation with atopic diseases, with SMD of 0.5, 95% CI: 0.32–0.68, and p value of 0.0002 (Fig. 1e). Different from the outcome of hyperactivity/impulsivity, substantial heterogeneity (I2 = 66%) was observed for the outcome of inattention. The funnel plot (Fig. 1f) and Egger’s test (Figure S2; p = 0.88) showed no statistically significant publication bias.
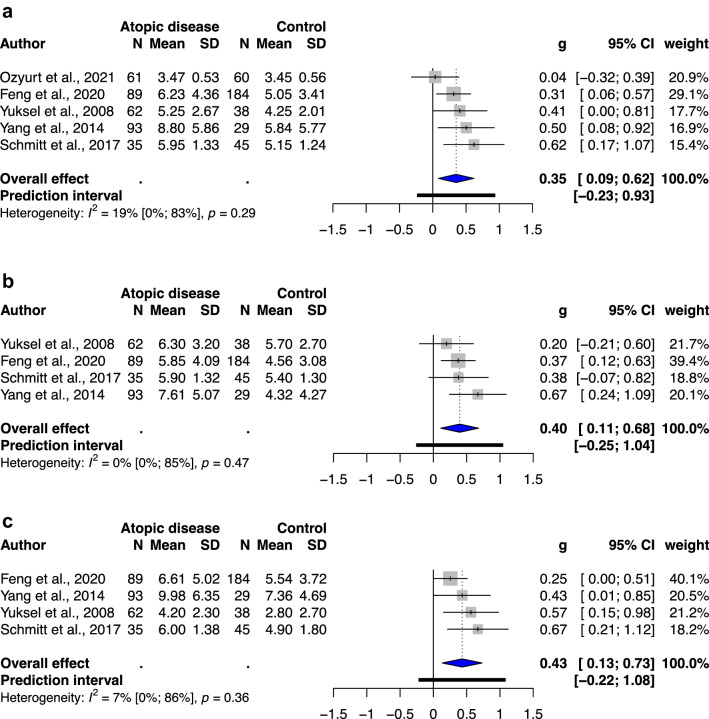
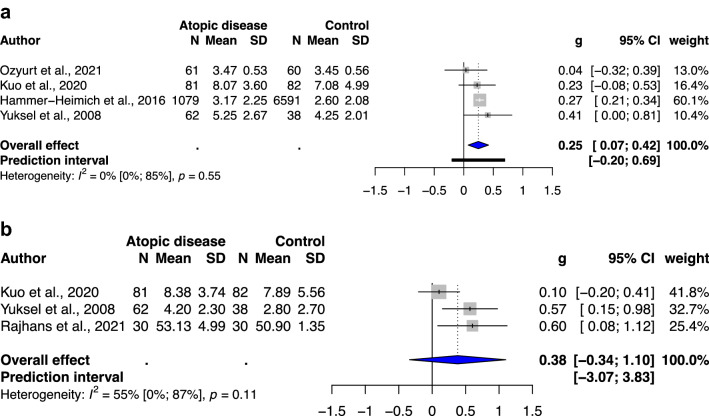
Meta-analysis of ADHD-related behavioral problems in atopic children without previous ADHD diagnosis
Five, four, and four studies included an atopic group without previous ADHD diagnosis and a healthy unexposed group to examine the outcomes of ADHD-related behavioral problems, which indicated total ADHD symptoms, hyperactivity/impulsivity, and inattention, respectively. All studies investigating total ADHD symptoms, hyperactivity/impulsivity, and inattention exhibited a statistically significant association, with SMD of 0.35(95% CI: 0.09–0.62, p value: 0.0212 (Fig. 2a)), SMD of 0.40(95% CI: 0.11–0.68, p value: 0.0212(Fig. 2b)), and SMD of 0.43(95% CI: 0.13–0.73, p value: 0.0193(Fig. 2c)), respectively. Low heterogeneity was noted in this meta-analysis (I2 = 0–19%).
Figure 2.
(a) Forest plot of the subgroup analysis of the severity of total ADHD symptoms in childhood and the presence of atopic diseases. (b) Forest plot of the subgroup analysis of the severity of hyperactivity/impulsivity in childhood and the presence of atopic diseases. (c) Forest plot of the subgroup analysis of the severity of inattention in childhood and the presence of atopic diseases. Abbreviations: CI, confidence interval; SMD, standardized mean difference.
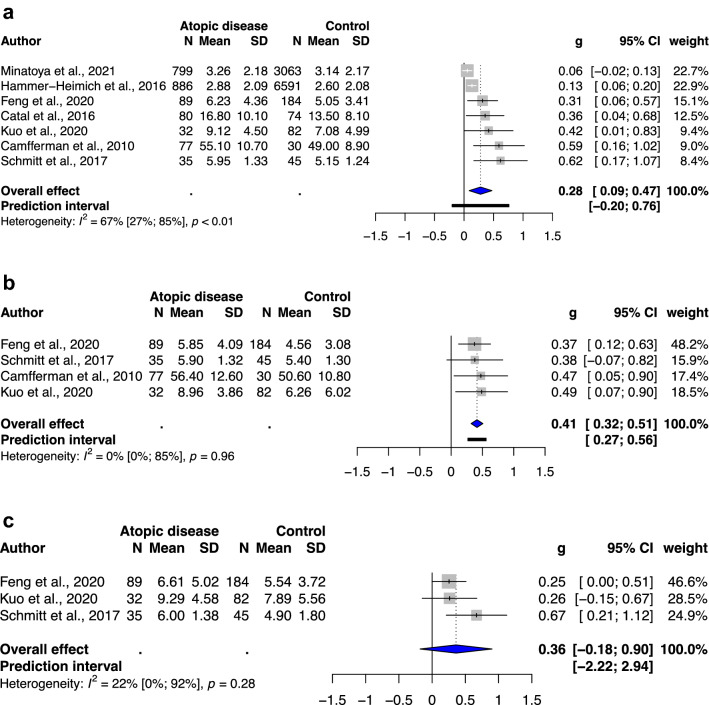
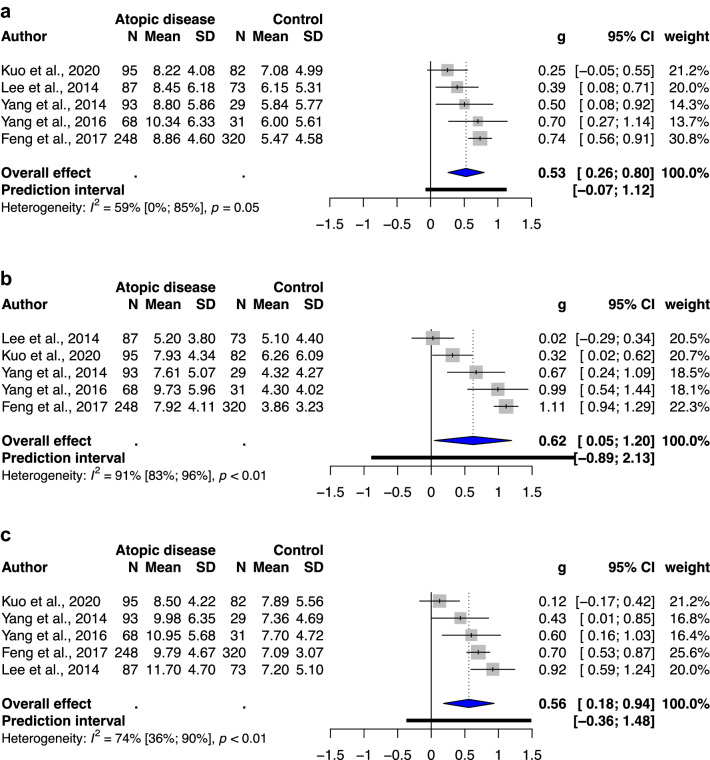
Subgroup analysis of different types of atopic diseases
A significant association was observed between atopic dermatitis and total ADHD symptoms (SMD: 0.28, 95% CI: 0.09–0.47, p value: 0.012) and hyperactivity/impulsivity (SMD: 0.41, 95% CI: 0.32–0.51, p value: 0.0008), with low to moderate heterogeneity (I2 = 0–67%; Fig. 3). A significant association was noted between allergic rhinitis and total ADHD symptoms (SMD: 0.53, 95% CI: 0.26–0.80, p value: 0.006), hyperactivity/impulsivity (SMD: 0.62, 95% CI: 0.05–1.20, p value: 0.04), and inattention (SMD: 0.56, 95% CI: 0.18–0.94, p value: 0.015), with moderate to substantial heterogeneity (I2 = 59–91%; Fig. 4). Furthermore, a significant association was observed between asthma and only total ADHD symptoms (SMD: 0.25, 95% CI: 0.07–0.42, p value: 0.02), with low to substantial heterogeneity (I2 = 0–55%; Fig. 5). The analysis of hyperactivity in children with asthma was not performed due to insufficient studies (n = 2).
Figure 3.
(a) Forest plot of the subgroup analysis of the severity of total ADHD symptoms in children with atopic dermatitis. (b) Forest plot of the subgroup analysis of the severity of hyperactivity/impulsivity in children with atopic dermatitis. (c) Forest plot of the subgroup analysis of the severity of inattention in children with atopic dermatitis. Abbreviations: CI, confidence interval; SMD, standardized mean difference.
Figure 4.
(a) Forest plot of the subgroup analysis of the severity of total ADHD symptoms in children with allergic rhinitis. (b) Forest plot of the subgroup analysis of the severity of hyperactivity/impulsivity in children with allergic rhinitis. (c) Forest plot of the subgroup analysis of the severity of inattention in children with allergic rhinitis. Abbreviations: CI, confidence interval; SMD, standardized mean difference.
Figure 5.
(a) Forest plot of the subgroup analysis of the severity of total ADHD symptoms in children with asthma. (b) Forest plot of the subgroup analysis of the severity of hyperactivity/impulsivity in children with asthma. (c) Forest plot of the subgroup analysis of the severity of inattention in children with asthma. Abbreviations: CI, confidence interval; SMD, standardized mean difference.
As sensitivity analysis, we observed decreased heterogeneity in meta-analysis of ADHD-related behavioral problems in children without previous ADHD diagnosis. However, in subgroups were categorized according to the types of atopic diseases, only the atopic dermatitis and asthma subgroup showed decreased heterogeneity (I2 = 0–67%), whereas allergic rhinitis subgroup showed low to considerable heterogeneity.
Discussion
The results of our study indicated that atopic diseases were related to not only increased odds of ADHD but also the severity of ADHD symptoms. Total ADHD symptoms, hyperactivity/impulsivity, and inattention were all significantly associated with atopic diseases. The results of the subgroup analysis indicated that children with subthreshold ADHD in the atopic disease groups had increased severity of ADHD symptoms, including total ADHD symptoms, hyperactivity/impulsivity, and inattention, and atopic dermatitis and allergic rhinitis were significantly associated with ADHD symptoms.
Although we included a small number of studies, these studies in total included more than 25,000 participants. In addition, this is the first systematic review and meta-analysis to investigate not only the association of atopic diseases with the severity of ADHD symptoms but also the presentation of ADHD-related behavioral symptoms in atopic children without previous ADHD diagnosis. The results of both the qualitative systematic review and meta-analysis tended to demonstrate higher severity of total ADHD symptoms and inattention in participants with atopic diseases, and the meta-analysis showed a significant association between atopic diseases and hyperactivity-impulsivity severity although qualitative synthesis showed relatively inconsistent outcome. Three studies that adopted the computerized CAT to assess attention deficits also demonstrated similar results, thus supporting our hypothesis. However, our qualitative systematic review and meta-analysis exhibited inconsistency in outcomes and considerable heterogeneity.
We performed a second meta-analysis of ADHD-related behavioral problems in atopic children without previous ADHD diagnosis, which not only consisted of studies with more strict exclusion criteria for diagnosed ADHD, but also reflected on the association between atopic diseases and subthreshold ADHD. The result showed statistical significance with low heterogeneity, indicating that atopic children was associated with subthreshold ADHD, as ADHD-related behavioral problems, despite of lack of diagnosed ADHD. The subgroup analysis of different types of atopic diseases showed that atopic dermatitis was significantly and positively correlated with the severity of total ADHD symptoms and hyperactivity/impulsivity, with low to moderate heterogeneity (I2 = 0–67%). Allergic rhinitis was significantly associated with the severity of total ADHD symptoms, hyperactivity/impulsivity, and inattention, with moderate to considerable heterogeneity (I2 = 59–91%). Asthma was significantly associated only with the severity of total ADHD symptoms, with low to substantial heterogeneity (I2 = 0–55%).
This inconsistency in heterogeneity can be attributed to differences in participants’ sex and mean age and the inclusion and exclusion criteria of related studies. A previous study reported a higher male to female ratio for hyperactivity but an equal male to female ratio for inattention27. This study also indicated that the distribution of sex differences within the severity of symptoms varied between children without ADHD and children with ADHD. The differences in the clinical course of participants can also result in these inconsistencies. Hyperactivity/impulsivity is usually observed from 4 years of age, peaks in severity at approximately 7 to 8 years, and then declines later, whereas inattention is not apparent until 8–9 years of age28. In this study, we observed a significantly decreased heterogeneity in the meta-analysis of ADHD-related behavioral problems in atopic children without previously diagnosed ADHD, indicating that inconsistent exclusion criteria for ADHD may have been the source of heterogeneity in our study. Moreover, the lack of standard inclusion and exclusion criteria for not only ADHD but also other neuropsychiatric disorders or developmental delays may be responsible for the high heterogeneity in our study. Furthermore, our results suggested that children with atopic diseases without previous ADHD diagnosis had a stronger association of more severe core symptoms of ADHD than healthy unexposed groups, indicating a more consistent result for inattention than hyperactivity/impulsivity, with remarkably decreased heterogeneity.
We also observed low to considerable heterogeneity in the subgroup analysis of different types of atopic diseases. Asthma had a significant association only with the severity of total ADHD symptoms, not with inattention. Considering that previous studies have reported that children with asthma had an increased risk of developing severe ADHD symptoms18,22,29, this result may be attributed to the small number of included studies (n = 3). The results of the subgroup analysis of different types of atopic diseases indicated that all atopic diseases were significantly associated with the severity of total ADHD symptoms; however, inconsistent heterogeneity was observed in the association between atopic diseases and the severity of hyperactivity/impulsivity and inattention. These findings suggest that different types of atopic diseases may have distinct interactions with ADHD symptoms, although our results demonstrated that any type of atopic disease was associated with the severity of ADHD symptoms.
Although the causal relationship and mechanism underlying the association between atopic diseases and ADHD remain unclear, many studies have provided several hypotheses30) (Figure S3). One of the more commonly accepted hypotheses is that atopic diseases induce inflammation, including Th1, Th2, and Th17 immune responses, which lead to the downstream hypersecretion of IgE31–33 (Figure S4). These inflammatory factors may affect the neuroactivity of the prefrontal cortex (PFC) and anterior cingulate cortex (ACC) that have been reported to be strongly associated with ADHD pathology34–36. This process affects the maturation of the PFC and ACC, which usually occurs in early life when the brain is undergoing profound changes and is important for the development of cognitive function37. In addition to the direct effect, cytokines may indirectly affect these brain areas by disturbing the hypothalamic–pituitary–adrenal axis (HPA) axis38, altering the central metabolism of neurotransmitters including norepinephrine and dopamine35,39.
In addition to neuroimmunological pathways, psychological mechanisms should also be considered. Atopic diseases cause psychological stress in not only patients but also their main caregivers since early childhood when the onset of atopic diseases occurs40,41. An unsatisfactory parent–child relationship characterized by overprotection, anxiety, low support, and poor sleep quality can lead to a decline in psychosocial and cognitive performance due to tiredness; emotional problems were reported to be associated with negative outcomes in a previous study42. Although the relationship between these effects and brain development in early life has not yet been well studied, stress in early childhood is believed to affect the balance between neurotransmitters and neuroendocrine systems, including norepinephrine, dopamine, and the HPA axis38,43. This eventually resulted in increased vulnerability to psychological diseases, such as ADHD, because of altered neuropsychologic pathways leading to unsuccessful brain development and maturation44.
An increased risk of the development and progression of atopic diseases was observed in children with ADHD because atopic diseases are attributed to stress45. Although these mechanisms were obscure, studies have found that stress may induce deficits in skin barriers, and a similar inflammatory cascade with atopy-associated immune responses was observed in patients with atopic diseases; some patients exhibited an increased tendency to exhibit Th1 responses46. These findings indicate that stress can exacerbate atopic diseases. ADHD was reported to be related to psychosocial stress because poor family support, school performance, and peer relationships can all be the sources of stress47. Therefore, ADHD-related stress can exacerbate atopic diseases. Recently, genetic factors and prenatal stress have been indicated as common risk factors for atopic diseases and ADHD. Although few studies have evaluated genetic susceptibility and other associated interaction factors leading to epigenetic reactions48,49, a twin study supported the hypothesis that common genetic factors between atopy and ADHD exist50. Moreover, studies reporting a relationship between maternal stress and symptoms of atopic diseases and ADHD have indicated that dysregulation of the HPA axis results in delayed brain development and a shift in Th1/Th2 balance, resulting in an atopic disease–prone immune profile51,52.
Previous systematic reviews and meta-analyses had discussed about increased risk of diagnosed ADHD in atopic group; however, the evidence of whether atopic diseases associated with increased severity of ADHD symptoms in participants with subthreshold ADHD remained unclear. This association could be observed in the meta-analysis of ADHD-related behavioral problems in atopic children without previously diagnosed ADHD in the present study, provided an evidence that atopic diseases are associated with “spectrum of ADHD symptom severity”, the term which we quoted following a previous study to explain how atopic diseases associated with ADHD symptoms53, and this association existed in subthreshold ADHD group in our result as well.
Limitations
This study has several limitations that should be considered. First, although more than 25,000 participants were included, the outcome of hyperactivity was examined in only 1700 participants, which may reduce the strength of evidence. Second, Atopic diseases were diagnosed based on physicians’ decisions or by using some questionnaires in the included studies; these might have caused heterogeneity. Third, we chose to combine scores of hyperactivity/impulsivity and inattention as the primary outcome, and this method has been used in several studies54. However, potential systematic errors may still occur. Forth, differences in exclusion criteria, including the exclusion of patients with ADHD and other neuropsychiatric disorders and development problems, caused significant heterogeneity in our study. Finally, some studies included children with multiple atopic diseases, which may be potential confounding factors in our study.
To minimize the effect of those limitations, we conducted sensitivity analysis and subgroup analysis to assess the effects of potential confounding factors, namely different types of atopic diseases and exclusion criteria for previous diagnosed ADHD and other neuropsychiatric disorders; this considerably reduced heterogeneity in sensitivity analysis and most subgroup analyses. Therefore, standardized and more strictly defined exclusion and inclusion criteria should be included in future studies. Moreover, additional studies investigating the relationship between different types of atopic diseases and ADHD symptoms should be conducted because we could not conduct a complete subgroup analysis of different atopic diseases owing to the limited number of studies.
Conclusion
Our study results indicated that atopic diseases not only increased the odds of ADHD but also were associated with more severe core symptoms of ADHD. We observed increased severity of ADHD-related behavioral symptoms in children with atopic diseases without previously diagnosed ADHD, indicating that atopic diseases may also associated with spectrum of ADHD symptom severity in participants with subthreshold ADHD, which was never been investigated in previous researches. According to the results of this study, while treating children with ADHD, clinicians should consider the possibility of comorbid atopic diseases. On the other hand, the comorbidity of ADHD should be considered when treating children with atopic diseases. Moreover, clinicians should be aware of the increased ADHD-related behavioral symptoms in children with atopic diseases. Additional studies including more strictly defined criteria, studies investigating the mechanism underlying this association, and randomized controlled trials of related therapeutic strategies should be conducted.
Methods
This systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines55. Related checklists are provided in the Supplementary Materials. Two researchers searched for and pooled observational studies examining atopic diseases and ADHD symptom severity to examine the association between them.
Eligibility criteria for study selection
To reduce selection bias, we defined eligibility criteria before the inclusion of studies. We included the following studies: (1) observational studies investigating the association between one of the three major types of atopic diseases (i.e., asthma, eczema, and allergic rhinitis) and the severity of ADHD symptoms, irrespective of whether they included patients with ADHD in the exposed group; (2) studies recruiting children and adolescents; (3) studies including any of the three atopic diseases as the exposure variable and ADHD symptom severity (scores of a behavior rating scale) as the outcome variable; (4) studies investigating the severity of ADHD symptoms in patients with at least one type of atopic disease by using any type of assessment method; (5) studies including a matched or an unmatched unexposed group for comparison with the exposed group; and (6) cross-sectional, case–control, or cohort studies. The following studies were excluded: (1) studies that did not provide adequate information regarding the relationship between atopic diseases and ADHD symptom severity, including the crude data of exposed cases and the outcome of the association between at least one type of atopic disease and the severity of hyperactivity/impulsivity, inattention, and/or total ADHD symptoms (hyperactivity/impulsivity + inattention) determined on the basis of the scores of a behavior rating scale; (2) studies including only outcomes measured after interventions or those not including a separate outcome of total ADHD symptoms, hyperactivity/impulsivity, and inattention; (3) studies using the same database in different published articles (studies with longer follow-up periods and higher quality, which were classified as included (see ‘Table S2 in the Supplementary Materials’) were included); and (4) studies whose full texts were not available or those for which only abstracts or editorial materials (i.e., comments, responses, and letters without original data) were available.
Search strategy and study selection
Two authors performed a literature search on PubMed (Medline), Embase, and Psycinfo for studies published up to December 18, 2021. The following search terms were combined and adjusted to fulfill the demand of the database.
“Atopic eczema” [MeSH] OR “atopic dermatitis” [MeSH] OR “asthma” [MeSH] OR “allergic rhinitis” [MeSH]
“ADHD” [MeSH] OR “attention deficit and hyperactivity disorder” [MeSH] OR “hyperactivity” [MeSH] OR “inattention” [MeSH] OR “attention deficit” [Mesh] OR “impulsivity’ [Mesh] OR “mental health” [MeSH] OR “behavior problem” [MeSH]
“Preschool children” OR “preschooler” OR “children” OR “adolescent” OR “toddler”
A three-step screening strategy was adopted. In the title screening step, studies that met the inclusion criteria and were not letters or replies were included. In the abstract screening step, studies that were original research and included relevant unexposed groups were included. In the full-text screening step, studies for which full texts and data were available and those that did not meet the exclusion criteria were finally included. A third author resolved any disagreement between the two authors in terms of the eligibility and inclusion of studies through discussion.
Data extraction
By using a customized data form, the first author extracted the following information from eligible studies: study title, study design, study characteristics (country, composition of participants, and outcome assessment scales used), and assessment methods and criteria for diagnosing atopic diseases and ADHD. Subsequently, the second author reviewed the extracted data. Any disagreement regarding data extraction was resolved by the third author through discussion. If required, data were calculated from the available data of included studies (see ‘Data abstraction for the meta-analysis’). The main outcome variables were the scores of the behavior rating scales used to evaluate hyperactivity/impulsivity and inattention in the atopic disease and unexposed groups. Although the included studies used different outcome scales, they were all based on the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) criteria. In addition, to minimize the potential confounding effects, we analyzed standardized data. Because of the limited availability of studies, we combined the three types of atopic diseases in the meta-analysis and conducted a subgroup analysis. The authors individually recorded abstracted data in Microsoft Excel.
Data abstraction for the meta-analysis
The relationship between one of the three main types of atopic diseases with the severity of hyperactivity/impulsivity, inattention, or total ADHD symptoms was independently investigated. To exclude confounding factors, any study including outcomes measured after interventions were excluded. For each study, the relative weight of outcome data to the whole data set was calculated using the generic inverse variance method along with the 95% confidence interval (95% CI) by using Rstudio software, Version 1.2.5042 Rstudio56. The random effects model with the Hartung–Knapp–Sidik–Jonkman method was used to determine the estimated variance for pooling effect sizes in our meta-analysis, with standardized mean difference as effect size. The I2 value was calculated to assess statistical heterogeneity, and this value represents the total variance of pooled data explained by the heterogeneity. According to the Cochrane handbook for systematic reviews of interventions, the I2 values of 0–40%, 30–60%, 50–90%, and 75–100% indicated low, moderate, substantial, and considerable heterogeneity57. We used a funnel plot to assess the potential publication bias.
For the outcome “severity of total ADHD symptoms,” if a study reported ADHD symptoms in “severity of hyperactivity/impulsivity” and “severity of inattention” separately, we calculated weighted mean and pooled standard deviation based on relevant formula before meta-analysis57.
For studies including a subgroup analysis, we pooled effect sizes two times. First, we combined subgroups within studies to pool effect sizes and calculated 95% CIs and standard errors. Subsequently, we included the calculated standard errors into our meta-analysis and pooled effect sizes a second time.
Sensitivity analysis
To assess the strength of the association between atopic diseases and ADHD in different scenarios, we performed a sensitivity analysis by investigating patients with strictly defined exclusion criteria for previous ADHD diagnosis. We included studies researching both exposed and unexposed groups with exclusion criteria for previous ADHD diagnosis for a second meta-analysis, which was mentioned as meta-analysis of ADHD-related behavioral problems in atopic children without previous ADHD diagnosis. Detailed information on the risk of bias assessment could be found in Table S2 in the Supplementary Materials.
Subgroup analysis of different type of atopic diseases
We conducted subgroup analysis of different type of atopic diseases in three outcomes: total ADHD symptoms, hyperactivity, and inattention, using a random effect model. If there were less than 3 studies included in each subgroup, we would not perform analysis.
Supplementary Information
Acknowledgements
We would like to acknowledge Yi-No Kang for his help and useful suggestions related to statistical measurements. This manuscript was edited by Wallace Academic Editing.
Author contributions
Conceived and designed the experiments: Yu-chieh Chuang, Yu-Jui Huang, Yang-Ching Chen /Analyzed the data: Yu-Chieh Chuang, Liang-Jen Wang, Yang-Ching Chen /Wrote the paper: Yu-Chieh Chuang, Yu-Jui Huang, Wei-Lieh Huang /Data acquisition, analysis and interpretation; manuscript drafting, editing and submission: Wei-Lieh Huang, Ching-Yun Wang, Ho-Chang Kuo /Abstracts review, evaluation of inclusion criteria and bias analysis: Wei-Lieh Huang, Ching-Yun Wang, Ho-Chang Kuo /All authors reviewed the manuscript.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-07232-1.
References
- 1.Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Lancet351, 1225–1232 (1998). [PubMed]
- 2.Asher MI, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–743. doi: 10.1016/s0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 3.Schmitt J, et al. Infant eczema, infant sleeping problems, and mental health at 10 years of age: the prospective birth cohort study LISAplus. Allergy. 2011;66:404–411. doi: 10.1111/j.1398-9995.2010.02487.x. [DOI] [PubMed] [Google Scholar]
- 4.Stanescu S, Kirby SE, Thomas M, Yardley L, Ainsworth B. A systematic review of psychological, physical health factors, and quality of life in adult asthma. NPJ Prim Care Respir Med. 2019;29:37. doi: 10.1038/s41533-019-0149-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferrante G, La Grutta S. The Burden of Pediatric Asthma. Front Pediatr. 2018;6:186. doi: 10.3389/fped.2018.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmitt J, et al. Increased attention-deficit/hyperactivity symptoms in atopic dermatitis are associated with history of antihistamine use. Allergy. 2018;73:615–626. doi: 10.1111/all.13326. [DOI] [PubMed] [Google Scholar]
- 7.Hill MK, Kheirandish Pishkenari A, Braunberger TL, Armstrong AW, Dunnick CA. Recent trends in disease severity and quality of life instruments for patients with atopic dermatitis: A systematic review. J. Am. Acad. Dermatol. 2016;75:906–917. doi: 10.1016/j.jaad.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 8.O'Connell EJ. The burden of atopy and asthma in children. Allergy. 2004;59(Suppl 78):7–11. doi: 10.1111/j.1398-9995.2004.00563.x. [DOI] [PubMed] [Google Scholar]
- 9.Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int. J. Epidemiol. 2014;43:434–442. doi: 10.1093/ije/dyt261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hinshaw SP. Attention Deficit Hyperactivity Disorder (ADHD): Controversy, developmental mechanisms, and multiple levels of analysis. Annu. Rev. Clin. Psychol. 2018;14:291–316. doi: 10.1146/annurev-clinpsy-050817-084917. [DOI] [PubMed] [Google Scholar]
- 11.Bozhilova NS, Michelini G, Kuntsi J, Asherson P. Mind wandering perspective on attention-deficit/hyperactivity disorder. Neurosci. Biobehav. Rev. 2018;92:464–476. doi: 10.1016/j.neubiorev.2018.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fayyad J, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br. J. Psychiatry. 2007;190:402–409. doi: 10.1192/bjp.bp.106.034389. [DOI] [PubMed] [Google Scholar]
- 13.Barkley RA, Fischer M, Smallish L, Fletcher K. The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. J. Abnorm. Psychol. 2002;111:279–289. doi: 10.1037/0021-843X.111.2.279. [DOI] [PubMed] [Google Scholar]
- 14.Pelham WE, et al. The long-term financial outcome of children diagnosed with ADHD. J. Consult. Clin. Psychol. 2020;88:160–171. doi: 10.1037/ccp0000461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGee R, Stanton WR, Sears MR. Allergic disorders and attention deficit disorder in children. J. Abnorm. Child. Psychol. 1993;21:79–88. doi: 10.1007/bf00910490. [DOI] [PubMed] [Google Scholar]
- 16.Kaas TH, et al. Association between childhood asthma and attention deficit hyperactivity or autism spectrum disorders: A systematic review with meta-analysis. Clin. Exp. Allergy. 2021;51:228–252. doi: 10.1111/cea.13750. [DOI] [PubMed] [Google Scholar]
- 17.Deckert S, Kopkow C, Schmitt J. Nonallergic comorbidities of atopic eczema: an overview of systematic reviews. Allergy. 2014;69:37–45. doi: 10.1111/all.12246. [DOI] [PubMed] [Google Scholar]
- 18.Borschuk AP, Rodweller C, Salorio CF. The influence of comorbid asthma on the severity of symptoms in children with attention-deficit hyperactivity disorder. J. Asthma. 2018;55:66–72. doi: 10.1080/02770903.2017.1306549. [DOI] [PubMed] [Google Scholar]
- 19.Berzosa-Grande MP, González-Fraile E, Sánchez-López R, Soria-Oliver M, Rueda-Esteban S. The relationship between allergic diseases and internalising and externalising behaviours in Spanish children: A cross-sectional study. Allergol. Immunopathol. (Madr) 2021;49:65–72. doi: 10.15586/aei.v49i3.78. [DOI] [PubMed] [Google Scholar]
- 20.Hong SB, et al. Subthreshold attention-deficit/hyperactivity disorder is associated with functional impairments across domains: A comprehensive analysis in a large-scale community study. Eur. Child Adolesc. Psychiatry. 2014;23:627–636. doi: 10.1007/s00787-013-0501-z. [DOI] [PubMed] [Google Scholar]
- 21.Schmitt J, Apfelbacher C, Heinrich J, Weidinger S, Romanos M. Association of atopic eczema and attention-deficit/hyperactivity disorder - meta-analysis of epidemiologic studies. Z. Kinder Jugendpsychiatr. Psychother. 2013;41:35–42. doi: 10.1024/1422-4917/a000208. [DOI] [PubMed] [Google Scholar]
- 22.Schans JV, Çiçek R, de Vries TW, Hak E, Hoekstra PJ. Association of atopic diseases and attention-deficit/hyperactivity disorder: A systematic review and meta-analyses. Neurosci. Biobehav. Rev. 2017;74:139–148. doi: 10.1016/j.neubiorev.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 23.He JP, Burstein M, Schmitz A, Merikangas KR. The Strengths and Difficulties Questionnaire (SDQ): the factor structure and scale validation in U.S. adolescents. J. Abnorm. Child Psychol. 2013;41:583–595. doi: 10.1007/s10802-012-9696-6. [DOI] [PubMed] [Google Scholar]
- 24.Algorta GP, Dodd AL, Stringaris A, Youngstrom EA. Diagnostic efficiency of the SDQ for parents to identify ADHD in the UK: A ROC analysis. Eur. Child Adolesc. Psychiatry. 2016;25:949–957. doi: 10.1007/s00787-015-0815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vugteveen J, De Bildt A, Hartman CA, Timmerman ME. Using the Dutch multi-informant Strengths and Difficulties Questionnaire (SDQ) to predict adolescent psychiatric diagnoses. Eur. Child Adolesc. Psychiatry. 2018;27:1347–1359. doi: 10.1007/s00787-018-1127-y. [DOI] [PubMed] [Google Scholar]
- 26.Camfferman D, et al. Eczema, sleep, and behavior in children. J Clin Sleep Med. 2010;6:581–588. doi: 10.5664/jcsm.27992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mowlem FD, et al. Sex differences in predicting ADHD clinical diagnosis and pharmacological treatment. Eur. Child Adolesc. Psychiatry. 2019;28:481–489. doi: 10.1007/s00787-018-1211-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Applegate B, et al. Validity of the age-of-onset criterion for ADHD: a report from the DSM-IV field trials. J. Am. Acad. Child Adolesc. Psychiatry. 1997;36:1211–1221. doi: 10.1097/00004583-199709000-00013. [DOI] [PubMed] [Google Scholar]
- 29.Kaas TH, et al. Association between childhood asthma and attention deficit hyperactivity or autism spectrum disorders: A systematic review with meta-analysis. Clin. Exp. Allergy. 2020 doi: 10.1111/cea.13750. [DOI] [PubMed] [Google Scholar]
- 30.Buske-Kirschbaum A, et al. Psychoendocrine and psychoneuroimmunological mechanisms in the comorbidity of atopic eczema and attention deficit/hyperactivity disorder. Psychoneuroendocrinology. 2013;38:12–23. doi: 10.1016/j.psyneuen.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 31.Czarnowicki T, et al. Early pediatric atopic dermatitis shows only a cutaneous lymphocyte antigen (CLA)(+) TH2/TH1 cell imbalance, whereas adults acquire CLA(+) TH22/TC22 cell subsets. J. Allergy Clin. Immunol. 2015;136:941–951.e943. doi: 10.1016/j.jaci.2015.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Czarnowicki T, et al. Evolution of pathologic T-cell subsets in patients with atopic dermatitis from infancy to adulthood. J. Allergy Clin. Immunol. 2020;145:215–228. doi: 10.1016/j.jaci.2019.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Looman KIM, et al. Associations of Th2, Th17, Treg cells, and IgA(+) memory B cells with atopic disease in children: The Generation R Study. Allergy. 2020;75:178–187. doi: 10.1111/all.14010. [DOI] [PubMed] [Google Scholar]
- 34.Puiu AA, et al. Impulsive aggression and response inhibition in attention-deficit/hyperactivity disorder and disruptive behavioral disorders: Findings from a systematic review. Neurosci. Biobehav. Rev. 2018;90:231–246. doi: 10.1016/j.neubiorev.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 35.Xing B, Li YC, Gao WJ. Norepinephrine versus dopamine and their interaction in modulating synaptic function in the prefrontal cortex. Brain Res. 2016;1641:217–233. doi: 10.1016/j.brainres.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim JI, et al. Interaction between DRD2 and lead exposure on the cortical thickness of the frontal lobe in youth with attention-deficit/hyperactivity disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2018;82:169–176. doi: 10.1016/j.pnpbp.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 37.Hiser J, Koenigs M. The multifaceted role of the ventromedial prefrontal cortex in emotion, decision making, social cognition, and psychopathology. Biol. Psychiatry. 2018;83:638–647. doi: 10.1016/j.biopsych.2017.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Buske-Kirschbaum A, et al. Altered hypothalamus-pituitary-adrenal axis function: A relevant factor in the comorbidity of atopic eczema and attention deficit/hyperactivity disorder? Psychoneuroendocrinology. 2019;105:178–186. doi: 10.1016/j.psyneuen.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 39.Park G, Jung YS, Park MK, Yang CH, Kim YU. Melatonin inhibits attention-deficit/hyperactivity disorder caused by atopic dermatitis-induced psychological stress in an NC/Nga atopic-like mouse model. Sci. Rep. 2018;8:14981. doi: 10.1038/s41598-018-33317-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xu YC, Wang JP, Zhu WJ, Li P. Childhood atopic dermatitis as a precursor for developing attention deficit/hyperactivity disorder. Int. J. Immunopathol. Pharmacol. 2020;34:2058738420962902. doi: 10.1177/2058738420962902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kuo HC, Chang LS, Tsai ZY, Wang LJ. Allergic diseases do not impair the cognitive development of children but do damage the mental health of their caregivers. Sci. Rep. 2020;10:13854. doi: 10.1038/s41598-020-70825-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chamlin SL, Frieden IJ, Williams ML, Chren MM. Effects of atopic dermatitis on young American children and their families. Pediatrics. 2004;114:607–611. doi: 10.1542/peds.2004-0374. [DOI] [PubMed] [Google Scholar]
- 43.Nicolaides NC, Kyratzi E, Lamprokostopoulou A, Chrousos GP, Charmandari E. Stress, the stress system and the role of glucocorticoids. NeuroImmunoModulation. 2015;22:6–19. doi: 10.1159/000362736. [DOI] [PubMed] [Google Scholar]
- 44.McCrory E, De Brito SA, Viding E. Research review: the neurobiology and genetics of maltreatment and adversity. J. Child Psychol. Psychiatry. 2010;51:1079–1095. doi: 10.1111/j.1469-7610.2010.02271.x. [DOI] [PubMed] [Google Scholar]
- 45.Lin TK, Zhong L, Santiago JL. Association between Stress and the HPA Axis in the Atopic Dermatitis. Int J Mol Sci. 2017;18:2131. doi: 10.3390/ijms18102131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Buske-Kirschbaum A, Gierens A, Höllig H, Hellhammer DH. Stress-induced immunomodulation is altered in patients with atopic dermatitis. J. Neuroimmunol. 2002;129:161–167. doi: 10.1016/s0165-5728(02)00168-6. [DOI] [PubMed] [Google Scholar]
- 47.Quinlan EB, et al. Psychosocial stress and brain function in adolescent psychopathology. Am. J. Psychiatry. 2017;174:785–794. doi: 10.1176/appi.ajp.2017.16040464. [DOI] [PubMed] [Google Scholar]
- 48.Lau M, et al. Loss of STAT6 promotes autoimmune disease and atopy on a susceptible genetic background. J. Autoimmun. 2012;39:388–397. doi: 10.1016/j.jaut.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 49.Tsai SJ. Signal transducer and activator of transcription 6 (STAT6) and attention-deficit hyperactivity disorder: A speculative hypothesis. Med. Hypotheses. 2006;67:1342–1344. doi: 10.1016/j.mehy.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 50.Wamboldt MZ, et al. Familial association between allergic disorders and depression in adult Finnish twins. Am. J. Med. Genet. 2000;96:146–153. doi: 10.1002/(sici)1096-8628(20000403)96:2<146::aid-ajmg4>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 51.Van den Bergh BRH, et al. Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neurosci. Biobehav. Rev. 2017 doi: 10.1016/j.neubiorev.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 52.Cowell WJ, Bellinger DC, Wright RO, Wright RJ. Antenatal active maternal asthma and other atopic disorders is associated with ADHD behaviors among school-aged children. Brain Behav. Immun. 2019;80:871–878. doi: 10.1016/j.bbi.2019.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Roigé-Castellví J, et al. Prenatal and perinatal factors associated with ADHD risk in schoolchildren: EPINED epidemiological study. Eur. Child Adolesc. Psychiatry. 2020 doi: 10.1007/s00787-020-01519-2. [DOI] [PubMed] [Google Scholar]
- 54.Sun CK, et al. Therapeutic effects of methylphenidate for attention-deficit/hyperactivity disorder in children with borderline intellectual functioning or intellectual disability: A systematic review and meta-analysis. Sci. Rep. 2019;9:15908. doi: 10.1038/s41598-019-52205-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Moher D, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.RStudio: Integrated Development for R. (2020).
- 57.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 58.Yuksel H, Sogut A, Yilmaz O. Attention deficit and hyperactivity symptoms in children with asthma. J. Asthma. 2008;45:545–547. doi: 10.1080/02770900801990016. [DOI] [PubMed] [Google Scholar]
- 59.Chang HY, et al. Allergic diseases in preschoolers are associated with psychological and behavioural problems. Allergy Asthma Immunol. Res. 2013;5:315–321. doi: 10.4168/aair.2013.5.5.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Goodwin RD, et al. Severity and persistence of asthma and mental health: a birth cohort study. Psychol. Med. 2013;43:1313–1322. doi: 10.1017/s0033291712001754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim DK, et al. Treatment of allergic rhinitis is associated with improved attention performance in children: the Allergic Rhinitis Cohort Study for Kids (ARCO-Kids) PLoS ONE. 2014;9:e109145. doi: 10.1371/journal.pone.0109145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee YS, et al. Attention deficit hyperactivity disorder like behavioral problems and parenting stress in pediatric allergic rhinitis. Psychiatry Investig. 2014;11:266–271. doi: 10.4306/pi.2014.11.3.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yang MT, et al. Hyperactivity and impulsivity in children with untreated allergic rhinitis: Corroborated by rating scale and continuous performance test. Pediatr. Neonatol. 2014;55:168–174. doi: 10.1016/j.pedneo.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 64.Catal F, et al. Psychiatric disorders and symptoms severity in preschool children with atopic eczema. Allergol. Immunopathol. 2016;44:120–124. doi: 10.1016/j.aller.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 65.Hammer-Helmich L, et al. Mental health associations with eczema, asthma and hay fever in children: a cross-sectional survey. BMJ Open. 2016;6:e012637. doi: 10.1136/bmjopen-2016-012637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Strom MA, Fishbein AB, Paller AS, Silverberg JI. Association between atopic dermatitis and attention deficit hyperactivity disorder in U.S. children and adults. Br. J. Dermatol. 2016;175:920–929. doi: 10.1111/bjd.14697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yang MT, et al. Attention-deficit/hyperactivity disorder-related symptoms improved with allergic rhinitis treatment in children. Am. J. Rhinol. Allergy. 2016;30:209–214. doi: 10.2500/ajra.2016.30.4301. [DOI] [PubMed] [Google Scholar]
- 68.Feng B, et al. Association of pediatric allergic rhinitis with the ratings of attention-deficit/hyperactivity disorder. Am. J. Rhinol. Allergy. 2017;31:161–167. doi: 10.2500/ajra.2017.31.4439. [DOI] [PubMed] [Google Scholar]
- 69.Abd El-Hamid ZB, et al. Impact of allergy on children with attention deficit hyperactivity disorder. Eur. Ann. Allergy Clin. Immunol. 2018;50:262–267. doi: 10.23822/EurAnnACI.1764-1489.72. [DOI] [PubMed] [Google Scholar]
- 70.Kuniyoshi Y, et al. Severity of eczema and mental health problems in Japanese schoolchildren: The ToMMo Child Health Study. Allergol. Int. 2018;67:481–486. doi: 10.1016/j.alit.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 71.Kruse LL, Cices A, Fishbein AB, Paller AS. Neurocognitive function in moderate-severe pediatric atopic dermatitis: A case-control study. Pediatr. Dermatol. 2019;36:110–114. doi: 10.1111/pde.13710. [DOI] [PubMed] [Google Scholar]
- 72.Tajdini M, et al. Associations of behavioral disorders with asthma in Iranian children. Iran J. Allergy Asthma Immunol. 2019;18:340–345. doi: 10.18502/ijaai.v18i3.1127. [DOI] [PubMed] [Google Scholar]
- 73.Zhou H, Chen Z, Zhao W, Liu Y, Cui Y. Evaluation of neuropsychiatric comorbidities and their clinical characteristics in Chinese children with asthma using the MINI kid tool. BMC Pediatr. 2019;19:454. doi: 10.1186/s12887-019-1834-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Feng LJ, Chen AW, Luo XY, Wang H. Increased attention deficit/hyperactivity and oppositional defiance symptoms of 6–12 years old Chinese children with atopic dermatitis. Medicine (Baltimore) 2020;99:e20801. doi: 10.1097/MD.0000000000020801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fuhrmann S, Tesch F, Romanos M, Abraham S, Schmitt J. ADHD in school-age children is related to infant exposure to systemic H1-antihistamines. Allergy. 2020;75:2956–2957. doi: 10.1111/all.14411. [DOI] [PubMed] [Google Scholar]
- 76.Guo MM, Wang LJ, Hsu TY, Yang KD, Kuo HC. Peanut sensitivity and allergic rhinitis in young children are associated with attention-deficit hyperactivity disorder symptoms in adolescence. Neuropsychiatr. Dis. Treat. 2020;16:1349–1357. doi: 10.2147/NDT.S232299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Huang AH, et al. Real-world comorbidities of atopic dermatitis in the pediatric ambulatory population in the United States. J. Am. Acad. Dermatol. 2021 doi: 10.1016/j.jaad.2021.03.016. [DOI] [PubMed] [Google Scholar]
- 78.Jackson-Cowan L, Cole EF, Silverberg JI, Lawley LP. Childhood atopic dermatitis is associated with cognitive dysfunction: A National Health Interview Survey study from 2008 to 2018. Ann. Allergy Asthma Immunol. 2021;126:661–665. doi: 10.1016/j.anai.2020.11.008. [DOI] [PubMed] [Google Scholar]
- 79.Minatoya M, Suyama S, Kishi R. Relationship between atopic dermatitis and children's mental and behavioral health: The Hokkaido Study. Nihon Koshu Eisei Zasshi. 2020;67:745–751. doi: 10.11236/jph.67.10_745. [DOI] [PubMed] [Google Scholar]
- 80.Montalbano L, et al. Relationship between quality of life and behavioural disorders in children with persistent asthma: A Multiple Indicators Multiple Causes (MIMIC) model. Sci. Rep. 2020;10:6957. doi: 10.1038/s41598-020-62264-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Edvinsson Sollander S, et al. Asthma and allergies correlate with mental health problems in preschool children. Acta Paediatr. 2021;110:1601–1609. doi: 10.1111/apa.15709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wan J, Takeshita J, Shin DB, Gelfand JM. Mental health impairment among children with atopic dermatitis: A United States population-based cross-sectional study of the 2013–2017 National Health Interview Survey. J. Am. Acad. Dermatol. 2020;82:1368–1375. doi: 10.1016/j.jaad.2019.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chai PH, Chang S, Cawthorpe D. The temporal hyper-morbidity of asthma and attention deficit disorder: Implications for interpretation based on comparison of prospective and cross-sectional population samples. Psychiatry Investig. 2021;18:166–171. doi: 10.30773/pi.2020.0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Galéra C, et al. Medical conditions and Attention-Deficit/Hyperactivity Disorder symptoms from early childhood to adolescence. Mol. Psychiatry. 2021 doi: 10.1038/s41380-021-01357-x. [DOI] [PubMed] [Google Scholar]
- 85.Hou A, Silverberg JI. Predictors and age-dependent pattern of psychologic problems in childhood atopic dermatitis. Pediatr. Dermatol. 2021;38:606–612. doi: 10.1111/pde.14588. [DOI] [PubMed] [Google Scholar]
- 86.Keller W, et al. Atopic diseases in children and adolescents are associated with behavioural difficulties. BMC Pediatr. 2021 doi: 10.1186/s12887-021-02663-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Özyurt G, et al. Adolescents with asthma reported more peer victimization, more anger repression, and less anger expression. J. Asthma. 2021;58:1307–1313. doi: 10.1080/02770903.2020.1782428. [DOI] [PubMed] [Google Scholar]
- 88.Rajhans P, Sagar R, Patra BN, Bhargava R, Kabra SK. Psychiatric morbidity and behavioral problems in children and adolescents with bronchial asthma. Indian J. Pediatr. 2021;88:968–973. doi: 10.1007/s12098-021-03661-4. [DOI] [PubMed] [Google Scholar]
- 89.Vittrup I, et al. Association between hospital-diagnosed atopic dermatitis and psychiatric disorders and medication use in childhood. Br. J. Dermatol. 2021;185:91–100. doi: 10.1111/bjd.19817. [DOI] [PubMed] [Google Scholar]
- 90.Yüksel AE, et al. Adhd and its associations with pregnancy, birth, developmental and medical-related characteristics. Curr. Psychol. 2021 doi: 10.1007/s12144-021-01817-1. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.