Abstract
Background
Inflammatory bowel diseases (IBD) are rising in prevalence and are associated with high health care costs. We estimated trends in U.S. health care spending in patients with IBD between 1996 and 2016.
Methods
We used data on national health care spending developed by the Institute for Health Metrics and Evaluations for the Disease Expenditure Project. We estimated corresponding U.S. age-specific prevalence of IBD from the Global Burden of Diseases Study. From these 2 sources, we estimated prevalence-adjusted, temporal trends in U.S. health care spending in patients with IBD, stratified by age groups (<20 years, 20-44 years, 45-64 years, ≥65 years) and by type of care (ambulatory, inpatient, emergency department [ED], pharmaceutical prescriptions, and nursing care), using joinpoint regression, expressed as an annual percentage change (APC) with 95% confidence intervals.
Results
Overall, annual U.S. health care spending on IBD increased from $6.4 billion (95% confidence interval, 5.7-7.4) in 1996 to $25.4 billion (95% confidence interval, 22.4-28.7) in 2016, corresponding to a per patient increase in annual spending from $5714 to $14,033. Substantial increases in per patient spending on IBD were observed in patients aged ≥45 years. Between 2011 and 2016, inpatient and ED care accounted for 55.8% of total spending and pharmaceuticals accounted for 19.9%, with variation across age groups (inpatient/ED vs pharmaceuticals: ages ≥65 years, 57.6% vs 11.2%; ages 45-64 years, 49.5% vs 26.9%; ages 20-44 years, 59.2% vs 23.6%).
Conclusions
Even after adjusting for rising prevalence, U.S. health care spending on IBD continues to progressively increase, primarily in middle-aged and older adults, with unplanned health care utilization accounting for the majority of costs.
Keywords: costs, expenses, value-based care, Crohn disease, colitis
INTRODUCTION
In the United States, approximately 1.8 to 3.1 million adults are affected by IBD, and although the incidence may have stabilized, prevalence of the disease continues to rise particularly among middle-aged and older adults.1, 2 Patients with IBD are typically diagnosed at a young age and experience a protracted, relapsing-and-remitting course that necessitates repeated health care encounters in both the elective and emergent setting, along with high associated health care costs. With the advent of biologic agents, clinical outcomes have improved with higher rates of remission and a lower risk of surgery, along with a decline in hospitalization in Canada and some European countries.3-5 However, rates of unplanned health care utilization, including inpatient care and emergency department (ED), visits have continued to rise in patients with IBD in the United States.6-8 Although health care spending in patients with IBD has shifted from inpatient care toward biologic therapy in Europe and Canada, there has been limited evaluation of trends and patterns in health care spending in patients with IBD in the United States.
We evaluated trends and patterns of health care spending in patients with IBD in the United States between 1996 and 2016, overall, by age, and by type of care, using 2 large publicly available databases. The U.S. Disease Expenditure (DEX) 2016 project aggregates data from 183 sources, leveraging the strength of each source to produce modeled estimates of spending and volume for 154 health conditions in the United States.9 The Global Burden of Disease (GBD) 2017 study aggregates data from multiple sources to estimate prevalence, incidence, deaths, and other epidemiologic metrics by age and sex groups for 354 conditions.10
METHODS
Data Sources and Study Population
This study used publicly available data from the DEX project and the GBD 2017 study.9, 10
DEX
Estimates of personal health care spending and service volume were extracted from the DEX project, available at www.healthdata.org/dex. Details of the data source have been specifically described previously.9 Briefly, the study estimated U.S. health care spending and service volume annually from 1996 to 2016 and synthesized information on health care spending from 183 sources, leveraging the strength of each source to produce modeled estimates of spending and volume disaggregated by 154 health conditions, 38 age and sex groups, and 6 types of care: ambulatory, inpatient, ED, dental, retail pharmaceutical, and nursing facility care. Microdata consisted of administrative records, insurance claims, or household surveys that reported health spending by cause of illness or reason for the health care event and type of good or service, along with necessary demographic information. Specifically, the primary data sources to ascertain spending and volume on each type of care in DEX are listed in Supplementary Table 1. Several adjustments were applied to improve the accuracy of the estimates to account for comorbidities and for the difference between charge and payment data. These adjusted data tracked spending associated with each disease rather than simply spending associated with the primary diagnosis appearing in the raw data. Spending estimates were also scaled to the official estimate of U.S. health spending from the National Health Expenditure Accounts, which ensured that no spending was counted twice. Note that spending estimates were produced to reflect actual spending on health, also known as expenditure or payments, rather than charges made by medical providers. All spending estimates from the project data set were adjusted for inflation and expressed in 2016 U.S. dollars. A more detailed approach to estimating health expenditure data in the DEX is reported in the Supplementary Material.
GBD study
The age-specific prevalence of IBD was extracted from the GBD study, which estimated prevalence, incidence, deaths, and other epidemiologic metrics by age and sex groups for 354 conditions for 1990, 1995, 2000, 2005, 2010, and 2015.10 To estimate the disease incidence and prevalence for each age and sex group in the United States, a total of 1604 data sources were used, including hospital data, claims data, and surveys. In general, a patient with prevalent IBD was diagnosed if a patient had at least 1 inpatient or 2 outpatient encounters with an appropriate International Classification of Diseases code as any diagnosis. The denominator for these estimates was the national population. A Bayesian meta-regression tool developed specifically for the GBD, DisMod-MR, was used to generate the modeled estimates of prevalence and incidence. Log-linear interpolation was used to estimate prevalence and incidence rates for years where data were not directly reported; substantive short-term variations were unlikely. A more detailed approach to estimating health expenditure data in GBD is reported in the Supplementary Material.
From these data sources, we specifically abstracted data on annual health care spending on IBD (DEX) and the age-specific prevalence of IBD in the United States (GBD) between 1996 and 2016. Separate estimates for Crohn disease and ulcerative colitis were not available.
Outcomes
Our primary outcome was annual health care spending on IBD, adjusted for age-specific disease prevalence. Trends in health care spending were analyzed between 1996 and 2016, overall, by age groups: ages <20 years (children and adolescents), ages 20 to 44 years (young adults), ages 45 to 64 years (middle-aged adults), and ages ≥65 years (older adults), and by type of care: ambulatory, inpatient, ED, pharmaceutical prescriptions, and nursing care.9 Ambulatory care included preventive, curative, and rehabilitative medical and psychiatric services; procedures (including elective outpatient endoscopy); and medications administered in a physician’s office, freestanding clinic, or hospital outpatient departments. Inpatient care included all spending in an inpatient hospital facility, whether diagnostics, pharmaceuticals, or devices. ED care included all services provided at hospital-based EDs. Nursing facility care included nursing care provided in nursing homes or other residential institutions. Pharmaceutical prescriptions included all prescription medications purchased in a retail pharmacy setting and specialty drugs, excluding over-the-counter medications and therapeutic devices. We excluded spending on general administrative costs.
To account for specialty drugs such as biologics that may not be captured in national surveys like the Medical Expenditure Panel Survey, the DEX project specifically obtained a dataset of drugs from 2010 to 2018 from the pharmaceutical consulting firm IQVIA that mapped 136 specialty drugs to a primary health condition for each year to generate a specialty drug spending model specific for year, age, sex, and health condition. These data, from 2010 to 2018, were backcasted for 1996 to 2009, using a hierarchical regression model estimating total spending per specialty drug to create a complete time series of specialty drug expenditures from 1996 to 2016. Per the DEX project, these data sources likely underestimated specialty drug spending.
Posthoc, based on reviewers’ comments, we examined drivers of change in health care spending for patients with IBD. Drivers of change were available for data between 1996 and 2013. Changes in spending were categorized into 5 variables: (1) adjustment for the total U.S. population size; (2) adjustment for the proportion of the population in each age and sex group, to account for differences in population aging; (3) changes in disease prevalence and incidence; (4) changes in service utilization; and (5) changes in service price and intensity.11 Service utilization was measured by mean visits per prevalent or incident patient with IBD for ambulatory costs and mean bed-days per prevalent patient with IBD for inpatient costs. Service price and intensity were measured by the mean spending per visit.
Statistical Analysis
Trends in health care spending on IBD adjusted for disease prevalence, overall and by predefined strata, were calculated as population-standardized annualized rates of change from 1996 through 2016. The annualized rate of change was the year-over-year rate of change necessary to reflect the total change in spending observed between 1996 and 2016. To calculate the population-standardized rate of change, the population size, age, and sex structure from 2016 was multiplied by the 1996 per-person spending rates for each age group and sex category. This process estimated what spending would have been in 1996 had the 2016 population been present.
Joinpoint regression was used to assess for statistical inflection points in temporal trends, testing whether a segmented line with inflections at joinpoints was a significantly better fit for the data than a straight line. The grid search method was used, and model selection was based on the permutation test with 4499 permutations and an overall significance level of 0.05. A minimum percentage point difference of 5 between consecutive annual percentage change segments was selected a priori, and we specified that a minimum of 2 observations between joinpoints was required to avoid overfitting. We evaluated relative spending by type of care in each age group over time by averaging total and proportional spending over a 5-year period.
All analyses were performed using Stata 14.2 (StataCorp LLC, College Station, TX) and the Joinpoint Regression Program 4.0.1 (Statistical Research and Applications Branch, National Cancer Institute, Bethesda, MD; available at https://surveillance.cancer.gov/joinpoint/). Institutional review board ethics approval was not required because all data in this analysis are deidentified and publicly available.
Role of Funding Source
This study did not receive any direct funding. This article contains information available for download from the Institute for Health Metrics and Evaluation website, which has been made available through the Creative Commons Attribution-Non Commercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), and from the GBD Study 2017 Database, which has been made available under the Open Data Commons Attribution License through the Global Burden of Disease Collaborative Network website (ghdx.healthdata.org).
RESULTS
Overall Health Care Spending and Prevalence
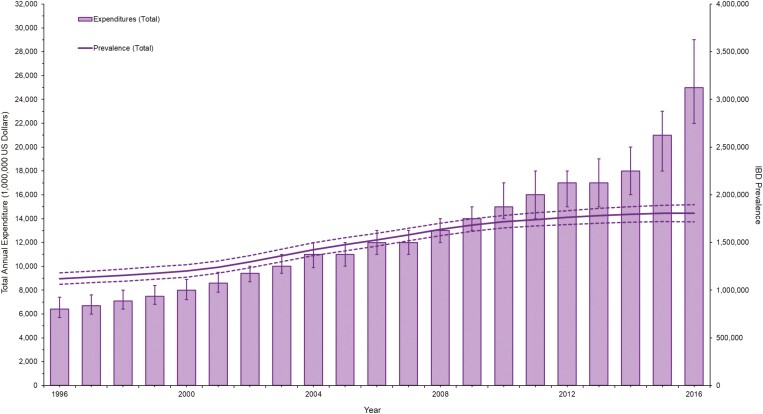
Fig. 1 shows the overall trends in health care spending, with corresponding changes in disease prevalence from 1996 to 2016. Table 1 shows population-standardized annualized rates of change in spending by type of care and age group. In 2016, estimated total health care spending in patients with IBD was $25.4 billion (95% confidence interval [CI], 22.3-28.7). Inpatient care ($10 billion [95% CI, 9.0-11.0]) and ED care ($4.6 billion [95% CI, 3.9-5.2]) accounted for the majority of spending, representing an annual 7.1% (95% CI, 6.2-7.9) increase in spending from estimated health care spending in 1996 of $6.4 billion. Corresponding to the increased health care spending, from 1996 to 2016, the total number of patients with IBD increased from 1.12 million (95% uncertainty interval [UI], 1.06-1.18) to 1.81 million (95% CI, 1.72-1.90), with a corresponding increase in estimated prevalence from 415 per 100,000 persons in 1996 (95% CI, 394-437) to 560 per 100,000 in 2016 (95% CI, 532-588). Overall, there was a disproportionate increase in annual spending per patient with IBD, increasing from $5714 to $14,033. Spending per patient increased by 3.1% (2.8-3.4) annually between 1996 and 2013, and then more rapidly by 18.6% per year (11.1-26.6) between 2014 and 2016.
Figure 1.
Trends in overall spending in patients with IBD by changes in prevalence of IBD.
Table 1.
Health Care Spending in Patients With IBD
| Age Group | Ambulatory Care | Inpatient Care | ED Care | Pharmaceuticals | ||||
|---|---|---|---|---|---|---|---|---|
| 2016 ($, in mi) | Percentage Change From 1996 | 2016 ($, in mi) | Percentage Change From 1996 | 2016 ($, in mi) | Percentage Change From 1996 | 2016 ($, in mi) | Percentage Change From 1996 | |
| <20 y | 836 | 8.1% | 494 | 2.6% | 595 | 2.2% | 20 | 2.1% |
| 20-44 y | 824 | 2.8% | 2500 | 6.0% | 1900 | 6.3% | 1100 | 7.5% |
| 45-64 y | 1600 | 6.8% | 4000 | 10.4% | 1300 | 12.7% | 1700 | 10.2% |
| ≥65 y | 706 | 3.6% | 3130 | 8.4% | 790 | 8.6% | 490 | 7.4% |
Overall and population-standardized annualized rates of change, by type of care and age, between 1996 and 2016. mi, millions.
Trends in Health Care Spending by Age and Type of Care
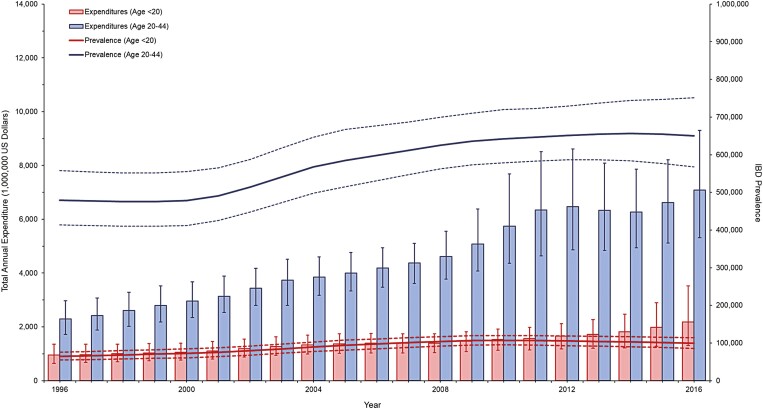
Figs. 2 and 3 show trends in health care spending in patients with IBD by age group with the corresponding change in disease prevalence from 1996 to 2016. Table 2 shows temporal trends in spending by age and by type of care. Overall, adjusting for disease prevalence, a rapid increase in health care spending was observed in middle-aged and older adults with IBD in the last decade. From 1996 to 2013, health care spending in middle-aged adults increased by 4.3% annually (95% CI, 3.7-4.8) to 18.1% annually (95% CI, 13.2-23.9) from 2013 to 2016. Similarly, from 1996 to 2014, health care spending in older adults increased by 1.1% annually (95% CI, 0.8-1.5) to 32.8% annually (95% CI, 24.0-42.2) from 2014 to 2016. In contrast, a more modest increase in spending was observed in younger adults and in adolescents.
Figure 2.
Trends in overall spending in patients with IBD ages < 20 years and ages 20-44 years with corresponding change in prevalence of IBD.
Figure 3.
Trends in overall spending in patients with IBD ages 45-64 years and ages ≥65 years with corresponding change in prevalence of IBD.
Table 2.
Temporal Trends in Health Care Spending in Patients With IBD,
| Category | APC Slope 1 (95% CI) | APC Slope 2 (95% CI) | Δ Slope 2-1 P | APC Slope 3 (95% CI) | Δ Slope 3-2 P | APC Slope 4 (95% CI) | Δ Slope 4-3 P |
|---|---|---|---|---|---|---|---|
| By age groups | |||||||
| < 20 y | –0.48 (–0.88 to –0.09; 1996-2010) | 5.87 (2.15-9.72; 2010-2014) | 0.003 | 11.50 (4.64-18.82; 2014-2016) | 0.15 | — | — |
| 20-44 y | 3.10 (2.15-4.06; 1996-2008) | 8.19 (–4.07 to 22.01; 2008-2011) | 0.40 | 1.71 (–0.71 to 4.19; (2011-2016) | 0.30 | — | — |
| 45-64 y | 4.26 (3.74-4.78; 1996-2013) | 18.11 (13.23-23.19; 2013-2016) | <0.0001 | — | — | — | — |
| ≥ 65 y | 1.11 (0.76-1.45; 1996-2014) | 32.78 (24.01-42.17; 2014-2016) | <0.0001 | — | — | — | — |
| By type of care | |||||||
| Ambulatory | 3.37 (1.85-4.92; 1996-2002) | –2.10 (–4.46 to 0.31; 2002-2007) | 0.001 | 5.54 (4.93-6.16; 2007-2016) | <0.0001 | — | — |
| Inpatient | 1.66 (1.29-2.03; 1996-2014) | 39.15 (29.60-49.41; 2014-2016) | <0.0001 | — | — | — | — |
| Emergency | 2.63 (2.34-2.93; 1996-2013) | 13.20 (10.02-16.46; 2013-2016) | <0.0001 | — | — | — | — |
| Prescriptions | 13.53 (7.71-19.66; 1996-1999) | 4.83 (3.97-5.70; 1999-2008) | 0.008 | 16.25 (10.09-22.75; 2008-2011) | 0.002 | –1.60 (–2.66 to –0.53; 2011-2016) | <0.0001 |
| Nursing Care | –0.51 (–4.15 to 3.27; 1996-1998) | –6.01 (–7.15 to –4.86; 1998-2003) | 0.009 | 2.05 (1.72-2.37; 2003-2013) | <0.0001 | 12.48 (10.92-14.05; 2013-2016) | <0.0001 |
Spending by age and type of care between 1996 and 2016 (per 1000-patient prevalence). Minimum percentage points difference 5% between consecutive APC segments.
APC indicates annual percentage change.
Overall, spending on ambulatory care, inpatient care, ED care, pharmaceutical prescriptions, and nursing care increased by 5.2%, 7.8%, 6.8%, 8.6%, and 3.7% annually, respectively, albeit with substantial variability over time. In evaluating trends, over the last decade, we observed a substantial increase in health care spending in patients with IBD in inpatient and ED care, with a more modest increase in spending on ambulatory care. In contrast, pharmaceutical spending increased progressively in the 2000s but then settled to a steady level between 2011 and 2016. With the rising prevalence of IBD in older adults, a progressive increase in spending on nursing care was observed in the last decade.
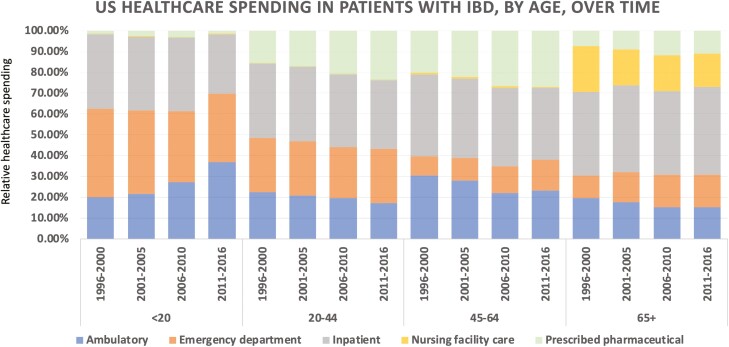
Supplementary Fig. 1 shows relative patterns of spending by type of care. Over the 2 decades of the study, relative spending on inpatient care decreased modestly from 37.7% of total health care costs in 1996 to 2000 to 35.1% in 2011 to 2016, without substantial changes in spending on ED care (1996-2000, 20.4% to 2011-2016, 20.7%); in contrast, relative spending on pharmaceuticals increased from 12.8% (1996-2000) to 19.9% (2011-2016).
Patterns of Health Care Spending by Age
Fig. 4 shows trends in patterns of health care spending by age group. In younger adults and middle-aged adults, a relative decrease in spending on inpatient care (younger adults: 1996-2000, 35.6% vs 2011-2016, 32.9%; middle-aged adults: 1996-2000, 39.4% vs 2011-2016, 34.6%) was accompanied by an increase in pharmaceutical spending (younger adults: 1996-2000, 15.7% vs 2011-2016, 23.6%; middle-aged adults: 1996-2000, 20.4% vs 2011-2016, 26.9%). In middle-aged adults, spending on ED care increased from 9.0% (1996-2000) to 14.9% (2011-2016), with an accompanying decrease in relative spending on ambulatory care (1996-2000, 30.7% vs 2011-2016, 23.2%). In contrast, in older adults, spending on inpatient care (1996-2000, 40.2% vs 2011-2016, 42.1%) and ED care (1996-2000, 11.0% vs 2011-2016, 15.5%) remained stable to slightly increased, and spending on pharmaceuticals only increased modestly (1996-2000, 7.2% vs 2011-2016, 11.2%).
Figure 4.
Patterns of health care spending in patients with IBD by age and over time.
Drivers of Change in Health Care Spending
From 1996 to 2013 for patients with IBD, the predominant driver of cost was an increase in the price and intensity of inpatient care, representing a total change of $1.49 billion (95% CI, $1.07 billion-$1.93 billion] and an annual percentage change of 8.20% (95% CI, 5.60%-11.50%). Data specifically for surgical vs medical admissions are not available.
DISCUSSION
Studies have shown that IBD is one of the top 5 most expensive gastrointestinal conditions, with annual costs in the United States exceeding $25 billion.7, 9 In a comprehensive analysis using 2 large publicly available databases used to generate national estimates of disease burden and spending, we estimated trends and patterns in health care spending in patients with IBD in the United States from 1996 to 2016, adjusting for disease prevalence, and made several key observations. First, annual health care spending in patients with IBD increased from $6.4 billion in 1996 to $25.4 billion in 2016, increasing by 7.1% per year, corresponding to an increase in annual spending per patient with IBD from $5714 to $14,033, after adjusting for disease prevalence and inflation. Second, despite an increase in spending on pharmaceuticals from 12.8% to 19.9% of total spending, inpatient and ED care still accounted for 56% of total health care spending in patients with IBD. The predominant driver of cost was an increase in the price and intensity of inpatient care. Third, patterns of health care spending vary significantly by age groups over time. Middle-aged and older adults with IBD saw the most rapid increases in health care spending in the last decade of the study. However, although spending on inpatient care decreased accompanied by an increase in pharmaceutical spending in middle-aged adults, relatively modest changes have been observed in patterns of health care spending in older adults, in whom disease prevalence is rising progressively. Taken together, our findings confirm IBD as an expensive and financially volatile condition with high ongoing spending on unplanned health care utilization, despite rising spending on pharmaceuticals. These findings call for prioritizing proactive population health management strategies to decrease unplanned health care utilization while simultaneously optimizing the rational and appropriate use of biologic agents.12
Prior studies have shown an increase in rates of unplanned health care utilization in patients with IBD, with an increase in IBD-related hospitalization and ED visits and a plateauing of outpatient visits.6 We observed similar patterns in health care spending over the 2 decades of this study with a disproportionate increase in spending on inpatient and ED care, without an increase in ambulatory care. These findings are of concern because the fundamental types of care delivered in ambulatory and hospital-based settings are different. Whereas ED and inpatient treatment focus on managing acute disease flares or disease-related complications, ambulatory care offers opportunities to proactively optimize disease and treatment monitoring that favor influence long-term outcomes. From a health systems perspective, accessing hospital-based services is also significantly costlier than ambulatory visits.13-15
The relative spending on pharmaceuticals increased over the 2 decades of this study, accounting for ~20% of total spending in patients with IBD, particularly in younger adults and middle-aged adults with IBD. Although we are unable to directly attribute costs to biologic therapy, it is likely that the relative increase in pharmaceutical health care spending is attributed to biologics. Prior studies using the pharmaceutical consulting firm IQVIA have suggested that specialty drugs may contribute to 43% of net pharmaceutical spending across all health conditions despite only being 2% of the volume in 2016.16 In a claims-based analysis, Yu and colleagues17 observed that the proportion of patients with IBD using biologics increased from 7.1% in 2007 to 20.5% in 2015. Note that our estimates of pharmaceutical spending on biologics may be conservative and are likely underestimated, as noted as a limitation in the original DEX project.9 Our findings are in contrast to a prior U.S. health claims–based study of 5000 patients with Crohn disease in which pharmacy utilization accounted for 45% of the total insurance-paid costs whereas inpatient costs accounted for only 23% of the costs.18 However, this study was not representative of the entire U.S. population and was limited to costs paid by commercial insurance, failing to account for patient-responsible copayments, deductibles, and coinsurance amounts paid by the members, along with the costs covered by public insurance.
Studies outside of the United States have suggested that in patients with IBD, there has been a gradual shift in total spending toward pharmaceuticals with biologics. In Canada, prescription drugs account for 42% of total direct costs in IBD patients, and there has been a decline in surgery and hospitalizations over the last 2 decades.3, 19, 20 In a European, prospective, population-based inception cohort of patients with IBD, medical therapies and surgeries accounted for 36% and 26% of total health care expenditures, respectively, in the first year after diagnosis, whereas biologic therapy and standard medical care accounted for 14% and 22% of total health care costs, respectively.21 In contrast, in a large Dutch cohort, hospitalization accounted for 20% to 23% and biologic therapy accounted for 31% to 64% of total health care costs in patients with IBD.5
These differences in relative spending on hospitalization and pharmaceutical therapy in the United States vs Western countries outside the United States may be related to differences in approaches to management and/or health care access and affordability. Most Western countries outside the United States have varying degrees of socialized medicine, where health care is deeply discounted, accessible, and affordable. Access to biologics may be more restrictive but is significantly discounted in socialized health care systems, as compared to the United States. As a result, patients with IBD in the United States frequently experience financial toxicity, with 1 in 4 patients reporting financial hardship because of medical bills, 1 in 6 reporting cost-related medication non-adherence, and two-thirds of patients reporting personal and/or health-related financial distress.22 These financial difficulties are not just limited to those without insurance, but they are not infrequent in those with private insurance, highlighting the problems of underinsurance.
We also confirmed a progressive increase in prevalence and a disproportionately rapid increase in health care spending in older adults with IBD. These findings are of particularly concern given trends suggesting increased spending on ED visits and hospitalization in these patients, with only a modest increase in spending on pharmaceuticals. There is rather limited evidence-based guidance on the management of older patients with IBD, who are at higher risk of treatment-related complications, and whose goals and targets of therapy may be different than those of younger adults.23 With older adults poised to form a significant proportion of patients with IBD over the next decade, the standardization of medical management with accurate risk stratification is warranted to mitigate disease-related health care costs in these older patients with IBD.24
Our study has several strengths. First, we used 2 comprehensive data sources designed to study the burden and health care spending of different diseases nationally, and hence the work is representative. Both the DEX project and the GBD are used nationally and globally and are routinely used to inform U.S. health policy and legislation. Second, by combining the assessment of health care spending with trends in disease prevalence, we were able to accurately assess trends in per capita spending.
With our approach, there are also inherent limitations. First, our findings may not accurately represent direct IBD-specific health care costs but may more broadly represent health care spending in patients with IBD. Whereas the former helps one to understand the direct impact of IBD, the latter is a more patient-centered approach. Second, the data used in the DEX project are imperfect. For example, the Medical Expenditure Panel Survey and other data sources exclude active military personnel, incarcerated individuals, and homeless individuals, and spending data on specialty drugs may be underestimated. However, overall, the DEX estimates represent the most comprehensive evaluation of health care spending in the United States and provide the best approximations of national health care spending, which is directly relevant to policy makers, patients and providers, and health care administrators. Third, it is difficult to infer causality based on trends in health care spending by age groups and type of care. Moreover, we did not have data on spending by IBD-specific factors such as phenotype (Crohn disease or ulcerative colitis) and behavior, along with demographic factors such as geographical region, race, or income.
CONCLUSIONS
In summary, using 2 large databases, we observed that health care spending in patients with IBD increased from $6.4 billion in 1996 to $25.4 billion in 2016, increasing by 7.1% annually, with per capita prevalence-adjusted annual health care spending increasing from $5714 to $14,033. Older and middle-aged adults saw the most rapid increases in spending over the last decade of the study. Despite an increase in pharmaceutical spending from 12.8% to 19.9% in 2020, inpatient and ED care still account for 56% of health care spending in patients with IBD. There is an urgent need to implement high-value population health management strategies in patients with IBD to achieve the triple aim of improving quality of care and population health outcomes while reducing health care costs.
Supplementary Material
Acknowledgments
We thank Joseph Dieleman, PhD, Associate Professor of Medicine, Institute for Health Metrics and Evaluation, Department of Health Metric Sciences, University of Washington, Seattle, who led the DEX project, for guiding us on the interpretation of the original study.
Supported by: Dr. Nguyen is supported by the National Institutes of Health (NIH)/National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK; T32DK007202) and the National Institutes of Health/National Library of Medicine (T15LM011271). Dr. Sandborn is partially supported by the NIDDK-funded San Diego Digestive Diseases Research Center (P30 DK120515). Dr. Singh is supported by NIH/NIDDK (K23DK117058), the International Organization for the Study of Inflammatory Bowel Diseases Operating Grant 2019, and the American College of Gastroenterology Junior Faculty Development Award (#144271).
Conflicts of interest: Dr. Singh has received research grants from AbbVie and Janssen. Dr. Jairath has received consulting fees from AbbVie, Eli Lilly, GlaxoSmithKline, Arena Pharmaceuticals, Genentech, Pendopharm, Sandoz, Merck, Takeda, Janssen, Robarts Clinical Trials, Topivert, and Celltrion and speaker’s fees from Takeda, Janssen, Shire, Ferring, Abbvie, and Pfizer. Dr. Sandborn has received research grants from Atlantic Healthcare Limited, Amgen, Genentech, Gilead Sciences, AbbVie, Janssen, Takeda, Lilly, Celgene/Receptos, Pfizer, Prometheus Laboratories (now Prometheus Biosciences); consulting fees from AbbVie, Allergan, Amgen, Arena Pharmaceuticals, Avexegen Therapeutics, BeiGene, Boehringer Ingelheim, Celgene, Celltrion, Conatus, Cosmo, Escalier Biosciences, Ferring, Forbion, Genentech, Gilead Sciences, Gossamer Bio, Incyte, Janssen, Kyowa Kirin Pharmaceutical Research, Landos Biopharma, Lilly, Oppilan Pharma, Otsuka, Pfizer, Progenity, Prometheus Biosciences, Reistone, Ritter Pharmaceuticals, Robarts Clinical Trials, Series Therapeutics, Shire, Sienna Biopharmaceuticals, Sigmoid Biotechnologies, Sterna Biologicals, Sublimity Therapeutics, Takeda, Theravance Biopharma, Tigenix, Tillotts Pharma, UCB Pharma, Ventyx Biosciences, Vimalan Biosciences, and Vivelix Pharmaceuticals; and stock or stock options from BeiGene, Escalier Biosciences, Gossamer Bio, Oppilan Pharma, Prometheus Biosciences, Progenity, Ritter Pharmaceuticals, Ventyx Biosciences, and Vimalan Biosciences. His spouse reports consulting work for Opthotech and Progenity; stock options from Progenity, Oppilan Pharma, Escalier Biosciences, Prometheus Biosciences, Ventyx Biosciences, and Vimalan Biosciences; and work as an employee for Oppilan Pharma, Escalier Biosciences, Prometheus Biosciences, Ventyx Biosciences, and Vimalan Biosciences. Dr. Ma reports consulting fees from AbbVie, AVIR Pharma Inc, Janssen, Takeda, Pfizer, Roche, and Alimentiv; speaker’s fees from AbbVie, Janssen, Takeda, and Pfizer; and research grants from Pfizer.
Author contributions: Study concept and design: SS, CM. Acquisition of data: ASQ, NHN, SH. Analysis and interpretation of data: ASQ, NHN, JL, CM, SS. Drafting of the manuscript: SS. Critical revision of the manuscript for important intellectual content: ASQ, NHN, SH, JL, VJ, WJS, CM. Approval of the final manuscript: All authors. Guarantor of article: SS.
References
- 1. GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 2020;5:17–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dahlhamer JM, Zammitti EP, Ward BW, et al. Prevalence of inflammatory bowel disease among adults aged ≥18 years—United States, 2015. MMWR Morb Mortal Wkly Rep 2016;65:1166–1169. [DOI] [PubMed] [Google Scholar]
- 3. Ma C, Moran GW, Benchimol EI, et al. Surgical rates for Crohn’s disease are decreasing: a population-based time trend analysis and validation study. Am J Gastroenterol. 2017;112:1840–1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Targownik LE, Kaplan GG, Witt J, et al. Longitudinal trends in the direct costs and health care utilization ascribable to inflammatory bowel disease in the biologic era: results from a Canadian population-based analysis. Am J Gastroenterol. 2020;115:128–137. [DOI] [PubMed] [Google Scholar]
- 5. van der Valk ME, Mangen MJ, Leenders M, et al. ; COIN study group and the Dutch Initiative on Crohn and Colitis . Healthcare costs of inflammatory bowel disease have shifted from hospitalisation and surgery towards anti-TNFα therapy: results from the COIN study. Gut. 2014;63:72–79. [DOI] [PubMed] [Google Scholar]
- 6. Ma C, Smith M, Guizzetti L, et al. Assessing national trends and disparities in ambulatory, emergency department, and inpatient visits for inflammatory bowel disease in the United States (2005–2016). Clin Gastroenterol Hepatol. 2020;18:2500–2509.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology. 2019;156:254–272.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Park KT, Ehrlich OG, Allen JI, et al. The cost of inflammatory bowel disease: an initiative from the Crohn’s & Colitis Foundation. Inflamm Bowel Dis. 2020;26:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996-2016. JAMA. 2020;323:863–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.GBD 2017 Disease and Injury Incidence and Prevalence Collabborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dieleman JL, Squires E, Bui AL, et al. Factors associated with increases in US health care spending, 1996-2013. Jama. 2017;318:1668–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dulai PS, Singh S, Ohno-Machado L, et al. Population health management for inflammatory bowel disease. Gastroenterology. 2018;154:37–45. [DOI] [PubMed] [Google Scholar]
- 13. Cross RK, Langenberg P, Regueiro M, et al. A randomized controlled trial of telemedicine for patients with inflammatory bowel disease (TELE-IBD). Am J Gastroenterol. 2019;114:472–482. [DOI] [PubMed] [Google Scholar]
- 14. de Jong MJ, Boonen A, van der Meulen-de Jong AE, et al. Cost-effectiveness of telemedicine-directed specialized vs standard care for patients with inflammatory bowel diseases in a randomized trial. Clin Gastroenterol Hepatol. 2020;18:1744–1752. [DOI] [PubMed] [Google Scholar]
- 15. George LA, Dominic MR, Cross RK. Integration of telemedicine into clinical practice for inflammatory bowel disease. Curr Opin Gastroenterol. 2020;36:304–309. [DOI] [PubMed] [Google Scholar]
- 16. IQVIA. Understand the drivers of drug expenditure in the US. September 12, 2017. https://www.iqvia.com/insights/the-iqvia-institute/reports/understanding-the-drivers-of-drug-expenditure-in-the-us. Accessed March 16, 2021. [Google Scholar]
- 17. Yu H, MacIsaac D, Wong JJ, et al. Market share and costs of biologic therapies for inflammatory bowel disease in the USA. Aliment Pharmacol Ther. 2018;47:364–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Park KT, Colletti RB, Rubin DT, et al. Health insurance paid costs and drivers of costs for patients with Crohn’s disease in the United States. Am J Gastroenterol. 2016;111:15–23. [DOI] [PubMed] [Google Scholar]
- 19. Kuenzig ME, Benchimol EI, Lee L, et al. The impact of inflammatory bowel disease in Canada 2018: direct costs and health services utilization. J Can Assoc Gastroenterol. 2019;2:S17–S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rahman A, Jairath V, Feagan BG, et al. Declining hospitalisation and surgical intervention rates in patients with Crohn’s disease: a population-based cohort. Aliment Pharmacol Ther. 2019;50:1086–1093. [DOI] [PubMed] [Google Scholar]
- 21. Odes S, Vardi H, Friger M, et al. Clinical and economic outcomes in a population-based European cohort of 948 ulcerative colitis and Crohn’s disease patients by Markov analysis. Aliment Pharmacol Ther. 2010;31:735–744. [DOI] [PubMed] [Google Scholar]
- 22. Nguyen NH, Khera R, Dulai PS, et al. National estimates of financial hardship from medical bills and cost-related medication nonadherence in patients with inflammatory bowel diseases in the United States. Inflamm Bowel Dis. 2021;27:1068–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Singh S, Picardo S, Seow CH. Management of inflammatory bowel diseases in special populations: obese, old, or obstetric. Clin Gastroenterol Hepatol. 2020;18:1367–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Coward S, Clement F, Benchimol EI, et al. Past and future burden of inflammatory bowel diseases based on modeling of population-based data. Gastroenterology. 2019;156:1345–1353.e4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.