Abstract
Background:
Several treatment modalities have been reported to minimize the recurrence after surgical treatment of benign bone cysts. In this study, we evaluated local tumor control, recurrence rate, and bone healing of benign bone cysts after treatment with a simple technique, percutaneous curettage and a local autologous cancellous bone graft.
Methods:
Retrospective analysis of the records of 16 patients diagnosed with benign bone cysts between 2003 and 2010. We documented the demographic data, radiographic signs of healing (progressive decrease in radiolucency, remineralisation, ossification, consolidation of the cyst, and reconstitution of the bone), healing rate, postoperative complications, and recurrence.
Results:
Seven of the 16 patients (43.75%) were diagnosed with a simple bone cyst (SBC), while nine (56.25%) had an aneurysmal bone cyst (ABC). On average, radiographic signs of healing were present within 3–6 months, but in two patients these signs presented after 16 months. During the follow-up period, there was no difference in the healing rate between patients with SBC and ABC; no signs of deep or superficial wound infection, no postoperative fracture, and no recurrence in any case over an average of 6.3 years of follow-up.
Conclusion:
Treatment of benign bone cysts (SBC/ABC) with minimally invasive percutaneous curettage and a local autologous cancellous bone graft is a simple and effective modality with a promising outcome in the local control of recurrence and in enhancing bony consolidation.
Key Words: Percutaneous curettage, autologous, bone graft, bone cysts, simple bone cyst, aneurysmal bone cyst, recurrence
Introduction
Aneurysmal bone cysts (ABCs) and simple bone cysts (SBCs) are considered the most common bone lesions in children and young adolescents; however, the underlying aetiological factors differ (1,2). The main aims of treatment are pain relief, healing promotion, and prevention of adverse complications like recurrence and pathologic fracture (3).
Traditionally, the main treatment options for SBCs include bone marrow injection, curettage and autologous bone grafting, intralesional steroid injections, demineralised bone matrix allograft or calcium-phosphate bone cement, decompression and internal fixation or other minimally invasive procedures (4-11).
Various treatment options for ABCs have been described, including surgical resection or curettage, with or without bone grafting, and optional adjuvant therapies such as argon beam, phenol, ethanol, cryotherapy, and poly methyl methacrylate bone cementing of the cavity (12-14).
Conventional surgical procedures are often associated with high morbidity due to intraoperative bleeding, prolonged hospitalisation, and wound-related complications. Less invasive methods such as selective arterial embolization, calcitonin with methylprednisolone injection, sclerotherapy with ethibloc or polidocanol and systemic therapy with RANKL inhibitors (denosumab) have been reported (15-19).
It should be noted that ABCs present a spectrum of aggressiveness, and less invasive techniques may fail for more aggressive lesions. All of the treatment modalities have specific recommendations as well as associated advantages and disadvantages.
Despite the best efforts of various treatment methods, the rate of local recurrence is still unacceptably high after curettage and grafting or local adjuvants (20-21). Hence, local recurrence remains a challenge to orthopaedic surgeons.
As the management of ABCs continues to be distinctively challenging, there is still a pressing need for the development of new innovative therapies. Minimally invasive percutaneous therapy is expected to facilitate the surgery and decrease such undesirable complications.
The objective of this study was to evaluate the effectiveness and clinical outcome (local control and bone healing) of minimally invasive percutaneous curettage and local autogenous cancellous bone grafting for benign bone cysts in children and young adolescents.
Materials and Methods
We retrospectively reviewed the data of 16 patients confirmed to have benign bone cysts who were treated with percutaneous curettage and a local autologous cancellous bone graft. The data included hospital charts and records, histopathology and operative reports, as well as all relevant imaging. The analysed data comprised the demographic information (age, sex), anatomical location, clinical presentation, cyst index, previous treatments, histopathology results, postoperative complications, and the length of follow-up.
Plain radiographs were reviewed to determine the anatomic location, presence of pathological fracture, cyst size (cyst index), postoperative osseous healing, and the presence of local recurrence.
The size of the cyst was measured using the cyst index, calculated as the area of the cyst divided by the square of the external diameter of the normal diaphysis (22). The area of the cyst was determined from the area of a trapezoid drawn around the borders of the cyst on the initial anteroposterior radiograph of the affected part of the bone surrounding the cyst.
In all cases, the diagnosis was confirmed by histopathology. A cyst was considered active preoperatively if the patient was aged <12 years, if it was symptomatic with activities of daily living, had experienced a previous fracture, or if the cyst was abutting the physis (23). All cystic lesions were active and multilocular at the time of surgery.
Routine plain radiographs and magnetic resonance imaging (MRI) were performed for all patients [Figure 1]. Histopathologic examination of the specimen obtained from percutaneous biopsy confirmed the diagnosis of primary bone cyst. The staging of the cysts was performed using the Enneking radiological criteria for benign bone lesions: stage I (latent), well-defined margin and an intact cortex or defined margin and an intact cortex; stage II (active), relatively well-defined margin and thinned cortex or defined margin and thinned cortex; or stage III (aggressive), indistinct borders and overall cortical destruction (24). All patients were reviewed clinically and underwent conventional plain radiography imaging as follow-up on semiregular intervals. All patients underwent the same surgical treatment, and the healing of cysts was graded according to the Neer classification (25).
Figure 1.
showing the timeline images of case 7 table 2. Preoperative images showed left proximal femur cystic lesion (ABC) as appeared on AP radiograph (A) and T2-weighted MRI (B). The local graft is visible on radiograph taken one month after surgery (C). Follow-up showed sequential signs of healing as appeared on radiographs at 3 months (D), 8 months (E), and 24 months (F) postoperatively. Complete remodeling is evident on radiograph at 14 years (G)
Informed consent was obtained from all included patients and families to share their information and relevant images. This study was approved by our institutional review board.
Surgical technique
All cases were treated by the senior author under general anaesthesia with the use of a tourniquet if applicable. We used fluoroscopy to locate the cyst and the physis.
After full skin preparation and draping, one Jamshidi needle (size 16) was introduced into the proximal part of the cystic cavity, and a second one was inserted into the distal part. The cystic fluid was spontaneously evacuated and slowly aspirated to confirm the presence of straw-coloured, bloody sanguineous fluid, or frank blood.
One or two small skin punctures (1 cm in length) were made over the proximal or distal sites of the aspiration needles, leaving minimal skin scarring at maturity [Figure 2].
Figure 2.

Photograph of a 3-year-old-boy who had SBC treated twice, showing residual minimal scars at the entry portals of surgery at the age of 19 years
Under fluoroscopy control, a 5-mm Steinmann pin or 6-mm drill bit was advanced into the cyst cavity, and the cortical entry holes were manually enlarged to an area of around 1 cm2.
The cystic content, septations and the lining membrane were broken up using curettes of various sizes and shapes. They were subsequently removed by wide-bore metallic suction and sent to the pathology lab for routine histological examination. Care was taken not to damage the adjacent physis by curettage. After that, the cyst was irrigated with normal saline.
An angled curette or bent tip of a 5-mm Steinmann pin or 5-mm drill bit was used to open the intramedullary canal proximally and distally accordingly. Angled curettes were used to curette the local cancellous metaphyseal bone surrounding the cyst to fill the defect as possible.
The wounds were closed by simple 4/0 nylon suture. A protective sling was used by patients who underwent cyst removal from an upper limb. Patients with lower-extremity cysts were non-weight-bearing on crutches for 8 weeks, after which they gradually returned to full-weight-bearing function as tolerated.
Results
Demographic, clinical and radiological data
The study group included 10 male and 6 female children. The average age at the time of surgical treatment was 9.875 years (range 3–16 years,). Twelve patients were younger than 12 years.
Pain was the presenting factor in 10 (62.5%) patients, and pathologic fractures were seen in six (37.5%) patients.
Seven patients were diagnosed with SBCs [Table 1]. The mean age was 10.28 years (range 3–16 years). The most common site was the proximal humerus (five cases). The average preoperative cyst index was 4.84 (range 4.1–5.4). The average follow-up duration was 5.4 years (range 3–16 years). Nine patients were diagnosed with ABCs [Table 2].
Table 1.
Details of patients diagnosed with simple bone syst
| Age/year | Sex | Site | Clinical presentation | Cyst index | The onset of surgery after fracture | Follow up /year | |
|---|---|---|---|---|---|---|---|
| 1 | 11 | M | Proximal Humerus | Pathological fracture | 5.3 | 4 months | 4 |
| 2 | 3 | M | Proximal Humerus | Pathological fracture | 4.6 | 10 months | 16 |
| 3 | 9 | M | Proximal Humerus | Pathological fracture | 5.4 | 3 months | 3 |
| 4 | 12 | M | Proximal Humerus | Pathological fracture | 4.4 | 5 months | 3 |
| 5 | 6 | M | Proximal Humerus | Pathological fracture | 5.1 | 4 months | 6 |
| 6 | 16 | F | Lateral malleolus | Pain | 5.0 | - | 3 |
| 7 | 15 | F | Calcaneum | Pain | 4.1 | - | 3 |
Table 2.
Details of patients diagnosed with aneurysmal bone cyst
| Age /year | Sex | Site | Clinical presentation | Size / cm | Distance from the physis / cm | Enneking staging | Follow up /year | |
|---|---|---|---|---|---|---|---|---|
| 1 | 6 | F | Proximal Humerus | Pain | 4X4 | 2 | II | 3 |
| 2 | 8 | F | Proximal Humerus | Pain | 6x4 | 2 | II | 6 |
| 3 | 14 | F | Distal Radius | Pathological fracture | 3X2 | 2 | II | 5 |
| 4 | 11 | M | Distal Radius | Pain | 2X2 | 4 | III | 4 |
| 5 | 5 | M | Distal Femur | Painful limping | 7X2 | 5 | II | 3 |
| 6 | 5 | M | Distal Femur | Knee Pain | 6x5 | 3 | III | 8 |
| 7 | 10 | M | Proximal Femur | Painful limping | 6x3 | 4 | II | 14 |
| 8 | 11 | M | Proximal tibia | Knee Pain | 7x3 | 0 | II | 18 |
| 9 | 16 | F | Medial malleolus | Pain | 1.5x1.5 | Closed physis | I | 2 |
The mean age was 9.55 years (range 5–16 years). The distribution was as follows: two cases in the humerus, two in the radius, three in the femur, and two in the tibia. Six cases were active (Enneking type II) and three were aggressive (type III). All were at risk of fracture (width of the lesion was more than 70% of bone). The distance from the growth plate (for ABCs lesions) ranged between 0 and 5 cm, with a mean of 2.75 cm. The average follow-up duration was 7 years (range 2–18 years). Three of the children had received previous treatment for their bone lesions 6–12 months earlier at other hospitals, including a bone marrow injection [Case 1, Table 1], two steroid injections [Case 2, Table 2], open curettage and corticocancellous bone grafting [Case 6, Table 2, Figure 3].
Figure 3.
showing the timeline images of case 6 table 2. Preoperative AP radiograph showed large cystic lesion (ABC) at the right distal femur (A). Incomplete healing was evident after 3 months (B) and 12 months (C) of open curettage and corticocancellous autogenous graft. At this time the patient had the second surgery of percutaneous curettage and local autogenous cancellous bone graft. Follow-up showed sequential signs of healing as appeared on radiographs at 1 month (D), 4 months (E), 12 months (F), and 24 months (G) postoperatively. Complete remodeling is evident on radiograph at 8 years (H)
None of the treated children who initially presented with undisplaced fracture showed evidence of spontaneous healing after a mean of 5.2 months of conservative therapy.
Treatment outcomes
The mean clinical follow-up period for all patients was 6.3 years (range 2–18 years).
At 4-6 weeks postoperative, all patients were pain-free and had a full range of motion in the adjacent joints. Radiographic signs of cyst healing in response to the procedure were present at 3–6 months in 14 patients, while the remaining two patients showed no signs until 16 months.
Most of the cystic lesions (14 cases) were graded as Neer stage I and required a single surgical procedure.
The procedure was repeated after 10 months in two patients; one had a proximal humerus SBC and the second had a proximal tibia ABC, both abutting the growth plate [Figure 4 and 5]. Signs of healing were achieved in both patients 6 months after the second procedure, which was performed due to inadequate nearby healthy cancellous bone to initiate healing.
Figure 4.
showing the timeline images of case 2 table 1. Initial presenting radiograph showing large cystic lesion (SBC) in the proximal humeral metaphysis abutting the growth plate with a tiny breach in the upper medial cortex (A). subsequent radiographs failed to show complete healing and cyst resolution after 4 months (B), 9 months (C), and 12 months (D) of conservative management. At this time, the patient has the first percutaneous curettage and local autogenous cancellous bone graft (E; 3 months postoperatively). After 9 months of surgery, the cyst failed to heal completely but started to get away from the growth plate (F). The cyst recurred after 19 months of surgery (G). At this time, we performed the second procedure of percutaneous curettage and local autogenous cancellous bone graft. Follow-up showed sequential signs of healing as appeared on radiographs at 4 months (H), and 12 months (I) after the second surgery. Complete remodeling is evident on radiograph at 16 years (J)
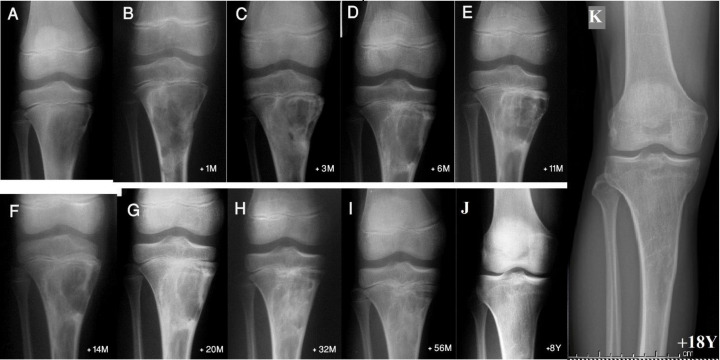
Figure 5.
showing the timeline images of case 8 table 2. Preoperative AP radiograph showed cystic lesion (ABC) at the right proximal tibial abutting the growth plate (A). Subsequent radiographs failed to show complete healing of the cyst after percutaneous curettage and local autogenous bone graft as appeared on images taken at 1 month (B), 3 months (C), 6 months (D), and 11 months (E) postoperatively. At this time, the patient had a second procedure of percutaneous curettage and local autogenous bone graft. Follow-up showed sequential signs of healing as appeared on radiographs at 3 months (F), 9 months (G), 21 months (H), and 45 months (I) after the second surgery. Complete remodeling is evident on radiograph at 7 years (J) and 17 years (K) after the second procedure
None of the patients developed deep or superficial wound infections. No intraoperative or postoperative complications (fractures or recurrence) occurred.
Discussion
This study highlights the results and safety of a percutaneous minimally invasive surgical technique in patients with benign bone cysts in variable anatomical locations. The safety of the procedure was assessed by evaluating the clinical outcomes and associated complications.
This technique maintains the structural integrity of the bone, minimising the risk of local soft tissue injury, and it maintains the periosteal sleeve of affected bones through the use of a small cortical opening. Thus, faster bone healing may be achieved with the help of the local surrounding osteogenic tissue.
Bone cysts, especially aneurysmal cysts, are characterised by their tenacity and prevalence of recurrence after treatment, which explains the diverse methods for achieving consolidation (21). Due to the high reoperation rate, excision remains the best form of surgical treatment; however, this often leads to considerable morbidity and impairment in the function of the extremities (15,16). The potential problems associated with surgical treatment include infection and growth plate injury, and the surgical approach is particularly difficult for lesions at certain sites.
Immobilisation is necessary following all open surgical procedures and may need to be prolonged for children with larger lesions, resulting in difficulties for the child and their family.
In this study, all patients who presented with pathologic fractures failed to show signs of healing after a mean of 5.2 months of conservative treatment; however, all patients who were treated with the procedure that we discussed were eventually healed.
Two patients required a repeat procedure 10 months after the initial surgery. Those cysts were abutting the growth plate. Thus, during the first operation, extra caution was taken to avoid damage to the growth plate. Besides, they
lacked sufficient local autologous cancellous bone despite opening the cyst into the medullary canal in the initial surgery. In both cases, the second operation revealed
minimal residual pathological tissue in the cyst, which indicates that bone cysts located near the growth plate can benefit from an initial surgical procedure to remove as much pathological tissue as possible. This will induce
partial healing and allow the cyst to move away from the growth plate, producing a zone of cancellous bone between the cyst and the growth plate and inducing partial ossification of the cyst. None of these cysts recurred on long-term follow-up.
Our results on the consolidation of cystic bone lesions are better than those reported in the literature (21,26).
The reduced rate of recurrence in this study may be attributed to the healing benefits of minimally invasive percutaneous curettage, the osteoblastic activity of the local autogenous cancellous bone graft, the osteoblasts in the inner layer of the periosteal wall, and the opening of channels to the bone marrow in the adjacent cancellous bone and medullary canal.
In the reported percutaneous surgical procedures, there is no mention of use of a local autologous cancellous graft to promote healing. This autologous graft is usually adequate as most bone cysts are localised in the highly vascular metaphyseal region.
Curettage of the surrounding cancellous bone to the cyst cavity leads to an increase in the vascularity of the region surrounding the cyst and opens all bone channels, stimulating the bone to build an alternative bridge from the healthy bone.
By opening the medullary canal proximal and distal to the cyst together with local cancellous grafting, local bone marrow can migrate to the cyst lesion. This enhances the healing process as human bone marrow contains osteoblastic progenitor cells that can differentiate into osteoblasts in vitro and into bone in vivo (27,28).
The time for complete remodelling until the normal bone tissue stage, with no remaining evidence of the cyst, ranged from 14 to 18 months in our series. However, it takes around 2 years according to reports in the literature (4,15,18). Complete healing has been reported to occur in 8–15 months (average 11.6 months) after surgical curettage and grafting procedure, and in 15–18 months (average 13.9 months) after treatment with injections (29). Differences in healing rates reported by various studies are probably due to the type of surgical procedure, patient age, location of the cyst, and the distance between the cyst and the growth plate. In all surgically treated patients, the cysts completely healed and none required further treatment to achieve bone consolidation. Our technique avoided the need to harvest a cancellous bone graft from the iliac crest or the use of allograft bone or bone substitutes.
Our technique may appear similar to the curopsy in principle; however, it includes complete curettage of the cyst in addition to local cancellous bone grafting and opening the medullary canal toward the lesion. The curopsy has been described by Reddy et al. (30) as a novel technique for treatment of ABCs. They reported a 19% recurrence rate of this technique and attributed their success toward the biased selection of smaller, less aggressive cysts. Although the sample size of our study is small, we reported no recurrence over the long-term follow-up for the larger and more aggressive lesions.
It is necessary to be mentioned that our technique carries a risk of iatrogenic fracture intraoperatively or postoperatively especially in high-risk areas such as proximal femoral lesions. Gentle surgical manipulation and limited or non-weight bearing are recommended to avoid this sequale.
The weaknesses of the current study include the lack of comparison to other operative modalities due to the small sample size. Thus, further trials are needed to compare the effectiveness of this technique on groups of patients with different types of bone cysts in variable anatomical locations. Treatment of benign bone cysts (SBCs/ABCs) with minimally invasive percutaneous curettage and a local autologous cancellous bone graft is an effective modality, with promising outcomes in the local control of recurrence and in enhanced bony consolidation.
Disclosure:
The Authors declare that there is no conflict of interest.
Role of the funding source:
None declared
References
- 1.Gerasimov AM, Toporova SM, Furtseva LN, Berezhnoy AP, Vilensky EV, Alekseeva RI. The role of lysosomes in the pathogenesis of unicameral bone cysts. Clin Orthop Relat Res. 1991;(266):53–63. [PubMed] [Google Scholar]
- 2.Cottalorda J, Kohler R, Sales de Gauzy J, Chotel F, Mazda K, Lefort G, et al. Epidemiology of aneurysmal bone cyst in children: a multicenter study and literature review. J Pediatr Orthop B. 2004;13(6):389–394. doi: 10.1097/01202412-200411000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Steffner R. Benign bone tumors. Cancer Treat Res. 2014;162:31–63. doi: 10.1007/978-3-319-07323-1_3. [DOI] [PubMed] [Google Scholar]
- 4.Flont P, Malecki K, Niewola A, Lipczyk Z, Niedzielski K. Predictive characteristic of simple bone cyst treated with curettage and bone grafting. BMC musculoskeletal disorders. 2015;16(1):1–6. doi: 10.1186/s12891-015-0797-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright JG, Yandow S, Donaldson S, Marley L, Simple Bone Cyst Trial Group. A randomized clinical trial comparing intralesional bone marrow and steroid injections for simple bone cysts. JBJS. 2008;90(4):722–30. doi: 10.2106/JBJS.G.00620. [DOI] [PubMed] [Google Scholar]
- 6.Kadhim M, Thacker M, Kadhim A, Holmes Jr L. Treatment of unicameral bone cyst: systematic review and meta analysis. Journal of children's orthopaedics. 2014;8(2):171–91. doi: 10.1007/s11832-014-0566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jamshidi K, Mirkazemi M, Izanloo A, Mirzaei A. Locking plate and fibular strut-graft augmentation in the reconstruction of unicameral bone cyst of proximal femur in the paediatric population. International orthopaedics. 2018;42(1):169–74. doi: 10.1007/s00264-017-3648-2. [DOI] [PubMed] [Google Scholar]
- 8.Couto A, Sá Rodrigues A, Nunes B, Torres J, Gutierres M. Arthroscopic approach to simple bone cyst of the humeral head-a step toward a minimally invasive technique. JSES Open Access. 2018;2(4):211–214. doi: 10.1016/j.jses.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aiba H, Kobayashi M, Waguri-Nagaya Y, Goto H, Mizutani J, Yamada S, et al. Treatment of simple bone cysts using endoscopic curettage: a case series analysis. J Orthop Surg Res. 2018;13(1):168. doi: 10.1186/s13018-018-0869-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aiba H, Kobayashi M, Waguri-Nagaya Y, Goto H, Mizutani J, Yamada S, et al. Treatment of aneurysmal bone cysts using endoscopic curettage. BMC Musculoskelet Disord. 2018;19(1):268. doi: 10.1186/s12891-018-2176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koch G, Cazzato RL, Gilkison A, Caudrelier J, Garnon J, Gangi A. Percutaneous Treatments of Benign Bone Tumors. Semin Intervent Radiol. 2018;35(4):324–332. doi: 10.1055/s-0038-1673640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park HY, Yang SK, Sheppard WL, Hegde V, Zoller SD, Nelson SD, et al. Current management of aneurysmal bone cysts. Curr Rev Musculoskelet Med. 2016;9(4):435–444. doi: 10.1007/s12178-016-9371-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Horstmann PF, Hettwer WH, Petersen MM. Treatment of benign and borderline bone tumors with combined curettage and bone defect reconstruction. J Orthop Surg (Hong Kong) 2018;26(3):2309499018774929. doi: 10.1177/2309499018774929. [DOI] [PubMed] [Google Scholar]
- 14.Chen CJ, Brien EW. Early postoperative compilations of bone filling in curettage defects. Journal of orthopaedic surgery and research. 2019;14(1):1–2. doi: 10.1186/s13018-019-1297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rossi G, Mavrogenis AF, Facchini G, Bartalena T, Rimondi E, Renzulli M, et al. How effective is embolization with N-2-butyl-cyanoacrylate for aneurysmal bone cysts? Int Orthop. 2017;41(8):1685–1692. doi: 10.1007/s00264-016-3364-3. [DOI] [PubMed] [Google Scholar]
- 16.Oliveira MBDR, Meohas W, de Carvalho GS, Rodrigues RR, Oliveira FCR, de Sa Lopes AC, et al. Primary Aneurysmal Bone Cyst of Long Bones Treated with a Single Dose of Calcitonin and Methylprednisolone Percutaneous Intralesional Injection: A Case Series and Literature Review. J Orthop Oncol. 2016;3:113. [Google Scholar]
- 17.Batisse F, Schmitt A, Vendeuvre T, Herbreteau D, Bonnard C. Aneurysmal bone cyst: A 19-case series managed by percutaneous sclerotherapy. Orthop Traumatol Surg Res. 2016;102(2):213–216. doi: 10.1016/j.otsr.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 18.Palmerini E, Ruggieri P, Angelini A, Boriani S, Campanacci D, Milano GM, et al. Denosumab in patients with aneurysmal bone cysts: A case series with preliminary results. Tumori. 2018;104(5):344–351. doi: 10.1177/0300891618784808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsagozis P, Brosjö O. Current Strategies for the Treatment of Aneurysmal Bone Cysts. Orthop Rev (Pavia) 2015;7(4):6182. doi: 10.4081/or.2015.6182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ulici A, Balanescu R, Topor L, Barbu M. The modern treatment of the simple bone cysts. J Med Life. 2012;5(4):469–473. [PMC free article] [PubMed] [Google Scholar]
- 21.Cottalorda J, Kohler R, Chotel F, de Gauzy JS, Lefort G, Louahem D, et al. Recurrence of aneurysmal bone cysts in young children: a multicentre study. J Pediatr Orthop B. 2005;14(3):212–218. doi: 10.1097/01202412-200505000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Kaelin AJ, MacEwen GD. Unicameral bone cysts Natural history and the risk of fracture. Int Orthop. 1989;13(4):275–282. doi: 10.1007/BF00268511. [DOI] [PubMed] [Google Scholar]
- 23.Capanna R, Campanacci DA, Manfrini M. Unicameral and aneurysmal bone cysts. Orthop Clin North Am. 1996;27(3):605–614. [PubMed] [Google Scholar]
- 24.Enneking WF. A system of staging musculoskeletal neoplasms. Clin Orthop Relat Res. 1986;(204):9–24. [PubMed] [Google Scholar]
- 25.Neer CS, Francis KC, Johnston AD, Kiernan HA Jr. Current concepts on the treatment of solitary unicameral bone cyst. Clin Orthop Relat Res. 1973;(97):40–51. doi: 10.1097/00003086-197311000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Gundle KR, Bhatt EM, Punt SE, Bompadre V, Conrad EU. Injection of Unicameral Bone Cysts with Bone Marrow Aspirate and Demineralized Bone Matrix Avoids Open Curettage and Bone Grafting in a Retrospective Cohort. Open Orthop J. 2017;11:486–492. doi: 10.2174/1874325001711010486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Benayahu D, Kletter Y, Zipori D, Wientroub S. Bone marrow-derived stromal cell line expressing osteoblastic phenotype in vitro and osteogenic capacity in vivo. J Cell Physiol. 1989;140(1):1–7. doi: 10.1002/jcp.1041400102. [DOI] [PubMed] [Google Scholar]
- 28.Beresford JN. Osteogenic stem cells and the stromal system of bone and marrow. Clin Orthop Relat Res. 1989;(240):270–280. [PubMed] [Google Scholar]
- 29.Mylle J, Burssens A, Fabry G. Simple bone cysts A review of 59 cases with special reference to their treatment. Arch Orthop Trauma Surg. 1992;111(6):297–300. doi: 10.1007/BF00420053. [DOI] [PubMed] [Google Scholar]
- 30.Reddy KI, Sinnaeve F, Gaston CL, Grimer RJ, Carter SR. Aneurysmal bone cysts: do simple treatments work? Clin Orthop Relat Res. 2014;472(6):1901–1910. doi: 10.1007/s11999-014-3513-1. [DOI] [PMC free article] [PubMed] [Google Scholar]