Abstract
Background:
Distal pole scaphoid resection (DPSR) is an effective way to manage chronic scaphoid non-union with limited degenerative arthritis. Studies have reported positive results in terms of pain relief, wrist range of motion and grip strength, and patient satisfaction. However, the biomechanical consequences of DPSR remain unclear. This study evaluates the effects of DPSR on carpal mechanics by assessing changes in radiographic parameters with varying quantities of scaphoid removal.
Methods:
Six fresh frozen cadaveric upper extremities were used. Resections of 25%, 50%, and 75% of the length of each scaphoid were performed under fluoroscopic image guidance. For the intact scaphoid and each resection level, the following radiographic parameters were assessed: radiolunate and capitolunate angles; carpal height and first metacarpal subsidence ratios, and ulnar carpal translation. Measurements were then repeated for grip and pinch as well as radial and ulnar wrist deviation positions. Radial styloid to trapezium distance in wrist radial deviation was also measured to assess for impingement.
Results:
There was a statistically significant increase in the mean radiolunate angle with increasing scaphoid resection quantities. No statistically significant correlations were found between radial styloid clearance and increasing scaphoid resection percentages. Changes in the remaining variables did not reach statistical significance.
Conclusion:
Increasing levels of scaphoid resection is associated with progressive signs of carpal malalignment best depicted by increasing radiolunate angles. Diminishing radial styloid clearance was clinically evident as more scaphoid was resected. For this, prophylactic radial styloidectomy may be considered to avoid bony impingement.
Key Words: Distal Pole Scaphoid, Radiolunate, Nonunion
Introduction
Malerich and colleagues popularized DPSR as an effective way to manage the painful chronic scaphoid non-union with limited degenerative arthritis (1). Other treatment options include, but are not limited to, proximal row carpectomy, scaphoid excision with selective intercarpal fusion, and total wrist arthrodesis. Comparatively, DPSR is a technically simpler procedure which has been shown to provide patients with reliable pain relief while preserving wrist range of motion and grip strength. In addition, DPSR foregoes the need for long-term immobilization and has potential cost-saving benefits by precluding the need for fusion and its associated implants. However, the biomechanical consequences of removing the distal scaphoid remains poorly understood and is only partially described in a limited number of investigations. Midcarpal arthrosis and increasing radiolunate angles are radiographic findings which have been described in the literature following DPSR, raising concerns for carpal instability or the loss of the ability to maintain internal joint congruency of the wrist under functional loads (2-4). Carpal instability non-dissociative (CIND) pattern – that is, a form of carpal instability caused by dysfunction between the proximal and distal row of the wrist or between the radius and proximal row – associated with worsening dorsal intercalated segment instability (DISI) pattern (characterized by radiolunate angle > 15°) has been reported by Garcia-Elias et al in 12 out of 21 patients who underwent distal scaphoid excision (5). Reassuringly, the authors of these investigations have not found any correlations between these radiographic observations and patient clinical outcomes (2-5). How DPSR can potentiate CIND-DISI is likely a multifactorial process partially explained by etiologies ranging from scaphoid resection resulting in loss of the scapho-trapezio-trapezoid (STT) ligamentous constraints and scaphoid resection resulting in loss of intrinsic force couples on the intact scaphoid (6-8). The exact mechanism(s) remain unclear and so the purpose of our study is to evaluate the effects of DPSR on carpal mechanics by assessing changes in radiographic parameters after varying percentages of distal scaphoid resection. We hypothesized that increasing percentages of scaphoid resection correlates with worsening radiographic signs of carpal collapse.
Materials and Methods
Six fresh frozen cadaveric upper extremities including the wrist, forearm, and elbow were prepared according to institutional protocols. They were thawed at room temperature and affixed to wooden supports with two screws placed through each radius. The wrist and forearms were positioned in neutral while the elbows were flexed to 90°. A dorsal approach was used to expose the scaphoid as described by Malerich et al (1). The dorsal wrist capsule was divided in line with the mid-dorsal intercarpal and mid-dorsal radiocarpal ligaments to create a radially-based flap as described by Berger et al (9). During our dissections, care was taken to avoid damaging the scapholunate ligament which was manually probed to confirm its integrity. Three 0.045’’ Kirschner wires were driven into the radial aspect of the intact scaphoids to mark planned resection levels of 25, 50, and 75% of each scaphoid length [Figure 1].
Figure 1.
(a) Anterior to posterior view of dorsal scaphoid exposure and Kirschner wire placement for scaphoid resection planning. (b) Lateral view. (c) Anterior to posterior radiograph showing Kirschner wires delineating planned scaphoid resections levels of 25, 50, and 75%.
Grip and pinch forces were replicated and based on in-vivo estimations of flexor tendon forces as measured by Schiund et al (10). To reproduce these forces, weights were mounted onto hooks attached to multiple, high-tensile strength suture loops (#2 FiberWire, Arthrex, Naples, FL) affixed to the wrist and finger flexor and extensor tendons. To simulate pinch, 2 and 10-kilogram weights were attached to the flexor pollicis longus (FPL) and flexor digitorum profundus (FDP) tendons respectively. Grip was simulated by attaching a 1-kilogram weight to the FPL tendon and a 5-kilogram weight to the FDP and flexor digitorum superficialis (FDS) tendons altogether. A total of 9 kilograms was attached around the tendons of the extensor digitorum communis (EDC) to help maintain an unassisted neutral wrist position.
For the intact scaphoid and each resection level, radiographic parameters were manually measured from printed images using a mini fluoroscopy machine (FD OR, Orthoscan, Inc. Scottsdale, AZ). Magnification disparities were proportionally adjusted by using an overlaid coin (quarter dollar) with a known diameter of 24.26 millimeters.
The following radiographic variables were measured. The radiolunate angle is subtended by a line tracing the long axis of the radius and a line bisecting the sagittal profile of the lunate. The capitolunate angle is subtended by a line tracing the long axis of the capitate and a line bisecting the sagittal profile of the lunate. Radiolunate and capitolunate angles were used as an index for DISI. Carpal height ratio was measured by dividing the carpal height (length between the distal radial cortical margin and the base of the third metacarpal on a posterior-anterior view) by the length of the capitate as described by Nattrass et al (11). First metacarpal subsidence ratio was measured in accordance to Soejima’s method by dividing the scaphoid resection height by the length of the first metacarpal (12). Ulnar carpal translation was measured as the percentage of lunate width uncovered by the lunate facet of the distal radius on a posterior-anterior view as described by Gilula and Weeks (13). Radial styloid clearance was assessed on a wrist posterior-anterior view as the length between the proximal-most face of the trapezium and the tip of the radial styloid in maximum wrist radial deviation. Wrist radial and ulnar deviation actions were manually performed by the same experimenter without changes to tendon-weight unit distribution.
After completing measurements for the intact scaphoids, the distal 25% of each scaphoid was resected with an oscillating saw and all measurements were repeated. Tendon loading by weight was unaltered. This process was also repeated with distal pole scaphoid resections at the 50% and 75% level [Figure 2]. Two experimenters performed these measurements which were then averaged.
Figure 2.
(a) Anterior to posterior view of a wrist in neutral in neutral position following 25% distal scaphoid resection. (b) Following 50% distal scaphoid resection. (c) Following 75% distal scaphoid resection
Statistical analysis was performed using repeated measures ANOVA at P <0.05 using SPSS version 22 (IBM Aramonk, NY).
Results
Increasing levels of scaphoid resection is associated with a statistically significant increase in radiolunate angles with a mean of 15° at 0% resection to a mean of 32° at 75% resection (P = 0.01) [Figure 3]. A post-hoc analysis using ANOVA with Bonferroni correction examining interval changes in radiolunate angles after scaphoid excision between 0 to 25%, 25 to 50%, and 50 to 75% showed no statistical significance. Mean capitolunate angles also increased from 9° at 0% resection to 23° at 75% resection; however, this variable did not reach statistical significance (P = 0.13). Distance between the radial styloid and trapezium in wrist radial deviation decreased with increasing scaphoid resection with noted clinical impingement on 2 out of 6 cadaveric specimens after 75% scaphoid resection and 1 out of 6 cadaveric specimens after 50% scaphoid resection; however, this variable did not achieve statistical significance. First metacarpal subsidence, carpal height ratio, and percentage of ulnar carpal translation did not show statistically significant changes with increasing scaphoid resection [Table 1].
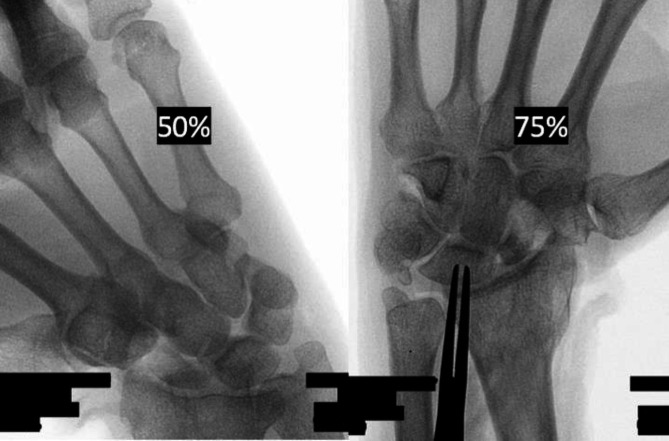
Figure 3.
Lateral view of a cadaveric wrist demonstrating radiolunate angle measurement prior to scaphoid resection (left) and following 75% scaphoid resection (right)
Table 1.
Measurement of the radiographic criteria after incremental distal pole scaphoid resection using Repeated Measure ANOVA (n=6 cadaver arms)
| Radiolunate angle, degree | Mean (SD) | P value | Radial styloid-Trapezium Distance | Mean (SD) mm | P value | |||
| 0% | 15 (3.3) | 0.013 | 0% | 12 (2.2) | 0.136 | |||
| 25% | 21 (2.5) | 25% | 10 (1.8) | |||||
| 50% | 25 (2.8) | 50% | 5.5 (2.0) | |||||
| 75% | 32 (3.4) | 75% | 3.6 (2.0) | |||||
| Capitolunate angle, degree | Ulnar carpal translation with Grip | |||||||
| 0% | 8.5 (2.4) | 0.129 | 0% | 30 (3.4) | 0.847 | |||
| 25% | 11 (3.4) | 25% | 32 (2.3) | |||||
| 50% | 18 (2.7) | 50% | 32 (2.8) | |||||
| 75% | 23 (5.0) | 75% | 34 (2.4) | |||||
| Carpal height ratio with Grip | Ulnar carpal translation with Pinch | |||||||
| 0% | 0.68 (0.006) | 0.187 | 0% | 28 (3.1) | 0.592 | |||
| 25% | 0.71 (0.023) | 25% | 30 (2.7) | |||||
| 50% | 0.73 (0.011) | 50% | 34 (2.2) | |||||
| 75% | 0.73 (0.013) | 75% | 40 (5.2) | |||||
| Carpal height ratio with Pinch | Ulnar carpal translation with Radial deviation | |||||||
| 0% | 0.68 (0.01) | 0.135 | 0% | 38 (4.4) | 0.823 | |||
| 25% | 0.70 (0.03) | 25% | 39 (3.9) | |||||
| 50% | 0.72 (0.03) | 50% | 31 (7.1) | |||||
| 75% | 0.72 (0.02) | 75% | 44 (5.8) | |||||
| Subsidence ratio with Grip | Ulnar carpal translation with Ulnar deviation | |||||||
| 0% | 0.76 (0.03) | 0.552 | 0% | 25 (3.0) | 0.098 | |||
| 25% | 0.73 (0.01) | 25% | 27 (4.1) | |||||
| 50% | 0.70 (0.04) | 50% | 25 (4.0) | |||||
| 75% | 0.74 (0.03) | 75% | 22 (3.7) | |||||
| Subsidence ratio with Pinch | ||||||||
| 0% | 0.77 (0.03) | 0.283 | ||||||
| 25% | 0.76 (0.01) | |||||||
| 50% | 0.70 (0.03) | |||||||
| 75% | 0.72 (0.03) | |||||||
Discussion
DPSR is an effective way to treat the painful chronic scaphoid non-union with concurrent radioscaphoid and even capitolunate arthritis (12). It is a technically simple procedure which can provide patients with favorable clinical outcomes and low rates of long-term complications as compared to alternative procedures like proximal row carpectomy, scaphoid excision with selective intercarpal fusion, and total wrist arthrodesis (14). These surgical options remain available in the event of DPSR failure. DPSR also foregoes the need for long-term immobilization and has potential cost-saving benefits by precluding the need for fusion and use of its associated implants. Malerich et al reported significant improvements in grip strength, wrist range of motion, and visual analog pain scale scores in 19 patients managed with DPSR and followed for 10 to 25 years (3). Ruch and colleagues also showed favorable results with significant gains in wrist range of motion and Disabilities of the Arm, Shoulder, and Hand (DASH) scores in 13 patients managed with DPSR after failed previous surgery (4). Similarly, Soejima et al reported significant improvements with wrist range of motion, grip strength, and modified Mayo clinical scores after a greater than one-year follow-up period for 9 patients with chronic, symptomatic scaphoid nonunion with concomitant distal radioscaphoid and capitolunate arthritis (12).
Though the literature supports its clinical efficacy, subtle radiographic carpal collapse following DPSR has been reported and can be discerned by increases in DISI and radiolunate angles and decreases in carpal height ratios (3, 15). Ruch et al reported a statistically significant increase in the mean radiolunate angle from 10.2° +/- 6.2° before distal scaphoid excision to 13.8° +/- 7.5° after excision; additionally, 2 patients were noted to have DISI (radiolunate angles >15.0°) prior to resection while 6 patients demonstrated DISI deformity after resection (4). In their 20-year report, Malerich and colleagues showed a 4% decrease in carpal height ratio from 1.42 pre-excision to 1.37 post-excision and a mean increase in radiolunate angle from -29° to -33°; however, statistical relevance was not reported (3). Soejima and colleagues reported an overall increase in radiolunate and decrease in carpal height ratios after DPSR, but neither variables reached statistical significance (12). In his study group, Garcia-Elias observed CIND-DISI deformities in 12 of 21 patients following distal scaphoid excision for STT arthritis (15). While these findings do not negate the overall positive clinical outcomes following DPSR, they do temper enthusiasm for DPSR.
In a cadaveric study examining the effects of the dorsal intercarpal (DIC) ligaments on lunate extension after distal scaphoid excision, Kamal et al measured statistically significant amounts of lunate extension after only excising 5-mm of bone from the distal scaphoid while leaving the DIC intact (7). DPSR for scaphoid non-union usually involves larger amounts of scaphoid resection and whether the resultant larger defect predisposes the carpus to greater degrees of carpal malalignment compared to that seen by Kamal has not, to our knowledge, been the subject of a biomechanical study. In our investigation, we found a statistically significant increase in the mean radiolunate angle after resecting 75% of the distal scaphoid, increasing from 15° to 32°. A post-hoc analysis using ANOVA with Bonferroni correction examining interval changes in radiolunate angles after scaphoid excision between 0 to 25%, 25 to 50%, and 50 to 75% showed no statistical significance. We attributed these findings to the study’s small sample size.
Several mechanisms describe how distal scaphoid excision can affect radiolunate angles. Tay et al showed that in the absence of scapholunate interosseous ligament pathology, disruption of the STT ligamentous complex unlinks the scaphoid from distal tethers which maintain its inherent flexed posture; this allows dorsiflexion forces to act unimpeded across the lunate resulting in worsening DISI (8). Garcia-Elias et al explained that when the wrist is loaded, the scaphoid rotates into flexion owing to the interface between its oblique shape and axial forces from the trapezium and trapezoid. Comparatively, under the same load, triquetrum rotates into extension when experiencing axial forces from the 4th and 5th metacarpals via the hamate. These opposing forces are tension-balanced much like a spring through the scapholunate ligament, lunate, and lunotriquetral ligament. Any diminishment of the scaphoid lever arm – as entailed by DPSR – diminishes the radial-sided flexion force couple which allows an ulnar-sided extension moment to predominate across the wrist (6, 15). DPSR effectively sacrifices both anatomic relationships and as demonstrated in our study, the minimum set resection level of 25% was sufficient to produce lunate extension beyond 15° in all specimens. DISI should be expected after DPSR and more proximal resections generally appear to correlate with worsening radiolunate angle measurements. Kamal et al showed that when the distal scaphoid is resected, the DIC ligaments act as secondary checkreins against excessive lunate extension (7). In a cadaveric study, Mitsuyasu et al also emphasized the importance of the DIC ligament integrity in preventing DISI deformity (16). More proximal scaphoid resection levels risk violating the DIC ligament insertions onto the dorsal scaphoid groove resulting in worsening radiolunate malalignment.
We expected to see statistically significant changes in the amount of ulnar carpal translation after distal scaphoid resection especially after 50% resection as this would risk compromising the mid-scaphoid traversing fibers of the RSC ligament which play an important role in preventing ulnar drift (17). While this value did not demonstrate any statistically significant change, there was a numerical trend towards increasing ulnar carpal translation with larger quantities of scaphoid resection. We were also unable to extrapolate whether resection levels greater than 50% resulted in any significant amount of ulnar carpal translation as compared to a resection level of 25%.
There were no statistically significant changes in 1st metacarpal subsidence and carpal height ratios with increasing scaphoid resection quantities. For both variables, grip and pinch were assessed because grip strength is often used as an outcome index following wrist surgery while pinch actions generate forces across the scaphotrapezoid-trapezial (STT) articulation which can theoretically cause thumb metacarpal subsidence in a scaphoid-deficient wrist. Despite this, there was no clear numerical trend towards increasing 1st metacarpal subsidence or carpal height ratios after DPSR. An intact capitolunate column and the preserved ligamentous structures between capitate, trapezoid, and trapezium may prevent shortening of the carpus and subsidence of the 1st metacarpal respectively. In Soejima’s 5-year follow-up study of 9 patients, there were no statistically significant changes in 1st metacarpal subsidence and carpal height ratios following DPSR (12).
We defined radial styloid clearance as the distance between the tip of the radial styloid and the proximal-most face of the trapezium in maximum wrist radial deviation on an anterior-posterior image. This variable showed a numerically decreasing trend as more scaphoid was resected; however, this was statistically insignificant. Despite this, we found clinically apparent bony impingement in 2 of 6 specimens after 75% distal scaphoid resection and in 1 of 6 specimens after 50% distal scaphoid resection [Figure 4]. Implicitly, we feel that radial styloid clearance should be clinically assessed for during DPSR especially after resection of greater than or equal to 50% of the scaphoid. Prophylactic radial styloidectomy following DPSR should be considered to circumvent potential issues arising from bony impingement.
Figure 4.
(a) Fluoroscopic image demonstrating bony impingement after 50% distal scaphoid resection with the wrist positioned in radial deviation. (b) Bony impingement after 75% scaphoid resection from a separate specimen
The results of our study need to be interpreted carefully after considering several shortcomings. First, a small sample size underpowered the study and hindered our ability to draw statistical conclusions from the data set despite some telling numerical trends. Second, we did not account for any pre-existing wrist pathology amongst the specimens used for the purposes of this study; however, we did not encounter any obvious derangement of ligament, bone, or the relationship between ligament and bone throughout our dissections and fluoroscopic examinations. Third, replicating physiologic forces across the wrist via attaching differential weights to collective tendon groups can mute any subtle influences from individual tendon force vectors which could lead to either an overrepresentation or underrepresentation of certain radiographic changes. Fourth, the dorsal capsular exposure was left unrepaired which may potentially exaggerate the magnitude of radiographic changes with increasing scaphoid resection. Fifth, due to the nature of the study, we were limited only to observations of immediate or acute changes about the wrist following scaphoid resection. Undoubtedly, the biomechanical consequences from additional undue stresses imparted by scaphoid resection on the surrounding soft tissue anatomy of the wrist may not reveal the entirety of its effect until the long-term.
DPSR is an effective means for treating the difficult chronic scaphoid nonunion with limited degenerative arthritis and warrants a closer look at its effect(s) on the wrist. Increasing quantities of scaphoid resection results in a trend suggestive for CIND-DISI carpal malalignment best depicted by changes in radiolunate angles. We also found that scaphoid resection quantities of up to 75% did not lead to loss of the ability of the carpus to maintain internal joint congruency under simulated loads; however, this observation must be considered with caution due to the study’s limitations. Secondarily, we found that increasing quantities of scaphoid resection results clinically diminishing radial styloid clearance and bony impingement in 3 out of 6 specimens. For this, we strongly recommend always performing intraoperative assessments for radial styloid impingement following DPSR and if deemed necessary, a concomitant radial styloidectomy may be performed. Despite the benefits of DPSR for the management of chronic scaphoid nonunions, this topic remains relatively scarce in the body of literature. We hope this investigation generates more interest in DPSR not only as a surgical option, but as a topic of research particularly in further expounding on its effects on wrist biomechanics involving larger sample sizes; on the effects of radial styloidectomy in avoiding impingement after DPSR; and even on cost-analysis comparisons to other accepted surgical treatments.
Statements
The authors declare that there is no conflict of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent was not needed for this cadaveric study.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Malerich MM, Littler JW, Eaton R. Distal scaphoid resection arthroplasty for the treatment of patients with degenerative arthritis secondary to scaphoid nonunion. Tech Hand Up Extrem Surg. 2002;6(2):98–102. doi: 10.1097/00130911-200206000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Elias M, Lluch A. Partial excision of scaphoid: is it ever indicated? Hand clinics. 2001;17(4):687–95. [PubMed] [Google Scholar]
- 3.Malerich MM, Catalano LW, Weidner ZD, Vance MC, Eden CM, Eaton RG. Distal scaphoid resection for degenerative arthritis secondary to scaphoid nonunion: a 20-year experience. J Hand Surg Am. 2014;39(9):1669–76. doi: 10.1016/j.jhsa.2014.05.031. [DOI] [PubMed] [Google Scholar]
- 4.Ruch DS, Papadonikolakis A. Resection of the scaphoid distal pole for symptomatic scaphoid nonunion after failed previous surgical treatment. J Hand Surg Am. 2006;31(4):588–93. doi: 10.1016/j.jhsa.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Elias M, Lluch A, Saffar P. Distal scaphoid excision in scaphoid-trapezium-trapezoid arthritis. Tech Hand Up Extrem Surg. 1999;3(3):169–73. doi: 10.1097/00130911-199909000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Garcia-Elias M. Kinetic analysis of carpal stability during grip. Hand Clin. 1997;13(1):151–8. [PubMed] [Google Scholar]
- 7.Kamal RN, Chehata A, Rainbow MJ, Llusá M, Garcia-Elias M. The effect of the dorsal intercarpal ligament on lunate extension after distal scaphoid excision. J Hand Surg Am. 2012;37(11):2240–5. doi: 10.1016/j.jhsa.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 8.Tay SC, Moran SL, Shin AY, Linscheid RL. The clinical implications of scaphotrapezium-trapezoidal arthritis with associated carpal instability. J Hand Surg Am. 2007;32(1):47–54. doi: 10.1016/j.jhsa.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 9.Berger RA, Bishop AT, Bettinger PC. New dorsal capsulotomy for the surgical exposure of the wrist. Ann Plast Surg. 1995;35(1):54–9. doi: 10.1097/00000637-199507000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Schuind F, Garcia-Elias M, Cooney WP, An KN. Flexor tendon forces: in vivo measurements. J Hand Surg Am. 1992;17(2):291–8. doi: 10.1016/0363-5023(92)90408-h. [DOI] [PubMed] [Google Scholar]
- 11.Nattrass GR, King GJ, McMurtry RY, Brant RF. An alternative method for determination of the carpal height ratio. J Bone Joint Surg Am. 1994;76(1):88–94. doi: 10.2106/00004623-199401000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Soejima O, Iida H, Hanamura T, Naito M. Resection of the distal pole of the scaphoid for scaphoid nonunion with radioscaphoid and intercarpal arthritis. J Hand Surg Am. 2003;28(4):591–6. doi: 10.1016/s0363-5023(03)00181-3. [DOI] [PubMed] [Google Scholar]
- 13.Gilula LA, Weeks PM. Post-traumatic ligamentous instabilities of the wrist. Radiology. 1978;129(3):641–51. doi: 10.1148/129.3.641. [DOI] [PubMed] [Google Scholar]
- 14.Saltzman BM, Frank JM, Slikker W, Fernandez JJ, Cohen MS, Wysocki RW. Clinical outcomes of proximal row carpectomy versus four-corner arthrodesis for post-traumatic wrist arthropathy: a systematic review. J Hand Surg Eur Vol. 2015;40(5):450–7. doi: 10.1177/1753193414554359. [DOI] [PubMed] [Google Scholar]
- 15.Garcia-Elias M, Lluch AL, Farreres A, Castillo F, Saffar P. Resection of the distal scaphoid for scaphotrapeziotrapezoid osteoarthritis. J Hand Surg Br. 1999;24(4):448–52. doi: 10.1054/jhsb.1999.0169. [DOI] [PubMed] [Google Scholar]
- 16.Mitsuyasu H, Patterson RM, Shah MA, Buford WL, Iwamoto Y, Viegas SF. The role of the dorsal intercarpal ligament in dynamic and static scapholunate instability. J Hand Surg Am. 2004;29(2):279–88. doi: 10.1016/j.jhsa.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Berger RA. The ligaments of the wrist A current overview of anatomy with considerations of their potential functions. Hand Clin. 1997;13(1):63–82. [PubMed] [Google Scholar]