Abstract
Objectives
To compare trajectories of marriage and parenthood in individuals with JIA vs the general population.
Methods
Patients with JIA (n = 4399) were identified in the Swedish National Patient Register (2001–2016) and individually matched to up to five general population comparators on birthyear, sex and residence county (n = 21 981). Marriage and parenthood data were retrieved from the Total Population Register from age 18 y, and parenthood from the Multigeneration Register from age 15 y, respectively. Hazard ratios (HRs) were estimated using Cox regression adjusted for parental education, parental marital status and number of siblings.
Results
During a median of 6.3 years of follow-up, 362 patients with JIA and 1744 comparators got married (12.9 vs. 12.5 per 1000 person-years; HR 1.03, 95%CI 0.93-1.15). During a median of 8.8 years of follow-up, 680 patients with JIA and 3477 matched comparators became parents (17.1 vs 17.8 per 1000 person-years; HR 0.94, 95%CI 0.87-1.01). In the subgroup of patients with systemic onset JIA (SJIA), the adjusted hazard ratios for marriage and parenthood were 0.79 (95%CI 0.53-1.17) and 0.73 (95%CI 0.55-0.97), respectively.
Conclusion
The times to first marriage and first parenthood are similar for patients with JIA and the general population, suggesting that adolescents with JIA transition into family life along a trajectory resembling their community peers. One exception is the subgroup of patients with systemic onset JIA, who become parents for the first time at a lower rate than general population comparators.
Keywords: juvenile idiopathic arthritis, marriage, parenthood
Rheumatology key messages.
We investigate probability that patients with juvenile idiopathic arthritis marry and have children for the first time.
Patients with juvenile idiopathic arthritis in Sweden marry and have children at rate similar to community peers.
The subgroup with systemic onset juvenile idiopathic arthritis are less likely to have children relative to community peers.
Introduction
JIA is the most common rheumatic disease in childhood [1]. During the last 20 years, the introduction of biologic therapies such as TNF inhibitors (TNFi) has greatly improved the treatment of JIA [2]. Without effective treatment, JIA may have devastating direct consequences in terms of pain, functional disability and growth [3]. Beyond but through these direct consequences, JIA may also impact future life trajectories such as marriage and parenting. These family events are important outcomes in the lives of young women and men, and likely closely connected to concerns that patients with JIA have about how the disease will affect their personal lives.
Previous research has produced mixed results on the marital relationships of patients with JIA, and largely reflects the impact of past treatment paradigms. A survey from 2005 among 123 patients in Finland showed similar rates of spousal relationships among patients relative to comparators matched on age, sex and municipality of residence [4]. A study from 2002 of 246 patients with JIA in the UK [5], in contrast, showed that patients with JIA were less likely to be involved in a stable relationship relative to their own siblings.
With respect to parenting, a Norwegian study [6] from 2011 compared 75 middle aged women with JIA to age- and sex-matched comparators from the general population, and reported that women with JIA had lower fecundity than their comparators. A second Norwegian study from 2000 based on a survey of 126 women with JIA [7] (median age 24 y) reported that married women had a similar fecundity as their healthy comparators.
The aim of this study was therefore to investigate the probability that men and women with JIA marry and have children for the first time, relative to men and women from the general population, based on larger and more recent populations.
JIA is a heterogeneous group of conditions. Systemic onset JIA (SJIA) is distinguished from other JIA subgroups by its clinical features, pathogenesis and treatment protocol [8], and has the highest morbidity and mortality [9]. A second aim of this study was to examine the probability of marriage and parenthood in this JIA subset.
Methods
This study was carried out with a linkage connecting several nationwide Swedish registers, using the unique personal identification number of each Swedish resident. Ethical approval was granted by the Regional Ethics Committee in Stockholm, Sweden.
Patients with JIA were required to have two or more diagnoses (main or supplementary) in the National Patient Register (in- or outpatient care) from 2001 to 2016 at an age below 16 y (ICD-10 codes M05, M06, M07, M08 and M09). Patients with only one diagnosis were excluded because they are more likely misdiagnosed or the result of a data entry error. It was further required that patients were born in 2000 or earlier, to ensure that they could reach age 18 y (the minimum age for legal marriage in Sweden) before end of follow-up, and also required that patients lived until age 15 y (start of follow-up for parenthood) (Supplementary Fig. S1, available at Rheumatology online). The subgroup of patients with SJIA were identified as having at least one registration listing ICD-10 code M08.2.
For each patient, up to five comparators from the general population were identified in the Total Population Register [10], matched on birth year, sex and residence county. General population comparators were excluded if they had a JIA diagnosis prior to inclusion, and if they died before age 15 y.
Outcomes
Time to first marriage was established up until 2018 through data from the Total Population Register, containing the marital status of Swedish residents at the end of each calendar year (31 December) [10]. Our registry data do not capture individuals who are living together without being married (cohabitants). Time to first parenthood was established up until the end of 2018 with the Multigeneration Register, linking children born in Sweden to their biological parents. Our data on parenthood covers biological children who were alive at birth (no adoptions). Individuals were followed until death, emigration or end of follow-up.
Parental data
Parents of patients with JIA and comparators were identified through the Multigeneration Register. Parents’ educational level was retrieved from the LISA Register [11] at Statistics Sweden and categorized into ≤9, 10–12 and >12 years. The data on the education of fathers and mothers was merged into one variable recording the highest education among the two parents. We lack data on the completed education of children at the start of follow-up when children are still young, and therefore use the education of parents to adjust for potential confounding across families due to socioeconomic status. The marital status of parents when the patient with JIA was 15 years old was combined into a dichotomous variable taking the value one when both parents were married in that year. The number of full and half siblings of patients with JIA and comparators was retrieved from the Multigeneration Register.
Statistical analysis
Kaplan–Meier cumulative hazard functions were used to present absolute probabilities of first marriage and parenthood. Cox regression was used to estimate hazard ratios for the outcomes among patients with JIA relative to matched comparators. The regressions were conditioned on the matching set with each set consisting of one patient and up to five comparators. Adjustment was made for the highest education of the parents, the number of siblings and parental marital status. The analyses were stratified by sex.
Data were analysed using SAS (version 9.4, SAS Institute, Cary, NC, USA) and Stata (version 13.1, College Station, TX, USA). All tests were two-sided and P-values <0.05 were considered statistically significant.
Results
In total, 4399 patients with JIA were identified in the National Patient Register from 2001 to 2016, together with 21 981 comparators from the general population, matched on birth year, sex and residence county (Table 1). Among the patients with JIA, 63.8% (n = 2808) were women and the mean age at identification was 11.0 y (SD 3.6) for girls and 10.8 y (SD 3.5) for boys. At the end of follow-up in 2018, the mean age of women and men with JIA was 25.0 y and 24.5 y, respectively. Relative to their matched comparators, patients with JIA had a similar number of siblings and their parents had a similar educational attainment. Slightly more parents of patients with JIA were married relative to the parents of the comparators. A total of 408 (9.3%) patients were identified as patients with SJIA (Table 1).
Table 1.
Characteristics of patients with juvenile idiopathic arthritis and matched (by birth year, sex and residence county) comparators
| Women |
Men |
|||
|---|---|---|---|---|
| JIA | Matched Comparators | JIA | Matched Comparators | |
| (n = 2808) | (n = 14 032) | (n = 1591) | (n = 7949) | |
| Age at identification (years), mean (s.d.) | 11.0 (3.6) | 11.0 (3.6) | 10.8 (3.5) | 10.8 (3.5) |
| Age 0–5 y, n (%) | 313 (11) | 1589 (11) | 199 (13) | 1007 (13) |
| Age 6–10 y, n (%) | 902 (32) | 4449 (32) | 500 (31) | 2521 (32) |
| Age 11–15 y, n (%) | 1593 (57) | 7994 (57) | 892 (56) | 4421 (56) |
| Age 2018 (years), mean (s.d.) | 25.0 (4.1) | 25.0 (4.1) | 24.5 (4.0) | 24.5 (4.0) |
| Year of identification, median (q1–q3) | 2003 | 2003 | 2004 | 2004 |
| (2001–2007) | (2001–2007) | (2001–2008) | (2001–2008) | |
| SJIA,an (%) | 241 (9) | 167 (10) | ||
| Number of siblings,b mean (s.d.) | 2.0 (1.4) | 2.1 (1.6) | 2.0 (1.4) | 2.1 (1.5) |
| Parents’ highest education | ||||
| Primary school, n (%) | 85 (3) | 730 (5) | 62 (4) | 438 (6) |
| High school, n (%) | 1304 (46) | 6148 (44) | 718 (45) | 3385 (43) |
| University, n (%) | 1376 (49) | 6798 (48) | 788 (50) | 3944 (50) |
| Education data missing, n (%) | 43 (2) | 356 (3) | 23 (1) | 182 (2) |
| Parents married when child 15 y, n (%) | 1529 (54) | 6860 (49) | 848 (53) | 3911 (49) |
Systemic onset juvenile idiopathic arthritis. bNot including the patient with JIA or the matched comparator. SJIA: systemic onset JIA.
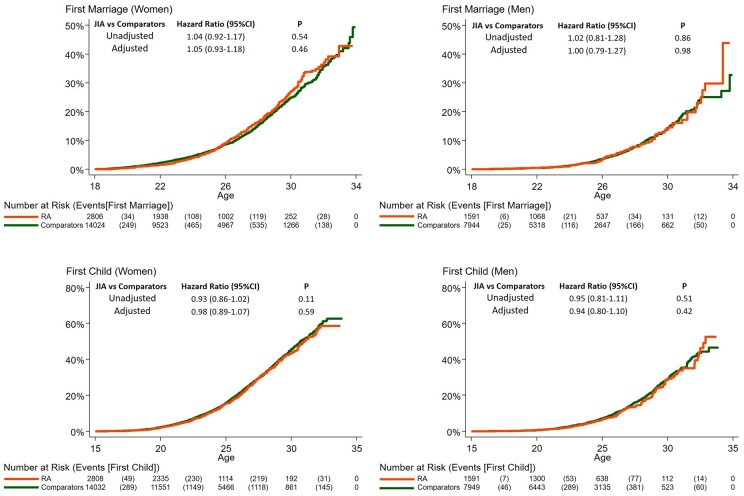
Marriage
During a median of 6.5 years of follow-up, 289 women with JIA and 1387 women among matched comparators married for the first time (15.9 vs 15.3 per 1000 person-years; adjusted hazard ratio 1.05, 95%CI 0.93-1.18; P=0.46; Figure 1). During a median of 6.0 years of follow-up, 73 men with JIA and 357 men among matched comparators married for the first time (7.3 vs 7.2 per 1000 person-years; adjusted hazard ratio 1.00, 95%CI 0.79-1.27; P=0.98).
Fig. 1.
Cumulative incidence of marriage and parenthood for patients with juvenile idiopathic arthritis
Cumulative incidence of marriage (top) and parenthood (bottom) for women (left) and men (right) with JIA and their matched general population comparators. The figure displays crude and adjusted hazard ratios from a Cox proportional hazard model adjusted for matching strata, highest parental education, parental marital status and number of siblings.
Parenthood
During a median of 8.8 years of follow-up, 529 women with JIA and 2701 women among matched comparators became parents for the first time (20.9 vs 21.6 per 1000 person-years; adjusted hazard ratio 0.98, 95%CI 0.89-1.07; P=0.59; Figure 1). During a median of 8.7 years of follow-up, 151 men with JIA and 776 men among matched comparators became parents for the first time (10.5 vs 10.9 per 1000 person-years; adjusted hazard ratio 0.94, 95%CI 0.80-1.10; P=0.42).
Subgroup analysis SJIA
During a median of 6.3 years of follow-up, 25 patients with SJIA and 145 matched comparators married for the first time (9.5 vs 11.0 per 1000 person-years; adjusted hazard ratio 0.79, 95%CI 0.53-1.17; P=0.24; Supplementary Fig. S2, available at Rheumatology online).
During a median of 9.0 years of follow-up, 47 patients with SJIA and 314 matched comparators became parents for the first time (12.6 vs 17.1 per 1000 person-years; adjusted hazard ratio 0.73, 95%CI 0.55-0.97; P=0.03; Supplementary Fig. S2, available at Rheumatology online).
Discussion
We examined the probability that patients with JIA in Sweden marry and have children, relative to general population comparators matched on birthyear, sex and residence county. In our main analysis, we did not find any difference between patients with JIA and their comparators regarding marriage and parenthood, suggesting that patients with JIA transition into early family life along a trajectory resembling their community peers.
In the subset with SJIA, however, the probability of becoming a parent was significantly lower than for the general population, and the probability of marriage was numerically lower than for the general population.
We cannot infer from our analysis why we do not detect any difference in the probabilities of patients with JIA marrying and having children relative to the matched comparators. We speculate that improvements over time in the clinical treatment of patients with JIA, such as the introduction of new biological drugs, has enhanced the general health of these patients and led to family outcomes similar to those of the general population. For the subgroup of patients with SJIA, we speculate that greater physical and mental health problems reduce their likelihood of becoming a parent.
The main strengths of our analysis are that we can identify a large group of patients with JIA, we have long follow-up for both marriage and parenthood, and a patient group identified from national registers ensuring high generalizability of the results. The main limitations are that we have data on legal marriage but not on partners who live together (cohabit) without being legally married. Another limitation is that we at most can follow patients and comparators until their mid-thirties.
In summary, our analysis shows that although JIA is a serious and potentially disabling disease, young men and women with JIA in Sweden who receive modern treatment are able to marry and have children (up until their mid-thirties) at a rate similar to their community peers. One exception is the group of patients with SJIA, who appear to transition from adolescence into early family life at a lower rate than general population comparators.
Supplementary Material
Acknowledgements
This study received funding from the patient organization The Swedish Rheumatism Association (Svenska Reumatikerförbundet) who evaluated the design of the study. We plan to present our results at events organized by the Association for patients and health care professionals.
All authors participated in the design of the study. G.B. conducted the statistical analyses. All authors contributed to interpretation of the results. G.B. and M.N. contributed to the drafting of the manuscript. All authors contributed to the critical revision of the manuscript for important intellectual content. The study was supervised by J.A.
Ethical approval was from Regional Ethics Committee, Stockholm, Sweden. 2015/1844–31/2.
Funding: This work was supported by a grant from the Swedish Rheumatism Association (Svenska Reumatikerförbundet) [R-931130]. Funders had no impact on the design or interpretation of the study or its results.
Disclosure statement: Karolinska Institutet has entered agreements (J.A. as principal investigator) with the following companies mainly regarding the safety monitoring of b/ts DMARDs in rheumatology: AbbVie, BMS, MSD, Eli Lilly, Pfizer, Roche, Samsung Bioepis, Sanofi and UCB.
Data availability statement
Data may be obtained from a third party and are not publicly available. The study data forms part of a register linkage performed by Karolinska Institutet, and for which further sharing of the data is limited by legal restrictions.
Supplementary data
Supplementary data are available at Rheumatology online.
References
- 1. Prakken B, Albani S, Martini A.. Juvenile idiopathic arthritis. Lancet 2011;377:2138–49. [DOI] [PubMed] [Google Scholar]
- 2. Stoll ML, Cron RQ.. Treatment of juvenile idiopathic arthritis: a revolution in care. Pediatr Rheumatol Online J 2014;12:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dewoolkar M, Cimaz R, Chickermane PR, Khubchandani RP.. Course, outcome and complications in children with systemic onset juvenile idiopathic arthritis. Indian J Pediatr 2017;84:294–8. [DOI] [PubMed] [Google Scholar]
- 4. Arkela-Kautiainen M, Haapasaari J, Kautiainen H. et al. Favourable social functioning and health related quality of life of patients with JIA in early adulthood. Ann Rheum Dis 2005;64:875–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Packham JC, Hall MA.. Long-term follow-up of 246 adults with juvenile idiopathic arthritis: social function, relationships and sexual activity. Rheumatology 2002;41:1440–3. [DOI] [PubMed] [Google Scholar]
- 6. Wallenius M, Skomsvoll JF, Irgens LM. et al. Fertility in women with chronic inflammatory arthritides. Rheumatology 2011;50:1162–7. [DOI] [PubMed] [Google Scholar]
- 7. Ostensen M, Almberg K, Koksvik HS.. Sex, reproduction, and gynecological disease in young adults with a history of juvenile chronic arthritis. J Rheumatol 2000;27:1783–7. [PubMed] [Google Scholar]
- 8. Barut K, Adrovic A, Sahin S. et al. Prognosis, complications and treatment response in systemic juvenile idiopathic arthritis patients: a single-center experience. Int J Rheum Dis 2019;22:1661–9. [DOI] [PubMed] [Google Scholar]
- 9. Lee JJY, Schneider R.. Systemic juvenile idiopathic arthritis. Pediatr Clin North Am 2018;65:691–709. [DOI] [PubMed] [Google Scholar]
- 10. Ludvigsson JF, Almqvist C, Bonamy AK. et al. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol 2016;31:125–36. [DOI] [PubMed] [Google Scholar]
- 11. Ludvigsson JF, Svedberg P, Olen O, Bruze G, Neovius M.. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur J Epidemiol 2019;34:423–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data may be obtained from a third party and are not publicly available. The study data forms part of a register linkage performed by Karolinska Institutet, and for which further sharing of the data is limited by legal restrictions.