Abstract
Background:
Different causative factors for revision total knee arthroplasty (TKA) surgeries are elucidated in the arthroplasty registry data of different countries and the patient records at tertiary care centers. We aimed to determine the changes in the causes for revision TKAs before and after 2011 (The year that the Musculoskeletal Infection Society proposed a new definition for periprosthetic joint infection) and the changes in the demographics of patients who underwent revision TKAs during the same time intervals.
Methods:
Patients who underwent revision TKAs between 2004 and 2017 were evaluated. A total of 291 patients operated before (period 1, n = 139) and after (period 2, n = 152) 2011 were included, while 53 patients with inconclusive diagnoses were excluded. The demographic data of patients and the causes for revision TKAs were collected and compared between the two periods.
Results:
Infection was the most common cause of revision TKAs during periods 1 (58%) and 2 (48%). Aseptic loosening (46%) and infection (37%) were the 2 most common causes for late revisions during period 2. Aseptic loosening almost doubled during period 2 compared with that in period 1. Age, sex, and body mass index distribution in patients were similar across both the periods.
Conclusion:
Although the incidence of aseptic loosening has significantly increased since 2011, infection is still the most common cause for revision knee arthroplasty surgery.
Key Words: Revision knee arthroplasty, Periprosthetic joint infection, Aseptic loosening
Introduction
Indications for total knee arthroplasty (TKA) have been expanded to include younger and more active patients. Consequently, more primary knee arthroplasty surgeries have been performed (1). The increased numbers of primary TKA surgeries, prolonged life expectancy, and changes in the demographics of patients, have led to an increase in the number of revision knee arthroplasty surgeries (2, 3). The underlying reasons for revision TKAs are expected to change with the adoption of new implants, technologies, and surgical techniques (4). The age and sex distribution of patients receiving primary total knee prostheses also change in time. This can affect the survival of prostheses and cause possible etiological differences (5). The duration of survival of TKAs may also differ depending on the different lifestyles of patients and advancements in material properties. Historically, until the 2000s; the need for revision was attributed to infection, instability, implant-related causes such as abrasion, and aseptic loosening. With the development of implant technology, polyethylene abrasion was excluded as the first reason for revision in 2010 (6). Currently, infection, loosening, and instability are considered as the main causes for revision surgeries (7-12).
In comparison with primary surgery, revision surgery entails higher costs and provides lower patient satisfaction (1, 13). Further insights into the need and epidemiology of revision TKA procedures may help in improving the outcomes and mitigating the need for future revisions. The underlying causes for revision should be well understood and precautions should be taken to account for the variations in sterilization procedures, surgical techniques, and implant technologies (1).
Our study aimed to determine the changes in the causes for knee arthroplasty revision surgeries before and after 2011 (The year that the Musculoskeletal Infection Society proposed a new definition for periprosthetic joint infection) and the changes in the demographics of patients who underwent revision knee replacements during the same time intervals.
Materials and Methods
The trends in the revision procedures and demographic features of the patients undergoing revision TKAs between 2004 and 2017 were assessed. Our study was approved by the Institutional Review Board and Ethics Committee (Number: 29.06.2018, 31/15). The records of the patients who underwent revision TKA surgery between 2004 and 2017 were scanned with an ICD code. Patients undergoing hinged and unicompartmental joint replacements during primary knee replacements were excluded. Patients’ data were collected from their digital charts, hospital admission notes, and operation notes. Revision was defined as removal, exchange, or addition of one or more prosthetic components (femur, tibia, tibial insert, and patella).
The diagnoses of all patients were re-examined per the new criteria of the Workgroup of the Musculoskeletal Infection Society (14).
Definite periprosthetic joint infection (PJI) exists when (14):
A sinus tract communicates with the endoprosthesis; or
A pathogen is isolated by culture from at least two separate tissue or fluid samples obtained from the affected prosthetic joint; or
Four of the following six criteria exist:
Elevated serum erythrocyte sedimentation rate and serum C-reactive protein concentration,
Elevated synovial leukocyte count,
Elevated synovial neutrophil percentage (PMN%),
Presence of purulence in the affected joint,
Isolation of a microorganism in one culture of periprosthetic tissue or fluid, or
Greater than five neutrophils per high-power field in five high-power fields observed from histologic analysis of periprosthetic tissue at 9400 magnification.
A total of 291 patients who underwent revision surgeries before (period 1, n = 139) and after (period 2, n = 152) 2011 were included in the study. Fifty-three patients with inconclusive diagnoses and insufficient data charts were excluded from the study. Patients with inconclusive diagnoses included those who were diagnosed with aseptic loosening per their preoperative digital data, patient charts, and laboratory information, and were treated in 2-stages, similar to the protocol followed for an infected prosthesis. Additionally, for some patients, the surgeon modified the indications for revisions intraoperatively, without the objective criteria of intraoperative frozen-section histology etc. Therefore, we excluded patients with incomplete hospital records and those with inconsistent preoperative laboratory and radiological findings and intraoperative findings. Patients who underwent a second revision were also excluded from the study. The causes of failures were listed as infection, aseptic loosening, insert fracture, instability, patellar tilting, unresolved pain, and fracture. Patients’ demographics and indications for primary and revision TKAs were recorded.
Statistics
The demographic structure (age, gender, BMI) of the two groups and the causes for revision TKAs were collected and compared. Statistical analysis was performed using MedCalc Statistical Software version 12.7.7 (MedCalc Software bvba, Ostend, Belgium). Shapiro–Wilk’s test was employed to ascertain the normality of continuous variables. Descriptive statistics were presented as mean (±standard deviation) for continuous variables. Parametric statistical methods were used for values with nonskewed distribution. Student’s t-test was performed to compare two normally distributed groups. Chi-square test was used to examine the categorical variables expressed as frequencies (and percentages). The patients in the study group were included from the end of 2004 (the year when the digital patient registration system at our center started) until the end of 2017. The reason we limited the study duration until the end of 2017 was to ensure an approximately equal patient distribution between the two groups. The causes for early revision (≥2 years) and late revision (<2 years) were considered/categorized separately. Trends in revision TKAs were determined by assessing the annual number of primary and revision TKAs, the revision burden, the annual number of each revision type, the annual proportion of each cause, and demographic data (age, sex, and BMI) during December 31, 2004–2011 and 2012–December 31, 2017. All tests were two-sided and the statistical significance level was set at 0.05.
Results
Patients’ demographic data and comparative statistics, including clinical information, such as indications for primary TKAs, causes of failure after primary TKAs, and types of revision TKAs, were assessed between the two groups [Table 1]. An average of 28 knee revision arthroplasty surgeries and an average of 318 primary knee arthroplasty surgeries were performed in each year between 2004 and 2017 [Figure 1]. The mean age of the patients undergoing revision was 65 years, and the ratio of obese to overweight patients was 62%. The average time durations until knee arthroplasty failures were 35 ± 30 months before 2011 and 47 ± 46 months after 2011 (p < 0.001) [Table 2].
Table 1.
Patients Demographics, Etiology of Primary or Revision Surgery, and Treatment Strategy
| Before 2011 | After 2011 | Total (n, %) | p value | ||
|---|---|---|---|---|---|
| Number (n) Revision Surgery | 139 | 151 | |||
| Female / Male (n %) | 115/2482- 18% | 124/2881- 19% | 0.79 | ||
| Revision Age of Patients mean ± SD, CI | 63.8 ± 8 64.5 ± 10 -2.9 / 1.4 | 0.49 | |||
| BMI (mean ± SD) | |||||
| Normal, n (%) | 52 (37.4) | 59 (38.8) | 111 (38) | 0.07 | |
| Overweight, n (%) | 84 (60.4) | 81 (53.3) | 165 (56.7) | ||
| Obese, n (%) | 3 (2.2) | 12 (7.9) | 15 (5.2) | ||
| Etiology of Primary Surgery of Revised Knees (n= 291) | |||||
| Primary (idiopathic) | 126 (90%) | 141 (92%) | 267 | ||
| Romatoid arthritis | 3 | 2 | 5 | ||
| Post-traumatic | 7 | 3 | 10 | ||
| Other | 3 | 6 | 9 | ||
| Total (n) | 139 | 152 | 291 | ||
| Etiology of Revision Surgeries | |||||
| Infection | 81 (58%) | 73 (48%) | 154 (52%) | 0.08 | |
| Aseptic loosening | 29 (20%) | 56 (36%) | 85 (29%) | 0.002 | |
| Unresolved pain | 11 | 6 | 17 | ||
| Instability | 10 | 6 | 16 | ||
| Periprosthetic fracture | 5 | 8 | 13 | ||
| Insert fracture | 3 | 3 | 6 | ||
| Total (n) | 139 | 152 | 291 | ||
| Treatment | |||||
| 1 stage | 72 | 104 | 176 | 0.004 | |
| 2 stage | 67 | 48 | 115 | ||
| Implants used during revision | |||||
| Revision P. | 87 (62%) | 83 (54%) | 167 (58%) | 0.16 | |
| Constraint Revision P. | 28 (20%) | 35 (23%) | 63 (21%) | 0.55 | |
| Tumor resection prothesis | 0 (0.0 %) | 6 (3.9%) | 6 (2.1%) | NS | |
| Arthrodesis (Ex. Fix. or Nail) | 4 (3 %) | 3 (2%) | 7 (2.4%) | 0.6 | |
| Insert exchange | 8 (6%) | 9 (5.9%) | 17 (5.9%) | 0.9 | |
| Exchange with Primary P. | 12 (9%) | 16 (10 %) | 28 (9.8 %) | 0.58 | |
| CI; Confidence interval of mean difference, n; number, SD; Standard Deviation, %; percentile, BMI; Body Mass Index, P; Prothesis, NS; Not studied, | |||||
Figure 1.
Changes in number of primary knee arthroplasty and revision knee arthroplasty with years
Table 2.
Time to revision represented with intervals
| Time to Revisions | Before 2011 | After 2011 | Total | pvalue | |
| N% | <12 moths | 59 | 55 | 114 | 0.27 |
| 42.4% | 36.2% | 39.2% | |||
| 12-24 moths | 47 | 49 | 96 | 0.08 | |
| 33.8% | 32.2% | 33.0% | |||
| 24-60 moths | 22 | 34 | 56 | 0.15 | |
| 15.8% | 22.4% | 19.2% | |||
| >120 moths | 11 | 14 | 25 | 0.69 | |
| 7.9% | 9.2% | 8.6% | |||
| Total | 139 | 152 | 291 |
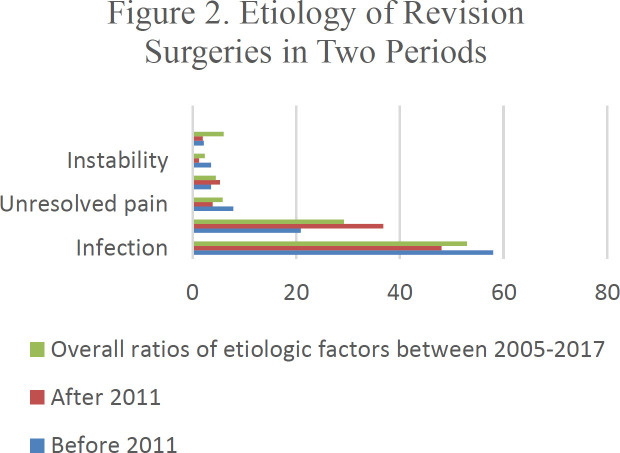
Overall, infection and aseptic loosening were the predominant contributing factors for knee arthroplasty failures. These two mechanisms were responsible for 82% of all failures, including those in the two periods. Failure mechanisms were recorded as percentiles and frequencies across the two periods of early (<2 years) and late (≥2 years) revisions [Figure 2 and Table 3]. Infection was the leading etiologic factor for early and late revisions during period 1 and for early revisions during period 2. Aseptic loosening was the most common cause of late revisions during period 2 [Table 3]. TKAs showed a decrease in revisions because of infection, unresolved pain, and instability from period 1 to period 2. The incidence of revisions due to aseptic loosening nearly doubled after 2011 [Table 1]. The risk of revisions because of infections significantly decreased during period 2 (RR = 1.3, 95% CI 0.9–1.6, p = 0.04). Conversely, the risk of revisions due to aseptic loosening increased during period 2 (RR = 0.63, 95% CI 0.43–0.94, p = 0.003).
Figure 2.
Etiology of revision surgeries in two periods and overall ratios of two periods demonstrated. Failure mechanism was presented with percentiles and numbers based on the two periods
Table 3.
Etiology of Revisions According to the Early and Late Periods in Two Time Intervals
| Periods | ||||||
|---|---|---|---|---|---|---|
| 2005-2011 | 2011-2017 | |||||
| Time to revision | Early (<2 year) |
Late (≥2 year) |
Total | Early (<2 year) |
Late (≥2 year) |
Total |
| Infection (n, %) | 37 | 44 | 81 | 39 | 34 | 73 |
| 62.7% | 55.0% | 58.3% | 62.9% | 37.8% | 48.0% | |
| Aseptic loosening (n, %) |
7 | 22 | 29 | 14 | 42 | 56 |
| 11.9% | 27.5% | 20.9% | 22.6% | 46.7% | 36.8% | |
| Periprosthetic Fracture (n, %) | 3 | 2 | 5 | 1 | 7 | 8 |
| 5.1% | 2.5% | 3.6% | 1.6% | 7.8% | 5.3% | |
| Unresolved pain (n, %) |
4 | 7 | 11 | 4 | 2 | 6 |
| 6.8% | 8.8% | 7.9% | 6.5% | 2.2% | 3.9% | |
| Instability (n, %) | 5 | 5 | 10 | 2 | 4 | 6 |
| 8.4% | 6.3% | 7.2% | 3.2% | 4.4% | 3.9% | |
| Insertfracture (n, %) | 3 | 0 | 3 | 2 | 1 | 3 |
| 5.1% | 0.0% | 2.2% | 3.2% | 1.1% | 2.0% | |
Early; <2 years, Late≥2 years. Boxes in bold type indicate the 2 most common causes of etiology.
Discussion
The causes for knee revision surgeries were first elaborated in the 1980s. Until the 1990s, the leading causes of knee revisions were loosening and instability, and infections were reported as rare causes (15, 16). In the early 2000s, a 5-year follow-up study by Fehring et al. reported infection and instability as the most common causes of revisions (17). Sharkey et al. further reported on the causes of revisions and categorized their results into early (<2 years) and late (≥2 years) revisions based on the time between the primary and revision surgery. The most common reasons for the revisions were infection followed by instability in early failures. After 2 years, the most common reason was polyethylene wear followed by loosening, instability, and infection. The most common factors in decreasing order were polyethylene wear, loosening, instability, and infection (6). In 2006, Mullhall et al. reported on the causes of knee revisions during early (<2 years) and late (≥2 years) periods (18). Infection seemed to be the most common reason for early revision surgeries, while after 2 years mechanical factors seemed to be more predominant. In 2008, Hussain et al. reported infection as the most common factor during early (<2 years) and late (≥2 years) periods (9). In 2013, Schorer et al. performed a multicenter study and reported aseptic loosening, instability, and infection as the most common failure mechanisms. Infection still remained the main cause of revision during early periods, while polyethylene wear was a rare cause across all periods (19). Sharkey et al. presented a 10-year update on a similar investigation and compared the results. Infection and aseptic loosening were identified as the most common failure mechanisms for early (<2 years from primary) and late revision surgeries, respectively. In comparison with a previous report, a separate paper did not present polyethylene wear and instability as major contributing factors (6).
In national database-based studies, Bozic et al. (2010) and Delanois et al. (2017) reported infection and implant loosening as the most common causes of knee arthroplasty revisions in the United States (10, 20). In 2015, Nimaaki provided the combined arthroplasty registry results from five countries (Australia, New Zealand, Norway, Sweden, and England and Wales) and from Europe. Aseptic loosening was the leading cause of revisions in all the countries. Infection was the second-most common cause in Australia, Sweden, and England and Wales, while pain was the most common cause in Norway and New Zealand (12). Nimaaki also indicated that results obtained from arthroplasty registry systems may be inconsistent because of the differences regarding the classifications of the causes of revisions in different countries. In Asia, Kasahara et al. reported that aseptic loosening, followed by infection, was the leading cause of revisions in a multicenter study between 2006 and 2011 in Japan (21). In 2014, Koh et al. found that infection, followed by aseptic loosening, was the leading cause of revision in a multicenter study in South Korea between 2008 and 2012 (22). In conclusion, clinical studies reported by tertiary referral centers and large registry data have indicated aseptic loosening as the most common reason for revision, whereas early failures were attributed to infection. The number of revisions due to polyethylene wear has decreased in the last two decades.
PJI was the dominant cause of revisions during 2004–2011 and 2012–2017. Aseptic loosening, followed by infection, was the most common cause of late revision during 2012–2017. Furthermore, aseptic loosening almost doubled during 2012–2017 compared with that in the previous period. In our study, we did not find any differences in age, sex, BMI distribution, and type of revision surgeries in patients who underwent revision TKAs during the two time periods. Tumor resection prosthesis was involved in revision knee arthroplasty mostly after 2010. However, our causes for revision surgeries were different from those in the Western and Asian countries. Infection was the most common cumulative cause of failure, and loosening emerged as the most common cause of late revisions in recent years. In our country, the number of primary TKAs and the number of revision TKAs has increased over time (2). In the coming years we may see a similarity in the pattern of causation of revision TKAs in our country with that in the developed countries. Surgical approaches used in the primary knee surgery, the type of implants used, and infection prophylaxis in our country are also similar to those in the developed countries. Patient-related variables and postoperative patient follow-up should be well evaluated to understand the background of infection (23). An increase in revision TKAs due to aseptic loosening in recent years should not be ignored. Consequently, risk factors such as male sex, younger age, and demand for high-flexion activities, should be investigated. Additionally, implant-related factors, such as design characteristics, should be clarified to propose innovations for improving the durability of TKAs.
Some limitations of this study were its retrospective design and a smaller sample size than in other studies. Nevertheless, the posthoc power analysis of our study was 86.2%. Further, we could not provide the results from different centers in our study. We also did not report on the incidence of revision knee arthroplasties since we excluded patients who had unexplained pain, showed signs of radiographic loosening, did not undergo revision due to medical reasons, or opted to forgo revision surgery. We also excluded 53 of 344 patients because of inadequate records and inconsistencies. Patients with infections may be referred to our center more commonly because revision knee arthroplasties performed due to infections are more complicated. We presented a single-institution experience, which had some advantages. We analyzed the causes for revisions as documented by the operating surgeon considering all aspects from individual patient chart data, radiographic, and laboratory findings. Thus, we avoided misdiagnoses and differences in the personal classification of causes for revisions that are commonly discussed in arthroplasty registry studies (24).
Although the incidence of aseptic loosening has significantly increased since 2011, infection has remained as the most common cause of revision knee arthroplasty surgery.
Declaration of conflicting interests:
The author(s) declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Funding:
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Kurtz SM, Ong KL, Schmier J, Mowat F, Saleh K, Dybvik E, et al. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89(3):144–151. doi: 10.2106/JBJS.G.00587. [DOI] [PubMed] [Google Scholar]
- 2.Ceyhan E, Gursoy S, Akkaya M, Ugurlu M, Koksal I, Bozkurt M. Toward the Turkish national registry system: aprevalence study of total knee arthroplasty in Turkey. J Arthroplasty. 2016: 1878–84. doi: 10.1016/j.arth.2016.02.033. [DOI] [PubMed] [Google Scholar]
- 3.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012;308(12):1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dyrhovden GS, Lygre SHL, Badawy M, Gøthesen Ø, Furnes O. Have the causes of revision for total and unicompartmental knee arthroplasties changed during the past two decades? Clin Orthop Relat Res. 2017: 1874–86. doi: 10.1007/s11999-017-5316-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bayliss LE, Culliford D, Monk AP, Glyn-Jones S, Prieto-Alhambra D, Judge A, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet . 2017;389(10077):1424–1430. doi: 10.1016/S0140-6736(17)30059-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J. Why are total knee arthroplasties failing today-has anything changed after 10 years? J Arthroplasty. 2014;29(9):1774–8. doi: 10.1016/j.arth.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 7.Lum ZC, Shieh AK, Dorr LD. Why total knees fail-A modern perspective review. World J Orthop . 2018;18(9):60–64. doi: 10.5312/wjo.v9.i4.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schroer WC, Berend KR, Lombardi A V, Barnes CL, Bolognesi MP, Berend ME, et al. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011. J Arthroplasty. 2013;28(8 Suppl):116–9. doi: 10.1016/j.arth.2013.04.056. [DOI] [PubMed] [Google Scholar]
- 9.Hossain F, Patel S, Haddad FS. Midterm assessment of causes and results of revision total knee arthroplasty. Clin Orthop Relat Res. 2010;468(5):1221–8. doi: 10.1007/s11999-009-1204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res., 2010;476(10):1951–1960. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lombardi A V, Berend KR, Adams JB. Why knee replacements fail in 2013: Patient, surgeon, or implant? Bone Joint J. 2014: :101–4. doi: 10.1302/0301-620X.96B11.34350. [DOI] [PubMed] [Google Scholar]
- 12.Niinimäki TT. The reasons for knee arthroplasty revisions are incomparable in the different arthroplasty registries. Knee. 2015;22(2):142–4. doi: 10.1016/j.knee.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 13.Greidanus N V, Peterson RC, Masri BA, Garbuz DS. Quality of life outcomes in revision versus primary total knee arthroplasty. J Arthroplasty. 2011;26(4):615–20. doi: 10.1016/j.arth.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 14.Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011;469(11):2992–2994. doi: 10.1007/s11999-011-2102-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moreland JR. Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res . 1988:49–64. [PubMed] [Google Scholar]
- 16.Rand JA, Bryan RS. Revision after total knee arthroplasty. Orthop Clin North Am. 1982;13(1):201–12. [PubMed] [Google Scholar]
- 17.Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001: :315–8. doi: 10.1097/00003086-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 18.Mulhall KJ, Ghomrawi HM, Scully S, Callaghan JJ, Saleh KJ. Current etiologies and modes of failure in total knee arthroplasty revision. Clin Orthop Relat Res. 2006: 45–50. doi: 10.1097/01.blo.0000214421.21712.62. [DOI] [PubMed] [Google Scholar]
- 19.Schroer WC, Berend KR, Lombardi A V, Barnes CL, Bolognesi MP, Berend ME, et al. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011. J Arthroplasty. 2013;28:116–9. doi: 10.1016/j.arth.2013.04.056. [DOI] [PubMed] [Google Scholar]
- 20.Delanois RE, Mistry JB, Gwam CU, Mohamed NS, Choksi US, Mont MA. Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty. 2017;32(9):2663–2668. doi: 10.1016/j.arth.2017.03.066. [DOI] [PubMed] [Google Scholar]
- 21.Kasahara Y, Majima T, Kimura S, Nishiike O, Uchida J. What are the causes of revision total knee arthroplasty in Japan? Clin Orthop Relat Res. 2013;471(5):1533–8. doi: 10.1007/s11999-013-2820-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koh IJ, Cho WS, Choi NY, Kim TK. Causes, risk factors, and trends in failures after TKA in Korea over the past 5 years: A multicenter study knee. Clin Orthop Relat Res. 2014;472(1):316–26. doi: 10.1007/s11999-013-3252-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shahi A, Parvizi J. Prevention of Periprosthetic Joint Infection. Arch Bone Jt Surg. 2015;3(2):72–81. [PMC free article] [PubMed] [Google Scholar]
- 24.Koh CK, Zeng I, Ravi S, Zhu M, Vince KG, Young SW. Periprosthetic joint infection is the main cause of failure for modern knee arthroplasty: an analysis of 11,134 knees. Clin Orthop Relat Res. 2017;475:2194–201. doi: 10.1007/s11999-017-5396-4. [DOI] [PMC free article] [PubMed] [Google Scholar]