Abstract
Dengue fever, a very old disease, has reemerged in the past 20 years with an expanded geographic distribution of both the viruses and the mosquito vectors, increased epidemic activity, the development of hyperendemicity (the cocirculation of multiple serotypes), and the emergence of dengue hemorrhagic fever in new geographic regions. In 1998 this mosquito-borne disease is the most important tropical infectious disease after malaria, with an estimated 100 million cases of dengue fever, 500,000 cases of dengue hemorrhagic fever, and 25,000 deaths annually. The reasons for this resurgence and emergence of dengue hemorrhagic fever in the waning years of the 20th century are complex and not fully understood, but demographic, societal, and public health infrastructure changes in the past 30 years have contributed greatly. This paper reviews the changing epidemiology of dengue and dengue hemorrhagic fever by geographic region, the natural history and transmission cycles, clinical diagnosis of both dengue fever and dengue hemorrhagic fever, serologic and virologic laboratory diagnoses, pathogenesis, surveillance, prevention, and control. A major challenge for public health officials in all tropical areas of the world is to devleop and implement sustainable prevention and control programs that will reverse the trend of emergent dengue hemorrhagic fever.
Although first reports of major epidemics of an illness thought to possibly be dengue occurred on three continents (Asia, Africa, and North America) in 1779 and 1780 (73, 75, 109, 128), reports of illnesses clinically compatible with dengue fever occurred even earlier. The earliest record found to date is in a Chinese encyclopedia of disease symptoms and remedies, first published during the Chin Dynasty (265 to 420 A.D.) and formally edited in 610 A.D. (Tang Dynasty) and again in 992 A.D. (Northern Sung Dynasty) (108). The disease was called water poison by the Chinese and was thought to be somehow connected with flying insects associated with water. Outbreaks of illness in the French West Indies in 1635 and in Panama in 1699 could also have been dengue (75, 103). Thus, dengue or a very similar illness had a wide geographic distribution before the 18th century, when the first known pandemic of dengue-like illness began. It is uncertain whether the epidemics in Batavia (Jakarta), Indonesia, and Cairo, Egypt, in 1779 were dengue, but it is quite likely that the Philadelphia epidemic of 1780 was dengue (19). A more detailed discussion of the history of dengue viruses has recently been published (41).
EMERGENCE OF DENGUE AS A GLOBAL PUBLIC HEALTH PROBLEM
The disease pattern associated with dengue-like illness from 1780 to 1940 was characterized by relatively infrequent but often large epidemics. However, it is likely that dengue viruses became endemic in many tropical urban centers during this time because during interepidemic periods, when there was no apparent disease transmission, nonimmune visitors invariably contracted a dengue-like illness within months of their arrival.
The ecologic disruption in the Southeast Asia and Pacific theaters during and following World War II created ideal conditions for increased transmission of mosquito-borne diseases, and it was in this setting that a global pandemic of dengue began. With increased epidemic transmission, hyperendemicity (the cocirculation of multiple dengue virus serotypes) developed in Southeast Asian cities and epidemic dengue hemorrhagic fever (DHF), a newly described disease, emerged (37, 48, 61, 63). The first known epidemic of DHF occurred in Manila, Philippines, in 1953 to 1954, but within 20 years the disease in epidemic form had spread throughout Southeast Asia; by the mid-1970s, DHF had become a leading cause of hospitalization and death among children in the region (1). In the 1970s, dengue was reintroduced to the Pacific Islands and epidemic activity increased there and in the Americas. During the 1980s and 1990s, epidemic dengue transmission intensified, and there is now a global resurgence of dengue fever, with expanding geographic distribution of both the mosquito vectors and the viruses, increased incidence of disease caused by an increased frequency of epidemic transmission, and the emergence of DHF in many new countries (36, 39, 41, 45, 48, 61, 63, 110, 111, 124).
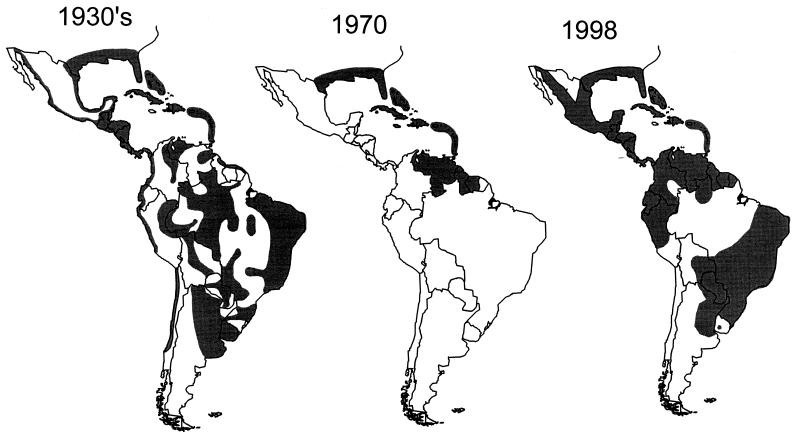
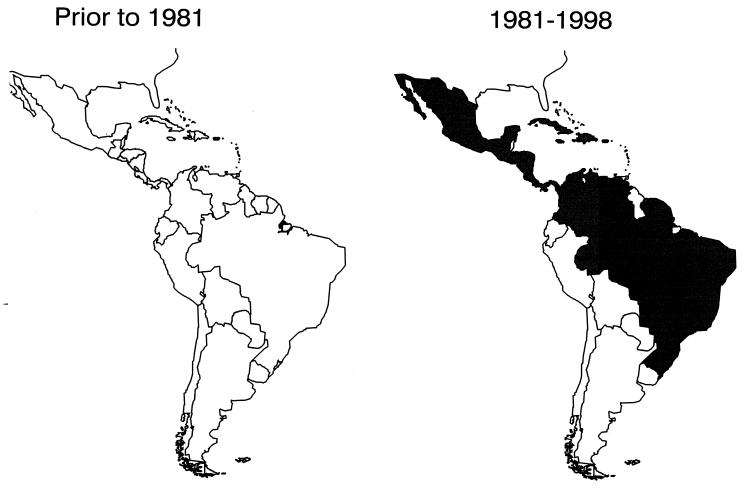
In Asia, epidemic DHF has expanded geographically from Southeast Asian countries west to India, Sri Lanka, the Maldives, and Pakistan and east to China (42). Several island countries of the South and Central Pacific (Niue, Palau, Yap, Cook Islands, Tahiti, New Caledonia, and Vanuatu) have experienced major or minor DHF epidemics (41). Epidemiologic changes in the Americas, however, have been the most dramatic. In the 1950s, 1960s, and most of the 1970s, epidemic dengue was rare in the American region because the principal mosquito vector, Aedes aegypti, had been eradicated from most of Central and South America (36–38, 110). The eradication program was discontinued in the early 1970s, and this species then began to reinvade the countries from which it had been eradicated (38, 110). By the 1990s, A. aegypti had nearly regained the geographic distribution it held before eradication was initiated (Fig. 1). Epidemic dengue invariably followed reinfestation of a country by A. aegypti. By the 1980s, the American region was experiencing major epidemics of dengue in countries that had been free of the disease for 35 to 130 years (36–38, 111). New dengue virus strains and serotypes were introduced (DEN-1 in 1977, a new strain of DEN-2 in 1981, DEN-4 in 1981, and a new strain of DEN-3 in 1994). Moreover, many countries of the region evolved from nonendemicity (no endemic disease) or hypoendemicity (one serotype present) to hyperendemicity (multiple serotypes present), and epidemic DHF emerged, much as it had in Southeast Asia 25 years earlier (36–38). From 1981 to 1997, 24 American countries reported laboratory-confirmed DHF (Fig. 2) (42, 43, 111).
FIG. 1.
A. aegypti distribution in the Americas during the 1930s and in 1970 and 1998.
FIG. 2.
DHF in the Americas before 1981 and from 1981 to the present.
While Africa has not yet had a major epidemic of DHF, sporadic cases have occurred, with increased epidemic dengue fever, in the past 15 years. Before the 1980s, little was known of the distribution of dengue viruses in Africa. Since then, however, major epidemics caused by all four serotypes have occurred in both East and West Africa (41, 48). Outbreaks have been more common in East Africa and the Middle East in the 1990s, with major epidemics in Djibouti in 1991 and in Jeddah, Saudi Arabia, in 1994; both were the first outbreaks in those countries in over 50 years (41, 120).
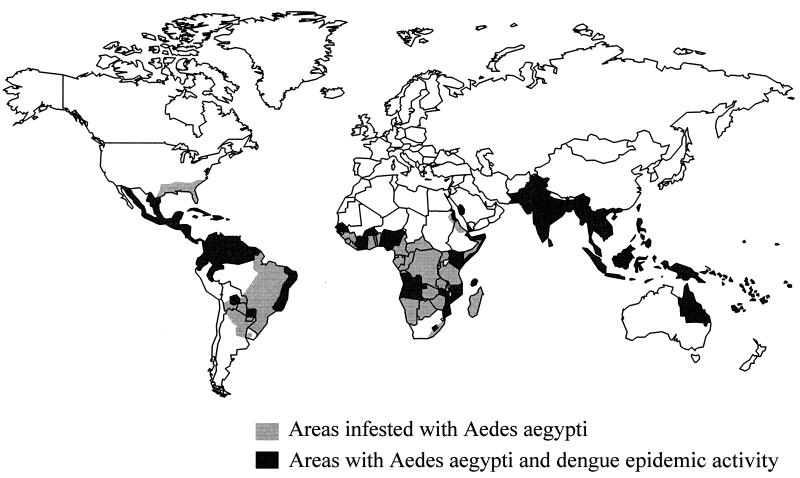
In 1997, dengue viruses and A. aegypti mosquitoes have a worldwide distribution in the tropics (Fig. 3); over 2.5 billion people now live in areas where dengue is endemic (42, 45, 48, 61, 63). Currently, dengue fever causes more illness and death than any other arbovirus disease of humans (124). Each year, an estimated 100 million cases of dengue fever and several hundred thousand cases of DHF occur, depending on epidemic activity (42, 45, 104). DHF is a leading cause of hospitalization and death among children in many Southeast Asian countries (1).
FIG. 3.
World distribution map of dengue and A. aegypti in 1998.
Factors Responsible for the Increased Incidence
The factors responsible for the dramatic resurgence and emergence of epidemic dengue and DHF, respectively, as a global public health problem in the past 17 years are complex and not fully understood. However, the resurgence appears to be closely associated with demographic and societal changes over the past 50 years (36, 41, 42, 48). Two major factors have been the unprecedented global population growth and the associated unplanned and uncontrolled urbanization, especially in tropical developing countries. The substandard housing, crowding, and deterioration in water, sewer, and waste management systems associated with unplanned urbanization have created ideal conditions for increased transmission of mosquito-borne diseases in tropical urban centers.
A third major factor has been the lack of effective mosquito control in areas where dengue is endemic (36, 38, 42, 48). The emphasis during the past 25 years has been on space spraying with insecticides to kill adult mosquitoes; this has not been effective (38, 107, 115) and, in fact, has been detrimental to prevention and control efforts by giving citizens of the community and government officials a “false sense of security” (38). Additionally, the geographic distribution and population densities of A. aegypti have increased, especially in urban areas of the tropics, because of increased numbers of mosquito larval habitats in the domestic environment. The latter include nonbiodegradable plastics and used automobile tires, both of which have increased dramatically in prevalence during this period.
A fourth factor responsible for the global emergence of dengue and DHF is increased air travel, which provides the ideal mechanism for the transport of dengue and other urban pathogens between population centers of the world (36, 40, 42, 48). For instance, in 1994, an estimated 40 million persons departed the United States by air, over 50% of whom traveled for business or holiday to tropical countries where dengue is endemic. Many travelers become infected while visiting tropical areas but become ill only after returning home, resulting in a constant movement of dengue viruses in infected humans to all areas of the world and ensuring repeated introductions of new dengue virus strains and serotypes into areas where the mosquito vectors occur (40, 119).
A fifth factor that has contributed to the resurgence of epidemic dengue has been the decay in public health infrastructures in most countries in the past 30 years. Lack of resources has led to a critical shortage of trained specialists who understand and can develop effective prevention and control programs for vector-borne diseases. Coincident with this has been a change in public health policy that placed emphasis on emergency response to epidemics by using high-technology mosquito control methods rather than on preventing those epidemics by using larval source reduction through environmental hygiene, the only method that has been shown to be effective (38).
In summary, demographic and societal changes, decreasing resources for vector-borne infectious disease prevention and control, and changes in public health policy have all contributed to increased epidemic dengue activity, the development of hyperendemicity, and the emergence of epidemic DHF.
Dengue in the Continental United States
Each year, dengue cases imported to the Continental United States are documented by the Centers for Disease Control and Prevention (CDC) (40, 119). These cases represent introductions of all four virus serotypes from all tropical regions of the world. Most cases of dengue introduced into the United States come from the American and Asian tropics, reflecting the increased number of persons traveling to and from those areas. Overall, from 1977 to 1995, a total of 2,706 suspected cases of imported dengue were reported to CDC (21, 40, 119). Although adequate blood samples were received from only some of these patients, 584 (22%) were confirmed in the laboratory as dengue.
These cases represent only the tip of the iceberg, because most physicians in the United States have a low index of suspicion for dengue, which is often not included in the differential diagnosis of acute febrile illness, even if the patient recently returned from a tropical country. As a result, the majority of imported dengue cases are never reported (21). It is important to increase awareness of dengue and DHF among physicians in temperate areas, however, because the disease can be life-threatening. For example, two cases of dengue shock syndrome (DSS) were recently described in Swedish tourists returning from holiday in Asia (152). In the United States, imported cases appear to be increasingly severe (21). From 1986 to 1993, for example, only 13 of 166 patients (8%) with laboratory-confirmed dengue were hospitalized. In 1994 and 1995, however, 6 of 46 patients (13%) and 11 of 86 patients (13%) with confirmed imported disease required hospitalization, respectively. Moreover, 3 (7%) of the patients in 1994 had severe, hemorrhagic disease (21). Therefore, it is important that physicians in the United States consider dengue in the differential diagnosis of a viral syndrome in all patients with a travel history to any tropical area.
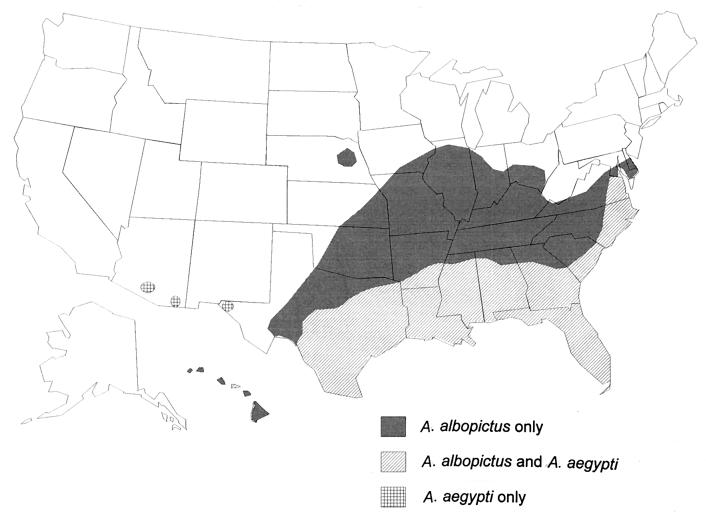
The potential for epidemic dengue transmission in the United States still exists. After an absence of 35 years, autochthonous transmission, secondary to importation of the virus in humans, occurred on four occasions in the past 17 years (1980, 1986, 1995, and 1997) (21, 22). Although all of these outbreaks were small, they underscore the potential for dengue transmission in the United States, where two competent mosquito vectors are found (48) (Fig. 4). A. aegypti, the most important and efficient epidemic vector of dengue viruses, has been in the United States for over 200 years and was responsible for transmitting major epidemics in the southern states in the 19th and early 20th centuries (34). Currently, this species is found only in the Gulf Coast states from Texas to Florida, although small foci have recently been reported in Arizona (Fig. 4). Aedes albopictus, a secondary vector of dengue virus, was introduced into the continental United States from Asia in the early 1980s and has since become widespread in the eastern half of the country. This species currently is found in 866 counties in 26 of the continental states (22, 105); it has also been found in Hawaii for over 90 years, as well as in Guam and Saipan. Both A. aegypti and A. albopictus can transmit dengue viruses to humans, and their presence in the United States increases the risk of autochthonous dengue transmission, secondary to imported cases (37, 40).
FIG. 4.
A. aegypti and A. albopictus distribution in the United States in 1998.
NATURAL HISTORY
The Viruses
There are four dengue virus serotypes, called DEN-1, DEN-2, DEN-3, and DEN-4. They belong to the genus Flavivirus, family Flaviviridae (of which yellow fever virus is the type species), which contains approximately 70 viruses (150). The flaviviruses are relatively small (40–50 mm) and spherical with a lipid envelope. The flavivirus genome is approximately 11,000 bases long and is made up of three structural and seven nonstructural proteins. There are three major complexes within this family—tick-borne encephalitis virus, Japanese encephalitis virus, and dengue virus. All flaviviruses have common group epitopes on the envelope protein that result in extensive cross-reactions in serologic tests. These make unequivocal serologic diagnosis of flaviviruses difficult. This is especially true among the four dengue viruses. Infection with one dengue serotype provides lifelong immunity to that virus, but there is no cross-protective immunity to the other serotypes. Thus, persons living in an area of endemic dengue can be infected with three, and probably four, dengue serotypes during their lifetime (37).
Transmission Cycles
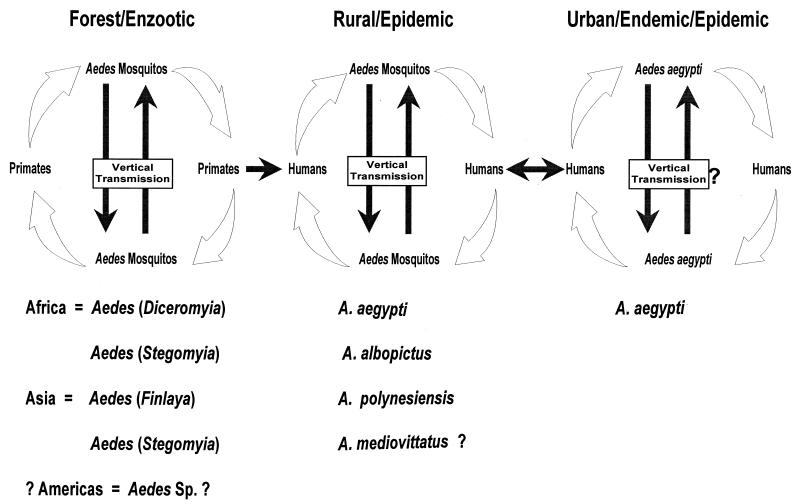
The primitive enzootic transmission cycle of dengue viruses involves canopy-dwelling Aedes mosquitoes and lower primates in the rain forests of Asia and Africa (Fig. 5) (37). Current evidence suggests that these viruses do not regularly move out of the forest to urban areas (116). An epidemic transmission cycle may occur in rural villages or islands, where the human population is small. Introduced viruses quickly infect the majority of susceptible individuals in these areas, and increasing herd immunity causes the virus to disappear from the population. A number of Aedes (Stegomyia) spp. may act as a vector in these situations, depending on the geographic area, including A. aegypti, A. albopictus, A. polynesiensis and other members of the A. scutellaris group (37). The most important transmission cycle from a public health standpoint is the urban endemic/epidemic cycle in large urban centers of the tropics (Fig. 5). The viruses are maintained in an A. aegypti-human-A. aegypti cycle with periodic epidemics. Often, multiple virus serotypes cocirculate in the same city (hyperendemicity).
FIG. 5.
Transmission cycles of dengue viruses.
Humans are infected with dengue viruses by the bite of an infective mosquito (37). A. aegypti, the principal vector, is a small, black-and-white, highly domesticated tropical mosquito that prefers to lay its eggs in artificial containers commonly found in and around homes, for example, flower vases, old automobile tires, buckets that collect rainwater, and trash in general. Containers used for water storage, such as 55-gallon drums, cement cisterns, and even septic tanks, are important in producing large numbers of adult mosquitoes in close proximity to human dwellings. The adult mosquitoes prefer to rest indoors, are unobtrusive, and prefer to feed on humans during daylight hours. There are two peaks of biting activity, early morning for 2 to 3 h after daybreak and in the afternoon for several hours before dark. However, these mosquitoes will feed all day indoors and on overcast days. The female mosquitoes are very nervous feeders, disrupting the feeding process at the slightest movement, only to return to the same or a different person to continue feeding moments later. Because of this behavior, A. aegypti females will often feed on several persons during a single blood meal and, if infective, may transmit dengue virus to multiple persons in a short time, even if they only probe without taking blood (46, 112, 114, 135). It is not uncommon to see several members of the same household become ill with dengue fever within a 24- to 36-h time frame, suggesting that all of them were infected by a single infective mosquito (43). It is this behavior that makes A. aegypti such an efficient epidemic vector. Inhabitants of dwellings in the tropics are rarely aware of the presence of this mosquito, making its control difficult.
After a person is bitten by an infective mosquito, the virus undergoes an incubation period of 3 to 14 days (average, 4 to 7 days), after which the person may experience acute onset of fever accompanied by a variety of nonspecific signs and symptoms (136). During this acute febrile period, which may be as short as 2 days and as long as 10 days, dengue viruses may circulate in the peripheral blood (51). If other A. aegypti mosquitoes bite the ill person during this febrile viremic stage, those mosquitoes may become infected and subsequently transmit the virus to other uninfected persons, after an extrinsic incubation period of 8 to 12 days (37, 46).
CLINICAL DIAGNOSIS
Dengue virus infection in humans causes a spectrum of illness ranging from inapparent or mild febrile illness to severe and fatal hemorrhagic disease (1). Infection with any of the four serotypes causes a similar clinical presentation that may vary in severity, depending on a number of risk factors (see below). The incubation period varies from 3 to 14 days (average, 4 to 7 days) (131, 136). In areas where dengue is endemic, the illness is often clinically nonspecific, especially in children, with symptoms of a viral syndrome that has a variety of local names. Important risk factors influencing the proportion of patients who have severe disease during epidemic transmission include the strain and serotype of the infecting virus and the immune status, age, and genetic background of the human host (1, 4, 37, 57, 62, 123).
Dengue Fever
Classic dengue fever is primarily a disease of older children and adults. It is characterized by the sudden onset of fever and a variety of nonspecific signs and symptoms, including frontal headache, retro-orbital pain, body aches, nausea and vomiting, joint pains, weakness, and rash (1, 71, 131, 136, 149). Patients may be anorexic, have altered taste sensation, and have a mild sore throat. Constipation is occasionally reported; diarrhea and respiratory symptoms are infrequently reported and may be due to concurrent infections.
The initial temperature may rise to 102 to 105°F, and fever may last for 2 to 7 days. The fever may drop after a few days, only to rebound 12 to 24 h later (saddleback). A relative bradycardia may be noted despite the fever. The conjunctivae may be injected, and the pharynx may be inflamed. Lymphadenopathy is common. Rash is variable but occurs in up to 50% of patients as either early or late eruptions. Facial flushing or erythematous mottling may occur coincident with or slightly before onset of fever and disappears 1 to 2 days after onset of symptoms. A second rash, varying in form from scarlatiniform to maculopapular, may appear between days 2 and 6 of illness. The rash usually begins on the trunk and spreads to the face and extremities. In some cases, an intense erythematous pattern with islands of normal skin is observed. The average duration of the second rash is 2 to 3 days. Toward the end of the febrile phase of illness or after the temperature falls to or below normal, petechiae may appear; these may be scattered or confluent. Intense pruritus followed by desquamation on the palms of the hands and soles of the feet may occur.
Hemorrhagic manifestations in dengue fever patients are not uncommon and range from mild to severe. Skin hemorrhages, including petechiae and purpura, are the most common, along with gum bleeding, epistaxis, menorrhagia, and gastrointestinal (GI) hemorrhage. Hematuria occurs infrequently, and jaundice is rare.
Clinical laboratory findings associated with dengue fever include a neutropenia followed by a lymphocytosis, often marked by atypical lymphocytes. Liver enzyme levels in the serum may be elevated; the elevation is usually mild, but in some patients, alanine aminotransferase and aspartate aminotransferase levels reach 500 to 1,000 U/liter. In one epidemic of DEN-4, 54% of confirmed patients with data reported on liver enzymes had elevated levels (32). Thrombocytopenia is also common in dengue fever; in the above epidemic, 34% of patients with confirmed dengue fever who were tested had platelet counts of less than 100,000/mm3 (32).
Dengue fever is generally self-limiting and is rarely fatal. The acute phase of illness lasts for 3 to 7 days, but the convalescent phase may be prolonged for weeks and may be associated with weakness and depression, especially in adults. No permanent sequelae are known to be associated with this infection.
Dengue Hemorrhagic Fever
DHF is primarily a disease of children under the age of 15 years, although it may also occur in adults (1, 32). It is characterized by sudden onset of fever, which usually lasts for 2 to 7 days, and a variety of nonspecific signs and symptoms. During the acute phase of illness, it is difficult to distinguish DHF from dengue fever and other illnesses found in tropical areas. The differential diagnoses during the acute phase of illness should include measles, rubella, influenza, typhoid, leptospirosis, malaria, other viral hemorrhagic fevers, and any other disease that may present in the acute phase as a nonspecific viral syndrome. Children frequently have concurrent infections with other viruses and bacteria causing upper respiratory symptoms. There is no pathognomonic sign or symptom for DHF during the acute stage; on the other hand, as fever remits, characteristic manifestations of plasma leakage appear, making accurate clinical diagnosis possible in many cases (1).
The critical stage in DHF is at the time of defervescence, but signs of circulatory failure or hemorrhagic manifestations may occur from about 24 h before to 24 h after the temperature falls to normal or below (1). Blood tests usually show that the patient has thrombocytopenia (platelet count, ≤100,000/mm3) and hemoconcentration relative to baseline as evidence of a vascular leak syndrome. Common hemorrhagic manifestations include skin hemorrhages such as petechiae, purpuric lesions, and ecchymoses. Epistaxis, bleeding gums, GI hemorrhage, and hematuria occur less frequently. The tourniquet test, which indicates that the patient has increased capillary fragility, may be diagnostically helpful to the physician.
Scattered petechiae are the most common hemorrhagic manifestation observed; they appear most often on the extremities but are also found on the trunk, other parts of the body, and on the face in patients with severe dengue shock syndrome (DSS). Purpuric lesions may appear on various parts of the body but are most common at the site of venipuncture. In some patients, large ecchymotic lesions develop on the trunk and extremities; other patients bleed actively at the site of venipuncture, some profusely. More severely ill patients have GI hemorrhage. Classic hematemesis with coffee-ground vomitus and melena usually occur after prolonged shock, but patients may develop massive, frank upper GI hemorrhage as well, often before the onset of shock. Without early diagnosis and proper management, some patients experience shock from blood loss, which may be mild or severe (35, 138, 139). More commonly, shock is caused by plasma leakage; it may be mild and transient or progress to profound shock with undetectable pulse and blood pressure (1). Children with profound shock are often somnolent, exhibit petechiae on the face, and have perioral cyanosis.
In patients with severe DHF or DSS, fever and nonspecific constitutional signs and symptoms of a few days duration are followed by the sudden deterioration of the patient’s condition (1). During or shortly before or after the fall in temperature, the patient’s skin may become cool, blotchy, and congested; circumoral cyanosis is frequently observed, and the pulse becomes rapid and weak. Although some patients appear lethargic at first, they become restless and then rapidly pass into a critical stage of shock. They frequently experience acute abdominal pain shortly before the onset of shock (1, 138, 139).
In patients with mild DHF, all signs and symptoms abate shortly after the fever subsides. Subsidence of fever, however, may be accompanied by profuse sweating and mild changes in pulse rate and blood pressure, together with coolness of the extremities and skin congestion. These changes reflect mild and transient circulatory disturbances as a result of plasma leakage. Patients usually recover spontaneously or after fluid and electrolyte therapy (1). Patients in shock are in danger of dying unless appropriately managed. The duration of shock is usually short; the patient may die within 8 to 24 h, but recovery is usually rapid following antishock therapy. Convalescence for patients with DHF, with or without shock, is usually short and uneventful. Once the shock is overcome, even patients with undetectable pulse and blood pressure will usually recover within 2 to 3 days (1).
As with dengue fever, leukopenia is common; thrombocytopenia and hemoconcentration are constant findings in DHF and DSS. A platelet count of ≤100,000/mm3 is usually found between the days 3 and 8 of illness. Hemoconcentration, indicating plasma leakage, is almost always present in classic DHF but is more severe in patients with shock. Hepatomegaly is a common but not constant finding (35, 138, 139). In some countries, most patients with confirmed DHF and DSS have enlarged livers. In other countries, however, hepatomegaly varies from one epidemic to another, suggesting that the strain and/or serotype of virus may influence liver involvement (35). Elevated liver enzyme levels are common.
The primary pathophysiologic abnormality seen in DHF and DSS is an acute increase in vascular permeability that leads to leakage of plasma into the extravascular compartment, resulting in hemoconcentration and decreased blood pressure (1, 77). Plasma volume studies have shown a reduction of more than 20% in severe cases. Supporting evidence of plasma leakage includes serous effusion found postmortem, pleural effusion on X-ray, hemoconcentration, and hypoproteinemia. Early diagnosis and aggressive fluid replacement therapy with good nursing care can decrease fatality rates to 1% or less. Normal saline or lactated Ringer’s solution can be used in patients with mild DHF and DSS, but plasma or plasma expanders may be necessary in those with severe cases. Details of effective management of DHF and DSS have been published previously (1). There are no apparent destructive vascular lesions, suggesting that the transient functional vascular changes are due to a short-acting mediator (1). Once the patient is stabilized and begins recovery, the extravasated fluid is rapidly reabsorbed, causing a drop in the hematocrit.
Hemostatic changes in DHF and DSS involve three factors: vascular changes, thrombocytopenia, and coagulation disorders (1). Almost all DHF patients have increased vascular fragility and thrombocytopenia, and many have abnormal coagulograms, suggesting disseminated intravascular coagulation, which is also evidenced by concomitant thrombocytopenia, a prolonged partial thromboplastin time, a decreased fibrinogen level, and increased levels of fibrinogen degradation products. GI hemorrhage is found at autopsy in the majority of patients who die.
PATHOGENESIS
The pathogenesis of DHF and DSS is still controversial. Two theories, which are not mutually exclusive, are frequently cited to explain the pathogenetic changes that occur in DHF and DSS. The most commonly accepted is known as the secondary-infection or immune enhancement hypothesis (57, 61, 62). This hypothesis implies that patients experiencing a second infection with a heterologous dengue virus serotype have a significantly higher risk for developing DHF and DSS (62). Preexisting heterologous dengue antibody recognizes the infecting virus and forms an antigen-antibody complex, which is then bound to and internalized by immunoglobulin Fc receptors on the cell membrane of leukocytes, especially macrophages. Because the antibody is heterologous, however, the virus is not neutralized and is free to replicate once inside the macrophage. Thus, it is hypothesized that prior infection, through a process known as antibody-dependent enhancement (ADE), enhances the infection and replication of dengue virus in cells of the mononuclear cell lineage (15, 62, 66, 67, 106). It is thought that these cells produce and secrete vasoactive mediators in response to dengue infection, which causes increased vascular permeability leading to hypovolemia and shock (see below).
The other hypothesis assumes that dengue viruses, like all animal viruses, vary and change genetically as a result of selection pressures as they replicate in humans and/or mosquitoes and that there are some virus strains that have greater epidemic potential (37, 49, 123). Phenotypic expression of genetic changes in the virus genome may include increased virus replication and viremia, severity of disease (virulence), and epidemic potential.
There is epidemiologic and laboratory evidence to support both of these hypotheses; however, a detailed discussion is beyond the scope of this review. They are not mutually exclusive, and both are most probably valid (37). Excellent reviews have recently been published on both viral pathogenesis and immunopathogenesis (92, 127), which have summarized the evidence concluding that both viral and host immunologic factors are involved in the pathogenesis of severe dengue disease. This evidence is briefly presented below.
Pathology
The pathology of DHF and DSS has been well studied (6, 7, 9), but that of dengue infections has not. Gross and microscopic pathologic studies of tissues taken at autopsy in Thailand have shown diffuse petechial hemorrhages of most organs, as well as serous effusions in the pericardial, pleural, and peritoneal cavities. Microscopically, perivascular edema and loss of integrity of endothelial junctions are found. Dengue antigen can be demonstrated in endothelial cells, but there is no apparent damage to the blood vessels or endothelial cells.
In the liver, midzonal necrosis is common and is often indistinguishable from the pathologic changes caused by the closely related yellow fever virus; Councilman bodies are common. In the brain, edema and hemorrhage have been observed but pathologic changes associated with encephalitis have not. However, recent isolations of dengue virus from the brain and cerebrospinal fluid and intrathecal antibody production in the latter suggest that on occasion, the dengue virus crosses the blood-brain barrier. There is increased proliferation of reticuloendothelial cells in the bone marrow, spleen, lymph nodes, and lungs.
Virologic Factors
Unfortunately, there are no good animal models for DHF and DSS, making studies on pathogenesis difficult to interpret. Primates are natural hosts for dengue virus, but those that have been studied generally show no signs of disease; these animals become infected and develop viremia, although at a lower titer than humans (126). However, the results obtained with these animals are conflicting. One of the few studies cited as evidence that ADE occurs in vivo showed that rhesus monkeys that experienced a secondary DEN-2 infection or had been infused with dengue immune serum had higher viremias than did monkeys with primary infections (60, 64, 65). All monkeys were infected parenterally by needle inoculation. These results could not be repeated in macaque monkeys infected naturally by a mosquito bite or in chimpanzees infected parenterally; primary and secondary infections of all serotypes and combinations routinely showed that monkeys with primary infection had viremia of the same or higher titer and longer duration (126, 134). Clinical and laboratory studies on humans have shown the same results (35, 47, 49, 51, 87).
In humans, viremias range in titer from barely detectable (103), measured as 50% mosquito infection doses (MID50) (125) to over 108.5 MID50 (51). Viremia usually peaks at the time of or shortly after the onset of illness and may remain detectable for various periods ranging from 2 to 12 days, depending on the strain of virus and the immune status of the individual (35, 43, 47, 49, 51, 87, 147). It has been suggested that the severity of the disease associated with dengue infection is determined by the number of cells infected with the virus and that the number of cells infected is related to ADE infection of peripheral blood leukocytes in secondary infections (77). It follows that viremias should be higher in secondary infections, but this is not borne out by experimental infection of lower primates or by clinical studies on humans (35, 49, 51, 87, 126, 134). In fact, the opposite has usually been observed; that is, viremias are usually higher in primary infections.
In secondary infections, the virus may be complexed with antibody, making it undetectable by most current virus isolation techniques. However, studies in humans during an outbreak of DEN-2 on an island in the Pacific (Tonga) showed great variation in both the magnitude and duration of viremia in primary infections (49). Some patients were identified on the day of onset of mild illness and monitored for as long as 8 days. Blood samples were taken daily for viremia studies, and uninfected mosquitoes were allowed to feed on some patients. The majority of patients, confirmed as DEN-2 infection by seroconversion, had undetectable viremia both by virus isolation and by isodiagnosis (feeding mosquitoes on patients) (49). When virus was detectable, viremia was at a low titer (≤106 MID50) and of short duration (1 to 3 days). The same DEN-2 virus had caused explosive epidemics associated with severe disease in neighboring islands in the previous 3 years, but in Tonga it circulated for nearly a year without being detected in a human population that was fully susceptible to DEN-2 virus (silent transmission) (49). Two species of vector mosquitoes (A. aegypti and Aedes tabu) were present in large numbers. The data suggested that the virus had changed from an epidemic strain to one that circulated in nature silently, causing mild or inapparent disease. Similar observations have been made with DEN-3 and DEN-1 viruses (41).
Molecular studies have demonstrated that dengue viruses vary genetically in nature; unfortunately, phenotypic changes that have been observed in the field have not yet been associated with genetic changes in the virus (26, 99, 100, 116, 117, 143). Collectively, however, the data suggest that viral factors play a significant role in the pathogenesis of severe dengue disease.
Host Immune Factors
There is a large body of evidence, mostly obtained in vitro, suggesting that heterotypic, nonneutralizing antibody binds with dengue virus, facilitating the entry of the virus into cells of the monocytic line and hence facilitating infection (15, 61, 62, 67, 68, 83). These data, along with epidemiologic observations that the majority of patients with reported DHF cases are experiencing a secondary infection, form the basis for the hypothesis that preexisting heterotypic dengue antibody is a risk factor for DHF (18, 57, 61, 62, 83, 133). The lack of a good animal model for human disease and limitations of human clinical studies have made it difficult to confirm this hypothesis. In recent years, however, detailed, well-designed studies that support the concept of immunopathogenesis of dengue infection in humans have been conducted. The results of these studies have been comprehensively reviewed in a recent article (92).
Briefly, the data show that dengue virus-specific memory CD4+ CD8− and CD4− CD8+ lymphocytes are detectable in humans after natural dengue infections. Infection with a single dengue serotype induces both serotype-specific and serotype-cross-reactive CD4+ memory T cells, while CD8+ T lymphocytes have virus-specific cytotoxic activity.
The pathogenetic mechanism responsible for the increased vascular permeability observed in DHF and DSS is not known, but it has been suggested that cytokines and chemical mediators such as tumor necrosis factor (TNF), interleukin-1 (IL-1), IL-2, IL-6, platelet-activating factor (PAF), complement activation products C3a and C5a, and histamine may play a role.
CD4+ T lymphocytes produce a number of cytokines, including gamma interferon (IFN-γ), IL-2, IL-4, IL-5, IL-6, IL-10, and lymphotoxin. Moreover, monocytes/macrophages which are infected by dengue viruses produce TNF, IL-1, IL-1B, IL-6, and PAF. Finally, cytokine and chemical mediator production is induced by other cytokines. Thus, once cytokines are produced, a complex network of induction may further increase the levels of cytokines and chemical mediators, resulting in even higher levels with synergistic effects on vascular permeability (92).
Kurane and Ennis have proposed a model of immunopathogenesis based on these observations (92). Briefly, it is hypothesized that dengue virus infections of monocytes/macrophages is enhanced by ADE. This enhancement is facilitated by the fact that the dengue virus-specific CD4+ T lymphocytes produce IFN-γ, which in turn up-regulates the expression of FC-γ receptors. The increased number of dengue virus-infected monocytes/macrophages results in increased T-cell activation, which results in the release of increased levels of cytokines and chemical mediators. Kurane and Ennis (92) hypothesized that the rapid increase in the levels and the synergistic effects of mediators such as TNF, IL-2, IL-6, IFN-γ, PAF, C3a, C5a, and histamine induce increased vascular permeability, plasma leakage, shock, and malfunction of the coagulation system, which may lead to hemorrhage.
In summary, available evidence suggests that both viral and host immune factors are involved in the pathogenesis of severe dengue disease. Unfortunately, the role of each is not fully understood and the lack of an animal model makes this a difficult area to study. It would appear that different clinical pathologic manifestations of the disease may be caused by different pathogenetic mechanisms (37). For example, it has been suggested that hepatic injury may relate more to viral factors whereas vascular permeability may be mediated predominantly by the immune response (92, 127). Clearly, the strain of virus is important since ADE apparently occurs only with selected virus strains when tested in vitro. Also, the rate of virus replication and infectivity in various tissues varies with the strain of virus. Collectively, the data suggest that only certain strains of dengue virus are associated with major epidemics and severe disease, and it is most likely that these are the viruses that infect cells of the monocytic line via ADE (12, 37, 49, 116, 117).
LABORATORY DIAGNOSIS
A definitive diagnosis of dengue infection can be made only in the laboratory and depends on isolating the virus, detecting viral antigen or RNA in serum or tissues, or detecting specific antibodies in the patient’s serum (47, 55, 148). There have been two recent reviews of this topic (55, 148).
An acute-phase blood sample should always be taken as soon as possible after the onset of suspected dengue illness, and a convalescent-phase sample should ideally be taken 2 to 3 weeks later. Because it is frequently difficult to obtain convalescent-phase samples, however, a second blood sample should always be taken from hospitalized patients on the day of discharge from hospital.
Serologic Diagnosis
Five basic serologic tests have been routinely used for diagnosis of dengue infection; hemagglutination-inhibition (HI), complement fixation (CF), neutralization test (NT), immunoglobulin M (IgM) capture enzyme-linked immunosorbent assay (MAC-ELISA), and indirect immunoglobulin G ELISA (47, 55, 148). Regardless of the test used, unequivocal serologic diagnosis depends upon a significant (fourfold or greater) rise in the titer of specific antibodies between acute- and convalescent-phase serum samples. The antigen battery for most of these serologic tests should include all four dengue virus serotypes, another flavivirus (such as yellow fever virus, Japanese encephalitis virus, or St. Louis encephalitis virus), a nonflavivirus (such as Chikungunya virus or eastern equine encephalitis virus), and ideally, an uninfected tissue control antigen (47).
Of the above tests, HI has been the most frequently used; it is sensitive, is easy to perform, requires only minimal equipment, and is very reliable if properly done (28). Because HI antibodies persist for long periods (up to 48 years and probably longer) (58), the test is ideal for seroepidemiologic studies. HI antibody usually begins to appear at detectable levels (titer of 10) by day 5 or 6 of illness, and antibody titers in convalescent-phase serum specimens are generally at or below 640 in primary infections, although there are exceptions (4, 47). By contrast, there is an immediate anamnestic response in secondary and tertiary dengue infections, and reciprocal antibody titers increase rapidly during the first few days of illness, often reaching 5,120 to 10,240 or more. Thus, a titer of ≥1,280 in an acute-phase or early convalescent-phase serum sample is considered presumptive evidence of a current dengue infection. Such high levels of HI antibody persist for 2 to 3 months in some patients, but antibody titers generally begin to wane by 30 to 40 days and fall below 1,280 in most patients (47). The major disadvantage of the HI test is its lack of specificity, which generally makes it unreliable for identifying the infecting virus serotype. However, some patients with primary infections show a relatively monotypic HI response that generally correlates with the virus isolated (47).
The CF test is not widely used for routine dengue diagnostic serologic testing. It is more difficult to perform, requires highly trained personnel, and therefore is not used in most dengue laboratories. It is based on the principle that complement is consumed during antigen-antibody reactions (20). CF antibodies generally appear later than HI antibodies, are more specific in primary infections, and usually persist for short periods, although low levels of antibodies persist in some persons (47). It is a valuable test to have in a diagnostic laboratory because of the late appearance of CF antibodies; some patients thus show a diagnostic rise in antibody titers by CF but have only stable antibody titers by HI or ELISA (47). The greater specificity of the CF test in primary infections is demonstrated by the monotypic CF responses when HI responses are broadly heterotypic; it is not specific in secondary infections. The CF test is useful for patients with current infections but is of limited value for seroepidemiologic studies, where detection of persistent antibodies is important.
The NT is the most specific and sensitive serologic test for dengue viruses (33, 129). The most common protocol used in dengue laboratories is the serum dilution plaque reduction NT. In general, neutralizing-antibody titers rise at about the same time or slightly more slowly than HI and ELISA antibody titers but more quickly than CF antibody titers and persist for at least 48 years (58). Because the NT is more sensitive, neutralizing antibodies are present in the absence of detectable HI antibodies in some persons with past dengue infection.
Because relatively monotypic neutralizing-antibody responses are observed in properly timed convalescent-phase serum, the NT can be used to identify the infecting virus in primary dengue infections (4, 47, 129, 148). As noted above, the HI and CF tests may also give monotypic responses to dengue infection that generally agree with NT results. In cases when the responses are monotypic, the interpretation of all these tests is generally reliable. In secondary and tertiary infections, determining the infecting virus serotype by NT or any other serologic test is not reliable (90). Because of the long persistence of neutralizing antibodies, the test may also be used for seroepidemiologic studies. The major disadvantages are the expense, time required to perform the test, and technical difficulty. It is therefore not used routinely by most laboratories.
MAC-ELISA has become the most widely used serologic test for dengue diagnosis in the past few years. It is a simple, rapid test that requires very little sophisticated equipment (17, 47, 78, 89, 97). Anti-dengue IgM antibody develops a little faster than IgG antibody. By day 5 of illness, most patients (80%) in Puerto Rico whose cases were subsequently confirmed by HI on paired serum samples or by virus isolation had detectable IgM antibody in the acute-phase serum in this assay (47). Nearly all patients (93%) developed detectable IgM antibody 6 to 10 days after onset, and 99% of patients tested between 10 and 20 days had detectable IgM antibody. The rapidity with which IgM develops varies considerably among patients. Although the dates of onset are not always recorded accurately, some patients have detectable IgM on days 2 to 4 after the onset of illness whereas others may not develop IgM for 7 to 8 days after onset (47). This variation is also reflected in the amount of IgM produced and the length of time detectable IgM persists after infection. IgM antibody is produced by patients with both primary and secondary dengue infections and probably by persons with tertiary infections, although the response in some secondary and probably most tertiary infections is low level and transient (89). IgM antibody titers in primary infections are significantly higher than in secondary infections, although it is not uncommon to obtain IgM titers of 320 in the latter cases (47). In some primary infections, detectable IgM persists for more than 90 days, but in most patients, it has waned to an undetectable level by 60 days. A small percentage of patients with secondary infections have no detectable IgM antibody (89).
MAC-ELISA with a single acute-phase serum sample is slightly less sensitive than the HI test with paired serum samples for diagnosing dengue infection (47). However, it has the advantage of frequently requiring only a single, properly timed blood sample. In one series of 288 patients during the 1986 epidemic in Puerto Rico, paired blood samples were tested by HI and the single acute-phase sample from the same pairs were tested by MAC-ELISA. The HI test on the pairs indicated that 228 (79%) were considered positive, while MAC-ELISA on the single samples indicated that 203 (70%) were positive. Five samples (1.7%) showed a false-positive response and 30 samples (10%) showed a false-negative response by MAC-ELISA (47). When one considers the difficulty in obtaining second blood samples and the long delay in obtaining conclusive results from the HI test, this low error rate would be acceptable in most surveillance systems. It must be emphasized, however, that because of the persistence of IgM antibody for 1 to 3 months, MAC-ELISA-positive results obtained with single serum samples are only provisional and do not necessarily mean that the dengue infection was current (47, 148). These results do mean that it is reasonably certain that the person had a dengue infection sometime in the previous 2 to 3 months. Similarly, a negative result with an acute-phase sample may be a false-negative result because the sample was taken before detectable IgM appeared. Unfortunately, many dengue diagnostic laboratories have adopted MAC-ELISA as a confirmatory test and do not conduct follow-up tests to confirm the presumptive IgM results. As noted above, this may be acceptable for surveillance reports, but it is unacceptable in a clinical setting. If this test is used to make patient management decisions, it could result in a higher case fatality rate among patients with false-negative results.
The specificity of MAC-ELISA is similar to that of HI. In both primary and secondary dengue infections, some monotypic responses may be observed, but in general, the response is broadly reactive among both dengue virus and other flavivirus antigens. With serum samples from patients with other flavivirus infections such as Japanese encephalitis, St. Louis encephalitis, and yellow fever, however, the response is generally more specific; while there may be some cross-reaction with dengue antigens, most specimens show relatively monotypic IgM responses to the infecting flavivirus (47). In dengue infections, monotypic IgM responses frequently do not correlate with the virus serotype isolated from a patient. Therefore, MAC-ELISA cannot be reliably used to identify the infecting virus serotype.
MAC-ELISA has become an invaluable tool for surveillance of dengue, DHF, and DSS. In areas where dengue is not endemic, it can be used in clinical surveillance for viral illness or for random, population-based serosurveys, with the certainty that any positive results detected indicate recent infections (within the last 2 to 3 months). A properly timed serosurvey by MAC-ELISA during an epidemic can determine very quickly how widespread transmission has become. In areas where dengue is endemic, MAC-ELISA can be used as an inexpensive way to screen large numbers of serum specimens with relatively little effort. It is especially useful for hospitalized patients, who are generally admitted late in the illness after detectable IgM is present in the blood (47), but it must be emphasized again that this test should not be used to make patient management decisions.
An indirect IgG-ELISA has been developed that is comparable to the HI test and can also be used to differentiate primary and secondary dengue infections (27). The test is simple and easy to perform and is thus useful for high-volume testing. The IgG-ELISA is very nonspecific and exhibits the same broad cross-reactivity among flaviviruses as the HI test does; therefore, it cannot be used to identify the infecting dengue virus serotype. However, it has a slightly higher sensitivity than the HI test. As more data are accumulated on the IgG-ELISA, it is expected to replace the HI test as the most commonly used IgG test in dengue laboratories.
A number of commercial test kits for anti-dengue IgM and IgG antibodies have become available in the past few years. Unfortunately, the accuracy of most of these tests is unknown because proper validation studies have not been done. Some evaluations have been published (91, 96, 146, 153), but the sample sizes have been too small to accurately measure sensitivity and specificity. Moreover, the samples generally used have represented only strong positives and negatives, with few samples representing optical densities or positive-negative values in the equivocal range. One exception to this were kits that were independently evaluated at CDC; both IgM and IgG test kits had a high rate of false-positive results compared to standard tests, especially with samples with optical densities in the equivocal range (91). Other studies, however, have given results comparable to those of standard tests (96, 146, 153). It is anticipated that these test kits can be reformulated to make them more accurate, making global laboratory-based surveillance for dengue and DHF an attainable goal in the near future.
Virus Isolation
Four isolation systems have routinely been used for dengue viruses; intracerebral inoculation of 1- to 3-day-old baby mice, the use of mammalian cell cultures (primarily LLC-MK2 cells), intrathoracic inoculation of adult mosquitoes, and the use of mosquito cell cultures (47, 55, 148).
Baby mice.
Although all four dengue serotypes were initially isolated from human serum by using baby mice (70, 74, 131), this method is very time-consuming, slow, and expensive. Moreover, because of the low sensitivity of the method, many wild-type viruses cannot be isolated with baby mice. Those that are isolated frequently require numerous passages to adapt the viruses to growth in mice. This method is no longer recommended for isolation of dengue viruses, but some laboratories continue to use it (47). One advantage of using baby mice, however, is that other arboviruses that cause dengue-like illness may be isolated with this system.
Mammalian cell culture.
Mammalian cell cultures have many of the same disadvantages as baby mice for isolation of dengue viruses—they are expensive, slow, and insensitive (47, 55, 148, 155). As with isolation systems that use baby mice, viruses that are isolated frequently require many passages before a consistent cytopathic effect can be observed in the infected cultures. Although the use of this method continues in some laboratories, it is not recommended (47, 148).
Mosquito inoculation.
Mosquito inoculation is the most sensitive method for dengue virus isolation (47, 125). Isolation rates of up to 100% of serologically confirmed dengue infections are not uncommon, and this is the only method sensitive enough for routine successful virologic confirmation of fatal DHF and DSS cases (47, 50, 139, 147). Moreover, there are many endemic dengue virus strains that can be recovered only by this method (47, 49, 54).
Four mosquito species have been used for virus isolation, A. aegypti, A. albopictus, Toxorhynchities amboinensis, and T. splendens. Male and female mosquitoes are equally susceptible; dengue viruses generally replicate to high titers (106 to 107 MID50) in as little as 4 to 5 days, depending on the temperature of incubation. Dengue viruses replicate in most mosquito tissues, including the brain. A recent variation on this method involves intracerebral inoculation of larval and adult Toxorhynchities mosquitoes (95, 142). However, these modifications neither increase sensitivity nor provide other advantages over intrathoracic inoculation (125).
Virus detection in the mosquito, regardless of the species, is generally performed by the direct fluorescent-antibody DFA test on mosquito tissues, usually brain or salivary glands (47, 50, 86). The direct conjugate is prepared from pooled human serum and has broadly reactive anti-dengue (or anti-flavivirus) activity. Alternatively, a polyclonal mouse ascitic fluid or a flavivirus group-reactive monoclonal antibody can be used in an indirect fluorescent-antibody (IFA) test with an anti-mouse immunoglobulin G–fluorescein isothiocyanate conjugate that is commercially available.
The mosquito inoculation technique has the disadvantages of being labor-intensive and requiring an insectary to produce large numbers of mosquitoes for inoculation. Also, unless strict safety precautions are maintained, the chance of laboratory infections increases, although this risk can be eliminated by using male Aedes mosquitoes or nonbiting Toxorhynchites species for inoculation (47, 125).
Mosquito cell culture.
Mosquito cell cultures are the most recent addition to dengue virus isolation methodology (47, 52, 76, 88, 141). Three cell lines of comparable sensitivity are most frequently used (88). The first cell line developed, and still the most widely used, is the C6/36 clone of A. albopictus cells (76). The use of these cell lines has provided a rapid, sensitive, and economical method for dengue virus isolation. Moreover, many serum specimens can be processed easily, making the method ideal for routine virologic surveillance (52). However, this system is less sensitive than mosquito inoculation (47). For example, on average, 10 to 15% more viruses were isolated from patients in Puerto Rico by the mosquito inoculation technique than by mosquito cell cultures (22, 43, 47). However, the sensitivity of the mosquito cell lines may vary with the strain of virus. In samples from an epidemic in Mozambique, more than twice as many DEN-3 viruses were isolated by mosquito inoculation than by the use of mosquito cells (54).
Dengue antigen can be detected in infected-cell cultures by DFA or IFA tests with the conjugates used for mosquito tissues (52). Some workers, however, prefer to use cytopathic effect to detect infection, especially with AP-61 cells. However, this method alone will miss many dengue viruses that do not replicate rapidly in mosquito cells (47).
The methods selected for virus isolation depend upon the laboratory facilities available. Because the mosquito inoculation technique is the most sensitive, it is the method of choice for fatal cases or patients with severe hemorrhagic disease. Use of the mosquito cell lines is the method of choice for routine virologic surveillance. Even though cell cultures are less sensitive than mosquito inoculation, this disadvantage is more than offset by the ease with which large numbers of samples can be processed in a relatively short time.
Virus Identification
The method of choice for dengue virus identification is IFA with serotype-specific monoclonal antibodies produced in tissue culture or mouse ascitic fluids and an anti-mouse immunoglobulin G-fluorescein isothiocyanate conjugate (47, 52, 55, 72). This test can be easily performed with infected cell cultures, mosquito brain or tissue squashes, mouse brain squashes, or even on formalin-fixed tissues embedded in paraffin and sectioned for histopathologic testing (56). It is simple and reliable and is the most rapid method. Moreover, it allows the detection of multiple viruses in patients with concurrent infections with more than one serotype (53, 94).
The success of isolating dengue virus from human serum depends on several factors (47). First, the manner in which the specimen has been handled and stored is important. Virus activity can be inhibited by heat, pH, and several chemicals; therefore, improper handling is often an important cause of unsuccessful virus isolation. Second, the level of viremia may vary greatly depending on the time after onset, the antibody titers, and/or the strain of the infecting virus. Viremia usually peaks at or shortly before the onset of illness and may be detectable for an average of 4 to 5 days (43, 47, 51, 147). The success of virus isolation decreases rapidly with the appearance of IgM antibody (47, 148). With some virus strains, however, viremia may remain below the level of detectability throughout the illness (47, 49). Finally, the virus isolation system used influences the success of isolation, as discussed above.
New Diagnostic Technology
In recent years, several new methods of diagnosis have been developed and have proven very useful in dengue diagnosis. This topic has recently been reviewed extensively (29). The various methods are discussed briefly below.
PCR.
Reverse transcriptase PCR (RT-PCR) has been developed for a number of RNA viruses in recent years and has the potential to revolutionize laboratory diagnosis; for dengue, RT-PCR provides a rapid serotype-specific diagnosis. The method is rapid, sensitive, simple, and reproducible if properly controlled and can be used to detect viral RNA in human clinical samples, autopsy tissues, or mosquitoes (29, 55, 98, 148). Although RT-PCR has similar sensitivity to virus isolation systems that use C6/36 cell cultures, poor handling, poor storage, and the presence of antibody usually do not influence the outcome of PCR as they do virus isolation. A number of methods involving primers from different locations in the genome and different approaches to detect the RT-PCR products have been developed over the past several years (29, 55, 148).
It must be emphasized, however, that RT-PCR should not be used as a substitute for virus isolation. The availability of virus isolates is important for characterizing virus strain differences, since this information is critical for viral surveillance and pathogenesis studies. Unfortunately, many laboratories are now conducting RT-PCR tests without proper quality control, i.e., virus isolation or serologic testing. Since RT-PCR is highly sensitive to amplicon contamination, without proper controls false-positive results may occur. Improvements in this technology, however, should make it even more useful in the future (29, 148).
Hybridization probes.
The hybridization probe method detects viral nucleic acids with cloned hybridization probes (29, 148). Probes with variable specificity ranging from dengue complex to serotype specific can be constructed depending on the genome sequences used. The method is rapid and relatively simple and can be used on human clinical samples as well as fixed autopsy tissues. Unfortunately, hybridization probes have not been widely used or evaluated in the diagnostic laboratory. Preliminary data suggest that this method is less sensitive than RT-PCR, but like PCR, the outcome of the test is not influenced by the presence of neutralizing antibodies or other inhibitory substances. Even so, the difficulties of working with RNA and the technical expertise required to obtain reproducible results make this method more suitable as a research tool than as a routine diagnostic test (29, 30, 148).
Immunohistochemistry.
A major problem in dengue laboratory diagnosis has been confirmation of fatal cases. In most instances, only a single serum sample is obtained and serologic testing is therefore of limited value. Also, most patients die at the time of or slightly after defervescence, when virus isolation is difficult. With new methods of immunohistochemistry, it is now possible to detect dengue viral antigen in a variety of tissues (56, 156). Although immunofluorescence tests were used in the past, newer methods involving enzyme conjugates such as peroxidase and phosphatase in conjunction with either polyclonal or monoclonal antibodies are greatly improved (156). Because tissues can be fresh or fixed, autopsies should be performed in all cases of suspected DHF with a fatal outcome (47, 50).
PREVENTION AND CONTROL
Prevention and control of dengue and DHF has become more urgent with the expanding geographic distribution and increased disease incidence in the past 20 years (36, 39, 41, 42, 45, 48, 61, 63, 104). Unfortunately, tools available to prevent dengue infection are very limited. There is no vaccine currently available (see below), and options for mosquito control are limited. Clearly, the emphasis must be on disease prevention if the trend of emergent disease is to be reversed.
Effective disease prevention programs must have several integrated components, including active laboratory-based surveillance, emergency response, education of the medical community to ensure effective case management, community-based integrated mosquito control, and effective use of vaccines when they become available (37, 44).
Vaccine Development
The first candidate dengue vaccines were developed shortly after the viruses were first isolated by Japanese and American scientists (81, 132). Despite considerable work over the years, an effective safe vaccine was never developed (3, 59, 69, 130, 151). The World Health Organization designated the development of a tetravalent dengue vaccine a priority for the most cost-effective approach to dengue prevention (13, 14). Effective vaccination to prevent DHF will most probably require a tetravalent vaccine, because epidemiologic studies have shown that preexisting heterotypic dengue antibody is a risk factor for DHF (18, 57, 61, 62, 133). With the support of the World Health Organization, considerable progress in developing a vaccine for dengue and DHF has been made in recent years (8, 10, 11, 145, 154). Promising candidate attenuated vaccine viruses have been developed and have been evaluated in phase I and II trials in Thailand as monovalent, bivalent, trivalent, and tetravalent formulations (8). A commercialization contract has been signed, and the tetravalent vaccine formulation is currently undergoing repeat phase I trials in the United States. Current progress on the live attenuated dengue vaccine has been recently reviewed (8).
Promising progress in the development of alternative vaccine strategies using new molecular technology has also been made in recent years. Recent approaches include the use of inactivated whole-virion vaccines (23), synthetic peptides (5, 121, 122), subunit vaccines (31, 101, 140), vector expression, recombinant live vector systems (23, 102), infectious cDNA clone-derived vaccines (16, 25, 79, 80, 82, 93, 113), and naked DNA (24, 84). The last two approaches appear to be the most promising. An infectious clone of the DEN-2, PDK-53 vaccine candidate virus from Thailand (11) has been constructed, and work is in progress to construct chimeric viruses by inserting the capsid, premembrane, and envelope genes of DEN-1, DEN-3 and DEN-4, into the DEN-2 PDK-53 backbone (82). Through genetic manipulation, these recombinants may be made to grow better and to be more immunogenic and safer than the original live attenuated virus vaccine candidates. In addition, chimeras are being constructed by inserting the structural proteins of dengue viruses into the infections clones of the 17D yellow fever and the SA14-14-2 Japanese encephalitis vaccine viruses (103a). The development of naked DNA vaccines is in its infancy but shows great promise (24). This area has been recently reviewed (23, 144).
Despite the promising progress, it is unlikely that an effective, safe, and economical dengue vaccine will be available in the near future. A major problem has been and continues to be lack of financial support for dengue vaccine research. Thus, other approaches to disease prevention must be developed by using the program components outlined above.
Disease Prevention Programs
Active surveillance.
Active disease surveillance is an important component of a dengue prevention program. In addition to monitoring secular trends, the goal of surveillance should be to provide an early-warning or predictive capability for epidemic transmission, the rationale being that if epidemics can be predicted, they can be prevented by initiating emergency mosquito control. For epidemic prediction, health authorities must be able to accurately monitor dengue virus transmission in a community and be able to tell at any point in time where transmission is occurring, which virus serotypes are circulating, and what kind of illness is associated with dengue infection (44, 118). To accomplish this, the system must be active and laboratory based.
This type of proactive surveillance system must have at least three components that place the emphasis on the inter- or preepidemic period. These components include a sentinel clinic and physician network, a fever alert system that uses community health workers, and a sentinel hospital system (Table 1). The sentinel clinic and physician network and fever alert system are designed to monitor nonspecific viral syndromes in the community. This is especially important for dengue viruses because they are frequently maintained in tropical urban centers in a silent or unrecognized transmission cycle, often presenting as nonspecific viral syndromes. The sentinel clinic and physician network and fever alert system are also very useful for monitoring other common infectious diseases such as influenza, measles, malaria, typhoid, and leptospirosis.
TABLE 1.
Components of laboratory-based, proactive surveillance for dengue and DHFa
| Type of surveillance | Samplesb | Approach |
|---|---|---|
| Sentinel clinic and physician network | Blood from representative cases of viral syndrome, taken 3–15 days after onset of illness | Representative samples taken year round and processed weekly for virus isolation and for IgM antibodies |
| Fever alert system | Blood samples from representative cases of febrile illness | Increased febrile illness in community investigated immediately; samples tested as above |
| Sentinel hospital systemc | Blood and tissue samples taken during hospitalization and/or at death | All hemorrhagic disease and all viral syndromes with fatal outcome investigated immediately and tested as above |
Emphasis should be placed on the interepidemic period, using a nonspecific case definition. After an epidemic begins and after the virus serotype(s) is known, the case definition should be made more specific and surveillance should be focused on severe disease.
All samples are processed weekly for virus isolation and/or for dengue virus-specific IgM antibodies.
Sentinel sites should be geographically representative.
In contrast to the sentinel clinic and physician component, which requires sentinel sites to monitor routine viral syndromes, the fever alert system relies on community health and sanitation workers to be alert to any increase in febrile activity in their community and to report this to the central epidemiology unit of the health department. Investigation by the health department should be immediate but flexible; it may involve telephone follow-up or active investigation by an epidemiologist who visits the area to take samples.
The sentinel hospital component should be designed to monitor severe disease. Hospitals used as sentinel sites should include all of those that admit patients for severe infectious diseases in the community. This network should also include infectious-disease physicians, who usually consult on such cases. The system can target any type of severe disease, but for dengue, it should include all patients with any hemorrhagic manifestation; an admission diagnosis of viral encephalitis, aseptic meningitis, or meningococcal shock; and/or a fatal outcome following a viral prodrome (50).
All three proactive surveillance components require a good public health laboratory to provide diagnostic support in virology, bacteriology, and parasitology. The supporting laboratory does not have to be able to test for all agents but should know where to refer specimens for testing, e.g., to the World Health Organization Collaborating Centers for Reference and Research.
This proactive surveillance system is designed to monitor disease activity during the interepidemic period, prior to epidemic transmission. Individually, the three components are not sensitive enough to provide effective early warning, but when used collectively, they can often accurately predict epidemic activity (44). Table 1 outlines the proactive surveillance system for dengue and DHF, listing the types of specimens and laboratory tests required. It must be emphasized that once epidemic transmission has begun, the surveillance system should be refocused on severe disease rather than viral syndromes. The surveillance system should be designed and adapted to the local conditions where it will be initiated. However, this system should be closely tied to the mosquito control programs that will be responsible for reacting to surveillance data to initiate emergency disease prevention in all areas.
Mosquito control.
Prevention and control of dengue and DHF currently depends on controlling the mosquito vector, A. aegypti, in and around the home, where most transmission occurs. Space sprays with insecticides to kill adult mosquitoes are not usually effective (38, 107, 115) unless they are used indoors. The most effective way to control the mosquitoes that transmit dengue is larval source reduction, i.e., elimination or cleaning of water-holding containers that serve as the larval habitats for A. aegypti in the domestic environment (38, 115, 137).
There are two approaches to effective A. aegypti control involving larval source reduction. In the past, the most effective programs have had a vertical, paramilitary organizational structure with a large staff and budget (137). These successful programs were also facilitated by the availability of residual insecticides, such as DDT, that contributed greatly to ridding the mosquito from the domestic environment. Unfortunately, in all of these programs, without exception, there has been no sustainability, because once the mosquito and the disease were controlled, limited health resources were moved to other competing programs and the A. aegypti population rebounded to levels where epidemic transmission occurred. The most recent example of this lack of sustainability is Cuba, where A. aegypti had been effectively controlled and dengue transmission had been prevented since 1981. The vertically structured Cuban program has recently failed, most probably because of lack of support; the result was a major dengue epidemic in 1997 (2, 85).
In recent years, emphasis has been placed on community-based approaches to larval source reduction to provide program sustainability (38). The rationale is that sustainable A. aegypti control can be accomplished only by the people who live in the houses where the problems occur and by the people who help create the mosquito larval habitats by their lifestyles (38). Community participation in and ownership of prevention programs require extensive health education and community outreach. Unfortunately, this approach is a very slow process. Therefore, it has been proposed that a combination top-down and bottom-up approach be used, the former to achieve immediate success and the latter to provide program sustainability (38). The effectiveness of this approach remains unknown. Mosquito control for dengue prevention has recently been reviewed (115).
Prevention of Dengue in Travelers
There is no completely effective method of preventing dengue infection in travelers visiting tropical areas. The risk of infection can be significantly decreased, however, by understanding the basic behavior and feeding habits of the mosquito vector and by taking a few simple precautions to decrease exposure to infective mosquito bites. Female A. aegypti mosquitoes prefer to feed indoors, with peak biting activity occurring for 2 to 3 hours after daybreak and for 3 to 4 hours before nightfall. Although the risk may be higher at these times, it is important to remember that the mosquito may feed indoors at anytime during the day as well as outdoors, especially on overcast days. Precautions, therefore, include staying in screened or air-conditioned rooms, spraying these rooms with aerosol bomb insecticides to kill adult mosquitoes indoors (especially in bedrooms), using a repellent containing dimethyl-metatoluamide (DEET) on exposed skin, and wearing protective clothing treated with a similar repellant. The risk of exposure may be lower in modern, air-conditioned hotels with well-kept grounds and in rural areas.
REFERENCES
- 1.Anonymous. Dengue hemorrhagic fever, diagnosis, treatment and control. Geneva, Switzerland: World Health Organization; 1986. [Google Scholar]
- 2.Anonymous. Dengue in the Americas—time to talk. Lancet. 1997;350:455. . (Editorial.) [PubMed] [Google Scholar]
- 3.Bancroft W H, Scott R M, Eckels K H, Hoke C H, Simms T E, Jesrani K D T, Summers P L, Dubois D R, Tsoulos D, Russell P K (Editorial.) Dengue virus type 2 vaccine: reactogenicity and immunogenicity in soldiers. J Infect Dis. 1984;149:1005–1010. doi: 10.1093/infdis/149.6.1005. [DOI] [PubMed] [Google Scholar]
- 4.Barnes W J S, Rosen L. Fatal hemorrhagic disease and shock associated with primary dengue infection on a pacific island. Am J Trop Med Hyg. 1974;23:495–506. doi: 10.4269/ajtmh.1974.23.495. [DOI] [PubMed] [Google Scholar]
- 5.Becker Y. Dengue fever virus and Japanese encephalitis virus synthetic peptides, with motifs to fit HLA class I haplotypes prevalent in human populations in endemic regions, can be used for applications to skin Langerhans cells to prime antiviral CD8+ cytotoxic T cells (CTLs)—a novel approach to the protection of humans. Virus Genes. 1994;9:33–45. doi: 10.1007/BF01703433. [DOI] [PubMed] [Google Scholar]
- 6.Bhamarapravati, N. 1989. Hemostatic defects in dengue hemorrhagic fever. J. Infect. Dis. 2(Suppl. 4):S826–S829. [DOI] [PubMed]
- 7.Bhamarapravati N. Pathology of dengue infections. In: Gubler D J, Kuno G, editors. Dengue and dengue hemmorhagic fever. London, United Kingdom: CAB International; 1997. pp. 115–132. [Google Scholar]
- 8.Bhamarapravati N. Live attenuated tetravalent dengue vaccine. In: Gubler D J, Kuno G, editors. Dengue and dengue hemorrhagic fever. London, United Kingdom: CAB International; 1997. pp. 367–378. [Google Scholar]
- 9.Bhamarapravati N, Tuchinda P, Boonyapaknavik V. Pathology of Thailand hemorrhagic fever: a study of 100 autopsy cases. Ann Trop Med Parasitol. 1967;61:500–510. doi: 10.1080/00034983.1967.11686519. [DOI] [PubMed] [Google Scholar]
- 10.Bhamarapravati N, Yoksan S. Study of bivalent dengue vaccine in volunteers. Lancet. 1989;i:1077. doi: 10.1016/s0140-6736(89)92471-9. [DOI] [PubMed] [Google Scholar]
- 11.Bhamarapravati N, Yoksan S, Chayaniyayothian T, Angsubhakorn S, Bunyaratvej A. Immunization with a live attenuated dengue-2 virus candidate vaccine (16681-PDK 53): clinical, immunological and biological responses in adult volunteers. Bull W H O. 1987;65:185–195. [PMC free article] [PubMed] [Google Scholar]
- 12.Bielefeldt-Ohmann H. Pathogenesis of dengue virus diseases: missing pieces in the jigsaw. Trends Microbiol. 1997;5:409–413. doi: 10.1016/S0966-842X(97)01126-8. [DOI] [PubMed] [Google Scholar]
- 13.Brandt W E. Current approaches to the development of dengue vaccines and related aspects of the molecular biology of flaviviruses. J Infect Dis. 1988;157:1105–1111. doi: 10.1093/infdis/157.5.1105. [DOI] [PubMed] [Google Scholar]
- 14.Brandt W E. Development of dengue and Japanese encephalitis vaccines. J Infect Dis. 1990;162:577–583. doi: 10.1093/infdis/162.3.577. [DOI] [PubMed] [Google Scholar]
- 15.Brandt W E, McCown J M, Gentry M K, Russell P K. Infection enhancement of dengue-2 virus in the U937 human monocyte cell line by antibodies to flavivirus cross-reactive determinants. Infect Immun. 1982;36:1036–1041. doi: 10.1128/iai.36.3.1036-1041.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bray M, Lai C-J. Construction of intertypic chimeric dengue viruses by substitution of structural protein genes. Proc Natl Acad Sci USA. 1991;88:10342–10346. doi: 10.1073/pnas.88.22.10342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burke D S, Nisalak A, Ussery M A. Antibody capture immunoassay detection of Japanese encephalitis virus immunoglobulin M and G antibodies in cerebrospinal fluid. J Clin Microbiol. 1982;15:1034–1042. doi: 10.1128/jcm.16.6.1034-1042.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burke D S, Nisalak A, Johnson D, Scott R M. A prospective study of dengue infections in Bangkok. Am J Trop Med Hyg. 1988;38:172–180. doi: 10.4269/ajtmh.1988.38.172. [DOI] [PubMed] [Google Scholar]
- 19.Carey D E. Chikungunya and dengue: a case of mistaken identity? J Hist Med Allied Sci. 1971;26:243–262. doi: 10.1093/jhmas/xxvi.3.243. [DOI] [PubMed] [Google Scholar]
- 20.Casey H L. Standardized diagnostic complement fixation method and adaptation to micro-test. Public health monograph 74. U.S. Washington, D.C: Government Printing Office; 1965. [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Imported dengue—United States, 1993 and 1994. Morbid Mortal Weekly Rep. 1995;44:353–356. [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Unpublished data.
- 23.Chambers T J, Tsai T F, Pervikov Y, Monath T P. Vaccine development against dengue and Japanese encephalitis: report of a World Health Organization Meeting. Vaccine. 1997;15:1494–1502. doi: 10.1016/s0264-410x(97)00195-3. [DOI] [PubMed] [Google Scholar]
- 24.Chang, G.-J. 1998. Personal communication.
- 25.Chen W, Kawano H, Men R, Clark D, Lai C-J. Construction of intertypic chimeric dengue viruses exhibiting type 3 antigenicity and neurovirulence for mice. J Virol. 1995;69:5186–5190. doi: 10.1128/jvi.69.8.5186-5190.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chungue E. Molecular epidemiology of dengue viruses. In: Saluzzo J F, Dodet B, editors. Factors in the emergence of arbovirus diseases. Paris, France: Elsevier; 1997. pp. 93–101. [Google Scholar]
- 27.Chungue E, Marche R, Plichart R, Boutin J P, Roux J. Comparison of immunoglobulin G enzyme-linked immunosorbent assay (IgG-ELISA) and hemagglutination inhibition (HI) test for the detection of dengue antibodies. Prevalence of dengue IgG-ELISA antibodies in Tahiti. Trans R Soc Trop Med Hyg. 1989;83:708–771. doi: 10.1016/0035-9203(89)90404-5. [DOI] [PubMed] [Google Scholar]
- 28.Clarke D H, Casals J. Techniques for hemagglutination and hemagglutination-inhibition with arthropod-borne viruses. Am J Trop Med Hyg. 1958;7:561–577. doi: 10.4269/ajtmh.1958.7.561. [DOI] [PubMed] [Google Scholar]
- 29.Deubel V. The contribution of molecular techniques to the diagnosis of dengue infection. In: Gubler D J, Kuno G, editors. Dengue and dengue hemorrhagic fever. London, United Kingdom: CAB International; 1997. pp. 335–366. [Google Scholar]
- 30.Deubel V, Pierre V. Molecular techniques for rapid and more sensitive detection and diagnosis of flaviviruses. In: Spencer R C, Wright E P, Newsom S W B, editors. Rapid methods and automation in microbiology and immunology. Andover, United Kingdom: Intercept; 1994. pp. 227–237. [Google Scholar]
- 31.Deubel V, Bordier M, Megret F, Gentry M K, Schlesinger J J, Girard M. Processing, secretion, and immunoreactivity of caboxy terminally truncated dengue-2 virus envelope proteins expressed in insect cells by recombinant baculoviruses. Virology. 1991;180:442–447. doi: 10.1016/0042-6822(91)90055-g. [DOI] [PubMed] [Google Scholar]
- 32.Dietz V, Gubler D J, Ortiz S, Kuno G, Casta-Velez A, Sather G E, Gomez I, Vergne E. The 1986 dengue and dengue hemorrhagic fever epidemic in Puerto Rico: epidemiologic and clinical observations. P R Health Sci J. 1996;15:201–210. [PubMed] [Google Scholar]
- 33.Dulbecco R. A study of the basic aspects of neutralization of two animal viruses, Western equine encephalitis virus and poliomyelitis virus. Virology. 1956;2:162–205. doi: 10.1016/0042-6822(56)90017-4. [DOI] [PubMed] [Google Scholar]
- 34.Ehrankramz N J, Ventura A K, Guadrado R R. Pandemic dengue in Caribbean countries and the southern United States: past, present and potential problems. N Engl J Med. 1971;285:1460–1469. doi: 10.1056/NEJM197112232852606. [DOI] [PubMed] [Google Scholar]
- 35.Eram S, Setyabudi Y, Sadono T I, Sutrisno D S, Gubler D J, Sulianti-Saroso J. Epidemic dengue hemorrhagic fever in rural Indonesia: clinical studies. Am J Trop Med Hyg. 1979;28:711–716. [PubMed] [Google Scholar]
- 36.Gubler D J. Dengue and dengue hemorrhagic fever in the Americas. P R Health Sci J. 1987;6:107–111. [PubMed] [Google Scholar]
- 37.Gubler D J. Dengue. In: Monath T P, editor. Epidemiology of arthropod-borne viral diseases. Boca Raton, Fla: CRC Press, Inc.; 1988. pp. 223–260. [Google Scholar]
- 38.Gubler D J. Aedes aegypti and Aedes aegypti-borne disease control in the 1990s: top down or bottom up. Am J Trop Med Hyg. 1989;40:571–578. doi: 10.4269/ajtmh.1989.40.571. [DOI] [PubMed] [Google Scholar]
- 39.Gubler D J. Dengue and dengue hemorrhagic fever in the Americas. In: Thoncharoen P, editor. Monograph on dengue/dengue hemorrhagic fever. W.H.O. regional publication SEARO no. 22. New Delhi, India: World Health Organization; 1993. pp. 9–22. [Google Scholar]
- 40.Gubler D J. Arboviruses as imported disease agents: the need for increased awareness. Arch Virol. 1996;11:21–32. doi: 10.1007/978-3-7091-7482-1_3. [DOI] [PubMed] [Google Scholar]
- 41.Gubler D J. Dengue and dengue hemorrhagic fever: its history and resurgence as a global public health problem. In: Gubler D J, Kuno G, editors. Dengue and dengue hemorrhagic fever. London, United Kingdom: CAB International; 1997. pp. 1–22. [Google Scholar]
- 42.Gubler, D. J. The global pandemic of dengue/dengue haemorrhagic fever: current status and prospects for the future. Ann. Acad. Med. Singapore, in press. [PubMed]
- 43.Gubler, D. J. Unpublished data.
- 44.Gubler D J, Casta-Velez A. A program for prevention and control of epidemic dengue and dengue hemorrhagic fever in Puerto Rico and the U.S. Virgin Islands Bull Pan Am Health Org. 1991;25:237–247. [PubMed] [Google Scholar]
- 45.Gubler D J, Clark G G. Dengue/dengue hemorrhagic fever: the emergence of a global health problem. Emerg Infect Dis. 1995;1:55–57. doi: 10.3201/eid0102.952004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gubler D J, Rosen L. A simple technique for demonstrating transmission of dengue viruses by mosquitoes without the use of vertebrate hosts. Am J Trop Med Hyg. 1976;25:146–150. doi: 10.4269/ajtmh.1976.25.146. [DOI] [PubMed] [Google Scholar]
- 47.Gubler D J, Sather G E. Laboratory diagnosis of dengue and dengue hemorrhagic fever. In: Homma A, Cunha J F, editors. Proceedings of the International Symposium on Yellow Fever and Dengue. 1988. pp. 291–322. [Google Scholar]
- 48.Gubler D J, Trent D W. Emergence of epidemic dengue/dengue hemorrhagic fever as a public health problem in the Americas. Infect Agents Dis. 1994;2:383–393. [PubMed] [Google Scholar]
- 49.Gubler D J, Reed D, Rosen L, Hitchcock J C J. Epidemiologic, clinical and virologic observations on dengue in the Kingdom of Tonga. Am J Trop Med Hyg. 1978;27:581–589. doi: 10.4269/ajtmh.1978.27.581. [DOI] [PubMed] [Google Scholar]
- 50.Gubler D J, Suharyono W, Sumarmo, Wulur H, Jahja E, Sulianti Saroso J. Virological surveillance for dengue haemorrhagic fever in Indonesia using the mosquito inoculation technique. Bull W H O. 1979;57:931–936. [PMC free article] [PubMed] [Google Scholar]
- 51.Gubler D J, Suharyono W, Tan R, Abidin M, Sie A. Viremia in patients with naturally acquired dengue infection. Bull W H O. 1981;59:623–630. [PMC free article] [PubMed] [Google Scholar]
- 52.Gubler D J, Kuno G, Sather G E, Vélez M, Oliver A. Use of mosquito cell cultures and specific monoclonal antibodies for routine surveillance of dengue viruses. Am J Trop Med Hyg. 1984;33:158–165. doi: 10.4269/ajtmh.1984.33.158. [DOI] [PubMed] [Google Scholar]
- 53.Gubler D J, Kuno G, Sather G E, Waterman S H. A case of natural concurrent human infection with two dengue viruses. Am J Trop Med Hyg. 1985;34:170–173. doi: 10.4269/ajtmh.1985.34.170. [DOI] [PubMed] [Google Scholar]
- 54.Gubler D J, Sather G E, Kuno G, Cabral J R. Dengue 3 virus transmission in Africa. Am J Trop Med Hyg. 1986;35:1280–1284. doi: 10.4269/ajtmh.1986.35.1280. [DOI] [PubMed] [Google Scholar]
- 55.Guzman M G, Kouri G. Advances in dengue diagnosis. Clin Diagn Lab Immunol. 1996;3:621–627. doi: 10.1128/cdli.3.6.621-627.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hall W C, Crowell T P, Watts D M, Barros V L R, Kruger H, Pinheiro F, Peters C J. Demonstration of yellow fever and dengue antigens in formalin-fixed paraffin embedded human liver by immunohistochemical analysis. Am J Trop Med Hyg. 1991;45:408–417. doi: 10.4269/ajtmh.1991.45.408. [DOI] [PubMed] [Google Scholar]
- 57.Halstead S B. Observations related to pathogenesis of dengue hemorrhagic fever. VI. Hypotheses and discussion. Yale J Biol Med. 1970;42:350–362. [PMC free article] [PubMed] [Google Scholar]
- 58.Halstead S B. Etiologies of the experimental dengues of Siler and Simmons. Am J Trop Med Hyg. 1974;23:974–982. doi: 10.4269/ajtmh.1974.23.974. [DOI] [PubMed] [Google Scholar]
- 59.Halstead S B. Studies on the attenuation of dengue 4. Asian J Infect Dis. 1978;2:112–117. [Google Scholar]
- 60.Halstead S B. In vivo enhancement of dengue virus infection in rhesus monkeys by passively transferred antibody. J Infect Dis. 1979;140:527–533. doi: 10.1093/infdis/140.4.527. [DOI] [PubMed] [Google Scholar]
- 61.Halstead S B. Dengue hemorrhagic fever—public health problem and a field for research. Bull W H O. 1980;58:1–21. [PMC free article] [PubMed] [Google Scholar]
- 62.Halstead S B. Pathogenesis of dengue: challenges to molecular biology. Science. 1988;239:476–481. doi: 10.1126/science.3277268. [DOI] [PubMed] [Google Scholar]
- 63.Halstead S B. The XXth century dengue pandemic: need for surveillance and research. Rapp Trimest Stat Sanit Mond. 1992;45:292–298. [PubMed] [Google Scholar]
- 64.Halstead S B, Shotwell H, Casals J. Studies on the pathogenesis of dengue infection in monkeys. I. Clinical laboratory responses to primary infection. J Infect Dis. 1973;128:7–14. doi: 10.1093/infdis/128.1.7. [DOI] [PubMed] [Google Scholar]
- 65.Halstead S B, Shotwell H, Casals J. Studies on the pathogenesis of dengue infection in monkeys. II. Clinical laboratory responses to heterologous infection. J Infect Dis. 1973;128:15–22. doi: 10.1093/infdis/128.1.15. [DOI] [PubMed] [Google Scholar]
- 66.Halstead S B, O’Rourke E J. Antibody-enhanced dengue virus infection in primate leukocytes. Nature (London) 1977;265:739–741. doi: 10.1038/265739a0. [DOI] [PubMed] [Google Scholar]
- 67.Halstead S B, O’Rourke E J. Dengue viruses and mononuclear phagocytes. I. Infection enchancement by non-neutralizing antibody. J Exp Med. 1977;146:210–217. doi: 10.1084/jem.146.1.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Halstead S B, Venkateshan C N, Gentry M K, Larsen L K. Heterogeneity of infection enhancement of dengue 2 strains by monoclonal antibodies. J Immunol. 1984;312:1529–1532. [PubMed] [Google Scholar]
- 69.Halstead S B, Diwan A R, Marchette J J, Palumbo N E, Srisukonth L. Selection of attenuated dengue 4 viruses by serial passage in primary kidney cells. 1. Attributes of uncloned virus at different passage levels. Am J Trop Med Hyg. 1984;33:654–665. doi: 10.4269/ajtmh.1984.33.654. [DOI] [PubMed] [Google Scholar]
- 70.Hammon W M, Rudnick A, Sather G. New hemorrhagic fevers of children in the Philippines and Thailand. Trans Assoc Am Physicians. 1960;73:140–155. [PubMed] [Google Scholar]
- 71.Hayes E B, Gubler D J. Dengue and dengue hemorrhagic fever. Pediatr Infect Dis J. 1992;11:311–317. doi: 10.1097/00006454-199204000-00010. [DOI] [PubMed] [Google Scholar]
- 72.Henchal E A, McCown J M, Sequin M C, Gentry M K, Brandt W E. Rapid identification of dengue virus isolates by using monoclonal antibodies in an indirect immunofluorescence assay. Am J Trop Med Hyg. 1983;32:164–169. doi: 10.4269/ajtmh.1983.32.164. [DOI] [PubMed] [Google Scholar]
- 73.Hirsch A. Handbook of geographical and historical pathology. Vol. 1. London, United Kingdom: Syndenham Society; 1883. Dengue, a comparatively new disease: its symptoms; pp. 55–81. [Google Scholar]
- 74.Hotta S, Kimura R. Experimental studies on dengue 1. Isolation identification and modification of the virus. J Infect Dis. 1952;90:1–9. doi: 10.1093/infdis/90.1.1. [DOI] [PubMed] [Google Scholar]
- 75.Howe G M. A world geography of human diseases. New York, N.Y: Academic Press, Inc.; 1977. [Google Scholar]
- 76.Igarashi A. Isolation of Singh’s Aedes albopictus cell clone sensitive to dengue and chikungunya viruses. J Gen Virol. 1978;40:530–544. doi: 10.1099/0022-1317-40-3-531. [DOI] [PubMed] [Google Scholar]
- 77.Innis B L. Dengue and dengue hemorrhagic fever. In: Porterfield J S, editor. Exotic viral infections—1995. London, United Kingdom: Chapman & Hall; 1995. pp. 103–146. [Google Scholar]
- 78.Innis B L, Nisalak A, Nimmannitya S, Kusalerdchariya S, Chongswasdi V, Suntayakorn S, Puttisri P, Hoke C H. An enzyme-linked immunosorbent assay to characterize dengue infections where dengue and Japanese encephalitis co-circulate. Am J Trop Med Hyg. 1989;40:418–427. doi: 10.4269/ajtmh.1989.40.418. [DOI] [PubMed] [Google Scholar]
- 79.Kapoor M, Zhang L, Mohan P M, Padmanabhan R. Synthesis and characterization of an infectious dengue virus type-2 RNA genome (New Guinea C strain) Gene. 1995;162:175–180. doi: 10.1016/0378-1119(95)00332-z. [DOI] [PubMed] [Google Scholar]
- 80.Kawano H, Rostapshow V, Rosen L, Lai C-J. Genetic determinants of dengue type 4 virus neurovirulence for mice. J Virol. 1993;67:6567–6575. doi: 10.1128/jvi.67.11.6567-6575.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kimura R, Hotta S. Studies on dengue: anti-dengue active immunization experiments in mice. Jpn J Bacteriol. 1944;1:96–99. [Google Scholar]
- 82.Kinney R M, Butrapet S, Chang G J, Roehrig J T, Tsuchiya K R, Bhamarapraviti N, Gubler D J. Construction of infectious cDNA clones for dengue 2 16681 virus and its attenuated vaccine derivative, strain PDK-53. Virology. 1997;230:300–308. doi: 10.1006/viro.1997.8500. [DOI] [PubMed] [Google Scholar]
- 83.Kliks S C, Nisalak A, Brandt W E, Wahl L, Burke D S. Antibody-dependent enhancement of dengue virus growth in human monocytes as a risk factor for dengue hemorrhagic fever. Am J Trop Med Hyg. 1989;40:444–451. doi: 10.4269/ajtmh.1989.40.444. [DOI] [PubMed] [Google Scholar]
- 84.Kochel T, Wu S-J, Raviprakash K, Hobart P, Hoffman S L, Hayes C G. Inoculation of plasmids expressing the dengue-2 envelope gene elicit neutralizing antibodies in mice. Vaccine. 1997;15:547–552. doi: 10.1016/s0264-410x(97)00215-6. [DOI] [PubMed] [Google Scholar]
- 85.Kouri G, Guzman M G, Valdes L, Carbonel I, del Rosario D, Vazquez S, Laferte J, Delgado J, Cabrera M V. Reemergence of dengue in Cuba: a 1997 epidemic in Santiago de Cuba. Emerg Infect Dis. 1998;4:89–92. doi: 10.3201/eid0401.980111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kuberski T T, Rosen L. A simple technique for the detection of dengue antigen in mosquitoes by immunofluorescence. Am J Trop Med Hyg. 1977;26:533–537. doi: 10.4269/ajtmh.1977.26.533. [DOI] [PubMed] [Google Scholar]
- 87.Kuberski T T, Rosen L, Reed D, Mataika J. Clinical and laboratory observations on patients with primary and secondary dengue type 1 infections with hemorrhagic manifestations in Fiji. Am J Trop Med Hyg. 1977;26:775–783. doi: 10.4269/ajtmh.1977.26.775. [DOI] [PubMed] [Google Scholar]
- 88.Kuno G, Gubler D J, Velez M, Oliver A. Comparative sensitivity of three mosquito cell lines for isolation of dengue viruses. Bull W H O. 1985;63:279–286. [PMC free article] [PubMed] [Google Scholar]
- 89.Kuno G, Gomez I, Gubler D J. An ELISA procedure for the diagnosis of dengue infections. J Virol Methods. 1991;33:101–113. doi: 10.1016/0166-0934(91)90011-n. [DOI] [PubMed] [Google Scholar]
- 90.Kuno G, Gubler D J, Oliver A. Use of original antigenic sin theory to determine the serotypes of previous dengue infections. Trans R Soc Trop Med Hyg. 1993;87:103–105. doi: 10.1016/0035-9203(93)90444-u. [DOI] [PubMed] [Google Scholar]
- 91.Kuno, G., C. B. Cropp, J. Wong-Lee, and D. J. Gubler. Dengue IgM Immunoblot. Am. J. Trop. Med. Hyg., in press. [DOI] [PubMed]
- 92.Kurane I, Ennis F A. Immunopathogenesis of dengue virus infections. In: Gubler D J, Kuno G, editors. Dengue and dengue hemorrhagic fever. London, United Kingdom: CAB International; 1997. pp. 273–290. [Google Scholar]
- 93.Lai C-J, Zhao B, Hori H, Bray M. Infectious RNA transcribed from stably cloned full-length cDNA of dengue type 4 virus. Proc Natl Acad Sci USA. 1991;88:5139–5143. doi: 10.1073/pnas.88.12.5139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Laille M, Deubel V, Flye Sainte Marie F. Demonstration of concurrent dengue 1 and dengue 3 infection in six patients by the polymerase chain reaction. J Med Virol. 1991;34:51–54. doi: 10.1002/jmv.1890340109. [DOI] [PubMed] [Google Scholar]
- 95.Lam S K, Chew C B, Poon G K, Ramalingam S, Seow S C, Pang T. Isolation of dengue viruses by intracerebral inoculation of mosquito larvae. J Virol Methods. 1986;14:133–140. doi: 10.1016/0166-0934(86)90044-3. [DOI] [PubMed] [Google Scholar]
- 96.Lam S K, Fong M Y, Chungue E, Doraisingham S, Igarashi A, Khin M A, Kyaw Z T, Nisalak A, Roche C, Vaughn D W, Vorndam V. Multicentre evaluation of dengue IgM dot enzyme immunoassay. Clin Diagn Virol. 1996;7:93–98. doi: 10.1016/s0928-0197(96)00257-7. [DOI] [PubMed] [Google Scholar]
- 97.Lam S K, Devi S, Pang T. Detection of specific IgM in dengue infections. Southeast Asian J Trop Med Public Health. 1987;18:532–538. [PubMed] [Google Scholar]
- 98.Lanciotti R S, Calisher C H, Gubler D J, Chang G-J, Vorndam A V. Rapid detection and typing of dengue viruses from clinical samples using reverse transcriptase chain reaction. J Clin Microbiol. 1992;30:545–551. doi: 10.1128/jcm.30.3.545-551.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lanciotti R S, Lewis J L, Gubler D J, Trent D W. Molecular evolution and epidemiology of dengue-3 viruses. J Gen Virol. 1994;75:65–75. doi: 10.1099/0022-1317-75-1-65. [DOI] [PubMed] [Google Scholar]
- 100.Lewis J A, Chang G J, Lanciotti R S, Kinney R M, Mayer L W, Trent D W. Phylogenetic relationships of dengue-2 viruses. Virology. 1993;197:216–224. doi: 10.1006/viro.1993.1582. [DOI] [PubMed] [Google Scholar]
- 101.Mason P W, Dalrymple J M, Gentry M K, McCown J M, Hoke C H, Burke D S, Fournier M J, Mason T L. Molecular characterization of a neutralizing domain of the Japanese encephalitis virus structural glycoprotein. J Gen Virol. 1989;70:2037–2049. doi: 10.1099/0022-1317-70-8-2037. [DOI] [PubMed] [Google Scholar]
- 102.Mason P W, Pincus S, Fournier M J, Mason T L, Shope R E, Paoletti E. Japanese encephalitis virus-vaccinia recombinants produce particulate forms of the structural membrane proteins and induce high levels of protection against lethal JEV infection. Virology. 1991;180:294–305. doi: 10.1016/0042-6822(91)90034-9. [DOI] [PubMed] [Google Scholar]
- 103.McSherry J A. Some medical aspects of the Darien schema: was it dengue? Scot Med J. 1982;27:183–184. doi: 10.1177/003693308202700215. [DOI] [PubMed] [Google Scholar]
- 103a.Monath, T. P. Personal communication.
- 104.Monath T P. Dengue: the risk to developed and developing countries. Proc Natl Acad Sci USA. 1994;91:2395–2400. doi: 10.1073/pnas.91.7.2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Moore C G, Mitchell C J. Aedes albopictus in the United States: ten-year presence and public health implications. Emerg Infect Dis. 1997;3:329–334. doi: 10.3201/eid0303.970309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Morens D M, Venkateshan C N, Halstead S B. Dengue 4 virus monoclonal antibodies indentify epitopes that mediate immune enhancement of dengue 2 viruses. J Gen Virol. 1987;68:91–98. doi: 10.1099/0022-1317-68-1-91. [DOI] [PubMed] [Google Scholar]
- 107.Newton E A C, Rieter P. A model of the transmission of dengue fever with an evolution of the impact of ultra-low volume (ULV) insecticide application on dengue epidemics. Am J Trop Med Hyg. 1992;47:709–720. doi: 10.4269/ajtmh.1992.47.709. [DOI] [PubMed] [Google Scholar]
- 108.Nobuchi H. The symptoms of a dengue-like illness recorded in a Chinese medical encyclopedia. Kanpo Rinsho. 1979;26:422–425. . (In Japanese.) [Google Scholar]
- 109.Pepper O H P. A note on David Bylon and dengue. Ann Med Hist 3rd Ser. 1941;3:363–368. [PMC free article] [PubMed] [Google Scholar]
- 110.Pinheiro F P. Dengue in the Americas, 1980–1987. Epidemiol Bull. 1989;10:1. [PubMed] [Google Scholar]
- 111.Pinheiro F P, Corber S J. Global situation of dengue and dengue haemorrhagic fever, and its emergence in the Americas. World Health Stat Q. 1997;50:161–169. [PubMed] [Google Scholar]
- 112.Platt K B, Linthicum K J, Myint K S A, Innis B L, Lerdthusnee K, Vaughn D W. Impact of dengue virus infection on feeding behavior of Aedes aegypti. Am J Trop Med Hyg. 1997;57:119–125. doi: 10.4269/ajtmh.1997.57.119. [DOI] [PubMed] [Google Scholar]
- 113.Polo S, Ketner G, Levis R, Falgout B. Infectious RNA transcripts from full-length dengue virus type 2 cDNA clones made in yeast. J Virol. 1997;71:5366–5374. doi: 10.1128/jvi.71.7.5366-5374.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Putnam J L, Scott T W. Blood feeding behavior of dengue-2 virus-infected Aedes aegypti. Am J Trop Med Hyg. 1995;55:225–227. doi: 10.4269/ajtmh.1995.52.225. [DOI] [PubMed] [Google Scholar]
- 115.Reiter P, Gubler D J. Surveillance and control of urban dengue vectors. In: Gubler D J, Kuno G, editors. Dengue and dengue hemorrhagic fever. London, United Kingdom: CAB International; 1997. pp. 425–462. [Google Scholar]
- 116.Rico-Hesse R. Molecular evolution and distribution of dengue viruses type 1 and 2 in nature. Virology. 1990;174:479–493. doi: 10.1016/0042-6822(90)90102-w. [DOI] [PubMed] [Google Scholar]
- 117.Rico-Hess R, Harrison L, Salas R, Tovar D, Nisalak A, Ramos C, Boshell J R, de Mesa M, Nogueira R, Travassos da Rosa A. Origins of dengue type 2 viruses associated with increased pathogenicity in the Americas. Virology. 1997;230:244–251. doi: 10.1006/viro.1997.8504. [DOI] [PubMed] [Google Scholar]
- 118.Rigau-Pérez J G, Gubler D J. Surveillance for dengue and dengue hemorrhagic fever. In: Gubler D J, Kono G, editors. Dengue and dengue hemorrhagic fever. London, United Kingdom: CAB International; 1997. pp. 405–423. [Google Scholar]
- 119.Rigau-Pérez J G, Gubler D J, Vorndam A V, Clark G G. Dengue surveillance—United States, 1986–1992. Morbid Mortal Weekly Rep. 1994;43(SS-2):7–19. [PubMed] [Google Scholar]
- 120.Rodier G, Gubler D J, Cope S E, Bercion R, Cropp C B, Soliman A K, Bouloumie J, Piccolo J-J, Polycarpe D, Abdourhaman J A, Delmaire P, Bonnet J-P, Parra J-P, Gray G G, Fryauff D J. Epidemic dengue 2 in the city of Djibouti, Horn of Africa, 1991–1992. Trans R Soc Trop Med Hyg. 1995;90:237–240. doi: 10.1016/s0035-9203(96)90228-x. [DOI] [PubMed] [Google Scholar]
- 121.Roehrig J T, Johnson A H, Hunt A R, Beaty B J, Mathews J H. Enhancement of the antibody response to flavivirus B-cell epitopes by using homologous or heterologous T-cell epitopes. J Virol. 1992;66:3385–3390. doi: 10.1128/jvi.66.6.3385-3390.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Roehrig J T, Mathews J H, Risi P A, Brubaker J R, Hunt A R. Mapping of biologically active helper T-cell epitopes on the flavivirus envelope glycoprotein. In: Brown F, Chanock R M, Ginsberg H, Lerner R A, editors. Vaccines 92. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory; 1992. pp. 277–281. [Google Scholar]
- 123.Rosen L. The Emperor’s new clothes revisited, or reflections on the pathogenesis of dengue hemorrhagic fever. Am J Trop Med Hyg. 1977;26:337–343. doi: 10.4269/ajtmh.1977.26.337. [DOI] [PubMed] [Google Scholar]
- 124.Rosen L. Dengue—an overview. In: Mackenzie J S, editor. Viral diseases in Southeast Asia and the Western Pacific. Sydney, Australia: Academic Press, Ltd.; 1982. pp. 484–493. [Google Scholar]
- 125.Rosen L, Gubler D J. The use of mosquitoes to detect and propagate dengue viruses. Am J Trop Med Hyg. 1974;21:1153–1160. doi: 10.4269/ajtmh.1974.23.1153. [DOI] [PubMed] [Google Scholar]
- 126.Rosen, L., and D. J. Gubler. Unpublished data.
- 127.Rothman A L. Viral pathogenesis of dengue infections. In: Gubler D J, Kuno G, editors. Dengue and dengue hemorrhagic fever. London, United Kingdom: CAB International; 1997. pp. 245–272. [Google Scholar]
- 128.Rush A B. An account of the bilious remitting fever, as it appeared in Philadelphia in the summer and autumn of the year 1780. Medical enquiries and observations. Philadelphia, Pa: Prichard and Hall; 1789. pp. 104–117. [Google Scholar]
- 129.Russell P K, Nisalak A A. Plaque reduction test for dengue virus neutralizing antibodies. J Immunol. 1967;99:285–290. [PubMed] [Google Scholar]
- 130.Russell P K. Progress toward dengue vaccines. Asian J Infect Dis. 1978;2:118–120. [Google Scholar]
- 131.Sabin A B. Research on dengue during World War II. Am J Trop Med Hyg. 1952;1:30–50. doi: 10.4269/ajtmh.1952.1.30. [DOI] [PubMed] [Google Scholar]
- 132.Sabin A B, Schlesinger R W. Production of immunity to dengue with virus modified by propagation in mice. Science. 1945;101:640–642. doi: 10.1126/science.101.2634.640. [DOI] [PubMed] [Google Scholar]
- 133.Sangkawibha N, Rojanasuphot S, Ahandrink S, Viriyapongse S, Jatanasen S, Salitul V, Phanthumachinda B, Halstead S B. Risk factors in dengue shock syndrome: a prospective epidemiologic study in Rayong, Thailand. Am J Epidemiol. 1984;120:653–669. doi: 10.1093/oxfordjournals.aje.a113932. [DOI] [PubMed] [Google Scholar]
- 134.Scherer W E, Russell P K, Rosen L, Casals J, Dickerman R W. Experimental infection of chimpanzees with dengue viruses. Am J Trop Med Hyg. 1978;27:590–599. doi: 10.4269/ajtmh.1978.27.590. [DOI] [PubMed] [Google Scholar]
- 135.Scott T W, Naksathit A, Day J F, Kittayapong P, Edman J D. A fitness advantage for Aedes aegypti and the viruses it transmits when females feed only on human blood. Am J Trop Med Hyg. 1997;57:235–239. doi: 10.4269/ajtmh.1997.57.235. [DOI] [PubMed] [Google Scholar]
- 136.Siler J F, Hall M W, Hitchens A. Dengue, its history, epidemiology, mechanism of transmission, etiology, clinical manifestations, immunity and prevention. Philipp J Sci. 1926;29:1–304. [Google Scholar]
- 137.Soper F L, Wilson D B, Lima S, Antunes W S. The organization of permanent nationwide anti-Aedes aegypti measures in Brazil. New York, N.Y: The Rockefeller Foundation; 1943. [Google Scholar]
- 138.Sumarmo S P S. Demam berdarah dengue pada anak di Jakarta. Ph.D. thesis. Jakarta: University of Indonesia; 1983. [Google Scholar]
- 139.Sumarmo S P S, Wulur H, Jahja E, Gubler D J. Clinical observations on virologically confirmed fatal dengue infections in Jakarta, Indonesia. Bull W H O. 1983;61:693–701. [PMC free article] [PubMed] [Google Scholar]
- 140.Tan B-H, Fu J, Sugrue R J, Yap E-H, Chan Y-C, Tan Y H. Recombinant dengue type 1 virus NS5 protein expressed in Escherichia coli exhibits RNA-dependent RNA polymerase activity. Virology. 1996;216:317–325. doi: 10.1006/viro.1996.0067. [DOI] [PubMed] [Google Scholar]
- 141.Tesh R B. A method for the isolation and identification of dengue viruses, using mosquito cell cultures. Am J Trop Med Hyg. 1979;28:1053–1059. doi: 10.4269/ajtmh.1979.28.1053. [DOI] [PubMed] [Google Scholar]
- 142.Thet-Win Detection of dengue virus by immunofluorescence after intracerebral inoculation of mosquitoes. Lancet. 1982;i:53–54. doi: 10.1016/s0140-6736(82)92604-6. [DOI] [PubMed] [Google Scholar]
- 143.Trent D W, Grant J A, Monath T P, Manske C L, Corina M, Fox G E. Genetic variation and microevolution of dengue 2 virus in Southeast Asia. Virology. 1989;172:523–535. doi: 10.1016/0042-6822(89)90195-5. [DOI] [PubMed] [Google Scholar]
- 144.Trent D W, Kinney R M, Huang C Y-H. Recombinant dengue virus vaccines. In: Gubler D J, Kuno G, editors. Dengue and dengue hemorrhagic fever. London, United Kingdom: CAB International; 1997. pp. 379–404. [Google Scholar]
- 145.Vaughn D W, Hoke C H, Yoksan S, LaChance R, Innis B L, Rice R, Bhamarapravati N. Testing of dengue-2 live attenuated vaccine (strain 16681) (PDK-53) in ten American volunteers. Vaccine. 1996;14:329–336. doi: 10.1016/0264-410x(95)00167-y. [DOI] [PubMed] [Google Scholar]
- 146.Vaughn D W, Nisalak A, Kalayanarooj S, Solomon T, Dung N M, Cuzzubbo A, Devine P L. Evaluation of a rapid immunochromatographic test for diagnosis of dengue virus infection. J Clin Microbiol. 1998;36:234–238. doi: 10.1128/jcm.36.1.234-238.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Vaughn D W, Green S, Kalayanarooj S, Innis B L, Nimmannitya S, Suntayakorn S, Rothman A L, Ennis F A, Nisalak A. Dengue in the early febrile phase: viremia and antibody responses. J Infect Dis. 1997;176:322–330. doi: 10.1086/514048. [DOI] [PubMed] [Google Scholar]
- 148.Vorndam V, Kuno G. Laboratory diagnosis of dengue virus infections. In: Gubler D J, Kuno G, editors. Dengue and dengue hemorrhagic fever—1997. London, United Kingdom: CAB International; 1997. pp. 313–334. [Google Scholar]
- 149.Waterman S H, Gubler D J. Dengue fever. Clin Dermatol. 1989;7:117–122. doi: 10.1016/0738-081x(89)90034-5. [DOI] [PubMed] [Google Scholar]
- 150.Westaway E G, Blok J. Taxonomy and evolutionary relationships of flaviviruses. In: Gubler D J, Kuno G, editors. Dengue and dengue hemorrhagic fever. London, United Kingdom: CAB International; 1997. pp. 147–173. [Google Scholar]
- 151.Wisseman C L, Jr, Sweet B H, Rosenzweig E C, Rylar O R. Attenuated living type 1 dengue vaccines. Am J Trop Med Hyg. 1963;12:620–623. [Google Scholar]
- 152.Wittesjo B, Eitrem R, Niklasson B. Dengue fever among Swedish tourists. Scand J Infect Dis. 1993;25:699–704. doi: 10.3109/00365549309008566. [DOI] [PubMed] [Google Scholar]
- 153.Wu S-J, Hanson B, Paxton H, Nisalak A, Vaughn D W, Rossi C, Henchal E A, Porter K R, Watts D M, Hayes C G. Evaluation of a dipstick enzyme-linked immunosorbent assay for detection of antibodies to dengue virus. Clin Diagn Lab Immunol. 1997;4:452–457. doi: 10.1128/cdli.4.4.452-457.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Yoksan S, Bhamarapravati N, Halstead S B. Dengue virus vaccine development: study on biological markers of uncloned dengue 1–4 viruses serially passaged in primary kidney cells. In: St. George T D, Kay B H, Blok J, editors. Arborvirus research in Australia. Proceedings of the Fourth Symposium. Brisbane, Australia: CSIRO and Queensland Institute of Medical Research; 1986. pp. 35–38. [Google Scholar]
- 155.Yuill T M, Sukkhavachana P, Nisalak A, Russell P K. Dengue-virus recovery by direct and delayed plagues in LLC-MK2 cells. Am J Trop Med Hyg. 1968;17:441–448. doi: 10.4269/ajtmh.1968.17.441. [DOI] [PubMed] [Google Scholar]
- 156.Zaki S R, Peters C J. Viral hemorrhagic fevers. In: Connor D H, Chandler F W, Schwartz D A, Manz H J, Lack E E, editors. Diagnostic pathology of infectious diseases. Stamford, Conn: Appleton & Lange; 1997. pp. 347–364. [Google Scholar]