Abstract
Background:
This study aimed to assess the results after soft-tissue posterior instability surgery and address possible challenges during these operations.
Methods:
The databases of two tertiary hospitals were reviewed to identify patients treated for posterior shoulder instability between 2000 and 2015. Out of 198 treated patients, 19 cases underwent surgery with a mean follow-up of 35 months. Chart review was performed to obtain recurrence rates, revision rates, return to sport, persistent pain, subjective instability, subjective feeling of being better, complications, and range of motion after operative treatment of posterior shoulder instability. These outcomes were compared using the Fisher’s exact and Mann-Whitney U tests.
Results:
After surgery, 6 (32%) patients had a recurrent subluxation, and 11 (58%) cases had persistent pain; moreover, 5 (26%) patients had a persistent feeling of instability, and 10 (53%) cases did not feel improvement after the operation. Furthermore, 10 (53%) patients required a revision, and there were 7 (37%) cases with a complication. Postoperatively, 75% of the patients had a full forward flexion, and 93% of the cases had full internal rotation; however, 64% of them had restrictions in external rotation.
Conclusion:
There is a high rate of recurrent instability, need for revision, and complications after soft-tissue posterior instability surgery. Postoperative external rotation was impaired in most patients. Patients should be informed about these unsatisfactory results.
Key Words: Bankart, Dislocation, Glenohumeral, Instability, Posterior, Shoulder, Soft-tissue Surgery
Introduction
Posterior shoulder instability has a prevalence of 1.1 per 100.000 persons per year, mostly affecting male patients in their twenties to forties and those above 70 years of age (1). Posterior dislocations are often caused by a traumatic impact on the anterior part of the shoulder or axial force on an adducted and internally rotated arm, and to a lesser extent, by intense muscle contractions caused by a seizure or electrocution (2-6). Robinson et al. (1) concluded that up to 17.7% of patients with a posterior shoulder dislocation develop recurrent instability within a year after receiving non-surgical treatment. Antosh et al. (7) suggested that surgical treatment should be considered in patients with pain, instability, or functional limitations after three to six months of non-operative treatment, patients with a symptomatic posterior labral tear, unilateral posterior instability with a patulous or insufficient posterior capsule, and in selected multidirectional instability patients with predominantly posterior symptoms. In contrast, there are no distinct criteria for choosing between a soft-tissue and a bony procedure. This is unlike anterior shoulder instability, where the instability severity index score, a scoring list based on risk factors of recurrent instability, can aid in the decision making between a soft-tissue and a bony procedure (8). Standard portal placement does not provide sufficient access to the posterior labrum, making arthroscopic posterior instability surgery challenging.
Chronic lesions tend to have more fibrosis, which provide additional difficulties to reach the posterior labrum (9). A study conducted by Garret et al. has shown that the missed diagnosis of shoulder osteoarthritis with posterior subluxation, technical errors, and postoperative complications result in poor postoperative results (12). Due to the challenging nature, it is useful to address the results of these procedures in a tertiary hospital in which difficult cases are presented. Previous studies have identified the presence of chondral damage, previous shoulder surgery, concomitant surgery, workman’s compensation, age below 40 years, dislocation during a seizure, large reverse Hill-Sachs lesion, and glenoid retroversion as possible risk factors for recurrent instability (10,11).
Although there are some studies existing in the literature addressing the outcomes of arthroscopic soft-tissue surgery for posterior shoulder instability, these studies are small and do not address the possible challenges for this type of surgery. The rarity of posterior shoulder instability is apparent from the latest systematic review performed by Longo et al. that includes only 847 shoulders, from which 691 shoulders underwent arthroscopic management. Since the posterior instability is rare, cohort studies can only be performed in high volume centers or in a multicenter setting. It is thought that our patient cohort can provide a good addition to the currently scarce literature. Accordingly, this study aimed to assess the outcomes of arthroscopic posterior instability surgery in our hospital and address what factors could pose the possible challenges.
Materials and Methods
Patient selection
A chart review was performed, and the data of patients diagnosed with posterior shoulder instability between 2000 and 2015 were collected using the International Classification of Diseases-codes (ICD-9) 831.02 and 831.12 from the Research Patient Data Registry. Only patients who had undergone arthroscopic soft-tissue surgery for their posterior shoulder instability were included in this study. Exclusion criteria were shoulder instability in directions other than posterior, multidirectional instability (records of instability in more than one direction during physical examination or imaging), voluntary instability, dislocation of prostheses, (not healed) glenoid fractures other than bony Bankart lesions, bony Bankart lesions encompassing more than half of the glenoid length, shoulder dislocations associated with proximal humeral head fractures, and patients treated with arthroplasties. Furthermore, the patients with a follow-up of less than 12 months were excluded in order to detect possible recurrences. Of patients with a bilateral dislocation, only the first operated shoulder was included since the first procedure may influence the outcome of the second procedure. Baseline characteristics and outcome measures were collected using chart review. Baseline characteristics consisted of the demographic characteristics, cause of injury, practiced sport, operative procedure, and number of sutures/anchors/screws. Outcome data were comprised of return to sport rates, recurrence rates, revision rates, subjective instability, pain, range of motion (ROM), and complications. Recurrent instability was defined as a postoperative reported subluxation or a dislocation. Subjective instability was defined as instability felt by the patient, without reporting that the shoulder is dislocating or nearly dislocating, and without any subluxation during physical examination.
Operative procedures
All patients obtained radiographic imaging, a computed tomography scan, and/or a magnetic resonance imaging before the procedure to assess accompanying lesions. Soft-tissue procedures were only assessed including capsulolabral procedures, such as a labral repair, capsular repair, capsular plication, and capsular shift. The methods for these procedures at our hospital have been described before by Millett et al. (13). Patients were positioned in the lateral decubitus position. The patient was positioned on a long bean bag with the arm in 20° of abduction and 20° of extension facilitated by a traction device. Furthermore, 2-5kg was used to add lateral traction to the proximal humerus. After examination under general anesthesia, a posterior arthroscopic portal was made. This portal was positioned more lateral in comparison with the standard lateral portal for better access to the posterior labrum. Subsequently, an anterior portal was placed superolateral of the coracoid process. For the labrum and capsular repair, the capsulolabral sleeve was mobilized until it could be shifted superolateral onto the glenoid rim. Afterward, the glenoid neck was decorticated with a shaver to facilitate healing. In the next stage, anchors were placed on the articular rim from inferior to superior, and the labrum was repaired. During capsular plication and capsular shift, the posterior capsule was abraded to promote healing. Subsequently, the capsule was sutured with the labrum using a shuttling instrument to tighten the capsule. The shift began at 6 o’clock, whereafter the same was repeated at 7, 8, and 9 o’clock to tighten the posterior capsule. Following that, the anteroinferior capsule was tightened at the same manner at 4 and 5 o’clock.
Postoperative rehabilitation
Postoperative rehabilitation differed among patients; however, generally, shoulders were immobilized for the first two to six weeks, followed by physical therapy targeting supervised progression of active and passive range of motion. Strengthening exercises started at two to three months after surgery and return to collision sports was allowed at six months.
Statistical analysis
The clinical outcomes were summarized as absolute numbers with frequencies. All results were reported narratively. The study was approved by the IRB of the Massachusetts General Hospital under IRB number 2014P002065.
Results
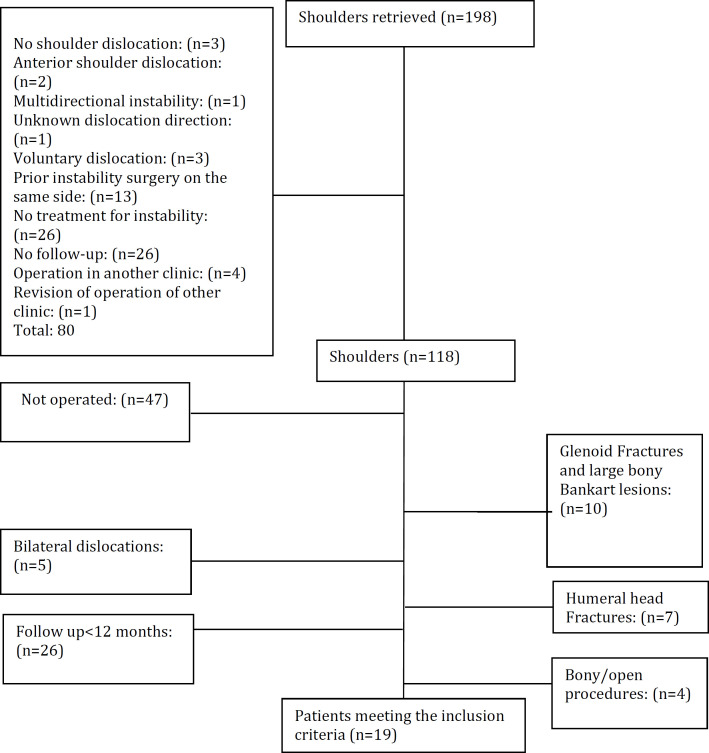
Out of 198 identified patients with a posterior shoulder dislocation, 19 cases met the inclusion criteria (Figure 1). Table 1 summarizes the demographic characteristics of these included 16 males and 3 females with a mean age of 34 years (age range: 19-69 years) and a mean follow-up of 35 months (13-105).
Figure 1.
Flow chart
Table 1.
Demographic characteristics
| N (%) | |||
|---|---|---|---|
| Number of patients | N patients | 19 | |
| Follow-up | 35 (13-105) | ||
| Gender | Male | 16 (87%) | |
| Female | 3 (13%) | ||
| Type of posterior instability | Dislocation | 5 (26%) | |
| Subluxation | 6 (32%) | ||
| Signs of previous dislocation | 5 (26%) | ||
| Subjective instability | 2 (11%) | ||
| Multiple episodes of instability | 1 (5%) | ||
| Sports | Recreational non-contact | 5 (26%) | |
| Recreational contact | 2 (11%) | ||
| Competitive non-contact | 1 (5%) | ||
| Competitive contact | 3 (16%) | ||
| No sports | 8 (42%) | ||
| Cause | Fall | 3 (16%) | |
| Sports related (collision) | 5 (26%) | ||
| Atraumatic | 5 (26%) | ||
| Motor vehicle accident | 1 (5%) | ||
| Lifting | 2 (11%) | ||
| Unknown | 3 (16%) | ||
| Arm | Right | 12 (63%) | |
| Left | 7 (37%) | ||
| Associated lesions on MRI/CT | Reverse Hill-Sachs | 1 (5%) | |
| Posterior Bankart lesion | 16 (84%) | ||
| Rotator cuff lesion | 2 (11%) | ||
| Arthrosis/cartilage loss | 5 (26%) | ||
| Previous dislocations (n) | 0 | 0 | |
| 1 | 9 (47%) | ||
| 2 | 0 | ||
| >3 | 5 (26%) | ||
| Unknown | 5 (26%) | ||
Recurrent instability and revisions
None of the patients suffered a recurrent dislocation; however, six patients had a recurrent subluxation (32%; Table 2).
Table 2.
Outcomes
| Total (N) | |
|---|---|
| Total number of patients | 19 |
| Redislocation | 0 |
| Resubluxation | 6 (32%) |
| Revision | 10 (53%) |
| Persistent pain | 11 (58%) |
| Subjective instability | 5 (26%) |
| Not feeling better after the procedure | 10 (53%) |
| Return to sports | 7 (78%)* |
* Return to sports was only reported in 9 patients
In total, 10 (53%) patients underwent a revision procedure. The mean time to recurrent subluxation was obtained at 19.4 months (range: 1.6-69 months), and the time to revision was estimated at 22 months (range: 3-77 months). There were nine patients who were referred from an outside hospital for a second opinion or for an expertise. Being referred by another hospital did not increase the recurrent subluxation (n=3; 16%) or revision rates (n=5; 26%).
The reasons for revision were trauma after operation in three patients resulting in recurrence (n=2) and extreme pain (n=1), loss of ROM (n=1), osteoarthrosis (n=1), persistent instability (n=1), recurrent subluxation (n=1), rotator cuff tear (n=1), biceps tendinitis in combination with impingement (n=1), and biceps tendinitis/degeneration in combination with impingement and loss of ROM (n=1) (Table 3). The main revision procedures were biceps tenodesis with subacromial decompression (n=2), biceps tenodesis with subacromial decompression and rotator interval release (n=1), a rotator cuff repair with a subacromial decompression (n=1), capsular release (n=2), manipulation under anesthesia (n=1), posterior labrum repair (n=2) (one with a biceps tenodesis), and a glenoid reconstruction (n=1).
Table 3.
Interventions
| Primary operation | Reasons for revision | Revision procedures | Time to revision (months) |
|---|---|---|---|
| Posterior and superior labral repair | Fall resulting in persistent pain | Biceps tenodesis, extensive debridement, and subacromial decompression | 9.07 |
| Posterior and superior labral repair | Osteoarthrosis | Capsular release | 21.50 |
| SLAP repair and posterior labral repair | ROM loss, biceps tendinitis, and impingement | Extensive debridement, subacromial decompression, biceps tenodesis, capsular release, rotator interval release, coracoidoplasty, and subcoracoid decompression | 9.10 |
| Extensive debridement, subacromial decompression, biceps tenotomy | Rotator cuff tear | Rotator cuff repair, extensive debridement, and subacromial decompression | 3.33 |
| Posterior labral repair | ROM loss | Manipulation under anesthesia | 4.37 |
| Posterior labral repair | Recurrence due to trauma | Posterior bankart repair | 76.53 |
| Posterior and superior labral repair | Persistent instability | Glenoid reconstruction with bone graft and capsulolabral reconstruction | 7.80 |
| Capsular shift | Recurrence due to trauma | Posterior Bankart repair, biceps tenodesis, and extensive debridement | 27.27 |
| Capsular shift | Impingement biceps degeneration | Biceps tenodesis, extensive debridement, and subacromial decompression | 23.50 |
| Posterior and superior labral repair | Persistent pain and resubluxation | Capsular release and extensive debridement | 7.43 |
Subjective outcomes, return to sport rates, and range of motion
In total, 11 (58%) patients experienced persistent pain with onset during one year after the operation, and 5 (26%) cases experienced subjective instability; moreover, 10 (53%) patients reported not experiencing improvement after the operation, and out of 9 patients with available data on return to sport, 7 (78%) cases returned to sport (Table 2). Persistent pain, subjective feeling of instability, and not experiencing improvement did not increase recurrent subluxation rates (n=4, 21%; n=3, 16%; and n=4, 21%, respectively), nor did they increase revision surgery rates (n=7, 36%; n=1, 5%; and n=6, 32%, respectively). Out of 16 patients of whom the postoperative forward flexion is known, 12 cases had full forward flexion, 3 patients had a restriction of up to 120-150 degrees, and one case up to 90-120 degrees. Out of 14 patients of whom the external rotation was known, 5 cases had full external rotation, 2 patients had a restriction up to 50-70 degrees, 4 cases had a restriction up to 30-50 degrees, and 3 patients had a restriction up to 30 degrees. Furthermore, out of 14 patients of whom the internal rotation was known, 13 cases could internally rotate above the L3 spine level, and 1 patient had a restriction to the lateral thigh.
Complications
There were 7 (39%) patients with complications (Table 4). The most common complication was osteoarthrosis in 2 patients (11% of complications). One patient had a shoulder mass at the follow-up visits. An arthroscopic removal was indicated for further analysis. However, the patient was lost to follow-up afterwards.
Table 4.
Complications
| Complications | N |
|---|---|
| Total number of patients with a complication | 7 |
| Osteoarthrosis | 2(11%) |
| Adhesive capsulitis | 1 (5%) |
| Recurrent posterior Bankart lesion | 1 (5%) |
| Pain at incision site | 1 (5%) |
| Mass in shoulder | 1 (5%) |
| Degeneration of biceps with pain | 1 (5%) |
The patients with a complication were not more associated with a recurrent subluxation (n=2, 29%), subjective feeling of instability (n=2, 29%), and not feeling better after surgery (26%). There were more patients with persistent pain (n=6, 86%), and patients that required revision surgery (n=5, 71%) in the complication group.
Discussion
In the current study, 32%, 53%, and 37% of the patients had a recurrent subluxation, a revision, and a complication, respectively. Although forward flexion and internal rotation results were satisfactory, most of the patients (64%) had a restriction in external rotation. Factors that were related to less satisfactory outcomes could not be defined. Although our study is underpowered, it is believed that it is a good addition to the literature because studies assessing the results of soft-tissue procedures for the treatment of posterior instability are scarce. Moreover, our results show that the results are not always satisfactory, and therefore, it is important to inform the patients about these results. Due to the rarity of posterior instability, it is quite difficult to perform a well powered study, and the best possible evidence might come from systematic reviews summarizing these cohorts.
In this study, not only recurrence rates and revision rates were assessed, but also other relevant outcomes, such as return to sport rates, persistent pain, and complication rates were analyzed. The results of this study could be highly useful when taking decisions regarding the operative treatment for patients with posterior shoulder instability.
The results of this study have to be interpreted in the light of several limitations. First, due to the retrospective design of this study, the range of motion and return to sports were not reported for all patients. The amount of bone loss could only be retrieved for one patient. Second, this study is underpowered rendering it impossible to perform any statistical tests. Third, our study shows a much higher revision rates (53% versus 7.57%), and higher complication rates (37% versus 2.48%), compared to those in the literature (14). Furthermore, our recurrence rate of 32% is higher than the average of 7.4% recurrence rate reported by a recent systematic review by Longo et al. (15). The results of systematic review show that although recurrence rates are thoroughly reported, most of the articles have not reported on complications. A recent systematic review assessing return to sport has shown similar return to sport rates (78% versus 62.7-100%) (16). The differences in recurrence, revision, and complication rates could be attributed to the fact that the results were assessed in a tertiary hospital which was consulted for many second opinions and treats more complex pathology, which could skew the data to a less satisfactory result. Although instability rates were not higher in patients referred from outside hospitals, patients with more complex pathology could preferentially choose to be seen in this hospital.
Future studies should aim to collect their data prospectively and compare soft-tissue and bony operation types, ensuring that all the data for all patients, including quantification of glenoid and humeral bone loss will be available, and have a large number of patients to be able to detect even small differences between the operation groups. However, due to the rarity of posterior instability, this might be a difficult task and multicenter studies and/or systematic reviews would be necessary to be able to draw any clear conclusion. Based on current results, patients should be informed about a relatively high complication rate after soft-tissue posterior instability surgery.
Conclusion
There is a high rate of recurrent instability, need for revision, and complications after soft-tissue posterior instability surgery. Postoperative external rotation was impaired in most patients. Patients should be informed about these unsatisfactory results.
Contribution of authors:
H. Alkaduhimi has contributed to the conceptualization, methodology, data acquisition, analysis of data, writing and reviewing this study; NFJ Hilgersom has contributed to the conceptualization, methodology, data acquisition, analysis of data, writing and reviewing; D. Eygendaal has contributed to the supervision and reviewing; MPJ van den Bekerom has contributed to the conceptualization, methodology, supervision and reviewing; LS Oh has contributed to the conceptualization, methodology and supervision.
Conflict of interest:
There is no conflict of interest in this study.
Acknowledgment
James W. Connelly is a native English speaker with experience in medical writing. He has edited the paper linguistically.
References
- 1.Robinson CM, Seah M, Akhtar MA. The epidemiology, risk of recurrence, and functional outcome after an acute traumatic posterior dislocation of the shoulder. J Bone Joint Surg Am [Internet] 2011;93(17):1605–13. doi: 10.2106/JBJS.J.00973. [DOI] [PubMed] [Google Scholar]
- 2.Cicak N. Posterior dislocation of the shoulder. J Bone Jt Surg Br. 2004;86(3):324. doi: 10.1302/0301-620x.86b3.14985. [DOI] [PubMed] [Google Scholar]
- 3.Perron a D, Jones RL. Posterior shoulder dislocation: avoiding a missed diagnosis. Am J Emerg Med. 2000;18(2):189–91. doi: 10.1016/s0735-6757(00)90017-2. [DOI] [PubMed] [Google Scholar]
- 4.Tan AH. Missed posterior fracture-dislocation of the humeral head following an electrocution injury to the arm. Singapore Med J [Internet] 2005;46(4):189–92. [PubMed] [Google Scholar]
- 5.Hashmi FR, Pugh M, Bryan S. Simultaneous bilateral posterior dislocation of shoulder. Am J Emerg Med. 2002;20(2):127. doi: 10.1053/ajem.2002.31132. [DOI] [PubMed] [Google Scholar]
- 6.Rouleau DM, Hebert-Davies J. Incidence of Associated Injury in Posterior Shoulder Dislocation. J Orthop Trauma [Internet] 2012;26(4):246–51. doi: 10.1097/BOT.0b013e3182243909. [DOI] [PubMed] [Google Scholar]
- 7.Antosh IJ, Tokish JM, Owens BD. Posterior Shoulder Instability. Sports Health [Internet] 2016 Nov;8(6):520–6. doi: 10.1177/1941738116672446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Balg F, Boileau P. The instability severity index score A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Jt Surg Br. 2007;89(11):1470–7. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 9.Poehling-Monaghan KL, Krych AJ, Dahm DL. Arthroscopic Repair of a Posterior Bony Bankart Lesion. Arthrosc Tech [Internet] 2015 ;4(6):e669–73. doi: 10.1016/j.eats.2015.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brelin A, Dickens JF. Posterior Shoulder Instability. Sports Med Arthrosc [Internet] 2017;25(3):136–43. doi: 10.1097/JSA.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 11.Jain SR, Sayampanathan AA, Hwee Chye Tan A. Arthroscopic management of posterior instability of the shoulder: A systematic review of predictive factors associated with poorer surgical outcomes. J Orthop Surg [Internet] 2017 Sep;25(3):230949901774310. doi: 10.1177/2309499017743102. [DOI] [PubMed] [Google Scholar]
- 12.Garret J, Nourissat G, Hardy MB, Antonucci D, Clavert P, Mansat P, et al. Painful posterior shoulder instability: Anticipating and preventing failure A study in 25 patients. Orthop Traumatol Surg Res. 2017;103(8S):S199–202. doi: 10.1016/j.otsr.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Millett PJ, Clavert P, Warner JJP. Arthroscopic management of anterior, posterior, and multidirectional shoulder instability: pearls and pitfalls. Arthroscopy. 2003;suppl 1:86–93. doi: 10.1016/j.arthro.2003.09.031. [DOI] [PubMed] [Google Scholar]
- 14.DeLong JM, Jiang K, Bradley JP. Posterior Instability of the Shoulder: A Systematic Review and Meta-analysis of Clinical Outcomes. Am J Sports Med [Internet] 2015;43(7):1805–17. doi: 10.1177/0363546515577622. [DOI] [PubMed] [Google Scholar]
- 15.Longo UG, Ciuffreda M, Locher J, Casciaro C, Mannering N, Maffulli N, et al. Posterior shoulder instability: a systematic review. Br Med Bull. 2020;134(1):34–53. doi: 10.1093/bmb/ldaa009. [DOI] [PubMed] [Google Scholar]
- 16.Fried JW, Hurley ET, Duenes ML, Manjunath AK, Virk M, Gonzalez-Lomas G, et al. Return to Play After Arthroscopic Stabilization for Posterior Shoulder Instability-A Systematic Review. Arthrosc Sport Med Rehabil. 2020;3(1):e249–56. doi: 10.1016/j.asmr.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]