Abstract
Distal radioulnar joint (DRUJ) instability and triangular fibrocartilage complex (TFCC) tears are more usual than estimated and are frequently overlooked. Diagnosis is often clinical, which can be confirmed using computed tomography (CT) scan and magnetic resonance imaging (MRI). In doubtful cases, bilateral computed tomography in neutral forearm rotation, supination, and pronation should also be performed. Wrist arthroscopy can be diagnostic and therapeutic for ulnar-sided wrist pain. Two systematic reviews showed equivalent outcomes between open and arthroscopic repair of the TFCC. There is scant proof to advise one technique over the other in clinical practice. TFCC repair and reconstruction are contraindicated when there is a bony deformation of the radius or ulna or osteoarthritis of the DRUJ. With the advancement of implant arthroplasty, salvage procedures are less desirable. Constrained distal radioulnar arthroplasty is stable, and the longevity is encouraging.
Key Words: Distal radioulnar joint, Instability, Triangular fibrocartilage complex, Treatment
Introduction
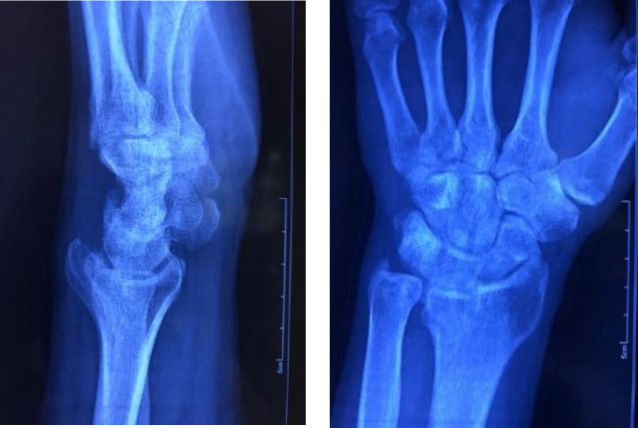
Instability of the distal radioulnar joint (DRUJ) can be dorsal, volar, or multidirectional (1). Acute dislocations of the DRUJ usually happen together with a fracture to the distal radius, radial metadiaphysis, or radial head (2) [Figure 1].
Figure 1.
DRUJ is subluxated following a displaced distal radius fracture
Other conditions may be present concomitantly, including triangular fibrocartilage complex (TFCC) tears, ulnocarpal abutment, lunotriquetral ligament tears, and extensor carpi ulnaris (ECU) tendinitis.
If instability is not appropriately addressed, it alters the kinematics of the wrist and forearm, producing pain, weakness, and potentially degenerative osteoarthritis. Instability of the DRUJ is considered when there is increased ulnar translation relative to the radius than the contralateral wrist (1, 3). The objective of this article is to carry out a current concept review on DRUJ instability.
Anatomy
To properly treat chronic instability of the DRUJ, several important anatomical features must be well understood. The sigmoid notch radius of curvature is much bigger than the ulnar head, resulting in inherent laxity and little bony constraint (4,5). Besides, there are only a few millimeters consistent with about 10% of articular surface contact (4). Tolat et al. reported several types of sigmoid notch according to its morphology comprising of flat (42%), type C (30%), ski slope (14%), and type S (14%) (6). There is also a fibrocartilaginous labrum that increases the bony edges to enlarge the sigmoid notch's depth. The joint's geometry provides approximately 20 per cent of the DRUJ stability, while the enclosing soft tissues account for the remaining 80% (7,8). According to Stuart et al a number anatomical structures fix the DRUJ, of which the TFCC and specifically its foveal insertion is the most significant (8). The joint's stability is more dependent on the ligamentous structures in a damaged sigmoid notch, in which case, a concurrent osseous procedure might be necessary (1). The TFCC transmits 16% of the axial load via the TFCC between the carpal bones and forearm (4) [Figure 2].
Figure 2.

ECU subsheath (left) and a part of the ulnocarpal ligaments (upper) are exposed during an open TFCC refixation procedure
Additional load is exerted to the ulnocarpal area with ulnar deviation. It happens with forearm pronation leading to a prominent ulnar head (9). Like the knee meniscus, the central disc is avascular, but the peripheral insertions to the fovea and radius are vascularized (10). A positive ulnar variance leads to the additional load to the ulnocarpal joint, which is considered a cause of failure following ligament repair and reconstructive (1).
DRUJ stabilizers can be either dynamic or static. Dynamic stability is given by the ECU tendon and pronator quadratus, while static stability is given by the distal interosseous membrane (DIOM) and the ECU subsheath (11). The DIOM comprises a thick band called distal oblique ligament (DOL), which runs diagonally from the ulnar dipahysis to the distal radius (12). The DOL's existence maintains the DRUJ stability when the TFCC is torn (12,13) [Figure 3]. The DOL should be preserved during Darrach distal ulnar resection to maintain ulnar stump stability. Cutting the radioulnar ligaments and maintaining the surplus soft tissue constraints has shown continued near normal kinematics, highlighting the importance of the adjacent structures (14).
Figure 3.
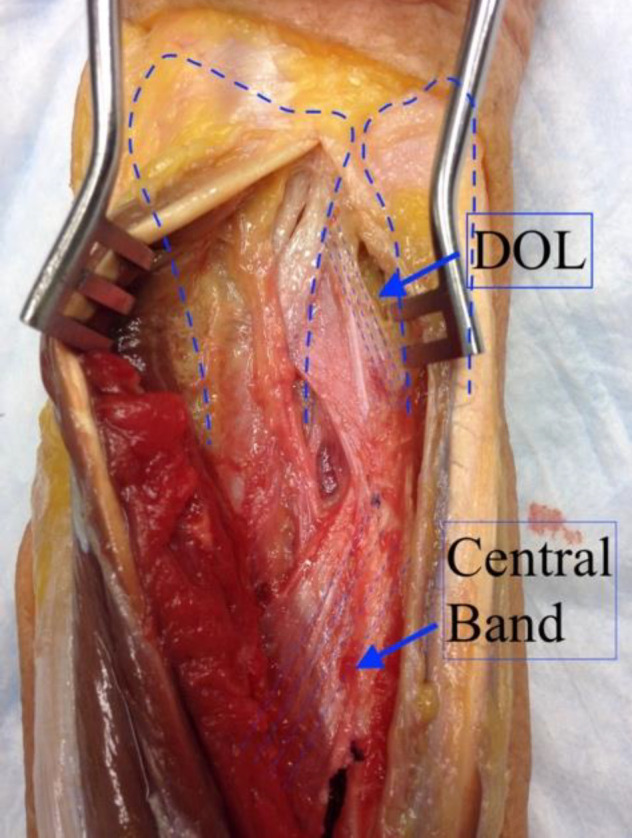
It shows the anatomy of the interosseous ligament and the distal oblique ligament, which plays a role in distal radioulnar stability and has to be avoided during the Darrach procedure
Although many structures contribute to the stability of the
DRUJ, the volar and dorsal radioulnar ligaments comprise the margins of the TFCC and are of utmost importance (15). Every radioulnar ligament has a superficial and a profound part. The profound fibers (ligamentum subcruentum) affix to the fovea, through which the axle of motion of the forearm passes. In contrast to the deep fibers, the superficial fibers follow a more straight route to the tip of the ulnar styloid. The deep dorsal and superficial volar fibers become tight and resist the ulna's dorsal subluxation in maximum supination, while the deep volar and superficial dorsal fibers come to be tight in pronation. At the ends of pronation and supination, superficial radioulnar fibers are less efficacious than profound fibers (16). The design and surgical precision of a ligament reconstruction must always consider the fovea's anatomical and mechanical importance (1).
Causes of instability
Instability may be secondary to generalized ligament laxity or from inflammatory arthritis. Laxity due to hypermobility or flat sigmoid notch has to be considered as they increase the chance of ligament reconstruction failure (17).
The most common cause of acquired instability is a failure to treat an injury. A typical presentation is a wrist sprain with a fast and forceful rotation of the car wheel during driving. Sole TFCC tears produced by a rotational force or a fall on the outstretched hand are usually at first considered as uncomplicated wrist sprains (1). We are not sure what is an adequate treatment to prevent instability in these circumstances. However, wrist immobilization is conventionally suggested. A recent clinical trial showed that ulnar styloid fracture fixation concomitant with extra-articular distal radius fractures (Fernandez type I) resulted in a more unsatisfactory outcome than not fixing the styloid (18). Although the two fixed and unfixed groups were comparable in almost all
outcome variables at three and six months, the DASH (Disabilities of the Arm, Shoulder and Hand) score was higher in the fixed group showing less acceptable result after fixation of the styloid.
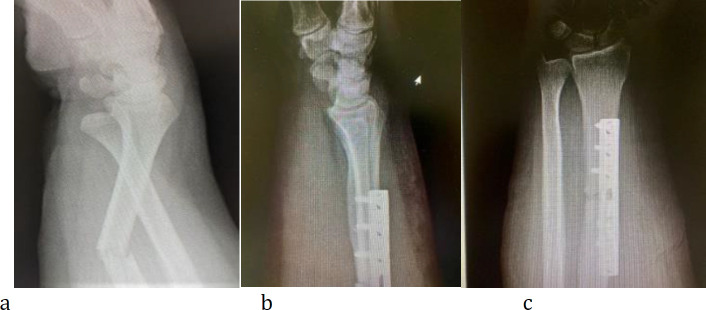
Fractures of the lunate facet, both dorsal and volar, are able to produce sigmoid notch incongruence (19,20). Reduction of the dorsal lunate fragment is more challenging and is more prone to subsequent DRUJ instability [Figure 4]. It can be reduced using bone reduction forceps (21) [Figure 5].
Distal radius malunion can significantly alter the alignment of the sigmoid notch, causing subluxation and instability of the DRUJ (22-24). The radial translation reduces the interosseous membrane's stabilizing effect and impedes the healing of the radioulnar ligaments to the fovea (19,25,26). Fractures of the distal third of the radial diaphysis with injury to the DRUJ or so-called Galeazzi may cause instability if the radial alignment and length are not restored (27) [Figure 6]. An extensive interosseous ligament tear in an acute longitudinal radioulnar dissociation (ALRUD) or so-called an Essex-Lopresti lesion, also causes instability (1).
Clinical examination
Instability of the DRUJ is not an easy diagnosis. There is usually a history of trauma, including a fall on an outstretched hand or twisting of the wrist. Patients often present with ulnar-sided pain, especially with forearm rotation, which might be due to subtle instability. With more serious instability, a clunk is felt with forearm rotation showing a positional dislocation-relocation of the ulnar head (1).
Resisted pronation and supination are usually painful, which can be present with TFCC tears. When in doubt, the contralateral side has to be compared for laxity.
Piano key sign: The ulnar head sits in a dorsal position. Like pressing a piano key, applying stress to the ulnar head causes substantial translation to volar (28,29). This test has 66% sensitivity and 68% specificity (29).
Grind test: during this test, we try to replicate the painful situation. The examiner holds the distal forearm still with one hand, holds the wrist with another hand and starts pro-supination of the wrist in ulnar deviation relative to the forearm. This test causes grinding of the carpus over the TFCC by ulnar deviation and pro-supination motion similar to the grind test for the knee meniscus.
Fovea sign: The point tenderness over the fovea is situated between the styloid process and flexor carpi ulnaris (FCU) tendon (30). This area may be innately tender, and it is necessary to compare this sensitivity with that of the contralateral healthy wrist (1).
DRUJ stress test or ballottement test: The radiocarpal joint is stabilized with one hand while the ulna is shucked with another hand against the radius. The test is positive if it is aching and severely unstable in symptomatic individuals. The test has a specificity of 96% but solely a sensitivity of 59% (31). Considering that there is naturally more laxity with the forearm in neutral rotation, the test's exactness can be ameliorated by repeating in pronation and supination (32).
Press test: The individual is asked to push up against the armrest to stand up from a seated position on an armed chair. A TFCC tear or instability causes ulnar-sided pain (33). The press test showed 100% sensitivity for the diagnosis of TFCC injuries (29,32). We can also ask the patient to remain seated on the examination table and apply downward force to the table to simulate a push-up. This maneuver causes ulnar head depression and pain in a symptomatic patient (34,35). In 2019 Nilsson et al reported a new method to evaluate distal radioulnar joint stability utilizing augmenting circulatory force (36).
Imaging
Although the confirmation of DRUJ instability is usually made by clinical examination, imaging tests must always confirm it. A radioulnar distance > 6 mm is suggestive of instability (29,37).
The dorsal tangential view is independent of variation in forearm rotation (38). Radiographs are also used to identify other lesions, such as malunion of the distal radius, pseudoarthrosis of the ulnar styloid , ulnocarpal impaction, and osteoarthritis (1).
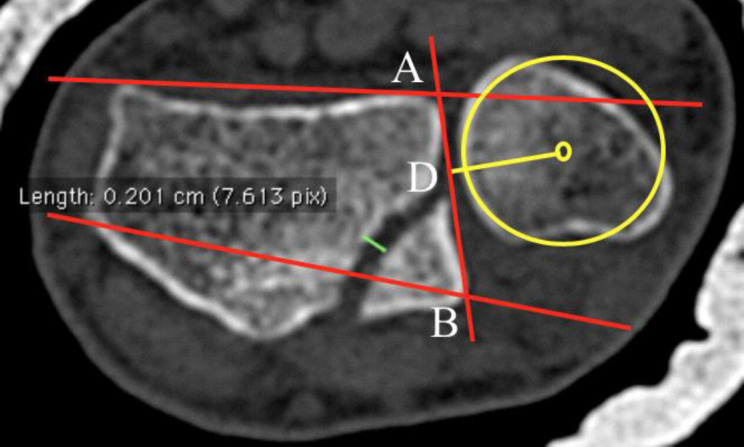
Computed tomography (CT) scanning often gives information regarding the sigmoid notch anatomy, alignment, and positioning of the ulnar head within the sigmoid notch, especially when comparing the joint on the injured side with the healthy side in multiple positions (neutral, full supination, full pronation) (39) [Figure 7].
Figure 7.
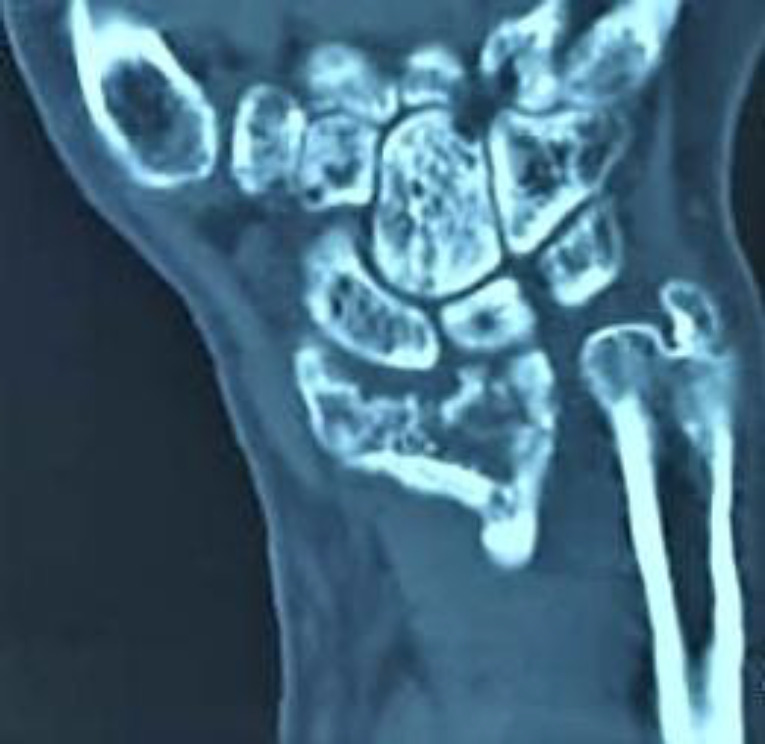
Coronal view of the wrist CT scan shows distal radius fracture with instability and incongruence in the sigmoid notch
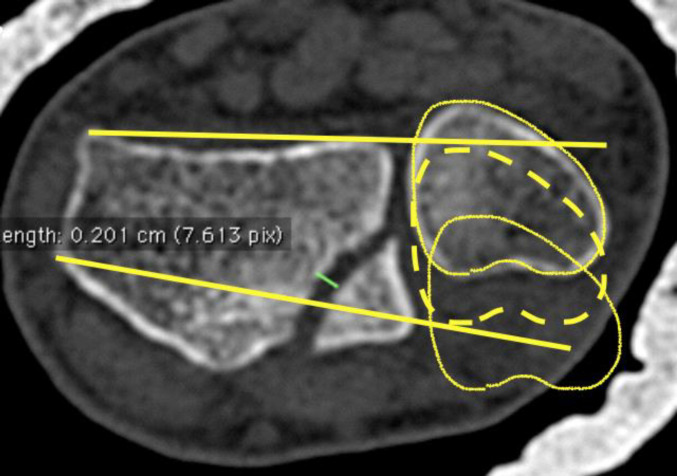
Methods to assess the DRUJ instability on a CT image are as follows (40).
Mino technique: we draw two lines, with the first through the dorsal ulnar and radial borders of the radius. The other line passes through the volar ulnar and radial borders of the radius (41) [Figure 8]. Instability exists if more than 25% of the head falls out volar or dorsal of the two lines.
Figure 8.
In the Mino technique, we draw two lines, with the first through the dorsal ulnar and radial borders of the radius. The other line passes through the volar ulnar and radial borders of the radius
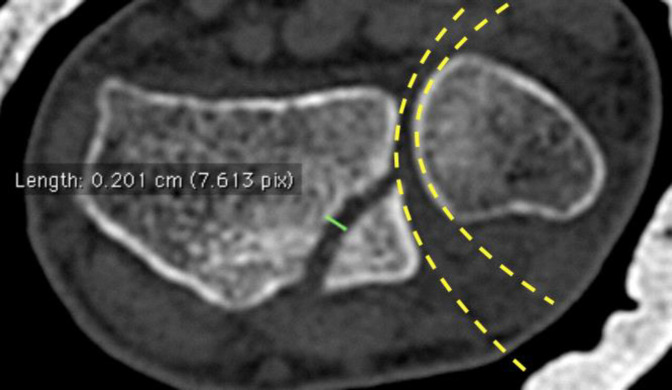
Congruency method: we assess the arc of the ulnar head in relation to the arc of the sigmoid notch (42) [Figure 9].
Figure 9.
In the congruency method, we assess the arc of the ulnar head relative to the arch of the sigmoid notch
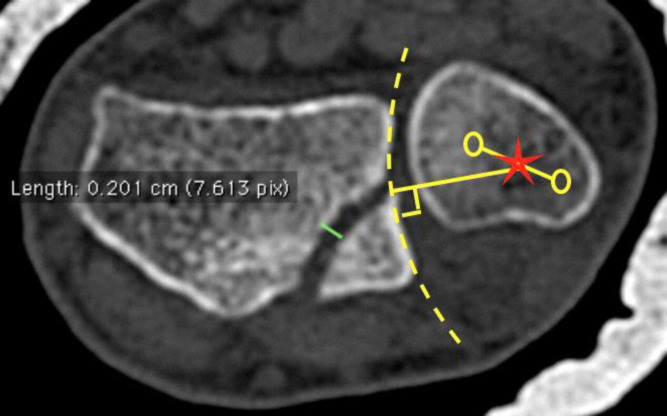
Epicenter method: we draw a line from the center of the ulnar head to the center of the ulnar styloid to determine the center of rotation of the DRUJ. We then draw a line perpendicular to the chord of the sigmoid notch to the center of the rotation of the DRUJ. The DRUJ is contemplated normal if this line falls in the middle half of the sigmoid notch (42) [Figure 10].
Figure 10.
In the epicenter method, we draw a line from the center of the head to the ulnar styloid center to determine the center of rotation of the DRUJ. We then draw a line perpendicular to the chord of the sigmoid notch to the center of the rotation of the DRUJ. The DRUJ is considered normal if this line falls in the middle half of the sigmoid notch
Ratio method: we use concentric circles to find the center of the ulnar head. A line is drawn from the volar to the dorsal edge of the sigmoid notch. A perpendicular line to this line is drawn toward the ulnar head center. The ratio is then measured. The typical ratio is equal to (43) [Figure 11].
Figure 11.
In the ratio method, we use the concentric circles to find the ulnar head center. A line is drawn from the volar to the dorsal edge of the sigmoid notch. A perpendicular line to this line is drawn toward the ulnar head center. The ratio is then measured. The typical ratio is equal to
The Mino and congruency methods yield elevated false-positive rates (44,45). Since the epicenter method considers physiological translation, it is the most specific and the most widely used (44,45). However, the combination of the epicenter method with contralateral comparative relation diminishes overestimation of stability (46).
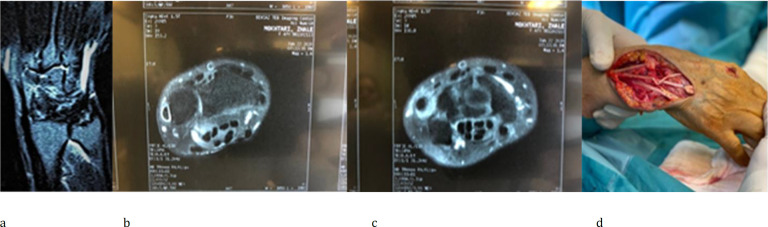
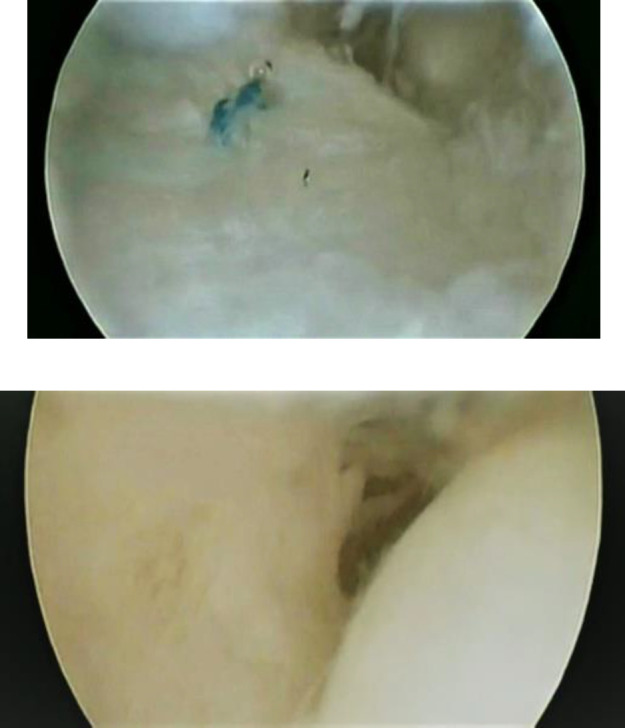
High-resolution 3 Tesla MRI is appropriate for assessing soft tissue lesions; nevertheless, its sensitivity and specificity vary (16) [Figure 12].
Figure 12.
MRI coronal and axial views show ECU tendinitis in distal radioulnar joint instability by caput ulnar syndrome (a, b, c), and intra-op (d)
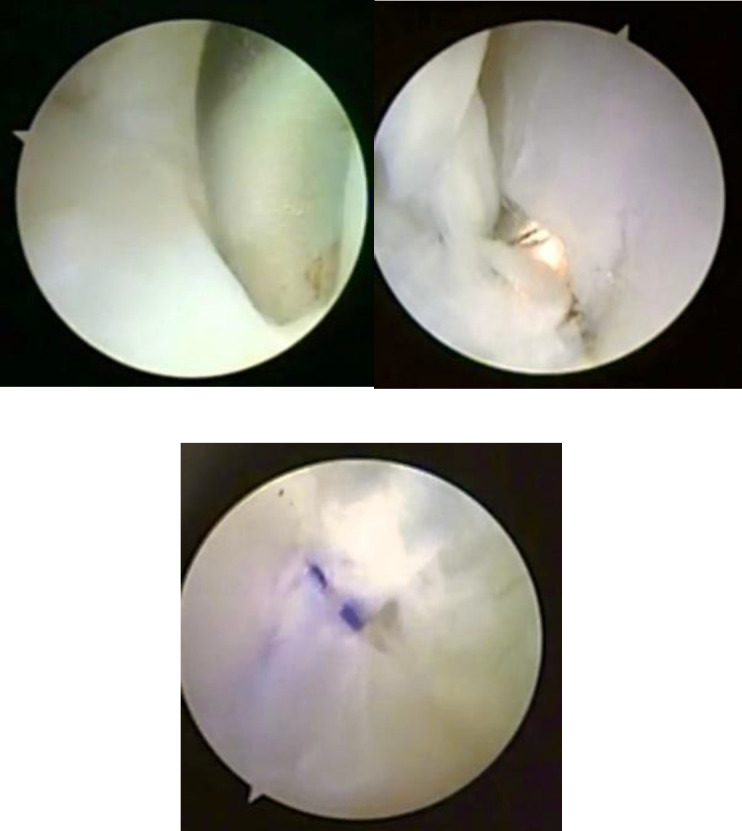
Arthroscopy is diagnostic and therapeutic in articular disc tears and allows direct assessment of other plausible associated injuries (47) [Figures 13 and 14].
Figure 13.
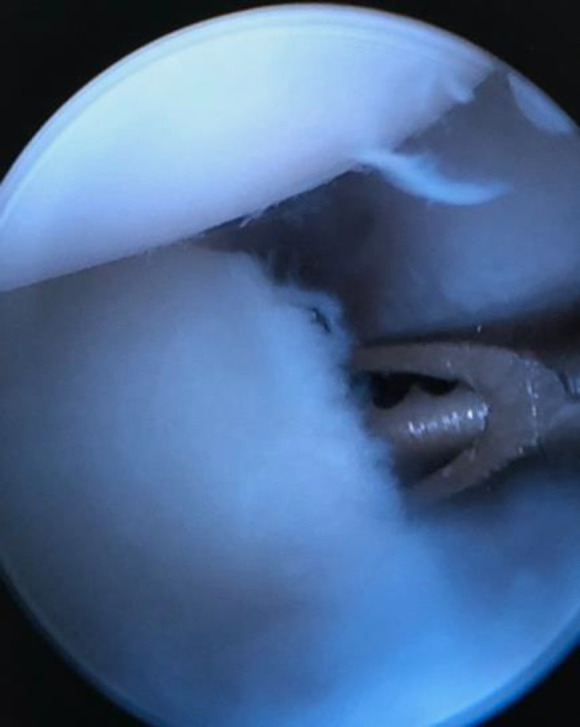
The shaver is under the TFCC through the ulnar-sided tear from the foveal attachment
Figure 14.
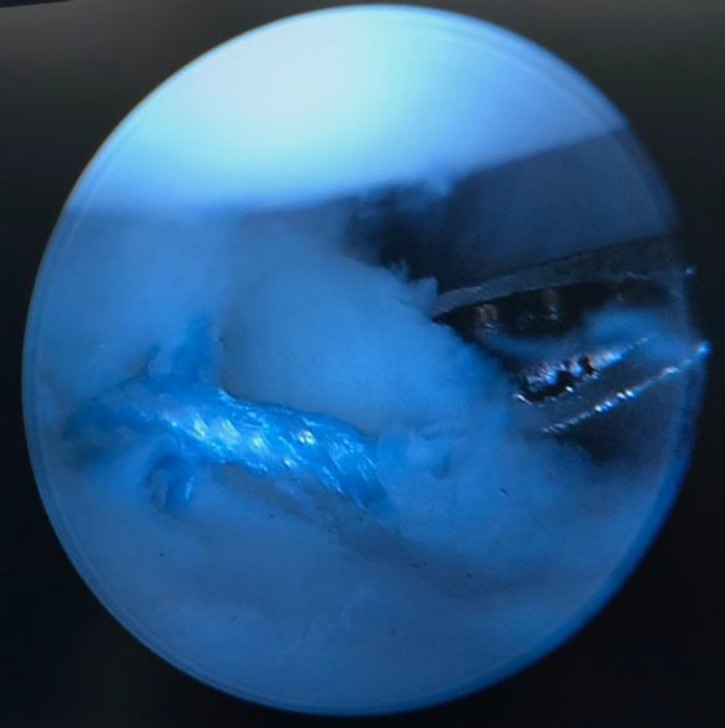
Arthroscopic repair of the TFCC with cross sutures passing through the TFCC and the bone tunnel existing at the fovea
Hess et al. have utilized ultrasonography to evaluate DRUJ laxity. They compared bilateral wrists in individuals with unilateral instability and wrists of the healthy volunteers. During the press-test maneuver, they measured the depression of the ulna. They detected abnormal laxity with a sensitivity of 88% and a specificity of 81%. However, they did not describe a method to detect supination instability (48). Dao et al reported the effectiveness of ultrasound in the assessment of dynamic scapholunate ligamentous instability (49). In 2019 Yoshii et al developed a pressure-monitor ultrasound system to quantitatively assess DRUJ stability. They stated that their methodology might be clinically valuable to study the mechanical properties of individuals with DRUJ instability (50).
Recently it has been shown that the measuring of forearm peak pronation and supination torque is a well-founded technique, with an elevated intraclass correlation (ICC) and excellent responsiveness. Forearm peak pronation and supination torque mensurations are carried out utilizing a wrist dynamometer provided with a digital pressure gauge (Model BL-2000, Baseline, White Plains, New York). The instrument was calibrated at the Research Institute of Sweden (RISE), division SP (Statens Provningsanstalt). The exactness of measurement of the dynamometer is 0.01 Nm. It has been considered a good clinical device for the diagnosis of TFCC 1B injuries (51,52). Wijffels et al compared four CT scoring systems for the detection of distal radioulnar joint instability: the radioulnar line test, subluxation ratio test, epicenter method and radioulnar ratio test. The epicenter test seemed the most dependable. Scanning of both wrists might be useful to avert the radiological overdiagnosis of instability (53). In 2021 Arimitsu et al reported that CT arthrography could be a encouraging technique for diagnosing proximal horizontal flap tears of the TFCC (54).
Treatment
In acute DRUJ instability with fracture of the distal radius, Lee et al. have found similar long-run results of conservative treatment (supination sugar-tong splinting) and surgical treatment (55). However, Poppler et al. have reported that in acute dislocations of the DRUJ, restoration of stability is commonly accomplished by simply reducing the dislocation under local anesthesia (2). If DRUJ stability is reestablished after closed reduction, treatment in a cast with the forearm in the position of stability (supination for dorsal dislocations; pronation for volar dislocations) is advised. Nonetheless, if open reduction is needed, direct repair of the TFCC to its foveal insertion is advised utilizing a suture anchor or bone tunnels.
Although nonoperative treatment does not usually work in chronic instability of the DRUJ , it can be used in mild situations in low-demand individuals. Non-surgical treatment and rehabilitation after surgery are usually done with a program of forearm and wrist strengthening exercises and proprioception (56). Several flexible functional orthoses exist for DRUJ to restrict translation, although they may restrain mobility (57).
Bony alignment has to be reestablished first to produce an acceptable long-run result after ligament reconstruction. Corrective osteotomy of a malunion of the distal radius usually restores stability and obviates the necessity of ligament reconstruction. Nevertheless, if intraoperative testing after bony correction discloses pertinacious instability, reconstruction may be necessary (1,58).
According to Krimmer, the indication for corrective osteotomy of a malunion of the distal end of the radius is a dorsal tilt or palmar tilt of the radius of 30° (58).
Individuals with negative ulnar variance usually have a robust and repairable TFCC, even in cases with chronic tears. MRI shows the TFCC thickness and the intensity of its retraction from the fovea. The most common and most reliable repair method is the transosseous sutures through the fovea exiting the ulnar neck (1) [Figures 15 and 16].
Figure 15.
TFCC tear type IB, the transosseous suture refixation provide reasonable fixation
Figure 16.
Triangular fibrocartilage complex repair through bone tunnels (Palmer type 1D).
In acute TFCC tears with DRUJ instability, arthroscopic suture repair with pronator quadratus advancement provides good clinical amelioration and adequate stability; consequently, it seems to be an adequate, efficacious treatment alternative for acute TFCC tears with DRUJ instability (59). In a dorsal ulnar head dislocation, we immobilize the forearm in mid-to full supination to stretch the pronator quadratus to pull the ulnar head into the sigmoid notch and to optimize the soft-tissue healing (60).
Notchplasty of a flat sigmoid notch may be performed concomitantly to add stability to a ligament reconstruction. It has been reported that if symptoms are not alleviated by anatomical distal radioulnar joint ligament reconstruction, a sigmoid notch osteotomy can reestablish the stability of the DRUJ (61).
Ulnar shortening osteotomy (USO) may be performed concomitantly when ulnar impaction syndrome exists. It increases load across the ulnocarpal predisposing the reconstruction to fail (62,63) [Figure 17]. USO can also be used in concomitant lunotriquetral (LT) ligament injury (64).
Figure 17.

Ulnar shortening osteotomy improves the osseous stability at the DRUJ in the ulnar impaction syndrome
DRUJ osteoarthritis relatively contraindicates ligament reconstruction. The reason is that it increases the joint's contact force, aggravating the condition and pain. However, in an active individual with osteoarthritis who does not do well with a salvage procedure, radioulnar ligament reconstruction may be attempted, reserving the salvage procedure at a later date if the reconstruction fails (1). In 2017 Atzei et al categorized five types on a management-oriented classification system of peripheral tears of the TFCC (65) [Table 1].
Table 1.
Classification of ulnar triangular fibrocartilage complex (TFCC) tears according to Atzei et al (63).
| Type 1 Isolated tears of the distal triangular fibrocartilage complex (TFCC) without distal radio-ulnar joint (DRUJ) instability and are amenable to arthroscopic suture. |
| Type 2 Rupture of both the distal triangular fibrocartilage complex (TFCC) and proximal attachments of the triangular fibrocartilage complex (TFCC) to the fovea. |
| Type 3 Isolated ruptures of the proximal attachment of the triangular fibrocartilage complex (TFCC) to the fovea; they are not visible at radio-carpal arthroscopy. |
| Type 4 Irreparable tears due to the size of the defect or to poor tissue quality and, if required, treatment is through distal radio-ulnar ligament reconstruction with tendon graft. |
| Type 5 They are associated with distal radio-ulnar joint (DRUJ) arthritis and can only be treated with salvage procedures. This subdivision of type IB triangular fibrocartilage complex (TFCC) tear provides more insights in the pathomechanics and treatment strategies. |
| Both class 2 and class 3 tears are diagnosed with a positive hook test and are typically associated with distal radio-ulnar joint instability. If required, treatment is through reattachment of the distal radio-ulnar ligament insertions to the fovea. |
Surgical Treatments
A systematic review showed similar outcomes between open and arthroscopic repair of the TFCC, in terms of DRUJ re-instability and functional outcome scores. There was incomplete evidence to advise one technique over the other in clinical practice (66). Other systematic review demonstrated a current lack of high-degree evidence needed to reach scientifically sound conclusions on the benefits of arthroscopic versus open repair of 1B TFCC tears (67).
Extraarticular reconstruction
Fulkerson and Watson reported a procedure by passing a tendon graft through a bone tunnel in the radius in the anteroposterior direction just proximal to the TFCC insertion. The tendon is passed around the ulnar neck extra-articularly to secure the ulnar head against the sigmoid notch (68) [Figure 18]. In a group of 5 individuals with a mean follow-up of 15 months, stability was achieved (69). However, pro-supination limitation occurred. Circumferential bone resorption around the ulnar neck caused by the graft was found in the radiological examination.
Figure 18.
A tendon graft is passed through a bone tunnel in the radius in the anteroposterior direction just proximal to the TFCC insertion. The tendon is passed around the ulnar neck extra-articularly to secure the ulnar head against the sigmoid notch
Similarly, brachioradialis has been utilized while maintaining the normal insertion as a tether point [70]. In another study, including 21 individuals, stability was achieved by passing the pronator quadratus around the ulna. Functionally, the patients ameliorated with no relevant limitation in mobility (71).
DOB (distal oblique bundle of the interosseous membrane) reconstruction or reinforcement is also described for DRUJ stability (72). Graft fixation is cumbersome, and its applicability is under question. Two of 14 patients showed persistent instability requiring reoperation; the ulnar bone tunnel was fractured in another patient (73).
Hui and Linscheid reported a sling design that utilizes a distal strip of the FCU with a distal base attached to the pisiform. The strip is brought to the dorsal-ulnar of the wrist and passed via a bony tunnel in the fovea. The tendon strip exits under the ECU and is then turned volar to be attached to the main FCU tendon bulk [74]. Pronation is limited in this technique (28).
Dy et al technique, an ulnar-based strip of the extensor retinaculum is used for capsulorrhaphy (75). Even though anatomic reconstruction of the DRUJ ligaments gives favorable stabilization of the radioulnar joint, individuals who have accompanying ulnocarpal instability need an option that sorts out both the DRUJ- and ulnocarpal-stabilizing functions of the TFCC. The Herbert sling, which is an extensor retinaculum capsulorrhaphy, is an efficacious technique of fabricating a robust tether among the distal radius, ulna, and ulnar carpus. Initial biomechanical and clinical outcomes have been satisfactory.
Intraarticular reconstruction
Scheker et al. described the intra-articular technique using multiple holes and passes, which restored stability but resulted in limited motion in many patients (32).
Adams described a technique using less invasive dissection (34,35). Depending on the graft length, one limb can be sutured to the other end after passing around the neck. If two divergent tunnels are made through the fovea, the ends can be tied together over a dorsal ulna bony bridge. The graft end can be passed around the ECU sheath too. Of 14 patients tested with a mean follow-up of 2 years, instability resolved in 12 individuals, and they could return to their pre-injury activities. One patient required a second surgery. Another preferred to wear a splint for symptomatic relief; in these two patients, a flat sigmoid notch was identified, which probably was correlated to the failure (34).
In a series of 16 individuals with more than one-year of follow-up using the Adams procedure, one patient underwent a second surgery for persistent instability by sigmoid notchplasty. Functional scores improved, and stability was maintained in the other patients (76).
In a series of 22 patients undergoing the Adams procedure, it was encountered that supination, pronation, and grip strength were substantially diminished in the operated wrist. Postoperative DASH and Patient-Rated Wrist and Hand Evaluation (PRWHE)-scores averaged 13.1 and 20.3, apiece. The Adams technique affected, but mainly restored pronation and supination, and clinical examination, DASH, and PRWHE scores indicated that the Adams technique left individuals with upper extremity functionality similar to healthy individuals (77).
Meyer et al. used two divergent osseous tunnels through the fovea and tied the graft over the bone bridge in 48 individuals (78). Forty-four patients showed restoration of stability in a mean follow-up of 16 months. Compared to the Adams and Berger series, patients lost approximately 10° more pronation and supination (34,78).
Gillis et al. used Adams procedure in 95 wrists and followed up the patients for a mean of 5.5 years (79). They fixed the tendon graft with three distinct techniques, including sutures alone, suture anchors, or an interference screw. The failure rate was 14%. Allograft was not considered to be the cause of any complications. More failure was observed with an interference screw which highlights proper graft tension and secure fixation. Failure was also related to women gender highlighting the contribution of inherent laxity in women compared to men.
Tse et al. described an arthroscopic-assisted anatomic reconstruction technique without violating the DRUJ capsule (80). Fifteen individuals were analyzed with a mean follow-up of 7 years. Two tears occurred 14 and 18 months after surgery and were considered traumatic. Pronation-supination improved after surgery but persisted restricted in comparison to the healthy side. Nearly all individuals went back to work or their pre-injury activities. Functional and pain scores improved significantly (80).
Luchetti and Atzei assessed 11 individuals with a mean follow-up of five years after an arthroscopic-assisted anatomic reconstruction utilizing a tendon graft fixed by an interference screw (81). The ulnar styloid fracture occurred in one patient. One patient had recurrent instability requiring a second surgery. Functional scores improved in the other patients, and all returned to their previous activities. Grip strength ameliorated significantly to about 96% of the contralateral side (81).
Anatomic reconstruction
In 2020 Frantz et al. investigated patients' clinical outcomes for chronic DRUJ instability by open anatomic reconstruction of the palmar and dorsal radioulnar ligaments (82). Of 30 individuals (31 wrists) treated with the above technique, 19 were followed for a mean of 10 years (range 3-21). Long-run statistically significant ameliorations occurred in ulnar-sided wrist pain on the visual analog scale and in distal radioulnar joint stability on the dorsopalmar stress test. The modified Mayo Wrist Scores were considered excellent in 3 individuals, good in 12, fair in 3, and poor in one. Of the 30 individuals analyzed, four failed, two for graft rupture and two for osteoarthritis of the DRUJ (82).
Factors influencing the failure were an incompetent sigmoid notch, lack of accuracy when performing the osseous tunnels, inadequate tensioning of the graft, and inappropriate immobilization. Reestablishment of DRUJ stability does not warrant elimination of the ulnar-sided wrist pain. Pertinacious symptoms may result from multiple other unrecognized causes (83).
Foveal reattachment of the TFCC with dorsal capsuloplasty and imbrications of the extensor retinaculum
In 2020 Neto and Neto described their results using a proprietary surgical technique to treat chronic post-traumatic DRUJ instability (84). They analyzed 11 patients treated with a foveal reattachment of the TFCC and dorsal capsule and extensor retinaculum imbrications. Follow-up was one year. All individuals reported pain alleviation and lack of instability, going back to normal activities at 3-6 months. The mean DASH questionnaire score was 9.5 (range: 2-25). Mean forearm rotation was 89° in pronation and 85° in supination. This technique was considered an efficacious surgical technique for the management of DRUJ chronic post-traumatic instability.
Dorsal capsular imbrications for post-traumatic dorsal instability
Unglaub et al. evaluated their long-term results using the dorsal capsular imbrication of the DRUJ in dorsal instability (85). They analyzed ten individuals (mean 38.7 years of age) with a mean follow-up of 11.2 years (9.3 to 14.3 years). The DASH questionnaire, MMWS score, range of motion compared to the healthy limb, pre and postoperative pain level, and DRUJ stability examination were assessed. Eight of the ten DRUJs were stable. The mean MMWS was 93 (65-100). The DASH score was 8.8 (0-60) on average. Grip strength achieved 94% of the unaffected hand. The range of motion did not vary substantially compared to the healthy contralateral limb. Nine of ten individuals considered the decrease in pain intensity to be very good. Eight of ten individuals considered the stability of the DRUJ to be very good following surgery. Dorsal capsular imbrication of the DRUJ is considered an effective surgical procedure for post-traumatic dorsal instability in the long-run (85).
Arthroscopic thermal stabilization
Helpster et al. analyzed the clinical results of individuals treated for chronic distal radioulnar joint instability by means of arthroscopic thermal annealing of the superficial radioulnar ligaments, ulnar palmar wrist ligaments, and dorsoulnar wrist capsule utilizing a radiofrequency probe (86). Sixty individuals (62 wrists) were treated with this technique over 18 years. After a mean follow-up of 10 years (range 3 to 19), 30 of the 33 individuals were pleased with the outcome. There were statistically significant ameliorations in ulnar-sided wrist pain on a visual analog scale and in DRUJ stability on the dorsopalmar stress test after the surgical procedure. The modified MWS and Quick DASH scores of the individuals were favorable. An early failure happened in 11 of the 62 wrists. Nine of these 11 wrists required a secondary surgical technique. Helpster et al. concluded that arthroscopic thermal shrinkage is adequate for most individuals with mild to moderate chronic DRUJ instability in long-run follow-up. Besides, in case of early failure, secondary open ligament reconstruction is an alternative.
Salvage procedures
Breyer and Vergara have pointed out that patients with an unstable and osteoarthritic DRUJ present serious functional impairment, ache, and weakness in gripping manipulation of things. Also, that various surgical options have been reported to treat these problems (87). Resection arthroplasties include different kinds of distal ulnar resection and soft tissue techniques, which have generally yielded good results; however, especially in the most active patients, such procedures have failed to relieve pain and restore stability satisfactorily. Since the late 1980s, partial and total joint arthroplasties are good options for young, active individuals.
Sauve-Kapandji arthrodesis (SKA)
Giberson-Chen et al. analyzed 57 patients operated on with the SKA. The surgical indications were post-traumatic and DRUJ osteoarthritis, rheumatoid arthritis, Madelung deformity, psoriatic arthritis, and giant cell bone tumor (88). During the first year after surgery, QuickDASH scores diminished from 52 prior to surgery to 28 at 1 year. QuickDASH scores at final follow-up showed substantial amelioration in individuals with osteoarthritis and inflammatory arthritis. Supination improved substantially after the surgical procedure, from 48° to 74°; however, there was no change in wrist flexion, wrist extension, and pronation. Substantial postoperative reductions in ulnar variance and McMurtry's translation index were encountered radiographically [Figure 19].
Figure 19.

Sauvé-Kapandji arthrodesis is a salvage procedure for post-traumatic instability and arthritis at the DRUJ
The percentage of postoperative adverse events was 21%, including revision osteotomy in 4 individuals (7%) and hardware removal in 4 individuals (7%). No nonunion of the DRUJ was observed.
In 2020 Barret et al. evaluated the stability of the DRUJ after performing a modified matched distal ulnar resection carried out alone or with partial or complete wrist fusion (89). The technique consisted of the reconstruction of the sixth compartment and dorsalization of the ECU. This modification of the matched distal ulnar resection minimized the adverse events specific to other ulnar head resection procedures or the SKA, i.e., radioulnar convergence and DRUJ instability.
In 2003 Zimmermann et al reported the long-run outcomes of a modified Sauvé-Kapandji technique in 43 patients (90). The average follow-up was 8 years (range 5-12 years). Forearm rotation ameliorated in all individuals, ulnar wrist pain was diminished in 97% of the individuals, and 9% had mild pain at the proximal ulnar stump. Grip strength ameliorated from a mean of 38% before surgery to a mean of 55% after surgery compared with the contralateral side. The DASH score was 28 points on average. In all patients the fusion consolidated within 8 weeks. In 74% of the cases the radiographic study revealed approximation between the proximal ulna stump and the radius compared with the preoperative situation (90). However, some authors believe that Sauve Kapanji is not a proper choice for the instability of DRUJ. According to Reissner et al (2021), because of the elevated frequency of revision surgery due to instability of the proximal ulnar stump, the utilization of the Sauvé-Kapandji technique must be restricted only to very selected cases (91)
In 2021 Verhiel et al studied 85 individuals who suffered post-traumatic DRUJ derangement and had experienced either a Darrach (n = 57) or Sauvé-Kapandji technique (n = 28) (92). Seventeen individuals (30%) in the Darrach group had an adverse event, and 14 individuals (50%) in the Sauvé-Kapandji group had an adverse event. The most frequent adverse event was instability of the ulnar stump (n = 10), followed by symptoms of the dorsal sensory branch of the ulnar nerve (n = 8). Individuals who experienced a Sauvé-Kapandji technique had more reoperations for excision of heterotopic ossification. Darrach and Sauvé-Kapandji techniques exhibited similar long-run patient-reported outcomes in management of post-traumatic DRUJ dysfunction. Adverse event and reoperation percentage were relatively elevated, with non-significant differences between the two techniques.Post-traumatic ulnar impaction syndrome (ulnocarpal impingement syndrome) can be managed by shortening the ulna. This can be accomplished by shaft or metaphyseal osteotomy, or by arthroscopic epiphyseal resection. In 2021 Auzias et al compared the outcomes of the shaft ulnar shortening osteotomy (SUSO, N = 9) and arthroscopic wafer procedure (AWP, N = 24) of the ulna in this indication (93). Mean follow-up was 103months in the SUSO group versus 55 months in the AWP group. There was no significant difference between groups in pain intensities, grip strength and PRWE score, and DASH score. The period of time away from work was greater in the SUSO group than in the AWP group (7.86 months versus 3.75 months). Seven individuals were reoperated in the SUSO group (5 plate removal, 1 nonunion and 1 delayed union) versus 3 in the AWP group (1 ECU stabilization, 1 ablation for painful ulnar styloid due to nonunion and 1 wrist denervation) .
Distal radioulnar prosthetic replacement
The alternative procedure for traditional reconstructive techniques is prosthetic arthroplasty. DRUJ prostheses mechanically stabilize the distal forearm after ulnar head resection; Besides, DRUJ prostheses yield a more normal transfer of the force throughout the wrist and forearm (94-102).
DRUJ prostheses can be classified into two types: DRUJ hemiarthroplasty and total radioulnar joint replacement. In DRUJ hemiarthroplasty, the prosthesis only includes the ulnar component (“UHP, Martin GMBH, Germany” and “U-Head, Small Bone Innovation, USA prostheses”). In total DRUJ replacement, the prosthesis and the ulnar component replace the sigmoid notch, including the radial component. (“Aptis DRUJ Prostheses, Aptis Medical, the USA” [Figure 20] as well as the prosthesis designed by Schuurman AH) (98). A short while ago, a newly-designed prosthesis based on the Sauvé-Kapanji technique has been developed with the encouraging result to restore near-normal anatomy (99,100) [Figure 21].
Figure 20.

Aptis DRUJ prostheses, Aptis Medical, USA DRUJ prosthesis: This prosthesis is a constrained ball and socket joint composed of a radial and an ulnar component that functions the sigmoid notch and ulnar head. The radial component is fixed to the radius by the distal peg and cortical screws
Figure 21.
Intraosseous distal radioulnar joint prosthesis is a new design based on the Sauvé-Kapadji procedure to help stabilize the DRUJ (a, b, c, d). (Reproduced with permission from the Archives of Bone and Joint Surgery Journal)
Prosthetic arthroplasty of the distal ulna combined with an appropriate soft-tissue repair is advised to ameliorate pain, function, and strength of the wrist and forearm secondary to instability. Prosthetic replacement restored DRUJ stability after symptomatic partial or complete excision of the ulnar head and resolved the radioulnar impingement. Various DRUJ implants are designed and available with very low complication and revision rates at a mean follow-up period of 32 months (range, 26–60 months). However, the long-run success of distal ulna prosthetic replacement has to be studied (94-102). At this point, the constrained prosthesis has shown good longevity and outcome (99).
The limitation is that knowledge in DRUJ prosthesis is limited, and reports with long-run follow-up and reports intending to compare distinct kinds of DRUJ prostheses are uncommon. Some guidelines can help the surgeon choose an adequate DRUJ prosthesis among the accessible ones; nevertheless, implant usage depends on surgeon experience and accessibility (96).
The diagnosis of the DRUJ instability and TFCC tear is clinical using the tests. MRI should confirm the diagnosis, and if necessary, by CT scan with three-dimensional reconstruction to assess the bony alignment and the sigmoid notch anatomy and congruity. Arthroscopy is the gold standard in diagnosing wrist ligament injuries and the structural quality of the ligaments.
It is crucial to accomplish apropriate bony alignment before restoring DRUJ stability. Depending on the chronicity and quality of the surrounding soft tissue, peripheral TFCC tears can be repaired primarily to address the subtle instability and ulnar-sided pain. In more extensive damage, chronic injuries, and frank instability, DRUJ ligament reconstruction may be necessary. If the sigmoid notch is flat, it may be necessary to add a sigmoid notchplasty. Following a ligament reconstruction, patients usually notice an improvement in pain and grip strength, although they may develop DRUJ stiffness. A salvage procedure or implant arthroplasty must be considered in individuals with significant osteoarthritis or uncorrected bone deformity.
Figure 4.
Dorsal lunate facet malunion causing instability, pain, and limited wrist motion
Figure 5.

Bone reduction forceps for reduction of the dorsal fragment through the volar approach
Figure 6.
Injury occurs to the DRUJ during a Galeazzi fracture-dislocation (a), which is restored after surgical intervention (b, c).
References
- 1.Carr LW, Adams B. Chronic distal radioulnar joint instability. Hand Clin. 2020;36(4):443–453. doi: 10.1016/j.hcl.2020.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Poppler LH, Moran SL. Acute distal radioulnar joint instability: Evaluation and treatment. Hand Clin. 2020;36(4):429–441. doi: 10.1016/j.hcl.2020.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez Merchan EC, De la Corte H. Injuries of the distal radioulnar joint. Contemp Orthop . 1994;29(3):193–200. [PubMed] [Google Scholar]
- 4.Ekenstam FA, Hagert CG. Anatomical studies on the geometry and stability of the distal radio ulnar joint. Scand J Plast Reconstr Surg. 1985;19(1):17–25. doi: 10.3109/02844318509052861. [DOI] [PubMed] [Google Scholar]
- 5.af Ekenstam FW, Palmer AK, Glisson RR. The load on the radius and ulna in different positions of the wrist and forearm A cadaver study. Acta Orthop Scand. 1984;55(3):363–365. doi: 10.3109/17453678408992375. [DOI] [PubMed] [Google Scholar]
- 6.Tolat AR, Stanley JK, Trail IA. A cadaveric study of the anatomy and stability of the distal radioulnar jointin the coronal and transverse planes. J Hand Surg Br. 1996;21(5):587–594. doi: 10.1016/s0266-7681(96)80136-7. [DOI] [PubMed] [Google Scholar]
- 7.Haugstvedt J-R, Berger RA, Nakamura T, Neale P, Berglund L, An K-N. Relative contributions of the ulnar attachments of the triangular fibrocartilage complex to the dynamic stability of the distal radioulnar joint. J Hand Surg Am. 2006;31(3):445–451. doi: 10.1016/j.jhsa.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 8.Stuart PR, Berger RA, Linscheid RL, An KN. The dorsopalmar stability of the distal radioulnar joint. J Hand Surg Am. 2000;25(4):689–699. doi: 10.1053/jhsu.2000.9418. [DOI] [PubMed] [Google Scholar]
- 9.Faucher GK, Zimmerman RM, Zimmerman NB. Instability and arthritis of the distal radioulnar joint: a critical analysis review. JBJS reviews. 2016;4:12. doi: 10.2106/JBJS.RVW.16.00005. [DOI] [PubMed] [Google Scholar]
- 10.Bednar MS, Arnoczky SP, Weiland AJ. The microvasculature of the triangular fibrocartilage complex: its clinical significance. J Hand Surg Am. 1991;16(6):1101–1105. doi: 10.1016/s0363-5023(10)80074-7. [DOI] [PubMed] [Google Scholar]
- 11.Hotchkiss RN, An KN, Sowa DT, Basta S, Weiland AJ. An anatomic and mechanical study of the interosseous membrane of the forearm: Pathomechanics of proximal migration of the radius. J Hand Surg Am. 1989;14(2 Pt 1):256–261. doi: 10.1016/0363-5023(89)90017-8. [DOI] [PubMed] [Google Scholar]
- 12.Moritomo H. The function of the distal interosseous membrane and its relevance to the stability of the distal radioulnar joint: An anatomical and biomechanical review. Handchir Mikrochir Plast Chir. 2015;47(5):277–280. doi: 10.1055/s-0035-1545348. [DOI] [PubMed] [Google Scholar]
- 13.Arimitsu S, Moritomo H, Kitamura T, Berglund LJ, Zhao KD, An K-N, et al. The stabilizing effect of the distal interosseous membrane on the distal radioulnar joint in an ulnar shortening procedure: a biomechanical study. J Bone Joint Surg Am. 2011;93(21):2022–2030. doi: 10.2106/JBJS.J.00411. [DOI] [PubMed] [Google Scholar]
- 14.Gofton WT, Gordon KD, Dunning CE, Johnson JA, King GJW. Soft-tissue stabilizers of the distal radioulnar joint: an in vitro kinematic study. J Hand Surg Am. 2004;29(3):423–431. doi: 10.1016/j.jhsa.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 15.Kleinman WB. Stability of the distal radioulna joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function what we have learned in 25 years. J Hand Surg Am. 2007;32(7):1086–1106. doi: 10.1016/j.jhsa.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 16.Omokawa S, Iida A, Kawamura K, Nakanishi Y, Shimizu T, Kira T, et al. A biomechanical perspective on distal radioulnar joint instability. J Wrist Surg. 2017;6(2):88–96. doi: 10.1055/s-0037-1601367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kakar S, Carlsen BT, Moran SL, Berger RA. The management of chronic distal radioulnar instability. Hand Clin. 2010;26(4):517–528. doi: 10.1016/j.hcl.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 18.Moradi A, Mousavi SM, Hassankhani GG, Chaharjouy NT, Rasouli A, Ebrahimzadeh MH. Fixing ulnar styloid fracture with stable distal radioulnar joint: A randomized clinical trial. Arch Bone Jt Surg. 2021: 189–194. doi: 10.22038/abjs.2020.46717.2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cole DW, Elsaidi GA, Kuzma KR, Kuzma GR, Smith BP, Ruch DS. Distal radioulnar joint instability in distal radius fractures: the role of sigmoid notch and triangular fibrocartilage complex revisited. Injury. 2006;37(3):252–258. doi: 10.1016/j.injury.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 20.Kleinman WB. Distal radius instability and stiffness: common complications of distal radius fractures. Hand Clin. 2010;26(2):245–264. doi: 10.1016/j.hcl.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 21.Lans J, Alvarez J, Kachooei AR, Ozcan S, Jupiter JB. Dorsal lunate facet fracture reduction using a bone reduction forceps. J Wrist Surg. 2019;8(2):118–123. doi: 10.1055/s-0038-1673407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adams BD. Effects of radial deformity on distal radioulnar joint mechanics. J Hand Surg Am. 1993;18(3):492–498. doi: 10.1016/0363-5023(93)90098-N. [DOI] [PubMed] [Google Scholar]
- 23.Kihara H, Palmer AK, Werner FW, Short WH, Fortino MD. The effect of dorsally angulated distal radius fractures on distal radioulnar joint congruency and forearm rotation. J Hand Surg Am. 1996;21(1):40–47. doi: 10.1016/S0363-5023(96)80152-3. [DOI] [PubMed] [Google Scholar]
- 24.Nishiwaki M, Welsh MF, Gammon B, Ferreira LM, Johnson JA, King GJW. Effect of volarly angulated distal radius fractures on forearm rotation and distal radioulnar joint kinematics. J Hand Surg Am. 2015;40(11):2236–2242. doi: 10.1016/j.jhsa.2015.07.034. [DOI] [PubMed] [Google Scholar]
- 25.Dy CJ, Jang E, Taylor SA, Meyers KN, Wolfe SW. The impact of coronal alignment on distal radioulnar joint stability following distal radius fracture. J Hand Surg Am. 2014;39(7):1264–1272. doi: 10.1016/j.jhsa.2014.03.041. [DOI] [PubMed] [Google Scholar]
- 26.Fujitani R, Omokawa S, Akahane M, Iida A, Ono H, Tanaka Y. Predictors of distal radioulnar joint instability in distal radius fractures. J Hand Surg Am. 2011;36(12):1919–1925. doi: 10.1016/j.jhsa.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 27.Korompilias AV, Lykissas MG, Kostas-Agnantis IP, Beris AE, Soucacos PN. Distal radioulnar joint instability (Galeazzi type injury) after internal fixation in relation to the radius fracture pattern. J Hand Surg Am. 2011;36(5):847–852. doi: 10.1016/j.jhsa.2010.12.020. [DOI] [PubMed] [Google Scholar]
- 28.Glowacki KA, Shin LA. Stabilization of the unstable distal ulna: the Linscheid-Hui procedure. Tech Hand Up Extrem Surg. 1999;3(4):229–236. doi: 10.1097/00130911-199912000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Wijffels M, Brink P, Schipper I. Clinical and nonclinical aspects of distal radioulnar joint instability. Open Orthop J. 2012: :204–210. doi: 10.2174/1874325001206010204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tay SC, Tomita K, Berger RA. The "ulnar fovea sign" for defining ulnar wrist pain: an analysis of sensitivity and specificity. J Hand Surg Am. 2007;32(4):438–444. doi: 10.1016/j.jhsa.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 31.Lindau T, Adlercreutz C, Aspenberg P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg Am. 2000;25(3):464–468. doi: 10.1053/jhsu.2000.6467. [DOI] [PubMed] [Google Scholar]
- 32.Scheker LR, Belliappa PP, Acosta R, German DS. Reconstruction of the dorsal ligament of the triangular fibrocartilage complex. J Hand Surg Br. 1994;19(3):310–318. doi: 10.1016/0266-7681(94)90079-5. [DOI] [PubMed] [Google Scholar]
- 33.Lester B, Halbrecht J, Levy IM, Gaudinez R. Press test" for office diagnosis of triangular fibrocartilage complex tears of the wrist. Ann Plast Surg. 1995;35(1):41–45. doi: 10.1097/00000637-199507000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Adams BD, Berger RA. An anatomic reconstruction of the distal radioulnar ligaments for posttraumaticdistal radioulnar joint instability. J Hand Surg Am. 2002;27(2):243–251. doi: 10.1053/jhsu.2002.31731. [DOI] [PubMed] [Google Scholar]
- 35.Adams BD. Anatomic reconstruction of the distal radioulnar ligaments for DRUJ instability. Tech Hand Up Extrem Surg. 2000;4(3):154–160. doi: 10.1097/00130911-200009000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Nilsson K, Hallberg P, Tesselaar E, Farnebo S. A novel technique to assess distal radioulnar joint stability using increasing torque. J Wrist Surg. 2019;8(4):327–334. doi: 10.1055/s-0038-1675561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nakamura R, Horii E, Imaeda T, Tsunoda K, Nakao E. Distal radioulnar joint subluxation and dislocation diagnosed by standard roentgenography. Skeletal Radiol. 1995;24(2):91–94. doi: 10.1007/BF00198067. [DOI] [PubMed] [Google Scholar]
- 38.El Naga AN, Jordan ME, Netscher DT, Adams BD, Mitchell SA. Reliability of the dorsal tangential view in assessment of distal radioulnar joint reduction in the neutral, pronated, and supinated positions in a cadaver model. J Hand Surg Am. 2020;45(4):359.e1–359. doi: 10.1016/j.jhsa.2019.08.004. [DOI] [PubMed] [Google Scholar]
- 39.Mino DE, Palmer AK, Levinsohn EM. The role of radiography and computerized tomography in the diagnosis of subluxation and dislocation of the distal radioulnar joint. J Hand Surg Am. 1983;8(1):23–31. doi: 10.1016/s0363-5023(83)80046-x. [DOI] [PubMed] [Google Scholar]
- 40.Squires JH, England E, Mehta K, Wissman RD. The role of imaging in diagnosing diseases of the distal radioulnar joint, triangular fibrocartilage complex, and distal ulna. AJR Am J Roentgenol. 2014;203(1):146–153. doi: 10.2214/AJR.13.11573. [DOI] [PubMed] [Google Scholar]
- 41.Mino DE, Palmer AK, Levinsohn EM. Radiography and computed tomography in the diagnosis of incongruity of the distal radio-ulnar joint. J Bone Joint Surg Am. 1985;67(2):247–252. [PubMed] [Google Scholar]
- 42.Wechsler RJ, Wehbe MA, Rifkin MD, Edeiken J, Branch HM. Computed tomography diagnosis of distal radioulnar subluxation. Skeletal Radiol. 1987;16(1):1–5. doi: 10.1007/BF00349919. [DOI] [PubMed] [Google Scholar]
- 43.Lo IK, MacDermid JC, Bennett JD, Bogoch E, King GJ. The radioulnar ratio: a new method of quantifying distal radioulnar joint subluxation. J Hand Surg Am. 2001;26(2):236–243. doi: 10.1053/jhsu.2001.22908. [DOI] [PubMed] [Google Scholar]
- 44.Chiang CC, Chang MC, Lin CF, Liu Y, Lo WH. Computerized tomography in the diagnosis of subluxation of the distal radioulnar joint. Zhonghua Yi Xue Za Zhi (Taipei) 1998;61(12):708–715. [PubMed] [Google Scholar]
- 45.Nakamura R, Horii E, Imaeda T, Nakao E. Criteria for diagnosing distal radioulnar joint subluxation by computed tomography. Skeletal Radiol. 1996;25(7):649–653. doi: 10.1007/s002560050152. [DOI] [PubMed] [Google Scholar]
- 46.Wijffels M, Stomp W, Krijnen P, Reijnierse M, Schipper I. Computed tomography for the detection of distal radioulnar joint instability: normal variation and reliability of four CT scoring systems in 46 patients. Skeletal Radiol. 2016;45(11):1487–1493. doi: 10.1007/s00256-016-2455-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anderson ML, Larson AN, Moran SL, Cooney WP, Amrami KK, Berger RA. Clinical comparison of arthroscopic versus open repair of triangular fibrocartilage complex tears. J Hand Surg Am. 2008;33(5):675–682. doi: 10.1016/j.jhsa.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 48.Hess F, Farshad M, Sutter R, Nagy L, Schweizer A. A novel technique for detecting instability of the distal radioulnar joint in complete triangular fibrocartilage complex lesions. J Wrist Surg. 2012;1(2):153–158. doi: 10.1055/s-0032-1312046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dao KD, Solomon DJ, Shin AY, Puckett ML. The efficacy of ultrasound in the evaluation of dynamic scapholunate ligamentous instability. JBJS. 2004;86(7):1473–8. doi: 10.2106/00004623-200407000-00016. [DOI] [PubMed] [Google Scholar]
- 50.Axelsson P, Fredrikson P, Nilsson A, Andersson JK, Kärrholm J. Forearm torque and lifting strength: normative data. The Journal of hand surgery. 2018;43(7):677–e1. doi: 10.1016/j.jhsa.2017.12.022. [DOI] [PubMed] [Google Scholar]
- 51.Andersson JK, Hagert EM, Fridén J. Patients with triangular fibrocartilage complex injuries and distal radioulnar joint instability gain improved forearm peak pronation and supination torque after reinsertion. Hand. 2020;15(2):281–6. doi: 10.1177/1558944718793198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wijffels M, Stomp W, Krijnen P, Reijnierse M, Schipper I. Computed tomography for the detection of distal radioulnar joint instability: normal variation and reliability of four CT scoring systems in 46 patients. Skeletal Radiol 2016. 45(11):1487–1493. doi: 10.1007/s00256-016-2455-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Arimitsu S, Masatomi T, Shigi A, Yukioka C, Moritomo H. Proximal horizontal flap tears of TFCC diagnosed by computed tomography arthrography: six case series. J Wrist Surg. 2021;10(1):36–41. doi: 10.1055/s-0040-1716510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee SK, Kim KJ, Cha YH, Choy WS. Conservative treatment is sufficient for acute distal radioulnar joint instability with distal radius fracture. Ann Plast Surg. 2016;77(3):297–304. doi: 10.1097/SAP.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 55.Mesplié G, Grelet V, Léger O, Lemoine S, Ricarrère D, Geoffroy C. Rehabilitation of distal radioulnar joint instability. Hand Surg Rehabil. 2017;36(5):314–321. doi: 10.1016/j.hansur.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 56.Millard GM, Budoff JE, Paravic V, Noble PC. Functional bracing for distal radioulnar joint instability. J Hand Surg Am. 2002;27(6):972–977. doi: 10.1053/jhsu.2002.36542. [DOI] [PubMed] [Google Scholar]
- 57.Hermann K, Rene S, Wolters R. Corrective osteotomy after malunited distal radius fractures. Archives of orthopaedic and trauma surgery. 2020;140(5):675–80. doi: 10.1007/s00402-020-03370-1. [DOI] [PubMed] [Google Scholar]
- 58.Lee SK, Chun YS, Bae JH, Yu YT, Choy WS. Arthroscopic suture repair with additional pronator quadratus advancement for the treatment of acute triangular fibrocartilage complex tear with distal radioulnar joint instability. Ann Plast Surg . 2019;83(4):411–418. doi: 10.1097/SAP.0000000000001982. [DOI] [PubMed] [Google Scholar]
- 59.Gordon KD, Dunnin CE, Johnson JA, King GJW. Influence of the pronator quadratus and supinator muscle load on DRUJ stability. J Hand Surg Am. 2003;28(6):943–950. doi: 10.1016/s0363-5023(03)00487-8. [DOI] [PubMed] [Google Scholar]
- 60.Kim BS, Song HS, Jung KH, Kim HT. Distal radioulnar joint volar instability after ligament reconstruction failure treated with sigmoid notch osteotomy. Orthopedics. 2012;35(6):e984–e987. doi: 10.3928/01477447-20120525-49. [DOI] [PubMed] [Google Scholar]
- 61.Moritomo H. The distal interosseous membrane: current concepts in wrist anatomy and biomechanics. J Hand Surg Am. 2012;37(7):1501–1507. doi: 10.1016/j.jhsa.2012.04.037. [DOI] [PubMed] [Google Scholar]
- 62.Nishiwaki M, Nakamura T, Nakao Y, Nagura T, Toyama Y. Ulnar shortening effect on distal radioulnar joint stability: a biomechanical study. J Hand Surg Am. 2005;30(4):719–726. doi: 10.1016/j.jhsa.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 63.Wagner ER, Elhassan BT, Rizzo M. Diagnosis and treatment of chronic lunotriquetral ligament injuries. Hand Clin. 2015;31(3):477–486. doi: 10.1016/j.hcl.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 64.Atzei A, Luchetti R, Garagnani L. Classification of ulnar triangular fibrocartilage complex tears A treatment algorithm for Palmer type IB tears. J Hand Surg Eur Vol. 2017;42(4):405–414. doi: 10.1177/1753193416687479. [DOI] [PubMed] [Google Scholar]
- 65.Andersson JK, Ahlén M, Andernord D. Open versus arthroscopic repair of the triangular fibrocartilage complex: a systematic review. J Exp Orthop. 2018;5(1) doi: 10.1186/s40634-018-0120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Robba V, Fowler A, Karantana A, Grindlay D, Lindau T. Open versus arthroscopic repair of 1B ulnar-sided triangular fibrocartilage complex tears: a systematic review. Hand (N Y) 2020;15(4):456–464. doi: 10.1177/1558944718815244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fulkerson JP, Watson HK. Congenital anterior subluxation of the distal ulna A case report. Clin Orthop Relat Res. 1978: 179–182. [PubMed] [Google Scholar]
- 68.Purisa H, Sezer I, Kabakas‚ F, Tuncer S, Ertürer E, Yazar M. Ligament reconstruction using the Fulkerson-Watson method to treat chronic isolated distal radioulnar joint instability: short-term results. Acta Orthop Traumatol Turc. 2011;45(3):168–174. doi: 10.3944/AOTT.2011.2380. [DOI] [PubMed] [Google Scholar]
- 69.Burke CS, Zoeller KA, Waddell SW, Nyland JA, Voor MJ, Gupta A. Assessment of distal radioulnar joint stability after reconstruction with the brachioradialis wrap. Hand (N Y) 2018;13(4):455–460. doi: 10.1177/1558944717708026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lee SK, Lee JW, Choy WS. Volar stabilization of the distal radioulnar joint for chronic instability using the pronator quadratus. Ann Plast Surg. 2016;76(4):394–398. doi: 10.1097/SAP.0000000000000354. [DOI] [PubMed] [Google Scholar]
- 71.Riggenbach MD, Wright TW, Dell PC. Reconstruction of the distal oblique bundle of the interosseous membrane: a technique to restore distal radioulnar joint stability. J Hand Surg Am. 2015;40(11):2279–2282. doi: 10.1016/j.jhsa.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 72.Brink PR, Hannemann PF. Distal oblique bundle reinforcement for treatment of DRUJ instability. J Wrist Surg. 2015;4(3):221–228. doi: 10.1055/s-0035-1556856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hui FC, Linscheid RL. Ulnotriquetral augmentation tenodesis: a reconstructive procedure for dorsal subluxation of the distal radioulnar joint. J Hand Surg Am. 1982;7(3):230–236. doi: 10.1016/s0363-5023(82)80171-8. [DOI] [PubMed] [Google Scholar]
- 74.Dy CJ, Ouellette EA, Makowski AL. Extensor retinaculum capsulorrhaphy for ulnocarpal and distal radioulnar instability: the Herbert sling. Tech Hand Up Extrem Surg. 2009;13(1):19–22. doi: 10.1097/BTH.0b013e318184c796. [DOI] [PubMed] [Google Scholar]
- 75.Seo KN, Park MJ, Kang HJ. Anatomic reconstruction of the distal radioulnar ligament for posttraumaticdistal radioulnar joint instability. Clin Orthop Surg. 2009;1(3):138–145. doi: 10.4055/cios.2009.1.3.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kootstra TJM, van Doesburg MH, Schuurman AH. Functional effects of the Adams procedure: a retrospective intervention study. J Wrist Surg. 2018;7(4):331–335. doi: 10.1055/s-0038-1660812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Meyer D, Schweizer A, Nagy L. Anatomic reconstruction of distal radioulnar ligaments with tendon graft for treating distal radioulnar joint instability: surgical technique and outcome. Tech Hand Up Extrem Surg. 2017;21(3):107–113. doi: 10.1097/BTH.0000000000000163. [DOI] [PubMed] [Google Scholar]
- 78.Gillis JA, Soreide E, Khouri JS, Kadar A, Berger RA, Moran SL. Outcomes of the Adams-Berger ligament reconstruction for the distal radioulnar joint instability in 95 consecutive cases. J Wrist Surg. 2019;8(4):268–275. doi: 10.1055/s-0039-1685235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tse WL, Lau SW, Wong WY, Cheng H-S, Chow C-S, Ho P-C, et al. Arthroscopic reconstruction of triangular fibrocartilage complex (TFCC) with tendon graft for chronic DRUJ instability. Injury. 2013;44(3):386–390. doi: 10.1016/j.injury.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 80.Luchetti R, Atzei A. Arthroscopic assisted tendon reconstruction for triangular fibrocartilage complex irreparable tears. J Hand Surg Eur Vol. 2017;42(4):346–351. doi: 10.1177/1753193417690669. [DOI] [PubMed] [Google Scholar]
- 81.Frantz ML, Helsper EA, Morris HA, Hearon BF. Outcomes after anatomic reconstruction of the radioulnar ligaments for distal radioulnar joint instability. J Hand Surg Eur Vol. 2020;45(9):909–915. doi: 10.1177/1753193420942668. [DOI] [PubMed] [Google Scholar]
- 82.Adams BD. Anatomic reconstruction of the distal radioulnar ligaments for DRUJ instability. Tech Hand Up Extrem Surg. 2000;4(3):154–160. doi: 10.1097/00130911-200009000-00003. [DOI] [PubMed] [Google Scholar]
- 83.Neto BC, Neto JHS. Chronic posttraumatic instability of the distal radioulnar joint: Foveal reattachment of the triangular fibrocartilage complex with dorsal capsuloplasty and extensor retinaculum imbrications. Hand (N Y) 2020 Apr;:1558944720912566. doi: 10.1177/1558944720912566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Unglaub JM, Heyse T, Bruckner T, Langer MF, Spies CK. Long-term functional outcome after dorsal capsular imbrication for post-traumatic dorsal instability of the distal radioulnar joint. Int Orthop. 2020;44(12):2683–2690. doi: 10.1007/s00264-020-04705-8. [DOI] [PubMed] [Google Scholar]
- 85.Helsper EA, Frantz LM , Adams JM, Morris HA, Hearon BF. Arthroscopic thermal stabilization for distal radioulnar joint instability: 3 to 19 years follow-up. J Hand Surg Eur Vol. 2020;45(9):916–922. doi: 10.1177/1753193420927882. [DOI] [PubMed] [Google Scholar]
- 86.Breyer JM, Vergara P. Solutions for the unstable and arthritic distal radioulnar joint. Hand Clin . 2020;36(4):523–530. doi: 10.1016/j.hcl.2020.07.008. [DOI] [PubMed] [Google Scholar]
- 87.Giberson-Chen CC, Leland HA, Benavent KA, Harper CL, Earp BE, Rozental TD. Functional outcomes after Sauve-Kapandji arthrodesis. J Hand Surg Am. 2020;45(5):408–416. doi: 10.1016/j.jhsa.2019.11.014. [DOI] [PubMed] [Google Scholar]
- 88.Barret H, Lazerges C, Chammas PE, Degeorge B, Coulet B, Chammas M. Modification of matched distal ulnar resection for distal radio-ulnar joint arthropathy: Analysis of distal instability and radio-ulnar convergence. Orthop Traumatol Surg Res. 2020;106(8):1597–1603. doi: 10.1016/j.otsr.2020.07.008. [DOI] [PubMed] [Google Scholar]
- 89.Zimmermann R, Gschwentner M, Arora R, Harpf C, Gabl M, Pechlaner S. Treatment of distal radioulnar joint disorders with a modified Sauve-Kapandji procedure: long-term outcome with special attention to the DASH Questionnaire. Arch Orthop Trauma Surg. 2003;123(6):293–298. doi: 10.1007/s00402-003-0529-5. [DOI] [PubMed] [Google Scholar]
- 90.Reissner L, Schweizer A, Unterfrauner I, Estermann L, Nagy L. Long-term results of Sauvé–Kapandji procedure. Journal of Hand Surgery. 2021:17531934211004459. doi: 10.1177/17531934211004459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Verhiel SH, Özkan S, Ritt MJ, Chen NC, Eberlin KR. A comparative study between Darrach and Sauvé-Kapandji procedures for post-traumatic distal radioulnar joint dysfunction. Hand. 2021;16(3):375–84. doi: 10.1177/1558944719855447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Auzias P, Delarue R, Camus EJ, Van Overstraeten L. Ulna shortening osteotomy versus arthroscopic wafer procedure in the treatment of ulnocarpal impingement syndrome. Hand Surg Rehabil. 2021;40(2):156–161. doi: 10.1016/j.hansur.2020.10.012. [DOI] [PubMed] [Google Scholar]
- 93.Sauerbier M, Hahn ME, Fujita M, Neale PG, Berglund LJ, Berger RA. Analysis of dynamic distal radioulnar convergence after ulnar head resection and endoprosthesis implantation. J Hand Surg. 2002;27(3):425–434. doi: 10.1053/jhsu.2002.31734. [DOI] [PubMed] [Google Scholar]
- 94.van Schoonhoven Jr, Fernandez DL, Bowers WH, Herbert TJ. Salvage of failed resection arthroplasties of the distal radioulnar joint using a new ulnar head prosthesis. J Hand Surg. 2000;25(3):438–446. doi: 10.1053/jhsu.2000.6006. [DOI] [PubMed] [Google Scholar]
- 95.Gordon KD, Dunning CE, Johnson JA, King GJ. Kinematics of ulnar head arthroplasty. Journal of hand surgery. 2003;28(6):551–8. doi: 10.1016/s0266-7681(03)00150-5. [DOI] [PubMed] [Google Scholar]
- 96.Kopylov P, Tägil M. Distal radioulnar joint replacement. Tech Hand Up Extrem Surg. 2007;11(1):109–114. doi: 10.1097/bth.0b013e3180337dd9. [DOI] [PubMed] [Google Scholar]
- 97.Schuurman AH, Teunis T. A new total distal radioulnar joint prosthesis: functional outcome. J Hand Surg. 2010;35(10):1614–1619. doi: 10.1016/j.jhsa.2010.06.026. [DOI] [PubMed] [Google Scholar]
- 98.Moradi A, Binava R, Hasanabadi SE, Vahedi E, Ebrahimzadeh MH. Introduction and early outcomes of intraosseus distal radioulnar joint prosthesis: A pilot study and a technique of a new design of the Sauvé-Kapandji procedure. Arch Bone Jt Surg. 2020;8(6):703–709. doi: 10.22038/abjs.2020.44520.2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Moradi A, Binava R, Vahedi E, Ebrahimzadeh MH, Jupiter J. Distal radioulnar joint prosthesis. Arch Bone Jt Surg. 2021;9(1):22–32. doi: 10.22038/abjs.2020.53537.2659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Willis AA, Berger RA, Cooney III WP. Arthroplasty of the distal radioulnar joint using a new ulnar head endoprosthesis: Preliminary report. J Hand Surg. 2007: 177–189. doi: 10.1016/j.jhsa.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 101.Kachooei AR, Chase SM, Jupiter JB. Outcome assessment after Aptis distal radioulnar joint (DRUJ) implant arthroplasty. Arch Bone Jt Surg. 2014:2:180–184. [PMC free article] [PubMed] [Google Scholar]