Abstract
Introduction
Xanthogranulomatous orchitis is an extremely rare condition of the test is marked by the necrosis and effacement of testicular parenchyma by an inflammatory process. The current study aims to report a case of xanthogranulomatous epididymo-orchitis.
Case report
A 35-year-old man presented with a history of recurrent attacks of dull pain and swelling of the right side of the scrotum for 3 weeks. He denied having any history of trauma or urinary symptoms. Physical examination revealed tenderness and warmth of the right side of the scrotum. Urine culture was negative. The patient managed operatively.
Discussion
The underlying pathophysiology of xanthogranulomatous orchitis is yet unknown. The pathogenesis of this inflammatory process in the testis is frequently driven by obstruction of the epididymis or the urinary tract. Urinary tract infection has also been considered as an etiologic factor.
Conclusion
Xanthogranulomatous orchitis is an uncommon testicular inflammatory condition. Histopathologic examination is required for definitive diagnosis and for the exclusion of occult germ cell malignancy.
Keywords: Xanthogranulmatous inflammation, Xanthogranulomatous orchitis, Xanthogranulomatous epididymitis, Testicular tumor
Highlights
-
•
Xanthogranulomatous inflammation is a rare, non-neoplastic disease.
-
•
It is responsible for approximately 0.6% to 1.4% of all renal infections.
-
•
On rare occasions, it can involve the prostate, epididymis, and testicles.
-
•
Only a limited number of cases have been published in the literature.
1. Introduction
Xanthogranulomatous inflammation (XGI) is a rare, non-neoplastic disease characterized by tissue damage and a prominent infiltrate of lipid-laden macrophages [1]. Although it commonly affects the kidneys and gallbladder, it can also affect the liver, appendix, ovaries, vagina, bones, and urinary bladder [2]. It is responsible for approximately 0.6% to 1.4% of all renal infections [2]. On rare occasions, it can affect the prostate, epididymis, and testicles. The specific pathophysiology is still unclear [3]. When it affects the testes, it's known as xanthogranulomatous orchitis (XGO), a rare benign disease of the testes marked by the death of testicular tissue and its subsequent replacement by an infiltrate of lipid-laden macrophage [4]. XGO is a rare occurrence; only a few cases have thus far been published in the literature [5].
The current study aims to report a rare occurrence of xanthogranulomatous epididymo-orchitis (XGEO) in a 35-year-old man. The report has been arranged in line with SCARE guidelines and includes a brief literature review [6].
2. Case report
2.1. Patient's information
A 35-year-old man presented with a history of recurrent attacks of right-sided scrotal dull pain and swelling for 3 weeks' duration. These symptoms were accompanied by fever, myalgia, and weakness. Two weeks prior, he had been seen for the same complaint, diagnosed as epididymo-orchitis, and received a 10-day course of antibiotics, but he had shown no response to the treatment. He denied having a history of trauma, recent sexual contact, urethral discharge, or urinary symptoms.
2.2. Clinical examination
Physical examination revealed tenderness, erythema, warmth, and swelling of the right side of the scrotum, with an overlying scrotal wall abscess.
2.3. Diagnostic assessment
Urine culture was negative. Ultrasound (US) of the testis demonstrated reduced vascularity of the right testis with a heterogeneous texture and a 55-mm multilocular scrotal collection. Complete blood count (CBC) revealed leukocytosis, and C-reactive protein level was elevated to 21.2 mg/dl. Serum tumor markers were within the laboratory reference range. Scrotal exploration was performed. The scrotal abscess was drained and the purulent material was sent for culture and sensitivity, revealing heavy growth of E. coli. The testis was necrotic and destroyed.
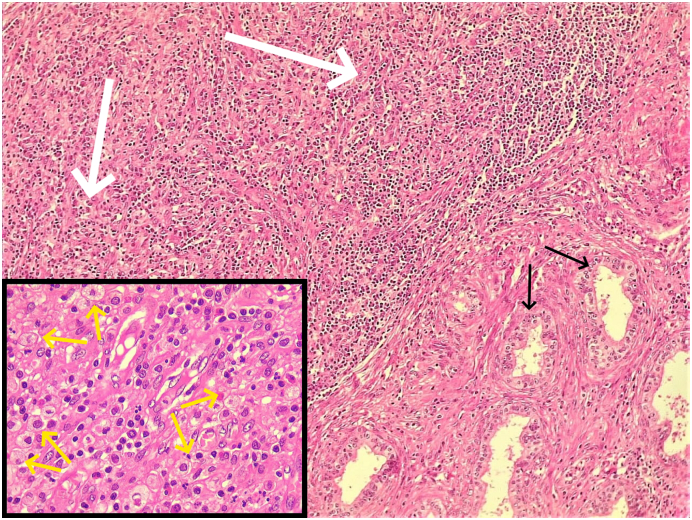
Therapeutic intervention: Simple orchidectomy was performed and the wound was washed with warm normal saline (Fig. 1). On the second postoperative day, the patient was discharged home on antibiotics, analgesics, and daily wound care. Histopathologic examination revealed heavy mixed inflammatory cell infiltration of the testicular parenchyma, rete testis, and epididymal tissue with complete destruction of the seminiferous tubules, associated with liquefactive necrosis, suppuration, and extensive fibrosis as well as accumulation of foamy histiocytes and multinucleated giant cells (Fig. 2). The histologic picture was consistent with XGEO associated with abscess formation.
Fig. 1.
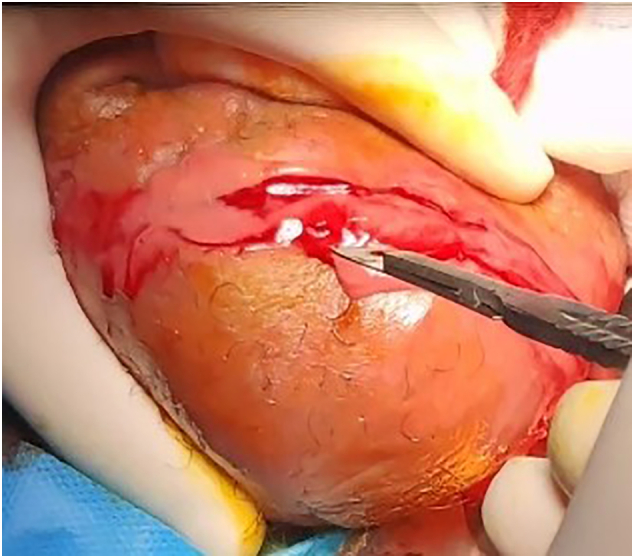
Intraoperative appearance of the pathology.
Fig. 2.
Microscopic examination of the testis shows diffuse effacement of the parenchyma by sheets of chronic inflammatory cells (white arrows) with a predominance of lymphocytes and histiocytes. There are no recognizable seminiferous tubules left, but remaining efferent ductules (black arrows) are noted. Higher magnification (inset) shows foamy histiocytes (yellow arrows) scattered among the inflammatory infiltrate. (Main: Hematoxylin and eosin stain, 10× magnification; inset: Hematoxylin and eosin stain, 40× magnification). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
2.4. Follow-up
The patient recovered without any complications and was discharged from the hospital on oral antibiotics and analgesics.
3. Discussion
XGI is a destructive process that reflects a stage in chronic suppuration in which stasis and host-microbe interactions give birth to a localized proliferation rich in macrophages and copious phagocytic material with distinct gross and microscopic characteristics. Macrophages are lipid-rich cells that are connected to gram-negative infections [7]. Although the exact cause is yet unknown, ascending or hematogenous infection is thought to be the most common [8]. A review of published cases demonstrated a predilection for this condition in the third to seventh decades of life [9]. XGO is a rare non-neoplastic destructive inflammatory condition of the testis that can result in a tumefactive lesion, mimicking malignant processes [10]. Young and elderly individuals are both susceptible to XGO. In most cases, the presentation is unilateral; however, bilateral cases have been observed. For unclear reasons, the right testis is more usually affected than the left [4]. Diabetes mellitus (DM) and spinal cord injury have been linked to the condition [7]. The current case was 35 years old and presented with unilateral right sided scrotal pain. He had a negative history of chronic disease and spinal cord injury.
The underlying pathophysiology of XGI is yet unknown. One of the most prominent etiologic determinants in the pathogenesis of this process in the testis is obstruction of the epididymis or the urinary tract [11]. The blockage of the spermatic cord can be mechanical, as in individuals who have had a prostatectomy or transurethral prostate resection, or functional, as in patients with diabetes mellitus who have neuropathy or in patients with spinal cord damage [9]. Urinary tract infection has also been considered as an etiologic agent [12]. Due to the chronic nature of the condition and the frequent unscrupulous use of broad-spectrum antibiotic regimens prior to microbiologic analysis, pathogenic bacteria are seldom detected by urine culture in the majority of patients [9]. There have been a few XGO case reports in which Escherichia coli and Pseudomonas aeruginosa were cultured [3]. The condition has been shown to occur following even blunt testicular trauma [8]. Although the exact pathophysiology of the trauma that causes XGI remains unclear, two hypotheses are being investigated: One theory postulates that macrophages invade the trauma-induced hematoma, resulting in XGO, whereas the second proposal is that macrophages enter necrotic tissue resulting from vascular injury [8]. The current case denied having prior infection or trauma to the testicles.
XGO has also been reported in older people subsequent to testicular ischemia resulting from atherosclerosis and in younger patients suffering from endarteritis or endo-phlebitis [12]. It may also occur as a local response to a coexistent tumor [2]. Urine reflux into the seminal vesicles or vasa deferentia, as well as urethral manipulation (catheterization or surgery), have been considered as potential risk factors for the development of the inflammatory process [13]. Other rare contributing factors include malnutrition, aberrant lipid metabolism, and lipid buildup in macrophages [2].
Preoperative diagnosis of XGO can be taxing due to the clinical and radiological overlap with testicular neoplasms. Both entities manifest with painless, tumefactive testicular enlargement and can generate the impression of a mass lesion on radiologic studies [10]. Imaging thus has negligible impact on the diagnosis of XGO [14]. The present case had dull pain and swelling in the right scrotum and US demonstrated reduced vascularity of the right testis with a heterogeneous texture and a multilocular scrotal collection. Scrotal ultrasound can assist in differentiating XGO from other acute scrotal disorders, including torsion, but no specific ultrasonographic features can distinguish XGO from testicular malignancies [4]. Preoperatively, elevated serum tumor biomarkers provide a clue to the diagnosis of testicular malignancy. However, serum tumor markers can be normal in some testicular neoplasms, making differentiation between the two disorders even more difficult and necessitating histopathologic examination of the resected tissue for definitive diagnosis [10]. The characteristic microscopic finding in XGO is the detection of aggregates of foamy histiocytes admixed with a heterogeneous inflammatory cell infiltrate, causing widespread destruction and effacement of the testicular parenchyma [10]. Histopathologic examination of the current case revealed extensive mixed inflammatory cell infiltration of the testicular parenchyma, rete testis, and epididymal tissue, as well as complete destruction of the seminiferous tubules, liquefactive necrosis, suppuration, extensive fibrosis, and accumulation of foamy histiocytes with multinucleated giant cells. The histopathologic differential diagnoses of XGO include infectious epididymo-orchitis, malakoplakia, Rosai-Dorfman disease, lepromatous orchitis, and idiopathic granulomatous orchitis [3]. A testicular neoplasm may coexist with XGO. Val-Bernal et al. described a case of XGO with an occult classical seminoma. Considering this possibility, histopathologic examination is of paramount importance and is the only definitive evidence for diagnosing XGI and for ruling out an occult malignancy [7]. Antibiotics may help with epididymo-orchitis. The presence of characteristic Michaelis–Gutmann bodies, coupled with macrophages having a granular eosinophilic or vacuolated cytoplasm, distinguishes malakoplakia from XGI [15].
Because tissue damage is a characteristic of XGI, definitive and curative therapy in most cases resides in surgical excision of the damaged organ, either completely or partially [5]. Antimicrobial treatment is suggested for anaerobic infections as anaerobes are recognized as a potential etiologic agent for XGI [1]. The current therapeutic gold standard is orchiectomy. However, histologic confirmation should be obtained in all patients, particularly in young patients and in those with a single testis, to avoid unnecessary radical orchiectomy, ineffective irradiation, and non-indicated chemotherapy [4]. In the present case, after surgical exploration revealed necrotic and destroyed testicular tissue, the patient underwent simple orchidectomy.
In conclusion, XGO is an uncommon testicular inflammatory condition. Pathologic examination is required for definitive diagnosis and for the exclusion of any occult germ cell malignancy.
Consent
Written informed consent was obtained from the patient's family for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
None is found.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Approval is not necessary for case report (till 3 cases in single report) in our locality.
The family gave consent for the publication of the report.
Guarantor
Fahmi Hussein Kakamad.
Research registration
Not applicable.
CRediT authorship contribution statement
Abdulwahid M. Salh: major contribution of the idea, literature review, final approval of the manuscript.
Rawa Bapir: Surgeon performing the operation, final approval of the manuscript.
Fahmi H. Kakamad: Writing the manuscript, literature review, final approval of the manuscript.
Shvan H. Mohammed, Rawa M. Ali, Dahat A. Hussien, Diyar A. Omar: literature review, final approval of the manuscript.
Declaration of competing interest
None to be declared.
References
- 1.Vaidyanathan S., Mansour P., Parsons K.F., Singh G., Soni B.M., Subramaniam R., et al. Xanthogranulomatous funiculitis and epididymo-orchitis in a tetraplegic patient. Spinal Cord. 2000;38(12):769–772. doi: 10.1038/sj.sc.3101045. [DOI] [PubMed] [Google Scholar]
- 2.Alazab R.S., Ghawanmeh H.M., Al-Okour R.K., Alshammari A., Lafi T., Al-Karasneh A.I., et al. Xanthogranulomatous orchitis: rare case with brief literature review. Urol. Case Rep. 2017;13:92–93. doi: 10.1016/j.eucr.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma P., Ramteke P., Satapathy A., Ray M.D. Xanthogranulomatous orchitis presenting as a scrotal mass in an elderly male: malignancy or mimicker? Clin. Med. Insights Case Rep. 2019;12:1–4. doi: 10.1177/1179547619890295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salako A.A., Olasode B.J., Eziyi A.K., Osasan S.A. Xanthogranulomatous orchitis in an adult Nigerian. Int. J. Urol. 2006;13(2):186–188. doi: 10.1111/j.1442-2042.2006.01258.x. [DOI] [PubMed] [Google Scholar]
- 5.Al-Said S., Ali A., Alobaidy A.K., Mojeeb E., Al-Naimi A., Shokeir A.A. Xanthogranulomatous orchitis: review of the published work and report of one case. Int. J. Urol. 2007;14(5):452–454. doi: 10.1111/j.1442-2042.2006.01714.x. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., et al. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Val-Bernal J.F., Argueta L., Fernández-Flórez A., Correas M.A., Val D., Garijo M.F., et al. Bilateral xanthogranulomatous orchitis in a tetraplegic patient. Pathol.Res. Pract. 2012;208(1):62–64. doi: 10.1016/j.prp.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Yamashita S., Umemoto H., Kohjimoto Y., Hara I. Xanthogranulomatous orchitis after blunt testicular trauma mimicking a testicular tumor: a case report and comparison with published cases. Urol. J. 2017;14(3):3094–3096. [PubMed] [Google Scholar]
- 9.Amin Said S.H., Abdalla R.Y., Aghaways I., Abdullah A.M. Xanthogranulomatous orchitis: review of the published work, and report of one case. Urol. Case Rep. 2019 Nov;1(27) doi: 10.1016/j.eucr.2019.100908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murshed K.A., Taha N.M., Ben-Gashir M. A case of xanthogranulomatous orchitis and its preoperative diagnostic challenges. Urol. Case Rep. 2020;32 doi: 10.1016/j.eucr.2020.101248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nistal M., Gonzalez-Peramato P., Serrano A., Regadera J. Xanthogranulomatous funiculitis and orchiepididymitis: report of 2 cases with immunohistochemical study and literature review. Arch. Pathol. Lab. Med. 2004;128(8):911–914. doi: 10.5858/2004-128-911-XFAORO. [DOI] [PubMed] [Google Scholar]
- 12.Ezer S.S., Oguzkurt P., Temiz A., Bal N., Hicsonmez A. Xanthogranulomatous orchiepididymitis: a very uncommon cause of scrotal mass in childhood. Urology. 2013;82(1):228–230. doi: 10.1016/j.urology.2013.01.039. [DOI] [PubMed] [Google Scholar]
- 13.Mannan A.A., Kahvic M., Sara Y.A., Bharati C. An unusual case of extensive xanthogranulomatous orchitis in a diabetic patient. Med. Princ. Pract. 2009;18(5):418–421. doi: 10.1159/000226299. [DOI] [PubMed] [Google Scholar]
- 14.Hill J.R., Gorgon G., Wahl S.J., Armenakas N.A., Fracchia J.A. Xanthogranulomatous orchitis in a patient with a history of instrumentation and bacillus calmette-guerin therapy. Urology. 2008;72(2):461–e11. doi: 10.1016/j.urology.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 15.Hajri M., Amna M.B., Derouich A., Ayed M., Zermani F., Jilani S.B. Orchites xanthogranulomateuses. À propos de sept cas. 2001;35(4):237–239. doi: 10.1016/s0003-4401(01)00028-6. [DOI] [PubMed] [Google Scholar]