Abstract
Objective:
To identify the clinical and epidemiological profile of adult intensive care units in Brazil.
Methods:
A systematic review was performed using a comprehensive strategy to search PubMed®, Embase, SciELO, and the Biblioteca Virtual em Saúde. The eligibility criteria for this review were observational studies that described the epidemiological and/or clinical profile of critically ill patients admitted to Brazilian intensive care units and were published between 2007 and 2020.
Results:
From the 4,457 identified studies, 27 were eligible for this review, constituting an analysis of 113 intensive care units and a final sample of 75,280 individuals. There was a predominance of male and elderly patients. Cardiovascular diseases were the main cause of admission to the intensive care unit. The Acute Physiology and Chronic Health Evaluation II score was the most widely used disease severity assessment system. The length of stay and mortality in the intensive care unit varied widely between institutions.
Conclusion:
These results can help guide the planning and organization of intensive care units, providing support for decision-making and the implementation of interventions that ensure better quality patient care.
Registration PROSPERO: CRD4201911808.
Keywords: Critical care outcomes, Health services research, Epidemiology, Intensive care units, Brazil
INTRODUCTION
Knowledge of the health conditions of a population, as well as its determinants, trends, and characteristics of the health/disease process, helps us plan actions and make strategic decisions, resulting in higher quality of care and better health services offered.(1,2)
However, translating research evidence into clinical practice is usually a slow and challenging process.(3) In Brazil, great socioeconomic inequality and regional disparities are factors that influence this process.(4) The complexity of the regionalization of health in the country is due to such characteristics as its continental dimensions, its number of potential users, its regional inequalities and diversities, the scope of the State’s role in health, and the multiplicity of agents (governmental and nongovernmental; public and private) involved in providing health care.(5)
Intensive care units (ICUs) are an essential component of modern medicine. Intensive care units are diverse, with substantial variation related to geographic location, patient demography, ICU size, disease severity, and availability of intensivism, further complicating the applicability of quality improvement initiatives.(6) The census conducted by the Associação de Medicina Intensiva Brasileira (AMIB)(7) in 2016, based on information from the National Registry of Health Establishments, indicated that in Brazil, there were 41,741 ICU beds, including in public, private, and philanthropic hospitals, and 27,709 beds were intended for adult patients in critical condition. In 2018, a survey conducted by the Federal Council of Medicine indicated that the number of ICU beds in Brazil was 44,253, and 49% were available for the Unified Health System (SUS - Sistema Único de Saúde).(8) In addition, of the 5,570 Brazilian municipalities, ICU beds were available in only 532, with 53.4% of them in the Southeast region.(8) This may lead to the need to travel between regions of the country to obtain these services.(9) The Brazilian scenario has heterogeneity both in its extent and in its sociodemographic development, which can lead to unequal growth, with important implications for the distribution of goods and services, especially those related to health.(10)
In this context, it is important to identify the characteristics of Brazilian ICUs so that health professionals and managers can have information that will promote the planning, safety, and quality of care for critically ill patients. The present study aimed to characterize the clinical and epidemiological profile of adult ICUs in Brazil based on published data through a systematic review.
METHODS
The studies were selected according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.(11) The study protocol was registered in PROSPERO (www.crd.york.ac.uk/prospera/) under number CRD42019118081. Two independent authors initially evaluated the title and abstract. After the selection of potentially relevant studies, the full-text versions were independently analyzed by two researchers. Disagreements were resolved by discussion.
Strategy for search and selection of studies
The potential studies going into this review were identified through a comprehensive strategy of searching the databases PubMed®, Embase, Scientific Electronic Library Online (SciELO), and Biblioteca Virtual em Saúde (BVS). A complementary search was performed on the reference lists of the selected articles to retrieve relevant publications.
The database searches were performed from August to December 2020, involving the cross-checking of descriptors selected in the medical subject heading (MeSH) terms of the National Library of Medicine of the United States. All terms were adapted for each database and combined using Boolean digits. The complete search strategy is shown in table 1.
Table 1.
Detailed search strategy by database
| Database | Research strategy |
|---|---|
| BVS | (“health profile” OR “health status” OR mortality OR demography OR epidemiology OR “epidemiological profile” OR “outcome measure” OR “Health level” OR “outcome studies” OR “outcomes research” OR “health service” OR “frequency” OR prevalence OR incidence)) AND (“intensive care unit” OR icu OR uti OR “critical care” OR “critical illness” OR “Critical care outcomes”)) AND (brazil OR brazil OR brazil OR “Latin America” OR “South America”))) AND (instance:”regional”) AND (limit:(“humans”) AND year_cluster :(“2013” OR “2014” OR “2012” OR “2015” OR “2010” OR “2011” OR “2008” OR “2016” OR “2009” OR “2007” OR “2017” OR “2018” OR “2019” OR “2020”)) |
| PubMed® | ((((“health status”[MeSH Terms] OR (“demography”[MeSH Terms] OR “demography”[All Fields]) OR ((“epidemiology”[MeSH Terms] OR “epidemiology” [Subheading] OR “epidemiological”[All Fields]) OR profile[All Fields])) AND ((“intensive care units”[MeSH Terms] OR UTI[All Fields] OR CTI[All Fields]) OR ICU[All Fields])) AND ((“brazil”[MeSH Terms] OR “brazil”[All Fields]) OR brasil[All Fields])) NOT ((“infant, newborn”[MeSH Terms] OR (“infant”[All Fields] AND “newborn”[All Fields]) OR “newborn infant”[All Fields] OR “neonatal”[All Fields]) OR (“pediatrics”[MeSH Terms] OR “pediatrics”[All Fields] OR “pediatric”[All Fields]) OR (“child”[MeSH Terms] OR “child”[All Fields] OR “children”[All Fields])) AND “humans”[MeSH Terms] |
| Embase | (‘health status’ OR demography OR epidemiology OR ‘health level’ OR ‘health service’) AND (‘intensive care unit’ OR icu OR uti OR ‘critical care’ and OR ‘critical illness’ OR ‘critical care outcomes’) AND (Brazil OR Brazil OR Brazilian OR ‘Latin America’ OR ‘South America’) AND [2007-2020]/py |
| SciELO | AND Profile “Intensive Care Units” |
BVS - Biblioteca Virtual em Saúde; SciELO - Scientific Electronic Library Online.
The eligibility criteria for this review were observational studies published from 2007 to 2020 that aimed to describe the epidemiological and/or clinical profile of critically ill adult patients of both sexes, as well as the length and outcome of hospitalization in Brazilian ICUs. The studies were excluded for the following reasons: studies that selected a subgroup of patients with specific disease or clinical condition, randomized clinical trials or review articles, theses or dissertations, full text not available, abstracts and publications at conferences, and studies that used the same data sources as another included study.
Data extraction and quality assessment
For the purposes of analysis and composition of the results, the following data were considered: study characteristics (design, sample size, institution profile, number of ICUs, Brazilian region, and state); sociodemographic aspects of the critical patient population treated in the ICUs (sex, age, race, education, marital status, and religion); and clinical characteristics (prognostic indices for assessment of disease severity upon admission to the ICU, origin of the patient as clinical or surgical, therapeutic interventions related to the use of invasive mechanical ventilation (IMV), vasoactive drugs and/or hemodialysis throughout the ICU stay, main causes of ICU admission, length of stay, and clinical outcome in the ICU as death or discharge).
The methodological quality and risk of bias of the included articles were evaluated by two researchers independently using the criteria of the Newcastle-Ottawa scale (NOS) and the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Analytical Cross-Sectional Studies, respectively. The JBI scale has nine questions to answer, divided between the participant domains (questions 1, 2, 4, and 9), measurement of results (questions 6 and 7), and statistics (questions 3, 5, and 8). A paper was classified as high quality when the methods were appropriate in all domains.(12) The NOS is graded through a star system from 0 to 9, delimited into three domains (selection, comparability, and result). Higher grades represent better quality.(13)
Data analysis
The variables were collected and tabulated in a spreadsheet to compose the results. Quantitative variables are reported as mean ± standard deviation or median (interquartile range). Categorical variables are given as absolute number (n) and frequency (%). All analyses were conducted using the Microsoft Excel 2013 descriptive statistics package.
RESULTS
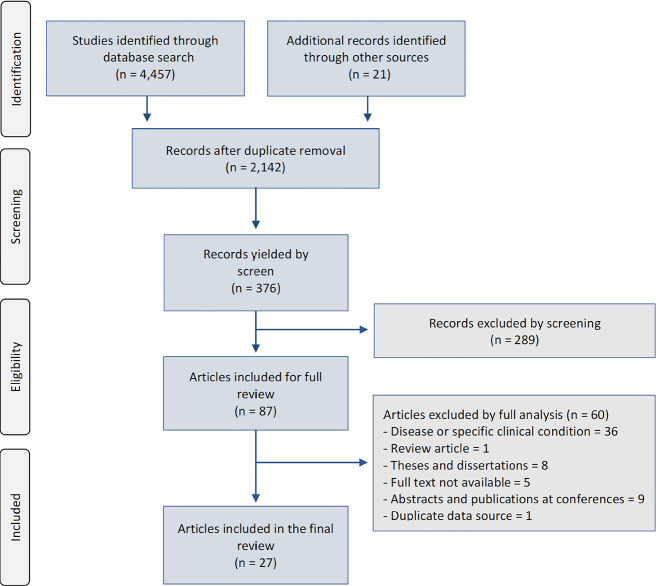
The research strategy yielded a total of 4,478 studies. After removing duplicates and screening the titles and abstracts, 87 studies were selected for verification of the full text, of which 27 were eligible to be evaluated by this review (Figure 1).
Figure 1.
Flowchart of the review study.
Characteristics of the studies
Of the 27 eligible studies (Table 2), 18 were descriptive, with a quantitative and retrospective approach,(15,17-20,24,26-28,30-32,34-39) and seven were prospectively performed.(14,16,22,23,25,29,40) Data from all studies were collected from patient records, sector record books, and computerized database systems.
Table 2.
Characteristics of the studies and institutions included
| Study | Year | State | Study design | ICU (n) | Sample (n) |
|---|---|---|---|---|---|
| Acuña et al.(14) | 2007 | Acre | Prospective | 1 | 79 |
| Albuquerque et al.(15) | 2017 | Rio de Janeiro | Cross -sectional | 1 | 573 |
| Bezerra et al.(16) | 2012 | Paraíba | Prospective | 1 | 140 |
| Castro et al.(17) | 2016 | Goiás | Retrospective | 3 | 2.579 |
| Cruz et al.(18) | 2019 | Mato Grosso | Retrospective | 1 | 86 |
| El-Fakhouri et al.(19) | 2016 | São Paulo | Retrospective | 1 | 2.022 |
| Favarin et al.(20) | 2012 | Rio Grande do Sul | Retrospective | 1 | 104 |
| França et al.(21) | 2013 | Paraíba | Cross -sectional | 1 | 102 |
| Freitas et al.(22) | 2010 | Paraná | Prospectivo | 4 | 146 |
| Galvão et al.(23) | 2019 | Paraná | Prospectivo | 1 | 3.711 |
| Guia et al.(24) | 2015 | Federal District | Retrospective | 1 | 189 |
| Marques et al.(25) | 2020 | Sergipe | Prospective | 1 | 43 |
| Matias et al.(26) | 2018 | Mato Grosso | Retrospective | 1 | 1.024 |
| Melo et al.(27) | 2014 | São Paulo | Retrospective | 1 | 479 |
| Nascimento et al.(28) | 2018 | Paraíba | Retrospective | 1 | 100 |
| Nogueira et al.(29) | 2009 | Ceará | Prospective | 1 | 157 |
| Nogueira et al.(30) | 2012 | São Paulo | Retrospective | 4 | 600 |
| Pauletti et al.(31) | 2017 | Rio de Janeiro | Retrospective | 2 | 975 |
| Perão et al.(32) | 2016 | Santa Catarina | Retrospective | 1 | 190 |
| Del Painter et al.(33) | 2015 | Paraná | Cross -sectional | 1 | 264 |
| Queiroz et al.(34) | 2013 | Rio Grande do Norte | Retrospective | 1 | 371 |
| Rodriguez et al.(35) | 2016 | Santa Catarina | Retrospective | 1 | 695 |
| Silva et al.(36) | 2008 | Maranhão | Retrospective | 1 | 297 |
| Silva et al.(37) | 2017 | Bahia | Retrospective | 1 | 284 |
| Soares et al.(38) | 2015 | Mix* | Retrospective | 78 | 59.693 |
| Sousa et al.(39) | 2014 | Paraíba | Retrospective | 1 | 310 |
| Vieira et al.(40) | 2012 | Federal District | Prospective | 1 | 67 |
ICU - intensive care unit.
Bahia, Ceará, Federal District, Espírito Santo, Maranhão, Minas Gerais, Paraíba, Pernambuco, Rio de Janeiro, São Paulo, and Rio Grande do Sul.
In total, the studies investigated 113 ICUs, 63 of them private, 22 public, and the others philanthropic, university, or mixed institutions. They were most often located in the Northeast region (33.3%), followed by the South region (22.3%), Southeast region (18.5%), Central-West region (18.5%), and the North region (3.7%). One study was conducted in more than one region.(40) Some 81.5% of the studies were published in 2012 or later, especially between 2014 and 2016, and they were conducted predominantly (52%) in private ICUs (Figure 2).
Figure 2.
Overview of the origins of the studies included in the review. Percentage distribution by region (A), by historical series (B), and by the institutional profile of the intensive care unit (C).
ICU - intensive care unit.
Sociodemographic and clinical profile of patients in Brazilian intensive care units
The sample studied in this review was 75,280 individuals, with a predominance of males in 81% of the included studies. The age of participants monitored in the ICUs ranged from a minimum age of 12 years to a maximum of 104 years, with a predominance of mean ages greater than 50 years. There was a predominance of married individuals,(14,18,27,28) the white and brown races,(14,19,28) and low educational levels.(14,19,27) Only one study identified religion, showing a predominance of Catholics (75.1%)(24) (Table 3).
Table 3.
Sociodemographic characteristics of patients admitted to adult intensive care units in Brazil in 2007 - 2020
| Study | Male sex (%) | Age (mean ± standard deviation) | Marital status (%) | Education (%) | Race (%) | Religion (%) |
|---|---|---|---|---|---|---|
| Acuña et al.(14) | 67.1 | 53.3 ± 18.6 | 59.5 married | 43 with <4 four years of study | 59.5 white | - - |
| Albuquerque et al.(15) | 53.0 | 66.5 ±19.4 | - - | - - | - - | - - |
| Bezerra et al.(16) | 49.6 | 65.8 ± 18.7 | - - | - - | - - | - - |
| Castro et al.(17) | 56.0 | 59.0 | - - | - - | - - | - - |
| Cruz et al.(18) | 43.1 | 39-59 years: 36.1%* | 53.4 married | - - | - - | - - |
| El-Fakhouri et al.(19) | 57.9 | 56.6 ± 19.18 | - - | 63.3 primary school | 77.1 white | 75.1 Catholic; 18.0 Protestant |
| Favarin et al.(20) | 58.0 | 64.8 ± 5.6 | - - | - - | - - | - - |
| França et al.(21) | 55.9 | 53.2 | - - | - - | - - | - - |
| Freitas et al.(22) | 53.8 | 60.5 ± 19.2 | - - | - - | - - | - - |
| Galvão et al.(23) | 59.0 | 60.0 | - - | - - | - - | - - |
| Guia et al.(24) | 43.4 | 77.4 ± 10.9 | - - | - - | - - | - - |
| Marques et al.(25) | 55.8 | 68.0 ± 19.3 | - - | - - | - - | - - |
| Matias et al.(26) | 60.0 | 62-71 years: 33.2%* | - - | - - | - - | - - |
| Melo et al.(27) | 64.9 | 49.0† | 45.5 married | 72.4 primary; 2.3 high school | - - | - - |
| Nascimento et al.(28) | 58.0 | 58.8 | 48.0 married | - - | 65.0 brown | - - |
| Nogueira et al.(29) | 56.7 | 66.0 | - - | - - | - - | - - |
| Nogueira et al.(30) | 56.5 | 60.8 ± 18.7 | - - | - - | - - | - - |
| Pauletti et al.(31) | 58.4 | - - | - - | - - | - - | - - |
| Perão et al.(32) | 60.5 | - - | - - | - - | - - | - - |
| Del Painter et al.(33) | - - | 57.3 ± 19.8 | - - | - - | - - | - - |
| Queiroz et al.(34) | 51.4 | 64.8 ± 19.6 | - - | - - | - - | - - |
| Rodriguez et al.(35) | 61.6 | 50.0 | - - | - - | - - | - - |
| Silva et al.(36) | 44.6 | - - | - - | - - | - - | - - |
| Silva et al.(37) | 53.9 | - - | - - | - - | - - | - - |
| Soares et al.(38) | 49.9 | 62.0 ± 2.0 | - - | - - | - - | - - |
| Sousa et al.(39) | 54.8 | - - | - - | - - | - - | - - |
| Vieira et al.(40) | 58.2 | 49.3 ± 18.9 | - - | - - | - - | - - |
Age expressed as frequency (%) by age group; † median.
The mean length of stay in the ICU ranged from 1 to 23 days. The mortality rate reported in the studies ranged from 9.6% to 58%. Only eight studies(14,22-24,30,36,38,40) indicated the severity of the patients by means of prognostic indices, Acute Physiology and Chronic Health Evaluation II (APACHE II) being the most used. Approximately 63% of the studies showed a predominance of clinical emergencies.
Regarding the causes of ICU admission, there was a wide variety of described diseases, though cardiovascular disease (CVD) predominated in 66.7% of the included studies. The therapeutic interventions applied to critically ill patients have rarely been addressed in studies. The use of IMV was evaluated in eight studies,(14,16,23-25,31,38,40) in which it was used in 10.7% to 74.3% of patients. The use of vasoactive drugs was addressed in five studies,(23-25,38,40) and renal replacement therapy was addressed in only three studies(14,39,40) (Table 4).
Table 4.
Clinical characteristics of patients admitted to adult intensive care units in Brazil in 2007-2020
| Study | Main cause of ICU admission | Surgical profile (%) | ICU stay (days; mean ± standard deviation) | Prognostic indices (mean ± standard deviation) | Mortality in the ICU (%) | Therapeutic interventions (%) | ||
|---|---|---|---|---|---|---|---|---|
| MV | VAD | Hemodialysis | ||||||
| Acuña et al.(14) | Multiple-organ dysfunction syndrome | 44.3 | 10.2 ± 9.6 | APACHE II (18.4 ± 9.1) | 38.0 | 51.9 | - - | 18.9 |
| Albuquerque et al.(15) | Neurological diseases | 42.0 | 10.7 ± 18.8 | - - | 26.0 | - - | - - | - - |
| Bezerra et al.(16) | Cardiovascular diseases | - - | 5.5 ± 5.6 | - - | 47.8 | 74.3 | - - | - - |
| Castro et al.(17) | Cardiovascular diseases | 37.0 | 7.6 | - - | 31.0 | - - | - - | - - |
| Cruz et al.(18) | Cardiovascular diseases | 34.9 | ≤ 10 | - - | 23.3 | - - | - - | - - |
| El-Fakhouri et al.(19) | Cardiovascular diseases | - - | 8.0 ± 10.7 | - - | 24.3 | - - | - - | - - |
| Favarin et al.(20) | Infectious diseases | 17.0 | 14.0 | - - | 50.0 | - - | - - | - - |
| França et al.(21) | Cardiovascular diseases | - - | 7.6 | - - | 48.0 | - - | - - | - - |
| Freitas et al.(22) | - - | 37.0 | 23.2 ± 23.7 | APACHE II (20 ± 7.3) | 58.2 | - - | - - | - - |
| Galvão et al.(23) | Sepsis | 38.7 | 16* | APACHE II (19) | 32.2 | 10.7 | 7.1 | - - |
| Guia et al.(24) | Respiratory diseases | - - | 13.1 ± 6.1 | APACHE II (1.6 ± 10.6) | 38.6 | 56.6 | 50.8 | - - |
| Marques et al.(25) | Cardiovascular diseases | 44.9 | 10 ± 8 | - - | - - | 16.3 | 11.6 | - - |
| Matias et al.(26) | Cardiovascular diseases | - - | - - | - - | 23.5 | - - | - - | - - |
| Melo et al.(27) | Cardiovascular and respiratory diseases | 25.8 | 11.4 | - - | 35.3 | - - | - - | - - |
| Nascimento et al.(28) | Cardiovascular diseases | 32.0 | 10.6 | - - | 38.0 | - - | - - | - - |
| Nogueira et al.(29) | Cardiovascular diseases | - - | - - | SAPS II (25.5) | 54.1 | - - | - - | - - |
| Nogueira et al.(30) | Cardiovascular diseases | 36.0 | 9.0 | - - | 20.0 | - - | - - | - - |
| Pauletti et al.(31) | Cardiovascular diseases | 32.0 | - - | - - | 16.1 | 32.9 | - - | - - |
| Perão et al.(32) | Cardiovascular diseases | 40.0 | - - | - - | 25.1 | - - | - - | - - |
| Del Painter et al.(33) | - | - | - | - | - | - | - | - |
| Queiroz et al.(34) | Cardiovascular diseases | 10.0 | 3.4 ± 3.7 | - - | 30.2 | - - | - - | - - |
| Rodriguez et al.(35) | Cardiovascular diseases | 52.5 | 6.0 | - - | 20.4 | - - | - - | - - |
| Silva et al.(36) | Neurological diseases | 69.0 | 5.4 | APACHE II (20.9) | 18.3 | - - | - - | - - |
| Silva et al.(37) | Cardiovascular diseases | - - | - - | - - | 29.0 | - - | - - | - - |
| Soares et al.(38) | Cardiovascular diseases | 27.9 | 5 ± 9 | SAPS III (43 ± 15) | 9.6 | 15.2 | 12.8 | 2.8 |
| Sousa et al.(39) | Cardiovascular diseases | 12.6 | - - | - - | 46.5 | - - | - - | - - |
| Vieira et al.(40) | Respiratory diseases | 25.4 | - - | APACHE II (25.8 ± 12.7) | 50.7 | 73.1 | 58.2 | 50.7 |
ICU - intensive care unit; MV - mechanical ventilation; VAD - vasoactive drugs; APACHE II - Acute Physiology and Chronic Health Evaluation; SAPS - Simplified Acute Physiology Score.
Median.
Methodological quality of the selected studies
The quality of the studies was analyzed by the NOS (Table 5). The 27 included studies had a mean score of 3, a minimum of 1, and a maximum of 6 stars, which are considered bad scores because the highest score is 10. The risk of bias was assessed using the JBI checklist (Table 6).
Table 5.
Newcastle-Ottawa scale of the included studies
| Author | Representativeness of the sample (*****) | Comparability (**) | Result (***) | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 (**) | 2 (*) | 3 (*) | 4 (***) | 1 (**) | 1 (*****) | 2 (*) | |||||||
| a (*) | b (*) | a (*) | a (*) | a (**) | b (*) | a (*) | b (*) | a (**) | b (**) | c (*) | a (*) | ||
| Acuña et al.(14) | * | * | ** | ||||||||||
| Albuquerque et al.(15) | * | * | * | * | * | ***** | |||||||
| Bezerra et al.(16) | * | * | * | * | **** | ||||||||
| Castro et al.(17) | * | * | |||||||||||
| Cruz et al.(18) | * | * | * | *** | |||||||||
| El-Fakhouri et al.(19) | * | * | * | *** | |||||||||
| Favarin et al.(20) | * | * | * | * | **** | ||||||||
| França et al.(21) | * | * | * | * | * | ***** | |||||||
| Freitas et al.(22) | * | * | |||||||||||
| Galvão et al.(23) | * | * | * | * | * | ***** | |||||||
| Guia et al.(24) | * | * | * | * | **** | ||||||||
| Marques et al.(25) | * | * | * | *** | |||||||||
| Matias et al.(26) | * | * | * | *** | |||||||||
| Melo et al.(27) | * | * | ** | ||||||||||
| Nascimento et al.(28) | * | * | ** | ||||||||||
| Nogueira et al.(29) | * | * | * | * | * | ***** | |||||||
| Nogueira et al.(30) | * | * | * | * | * | ***** | |||||||
| Pauletti et al.(31) | * | * | * | *** | |||||||||
| Perão et al.(32) | * | * | |||||||||||
| Del Painter et al.(33) | * | * | |||||||||||
| Queiroz et al.(34) | * | * | * | * | **** | ||||||||
| Rodriguez et al.(35) | * | * | * | * | * | ***** | |||||||
| Silva et al.(36) | * | * | |||||||||||
| Silva et al.(37) | * | * | * | *** | |||||||||
| Soares et al.(38) | * | * | * | * | * | ***** | |||||||
| Sousa et al.(39) | * | * | |||||||||||
| Vieira et al.(40) | * | * | |||||||||||
Table 6.
Intrastudy risk of bias of the included studies according to the Joanna Briggs Institute Critical Appraisal Checklist for Analytical Cross-Sectional Studies
| Author | Were the inclusion criteria in the sample clearly defined? | Were the study subjects and the environment described in detail? | Was exposure measured in a valid and reliable manner? | Were objective and standardized criteria used to measure the condition? | Have confounding factors been identified? | Were strategies established to deal with confounding factors? | Were the outcomes measured in a valid and reliable manner? | Was appropriate statistical analysis used? |
|---|---|---|---|---|---|---|---|---|
| Acuña et al.(14) | No | No | Yes | Yes | No | Not applicable | Yes | Yes |
| Albuquerque et al.(15) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Bezerra et al.(16) | Yes | Yes | Yes | No | No | Not applicable | Yes | Yes |
| Castro et al.(17) | No | Yes | Yes | Not clear | No | Not applicable | Not clear | Not clear |
| Cruz et al.(18) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | No |
| El-Fakhouri et al.(19) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | No |
| Favarin et al.(20) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | No |
| França et al.(21) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Freitas et al.(22) | No | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Galvão et al.(23) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Guia et al.(24) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Marques et al.(25) | Yes | Yes | No | Yes | No | Not applicable | Yes | Not clear |
| Matias et al.(26) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Melo et al.(27) | Yes | Yes | Yes | Yes | No | Not applicable | Not clear | Not clear |
| Nascimento et al.(28) | No | Yes | Yes | Yes | Yes | No | Yes | No |
| Nogueira et al.(29) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Nogueira et al.(30) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Pauletti et al.(31) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Perão et al.(32) | No | No | Not clear | Not clear | No | Not applicable | Not clear | Not clear |
| Del Painter et al.(33) | No | Yes | Yes | Yes | No | Not applicable | Yes | No |
| Queiroz et al.(34) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Rodriguez et al.(35) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | No |
| Silva et al.(36) | No | No | Yes | Yes | No | Not applicable | Not clear | Not clear |
| Silva et al.(37) | No | No | Yes | Yes | No | Not applicable | Not clear | Not clear |
| Soares et al.(38) | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Sousa et al.(39) | Yes | Yes | Yes | Not clear | No | Not applicable | Not clear | Not clear |
| Vieira et al.(40) | No | Yes | Yes | Yes | No | Yes | Yes | Yes |
DISCUSSION
The present study identified the profile of Brazilian ICUs, characterizing them by the sex, age group, cause of ICU admission, length of stay, and ICU mortality of their patients as well as the most commonly used disease severity assessment system. These results are relevant because they allow us to understand the profile of both the user and the intensive care services and resources offered. Twelve of the 27 studies in this review reported that the ICU evaluated was the one primarily responsible for meeting the demand of the region, meaning that it received patients from other municipalities, which resulted in the overload of the service,(14,16,17,19,24,26,28,29,32,33,37,40) the reallocation of more technological and human resources to these units, and the expansion of the network. This review found a predominance of male patients in the analyzed ICUs, which corroborates the findings of other studies.(41) The factors that lead to the greater vulnerability of this population are the sociocultural construction of masculinity, neglect of risk control, poorer prevention of diseases and their complications, lower or late adherence to primary and secondary health services, inefficiency of specific policies, fear of serious illness, shame of exposing the body, absence of specialized units for human health, limited availability of public services, and more accidents and violence.(17,19,28,32,34,35,38,39)
There was a predominance of patients older than 60 years admitted to the ICUs. Studies have estimated that 60% of ICU beds are occupied by patients older than 65 years, and the average length of stay of this group is 7 times greater than that of the younger population.(8) The management of critically ill elderly patients is a complex issue that involves understanding the demographic changes of society and the physiology of aging. Decisions about the care of these patients in the ICU are based on criteria such as the reversibility of the causes of acute health deterioration, life expectancy, the baseline level of function of the patient, the severity of the disease, previous health status, and compliance with the patients’ and family members’ desire to perform invasive measures.(42-44)
In this review, the main cause of hospitalization in Brazilian ICUs was CVD. Brazil is among the countries with the highest mortality rate from CVD.(45,46) Patients with these conditions require hospitalization in cardiac ICUs, coronary ICUs, or cardiothoracic surgery recovery units of to stabilize their clinical condition. In Brazil, the regional variations in the mortality rate from CVD can be attributed to specific profiles of the regions, which have different geographic characteristics, epidemiological characteristics, and organization of health services(47,48)
The ICU stay in this review ranged from 1 to 23 days. This measure is an important indicator of productivity and for planning care, as it reflects the peculiarities of the profile of each population.(19,49) The patient’s stay in the ICU should be made as short as possible by reversing the acute condition to allow the patient to be transferred to another hospital unit of less complexity, avoiding the inappropriate use of the ICU.(16,27,39) That is, in those with a high risk of death and limited medical care, interventions that painfully prolong the dying process should be avoided.(50,51) In this context, the inclusion of palliative care in the ICU has been an important way to shorten ICU stays and lower overall health costs without hastening death, providing effective management of the pain and suffering of patients and their family members at the end of life.(52)
The studies in this review showed ICU mortality rates between 9.6% and 58%. Some factors associated with death were a longer stay (> 8 days), advanced age, greater disease severity (APACHE II > 20 points), comorbidities, decline in previous functional status, use of mechanical ventilation or vasoactive amines, acute renal failure, sepsis, and quality of care provided, which corroborates the findings of other national and international publications.(53.54) Importantly, the mortality of critically ill patients admitted to the ICU may also be related to the natural evolution of the disease after the therapeutic possibilities have been exhausted.(15)
Few included studies used assessment systems for disease severity in the ICU. In recent decades, several scoring systems have been developed, among which APACHE II remains the most commonly used.(40,55) The studies also rarely mentioned invasive therapies in the ICU. The use of MV, acute renal failure requiring renal replacement therapy, and the use of vasoactive drugs are factors associated with prolonged hospitalization and increased risk of morbidity and mortality.(56) Knowing the therapeutic profile of ICUs is essential for the management of critical patients and the clinical and strategic decision-making of a healthcare unit.
This study has some strengths. It is the first systematic review to identify the profile of Brazilian ICUs in general based on published data, including studies from all regions of the country, with different kinds of institutions and a large final sample, which improves the representativeness of this study. Some of the results of this study agree with those of international studies. In the future, studies with greater methodological rigor and homogeneity of information should be done to allow meta-analyses to be run on their data, which would contribute to the consolidation of the national literature focused on high-complexity care.
This review also has some limitations. Observational studies are more vulnerable to methodological problems, which precluded a systematic review with meta-analysis. There was the possibility of publication bias: given our objective of delivering a broad and general characterization of ICUs, it is possible that some studies in specific populations did not meet the selection criteria for this review. Even so, to minimize the occurrence of this bias and gather as many results as we could, the literature search was broad, including in national and international scientific databases. It is also noteworthy that most of the included publications retrospectively profiled their ICUs, which could bring some information bias. Our evaluation of the quality of the studies highlighted methodological deficiencies.
CONCLUSION
This systematic review on the profile of Brazilian intensive care units indicated that a growing number of studies have been conducted in different Brazilian regions in recent years, especially in public and general intensive care units covering all clinical specialties. Regarding the profile of these units, there was a predominance of male patients with a mean age greater than 50 years and elderly patients. Cardiovascular disease was the main cause of hospitalization in these intensive care units. The length of stay and mortality varied widely between institutions, depending on factors such as severity profile and region of residence of the patients. APACHE II is the disease severity assessment system most commonly used in Brazilian intensive care units, and most patients come from clinical emergency units. Few studies have investigated the sociodemographic characteristics or therapeutic interventions in intensive care units, which will be important to cover in new studies.
These results can help guide the planning and organization of intensive care units, both in the management of institutions and in regard to clinical practice, as they can support decision-making and the implementation of interventions to ensure better quality of patient care. We suggest conducting studies that better describe Brazilian intensive care units, using more rigorous methodological criteria and ensuring a higher quality of publications.
Footnotes
Conflicts of interest: None.
Responsible editor: Jorge Ibrain Figueira Salluh
REFERENCES
- 1.Lisboa DD, Medeiros EF, Alegretti LG, Badalotto D, Maraschin R. Perfil de pacientes em ventilação mecânica invasiva em uma unidade de terapia intensiva. J Biotec Biodivers. 2012;3(1):18–24. [Google Scholar]
- 2.Lanetzki CS, Oliveira CA, Bass LM, Abramovici S, Troster EJ. The epidemiological profile of Pediatric Intensive Care Center at Hospital Israelita Albert Einstein. einstein (Sao Paulo) 2012;10(1):16–21. doi: 10.1590/s1679-45082012000100005. [DOI] [PubMed] [Google Scholar]
- 3.Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yearb Med Inform. 2000;(1):65–70. [PubMed] [Google Scholar]
- 4.Brasil . Síntese de evidências para políticas de saúde: estimulando o uso de evidências científicas na tomada de decisão. 2a. Brasília: Ministério da Saúde; EVIPNet Brasil;; 2016. Ministério da Saúde. Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Departamento de Ciência e Tecnologia. [Google Scholar]
- 5.Viana AL, Bousquat A, Pereira AP, Uchimura LY, Albuquerque MV, Mota PH, et al. Typology of health regions: structural determinants of regionalization in Brazil. Saúde Soc São Paulo. 2015;24(2):413–22. [Google Scholar]
- 6.Bauman KA, Hyzy RC. ICU 2020: five interventions to revolutionize quality of care in the ICU. J Intensive Care Med. 2014;29(1):13–21. doi: 10.1177/0885066611434399. [DOI] [PubMed] [Google Scholar]
- 7.Associação de Medicina Intensiva Brasileira (AMIB) Das UTIs brasileiras. Censo AMIB. 2016. Disponível em: http://www.amib.org.br/censo-amib/censo-amib-2016.
- 8.Conselho Federal de Medicina (CFM) Medicina Intensiva no Brasil . Menos de 10% dos municípios brasileiros possuem leito de UTI [atualizado12/09/2018] Brasília (DF): CFM; 2018. [citado 2018 Nov 11]. 2018. Disponível em: https://portal.cfm.org.br/noticias/menos-de-10-dos-municipios-brasileiros-possuem-leito-de-uti/ [Google Scholar]
- 9.Toledo EF. São Paulo, Rio de Janeiro e Belo Horizonte: a manutenção da concentração socioeconômica nas metrópoles da região sudeste do Brasil. Rev Geográf Am Central. 2011;2(47E):1–16. [Google Scholar]
- 10.Viacava F, Xavier DR, Bellido JG, Matos VP, Magalhães MA, Velasco W. Relatório de pesquisa sobre internações na esfera municipal. Rio de Janeiro: Ministério da Saúde, Fiocruz; 2014. Saúde Amanhã. Projeto Brasil Saúde Amanhã. [Google Scholar]
- 11.Galvão TF, Pansani TS, Harrad D. Principais itens para relatar revisões sistemáticas e meta-análises: a recomendação PRISMA. Epidemiol Serv Saúde. 2015;24(2):335–42. [Google Scholar]
- 12.Joanna Briggs Institute . Methodology for JBI Scoping Reviews. Australia: Joanna Briggs Institute; 2015. The Joanna Briggs Institute. Reviewers’ Manual 2015. Available from: https://nursing.lsuhsc.edu/JBI/docs/ReviewersManuals/Scoping-.pdf. [Google Scholar]
- 13.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 14.Acuña K, Costa E, Grover A, Camelo A, Santos R., Júnior Características clínico-epidemiológicas de adultos e idosos atendidos em unidade de terapia intensiva pública da Amazônia (Rio Branco, Acre) Rev Bras Ter Intensiva. 2007;19(3):304–9. [PubMed] [Google Scholar]
- 15.Albuquerque JM, Silva RF, Souza RF. Perfil epidemiológico e seguimento após alta de pacientes internados em unidade de terapia intensiva. Cogitare Enferm. 2017;22(3):1–9. [Google Scholar]
- 16.Bezerra GK. Unidade de Terapia Intensiva - Perfil das Admissões: Hospital Regional de Guarabira, Paraíba, Brasil. Rev Bras Ci Saúde. 2012;16(4):49–6. [Google Scholar]
- 17.Castro RR, Barbosa NB, Alves T, Najberg E. Perfil das internações em unidades de terapia intensiva adulto na cidade de Anápolis - Goiás - 2012. Rev Gest Sist Saúde. 2016;5(2):115–24. [Google Scholar]
- 18.Cruz YV, Cardoso JD, Cunha CR, Vechia AD. Perfil de morbimortalidade da unidade de terapia intensiva de um hospital universitário. J Health NPEPS. 2019;4(2):230–9. [Google Scholar]
- 19.El-Fakhouri S, Carrasco HV, Araújo GC, Frini IC. Epidemiological profile of ICU patients at Faculdade de Medicina de Marília. Rev Assoc Med Bras. 2016;62(3):248–54. doi: 10.1590/1806-9282.62.03.248. [DOI] [PubMed] [Google Scholar]
- 20.Favarin SS, Camponogara S. Perfil dos pacientes internados na unidade de terapia intensiva adulto de um hospital universitário. Rev Enferm UFSM. 2012;2(2):320–9. [Google Scholar]
- 21.França CD, Albuquerque PR, Santos AC. Perfil epidemiológico da unidade de terapia intensiva de um Hospital Universitário. InterScientia. 2013;1(2):72–82. [Google Scholar]
- 22.Freitas ER. Perfil e gravidade dos pacientes das unidades de terapia intensiva: aplicação prospectiva do escore APACHE II. Rev Lat Am Enferm. 2010;18(3):317–23. [Google Scholar]
- 23.Galvão G, Mezzaroba AL, Morakami F, Capeletti M, Franco O, Filho, Tanita M, et al. Seasonal variation of clinical characteristics and prognostic of adult patients admitted to an intensive care unit. Rev Assoc Med Bras. 2019;65(11):1374–83. doi: 10.1590/1806-9282.65.11.1374. [DOI] [PubMed] [Google Scholar]
- 24.Guia CM, Biondi RS, Sotero S, Lima AA, Almeida KJ, Amorim FF. Perfil epidemiológico e preditores de mortalidade de uma unidade de terapia intensiva geral de hospital público do Distrito Federal. Com Ciências Saúde. 2015;26(1/2):9–19. [Google Scholar]
- 25.Marques CR, Santos MR, Passos KS, Naziazeno SD, Sá LA, Santos ES. Caracterização do perfil clínico e sociodemográfico de pacientes admitidos em uma unidade de terapia intensiva. Interfaces Cient Saúde Ambiente. 2020;8(2):446–56. [Google Scholar]
- 26.Matias G, D’Artibale EF, Almeida MM, Tenuta TF, Caporossi C. Perfil dos pacientes em unidade de terapia intensa em um hospital privado de Mato Grosso no período de 2013 a 2017. COORTE. 2018;(8):16–26. [Google Scholar]
- 27.Melo AC, Menegueti MG, Laus AM. Perfil de pacientes de terapia intensiva: subsídios para equipe de enfermagem. Rev Enferm UFPE. 2014;8(9):3142–8. [Google Scholar]
- 28.Nascimento MS, Nunes EM, Medeiros RC, Souza WI, Sousa LF, Filho, Alves ES. Perfil epidemiológico de pacientes em uma unidade de terapia intensiva adulto de um hospital regional paraibano. Temas Saúde. 2018;18(1):247–65. [Google Scholar]
- 29.Nogueira NA, Sousa PC, Sousa FS. Perfil dos pacientes atendidos em uma Unidade de Terapia Intensiva de um hospital público do Brasil. Inter Science Place. 2009;2(5):1–17. [Google Scholar]
- 30.Nogueira LS, Sousa RM, Padilha KG, Koike KM. Clinical characteristics and severity of patients admitted to public and private ICUS. Texto Contexto Enferm. 2012;21(1):59–67. [Google Scholar]
- 31.Pauletti M, Otaviano ML, Moraes AS, Schneider DS. Perfil epidemiológico dos pacientes internados em um Centro de Terapia Intensiva. Aletheia. 2017;50(1-2):38–46. [Google Scholar]
- 32.Perão OF, Bub MB, Zandonadi GC, Martins MA. Características sociodemográficas e epidemiológicas de pacientes internados em uma unidade de terapia intensiva de adultos. Rev Enferm UERJ. 2016;25:e7736. [Google Scholar]
- 33.Del Pintor R, de Moraes Gil NL. Perfil epidemiológico dos pacientes internados na unidade de terapia intensiva do Hospital Santa Casa de Campo Mourão PR. Rev Catarse. 2015;2(1):85–95. [Google Scholar]
- 34.Queiroz F, Rego D, Nobre G. Morbimortalidade na unidade de terapia intensiva de um hospital público. Rev Baiana Enferm. 2013;27(2):164–71. [Google Scholar]
- 35.Rodriguez AH, Bub MB, Perão OF, Zandonadi G, Rodriguez MJ. Epidemiological characteristics and causes of deaths in hospitalized patients under intensive care. Rev Bras Enferm. 2016;69(2):210–4. doi: 10.1590/0034-7167.2016690204i. [DOI] [PubMed] [Google Scholar]
- 36.Silva JM, Pimentel MI, Silva MC, Araújo RJ, Barbosa MC. Perfil dos pacientes da unidade de terapia intensiva de um hospital universitário. Rev Hosp Univ UFMA. 2008;9(2):37–41. [Google Scholar]
- 37.Silva JS, Maciel RR, Carvalho LS, Oliveira NQ. Perfil de pacientes críticos de um hospital/maternidade do Estado da Bahia. Rev Estação Científica. 2017;(Ed esp):1–11. [Google Scholar]
- 38.Soares M, Bozza FA, Angus DC, Japiassú AM, Viana WN, Costa R, et al. Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med. 2015;41(12):2149–60. doi: 10.1007/s00134-015-4076-7. [DOI] [PubMed] [Google Scholar]
- 39.Sousa MN, Cavalcante AM, Sobreira RE, Bezerra AL, Assis EV, Feitosa AN. Epidemiologia das internações em uma unidade de terapia intensiva. C&D Rev Eletron Fainor. 2014;7(2):178–86. [Google Scholar]
- 40.Vieira MS. Perfil geográfico e clínico de pacientes admitidos na UTI através da Central de Regulação de Internações Hospitalares. Comun Ciênc Saúde. 2012;22(3):201–10. [Google Scholar]
- 41.Fowler RA, Filate W, Hartleib M, Frost DW, Lazongas C, Hladunewich M. Sex and critical illness. Curr Opin Crit Care. 2009;15(5):442–9. doi: 10.1097/MCC.0b013e3283307a12. [DOI] [PubMed] [Google Scholar]
- 42.Grigorakos L, Nikolopoulos I, Sakagianni K, Markou N, Nikolaou D, Kechagioglou I, et al. Intensive care management of the critically ill elderly population: the case of ‘Sotiria’ Regional Chest Diseases Hospital of Athens, Greece. J Nurs Health Care. 2015;2(2):1–4. [Google Scholar]
- 43.Marik PE. Management of the critically ill geriatric patient. Crit Care Med. 2006;34(9 Suppl):S176–82. doi: 10.1097/01.CCM.0000232624.14883.9A. [DOI] [PubMed] [Google Scholar]
- 44.Nguyen YL, Angus DC, Boumendil A, Guidet B. The challenge of admitting the very elderly to intensive care. Ann Intensive Care. 2011;1(1):29. doi: 10.1186/2110-5820-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mayr VD, Dunser MW, Greil V, Jochberger S, Luckner G, Ulmer H, et al. Causes of death and determinants of outcome in critically ill patients. Crit Care. 2006;10(6):R154. doi: 10.1186/cc5086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Freire AK, Alves NC, Santiago EJ, Tavares AS, Teixeira DS, Carvalho IA, et al. Panorama no Brasil das doenças cardiovasculares dos últimos quatorze anos na perspectiva da promoção à saúde. Rev Saúde Desenvol. 2017;11(9):21–44. [Google Scholar]
- 47.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P, American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–e492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 48.Guimarães RM, Andrade SS, Machado EL, Bahia CA, Oliveira MM, Jacques FV. Diferenças regionais na transição da mortalidade por doenças cardiovasculares no Brasil, 1980 a 2012. Rev Panam Salud Publica. 2015;37(2):83–9. [PubMed] [Google Scholar]
- 49.Oliveira AB, Dias OM, Mello MM, Araújo S, Dragosavac D, Nucci A, et al. Fatores associados à maior mortalidade e tempo de internação prolongado em uma unidade de terapia intensiva de adultos. Rev Bras Ter Intensiva. 2010;22(3):250–6. [PubMed] [Google Scholar]
- 50.Ramos JG, Teles Correa MD, de Carvalho RT, Jones D, Forte DN. Clinical significance of palliative care assessment in patients referred for urgent intensive care unit admission: a cohort study. J Crit Care. 2017;37:24–9. doi: 10.1016/j.jcrc.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 51.Kyeremanteng K, Gagnon LP, Thavorn K, Heyland D, D’Egidio G. The impact of palliative care consultation in the ICU on length of stay: a systematic review and cost evaluation. J Intensive Care Med. 2018;33(6):346–53. doi: 10.1177/0885066616664329. [DOI] [PubMed] [Google Scholar]
- 52.Martins BD, Oliveira RA, Cataneo AJ. Palliative care for terminally ill patients in the intensive care unit: systematic review and metaanalysis. Palliat Support Care. 2017;15(3):376–83. doi: 10.1017/S1478951516000584. [DOI] [PubMed] [Google Scholar]
- 53.Gulini JE, Nascimento ER, Moritz RD, Vargas MA, Matte DL, Cabral RP. Predictors of death in an intensive care unit: contribution to the palliative approach. Rev Esc Enferm USP. 2018;52:e03342. doi: 10.1590/S1980-220X2017023203342. [DOI] [PubMed] [Google Scholar]
- 54.Ghorbani M, Ghaem H, Rezaianzadeh A, Shayan Z, Zand F, Nikandish R. Predictive factors associated with mortality and discharge in intensive care units: a retrospective cohort study. Electron Physician. 2018;10(3):6540–7. doi: 10.19082/6540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mnatzaganian G, Bish M, Fletcher J, Knott C, Stephenson J. Application of accelerated time models to compare performance of two comorbidity-adjusting methods with APACHE II in predicting short-term mortality among the critically ill. Methods Inf Med. 2018;57(1):81–8. doi: 10.3414/ME17-01-0097. [DOI] [PubMed] [Google Scholar]
- 56.Mohammadi Kebar S, Hosseini Nia S, Maleki N, Sharghi A, Sheshgelani A. The incidence rate, risk factors and clinical outcome of acute kidney injury in critical patients. Iran J Public Health. 2018;47(11):1717–24. [PMC free article] [PubMed] [Google Scholar]