Abstract
This Medicare database review tracks the long-term incidence of operative hernia recurrence up to 10 years after surgery among older US adults.
Hernia recurrence following ventral or incisional hernia repair is a serious outcome that can occur years after surgery.1 Many studies of hernia recurrence are limited to short-term outcomes at single centers.2 The last study to characterize hernia recurrence at 10 or more years in a large US population was conducted from 1987 to 1999 and found a 20% rate of reoperation for recurrence at 10 years.3 We sought to characterize the long-term incidence of operative hernia recurrence up to 10 years after surgery in a contemporary US population of older adults.
Methods
We performed a retrospective review of 100% fee-for-service Medicare claims data to identify adult patients undergoing elective, inpatient, ventral or incisional and umbilical hernia repair from January 1, 2007, to December 31, 2018, using appropriate International Classification of Diseases, Ninth Revision (ICD-9) or International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) and Current Procedural Terminology (CPT) procedure codes with a corresponding ICD-9 or ICD-10 diagnosis code for the relevant type of hernia (eTable 1 in the Supplement).
The primary outcome was reoperation for hernia recurrence, defined using the same ICD-9 or ICD-10 and CPT codes used to identify the index operation, as well as codes specific to recurrent hernia repair. Reoperation was identified during the follow-up period up to 10 years after the index hernia repair using patients’ unique Medicare Beneficiary Identifier.
A Cox proportional hazards model was used to calculate the cumulative incidence of hernia recurrence while adjusting for patient age, sex, race and ethnicity (see eMethods in the Supplement for race and ethnicity identification in the Medicare claims database), 29 Elixhauser comorbidities (eTable 2 in the Supplement), hernia type (ventral or incisional vs umbilical), and surgical approach (open vs minimally invasive). Patients were censored if they died, disenrolled from Medicare, or reached the end of the study period. Analyses were performed using Stata version 15.1 (StataCorp). No covariates were missing. This study of deidentified patient data was exempted from regulation by the University of Michigan Institutional Review Board and the need for informed consent was waived.
Results
Of the 175 735 patients who had undergone hernia repair, 162 292 underwent ventral or incisional hernia repair and 13 443 underwent umbilical hernia repair. The mean age was 68.9 years (SD, 11.1 years); 68 943 patients (39.2%) were men; 808 (0.5%) were Asian, 14 235 (8.1%) were Black, 3348 (1.9%) were Hispanic, 1102 (0.6%) were North American Native, 153 148 (87.2%) were White, 1852 (1.1%) were of other race or ethnicity, and 1242 (0.7%) were of unknown race or ethnicity. A total of 35 327 patients (20.1%) had a diagnosis of obesity at the time of index hernia repair. Median follow-up time was 5.3 years (IQR, 1.9-8.7 years).
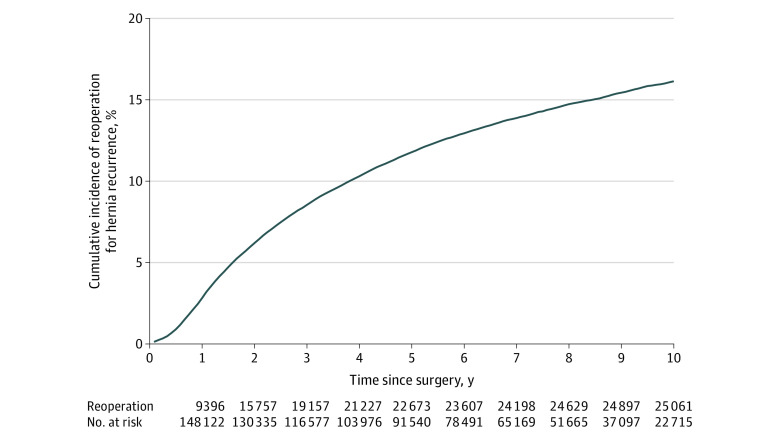
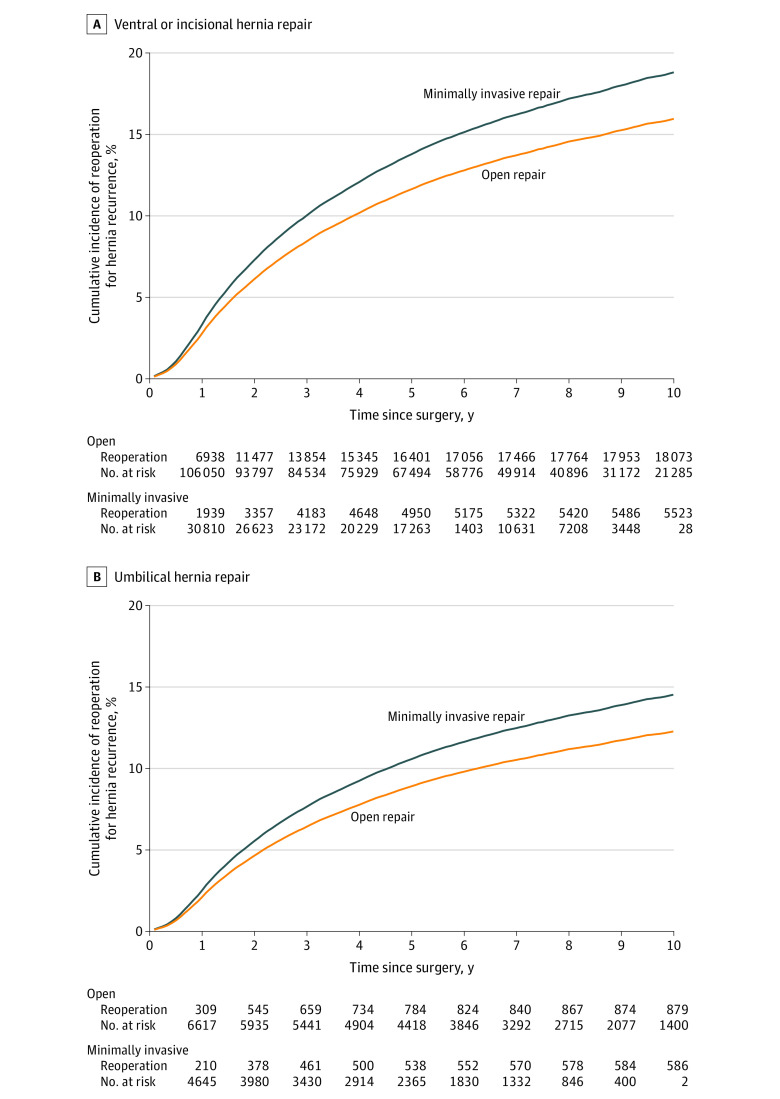
A total of 25 061 patients (14.3%) underwent reoperation for hernia recurrence. The adjusted cumulative incidence of reoperation for recurrence was 16.1% (95% CI, 16.1%-16.2%) at 10 years after the index operation (Figure 1). Among patients who underwent ventral or incisional hernia repair, the 10-year adjusted cumulative incidence of reoperation for recurrence was 16.0% (95% CI, 15.9%-16.0%) following open repair and 18.8% (95% CI, 18.7%-18.8%) following minimally invasive repair (Figure 2A). Among patients who underwent umbilical hernia repair, the 10-year adjusted cumulative incidence of reoperation for recurrence was 12.3% (95% CI, 12.2%-12.3%) following open repair and 14.5% (95% CI, 14.5%-14.6%) following minimally invasive repair (Figure 2B).
Figure 1. Overall Cumulative Incidence of Reoperation for Recurrence Following Elective Inpatient Ventral or Incisional and Umbilical Hernia Repair.
Cumulative incidence of reoperation for recurrence was calculated using a Cox proportional hazards model that included patient age, sex, race and ethnicity, 29 Elixhauser comorbidities, hernia type, and surgical approach.
Figure 2. Cumulative Incidence of Reoperation for Recurrence Stratified by Surgical Approach Following Ventral or Incisional Hernia Repair and Umbilical Hernia Repair.
Cumulative incidence of reoperation for recurrence was calculated using a Cox proportional hazards model that included patient age, sex, race and ethnicity, 29 Elixhauser comorbidities, hernia type, and surgical approach.
Discussion
In a contemporary population of older adults in the US, approximately 1 in 6 patients underwent reoperation for recurrence within 10 years of surgery. Compared with historical 10-year reoperation rates of approximately 1 in 5 patients reported by Flum et al in 2003,3 these results suggest that outcomes have only marginally improved. This study likely underestimated the incidence of clinical hernia recurrence because not all patients with recurrence undergo reoperation for repair.4 The incidence of reoperation for recurrence was lower following umbilical hernia repair, which may reflect the greater complexity of ventral or incisional hernias in this cohort. Compared with open hernia repair, minimally invasive hernia repair was associated with a higher incidence of reoperation for hernia recurrence in both groups, which is consistent with prior shorter-term clinical trials.5,6
This study is limited by its observational design. Its generalizability may be limited by the use of Medicare claims, although studies of non-Medicare patients have demonstrated similar recurrence rates.1 Also, although this study controlled for patient comorbidities, future work should investigate the relationship between specific comorbidities and hernia-related outcomes to help inform surgical decision-making.
Section Editors: Jody W. Zylke, MD, Deputy Editor; Kristin Walter, MD, Associate Editor.
eMethods. Race and Ethnicity Use in Medicare Claims Database
eTable 1. ICD-9/10 and CPT codes used to identify index hernia repair operation
eTable 2. 29 Elixhauser Comorbidities
eReferences
References
- 1.Kokotovic D, Bisgaard T, Helgstrand F. Long-term recurrence and complications associated with elective incisional hernia repair. JAMA. 2016;316(15):1575-1582. doi: 10.1001/jama.2016.15217 [DOI] [PubMed] [Google Scholar]
- 2.Liang MK, Holihan JL, Itani K, et al. Ventral hernia management: expert consensus guided by systematic review. Ann Surg. 2017;265(1):80-89. doi: 10.1097/SLA.0000000000001701 [DOI] [PubMed] [Google Scholar]
- 3.Flum DR, Horvath K, Koepsell T. Have outcomes of incisional hernia repair improved with time? a population-based analysis. Ann Surg. 2003;237(1):129-135. doi: 10.1097/00000658-200301000-00018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T. Reoperation versus clinical recurrence rate after ventral hernia repair. Ann Surg. 2012;256(6):955-958. doi: 10.1097/SLA.0b013e318254f5b9 [DOI] [PubMed] [Google Scholar]
- 5.Eker HH, Hansson BM, Buunen M, et al. Laparoscopic vs open incisional hernia repair: a randomized clinical trial. JAMA Surg. 2013;148(3):259-263. doi: 10.1001/jamasurg.2013.1466 [DOI] [PubMed] [Google Scholar]
- 6.Itani KM, Hur K, Kim LT, et al. ; Veterans Affairs Ventral Incisional Hernia Investigators . Comparison of laparoscopic and open repair with mesh for the treatment of ventral incisional hernia: a randomized trial. Arch Surg. 2010;145(4):322-328. doi: 10.1001/archsurg.2010.18 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Race and Ethnicity Use in Medicare Claims Database
eTable 1. ICD-9/10 and CPT codes used to identify index hernia repair operation
eTable 2. 29 Elixhauser Comorbidities
eReferences