The COVID-19 sanitary crisis has shed an unprecedented light on the role of modellers, mathematicians, computer scientists and data scientists in the monitoring and in the understanding of the dynamics of an epidemic. The general audience became rapidly acquainted with the concepts of R0, of quasi-exponential growth of the number of cases, as well as with the burden that such an explosive dynamics puts on medical structures. But mathematical and computational approaches have even more to offer.
From the early stages of the pandemic, many organisational issues arose to cope with the wave of patients, which overwhelmed many hospitals and care structures. Emergency call centres faced a sharp increase in the number of calls, which had to be efficiently sorted according to the urgency of the patient’s condition. The saturation of critical care services led to the need to re-orient incoming patients to other hospitals with available beds, or to organise the transfer of patients from a heavily burdened region to a region under a weaker capacity strain. Hospital services had to find humanly manageable ways to deal with the work surplus, in conditions where health workers were not only at risk of physical and psychological exhaustion, but also at risk of being infected with SARS-CoV-2. In this context, already existing collaborations between mathematicians or computer scientists and medical doctors or emergency call centres gave rise to the extraordinarily quick emergence of tools to help operators and medical staff with logistic decisions.
Below, we present four such initiatives, which arose during the first COVID-19 wave in France in 2020. They illustrate what close collaborations between medical staff and researchers from the fields of operations research, modelling of complex dynamics or data sciences can bring to the management of critical situations in health services. Beyond the current pandemic, they also pose the question of how to improve our preparedness to future crises.
ICUBAM – An App for Real-Time ICU Bed Availability Monitoring
The French Grand Est region was severely affected by COVID-19 from the end of February 2020. The capacity to receive mechanically ventilated patients in intensive care, saturating quickly, proved to be a crucial issue in the management of the sanitary crisis. As the circulation of information on the location or capacity of resuscitation beds was difficult, resuscitators expressed the need for a field IT tool dedicated to the management of resuscitation beds. To respond to this request, the ICUBAM application (Intensive Care Unit Bed Activity Monitor) was developed by a consortium of engineers, applied mathematicians and computer scientists from École polytechnique, INRIA and the University Hospital of Nancy.
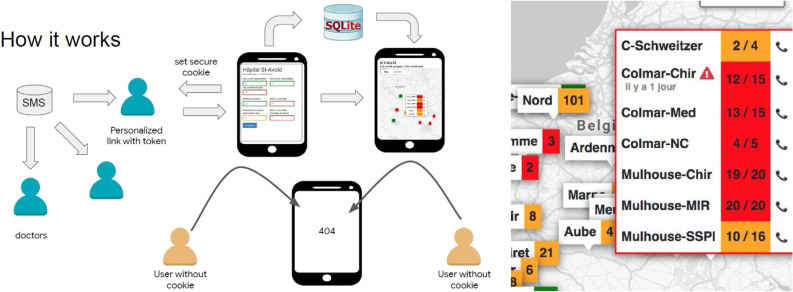
ICUBAM enables the network of resuscitators to add information to a database in real time (in particular on the reception capacity of their unit) via their mobile phone, and to turn it into a cartographic visualisation (Fig. 1 ). Its efficiency results from the direct involvement of the concerned medical staff, keeping the tool up-to-date, and from the possibility of analysing and visualising the data collected in real time to anticipate the needs in resuscitation beds.
Fig. 1.
Operation scheme of the ICUBAM app and its security protocol (left). Number of available beds over the total number of beds in each unit listed in the app (right). Lines coloured in red indicate that more than 80% of beds are occupied, orange corresponds to 50-80% of occupied beds, and green corresponds to less than 50%.
The project is open-source, available on GitHub [1], and can be deployed easily. ICUBAM was launched at the end of March 2020 in the Grand Est region with the agreement of the Regional Health Agency and in two weeks, it was used by 130 services and a network of 300 resuscitators in 40 French departments, which represents more than 2,000 resuscitation beds that can accommodate a COVID+ patient. ICUBAM collected data during the first three waves of the epidemic and helped resuscitators on a day-to-day basis by measuring and nowcasting the load imposed on resuscitation services during the pandemic [2].
Operations Research Tools for the Sizing of Emergency Call Centres
From 2019, the Tropical research team (INRIA and École polytechnique) collaborated with the Medical Emergency Services of the four departments of the Paris area (SAMU 75, 92, 93 and 94) of the public hospital administration (AP-HP), in charge of the call centres-15. They developed models to determine the staffing necessary for a swift processing of incoming calls. In these models, various chains of actions driven by priority rules are taken into account: after a preliminary treatment by assistants of regulation, the patients are handled by emergency physicians or by general practitioners, resulting in the dispatch of medical teams or ambulances, or in medical advice.
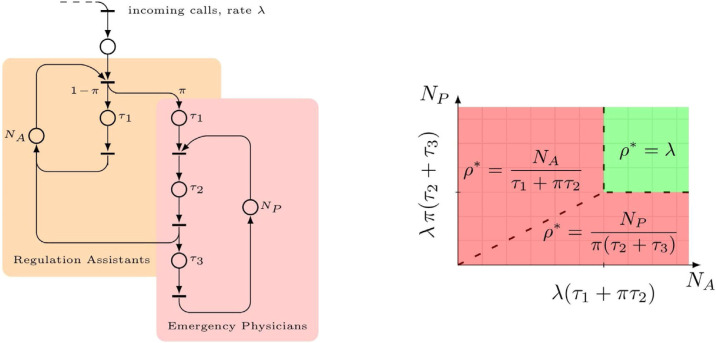
The models use Petri nets, a graphical formalism allowing a detailed description of the processes, while being suited to mathematical analysis (Fig. 2 ). The throughput, i.e. the maximal number of incoming calls per time unit that can be handled, can be computed knowing the staffing (number of assistants, of emergency physicians, etc.), the treatment times of elementary tasks, and the proportions of the different types of calls [3]. These parameters were obtained from the journal files of the phone system.
Fig. 2.
Simplified Petri net representing a SAMU call centre, showing the chains of treatments by medical regulation assistants and emergency physicians (left); the throughput ρ as a function of the number of assistants NA, of the number of physicians NP, of the proportion of urgent calls π, of the conversation times τi and of the input rate λ, following [3] – the congestion-free (sufficiently staffed) region is shown in green (right).
By mid-March 2020, around the peak of contaminations of the first COVID-19 wave, the four SAMU call centres of the Paris area received an unprecedented number of calls. The models had to be extended to capture innovative mechanisms implemented by the physicians, like the deployment of an interactive voice server or the creation of rooms handling COVID-19 calls [4]. The medical classification was exploited: some patients call at early stages of the disease (needing only medical advice), and this can be used to anticipate the load over a horizon of one week for medical emergency services [5] and of around two weeks for ICU admissions [6]. A daily cartography of the epidemic based on the calls to SAMU was thus produced.
These staffing methods are useful independently of the pandemic context. For instance, they may be used to compare different mechanisms of treatment of calls proposed by practitioners.
Regulation of Patients and Allocation of Medical Resources
Despite the rapid dissemination of tools able to monitor resource availability and to forecast demands, early in the COVID-19 crisis health care managers realised they lacked adapted prepared response plans and decision-support tools for patient flow and medical resource management.
The research team of the CNRS lab LIMOS and Mines Saint-Étienne developed several methods and tools to evaluate and support patient flow and resource management decisions. This research is rooted in several studies conducted on emergency management during epidemics or floods [7], [8], [9], [10], home health care services [11] and cancer treatments [12]. All these works do not consider some specificities of pandemics like COVID-19, with the burden put on the complete health care network and the high risk of contamination for patients and caregivers.
Four performance indicators were defined: the number of patients without or with delayed adapted care; the number of urgent transfers of patients; the number of medical procedures postponed or cancelled with a serious impact on the health condition of the patient; the number of health workers who suffered from bad working conditions.
The capacity planning problem assigns roles, resources and case-mix of patients to medical services. Based on the analysis of optimal conditions of the underlying stochastic dynamic problem, the solution [13] proposes a staggering resource assignment plan with a low risk of patient rejection, enough time for implementation, and a minimal wasted capacity. Several patient flow control policies through the care network are evaluated in a discrete event simulation framework that models several care pathways including hospitalisation, intensive care and follow-up care. This tool allows to determine the best strategies for patient admission and transfers in different hospitals. The main parameter of each strategy is a threshold on the occupancy rate, which triggers rejections and transfers.
The current projects aim to extend these tools to larger networks with more complex care pathways and caregivers acceptance of reorganisation, and to compute standardised guidelines for decision makers on several pandemic scenarios.
ONADAP - A Digital Tool to Help with Staff Organisation and Resource Allocation in Hospitals in Conditions of High Pressure on Personnel Availability During an Epidemic
The Borelli Centre (ENS Paris-Saclay) and the Percy Army Training Hospital, with the Institute of Biomedical Research of the Army (IRBA) and the INSEAD business school as partners, imagined the software platform ONADAP to support decision-making for human resource allocation and spatial reorganisation of services and pathways. This digital platform was delivered in January 2022 to operate at the scale of a care unit and pursues the following main objectives:
-
-
Provide a monitoring tool to follow the propagation of COVID-19 among the medical staff (number of symptomatic individuals, COVID+ and COVID-, etc.), at the level of the whole hospital, and to propose short-term projections in terms of human resources (sick leaves, returns from leaves, categories of missing staff, etc.) in each unit.
-
-
Simulate alternative organisation schemes based on artificial intelligence algorithms to support decision-making from the perspective of hospital management. These algorithms make use of the data collected and rely on epidemiological models for micro-communities to anticipate the efficiency of each strategy in terms of risk indicators describing the situation of the hospital.
The ONADAP project revealed that, while it was difficult to translate the state-of-the-art of epidemic modelling in specific prevention and control actions at the level of state policies during the pandemic, it was possible to set up an efficient detection system at the level of a single care unit within a few weeks with immediate impact. Furthermore, this initiative also illustrated how fruitful the retro-transfer from field experts dealing with issues in the real world to academic researchers may be, since ONADAP nourished a series of works developed by researchers from the consortium on various topics related to mathematical models in the context of the pandemic such as graph inference based on epidemic models [14], modelling of the phylogeny of SARS-CoV-2 [15], methodological review on epidemic models used for SARS-CoV-2 [16], exit policies with differential screening of the population [17], symptom-serology correlation at Percy hospital [18] and accurate estimation of the reproduction number [19].
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgements
T.G. acknowledges the Hospital William Morey of GHT Bourgogne Méridionale, the two Regional Health Agencies, ARS Auvergne-Rhône-Alpes and ARS Bourgogne-Franche-Comté, the University Hospital of Saint-Étienne and the MODCOV19 CNRS platform for their collaboration, their expertise and their financial support. S.G. thanks the emergency physicians of SAMU 75, 92, 93, 94 and other AP-HP members, together with the INRIA researchers, PhD students and engineers, with whom the collective work on medical emergency call centres was performed. He thanks especially Xavier Allamigeon and Marin Boyet. He also thanks members of the INRIA administration and other contributors; see [5] for detailed credits. He thanks SAMU 69 and SAMU 77 for additional insights. He thanks the programme direction of PFAU (Plateforme d'appels d'urgence 17-18-112), and students of École polytechnique and CMAP with whom models of call centres were initially developed. J.J. would like to thank Antoine Kimmoun (the intensivist in Nancy at the origin of ICUBAM), Gabriel Dulac-Arnold (Google), Olivier Teboul (Google), and Hugues Berry (INRIA) for their invaluable work for the project and all the members of the ICUBAM consortium. N.V. warmly thanks the AID (Agence Innovation Défense) who funded ONADAP between May 2020 and January 2022 and made the research described here possible, but also Professor Damien Ricard (neurology service, Percy hospital) who was the initiator of this project, as well as the PhD students of Centre Borelli for their engagement during the pandemic, and Brian Tervil who was the master of project management in ONADAP while being an expert in algebraic geometry. A.V. acknowledges support from the MODCOV19 platform.
References
- 1.The ICUBAM consortium ICUBAM - ICU Bed Availability Monitor (GitHub repository) 2020. https://github.com/icubam
- 2.ICUBAM Consortium, Bonnasse-Gahot L., Dénès M., Dulac-Arnold G., Girgin S., Husson F., et al. ICUBAM: ICU Bed Availability Monitoring and analysis in the Grand Est region of France during the COVID-19 epidemic. To appear in Statistique et Société. 2022. https://www.medrxiv.org/content/10.1101/2020.05.18.20091264v1
- 3.Allamigeon X., Boyet M., Gaubert S. Piecewise Affine Dynamical Models of Timed Petri Nets -- Application to Emergency Call Centers. Fundamentae Informaticae. 2021;183(3-4):169–201. [Google Scholar]
- 4.Télion C., Marx J.-S., Dautreppe C., Carli P. Feedback on the Regulation of Samu de Paris during the COVID-19 Crisis (in French) Ann. Fr. Med. Urgence. 2020;10:202–211. [Google Scholar]
- 5.Gaubert S., Akian M., Allamigeon X., Boyet M., Colin B., Grohens Th., et al. Understanding and monitoring the evolution of the Covid-19 epidemic from medical emergency calls: the example of the Paris area. Comptes Rendus -- Mathématique. 2020;358(7):843–875. [Google Scholar]
- 6.The COVID-19 APHP-Universities-INRIA-INSERM Group Early indicators of intensive care unit bed requirement during the COVID-19 epidemic: A retrospective study in Ile-de-France region, France. PLoS ONE. 2020;15(11) doi: 10.1371/journal.pone.0241406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Rifai O., Garaix T., Augusto V., Xie X. A stochastic optimization model for shift scheduling in emergency departments. Health care management science. 2015;18(3):289–302. doi: 10.1007/s10729-014-9300-4. [DOI] [PubMed] [Google Scholar]
- 8.El-Rifai O., Garaix T., Xie X. Proactive on-call scheduling during a seasonal epidemic. Operations Research for Health Care. 2016;8:53–61. [Google Scholar]
- 9.Bargetto R., Garaix T., Xie X. Dynamic Insertion of Emergency Surgeries With Different Waiting Time Targets. IEEE Transactions on Automation Science and Engineering. 2018;16(1):87–99. [Google Scholar]
- 10.Zehrouni A., Augusto V., Garaix T., Phan R., Xie X., Denis S., et al. Hospital flood emergency management planning using Markov models and discrete-event simulation. Operations Research for Health Care. 2021;30 [Google Scholar]
- 11.Rodriguez C., Garaix T., Xie X., Augusto V. Staff dimensioning in homecare services with uncertain demands. International Journal of Production Research. 2015;53(24):7396–7410. [Google Scholar]
- 12.Garaix T., Rostami S., Xie X. Daily outpatient chemotherapy appointment scheduling with random deferrals. Flexible Services and Manufacturing Journal. 2020;32(1):129–153. [Google Scholar]
- 13.Breen C., Benoist A., Garaix T., Kirche S., Xie X. Capacity Planning in Intensive Care Unit During a Pandemic Crisis. IEEE 17th International Conference on Automation Science and Engineering; 23-27 August in Lyon; 2021. [Google Scholar]
- 14.Beaufort L.B., Massé P.Y., Reboulet A., Oudre L. Network Reconstruction Problem for an Epidemic Reaction-Diffusion. arXiv preprint. 2021 arXiv:2109.11334. [Google Scholar]
- 15.Laborde Q., Massé P.Y. A New Bayesian Structured Coalescent Approximation That Incorporates Dynamic Epidemiological Data. Preprint Centre Borelli. 2022 [Google Scholar]
- 16.Garin M., Limnios M., Nicolaï A., Bargiotas I., Boulant O., Chick S.E., et al. Epidemic Models for COVID-19 during the First Wave from February to May 2020: a Methodological Review. arXiv preprint. 2021 arXiv:2109.01450. [Google Scholar]
- 17.Evgeniou T., Fekom M., Ovchinnikov A., Porcher R., Pouchol C., Vayatis N. Epidemic Models for Personalised COVID-19 Isolation and Exit Policies Using Clinical Risk Predictions. Production and Operations Management, to appear in 2022. Online demo: https://ipolcore.ipol.im/demo/clientApp/demo.html?id=305. [DOI] [PMC free article] [PubMed]
- 18.Nicolaï A., Moreau A., Ricard D., Tervil B. A retrospective analysis of the relation between self-declared Covid-19 symptoms within hospital staff members and their SARS-CoV-2 serological status prediction. Preprint Centre Borelli. 2022 [Google Scholar]
- 19.Alvarez L., Colom M., Morel J.D., Morel J.M. Computing the daily reproduction number of COVID-19 by inverting the renewal equation using a variational technique. Proceedings of the National Academy of Sciences. 2021;118(50) doi: 10.1073/pnas.2105112118. https://ipolcore.ipol.im/demo/clientApp/demo.html?id=304 1. Online demo: [DOI] [PMC free article] [PubMed] [Google Scholar]