Abstract
Objectives
To evaluate the safety of each anti-TNF therapy for patients with rheumatoid arthritis (RA) and then make the best choice in clinical practice.
Methods
We searched PUBMED, EMBASE, and the Cochrane Library. The deadline for retrieval is August 2021. The ORs, Confidence Intervals (CIs), and p values were calculated by STATA.16.0 software for assessment.
Result
72 RCTs involving 28332 subjects were included. AEs were more common with adalimumab combined disease-modifying anti-rheumatic drugs (DMARDs) compared with placebo (OR = 1.60, 95% CI: 1.06, 2.42), DMARDs (1.28, 95% CI: 1.08, 1.52), etanercept combined DMARDs (1.32, 95% CI: 1.03, 1.67); certolizumab combined DMARDs compared with placebo (1.63, 95% CI: 1.07, 2.46), DMARDs (1.30, 95% CI: 1.10, 1.54), etanercept combined DMARDs (1.34, 95% CI: 1.05, 1.70). In SAEs, comparisons between treatments showed adalimumab (0.20, 95% CI: 0.07, 0.59), etanercept combined DMARDs (0.39, 95% CI: 0.15, 0.96), golimumab (0.19, 95% CI: 0.05, 0.77), infliximab (0.15, 95% CI: 0.03,0.71) decreased the risk of SAEs compared with golimumab combined DMARDs. In infections, comparisons between treatments showed adalimumab combined DMARDs (0.59, 95% CI: 0.37, 0.95), etanercept (0.49, 95% CI: 0.28, 0.88), etanercept combined DMARDs (0.56, 95% CI: 0.35, 0.91), golimumab combined DMARDs (0.51, 95% CI: 0.31, 0.83) decreased the risk of infections compared with infliximab combined DMARDs. No evidence indicated that the use of TNF-α inhibitors influenced the risk of serious infections, malignant tumors.
Conclusion
In conclusion, we regard etanercept monotherapy as the optimal choice for RA patients in clinical practice when the efficacy is similar. Conversely, certolizumab + DMARDs therapy is not recommended.
Systematic Review Registration
identifier PROSPERO CRD42021276176.
Keywords: adverse effects, TNF-α inhibitors, rheumatoid arthritis, network meta-analysis, serious adverse events
Introduction
Rheumatoid arthritis (RA) is one of the most prevalent chronic inflammatory diseases, which can cause cartilage and bone damage as well as a disability that carries a substantial burden for both the individual and society (1). Currently, antitumors necrosis factor (anti-TNF) therapy has been established as an efficacious therapeutic strategy in RA (2). TNF-α is a pro-inflammatory cytokine known to have a key role in the pathogenesis of chronic immune-mediated diseases (3). Five TNF-α inhibitors have received regulatory approval for clinical use in rheumatology: adalimumab, golimumab, infliximab, certolizumab, and etanercept (4). They are commonly used in the treatment of rheumatoid arthritis.
Besides therapeutic effects, some studies reported that TNF-α inhibitors may also cause some adverse effects in patients with RA (5–8). Although there have been some pair-wise meta-analyses and network meta-analyses that evaluate the safety of different TNF-α inhibitors therapies for patients with RA. Nevertheless, most of the trials only focused on total AEs and SAEs or just one kind of detailed AEs, and some of the initial meta-analyses were contradicted by subsequent studies. For instance, Bongartz et al. reported that RA patients who were treated by anti-TNF therapies had an increased risk of serious infections and malignancies (9), while another trial evaluating malignancy risk in RA patients concluded that there was no significant evidence of an increased risk of malignancy using TNF-α inhibitors (10).
To evaluate the safety of TNF-α inhibitors in patients with RA, we choose six safety outcomes to systematically assess 10 anti-TNF therapies from 72 RCTs with a sample size of 28332 patients. Our network meta-analysis seeks to infer the risk of adverse effects of two therapies in patients with rheumatoid arthritis by direct and indirect comparisons. Simultaneously, it extracts and analyzes data from all randomized control trials (RCTs) to select the best therapy. The objective of the current study is to better characterize the safety of each anti-TNF therapy for patients with RA and then make the best choice in clinical practice.
Method
Study Selection
We searched PUBMED, EMBASE, and the Cochrane Library with the terms of drugs (adalimumab, certolizumab, etanercept, infliximab, and golimumab) and diseases (rheumatoid arthritis). After matching each “drug” and “disease”, restricting search results with the condition “randomized controlled trial”, we finally form the retrieval expressions that adapt to different databases. The deadline for retrieval is August 2021. Two investigators performed the literature screening according to the inclusion and exclusion criteria independently. The repeated studies were excluded firstly. Afterward, excluded unrelated studies by reading the titles and abstracts. The literature that met the inclusion and exclusion criteria was further screened by reading the full text. Disagreements were resolved by consensus Equations.
Inclusive Criteria
RCTs associated with adalimumab, certolizumab, etanercept, infliximab, and golimumab in the treatment of rheumatic diseases are included. Subjects should be greater than or equal to 18 years old and should be diagnosed with rheumatoid arthritis according to American College of Rheumatology criteria or other authoritative criteria. Disease progression, race, nationality, and complications are not limited. For the types of interventions, the experimental groups use TNF-α inhibitors, with or without disease-modifying antirheumatic drugs (DMARDs). The control groups use placebo (with or without DMARDs) or DMARDs alone.
Exclusive Criteria
RCTs that accord with any of the following criteria will be excluded: (1) studies with no accessible records of AE, SAE, malignant tumors, infections, severe infections, or malignant tumors (requiring intravenous antibiotic treatment or hospitalization or threatening patient’s life); (2) repetitive studies with shorter follow-up time; (3) studies with improper control (other therapy in experimental group or control group); (4) studies with Jadad score lower than or equal to 3 points; (5) studies with full texts not available.
Data Extraction
Data extraction was performed independently by He Bei and Li Yun, and the EndNote software was used to filter duplications and irrelevant literature by reading titles and abstracts. The remaining articles were then browsed in full text to determine whether they met the inclusion criteria. After removing ineligible publications, the two reviewers independently extracted data from each study, and disagreements were resolved by reaching a consensus. From each eligible study, we extracted and summarized the following details: the first author, year of publication, country, the total number of participants, type of TNF-α inhibitors, age range, follow-up time, duration of trials.
Assessment of Risk of Bias
Two investigators independently assessed each study’s risk of bias as low, unclear, and high. Disagreements were resolved by consensus. The items included: Random sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; selective reporting; other bias.
Quality Assessment
Two reviewers independently used the modified Jadad scale to assess the quality of RCTs (randomized control trials). NOS includes three aspects (selection, comparability, and exposure for case-control studies or outcomes for cohort studies), as well as scores of 4, 2, and 3, respectively. The modified Jadad scale comprises four parts: generation of the allocation sequence, concealment of allocation, blinding, and incomplete outcome data, and scores of 2, 2, 2, and 1 for four parts, respectively. Studies with scores of 1-3 were considered to be of low quality; 4-7 high quality.
Data Synthesis and Analysis
Network meta-analysis was performed to compare each of the 10 anti-TNF therapies. Based on the multivariate framework, the network meta-analysis was conducted using frequency theory, and two program packages, network, and mvmeta, developed by STATA 16 software based on multiple regression theory, were used for statistical analysis. Firstly, an evidence network diagram was drawn to show the comparison between interventions, and the consistency test was conducted according to the existence of closed rings. Second, for counting data, OR was used for calculation, the network meta of adverse drug reactions was analyzed, 95% confidence interval was used for all effect sizes, and 95%CI of OR did not cross effect line 1, indicating that P<0.05 was statistically significant. SUCRA analysis was used to seek therapies that had the highest probability of adverse events, with the higher the SUCRA value, the higher the risk. Stata 16.0 draws a comparative-correction funnel plot to determine whether there is a small sample effect in the analysis and recognition network, to evaluate the publication bias of the final screening. All tests were two-sided with a significance level of 0.05.
Result
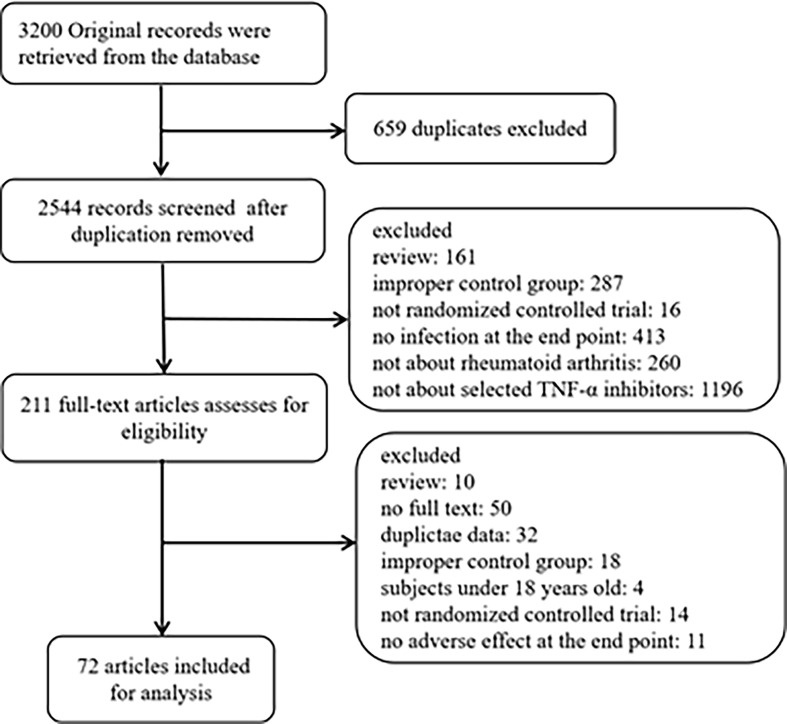
By searching databases, we retrieved 3200 original records. After excluding duplicates and irrelevant articles, 211 full-text articles were assessed for eligibility. By reading full-text, 72 articles met the inclusive criteria and exclusive criteria (11–82). The following diagram of the study selection process for this meta-analysis is shown in Figure 1 . The 72 articles included 28332 patients, followed up for about 16-104 weeks. 72 articles involved RCT experiments, including 21 adalimumab trials, 13 certolizumab trials, 21 etanercept trials, 9 golimumab trials, and 8 infliximab trials. Table 1 summarizes the relevant characteristics.
Figure 1.
Flow diagram of search results.
Table 1.
Characteristics of included studies.
| Author, Year | Duration of trials (years) | Quality score | Follow-up time(Week) | Average age(years old) | Duration of rheumatoid arthritis (years) | Number of women(n) | Number of patients (n) | Total number of cases (n) | Intervention measures | |
|---|---|---|---|---|---|---|---|---|---|---|
| Den et al. (11) | NA | 4 | 4 | 55 | 11.9 | 22 | 31 | 120 | Placebo | |
| 54 | 11 | 10 | 17 | adalimumab 0.5mg/Kg | ||||||
| 58 | 11.2 | 10 | 18 | adalimumab 1mg/Kg | ||||||
| 54 | 10.8 | 8 | 18 | adalimumab 3mg/Kg | ||||||
| 59 | 14.5 | 15 | 18 | adalimumab 5mg/Kg | ||||||
| 53 | 8.9 | 12 | 18 | adalimumab 10mg/Kg | ||||||
| Frust et al. (15) | NA | 4 | 24 | 55 | 9.3 | 253 | 318 | 636 | adalimumab 40mg eow+DMARD | |
| 55.8 | 11.5 | 252 | 318 | placebo+DMARD | ||||||
| Van der Putte et al. (13) | NA | 4 | 12 | 53.7 | 10.4 | 61 | 72 | 284 | adalimumab 20mg qw | |
| 52.6 | 10 | 57 | 70 | adalimumab 40mg qw | ||||||
| 53.2 | 10.1 | 50 | 72 | adalimumab 80mg qw | ||||||
| 50.2 | 9.4 | 57 | 70 | placebo | ||||||
| Weinblatt et al. (14) | NA | 5 | 24 | 53.5 | 13.1 | 52 | 69 | 271 | adalimumab 20mg eow+MTX | |
| 57.2 | 12.2 | 50 | 67 | adalimumab 40mg eow+MTX | ||||||
| 55.5 | 12.8 | 55 | 73 | adalimumab 80mg eow+MTX | ||||||
| 56 | 11.1 | 51 | 62 | placebo+MTX | ||||||
| Keystone et al. (16) | NA | 5 | 52 | 56.1 | 11 | 158 | 207 | 619 | adalimumab 40mg eow+MTX | |
| 57.3 | 11 | 160 | 212 | adalimumab 20mg qw+MTX | ||||||
| 56.3 | 10.9 | 146 | 200 | placebo+MTX | ||||||
| van der Putte et al. (19) | 2000.1-2001.6 | 7 | 26 | 53.1 | 9.3 | 84 | 106 | 544 | adalimumab 20mg eow | |
| 54.4 | 11.3 | 81 | 112 | adalimumab 20mg qw | ||||||
| 52.7 | 10.6 | 90 | 113 | adalimumab 40mg eow | ||||||
| 51.8 | 11.9 | 81 | 103 | adalimumab 40mg qw | ||||||
| 53.5 | 11.6 | 85 | 110 | placebo | ||||||
| Breedveld et al. (20) | PREMIER(NCT00195663) | NA | 6 | 104 | 51.9 | 0.7 | 193 | 268 | 799 | adalimumab 40mg eow+MTX |
| 52.1 | 0.7 | 212 | 274 | adalimumab 40mg eow | ||||||
| 52 | 0.8 | 190 | 257 | placebo+MTX | ||||||
| Kim et al. (25) | NA | 5 | 18 | 48.5 | 6.8 | 62 | 65 | 128 | 40 mg adalimumab eow+MTX | |
| 49.8 | 6.9 | 53 | 63 | placebo +MTX | ||||||
| Miyasaka et al. (31) | CHANGE | 2004.2-2005.6 | 5 | 24 | 54.8 | 10 | 69 | 87 | 352 | adalimumab 20mg eow |
| 56.9 | 9.9 | 72 | 91 | adalimumab 40mg eow | ||||||
| 54.3 | 9.5 | 72 | 87 | adalimumab 80mg eow | ||||||
| 53.4 | 8.4 | 67 | 87 | placebo | ||||||
| Bejarano et al. (28) | 2003.3.5-2004.12.2 | 7 | 56 | 47 | 9.5 | 44 | 75 | 148 | adalimumab 40mg eow+MTX | |
| 47 | 7.9 | 39 | 73 | placebo+MTX | ||||||
| Chen et al. (33) | NA | 5 | 12 | 53 | 6.2 | 26 | 35 | 47 | adalimumab 40mg eow+MTX | |
| 53 | 8.3 | 11 | 12 | MTX | ||||||
| van Vollenhoven et al. (46) | NCT00853385 | 2009.1.30-2011.2.10 | 3 | 12 | 52.5 | 8.1 | 162 | 204 | 312 | adalimumab 40 mg eow |
| 53.7 | 7.9 | 82 | 108 | placebo | ||||||
| Detert et al. (48) | HIT HARD | 2007.6-2010.9 | 5 | 24 | 47.2 | 0.15 | 61 | 87 | 172 | adalimumab 40mg eow+MTX |
| 52.5 | 0.14 | 57 | 85 | MTX | ||||||
| Kavanaugh et al. (49) | OPTIMA(NCT00420927) | 2006.12-2010.7 | 5 | 26 | 50.7 | 0.33 | 380 | 515 | 1032 | adalimumab 40mg eow+MTX |
| 50.4 | 0.38 | 382 | 517 | placebo+MTX | ||||||
| Hørslev-Petersen et al. (57) | OPERA | 2007.8-2009.12 | 5 | 104 | 56.2 | 0.24 | 56 | 89 | 180 | adalimumab 40mg eow+MTX |
| 54.2 | 0.23 | 63 | 91 | placebo+MTX | ||||||
| Kennedy et al. (58) | ALTARA | 2010.11-2012.7 | 5 | 12 | 50.2 | NR | 78 | 85 | 214 | patecilizumab |
| 50.6 | NR | 68 | 85 | adalimumab 40mg eow | ||||||
| 48.8 | NR | 37 | 44 | placebo | ||||||
| Takeuchi et al. (62) | HOPEFUL 1 | 2009.3-2010.11 | 5 | 26 | 54 | 0.3 | 144 | 171 | 334 | adalimumab 40mg eow+MTX |
| 54 | 0.3 | 128 | 163 | placebo+MTX | ||||||
| Taylor et al. (74) | RA-BEAM | 2012.11-2015.9 | 5 | 24 | 53 | 10 | 251 | 330 | 818 | adalimumab 40mg eow |
| 53 | 10 | 382 | 488 | placebo | ||||||
| Fleischmann et al. (77) | SELECT - COMPARE | 2015.12-2017.6 | 6 | 26 | 54 | 8 | 512 | 651 | 1629 | placebo +MTX |
| 54 | 8 | 159 | 327 | adalimumab 40 mg+MTX | ||||||
| Ducourau et al. (78) | (NCT01895764) | 2013.3-2014.10 | 4 | 26 | 43 | 3 | 22 | 52 | 107 | adalimumab 40mg qw+MTX |
| 41 | 2 | 28 | 55 | adalimumab 40 mg qw | ||||||
| Combe et al. (81) | NCT02889796 | 2016.8.30-2019.6.20 | 7 | 24 | 53 | 8 | 266 | 325 | 800 | adalimumab 40 mg biw+MTX |
| 53 | 7.3 | 391 | 475 | placebo +MTX | ||||||
| Fleischman et al. (77) | FAST4WARD | 2003.6-2004.7 | 6 | 24 | 52.7 | 8.7 | 87 | 111 | 220 | certolizumab 400mg |
| 54.9 | 10.4 | 97 | 109 | placebo | ||||||
| Smolen et al., 2009 | RAPID 2 | 20005.6-2006.9 | 4 | 24 | 51.9 | 6.5 | 192 | 246 | 619 | certolizumab 400mg + MTX |
| 52.2 | 6.1 | 206 | 248 | certolizumab 200mg + MTX | ||||||
| 51.5 | 5.6 | 107 | 125 | placebo + MTX | ||||||
| Choy et al. (42) | NCT00544154 | 2002.10-2004.1 | 7 | 24 | 53 | 9.4 | 91 | 126 | 247 | certolizumab 400mg + MTX |
| 55.6 | 9.9 | 80 | 121 | placebo + MTX | ||||||
| Weinblatt et al. (47) | REALISTIC(NCT00717236) | 2008.7-2010.3 | 7 | 12 | 55.4 | 8.6 | 660 | q | 1063 | certolizumab (certolizumab 400 mg qw 0, 2 and 4,followed by certolizumab 200 mg eow)+DMARDs |
| 53.9 | 8.9 | 169 | 212 | placebo +DMARDs | ||||||
| schiff et al. (61) | NCT01147341 | 4 | 52 | 56.1 | 12 | NR | 27 | 37 | certolizumab(400 mg qw 0, 2 and 4, followed by 200mg eow)+DMARDs | |
| 59 | 14 | NR | 10 | placebo +DMARDs | ||||||
| Yamamoto et al. (63) | J-RAPID | 2008.11.19-2010.8.18 | 7 | 24 | 54.3 | 6.0 | 58 | 72 | 316 | certolizumab 100mg eow + MTX |
| 50.6 | 5.6 | 69 | 82 | certolizumab 200mg eow + MTX | ||||||
| 55.4 | 6.0 | 69 | 85 | certolizumab 400mg eow + MTX | ||||||
| 51.9 | 5.8 | 66 | 77 | placebo + MTX | ||||||
| Furst et al. (64) | DOSEFLEX | 5 | 16 | 51.5 | 6.5 | 56 | 69 | 208 | Placebo +MTX | |
| 55.6 | 5.9 | 49 | 70 | certolizumab 200 mg eow +MTX | ||||||
| 53.1 | 6.4 | 57 | 69 | certolizumab 400 mg q4w +MTX | ||||||
| Smolen et al. (65) | CERTAIN | 2008.6-2010.12 | 5 | 24 | 53.6 | 4.5 | 81 | 96 | 194 | certolizumab(400 mg certolizumab qw 0, 2 and 4, followed by 200 mg certolizumab eow)+DMARDs |
| 54 | 4.7 | 75 | 98 | placebo +DMARDs | ||||||
| Atsumi et al. (66) | C-OPERA (NCT01451203) | 2011.10-2013.8 | 7 | 52 | 49.4 | 4.0 | 129 | 159 | 316 | certolizumab 400mg/200mg eow +MTX |
| 49 | 4.3 | 127 | 157 | placebo + MTX | ||||||
| Emery et al. (72) | C-EARLY (NCT01519791) | 2012.1-2015.9 | 6 | 52 | 50.4 | 0.24 | 497 | 660 | 879 | certolizumab 400mg/200mg eow +MTX |
| 51.2 | 0.24 | 170 | 219 | placebo + MTX | ||||||
| Kang et al. (75) | (NCT00993317) | 2009.12-2011.8 | 4 | 24 | 51.6 | 6.5 | 72 | 85 | 127 | certolizumab 400mg/200mg eow +MTX |
| 50.8 | 5.5 | 35 | 42 | placebo + MTX | ||||||
| Bi et al. (76) | RAPID-C (NCT02151851) | 2014.7.23-2016.6.17 | 6 | 24 | 48.2 | 7.0 | 268 | 316 | 429 | certolizumab 200 mg eow (loading dose: 400 mg certolizumab qw 0, 2 and 4) + MTX |
| 47.1 | 6.6 | 95 | 113 | (PBO) + MTX | ||||||
| Hetland et al. (79) | NCT01491815 | 2012.12.3-2018.12.11 | 6 | 24 | 54.6 | 0.53 | 139 | 197 | 399 | active conventional treatment |
| 55.3 | 0.56 | 139 | 202 | certolizumab 200 mg qw (400 mg qw 0, 2, and 4)+MTX | ||||||
| Genovese et al. (39) | 1997.5-1999.3 | 5 | 104 | 49 | 1 | 75 | 217 | 632 | three 2.5-mg MTX qw and placebo biw | |
| 50 | 0.9 | 75 | 208 | 10 mg of etanercept biw and three placebo tablets qw, | ||||||
| 51 | 1 | 74 | 207 | 25 mg of etanercept biw and three placebo tablets qw | ||||||
| Smolen et al. (1) | 2011.12.14-2013.11.11 | 4 | 12 | 53 | 5.9 | 96 | 457 | 914 | certolizumab pegol (400 mg weeks 0, 2, | |
| 457 | adalimumab (40 mg once q2w) plus | |||||||||
| Keystone et al. (16) | NA | 5 | 8 | 54 | 10.8 | 38 | 53 | 420 | placebo | |
| 53 | 9.0 | 169 | 214 | 50 mg etanercept qw | ||||||
| 52 | 8.2 | 121 | 153 | 25 mg etanercept biw | ||||||
| van der Heijde et al. (26) | TEMPO | 2000.10-2001.7 | 6 | 104 | 52.5 | 6·8 | 171 | 231 | 682 | etanercept 25mg biw + MTX |
| 53.2 | 6·8 | 171 | 223 | etanercept 25mg biw + placebo | ||||||
| 53 | 6·3 | 180 | 228 | placebo + MTX | ||||||
| Lan et al. (21) | NR | 4 | 12 | 47.55 | NR | 50 | 29 | 58 | etanercept 25mg biw + MTX | |
| 50.79 | 29 | placebo +MTX | ||||||||
| van Riel et al. (22) | ADORE | 2003.3-2004.5 | 4 | 16 | 53 | 10 | 126 | 159 | 314 | etanercept 25 mg biw |
| 54 | 9.8 | 119 | 155 | etanercept 25 mg biw + MTX | ||||||
| Weisman et al. (27) | RA | NA | 6 | 16 | 60.6 | 10.1 | 192 | 266 | 535 | etanercept 25mg biw |
| 59.3 | 9.4 | 210 | 269 | placebo | ||||||
| Emery et al. (29) | COMET | 2004.10-2006.2 | 7 | 52 | 50.5 | 8·8 | 196 | 274 | 542 | etanercept 50mg qw + MTX |
| 52.3 | 9·3 | 191 | 268 | MTX | ||||||
| Kameda et al. (41) | JESMR(NCT00688103) | 2005.6-2007.1 | 4 | 24 | 58.1 | 10.6 | 62 | 71 | 146 | etanercept 25 mg eow |
| 56.5 | 8.1 | 60 | 75 | MTX+etanercept | ||||||
| Jobanputra et al. (43) | EU Clinical | 2007.5-2010.4 | 4 | 52 | 55 | 7.0 | 15 | 60 | 120 | adalimumab 40 mg qw |
| Trials Register 2006-006275-21/GB | 53.2 | 5.5 | 18 | 60 | etanercept 50 mg qw | |||||
| Kim et al. (44) | APPEAL | 2007.6-2009.3 | 6 | 16 | 48.4 | 6.5 | 17 | 197 | 300 | etanercept 25 mg biw+MTX |
| 48.5 | 6.9 | 12 | 103 | DMARD+MTX | ||||||
| Takeuchi et al. (80) | NCT00445770 | NA | 6 | 52 | 51.8 | 3.0 | 145 | 182 | 550 | etanercept 25 mg biw |
| 51.5 | 2.9 | 154 | 192 | etanercept 10 mg biw | ||||||
| 50.4 | 3.0 | 140 | 176 | MTX | ||||||
| Emery et al. (56) | NCT00913458 | 2009.10.20-2012.12.17 | 5 | 39 | 49.6 | 0.54 | 47 | 63 | 193 | etanercept (25 mg)+MTX |
| 47.7 | 0.58 | 36 | 65 | placebo +MTX | ||||||
| 50.9 | 0.59 | 42 | 65 | placebo | ||||||
| Machado et al. (59) | NCT00848354 | 2009.6-2011.3 | 5 | 24 | 48.4 | 7.9 | 248 | 281 | 423 | etanercept(50 mg qw)+MTX |
| 48.6 | 9.0 | 128 | 142 | (DMARD) + MTX | ||||||
| Nam et al. (60) | EMPIRE | 2006.10-2009.5 | 7 | 78 | 47.9 | 0.5 | 44 | 55 | 110 | etanercept 50mg qw + MTX |
| 48.4 | 0.67 | 40 | 55 | placebo + MTX | ||||||
| Smolen et al. (52) | PRESERVE(NCT00565409) | 2008.3.6-2009.9.9 | 3 | 52 | 46.4 | 6·4 | 157 | 202 | 34 | etanercept 25mg qw+MTX |
| 48.1 | 6·8 | 164 | 202 | etanercept 50mg qw+MTX | ||||||
| 48.3 | 7·3 | 167 | 200 | placebo+MTX | ||||||
| Keystone et al. (67) | CAMEO (NCT00654368) | 2008.6-2012.12 | 6 | 104 | 54.3 | 9.0 | 72 | 98 | 205 | etanercept 50 mg qw |
| 54.4 | 9.3 | 84 | 107 | etanercept 50 mg qw + MTX | ||||||
| van Vollenhovn et al. (70) | NCT00858780 | NR | 4 | 20 | 53.8 | 11.5 | 17 | 23 | 73 | etanercept50mg qw + MTX |
| 59.6 | 16.6 | 18 | 27 | etanercept25mg qw + MTX | ||||||
| 56.1 | 12.3 | 16 | 23 | placebo +MTX | ||||||
| Yamanaka et al. (71) | ENCOURAGE (UMIN000002687) | 2009.8-2014.4 | 5 | 52 | 52.8 | 2.0 | 138 | 161 | 191 | etanercept 25 mg biw + MTX |
| 54.6 | 1.9 | 25 | 30 | MTX | ||||||
| Pavelka et al. (73) | NCT01578850 | 2012.7-2015.3 | 6 | 28 | 46.1 | 8.0 | 136 | 167 | 343 | etanercept 50mg qw +DMARDs |
| 47.2 | 8.3 | 143 | 176 | placebo +DMARDs | ||||||
| Curtis et al. (82) | SEAM- RA | 2015.2.20-2018.6.26 | 6 | 48 | 56.2 | 9.7 | 76 | 101 | 153 | MTX |
| 54.8 | 11.0 | 77 | 101 | etanercept | ||||||
| 55.9 | 10.3 | 40 | 51 | MTX + etanercept | ||||||
| Kay et al. (30) | 2003.12.1-2006.2.21 | 5 | 20 | 52 | 5.6 | 26 | 35 | 172 | placebo + MTX | |
| 57 | 8.2 | 30 | 35 | 50mg golimumab q4w + MTX | ||||||
| 48 | 8.2 | 23 | 34 | 50mg golimumab eow + MTX | ||||||
| 57.5 | 6.3 | 26 | 34 | 100mg golimumab eow + MTX | ||||||
| 53.5 | 9.0 | 27 | 34 | 50mg golimumab eow + MTX | ||||||
| Emery et al. (34) | GO-BEFORE | 2005.12.12-2007.10.1 | 6 | 24 | 50.9 | 3.5 | 135 | 159 | 634 | Golimumab 50 mg q4w + MTX |
| 50.2 | 3.6 | 125 | 159 | Golimumab 100 mg q4w + MTX | ||||||
| 48.2 | 4.1 | 159 | 159 | Golimumab 100 mg q4w + Placebo | ||||||
| 48.6 | 2.9 | 134 | 160 | Placebo+MTX | ||||||
| Keystone et al. (36) | GO-FORWARD | 20005.12.19-2007.9.17 | 5 | 16 | 52 | 4.5 | 72 | 89 | 444 | Golimumab 50 mg q4w + MTX |
| 50 | 6.7 | 72 | 89 | Golimumab 100 mg q4w + MTX | ||||||
| 51 | 5.9 | 105 | 133 | Golimumab 100 mg q4w + Placebo | ||||||
| 52 | 6.5 | 109 | 133 | Placebo+MTX | ||||||
| Smolen et al. (38) | GO-AFTER (NCT00299546) | 2006.2.21-2007.9.26 | 7 | 16 | 55 | 9.6 | 113 | 153 | 461 | Golimumab 50 mg q4w |
| 55 | 8.7 | 122 | 153 | Golimumab 100 mg q4w | ||||||
| 54 | 9.8 | 132 | 155 | Placebo | ||||||
| Kremer et al. (40) | NCT00361335 | 2006.8.24-2008.8.25 | 6 | 16 | 49.9 | 7.4 | 21 | 128 | 643 | Golimumab 2mg/kg q12w |
| 48.4 | 8.4 | 10 | 129 | Golimumab 4mg/kg q12w | ||||||
| 49.7 | 8.1 | 30 | 129 | Golimumab 2mg/kg q12w + MTX | ||||||
| 49.6 | 9.4 | 25 | 128 | Golimumab 4mg/kg q12w + MTX | ||||||
| 50.2 | 7.4 | 24 | 129 | Placebo + MTX | ||||||
| Tanaka et al. (45) | GO-FORTH | 2008.5-2009.11 | 5 | 16 | 50.4 | 8.8 | 15 | 86 | 261 | Golimumab 50 mg q4w + MTX |
| 50 | 8.1 | 78 | 87 | Golimumab 100 mg q4w + MTX | ||||||
| 51.1 | 8.7 | 73 | 88 | Placebo + MTX | ||||||
| Takeuchi et al. (53) | GO-MONO | NA | 4 | 16 | 52.9 | 8.1 | 81 | 101 | 308 | Golimumab 50 mg q4w |
| 51.6 | 9.4 | 85 | 102 | Golimumab 100 mg q4w | ||||||
| 52.4 | 9.2 | 86 | 105 | Placebo | ||||||
| Weinblatt et al. (55) | GO-FURTHER(NCT00973479) | 2009.9.14-2011.5.18 | 7 | 16 | 51.4 | 7.0 | 157 | 197 | 592 | Placebo +MTX |
| 51.9 | 6.9 | 326 | 395 | Golimumab2 mg/kg+MTX | ||||||
| Li et al. (68) | NCT01248780 | 2010.8-2012.7 | 4 | 24 | 47.7 | 7.6 | 110 | 132 | 264 | Golimumab 50 mg q4w + MTX |
| 46.7 | 8.0 | 104 | 132 | Placebo + MTX | ||||||
| Maini et al. (17) | 1997.3.31-2000.3.9 | 7 | 102 | 54 | 10 | 70 | 86 | 428 | infliximab 3mg/kg, q8w+MTX | |
| 52 | 9 | 66 | 86 | infliximab 3mg/kg, q4w+MTX | ||||||
| 54 | 11 | 67 | 87 | infliximab 10mg/kg, q8w+MTX | ||||||
| 52 | 12 | 59 | 81 | infliximab 10mg/kg, q4w+MTX | ||||||
| 51 | 11 | 70 | 88 | placebo +MTX | ||||||
| St. Clair et al. (18) | 2000.7.21-2002.2.28 | 7 | 54 | 51 | 0.8 | 255 | 359 | 1004 | infliximab 3mg/kg, q8w+MTX | |
| 50 | 0.9 | 247 | 363 | infliximab 6mg/kg, q8w+MTX | ||||||
| 50 | 0.9 | 212 | 282 | placebo +MTX | ||||||
| Abe et al. (12) | 2000.4.19-2000.10.27 | 4 | 6 | 55.2 | 9.1 | 40 | 49 | 147 | infliximab 3mg/kg, q8w+MTX | |
| 56.8 | 7.1 | 40 | 51 | infliximab 10mg/kg, q8w+MTX | ||||||
| 55.1 | 7.5 | 35 | 47 | placebo +MTX | ||||||
| Westhoven et al. (23) | START | 2001.9-2003.11 | 6 | 22 | 53 | 7.8 | 288 | 360 | 1082 | infliximab 3mg/kg +MTX |
| 52 | 6.3 | 281 | 361 | infliximab 10mg/kg +MTX | ||||||
| 52.0 | 8.4 | 302 | 361 | placebo+MTX | ||||||
| Zhang et al. (24) | 2003.7-2004.7 | 4 | 18 | 47.9 | NR | 13 | 87 | 173 | infliximab (Remicade, Centocor) at a dose of 3 mg/kg body weight qw 0, 2, 6 and 14. | |
| 48.9 | NR | 13 | 86 | placebo | ||||||
| Schiff et al. (32) | ATTEST | 2005.2-2007.2 | 6 | 28 | 49.1 | 7.3 | 136 | 165 | 275 | infliximab 3mg/kg, q8w+MTX |
| 49.4 | 8.4 | 96 | 110 | placebo +MTX | ||||||
| Kim et al. (50) | NCT00202852, NCT00732875 | 2005.6-2006.5 | 5 | 30 | 49.3 | 7.4 | 64 | 69 | 138 | Infliximab |
| 51.4 | 9.8 | 64 | 69 | placebo | ||||||
| Leirisalo-Repo et al. (51) | NCT00908089 | 2003.3-2005.4 | 6 | 102 | 47 | 0.33 | 35 | 50 | 3403 | infliximab |
| 46 | 0.33 | 31 | 49 | placebo |
biw, twice a week; qw, weekly; eow, every two weeks; q4w, every four weeks; q8w, every 8 weeks; q12w, every 12 weeks; MTX, methotrexate; DMARD, disease-modifying anti-rheumatic drugs; NA, not re.
Adverse Events
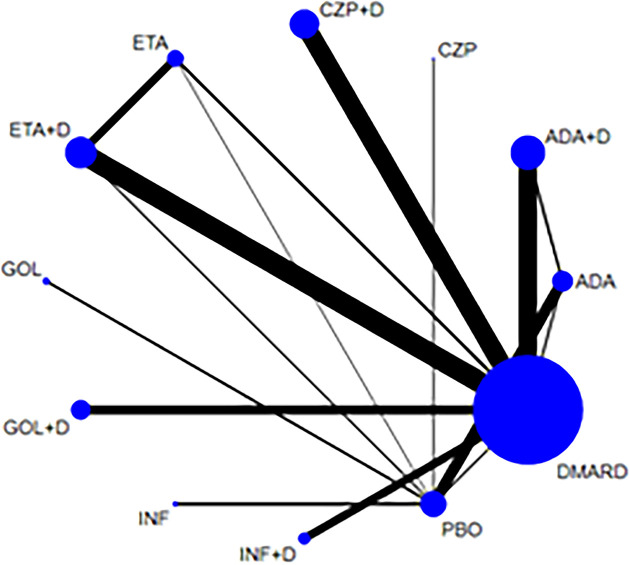
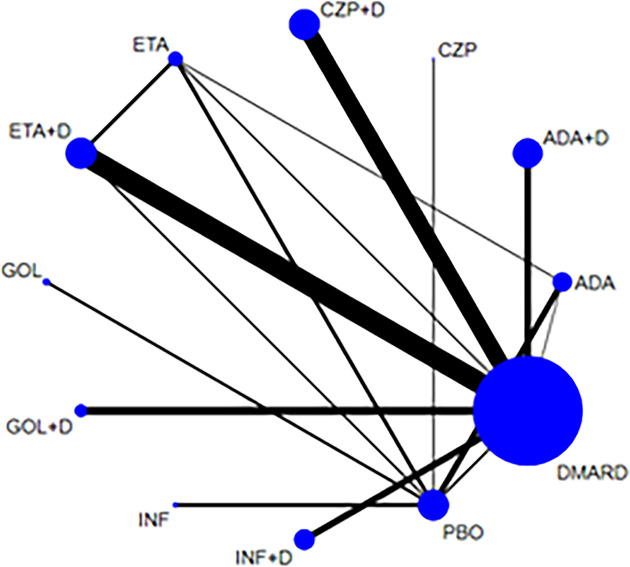
58 articles (12, 15, 16, 19, 21–26, 28–38, 40–42, 44–47, 49–56, 58–69, 71–75, 77, 79–82) reported the occurrence of AEs and 23778 RA patients was included. The network of eligible comparisons is shown in Figure 2 . Network meta-analysis showed that adalimumab combined DMARDs compared with placebo therapy statistically significantly increased the risk of AEs by 60% (1.60, 95% CI: 1.06, 2.42); compared with DMARDs, the risk of AEs increased by 28% (1.28, 95% CI: 1.08, 1.52) ( Table 2 and Figure 3 ). Certolizumab also found that compared with placebo therapy, the risk of AE increased by 127% (2.27, 95% CI: 1.22, 4.24). In addition, certolizumab combined DMARDs compared with placebo therapy statistically significantly increased the risk of AEs by 63% (1.63, 95% CI: 1.07, 2.46); compared with DMARDs, the risk of AEs increased by 30% (1.30, 95% CI: 1.10, 1.54). Comparisons between treatments showed certolizumab combined DMARDs increased the risk of AEs compared with etanercept combined DMARDs (1.34, 95% CI: 1.05, 1.70); adalimumab combined DMARDs increased the risk of AEs compared with etanercept combined DMARDs (1.32, 95% CI: 1.03, 1.67) ( Table 2 ). There was no statistically significant difference between other comparisons.
Figure 2.
Network of treatment comparisons for adverse events. The size of the circles corresponds to the total number of people. Direct comparable treatments are connected with a line. ADA, adalimumab; + D, plus DMARD; CZP, certolizumab; ETA, etanercept; GOL, golimumab; INF, infliximab; PBO, placebo; DMARD, disease-modifying anti-rheumatic drugs.
Table 2.
OR of adverse events for 12 therapies.
| ADA | 1.31 (0.83,2.07) | 1.86 (0.93,3.71) | 1.33 (0.84,2.12) | 1.04 (0.68,1.60) | 1.00 (0.64,1.55) | 1.16 (0.72,1.85) | 1.20 (0.74,1.92) | 1.15 (0.65,2.03) | 1.21 (0.71,2.06) | 0.82 (0.61,1.10) | 1.02 (0.66,1.58) |
| 0.76 (0.48,1.20) | ADA+DMARD | 1.42 (0.67,3.00) | 1.02 (0.80,1.29) | 0.79 (0.57,1.10) | 0.76 (0.60,0.97) | 0.88 (0.50,1.55) | 0.91 (0.70,1.18) | 0.88 (0.46,1.67) | 0.92 (0.65,1.30) | 0.62 (0.41,0.94) | 0.78 (0.66,0.92) |
| 0.54 (0.27,1.07) | 0.70 (0.33,1.49) | CZP | 0.72 (0.34,1.51) | 0.56 (0.27,1.15) | 0.54 (0.26,1.11) | 0.62 (0.30,1.31) | 0.64 (0.30,1.37) | 0.62 (0.28,1.37) | 0.65 (0.30,1.42) | 0.44 (0.24,0.82) | 0.55 (0.26,1.14) |
| 0.75 (0.47,1.20) | 0.98 (0.78,1.25) | 1.40 (0.66,2.96) | CZP+DMARD | 0.78 (0.56,1.09) | 0.75 (0.59,0.95) | 0.87 (0.49,1.54) | 0.90 (0.69,1.17) | 0.86 (0.45,1.64) | 0.91 (0.65,1.27) | 0.62 (0.41,0.93) | 0.77 (0.65,0.91) |
| 0.96 (0.63,1.48) | 1.26 (0.91,1.75) | 1.79 (0.87,3.69) | 1.28 (0.92,1.78) | ETA | 0.96 (0.73,1.25) | 1.11 (0.65,1.90) | 1.15 (0.81,1.63) | 1.11 (0.60,2.04) | 1.16 (0.77,1.75) | 0.79 (0.55,1.14) | 0.98 (0.74,1.30) |
| 1.00 (0.65,1.56) | 1.32 (1.03,1.67) | 1.87 (0.90,3.88) | 1.34 (1.05,1.70) | 1.04 (0.80,1.36) | ETA+DMARD | 1.16 (0.67,2.01) | 1.20 (0.92,1.56) | 1.15 (0.62,2.14) | 1.21 (0.86,1.70) | 0.82 (0.56,1.20) | 1.02 (0.86,1.21) |
| 0.86 (0.54,1.38) | 1.13 (0.64,1.99) | 1.61 (0.77,3.38) | 1.15 (0.65,2.04) | 0.90 (0.53,1.53) | 0.86 (0.50,1.49) | GOL | 1.03 (0.58,1.84) | 0.99 (0.53,1.87) | 1.04 (0.56,1.95) | 0.71 (0.47,1.06) | 0.88 (0.51,1.52) |
| 0.84 (0.52,1.34) | 1.10 (0.85,1.42) | 1.56 (0.73,3.32) | 1.11 (0.86,1.44) | 0.87 (0.61,1.23) | 0.83 (0.64,1.09) | 0.97 (0.54,1.73) | GOL+DMARD | 0.96 (0.50,1.85) | 1.01 (0.70,1.45) | 0.69 (0.45,1.05) | 0.85 (0.70,1.04) |
| 0.87 (0.49,1.54) | 1.14 (0.60,2.17) | 1.62 (0.73,3.58) | 1.16 (0.61,2.20) | 0.90 (0.49,1.67) | 0.87 (0.47,1.61) | 1.01 (0.53,1.90) | 1.04 (0.54,2.00) | INF | 1.05 (0.53,2.09) | 0.71 (0.44,1.16) | 0.89 (0.48,1.65) |
| 0.83 (0.49,1.41) | 1.09 (0.77,1.53) | 1.54 (0.70,3.39) | 1.10 (0.79,1.55) | 0.86 (0.57,1.30) | 0.83 (0.59,1.16) | 0.96 (0.51,1.79) | 0.99 (0.69,1.42) | 0.95 (0.48,1.89) | INF+DMARD | 0.68 (0.42,1.10) | 0.85 (0.63,1.14) |
| 1.22 (0.91,1.63) | 1.60 (1.06,2.42) | 2.27 (1.22,4.24) | 1.63 (1.07,2.46) | 1.27 (0.88,1.83) | 1.22 (0.83,1.78) | 1.41 (0.95,2.11) | 1.46 (0.95,2.25) | 1.40 (0.86,2.29) | 1.47 (0.91,2.38) | PBO | 1.25 (0.85,1.82) |
| 0.98 (0.63,1.51) | 1.28 (1.08,1.52) | 1.82 (0.88,3.79) | 1.30 (1.10,1.54) | 1.02 (0.77,1.35) | 0.98 (0.82,1.16) | 1.13 (0.66,1.96) | 1.17 (0.96,1.43) | 1.13 (0.60,2.10) | 1.18 (0.88,1.59) | 0.80 (0.55,1.17) | DMARD |
Results below the diagonal are the rate ratios with 95% confidence intervals from the network meta-analysis of direct and indirect comparisons between the row-defining treatment and the column-defining treatment. Numbers in red highlight statistically significant results. ADA, adalimumab; + D, plus DMARD; CZP, certolizumab; ETA, etanercept; GOL, golimumab; INF, infliximab; PBO, placebo; DMARD, disease-modifying anti-rheumatic drugs.
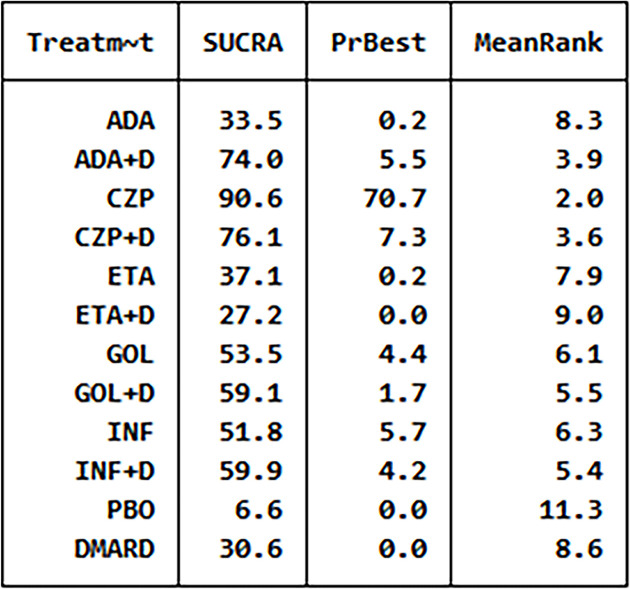
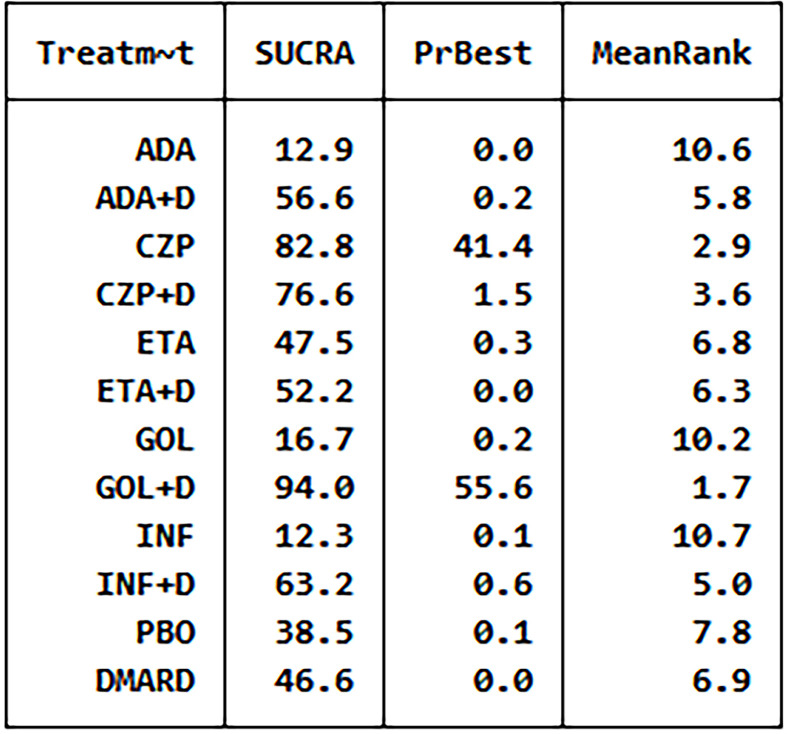
Figure 3.
The analysis SUCRA of adverse events for 12 therapies. ADA, adalimumab; + D, plus DMARD; CZP, certolizumab; ETA, etanercept; GOL, golimumab; INF, infliximab; PBO, placebo; DMARD, disease-modifying anti-rheumatic drugs.
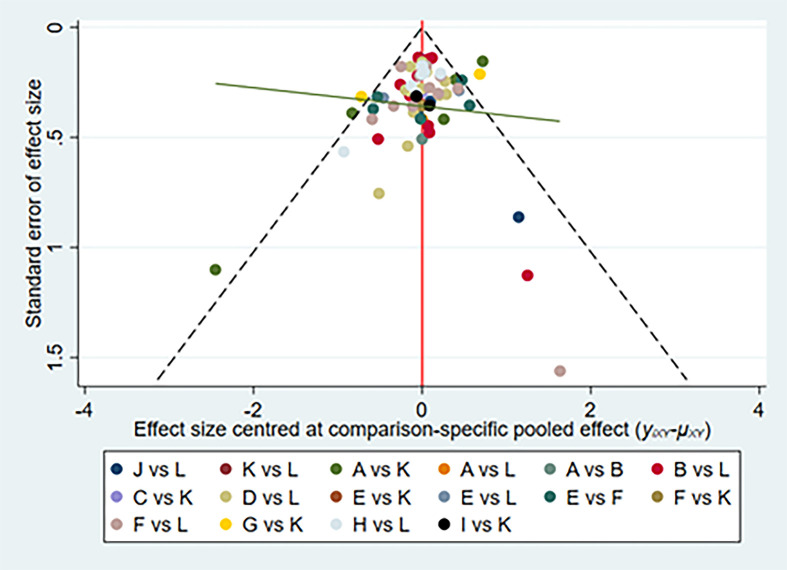
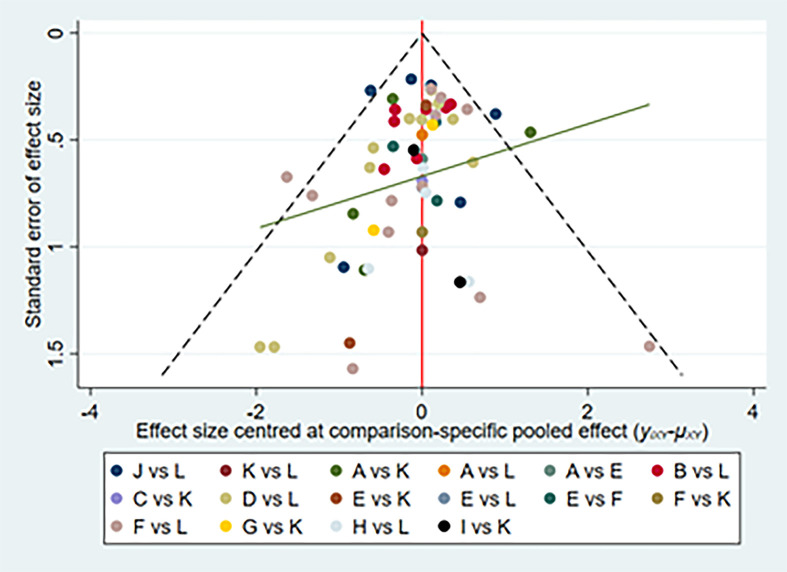
We have made global consistency. The test result p-value was 0.9095, so the consistency model could be used. We also established local consistency and the p-value of the test result exceeded 0.05, which was considered local. We analyzed SUCRA to research the probability of adverse events for each therapy. The results indicated that certolizumab had the highest probability to cause AEs (SUCRA = 0.906), while PBO had the lowest probability to cause AEs (SUCRA = 0.066) compared with the other therapies ( Figure 3 ). There was a funnel plot with no obvious asymmetry, indicating no publication bias ( Figure 4 ).
Figure 4.
Network of funnel plot for adverse events. A, adalimumab; B, adalimumab + DMARD; C, certolizumab; D, certolizumab + DMARD; F, etanercept; G, etanercept + DMARD; H, golimumab; I, golimumab + DMARD; J, infliximab; K, infliximab + DMARD; L, DMARD; DMARD, disease-modifying anti-rheumatic drugs.
Serious Adverse Events
58 articles (12, 13, 15, 17–19, 22, 24–27, 29–32, 34–36, 38, 40–52, 54, 56–60, 62–70, 72–82) reported the occurrence of SAEs and 23805 RA patients was included. The network of eligible comparisons was shown in Figure 5 . Network meta-analysis showed that golimumab combined DMARDs compared with placebo therapy statistically significantly increased the risk of SAEs by 227% (3.27, 95% CI: 1.08, 9.92); Compared with DMARDs, the risk of SAEs increased by 170% (2.70, 95% CI: 1.15, 6.32). Comparisons between treatments showed adalimumab (0.20, 95% CI: 0.07, 0.59), etanercept(0.35, 95% CI: 0.12, 1.00), etanercept combined DMARDs (0.39, 95% CI: 0.15, 0.96), golimumab (0.19, 95% CI: 0.05, 0.77) decreased the risk of SAEs compared with golimumab combined DMARDs; adalimumab (0.39, 95% CI: 0.18, 0.84) decreased the risk of SAEs compared with certolizumab combined DMARDs; golimumab combined DMARDs increased the risk of SAEs compared with infliximab (6.50, 95% CI: 1.41, 29.90) ( Table 3 ). There was no statistically significant difference between other comparisons.
Figure 5.
Network of treatment comparisons for serious adverse events. The size of the circles corresponds to the total number of people. Direct comparable treatments are connected with a line. ADA, adalimumab; + D, plus DMARD; CZP, certolizumab; ETA, etanercept; GOL, golimumab; INF, infliximab; PBO, placebo; DMARD, disease-modifying anti-rheumatic drugs.
Table 3.
OR of serious adverse events of 12 therapies.
| ADA | 2.05 (0.94,4.49) | 4.27 (0.94,19.46) | 2.57 (1.19,5.56) | 1.80 (0.94,3.42) | 1.96 (0.97,3.97) | 0.96 (0.36,2.60) | 5.08 (1.68,15.30) | 0.78 (0.24,2.49) | 2.20 (1.00,4.81) | 1.55 (0.94,2.56) | 1.88 (0.93,3.80) |
| 0.49 (0.22,1.07) | ADA+DMARD | 2.08 (0.40,10.71) | 1.25 (0.78,2.02) | 0.88 (0.44,1.75) | 0.95 (0.59,1.54) | 0.47 (0.15,1.52) | 2.48 (0.99,6.22) | 0.38 (0.10,1.42) | 1.07 (0.65,1.75) | 0.76 (0.34,1.68) | 0.92 (0.65,1.30) |
| 0.23 (0.05,1.07) | 0.48 (0.09,2.47) | CZP | 0.60 (0.12,3.08) | 0.42 (0.09,1.99) | 0.46 (0.09,2.27) | 0.23 (0.04,1.20) | 1.19 (0.19,7.30) | 0.18 (0.03,1.08) | 0.51 (0.10,2.65) | 0.36 (0.09,1.53) | 0.44 (0.09,2.19) |
| 0.39 (0.18,0.84) | 0.80 (0.49,1.29) | 1.66 (0.32,8.50) | CZP+DMARD | 0.70 (0.35,1.38) | 0.76 (0.48,1.21) | 0.38 (0.12,1.20) | 1.98 (0.79,4.92) | 0.30 (0.08,1.12) | 0.85 (0.53,1.38) | 0.61 (0.28,1.32) | 0.73 (0.53,1.02) |
| 0.56 (0.29,1.06) | 1.14 (0.57,2.29) | 2.38 (0.50,11.25) | 1.43 (0.72,2.83) | ETA | 1.09 (0.62,1.91) | 0.54 (0.19,1.53) | 2.83 (1.00,8.02) | 0.43 (0.13,1.45) | 1.22 (0.61,2.45) | 0.87 (0.47,1.58) | 1.05 (0.57,1.91) |
| 0.51 (0.25,1.04) | 1.05 (0.65,1.69) | 2.18 (0.44,10.77) | 1.31 (0.83,2.08) | 0.92 (0.52,1.61) | ETA+DMARD | 0.49 (0.16,1.50) | 2.59 (1.04,6.47) | 0.40 (0.11,1.41) | 1.12 (0.69,1.82) | 0.79 (0.39,1.61) | 0.96 (0.69,1.34) |
| 1.04 (0.38,2.80) | 2.13 (0.66,6.85) | 4.42 (0.83,23.50) | 2.66 (0.83,8.50) | 1.86 (0.65,5.32) | 2.03 (0.67,6.15) | GOF | 5.26 (1.29,21.45) | 0.81 (0.21,3.13) | 2.28 (0.70,7.36) | 1.61 (0.68,3.80) | 1.95 (0.64,5.97) |
| 0.20 (0.07,0.59) | 0.40 (0.16,1.01) | 0.84 (0.14,5.15) | 0.51 (0.20,1.26) | 0.35 (0.12,1.00) | 0.39 (0.15,0.96) | 0.19 (0.05,0.77) | GOF+DMARD | 0.15 (0.03,0.71) | 0.43 (0.17,1.08) | 0.31 (0.10,0.93) | 0.37 (0.16,0.87) |
| 1.28 (0.40,4.08) | 2.63 (0.71,9.76) | 5.46 (0.93,32.24) | 3.29 (0.89,12.15) | 2.30 (0.69,7.70) | 2.51 (0.71,8.85) | 1.24 (0.32,4.79) | 6.50 (1.41,29.90) | INF | 2.81 (0.76,10.45) | 1.99 (0.70,5.67) | 2.41 (0.68,8.55) |
| 0.46 (0.21,1.00) | 0.93 (0.57,1.53) | 1.94 (0.38,10.02) | 1.17 (0.72,1.89) | 0.82 (0.41,1.64) | 0.89 (0.55,1.45) | 0.44 (0.14,1.42) | 2.31 (0.92,5.79) | 0.36 (0.10,1.32) | INF+DMARD | 0.71 (0.32,1.57) | 0.86 (0.61,1.21) |
| 0.64 (0.39,1.06) | 1.32 (0.60,2.92) | 2.74 (0.65,11.51) | 1.65 (0.76,3.61) | 1.16 (0.63,2.11) | 1.26 (0.62,2.55) | 0.62 (0.26,1.46) | 3.27 (1.08,9.92) | 0.50 (0.18,1.43) | 1.41 (0.64,3.13) | PBO | 1.21 (0.59,2.47) |
| 0.53 (0.26,1.07) | 1.09 (0.77,1.55) | 2.27 (0.46,11.25) | 1.37 (0.98,1.90) | 0.95 (0.52,1.74) | 1.04 (0.75,1.45) | 0.51 (0.17,1.57) | 2.70 (1.15,6.32) | 0.41 (0.12,1.47) | 1.17 (0.83,1.65) | 0.83 (0.40,1.69) | DMARD |
Results below the diagonal are the rate ratios with 95% confidence intervals from the network meta-analysis of direct and indirect comparisons between the row-defining treatment and the column-defining treatment. Numbers in red highlight statistically significant results. ADA, adalimumab; + D, plus DMARD; CZP, certolizumab; ETA, etanercept; GOL, golimumab; INF, infliximab; PBO, placebo; DMARD, disease-modifying anti-rheumatic drug.
We did the global consistency test. The test result p-value was 0.8840. We also made local consistency and the test result p-value was greater than 0.05, which was considered to be locally consistent. According to the SUCRA analysis, golimumab combined DMARDs had the highest risk to cause SAEs (SUCRA = 0.940), while adalimumab had the lowest risk to cause SAEs (SUCRA = 0.130) compared with the other 11 therapies ( Figure 6 ). There was a funnel plot asymmetry, with the right corner of the pyramidal part of the funnel missing, which suggested a possible bias ( Figure 7 ).
Figure 6.
The analysis SUCRA of serious adverse events for 12 therapies. ADA, adalimumab; + D, plus DMARD; CZP, certolizumab; ETA, etanercept; GOL, golimumab; INF, infliximab; PBO, placebo; DMARD, disease-modifying anti-rheumatic drugs.
Figure 7.
Network of funnel plot for serious adverse events. A, adalimumab; B, adalimumab + DMARD; C, certolizumab; D, certolizumab + DMARD; F, etanercept; G, etanercept + DMARD; H, golimumab; I, golimumab + DMARD; J, infliximab; K, infliximab + DMARD; L, DMARD; DMARD, disease-modifying anti-rheumatic drugs.
Infections
40 articles (12, 15, 17, 22, 25–28, 30, 31, 33, 34, 36, 38, 40–42, 45, 49, 54–56, 58–60, 62–66, 72–77, 79–82) reported the occurrence of AEs and 15285 RA patients was included. The network of eligible comparisons was shown in the Supplementary Figure 1 . Network meta-analysis showed that golimumab combined DMARDs compared with DMARDs increased the risk of infections by 35% (1.35, 95% CI: 1.10, 1.66); infliximab combined DMARDs compared with DMARDs increased the risk of infections by 102% (2.02, 95% CI: 1.31, 3.11). Comparisons between treatments showed adalimumab combined DMARDs (0.59, 95% CI: 0.37, 0.95), etanercept(0.49, 95% CI: 0.28, 0.88), etanercept combined DMARDs (0.56, 95% CI: 0.35, 0.91), golimumab combined DMARDs (0.51, 95% CI: 0.31, 0.83) decreased the risk of infections compared with infliximab combined DMARDs ( supplementary Table 1 ). There was no statistically significant difference between other comparisons.
We did the global consistency test. The test result p-value was 0.6713. We also established local consistency and the p-value of the test result exceeded 0.05, which was considered local. According to the SUCRA analysis, infliximab combined DMARDs had the highest risk to cause infections (SUCRA = 0.910), while DMARDs had the lowest risk to cause infections SUCRA = 0.210) compared with the other 11 therapies ( Supplementary Figure 2 ). There was a funnel plot ( Supplementary Figure 3 ) with no obvious asymmetry, indicating no publication bias.
Serious Infections
55 articles (11–20, 22, 23, 26–38, 40, 42, 45, 47–49, 51, 52, 54, 56–60, 62–66, 68, 69, 72–77, 80–82) reported the occurrence of serious infections, involving a total of 24740 RA patients. The network of eligible comparisons was shown in the Supplementary Figure 4 . Network meta-analysis showed that there was no statistically significant difference between 12 therapies ( Supplementary Table 2 ).
We did the global consistency test. The resulting p-value was 0.4900. We also made local consistency and the test result p-value was greater than 0.05, which was considered to be locally consistent. According to the SUCRA analysis, certolizumab had the highest risk to cause serious infections (SUCRA =0.817), while etanercept combined DMARDs had the lowest risk to cause serious infections (SUCRA = 0.285) compared with the other 11 therapies ( Supplementary Figure 5 ). There was a funnel plot asymmetry, with the right corner of the pyramidal part of the funnel missing, which suggested a possible bias ( Supplementary Figure 6 ).
Malignant Tumors
32 articles (14–20, 23, 26, 27, 29–32, 34–39, 43, 47–49, 52, 57, 60, 65, 74, 75, 77, 79) reported the occurrence of malignant tumors, involving 16947 RA patients. The network of eligible comparisons was shown in the Supplementary Figure 7 . Mesh meta-analysis showed that there was no statistically significant difference between 12 therapies ( Supplementary Table 3 ).
We did the global consistency test. The test result p-value was 0.6219. We also made local consistency and the test result p-value was greater than 0.05, which was considered to be locally consistent. According to the SUCRA analysis ( Supplementary Figure 8 ), golimumab had the highest risk to cause malignant tumors (SUCRA =0.778), while golimumab combined DMARDs had the lowest risk to cause malignant tumors (SUCRA = 0.285) compared with the other 11 therapies.
Discussion
Based on the data and information of included RCTs, our study aims to evaluate the risk of adverse effects of 10 anti-TNF therapies in patients with rheumatoid arthritis. All available direct and indirect evidence of various treatment options was analyzed and compared simultaneously by network meta-analysis, which has a great advantage over traditional meta-analysis and makes up for the lack of head-to-head comparisons (83). To comprehensively assess the safety of anti-TNF therapies in RA patients, we also pay attention to detailed AEs like infections, serious infections, malignant tumors. What’s more, our meta-analysis included all RCTs with medium or high quality more recent studies to August 2021, which avoided the deficiency of observational studies and low-quality studies. Therefore, our studies are much more reliable than the other meta-analyses or network meta-analyses.
After analysis of 10 therapies for patients with RA from 72 RCTs, we found golimumab monotherapy, infliximab monotherapy, etanercept monotherapy, adalimumab monotherapy, and etanercept+DMARDs therapy are the safer treatments when the efficacies are similar, they did not increase the risk of all analyzed safety indexes. A comprehensive analysis of the results of network meta-analysis and SUCRA sequencing diagram of adverse reactions showed that etanercept monotherapy is the safest therapy of the 10 therapies was etanercept monotherapy. Etanercept monotherapy was recommended as an alternative treatment due to its good safety outcomes. Certolizumab+DMARDs was considered the worst therapy, so it was necessary to avoid using this therapy. Besides, etanercept may be able to reduce the expression and production of vascular endothelial growth factor, NO, and inducible NO synthase and contribute to having a beneficial effect upon the progression of atherosclerosis, reducing the risk of acute cardiovascular and/or cerebrovascular events (84). This is further demonstrated that etanercept therapy is safer. In 2014, Murdaca et al. investigated the role of single-nucleotide polymorphisms (SNPs) at positions -238, - 308, and + 489 of the TNF-a gene in the response to TNF-a inhibitors (adalimumab, etanercept, or infliximab) and found that the SNP + 489 G allele may promote the response to etanercept. Thus, genetic polymorphisms could be performed before treatment to determine suitability for the etanercept monotherapy (85).
After head-to-head comparisons for the effects of these 10 anti-TNF therapies on the risk of serious infections, malignant tumors, we found no difference of 10 therapies. And compared with PBO therapy or DMARDs therapy, these 10 anti-TNF therapies did not affect the risk of serious infections, malignant tumors, and tuberculosis infection. This may be indicated that these 10 anti-TNF therapies are safe for serious infections, malignant tumors, and tuberculosis infection.
Interestingly, among these 10 anti-TNF therapies, five are TNF-a inhibitor monotherapies and another five are TNF-α inhibitors combinations of DMARDs. It was easy to find that in most cases the safety of TNF-α inhibitor monotherapy was superior to the corresponding TNF-α inhibitors combinations of DMARDs. For example, the SUCRAs of safety outcomes for golimumab+ DMARDs are as follows: 59.1% (AEs), 94.0% (SAEs), and 57.5% (serious infections). By contrast, golimumab monotherapy was safer with corresponding SUCRAs of 53.5%, 16.7%, and 31.8%. Previous researchers have also conducted comparisons between TNF-α inhibitor monotherapy and TNF-α inhibitor combined with MTX. For instance, Breedveld et al. demonstrated that the proportions of RA patients inducing AEs and serious infections were higher under the treatment of adalimumab + DMARDs than the adalimumab monotherapy, which was in line with our results. However, some studies published before also presented no difference between the two kinds of treatment groups (86). Patients with RA treated with etanercept and those treated with etanercept + DMARDs were similar. Thus, further research should be conducted to estimate whether TNF-α inhibitor combined with DMARDs therapy benefits TNF-α inhibitor monotherapy or not.
Although we have made the study as comprehensive as possible, there are still some limitations. Firstly, even though the included trials were all RCTs, the results of safety comparisons among 10 drug therapies still showed some statistical inconsistency. Perhaps the RCTs with contradictions between direct and indirect evidence should be reconsidered. Secondly, 22 trials only had a follow-up time of fewer than 20 weeks. A short duration was not enough to judge the safety of treatment. Thirdly, medication dose, treatment cost, patient compliance, and other influential factors also affected trial homogeneity. Last but not least, different RCTs included in our research had different definitions of safety outcomes. There was still a shortage of clear definitions of AEs and SAEs.
In conclusion, we regard etanercept monotherapy as the optimal choice for RA patients in clinical practice when the efficacy was similar. Conversely, certolizumab+DMARDs therapy was not recommended. It was necessary to conduct long-term studies on patients with RA to provide a more complete assessment of diverse treatments and make a more judicious choice in clinical practice. All efforts should be made to improve the life quality and health standards for patients with RA.
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.
Author Contributions
W-xP, YL, and BH conceived this meta-analysis. YL and XC extracted data. H-rX provided statistical advice and Q-zZ did all statistical analyses. YL, BH, H-rX, and XC checked for statistical inconsistency and interpreted data. YL, BH, and W-wL contributed to data interpretation. YL, BH, and JH drafted the report. H-rX, XC, and JH critically reviewed the article. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2022.814429/full#supplementary-material
References
- 1. Smolen JS, Aletaha D, McInnes IB. Rheumatoid Arthritis. Lancet (2016) 388:2023–38. doi: 10.1016/S0140-6736(16)30173-8 [DOI] [PubMed] [Google Scholar]
- 2. Koga T, Kawakami A, Tsokos GC. Current Insights and Future Prospects for the Pathogenesis and Treatment for Rheumatoid Arthritis. Clin Immunol (2021) 225:108680. doi: 10.1016/j.clim.2021.108680 [DOI] [PubMed] [Google Scholar]
- 3. Bradley JR. TNF-Mediated Inflammatory Disease. J Pathol (2008) 214:149–60. doi: 10.1002/path.2287 [DOI] [PubMed] [Google Scholar]
- 4. Smolen JS, Landewé R, Bijlsma J, Burmester G, Chatzidionysiou K, Dougados M, Nam J, et al. EULAR Recommendations for the Management of Rheumatoid Arthritis With Synthetic and Biological Disease-Modifying Antirheumatic Drugs: 2016 Update. Ann Rheum Dis (2017) 76:960–77. doi: 10.1136/annrheumdis-2016-210715 [DOI] [PubMed] [Google Scholar]
- 5. Gottenberg JE, Morel J, Perrodeau E, Bardin T, Combe B, Dougados M, et al. Comparative Effectiveness of Rituximab, Abatacept, and Tocilizumab in Adults With Rheumatoid Arthritis and Inadequate Response to TNF Inhibitors: Prospective Cohort Study. BMJ (2019) 364:l67. doi: 10.1136/bmj.l67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Genovese MC, Fleischmann R, Kivitz A, Lee EB, Hoogstraten HV, Kimura T, et al. Efficacy and Safety of Sarilumab in Combination With csDMARDs or as Monotherapy in Subpopulations of Patients With Moderately to Severely Active Rheumatoid Arthritis in Three Phase III Randomized, Controlled Studies. Arthritis Res Ther (2020) 22:139. doi: 10.1186/s13075-020-02194-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dantes E, Tofolean DE, Fildan AP, Craciun L, Dumea E, Tofolean I, et al. Lethal Disseminated Tuberculosis in Patients Under Biological Treatment - Two Clinical Cases and a Short Review. J Int Med Res (2018) 46:2961–9. doi: 10.1177/0300060518771273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Papadopoulos CG, Gartzonikas IK, Pappa TK, Markatseli TE, Migkos MP, Voulgari PV, et al. Eight-Year Survival Study of First-Line Tumour Necrosis Factor Alpha Inhibitors in Rheumatoid Arthritis: Real-World Data From a University Centre Registry. Rheumatol Adv Pract (2019) 3:rkz007. doi: 10.1093/rap/rkz007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bongartz T, Sutton AJ, Sweeting MJ. Anti-TNF Antibody Therapy in Rheumatoid Arthritis and the Risk of Serious Infections and Malignancies: Systematic Review and Meta-Analysis of Rare Harmful Effects in Randomized Controlled Trials. JAMA (2006) 295:2275–85. doi: 10.1001/jama.295.19.2275 [DOI] [PubMed] [Google Scholar]
- 10. Maneiro JR, Souto A, Gomez-Reino JJ. Risks of Malignancies Related to Tofacitinib and Biological Drugs in Rheumatoid Arthritis: Systematic Review, Meta-Analysis, and Network Meta-Analysis. Semin Arthritis Rheum (2017) 47:149–56. doi: 10.1016/j.semarthrit.2017.02.007 [DOI] [PubMed] [Google Scholar]
- 11. Den Broeder A, van de Putte L, Rau R, Schattenkirchner M, Riel PV, Sander O, et al. A Single Dose, Placebo Controlled Study of the Fully Human Anti-Tumor Necrosis Factor-α Antibody Adalimumab (D2E7) in Patients With Rheumatoid Arthritis. J Rheumatol (2002) 29:2288–98. [PubMed] [Google Scholar]
- 12. Abe T, Takeuchi T, Miyasaka N, Hashimoto H, Kondo H, Ichikawa Y, et al. A Multicenter, Double-Blind, Randomized, Placebo Controlled Trial of Infliximab Combined With Low Dose Methotrexate in Japanese Patients With Rheumatoid Arthritis. J Rheumatol (2006) 33:37–44. [PubMed] [Google Scholar]
- 13. van de Putte LBA, Rau R, Breedveld FC, Kalden JR, Malaise MG, van Riel PLC M, et al. Efficacy and Safety of the Fully Human Anti-Tumour Necrosis Factor Alpha Monoclonal Antibody Adalimumab (D2E7) in DMARD Refractory Patients With Rheumatoid Arthritis: A 12 Week, Phase II Study. Ann Rheum Dis (2003) 62:1168–77. doi: 10.1136/ard.2003.009563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Weinblatt ME, Keystone EC, Furst DE, Moreland LW, Weisman MH, Birbara CA, et al. Adalimumab, A Fully Human Anti-Tumor Necrosis Factor Alpha Monoclonal Antibody, for the Treatment of Rheumatoid Arthritis in Patients Taking Concomitant Methotrexate: The ARMadalimumab Trial. Arthritis Rheum (2003) 48:35–45. doi: 10.1002/art.10697 [DOI] [PubMed] [Google Scholar]
- 15. Furst DE, Schiff MH, Fleischman n RM, Strand V, Birbara CA, Compagnone D, et al. Adalimumab, A Fully Human Anti-Tumor Necrosis Factor-α Monoclonal Antibody, and Concomitant Standard Antirheumatic Therapy for the Treatment of Rheumatoid Arthritis: Results of STAR (Safety Trial of Adalimumab in Rheumatoid Arthritis). J Rheumatol (2003) 30:2563–71. [PubMed] [Google Scholar]
- 16. Keystone EC, Kavanaugh AF, Sharp JT, Tannenbaum H, Hua Y, Teoh L, et al. Radiographic, Clinical, and Functional Outcomes of Treatment With Adalimumab (a Human Anti-Tumor Necrosis Factor Monoclonal Antibody) in Patients With Active Rheumatoid Arthritis Receiving Concomitant Methotrexate Therapy: A Randomized, Placebo-Controlled, 52-Week Trial. Arthritis Rheum (2004) 50:1400–11. doi: 10.1002/art.20217 [DOI] [PubMed] [Google Scholar]
- 17. Maini RN, Breedveld FC, Kalden JR, Smolen JS, Furst D, Weisman MH, et al. Sustained Improvement Over Two Years in Physical Function, Structural Damage, and Signs and Symptoms Among Patients With Rheumatoid Arthritis Treated With Infliximab and Methotrexate. Arthritis Rheum (2004) 50:1051–65. doi: 10.1002/art.20159 [DOI] [PubMed] [Google Scholar]
- 18. St.Clair EW, van der Heijde D, Smolen JS, Maini RN, Bathon JM, Emery P, et al. Combination of Infliximab and Methotrexate Therapy for Early Rheumatoid Arthritis: A Randomized, Controlled Trial. Arthritis Rheum (2004) 50:3432–43. doi: 10.1002/art.20568 [DOI] [PubMed] [Google Scholar]
- 19. van de Putte LB, Atkins C, Malaise M, Sany J, Russell AS, van Riel P, et al. Efficacy and Safety of Adalimumab as Monotherapy in Patients With Rheumatoid Arthritis for Whom Previous Disease Modifying Antirheumatic Drug Treatment Has Failed. Ann Rheum Dis (2004) 63:508–16. doi: 10.1136/ard.2003.013052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Breedveld FC, Weisman MH, Kavanaugh AF, Cohen SB, Pavelka K, Vollenhoven R, et al. The PREMIER Study: A Multicenter, Randomized, Double-Blind Clinical Trial of Combination Therapy With Adalimumab Plus Methotrexate Versus Methotrexate Alone or Adalimumab Alone in Patients With Early, Aggressive Rheumatoid Arthritis Who Had Not Had Previous Methotrexate Treatment. Arthritis Rheum (2006) 54:26–37. doi: 10.1002/art.21519 [DOI] [PubMed] [Google Scholar]
- 21. Lan JL, Chou SJ, Chen DY, Chen YH, Hsieh TY, Young M., Jr. A Comparative Study of Etanercept Plus Methotrexate and Methotrexate Alone in Taiwanese Patients With Active Rheumatoid Arthritis: A 12-Week, Double-Blind, Randomized, Placebo-Controlled Study. J Formos Med Assoc (2004) 103(8):618–23. [PubMed] [Google Scholar]
- 22. van Riel PL, Taggart AJ, Sany J, Gaubitz M, Nab HW, Pedersen R, et al. Efficacy and Safety of Combination Etanercept and Methotrexate Versus Etanercept Alone in Patients With Rheumatoid Arthritis With an Inadequate Response to Methotrexate: The ADORE Study. Ann Rheum Dis (2006) 65:1478–83. doi: 10.1136/ard.2005.043299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Westhovens R, Yocum D, Han J, Berman A, Strusberg I, Geusens P, et al. The Safety of Infliximab, Combined With Background Treatments, Among Patients With Rheumatoid Arthritis and Various Comorbidities: A Large, Randomized, Placebo-Controlled Trial. Arthritis Rheum (2006) 54:1075–86. doi: 10.1002/art.21734 [DOI] [PubMed] [Google Scholar]
- 24. Zhang FC, Hou Y, Huang F, Wu DH, Bao CD, Ni LQ, et al. Infliximab Versus Placebo in Rheumatoid Arthritis Patients Receiving Concomitant Methotrexate: A Preliminary Study From China. APLAR J Rheumatol (2006) 9:127–30. doi: 10.1111/j.1479-8077.2006.00186.x [DOI] [Google Scholar]
- 25. Kim HY, Lee SK, Song YW, Yoo DH, Koh EM, Yoo B, et al. A Randomized, Double-Blind, Placebo-Controlled, Phase III Study of the Human Anti-Tumor Necrosis Factor Antibody Adalimumab Administered as Subcutaneous Injections in Korean Rheumatoid Arthritis Patients Treated With Methotrexate. APLAR J Rheumatol (2007) 10:9–16. doi: 10.1111/j.1479-8077.2007.00248.x [DOI] [Google Scholar]
- 26. Van Der Heijde D, Klareskog L, Landewé R, Bruyn GAW, Cantagrel A, Durez P, et al. Disease Remission and Sustained Halting of Radiographic Progression With Combination Etanercept and Methotrexate in Patients With Rheumatoid Arthritis. Arthritis Rheum (2007) 56:3928–39. doi: 10.1002/art.23141 [DOI] [PubMed] [Google Scholar]
- 27. Weisman MH, Paulus HE, Burch FX, Kivitz AJ, Fierer J, Dunn M, et al. A Placebo-Controlled, Randomized, Double-Blinded Study Evaluating the Safety of Etanercept in Patients With Rheumatoid Arthritis and Concomitant Comorbid Diseases. Rheumatol (Oxford) (2007) 46:1122–5. doi: 10.1093/rheumatology/kem033 [DOI] [PubMed] [Google Scholar]
- 28. Bejarano V, Quinn M, Conaghan PG, Reece R, Keenan A-M, Walker D, et al. Effect of the Early Use of the Anti-Tumor Necrosis Factor Adalimumab on the Prevention of Job Loss in Patients With Early Rheumatoid Arthritis. Arthritis Rheum (2008) 59:1467–74. doi: 10.1002/art.24106 [DOI] [PubMed] [Google Scholar]
- 29. Emery P, Breedveld FC, Hall S, Durez P, Chang DJ, Robertson D, et al. Comparison of Methotrexate Monotherapy With a Combination of Methotrexate and Etanercept in Active, Early, Moderate to Severe Rheumatoid Arthritis (COMET): A Randomised, Double-Blind, Parallel Treatment Trial. Lancet (2008) 372:375–82. doi: 10.1016/s0140-6736(08)61000-4 [DOI] [PubMed] [Google Scholar]
- 30. Kay J, Matteson EL, Dasgupta B, Nash P, Durez PS, Hall S, et al. Golimumab in Patients With Active Rheumatoid Arthritis Despite Treatment With Methotrexate: A Randomized, Double-Blind, Placebo-Controlled, Dose-Ranging Study. Arthritis Rheum (2008) 58:964–75. doi: 10.1002/art.23383 [DOI] [PubMed] [Google Scholar]
- 31. Miyasaka N. Clinical Investigation in Highly Disease-Affected Rheumatoid Arthritis Patients in Japan With Adalimumab Applying Standard and General Evaluation: The CHANGE Study. Mod Rheumatol (2008) 18:252–62. doi: 10.1007/s10165-008-0045-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schiff M, Keiserman M, Codding C, Songcharoen S, Berman A, Nayiager S, et al. Efficacy and Safety of Abatacept or Infliximab vs Placebo in ATTEST: A Phase III, Multi-Centre, Randomised, Double-Blind, Placebo-Controlled Study in Patients With Rheumatoid Arthritis and an Inadequate Response to Methotrexate. Ann Rheum Dis (2008) 67:1096–103. doi: 10.1136/ard.2007.080002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chen DY, Chou SJ, Hsieh TY, Chen YH, Chen HH, Hsieh CW, et al. Randomized, Double-Blind, Placebo-Controlled, Comparative Study of Human Anti-TNF Antibody Adalimumab in Combination With Methotrexate and Methotrexate Alone in Taiwanese Patients With Active Rheumatoid Arthritis. J Formos Med Assoc (2009) 108:310–9. doi: 10.1016/s0929-6646(09)60071-1 [DOI] [PubMed] [Google Scholar]
- 34. Emery P, Fleischmann RM, Moreland LW, Hsia EC, Strusberg I, Durez P, et al. Golimumab, a Human Anti-Tumor Necrosis Factor α Monoclonal Antibody, Injected Subcutaneously Every Four Weeks in Methotrexate-Naive Patients With Active Rheumatoid Arthritis: Twenty-Four-Week Results of a Phase III, Multicenter, Randomized, Double-Blind, Placebo-Controlled Study of Golimumab Before Methotrexate as First-Line Therapy for Early-Onset Rheumatoid Arthritis. Arthritis Rheum (2009) 60:2272–83. doi: 10.1002/art.24638 [DOI] [PubMed] [Google Scholar]
- 35. Fleischmann R, Vencovsky J, van Vollenhoven RF, Borenstein D, Box J, Coteur G, et al. Efficacy and Safety of Certolizumab Pegol Monotherapy Every 4 Weeks in Patients With Rheumatoid Arthritis Failing Previous Disease-Modifying Antirheumatic Therapy: The FAST4WARD Study. Ann Rheum Dis (2009) 68:805–11. doi: 10.1136/ard.2008.099291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Keystone EC, Genovese MC, Klareskog L, Hsia EC, Hall ST, Miranda PC, et al. Golimumab, a Human Antibody to Tumour Necrosis Factor {Alpha} Given by Monthly Subcutaneous Injections, in Active Rheumatoid Arthritis Despite Methotrexate Therapy: The GO-FORWARD Study. Ann Rheum Dis (2009) 68:789–96. doi: 10.1136/ard.2008.099010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Smolen J, Landewé RB, Mease P, Brzezicki J, Mason D, Luijtens K, et al. Efficacy and Safety of Certolizumab Pegol Plus Methotrexate in Active Rheumatoid Arthritis: The RAPID 2 Study. A Randomised Controlled Trial. Ann Rheum Dis (2009) 68:797–804. doi: 10.1136/ard.2008.101659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Smolen JS, Kay J, Doyle MK, Landewé R, Matteson EL, Wollenhaupt J, et al. Golimumab in Patients With Active Rheumatoid Arthritis After Treatment With Tumour Necrosis Factor Alpha Inhibitors (GO-AFTER Study): A Multicentre, Randomised, Double-Blind, Placebo-Controlled, Phase III Trial. Lancet (2009) 374:210–21. doi: 10.1016/s0140-6736(09)60506-7 [DOI] [PubMed] [Google Scholar]
- 39. Genovese MC, Bathon JM, Martin RW, Fleischmann RM, Tesser JR, Schiff MH, et al. Etanercept Versus Methotrexate in Patients With Early Rheumatoid Arthritis: Two-Year Radiographic and Clinical Outcomes. Arthritis Rheum (2002) 46(6):1443–50. doi: 10.1002/art.10308 [DOI] [PubMed] [Google Scholar]
- 40. Kremer J, et al. Golimumab, a New Human Anti-Tumor Necrosis Factor α Antibody, Administered Intravenously in Patients With Active Rheumatoid Arthritis: Forty-Eight-Week Efficacy and Safety Results of a Phase III Randomized, Double-Blind, Placebo-Controlled Study. Arthritis Rheum (2010) 62:917–28. doi: 10.1002/art.27348 [DOI] [PubMed] [Google Scholar]
- 41. Kameda H, Kanbe K, Sato E, Ueki Y, Saito K, Nagaoka S, et al. Continuation of Methotrexate Resulted in Better Clinical and Radiographic Outcomes Than Discontinuation Upon Starting Etanercept in Patients With Rheumatoid Arthritis: 52-Week Results From the JESMR Study. J Rheumatol (2011) 38:1585–92. doi: 10.3899/jrheum.110014 [DOI] [PubMed] [Google Scholar]
- 42. Choy E, McKenna F, Vencovsky J, Valente R, Goel N, VanLunen B, et al. Certolizumab Pegol Plus MTX Administered Every 4 Weeks Is Effective in Patients With RA Who Are Partial Responders to MTX. Rheumatol (Oxford) (2012) 51:1226–34. doi: 10.1093/rheumatology/ker519 [DOI] [PubMed] [Google Scholar]
- 43. Jobanputra P, Maggs F, Deeming A, Carruthers D, Rankin E, Jordan AC, et al. A Randomised Efficacy and Discontinuation Study of Etanercept Versus Adalimumab (RED SEA) for Rheumatoid Arthritis: A Pragmatic, Unblinded, Non-Inferiority Study of First TNF Inhibitor Use: Outcomes Over 2 Years. BMJ Open (2012) 2(6):e001395. doi: 10.1136/bmjopen-2012-001395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kim HY, Hsu PN, Barba M, Sulaiman W, Robertson D, Vlahos B, et al. Randomized Comparison of Etanercept With Usual Therapy in an Asian Population With Active Rheumatoid Arthritis: The APPEAL Trial. Int J Rheum Dis (2012) 15:188–96. doi: 10.1111/j.1756-185X.2011.01680.x [DOI] [PubMed] [Google Scholar]
- 45. Tanaka Y, Harigai M, Takeuchi T, Yamanaka H, Ishiguro N, Yamamoto K, et al. Golimumab in Combination With Methotrexate in Japanese Patients With Active Rheumatoid Arthritis: Results of the GO-FORTH Study. Ann Rheum Dis (2012) 71:817–24. doi: 10.1136/ard.2011.200317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Van Vollenhoven RF, Fleischmann R, Cohen S, Lee EB, García Meijide JA, Wagner S, et al. Tofacitinib or Adalimumab Versus Placebo in Rheumatoid Arthritis. N Engl J Med (2012) 367:508–19. doi: 10.1056/NEJMoa1112072 [DOI] [PubMed] [Google Scholar]
- 47. Weinblatt ME, Fleischmann R WJ, Huizinga T, Emery P, Pope J, Massarotti EM, et al. Efficacy and Safety of Certolizumab Pegol in a Broad Population of Patients With Active Rheumatoid Arthritis: Results From the REALISTIC Phase IIIb Study. Rheumatol (Oxford) (2012) 51:2204–14. doi: 10.1093/rheumatology/kes150 [DOI] [PubMed] [Google Scholar]
- 48. Detert J, Bastian H, Listing J, Weiß A, Wassenberg S, Liebhaber A, et al. Induction Therapy With Adalimumab Plus Methotrexate for 24 Weeks Followed by Methotrexate Monotherapy Up to Week 48 Versus Methotrexate Therapy Alone for DMARD-Naïve Patients With Early Rheumatoid Arthritis: HIT HARD, Aninvestigator-Initiated Study. Ann Rheum Dis (2013) 72:844–50. doi: 10.1136/annrheumdis-2012-201612 [DOI] [PubMed] [Google Scholar]
- 49. Kavanaugh A, Fleischmann RM, Emery P, Kupper H, Redden L, Guerette B, et al. Clinical, Functional and Radiographic Consequences of Achieving Stable Low Disease Activity and Remission With Adalimumab Plus Methotrexate or Methotrexate Alone in Early Rheumatoid Arthritis: 26-Week Results From the Randomised, Controlled OPTIMA Study. Ann Rheum Dis (2013) 72:64–71. doi: 10.1136/annrheumdis-2011-201247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kim J, Ryu H, Yoo DH, Park SH, Song GG, Park PW, et al. A Clinical Trial and Extension Study of Infliximab in Korean Patients With Active Rheumatoid Arthritis Despite Methotrexate Treatment. J Korean Med Sci (2013) 28:1716–22. doi: 10.3346/jkms.2013.28.12.1716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Leirisalo-Repo M, Kautiainen H, Laasonen H, Korpela M, Kauppi MJ, Kaipiainen-Seppänen O, et al. Infliximab for 6 Months Added on Combination Therapy in Early Rheumatoid Arthritis: 2-Year Results From an Investigator-Initiated, Randomised, Double-Blind, Placebo-Controlled Study (the NEO-RACo Study). Ann Rheum Dis (2013) 72:851–7. doi: 10.1136/annrheumdis-2012-201365 [DOI] [PubMed] [Google Scholar]
- 52. Smolen JS, Nash P, Durez P, Hall P, Ilivanova E, Irazoque-Palazuelos F, et al. Maintenance, Reduction, or Withdrawal of Etanercept After Treatment With Etanercept and Methotrexate in Patients With Moderate Rheumatoid Arthritis (PRESERVE): A Randomised Controlled Trial. Lancet (2013) 381:918–29. doi: 10.1016/s0140-6736(12)61811-x [DOI] [PubMed] [Google Scholar]
- 53. Takeuchi T, Harigai M, Tanaka Y, Yamanaka H, Ishiguro N, Yamamoto K, et al. Golimumab Monotherapy in Japanese Patients With Active Rheumatoid Arthritis Despite Prior Treatment With Disease-Modifying Antirheumatic Drugs: Results of the Phase 2/3, Multicentre, Randomised, Double-Blind, Placebo-Controlled GO-MONO Study Through 24 Weeks. Ann Rheum Dis (2013) 72:1488–95. doi: 10.1136/annrheumdis-2012-201796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Takeuchi T, Miyasaka N, Zang C, Alvarez D, Fletcher T, Wajdula J, et al. A Phase 3 Randomized, Double-Blind, Multicenter Comparative Study Evaluating the Effect of Etanercept Versus Methotrexate on Radiographic Outcomes, Disease Activity, and Safety in Japanese Subjects With Active Rheumatoid Arthritis. Mod Rheumatol (2013) 23:623–33. doi: 10.1007/s10165-012-0742-6 [DOI] [PubMed] [Google Scholar]
- 55. Weinblatt ME, Bingham CO, Mendelsohn AM, Kim L, Mack M, Lu J, et al. Intravenous Golimumab Is Effective in Patients With Active Rheumatoid Arthritis Despite Methotrexate Therapy With Responses as Early as Week 2: Results of the Phase 3, Randomised, Multicentre, Double-Blind, Placebo-Controlled GO-FURTHER Trial. Ann Rheum Dis (2013) 72:381–9. doi: 10.1136/annrheumdis-2012-201411 [DOI] [PubMed] [Google Scholar]
- 56. Emery P, Hammoudeh M, FitzGerald O, Combe B, Martin-Mola E, H. Buch M, et al. Sustained Remission With Etanercept Tapering in Early Rheumatoid Arthritis. N Engl J Med (2014) 371:1781–92. doi: 10.1056/NEJMoa1316133 [DOI] [PubMed] [Google Scholar]
- 57. Hørslev-Petersen K, Hetland ML, Junker P, Pødenphant J, Ellingsen T, Ahlquist P, et al. Adalimumab Added to a Treat-to-Target Strategy With Methotrexate and Intra-Articular Triamcinolone in Early Rheumatoid Arthritis Increased Remission Rates, Function and Quality of Life. The OPERA Study: An Investigator-Initiated, Randomised, Double-Blind, Parallel-Group, Placebo-Controlled Trial. Ann Rheum Dis (2014) 73:654–61. doi: 10.1136/annrheumdis-2012-202735 [DOI] [PubMed] [Google Scholar]
- 58. Kennedy WP, Simon JA, Offutt C, Horn P, Herman A, Townsend MJ, et al. Efficacy and Safety of Pateclizumab (Anti-Lymphotoxin-α) Compared to Adalimumab in Rheumatoid Arthritis: A Head-to-Head Phase 2 Randomized Controlled Study (The ALTARA Study). Arthritis Res Ther (2014) 16:467. doi: 10.1186/s13075-014-0467-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Machado DA, Guzman RM, Xavier RM, Simon J, Abraham, Mele L, et al. Open-Label Observation of Addition of Etanercept Versus a Conventional Disease-Modifying Antirheumatic Drug in Subjects With Active Rheumatoid Arthritis Despite Methotrexate Therapy in the Latin American Region. J Clin Rheumatol (2014) 20:25–33. doi: 10.1097/rhu.0000000000000055 [DOI] [PubMed] [Google Scholar]
- 60. Nam JL, Villeneuve E, Hensor EMA, Wakefield RJ, Conaghan PG, Green MJ, et al. A Randomised Controlled Trial of Etanercept and Methotrexate to Induce Remission in Early Inflammatory Arthritis: The EMPIRE Trial. Ann Rheum Dis (2014) 73:1027–36. doi: 10.1136/annrheumdis-2013-204882 [DOI] [PubMed] [Google Scholar]
- 61. Schiff MH, von Kempis J, Goldblum R, Tesser JR, Mueller RB. Rheumatoid Arthritis Secondary Non-Responders to TNF can Attain an Efficacious and Safe Response by Switching to Certolizumab Pegol: A Phase IV, Randomised, Multicentre, Double-Blind, 12-Week Study, Followed by a 12-Week Open-Label Phase. Ann Rheum Dis (2014) 73:2174–7. doi: 10.1136/annrheumdis-2014-205325 [DOI] [PubMed] [Google Scholar]
- 62. Takeuchi T, Yamanaka H, Ishiguro N, Miyasaka N, Mukai M, Matsubara T, et al. Adalimumab, a Human Anti-TNF Monoclonal Antibody, Outcome Study for the Prevention of Joint Damage in Japanese Patients With Early Rheumatoid Arthritis: The HOPEFUL 1 Study. Ann Rheum Dis (2014) 73:536–43. doi: 10.1136/annrheumdis-2012-202433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Yamamoto K, Takeuchi T, Yamanaka H, Ishiguro N, Tanaka Y, Eguchi K, et al. Efficacy and Safety of Certolizumab Pegol Plus Methotrexate in Japanese Rheumatoid Arthritis Patients With an Inadequate Response to Methotrexate: The J-RAPID Randomized, Placebo-Controlled Trial. Mod Rheumatol (2014) 24:715–24. doi: 10.3109/14397595.2013.864224 [DOI] [PubMed] [Google Scholar]
- 64. Furst DE, Shaikh SA, Greenwald M, Bennett B, Davies O, Luijtens K, et al. Two Dosing Regimens of Certolizumab Pegol in Patients With Active Rheumatoid Arthritis. Arthritis Care Res (Hoboken) (2015) 67:151–60. doi: 10.1002/acr.22496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Smolen JS, Emery P, Ferraccioli GF, Samborski W, Berenbaum F, Davies OR, et al. Certolizumab Pegol in Rheumatoid Arthritis Patients With Low to Moderate Activity: The CERTAIN Double-Blind, Randomised, Placebo-Controlled Trial. Ann Rheum Dis (2015) 74:843–50. doi: 10.1136/annrheumdis-2013-204632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Atsumi T, Yamamoto K, Takeuchi T, Yamanaka H, Ishiguro N, Tanaka Y, et al. The First Double-Blind, Randomised, Parallel-Group Certolizumab Pegol Study in Methotrexate-Naive Early Rheumatoid Arthritis Patients With Poor Prognostic Factors, C-OPERA, Shows Inhibition of Radiographic Progression. Ann Rheum Dis (2016) 75:75–83. doi: 10.1136/annrheumdis-2015-207511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Keystone EC, Pope JE, Thorne JC, Poulin-Costello M, Phan-Chronis K, Vieira A, et al. Two-Year Radiographic and Clinical Outcomes From the Canadian Methotrexate and Etanercept Outcome Study in Patients With Rheumatoid Arthritis. Rheumatol (Oxford) (2016) 55:327–34. doi: 10.1093/rheumatology/kev338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Li Z, Zhang F, Kay J, Fei K, Han C, Zhuang Y, et al. Efficacy and Safety Results From a Phase 3, Randomized, Placebo-Controlled Trial of Subcutaneous Golimumab in Chinese Patients With Active Rheumatoid Arthritis Despite Methotrexate Therapy. Int J Rheum Dis (2016) 19:1143–56. doi: 10.1111/1756-185x.12723 [DOI] [PubMed] [Google Scholar]
- 69. Smolen JS, Burmester GR, Combe B, Curtis JR, Hall S, Haraoui B, et al. Head-To-Head Comparison of Certolizumab Pegol Versus Adalimumab in Rheumatoid Arthritis: 2-Year Efficacy and Safety Results From the Randomised EXXELERATE Study. Lancet (2016) 388:2763–74. doi: 10.1016/s0140-6736(16)31651-8 [DOI] [PubMed] [Google Scholar]
- 70. van Vollenhoven RF, Østergaard M, Leirisalo-Repo M, Uhlig T, Jansson M, Larsson E, et al. Full Dose, Reduced Dose or Discontinuation of Etanercept in Rheumatoid Arthritis. Ann Rheum Dis (2016) 75:52–8. doi: 10.1136/annrheumdis-2014-205726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Yamanaka H, Nagaoka S, Lee SK, Bae SC, Kasama T, Kobayashi H, et al. Discontinuation of Etanercept After Achievement of Sustained Remission in Patients With Rheumatoid Arthritis Who Initially Had Moderate Disease Activity—Results From the ENCOURAGE Study, A Prospective, International, Multicenter Randomized Study. Modern Rheumatol (2016) 26:651–61. doi: 10.3109/14397595.2015.1123349 [DOI] [PubMed] [Google Scholar]
- 72. Emery P, Bingham CO, Burmester GR, Bykerk VP, Furst DE, Mariette X, et al. Certolizumab Pegol in Combination With Dose-Optimised Methotrexate in DMARD-Naïve Patients With Early, Active Rheumatoid Arthritis With Poor Prognostic Factors: 1-Year Results From C-EARLY, A Randomised, Double-Blind, Placebo-Controlled Phase III Study. Ann Rheum Dis (2017) 76:96–104. doi: 10.1136/annrheumdis-2015-209057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Pavelka K, Akkoç N, Al- Maini M, Zerbini C, Karateev DE, Nasonov EL, et al. Maintenance of Remission With Combination Etanercept–DMARD Therapy Versus DMARDs Alone in Active Rheumatoid Arthritis: Results of an International Treat-to-Target Study Conducted in Regions With Limited Biologic Access. Rheumatol Int (2017) 37:1469–79. doi: 10.1007/s00296-017-3749-7 [DOI] [PubMed] [Google Scholar]
- 74. Taylor PC, Keystone FC, van der Heide D, Weinblatt ME, del Carmen Morales L, Gonzaga JR, et al. Baricitinib Versus Placebo or Adalimumab in Rheumatoid Arthritis. N Engl J Med (2017) 376:652–62. doi: 10.1056/NEJMoa1608345 [DOI] [PubMed] [Google Scholar]
- 75. Kang YM, Park YE, Park W, Choe JY, Cho CS, Shim SC, et al. Rapid Onset of Efficacy Predicts Response to Therapy With Certolizumab Plus Methotrexate in Patients With Active Rheumatoid Arthritis. Korean J Intern Med (2018) 33:1224–33. doi: 10.3904/kjim.2016.213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Bi L, Li Y, He L, Xu H, Jiang Z, Wang Y, et al. Efficacy and Safety of Certolizumab Pegol in Combination With Methotrexate in Methotrexate-Inadequate Responder Chinese Patients With Active Rheumatoid Arthritis: 24-Week Results From a Randomised, Double-Blind, Placebo-Controlled Phase 3 Study. Clin Exp Rheumatol (2019) 37:227–34. [PubMed] [Google Scholar]
- 77. Fleischmann R, Pangan A, Song IH, Mysler E, Bessette L, Peterfy C, et al. Upadacitinib Versus Placebo or Adalimumab in Patients With Rheumatoid Arthritis and an Inadequate Response to Methotrexate: Results of a Phase III, Double-Blind, Randomized Controlled Trial. Arthritis Rheumatol (2019) 71:1788–800. doi: 10.1002/art.41032 [DOI] [PubMed] [Google Scholar]
- 78. Ducourau E, Rispens T, Samain M, Dernis E, Guilchard FE, Andras L, et al. Methotrexate Effect on Immunogenicity and Long-Term Maintenance of Adalimumab in Axial Spondyloarthritis: A Multicentric Randomised Trial. RMD Open (2020) 6(1):e001047. doi: 10.1136/rmdopen-2019-001047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Hetland ML, Haavardsholm EA, Rudin A, Nordström D, Nurmohamed M, Gudbjornsson B, et al. Active Conventional Treatment and Three Different Biological Treatments in Early Rheumatoid Arthritis: Phase IV Investigator Initiated, Randomised, Observer Blinded Clinical Trial. BMJ (Clinical Res ed.) (2020) 371:m4328. doi: 10.1136/bmj.m4328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Takeuchi T, Miyasaka N, Pedersen R, Sugiyama N, Hirose T. Radiographic and Clinical Outcomes Following Etanercept Monotherapy in Japanese Methotrexate-Naïve Patients With Active Rheumatoid Arthritis. Mod Rheumatol (2020) 30:259–68. doi: 10.1080/14397595.2019.1589918 [DOI] [PubMed] [Google Scholar]
- 81. Combe B, Kivitz A, Tanaka Y, van der Heijde D, Simon JA, Baraf HSB, et al. Filgotinib Versus Placebo or Adalimumab in Patients With Rheumatoid Arthritis and Inadequate Response to Methotrexate: A Phase III Randomised Clinical Trial. Ann Rheum Dis (2021) 80:848–58. doi: 10.1136/annrheumdis-2020-219214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Curtis JR, Emery P, Karis E, Haraoui B, Bykerk V, Yen PK, et al. Etanercept or Methotrexate Withdrawal in Rheumatoid Arthritis Patients in Sustained Remission. Arthritis Rheumatol (2021) 73:759–68. doi: 10.1002/art.41589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Jansen JP, Fleurence R, Devine B, Boersma C, Annemans L, Cappelleri JC, et al. Interpreting Indirect Treatment Comparisons and Network Meta-Analysis for Health-Care Decision Making: Report of the ISPOR Task Force on Indirect Treatment Comparisons Good Research Practices: Part 1. Value Health (2011) 14:417–28. doi: 10.1016/j.jval.2011.04.002 [DOI] [PubMed] [Google Scholar]
- 84. Murdaca G, Spanò F, Cagnati P, Puppo F. Free Radicals and Endothelial Dysfunction: Potential Positive Effects of TNF-α Inhibitors. Redox Rep (2013) 18:95–9. doi: 10.1179/1351000213Y.0000000046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Murdaca G, Gulli R, Spanò F, Lantieri F, Burlando M, Parodi A, et al. TNF-Alpha Gene Polymorphisms: Association With Disease Susceptibility and Response to Anti-TNF-Alpha Treatment in Psoriatic Arthritis. J Invest Dermatol (2014) 134:2503–9. doi: 10.1038/jid.2014.123 [DOI] [PubMed] [Google Scholar]
- 86. van Riel PL, Taggart AJ, Sany J, Gaubitz M, Nab HW, Pedersen R, et al. Efficacy and Safety of Combination Etanercept and Methotrexate Versus Etanercept Alone in Patients With Rheumatoid Arthritis With an Inadequate Response to Methotrexate: The ADORE Study. Ann Rheum Dis (2006) 65:1478–83. doi: 10.1136/ard.2005.043299 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.