Abstract
This collaborative statement from the Digital Health Committee of the Heart Rhythm Society provides everyday clinical scenarios in which wearables may be utilized by patients for cardiovascular health and arrhythmia management. We describe herein the spectrum of wearables that are commercially available for patients, and their benefits, shortcomings and areas for technological improvement. Although wearables for rhythm diagnosis and management have not been examined in large randomized clinical trials, undoubtedly the usage of wearables has quickly escalated in clinical practice. This document is the first of a planned series in which we will update information on wearables as they are revised and released to consumers.
Keywords: Arrhythmia, Digital health, Remote monitoring, Wearables
Introduction
Consumer and patient relationships with clinicians have changed drastically due to the expanded use of wearable health devices. As patients/consumers gain access to a wide variety of over-the-counter wearable tools, they are empowered by possessing, controlling, and managing their own health data. This shift is redefining the role of consumers and patients in driving their medical management.1,2 Moreover, the technology industry continues to invest in the ability of consumers and patients to self-monitor their health data. Thus, it becomes necessary to account for the patient/consumer in any initiative aiming to expand and guide the use of available wearables in daily clinical practice. On the other hand, clinicians are facing a new and large pipeline of health data from multitudes of wearable devices.3
This document will be annually updated with information on the rapid technology developments to guide the use of wearables among consumers, patients and clinicians. We present common clinical scenarios seen in everyday clinical practice in which the provider will be confronted by health data obtained through wearable devices for screening, diagnostic or monitoring purposes. The document will also serve to help consumers, patients, industry and clinicians update their knowledge of available and upcoming wearable technologies and help decide which device best fits the patient’s needs (Figure 1).
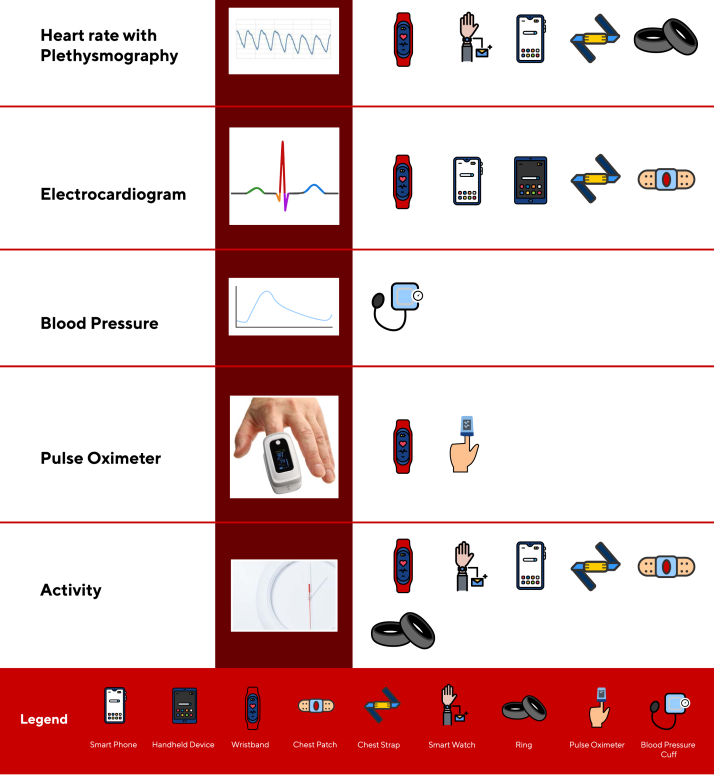
Figure 1.
Wearables such as smartwatches, wristbands, rings, handhelds, chest patches and chest straps may provide real time data such as heart rate using plethysmography, heart rhythm using electrocardiogram, blood pressure, pulse oximetry and activity/sleep.
This document should be used by providers as a guide to navigate this complex and rapidly evolving field. Due to a lack of large randomized controlled trials, we do not make any specific recommendations on the use of specific devices.
Clinical Scenario #1: A 76-year-old man with diabetes, hypertension and coronary artery disease but with no known atrial fibrillation (AF). He has not had palpitations, but he is worried about his risk of AF.
Many studies have shown that screening for AF in a population with high prevalence will lead to detection of a substantial number of patients with AF. In a Swedish systematic screening study, individuals aged 75-76 years had 3% new AF detected using 2 weeks of intermittent electrocardiography (ECG).4 In the mSToPS study, an ECG patch was used for up to 4 weeks in an elderly population (mean age 72.4) and 3.9 % new AF was detected.5 Implanted loop recorders (ILRs) with longer monitoring periods in an older high-risk population can detect AF at a rate of 34.4% per person-year (95% confidence interval [CI], 27.7–42.3).6 In contrast, detection of AF was low in studies of younger individuals, using either single time point ECG screening or prolonged screening using photoplethysmography (PPG) in owners of smartwatches.7 A meta-analysis of 10 studies found that smartphone camera applications to detect AF had reasonably high sensitivity (94.2%), specificity (95.8%), and negative predictive value (99.8%), but the positive predictive value was generally low and false-positive AF results exceeded true-positive results.8
Overall, AF detection through screening depends on the underlying prevalence in the population and the method and duration of detection. In countries with low health care consumption, AF is more likely to remain undiagnosed and AF screening efforts may lead to a higher number of diagnosed AF patients. Traditionally, the diagnosis of AF required a 12-lead ECG.9 More recent digital developments have allowed for easier access to portable ECGs through ambulatory equipment, watches with 1-lead ECGs or ECG patches. It remains difficult to monitor the heart rhythm using an ECG for prolonged periods of time without an invasive device. However, PPG-enabled devices can enable heart rhythm monitoring for longer periods of time and allow for real time ECG capture when prompted by the device or patient. The Apple Heart study enrolled 419,297 participants in the USA over 8 months to evaluate whether a PPG-enabled device could detect AF in individuals without a known history of the disease. Once an initial tachogram met irregularity criteria, the algorithm scanned for PPG irregularities during periods of minimal arm movement. If four subsequent irregular tachograms were confirmed, the participant was notified of an irregular pulse via a notification on the smartwatch and study app. The positive predictive value for AF detection was 84% and was 71% for the irregular notification algorithm and individual tachograms.10 Advanced machine learning techniques may improve AF detection more as deep neural networks have shown excellent performance against gold standard 12-lead ECG.11 Indeed, in a recent multi-center trial of 203 patients with history of cryptogenic stroke or transient ischemic attack, a 30-day smartphone ECG recording was superior for the detection of AF when compared with the standard repeat 24-h Holter monitoring.12
While wearables have potential to diagnose AF early and prevent AF progression and complications, many uncertainties remain, including what patient groups to target for screening and the need to prove that early detection of AF prevents adverse outcomes. The ongoing HEARTLINE trial is the first randomized trial to investigate whether detecting symptomatic and asymptomatic AF with the use of a smartwatch device (with combined PPG and ECG) would improve clinical AF diagnosis, reduce hard outcomes and increase compliance with anticoagulation therapy (NCT04276441 2020).
Future Directions
While screening for AF is gaining substantial and broad interest in the clinical community, numerous uncertainties remain. First, it is important to define the population that should be screened for AF. There is consensus for the need to screen patients with embolic stroke of undetermined source and those with symptoms that suggest AF.13 However, it is not clear who beyond these groups of patients should be screened for AF. Studies have also shown that the longer monitoring periods will lead to higher yield for AF screening.6 There is a need to define the ideal patient population and monitoring period to identify those who would benefit from screening for AF. Whether intervening by initiating anticoagulation would lead to better outcomes is yet to be determined.14 For screening to be beneficial and justified, evidence of improvement in patient care and outcomes as a result of earlier AF detection is needed.14 Future studies should focus on patient populations who may particularly benefit from screening (people >75 years and patients with risk factors for AF) and determine the ideal monitoring period for detection of undiagnosed AF. Second, the most accurate, user-friendly, and cost-effective modalities should be defined. Third, more prognostic information on subclinical AF is needed. It is not clear if this entity portends the same risk of stroke and heart failure as clinical AF. Finally, more data are needed on the outcomes of potential interventions for subclinical AF, including anticoagulation and rate and rhythm control strategies.
Incentive for Innovation
There are several incentives for innovation, including the significance and large magnitude of the problem.15 In one study, of the 5.3 million Americans with AF, 698,900 (13.1%) were found to have undiagnosed AF, and this is likely the tip of the iceberg.15 Another incentive for innovation is the potential of early detection of AF to result in improved attention to lifestyle modification and better outcomes, including reduced risk of stroke and heart failure and prevention of cardiac remodeling. The potential for cost savings is noteworthy, as with early detection and management of AF one may prevent adverse sequelae such as stroke and heart failure.
Clinical Scenario #2: A 40-year-old man with no past medical history presents to your clinic with palpitations.
Palpitations may be due to changes in emotional or psychological states, prescribed or illicit drugs, excessive alcohol use, smoking, strenuous exercise, or excessive consumption of caffeinated drinks. Palpitations may also be due to cardiac arrhythmias such as sinus tachycardia, premature atrial and ventricular ectopy, supraventricular tachycardia (SVT), ventricular tachycardia (VT), AF or atrial flutter.16
Wearable devices offer a unique opportunity to capture and diagnose such arrhythmias during infrequent episodes of palpations by using one or both types of sensors: the ECG, which is a recording of the heart electrical activity, and PPG, which uses light to detect changes of blood volume in the microvascular bed of tissue. As the PPG is not measuring the electrical signals and is a measurement of cardiac mechanical changes, it can only be used as a proxy for the actual rhythm. It may be used as a screening tool to identify patients at risk for having AF or SVT, but these patients would ultimately require an ECG for diagnosis.17, 18, 19 The frequency of the palpitations is important in determining the monitor needed for diagnosis. Rare or short-lasting episodes in which the patient would not have sufficient time to activate a wearable device would require a physician prescribed monitor.
By analyzing the continuous heart rate recorded using the PPG along with the data from an accelerometer, a wearable can detect the discrepancy between user activity and heart rate. If the heart rate changes significantly while the user is resting, it may prompt the user to record an ECG to determine if the change in heart rate is due to an arrhythmia (https://support.apple.com/en-us/HT208931).18,19 Smartwatches and consumer device grade handheld single lead ECGs have been validated for detection of AF versus sinus rhythm. However, they have been shown to have variable sensitivities ranging from 54.5% to 100%.20,21 Lowres et al22 reported 98.5% sensitivity and 91.4% specificity for AF detection, with a further study indicating sensitivity of 94.6% (95% CI, 85.1–98.9) and 92.9% specificity (95% CI, 92.0–93.8).
A randomized trial compared symptomatic rhythm detection rate of smartphone based handheld ECG devices alongside standard care versus standard care alone for 242 patients presenting to the emergency department with palpitations and pre-syncope with no obvious cause evident at initial consultation. A symptomatic rhythm was detected at 90 days in 69 participants (n = 124; 55.6%; 95% CI, 46.9–64.4%) in the intervention group versus 11 (n = 116; 9.5%; 95% CI, 4.2–14.8) in the control group (relative risk 5.9; 95% CI, 3.3–10.5; P <.0001). The most common symptomatic rhythms detected were sinus rhythm (in 53 participants; 66.3%), sinus tachycardia (in 19; 23.8%) and ectopic beats (in 13; 16.3%). Some participants had more than one symptomatic rhythm recorded. Eighty participants had a symptomatic rhythm detected, with 12 of these having a symptomatic cardiac arrhythmia (atrial fibrillation or flutter, SVT and sinus bradycardia) and 68 having sinus rhythm, sinus tachycardia or ectopic rhythm. Rhythm classifications were confirmed by clinicians.23
Recent advances in machine learning have enabled handheld ECG devices to automatically detect premature ventricular contractions and supraventricular ectopic beats in addition to AF that contribute to a significant number of events in patients with palpitations. Further research will improve detection of other rhythms such as premature atrial and ventricular beats using PPG. However, these algorithms need to be validated in large and diverse patients populations before clinical adaptation.24
Future Directions
Digital health technologies hold great promise for detection of arrhythmias that may cause palpitations. There is a need for large clinical studies that validate detection of a wide range of arrhythmias that may be responsible for palpitations. Although most consumer ECG devices today provide high quality signals and with the right algorithm may be able to detect a wide spectrum of arrhythmias, many of the devices have only been validated for AF detection. Further algorithm developments will increase their accuracy and reliability and improve the clinical use of wearable devices for investigating all arrhythmic causes of palpitations.
Incentive for Innovation
One of the incentives for innovation is to lower the false positive rate of detection of arrhythmias while improving specificity, especially during increased heart rate due to patient activity. This would reduce patient anxiety prior to physician verification, increase utilization of wearables for diagnosis of arrhythmias and reduce dependency on physician prescribed ECG patches, 24-hour Holter and ILRs for arrhythmia diagnosis.
Clinical Scenario #3: A 22-year-old woman with no past medical history has noticed she frequently has an elevated heart rate.
Elevated resting heart rate is a marker of increased autonomic state or decreased vagal tone in many diseases, including hyperthyroidism, dysautonomia, neoplastic disease, substance abuse, anorexia nervosa, or deconditioning.25,26 Heart rate variability may be a marker of cardiovascular fitness revealing a person’s flexibility between the sympathetic and parasympathetic states, and its temporal indices have been correlated with predictions of mortality27 and overall general health.26, 27, 28 Many wearables are able to provide long-term monitoring of heart rate and heart rate variability using PPG technology over an extended period of time.29
PPG-based technology has the advantage of providing continuous and long-term non-invasive monitoring of heart rate through wearable or smartphone devices.19 PPG-based monitoring can detect sporadic episodes of supraventricular tachyarrhythmias (SVT) that are particularly frequent in the young population (<50 years old), who also constitute the majority of consumers in the digital health market. It is critical for providers and consumers to become familiarized with the efficacy and reliability of different wearable devices for the assessment of heart rate to properly integrate the biometric data into clinical care and decision-making processes.
The reliability of PPG-based devices in assessing heart rate has been investigated in multiple studies, comparing it to either a 12-lead ECG, other forms of continuous ECG monitoring, or pulse oximeter measurements.19,24 There have been encouraging results regarding the accuracy of PPG-based wearable devices for the assessment of heart rate in both controlled30, 31, 32 and free-living conditions,33, 34, 35, 36, 37 although several challenges remain to achieve optimal accuracy.38 In most studies, the percentage of errors in heart rate measurements for wearable devices did not exceed 10% compared to standard reference tools. Most devices had a slight tendency to underestimate heart rate measurements, within a range of 5 beats per minute. These observations have also been confirmed in a meta-analysis of 29 studies34 assessing the accuracy of PPG-based heart rate measurements, suggesting careful interpretation of PPG-measured heart rate in medical settings where high reliability is required.31,39
On the other hand, testing the accuracy of PPG devices in different real-life settings has unveiled several sources of inaccuracy.38,40 Darker skin tones absorb more green light than lighter ones, interfering with PPG-based mechanisms and decreasing the accuracy of PPG-based devices in measuring heart rate.34,41,42 Nevertheless, prospective studies and meta-analysis have contradicted this observation, showing no significant change in accuracy of multiple consumer grade PPG devices across a wide range of skin tones.38 Additionally, significant discrepancies in accuracy and consistency of heart rate measurements exist between different wearable devices.34 Moreover, physical activity can generate significant motion artifacts, resulting in false or missing beats.43 Thus, the accuracy of real-time heart rate monitoring decreases as exercise intensity increases.29,30,38,44,45 In an observational study evaluating four devices in different activity settings, the accuracy decreased by 30% during physical activity and all devices tended to overestimate heart rate measurements during exercise.38 Cardiovascular conditions associated with low blood pressure or vasoconstriction could decrease the accuracy of the PPG measurement. Other reported sources of inaccuracy include body mass index, contact pressure with the skin, larger wrists, and gender.40
Additionally, the assessment of heart rate during tachyarrhythmia episodes seems to be more challenging. Sequeira et al46 measured heart rate during paroxysmal SVT episodes using 4 different devices (Apple Watch, Polar A360 , Garmin, Fitbit). During short runs of SVT (<60 seconds), all devices demonstrated a high error rate in detecting the sudden elevation in heart rate. Only two devices, Apple Watch and Polar A360, showed an acceptable accuracy in detecting episodes of SVT that were longer than 60 seconds. The SAFETY study investigating the Polar H7, an electrode-based chest strap, found it to be reliable in detecting AF with >95% specificity and specificity.47 In another study, smartwatch and wristband wearables were tested on 102 hospitalized patients and demonstrated a strong accuracy in estimating heart rate during sinus rhythm and atrial flutter, but underestimated heart rate during AF episodes when compared to continuous ECG.48
Future Directions
The cost of heart rate sensors has markedly dropped in the past decade, with the raw component pricing of light emitting diodes and photodiodes in bulk allowing creation of near-disposable devices. As the cost of complete monitoring devices drops to allow more ubiquitous use, numerous creative screening and diagnostic applications are likely, and physicians should be prepared to evaluate previously asymptomatic individuals with abnormal readings. The detected elevated heart rate may be a “surrogate marker” for an underlying condition, and real time or early detection may enable prompt treatment of the root cause of the inappropriate tachycardia.
Incentive for Innovation
Notably, all previously mentioned data explored the accuracy of heart rate measurements in relatively healthy participants who were presumably in sinus rhythm. Data evaluating wearables usage for abnormalities in heart rate and heart rate variability with cardiovascular conditions are scarce.39 Moreover, there have been no large clinical trials evaluating the clinical implications of high heart rates detected on a wearable device in real-life settings. Thus, more research is needed to determine how to interpret the data and how these data can be utilized for early prevention or to improve cardiovascular health in patients with cardiovascular disease.
Clinical Scenario #4: A 65-year-old man with hypertension and now 3 months post–pulmonary vein isolation for paroxysmal AF. Patient wants to stop oral anticoagulant (OAC) after shared decision making if no prolonged AF episodes post-ablation.
While many patients may be eager to discontinue anticoagulation in the setting of an effective rhythm control strategy, to date there are no completed randomized trials assessing the risks and benefits of anticoagulation cessation following AF ablation. Upcoming clinical trials, such as Higher Risk Patients Post-Catheter Ablation for Atrial Fibrillation (OCEAN) trial (NCT02168829), will help us better our understanding of what to do with anticoagulation after AF ablation. The ideal option for monitoring using wearables post-AF ablation is dependent, in part, on the sensitivity of the monitoring technique for the minimum duration of AF that may be associated with stroke. Duration of AF in hours, not minutes, appears to be associated with stroke.49, 50, 51, 52, 53, 54 While ILRs would provide sensitivity for AF episodes as brief as 2 minutes in duration, the cost and invasive nature limit their routine use for this indication. Daily ECG checks with wearable technologies have an estimated sensitivity of only 50%55 and are likely to detect only very prolonged episodes of AF. A wearable device capable of passive AF surveillance with PPG and ECG confirmation of the suspected episodes would be a reasonable choice to provide ongoing surveillance for recurrence of AF. When compared with ILRs, sensitivity and specificity for AF detection from these wearables can exceed 95%.56 A previous study performed simultaneous comparison between ILR and a PPG smartwatch with ECG confirmation and demonstrated a sensitivity of 97.5% for AF episodes >1 hour.57 This suggests that wearables may be a viable alternative to ILRs or event monitors for screening of AF and may be utilized in monitoring for recurrence of AF after ablation.
Guidelines state that decisions regarding continuation of OAC more than 2 months post-ablation should be based on a patient’s stroke risk profile and not on the apparent success or failure of the ablation procedure.58 Shared decision making is required to discuss the benefits and risks of anticoagulation discontinuation in the post-ablation setting.59,60 The recommendation against anticoagulation discontinuation is based, in part, on the modest long-term success rate of ablation, the high burden of asymptomatic AF following intervention, and the uncertain role of atrial myopathy that may promote thromboembolic events in the absence of AF.61 However, given the high prevalence of asymptomatic AF following ablation, anticoagulation cessation based on symptom resolution alone fails to account for the high proportion of asymptomatic AF episodes and may expose the patient to a risk of cardioembolic events.62
Retrospective cohort studies of anticoagulation cessation post-ablation have found conflicting results. In a study of 6886 post-ablation patients from a US administrative claims database, only 31.3% of patients remained on OAC 12 months post-procedure. The risk of cardioembolism beyond 3 months was increased with OAC discontinuation among high-risk patients, those with a CHA2DS2VASc score of 2 or more (hazard ratio 2.48 [95% CI, 1.11–5.52]; P <.05), but not in low-risk patients, CHA2DS2VASc score 0–1.63 Similar results were seen in a Swedish registry of 1175 post-ablation patients followed for at least a year. Of these, 30.6% discontinued anticoagulation treatment during the first year. In patients with a CHA2DS2VASc score of 2 or more, those who discontinued anticoagulation treatment had a higher rate of ischemic stroke compared with those continuing anticoagulation [1.6% per year vs 0.3% per year] (P = .046). Patients with a CHA2DS2-VASc score of 2 or more or those who had previously experienced an ischemic stroke displayed a higher risk of stroke if anticoagulation treatment was discontinued (hazard ratio, 4.6; 95% CI, 1.2–17.2; P = .02; and hazard ratio, 13.7; 95% CI, 2.0–91.9; P = .007, respectively). In contrast, in a study of 3355 post-ablation patients, no difference in stroke rate was observed in the 2692 whose anticoagulation was discontinued, including the 40% with CHADS2 score >2.53 Given the high recurrence rate of AF post-ablation and the tendency for recurrences to be asymptomatic in nature, long-term monitoring would be appropriate if anticoagulation discontinuation were to be considered.
Future Directions
Current wearable devices provide information on the presence or absence of AF. In the future, wearable technologies that provide information on AF duration and burden could prove useful in assessing stroke risk and effectiveness of treatment measured by AF burden reduction. In addition, customizable software balancing sensitivity and specificity in a population with known AF will likely improve device accuracy. Prospective trials assessing the feasibility of targeted, time-delimited non-vitamin K antagonist oral anticoagulant using AF-sensing wearables could potentially limit OAC usage while still maintaining stroke prevention.
Incentive for Innovation
Discontinuation of OAC after AF ablation happens frequently in clinical practice and is often driven by patient demands despite a lack of consistent data supporting its safety. Conversely, chronic anticoagulation for patients with infrequent episodes of AF either spontaneously or as the result of an effective rhythm control strategy including antiarrhythmic drugs or ablation exposes the patient to the untoward effects of the drugs during prolonged periods of sinus rhythm when stroke risk appears to be low. Wearable devices today are most often used for AF screening. Improvement in device capabilities and rigorous clinical trial data establishing the utility of these devices in a population with known AF would expand their use and potentially improve patient outcomes. This strategy would reduce health care costs given the economic burden of OAC and associated bleeds, thus making payment for wearable devices of interest to payors and patients. The utilization of wearable technologies to assess the presence and treatment impact on AF-related comorbidities (e.g., hypertension, obstructive sleep apnea [OSA], poor sleep, and inactivity) may also prove useful in both primary and secondary AF prevention.
Clinical Scenarios #5A and 5B: A 64-year-old man with symptomatic paroxysmal AF, creatinine clearance of 50 milliliters/minute, prior coronary stenting who has been satisfactorily treated with dofetilide 250 micrograms every 12 hours for the past 3 months. He is not interested in catheter ablation. Pre-treatment QTc was 410 ms; 12 lead ECG last week showed a QTc of 480 ms. Open-ended QT monitoring was prescribed using “wearable” technology with a plan for weekly transmission of a resting single-lead rhythm strip via electronic medical record. A 25-year-old woman with genotype positive/phenotype negative long QT syndrome (LQTS) (KCNH2; has a sister with clinical LQTS) suffers from schizophrenia, for which risperidone has been the only effective and tolerated drug. Open-ended QT monitoring was prescribed using “wearable” technology with a plan for weekly transmission of resting single lead rhythm strip by patient via electronic medical record.
Currently, the BioTel mobile cardiac outpatient telemetry (MCOT) device has been Food and Drug Administration (FDA) cleared for QTc monitoring (https://www.accessdata.fda.gov/cdrh_docs/pdf15/K153473.pdf), and Kardia has been approved for QTc monitoring in COVID-19 patients. The ECGs generated by “wearable” devices that generate one or more limb lead ECG recordings might permit assay of the static QT interval with reasonable accuracy.64 In a small group of patients with persistent AF treated with dofetilide, there were no significant differences between ECG obtained through handheld ECG devices and QTc obtained from a 12 lead ECG.65 Advanced machine learning techniques such as deep learning can significantly improve the performance of QTc measurement in handheld ECG recorders and help their wide adoption for measurement of QTc interval. Deep learning enabled QTc interval measurements derived from handheld mobile ECG recorders have been shown to yield similar results to QTc measurements using 12 lead ECGs annotated by human experts (−0.45 ± 24.73 ms vs +10.52 ± 25.64 ms).64
The performance of smartwatch ECG for measurement of QT depends on several factors, including ECG tracing quality, T-wave amplitude and recording lead. There are several strategies that have been suggested to improve the accuracy of QT measurement using smartwatch ECGs. Identifying the best smartwatch position using T-wave mapping at baseline can improve accuracy. Further, the lead recorded by smartwatches (lead I) may be suboptimal for measuring the QT interval, and other leads can be reproduced by placing the smartwatch on the left ankle or chest.66 QT interval measurement from smartwatch equivalents of lead I with the watch on the left wrist, lead II with the watch on the left ankle, and a simulated lead V6 with the watch on the left lateral chest showed a median absolute error in QT of 18, 20 and 16 ms, respectively, compared to QT measurements from a 12 lead ECG.67 Although there has been initial study on use of smartwatches for QT measurement,68 there is a need for larger studies to validate the findings in diverse patient cohorts with different clinical indications for QT monitoring.
Future Directions
It is reasonable to anticipate greater accuracy in QT interval measurement using devices that incorporate simultaneous multi-lead vector acquisition. It will be important to demonstrate accuracy of QT analysis using serial measurements of the QT interval in individuals and among different populations and clinical indications. The ability to perform serial recordings may permit dynamic QT assessment and assess QT “trajectory,” which may improve safety. There is also a need for clinical trials to establish the safety of these devices for monitoring QT intervals in clinical scenarios where close monitoring of QT interval is paramount, for instance, during drug initiation or loading. Termination or reduction of the dose of the drug based on the QT interval is achieved by an active intervention such as reduction of dosage or cessation of a drug or temporary pacing. It is therefore reasonable that, at least in “high risk” scenarios, an ambulatory QT monitoring strategy without defibrillation backup would not be utilized for initial administration of the drug. It remains to be demonstrated whether and how the use of a wearable ambulatory QT monitoring strategy for previously loaded drugs fares against current care paradigms. Wearables can provide real time QT monitoring that potentially allows for continuation of drugs in the setting of metabolic decline (e.g., glomerular filtrate rate) beyond the time that they are discontinued in current practice, which may otherwise have adverse clinical repercussions.
Incentive for Innovation
Clinical safety and efficacy of wearable QT monitoring strategies need to be established through rigorous clinical trials in diverse populations with different clinical indications. Other considerations that may stymie the development of wearable QT monitoring strategies may also include medicolegal risk and lack of financial models that incentivize the clinicians and patients to adopt these technologies.
Clinical Scenarios #6A and 6B: A 64-year-old man who is a marathoner training for a race develops intermittent, sudden palpitations associated with shortness of breath. A 25-year-old woman who is a competitive track and field athlete wants to optimize her cardiac performance during training.
For the competitive athlete, digital health has the potential to impact training and performance, preparticipation evaluation, and assessment of symptoms potentially associated with cardiovascular disease. Recent advances in wearables allow athletes and their sports medicine trainers and clinicians to monitor movement, workload, performance, and endurance through specific biometrics such as heart rate, heart rate variability, activity levels, oxygen saturation, and sleep.69, 70, 71 Digital health technology permits personalized data collection via wearable sensors, wristbands, or chest patches and can provide real time physiological and action monitoring with position specific patterns in movement, performance optimization, caloric expenditure, altitude, mileage, steps, pace and screening for potential injury. Some commercially available global position systems can even monitor a full team. Unfortunately, evidence for their utilization is still limited.72,73
Arrhythmias that may be detected during exercise may include AF, VT, SVT, premature atrial or ventricular beats, and change in QT interval with exercise. Capture of these arrhythmias may be helpful in management of patients with cardiac disease such as hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy or LQTS.74
Global positioning system technologies in wearables can track external workload metrics such as resistance, duration, and speed. While measuring training volume and performance can guide training, the same measurements can also guide pre-competition tapering of training. Furthermore, measuring cadence, stride length, and contact time with surfaces provides biomechanical load data that can be used to prevent injuries. Accelerometers, inertia sensors, and insole pressure measurement systems imbedded in wearables can provide biomechanical data. Average, heart rate variability, activity levels, oxygen saturation, and sleep assessments can be combined with the above performance metrics to optimize running performance.69,73
Conventional options to capture arrhythmias that are common include a patch based ECG monitor; rarely is ILR used.72 Wearables offer form factors that may be more conducive to capturing arrhythmia given the practicalities around training. Heart rate trends recorded from a watch and tabulated on an app may identify higher ranges higher than normal and, if correlating with symptoms, may be suggestive of an arrhythmia.75 Graphical representation on smartphone apps may be akin to heart rate trends seen on telemetry units in the hospital. For those with clear symptoms in the absence of syncope or significant lightheadedness/dizziness, ECG capable wearables provide important adjunctive rhythm information.
Future Directions
More evidence and standardization of data are needed for guidance of how sensors and monitors can be used for risk optimization of training and performance while minimizing risk of injury. Limited evidence is available on how heart rate and heart rate variability can be clinically used for various sports having different cardiopulmonary demands and differences that may be seen in athletes of varied ages, gender and race who may have underlying cardiovascular conditions.
Incentive for Innovation
More research is necessary to personalize heart rate expectations and recommendations and heart rate variability in various sports and at certain levels of activity based on age, gender, race, cardiovascular fitness and exercise capacity. Form factors need to be compatible with sport and take into consideration athlete comfort and stability and not impose risk for injury to the wearer and others on the court or field.74 For example, for contact sports, arm bands and vests with pouch form factors would be less likely to risk injury and damage than rings and watches or wristbands. Furthermore, more information is needed for clinicians to understand, analyze and determine how to utilize these data for risk stratification of arrhythmias such as sudden cardiac death.
Clinical Scenario #7: A patient with OSA, a known risk factor for AF, is counseled about risk reduction and is actively working on weight loss and continuous positive airway pressure (CPAP) therapy. Various options for screening for and diagnosis of OSA, as well as monitoring response to therapy in this setting, are summarized.
OSA is associated with an increased risk of pulmonary and systemic hypertension, heart failure, stroke, bradycardia and AF.76 OSA is suspected when patients report tiredness, daytime sleepiness, and unrestful sleep and when they are told they snore or stop breathing while asleep. Polysomnography or sleep study is the gold standard diagnostic test and includes recording of brain waves with electro-encephalograms, oxygen saturation and breathing, leg movement and ECG. Sleep studies are typically performed at dedicated sleep centers but can also be performed at home. CPAP is the usual therapy of choice to reduce hypoxia and alleviate symptoms. The severity of OSA can vary within the individual patient from one sleep period to another, which is a limitation of overnight sleep studies. Studies from patients with pacemakers show a wide range of variability in abnormal sleep indices, with a clear association between the severity of OSA and the burden of AF.77
Instead of undergoing a formal sleep study, apps and wearables now offer feedback on sleep and oxygenation to patients from their phone, ring, wristband or watch. Some smartwatches such as the Apple Watch, Fitbit Sense, Samsung Galaxy Watch 3 and Withings Scanwatch offer a blood oxygen app that uses the photodiodes on the back of the device to measure oxygen levels. There are several available apps for smartphone and wearable devices that guide sleep hygiene, such as when one would like to sleep and wake up, and also apps that leave the phone’s microphone on while one sleeps to notate when one may be having an apneic event and gasping for air, with a sensitivity of 88.3% and specificity of 80.0%.78 Past studies have examined the relationship of bedtime regularity and resting heart rate monitoring by digital wristband and showed that going to bed 30 minutes later than one’s normal bedtime was associated with a significantly higher resting heart rate throughout sleep that persisted into the following day, demonstrating that proper sleep habits may affect cardiovascular health.79,80 Wearables can measure how much time you spend in various sleep phases and even give sleep quality scores based on duration of sleep, movement disturbances and heart rate.81 In a recent study of patients with OSA, a smartwatch provided acceptable heart rate measurement on telemetry.82 More definitively, in a study evaluating the incidence of AF in patients with severe OSA, implantable loop monitors diagnosed AF in 20% of study participants,83 after an average monitoring period of 11 months.
Future Directions
Wearable technologies, using sensors on the wrist, chest straps, rings, and smartphones, have been used to track rest and sleep as part of a package to monitor activity and fitness, and have an important role to play not only in diagnosing OSA and tracking sleep patterns but also in diagnosing AF and other arrhythmias that are prevalent in this population. These technologies can also be used in surveillance and evaluation of response to therapy, such as CPAP, in these patients. It is unclear if other recorded bio-signals such as skin temperature and skin conductance may further advance the staging of sleep.84 However, recent evaluations of these sleep technologies suggest there is significant room for improvement because of the high degree of variability in the accuracy of these technologies, as they displayed lower error and bias values when quantifying sleep/wake states compared to sleep staging duration, which seems to be lacking in accuracy.84,85 Collaboration with and inclusion of recommendations from sleep experts may be helpful in developing further applications and understanding how to analyze data recorded.
Incentive for Innovation
There is a wide range of variability in reported sensitivity and specificity in OSA diagnosis using currently available technology compared to standard polysomnography.86 This provides a continuous incentive for improvement of the diagnostic accuracy of existing or development of alternative approaches in wearable tools. In addition, with higher AF risk in the OSA population, adjunctive or concomitant arrhythmia monitoring in a longitudinal fashion, extended over a longer duration, is key in diagnosing and identifying parametric profiles that characterize patients at risk for this arrhythmia.87
Concluding Remarks
Wearables are now available to consumers in many forms, such as watches, wristbands, rings, chest straps, and patches, and are able to provide the wearer with vital health information in real time and, at times, a cursory diagnosis. This document may serve as a guide for clinicians to traverse the growing and upcoming digital technologies that are available to patients for procurement. More research is needed to determine how these devices can be used in adults and perhaps even expanded to adolescents and children. Naturally, as more patients adopt the usage of these technologies into their lives for fitness and health monitoring of their heart rate, heart rhythm, blood pressure, oxygenation, activity, and sleep, it is critical for us as clinicians to understand how data from wearables can be incorporated into a patient’s electronic medical record, reduce hospitalization, or improve preventative care.
Appendix A.
Author’s Disclosure Table
| Writing Group Member | Employment | Honoraria/Speaking/Consulting | Speakers’ Bureau | Research∗ | Fellowship Support∗ | Ownership/Partnership/Principal/Majority Stockholder | Stock or Stock Options | Intellectual Property/Royalties | Other |
|---|---|---|---|---|---|---|---|---|---|
| Elaine Y. Wan, MD | Vagelos College of Physicians and Surgeons, New York-Presbyterian/Columbia University Irving Medical Center, New York, NY, USA | 1 Boston Scientific; Medtronic; Abbott | None | 5 National Institutes of Health | None | None | None | None | None |
| Hamid Ghanbari, MD | University of Michigan, Ann Arbor, MI, USA | Preventice | None | 0 Medtronic; Boston Scientific; Biotronik; Toyota | None | None | None | None | 3 Verily |
| Nazem Akoum, MD, MS | University of Washington, Seattle, WA, USA | None | None | None | None | None | None | None | None |
| Zachi Itzhak Attia, MSEE, PhD | Mayo Clinic, Rochester, MN, USA | None | None | None | None | None | 0 Eko Devices; AliveCor; Myant Canada; TripleBlind | None | None |
| Samuel J. Asirvatham, MD | Mayo Clinic, Rochester, MN, USA | 1 St. Jude Medical; Medtronic; Biotronik; Boston Scientific; Biosig Technologies; MediLynx | None | None | None | None | None | 1 AliveCor | None |
| Eugene H. Chung, MD | University of Michigan, Ann Arbor, MI, USA | None | None | None | None | None | None | None | None |
| Lilas Dagher, MD | Tulane Research Innovation for Arrhythmia Discoveries (TRIAD), Heart and Vascular Institute, Tulane University School of Medicine, New Orleans, LA, USA | None | None | None | None | None | None | None | Non |
| Sana M. Al-Khatib, MD, MHS | Duke Clinical Research Institute, Durham, NC, USA | 1 Milestone Pharmaceuticals; Medtronic | None | Medtronic; Abbott; Boston Scientific | None | None | None | 0 Grektek, LLC | 2 American Heart Association |
| G. Stuart Mendenhall, MD | Scripps Memorial Hospital-La Jolla, La Jolla, CA, USA | 1 Boston Scientific; Medtronic | None | None | None | None | None | None | None |
| David D. McManus, MD, MSCi | University of Massachusetts Medical School, Worchester, MA, USA | 1 Fitbit | None | 5 Boehringer Ingelheim; Bristol-Myers Squibb; Philips; Samsung; Apple Inc.; Biotronik; Boehringer Ingelheim; Fitbit; Pfizer, Inc.; Otsuka Pharmaceuticals; Sanofi; Care Evolution; Flexcon | None | None | None | 3 Heart Rhythm Society | |
| Rajeev K. Pathak, MBBS, PhD | Cardiac Electrophysiology Unit, Department of Cardiology, Canberra Hospital and Health Services, Australian National University, Canberra, Australia | None | None | None | None | None | None | None | None |
| Rod S. Passman, MD | Northwestern University Feinberg School of Medicine, Chicago, IL, USA | 1 Janssen Pharmaceuticals; Medtronic | 5 AHA Foundation Award | None | None | None | 2 Up to Date | None | |
| Nicolas S. Peters, MD | Imperial College London, and NHS Trust, London, United Kingdom | 1 Cardialen, Inc. 4 Verily/Google |
None | None | None | None | None | None | 1 Boston Scientific; St. Jude Medical |
| David S. Schwartzman, MD | Butler Health System, Cardiac Electrophysiology, Pittsburgh, PA, USA | None | None | None | None | None | None | None | None |
| Emma Svennberg, MD | Karolinska Institutet, Department of Medicine Huddinge, Karolinska University Hospital, Stockholm, Sweden | 1 Bayer Healthcare Pharmaceuticals; Bristol-Myers Squibb; Pfizer, Inc.; Boehringer Ingelheim; Sanofi; Merck | None | 5 Roche Diagnostics | None | None | None | None | None |
| Khaldoun G. Tarakji, MD | Department of Cardiovascular Medicine, Cleveland Clinic Foundation, Cleveland, OH, USA | 1 Medtronic; Janssen Pharmaceuticals 2 AliveCor |
None | None | None | None | None | None | None |
| Mintu P. Turakhia, MD, MS | Department of Medicine, Stanford University, Stanford, CA, USA; Veterans Affairs Palo Alto Health Care System, Palo Alto, CA, USA; and Center for Digital Health, Stanford, CA, USA | 1 Biotronik; Medtronic; Abbott; Myokardia; Milestone Pharmaceuticals; Pfizer, Inc.; Janssen Pharmaceuticals | None | 5 Apple Inc.; Bristol-Myers Squibb; American Heart Association; Bayer Healthcare Pharmaceuticals | None | None | None | None | None |
| Anthony Trela, NP, RN | Lucile Packard Children's Hospital, Pediatric Cardiology, Palo Alto, CA, USA | None | None | None | None | None | None | None | None |
| Hirad Yarmohammadi, MD | Vagelos College of Physicians and Surgeons, New York-Presbyterian/Columbia University Irving Medical Center, New York, NY, USA | None | None | None | None | None | None | None | None |
| Nassir F. Marrouche, MD | Tulane Research Innovation for Arrhythmia Discoveries (TRIAD), Heart and Vascular Institute, Tulane University School of Medicine, New Orleans, LA, USA | 0 Medtronic; Biotronik; Biosense Webster, Inc.; Cardiac Design 1 Preventice |
None | 0 Abbott; Boston Scientific; GE Healthcare; Janssen Pharmaceuticals; Siemens Healthcare 3 Biosense Webster, Inc. |
None | None | None | None |
Number value: 0 = $0; 1 = ≤$10,000; 2 = >$10,000 to ≤$25,000; 3 = >$25,000 to ≤$50,000; 4 = >$50,000 to ≤$100,000; 5 = >$100,000.
Research and fellowship support are classed as programmatic support. Sources of programmatic support are disclosed but are not regarded as a relevant relationship with industry for writing group members or reviewers.
Disclaimer
The development and editorial review was conducted by the Heart Rhythm Society, and included a peer-review phase and a public comment period. Drs McManus, Marrouche, and Ghanbari had no involvement in peer review for acceptance to this journal.
Ethics Statement
Not applicable.
Conflict of Interest
Please see Appendix A.
Authorship
All authors attest they meet the current ICMJE criteria for authorship.
Appendix
Table 1.
Available wearable technology
| Device | Measurements (HR, ECG, Activity Hours, Temperature, Pulse Oximetry) | ECG Recording Duration | Regulatory Decisions/FDA Approval | Battery Life | Autodetect or Patient Triggered | Wear Location | Connectivity (Bluetooth, WiFi, Cellular) | Compatible OS |
|---|---|---|---|---|---|---|---|---|
| AliveCor Kardia mobile | ECG | 30 seconds | FDA cleared | Connected to smartphone | Patient triggered | Handheld | Bluetooth | iOS, Android |
| Apple watch (Series 6) | HR ECG Activity Temperature Pulse oximetry |
30 seconds | Heart-tracking features are cleared by the FDA but the oxygen monitor is not | Charging | Patient triggered | Wrist | Wi-Fi, Bluetooth | iOS |
| Beurer ME 90 | ECG | 30 seconds | FDA cleared | Battery | Patient triggered | Handheld | Bluetooth | N/A |
| Bittium Faros | ECG HRV |
180 days | FDA cleared and CE marked | Rechargeable battery | N/A | Patch to the anterior chest or electrode | USB download | N/A |
| Cardiac Designs ECG Check | ECG | 30 seconds | FDA cleared and CE marked | Rechargeable battery | Patient triggered | Handheld | Cloud server or email | N/A |
| CardiBeat and HeartCheck ECG Pen | ECG | 30 seconds | FDA cleared and CE marked | AA battery | Patient triggered | Handheld | Information unavailable | |
| CardioComm Solutions HeartCheck | ECG | 30 seconds | FDA cleared | AA battery | Patient triggered | Handheld | ||
| COALA | ECG | Yes, 2 leads | FDA cleared | Rechargeable via charging station using wall adapter or USB | Patient triggered | Handheld | Wi-Fi, Bluetooth | iOS |
| Eko DUO | ECG | Yes, single lead, 15, 30. 60, 120 seconds | FDA cleared | Charging | Patient triggered | Handheld | Wi-Fi, Bluetooth | iOS, Android |
| Fitbit (Sense) | HR ECG Activity Pulse oximetry Temperature |
30 seconds | FDA cleared | Charging | Patient triggered | Wrist | Wi-Fi, Bluetooth | iOS, Android |
| Garmin | Pulse oximetry Hydration HR |
No | N/A | N/A | N/A | Wrist | Wi-Fi, Bluetooth | iOS, Android |
| Huawei (GT2 Pro) | HR ECG Activity Pulse oximetry Temperature |
Information unavailable | National Medical Products Administration’s Class II medical device registration certificate (Chinese) | Charging | Unavailable | Wrist | Bluetooth | Android, ECG function is not compatible with iOS, Windows |
| MyDiagnostick | ECG | 60 seconds | Not cleared | Charged by USB | Patient triggered | Handheld | USB connection by the physician | N/A |
| Omron HCG-801 | ECG | 30 seconds | FDA cleared | Battery | Patient triggered | Handheld | PC download | N/A |
| Oura ring | HR ECG HRV Skin temperature Activity Respiratory rate |
Continuous | FDA cleared and CE marked | Battery | N/A | Chest | Bluetooth | iOS |
| Qardiocore | Activity HR HRV Temperature |
No | Not cleared | Charging | Autodetect | Finger | Bluetooth | iOS, Android |
| Samsung (Galaxy 3) | HR Pulse oximetry Activity ECG |
30 seconds | Cleared | Charging | Patient triggered | Wrist | Wi-Fi, Bluetooth | iOS, Android |
| Smartphone ECG Devices | ||||||||
| VitalPatch 7-day patch | Body temperature ECG HR HRV Accelerometer Body temperature |
|||||||
| Vivalink 96-hour ECG patch | ECG HR RR Accelerometer |
96 hours to 7 days | FDA cleared | Battery | Unavailable | Patch to the anterior chest | N/A | N/A |
| Whoop | HR Respiratory rate |
Information unavailable | FDA cleared | Charging | Autodetect | Wrist | Bluetooth | iOS, Android |
| Withings Move ECG https://www.withings.com/move-ecg | ECG Activity |
30 seconds | ECG monitor of Move ECG has received a CE marking, following the medical device directive. Withings is working with the FDA to receive medical clearance. | Battery | Patient triggered | Wrist | Bluetooth | iOS, Android |
| Withings ScanWatch https://www.withings.com/scanwatch | HR ECG Activity Pulse oximetry |
30 seconds | The Scan Monitor of the ScanWatch has received a CE marking for HR, ECG and SpO2 features following the medical device directive. Withings is working with the FDA to receive medical clearance. | Charging | Autodetect, patient-triggered | Wrist | Bluetooth | iOS, Android |
| Xiaomi (Amazfit Smart Watch 2) | HR ECG Activity |
60 seconds | Not cleared | Charging | Patient triggered | Wrist | Wi-Fi, Bluetooth | iOS, Android |
| Zenicor | ECG | 30 seconds | Zenicor’s system solution is CE marked Class IIa, and Zenicor Medical Systems AB is certified according to ISO13485. | Battery | Patient triggered | Handheld | Web-based service, Zenicor-ECG Doctor System | N/A |
| Physician Prescribed Devices | ||||||||
| BardyDx CAM Patch | ECG | Up to 14 days of extended Holter monitoring | FDA cleared and CE marked | 14 days | Autodetect, patient triggered | Patch to the anterior chest | Sent to physician | N/A |
| BioTel Heart ePatch | ECG | ePatch 1-channel 14 days ePatch 3-channel 5 days |
FDA cleared and CE marked | 14 days | Autodetect, patient triggered | Patch to the anterior chest or electrode | Sent to physician | N/A |
| BioTel Heart MCOT | ECG | Up to 30 days of near real-time continuous monitoring | FDA cleared | Rechargeable sensor and gateway | Autodetect, patient triggered | Patch to the anterior chest or electrodes or electrode | 4G data networking Sent to physician |
N/A |
| Medilynx | ECG | Yes, 3 leads up to 30 days | FDA cleared | Self-applied | Autodetect | Attach the electrode to the anterior chest and put the device in the pocket | Wirelessly transmitted via nationwide carrier networks | N/A |
| Boston Scientific Preventice Solutions |
ECG | Yes, may be up to 30 days | FDA cleared | Will be applied by physician or self-applied | Autodetect | Patch to the anterior chest | Sent to physician | N/A |
| iRhythm Ziopatch/Zio XT/AT | ECG | Yes, up to 14 days | FDA cleared | Pre-charged in the mail and will be sent back by the patient | Autodetect but will be self-applied by the patient | Patch to the anterior chest | Sent to physician | N/A |
CE = Conformitè Europëenne; ECG = electrocardiogram; FDA = Food and Drug Administration; HR = heart rate; HRV = heart rate variability; N/A = not applicable.
References
- 1.Coravos A., et al. Modernizing and designing evaluation frameworks for connected sensor technologies in medicine. NPJ Digit Med. 2020;3:37. doi: 10.1038/s41746-020-0237-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tarakji K.G., et al. Digital health and the care of the patient with arrhythmia: what every electrophysiologist needs to know. Circ Arrhythm Electrophysiol. 2020;13 doi: 10.1161/CIRCEP.120.007953. [DOI] [PubMed] [Google Scholar]
- 3.Ding E.Y., et al. Survey of current perspectives on consumer-available digital health devices for detecting atrial fibrillation. Cardiovasc Digit Health J. 2020;1:21–29. doi: 10.1016/j.cvdhj.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Svennberg E., et al. Mass screening for untreated atrial fibrillation: the STROKESTOP study. Circulation. 2015;131:2176–2184. doi: 10.1161/CIRCULATIONAHA.114.014343. [DOI] [PubMed] [Google Scholar]
- 5.Steinhubl S.R., et al. Effect of a home-based wearable continuous ECG monitoring patch on detection of undiagnosed atrial fibrillation: the mSToPS randomized clinical trial. JAMA. 2018;320:146–155. doi: 10.1001/jama.2018.8102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Healey J.S., et al. Subclinical atrial fibrillation in older patients. Circulation. 2017;136:1276–1283. doi: 10.1161/CIRCULATIONAHA.117.028845. [DOI] [PubMed] [Google Scholar]
- 7.Chan P.H., et al. Diagnostic performance of an automatic blood pressure measurement device, Microlife WatchBP Home A, for atrial fibrillation screening in a real-world primary care setting. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-013685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O'Sullivan J.W., et al. Accuracy of smartphone camera applications for detecting atrial fibrillation: a systematic review and meta-analysis. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hindricks G., et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS) Eur Heart J. 2021;42:373–498. doi: 10.1093/eurheartj/ehaa612. [DOI] [PubMed] [Google Scholar]
- 10.Perez M.V., et al. Large-scale assessment of a smartwatch to identify atrial fibrillation. N Engl J Med. 2019;381:1909–1917. doi: 10.1056/NEJMoa1901183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tison G.H., et al. Passive detection of atrial fibrillation using a commercially available smartwatch. JAMA Cardiol. 2018;3:409–416. doi: 10.1001/jamacardio.2018.0136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koh K.T., et al. Smartphone electrocardiogram for detecting atrial fibrillation after a cerebral ischaemic event: a multicentre randomized controlled trial. Europace. 2021 doi: 10.1093/europace/euab036. [DOI] [PubMed] [Google Scholar]
- 13.Nouh A., Hussain M., Mehta T., Yaghi S. Embolic strokes of unknown source and cryptogenic stroke: implications in clinical practice. Front Neurol. 2016;7:37. doi: 10.3389/fneur.2016.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benjamin E.J., et al. Research priorities in atrial fibrillation screening: a report from a National Heart, Lung, and Blood Institute Virtual Workshop. Circulation. 2021;143:372–388. doi: 10.1161/CIRCULATIONAHA.120.047633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turakhia M.P., et al. Estimated prevalence of undiagnosed atrial fibrillation in the United States. PLoS One. 2018;13 doi: 10.1371/journal.pone.0195088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wexler R.K., Pleister A., Raman S.V. Palpitations: evaluation in the primary care setting. Am Fam Physician. 2017;96:784–789. [PubMed] [Google Scholar]
- 17.Benedetto S., et al. Assessment of the Fitbit Charge 2 for monitoring heart rate. PLoS One. 2018;13 doi: 10.1371/journal.pone.0192691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheung C.C., Krahn A.D., Andrade J.G. The emerging role of wearable technologies in detection of arrhythmia. Can J Cardiol. 2018;34:1083–1087. doi: 10.1016/j.cjca.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Pereira T., et al. Photoplethysmography based atrial fibrillation detection: a review. NPJ Digit Med. 2020;3:3. doi: 10.1038/s41746-019-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Desteghe L., et al. Performance of handheld electrocardiogram devices to detect atrial fibrillation in a cardiology and geriatric ward setting. Europace. 2017;19:29–39. doi: 10.1093/europace/euw025. [DOI] [PubMed] [Google Scholar]
- 21.Tarakji K.G., et al. Using a novel wireless system for monitoring patients after the atrial fibrillation ablation procedure: the iTransmit study. Heart Rhythm. 2015;12:554–559. doi: 10.1016/j.hrthm.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 22.Lowres N., et al. Feasibility and cost-effectiveness of stroke prevention through community screening for atrial fibrillation using iPhone ECG in pharmacies. The SEARCH-AF study. Thromb Haemost. 2014;111:1167–1176. doi: 10.1160/TH14-03-0231. [DOI] [PubMed] [Google Scholar]
- 23.Reed M.J., et al. Multi-centre randomised controlled trial of a smart phone-based event recorder alongside standard care versus standard care for patients presenting to the Emergency Department with palpitations and pre-syncope—the IPED (Investigation of Palpitations in the ED) study: study protocol for a randomised controlled trial. Trials. 2018;19:711. doi: 10.1186/s13063-018-3098-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Han D., et al. Smartwatch PPG peak detection method for sinus rhythm and cardiac arrhythmia. Annu Int Conf IEEE Eng Med Biol Soc. 2019;2019:4310–4313. doi: 10.1109/EMBC.2019.8857325. [DOI] [PubMed] [Google Scholar]
- 25.Krahn A.D., Yee R., Klein G.J., Morillo C. Inappropriate sinus tachycardia: evaluation and therapy. J Cardiovasc Electrophysiol. 1995;6:1124–1128. doi: 10.1111/j.1540-8167.1995.tb00391.x. [DOI] [PubMed] [Google Scholar]
- 26.Kemp A.H., Quintana D.S. The relationship between mental and physical health: insights from the study of heart rate variability. Int J Psychophysiol. 2013;89:288–296. doi: 10.1016/j.ijpsycho.2013.06.018. [DOI] [PubMed] [Google Scholar]
- 27.Seccareccia F., et al. Heart rate as a predictor of mortality: the MATISS project. Am J Public Health. 2001;91:1258–1263. doi: 10.2105/ajph.91.8.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Acharya U.R., Kannathal N., Krishnan S.M. Comprehensive analysis of cardiac health using heart rate signals. Physiol Meas. 2004;25:1139–1151. doi: 10.1088/0967-3334/25/5/005. [DOI] [PubMed] [Google Scholar]
- 29.Thomson E.A., et al. Heart rate measures from the Apple Watch, Fitbit Charge HR 2, and electrocardiogram across different exercise intensities. J Sports Sci. 2019;37:1411–1419. doi: 10.1080/02640414.2018.1560644. [DOI] [PubMed] [Google Scholar]
- 30.Baek S., Ha Y., Park H.W. Accuracy of wearable devices for measuring heart rate during conventional and Nordic walking. PM R. 2021;13:379–386. doi: 10.1002/pmrj.12424. [DOI] [PubMed] [Google Scholar]
- 31.Nelson B.W., et al. Guidelines for wrist-worn consumer wearable assessment of heart rate in biobehavioral research. NPJ Digit Med. 2020;3:90. doi: 10.1038/s41746-020-0297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shcherbina A., et al. Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. J Pers Med. 2017;7:3. doi: 10.3390/jpm7020003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dur O., et al. Design rationale and performance evaluation of the wavelet health wristband: benchtop validation of a wrist-worn physiological signal recorder. JMIR Mhealth Uhealth. 2018;6 doi: 10.2196/11040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fuller D., et al. Reliability and validity of commercially available wearable devices for measuring steps, energy expenditure, and heart rate: systematic review. JMIR Mhealth Uhealth. 2020;8 doi: 10.2196/18694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hahnen C., et al. Accuracy of vital signs measurements by a smartwatch and a portable health device: validation study. JMIR Mhealth Uhealth. 2020;8 doi: 10.2196/16811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sartor F., et al. Wrist-worn optical and chest strap heart rate comparison in a heterogeneous sample of healthy individuals and in coronary artery disease patients. BMC Sports Sci Med Rehabil. 2018;10:10. doi: 10.1186/s13102-018-0098-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wallen M.P., Gomersall S.R., Keating S.E., Wisloff U., Coombes J.S. Accuracy of heart rate watches: implications for weight management. PLoS One. 2016;11 doi: 10.1371/journal.pone.0154420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bent B., Goldstein B.A., Kibbe W.A., Dunn J.P. Investigating sources of inaccuracy in wearable optical heart rate sensors. NPJ Digit Med. 2020;3:18. doi: 10.1038/s41746-020-0226-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Etiwy M., et al. Accuracy of wearable heart rate monitors in cardiac rehabilitation. Cardiovasc Diagn Ther. 2019;9:262–271. doi: 10.21037/cdt.2019.04.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Muhlen J.M., et al. Recommendations for determining the validity of consumer wearable heart rate devices: expert statement and checklist of the INTERLIVE Network. Br J Sports Med. 2021 doi: 10.1136/bjsports-2020-103148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dooley E.E., Golaszewski N.M., Bartholomew Z.J.B. Estimating accuracy at exercise intensities: a comparative study of self-monitoring heart rate and physical activity wearable devices. JMIR Mhealth Uhealth. 2017;5:e34. doi: 10.2196/mhealth.7043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pasadyn S., et al. Accuracy of commercially available heart rate monitors in athletes: a prospective study. Cardiovasc Diagn Ther. 2019;9:379–385. doi: 10.21037/cdt.2019.06.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang Y., et al. Motion artifact reduction for wrist-worn photoplethysmograph sensors based on different wavelengths. Sensors (Basel) 2019;19:673. doi: 10.3390/s19030673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boudreaux B.D., et al. Validity of wearable activity monitors during cycling and resistance exercise. Med Sci Sports Exerc. 2018;50:624–633. doi: 10.1249/MSS.0000000000001471. [DOI] [PubMed] [Google Scholar]
- 45.Jo E., Lewis K., Directo D., Kim M.J., Dolezal B.A. Validation of biofeedback wearables for photoplethysmographic heart rate tracking. J Sports Sci Med. 2016;15:540–547. [PMC free article] [PubMed] [Google Scholar]
- 46.Sequeira N., D'Souza D., Angaran P., Aves T., Dorian P. Common wearable devices demonstrate variable accuracy in measuring heart rate during supraventricular tachycardia. Heart Rhythm. 2020;17:854–859. doi: 10.1016/j.hrthm.2020.02.018. [DOI] [PubMed] [Google Scholar]
- 47.Lown M., et al. Screening for atrial fibrillation using economical and accurate technology (from the SAFETY study) Am J Cardiol. 2018;122:1339–1344. doi: 10.1016/j.amjcard.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 48.Koshy A.N., et al. Smart watches for heart rate assessment in atrial arrhythmias. Int J Cardiol. 2018;266:124–127. doi: 10.1016/j.ijcard.2018.02.073. [DOI] [PubMed] [Google Scholar]
- 49.Capucci A., et al. Monitored atrial fibrillation duration predicts arterial embolic events in patients suffering from bradycardia and atrial fibrillation implanted with antitachycardia pacemakers. J Am Coll Cardiol. 2005;46:1913–1920. doi: 10.1016/j.jacc.2005.07.044. [DOI] [PubMed] [Google Scholar]
- 50.Glotzer T.V., et al. The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circ Arrhythm Electrophysiol. 2009;2:474–480. doi: 10.1161/CIRCEP.109.849638. [DOI] [PubMed] [Google Scholar]
- 51.Kaplan R.M., et al. Stroke risk as a function of atrial fibrillation duration and CHA2DS2-VASc SCORE. Circulation. 2019;140:1639–1646. doi: 10.1161/CIRCULATIONAHA.119.041303. [DOI] [PubMed] [Google Scholar]
- 52.Swiryn S., et al. Clinical implications of brief device-detected atrial tachyarrhythmias in a cardiac rhythm management device population: results from the Registry of Atrial Tachycardia and Atrial Fibrillation Episodes. Circulation. 2016;134:1130–1140. doi: 10.1161/CIRCULATIONAHA.115.020252. [DOI] [PubMed] [Google Scholar]
- 53.Themistoclakis S., et al. The risk of thromboembolism and need for oral anticoagulation after successful atrial fibrillation ablation. J Am Coll Cardiol. 2010;55:735–743. doi: 10.1016/j.jacc.2009.11.039. [DOI] [PubMed] [Google Scholar]
- 54.Van Gelder I.C., et al. Duration of device-detected subclinical atrial fibrillation and occurrence of stroke in ASSERT. Eur Heart J. 2017;38:1339–1344. doi: 10.1093/eurheartj/ehx042. [DOI] [PubMed] [Google Scholar]
- 55.Yano Y., et al. Simulation of daily snapshot rhythm monitoring to identify atrial fibrillation in continuously monitored patients with stroke risk factors. PLoS One. 2016;11 doi: 10.1371/journal.pone.0148914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Eerikainen L.M., Bonomi A.G., Dekker L.R.C., Vullings R.K., Aarts R.N. Atrial fibrillation monitoring with wrist-worn photoplethysmography-based wearables: state-of-the-art review. Cardiovasc Digital Health J. 2020;1:45–51. doi: 10.1016/j.cvdhj.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wasserlauf J., et al. Smartwatch performance for the detection and quantification of atrial fibrillation. Circ Arrhythm Electrophysiol. 2019;12 doi: 10.1161/CIRCEP.118.006834. [DOI] [PubMed] [Google Scholar]
- 58.Freeman J.V., et al. Outcomes and anticoagulation use after catheter ablation for atrial fibrillation. Circ Arrhythm Electrophysiol. 2019;12 doi: 10.1161/CIRCEP.119.007612. [DOI] [PubMed] [Google Scholar]
- 59.Birnie D.H., Smith E.E., Verma A. To continue or stop oral anti-coagulation in higher-risk patients after a "successful" AF ablation; that is the question. J Cardiovasc Electrophysiol. 2019;30:1258–1260. doi: 10.1111/jce.14056. [DOI] [PubMed] [Google Scholar]
- 60.Liang J.J., Callans D.J. Can anticoagulation be stopped after ablation of atrial fibrillation? Curr Cardiol Rep. 2020;22:58. doi: 10.1007/s11886-020-01313-1. [DOI] [PubMed] [Google Scholar]
- 61.Lohrmann G., Kaplan R., Ziegler P.D., Monteiro J., Passman R. Atrial fibrillation ablation success defined by duration of recurrence on cardiac implantable electronic devices. J Cardiovasc Electrophysiol. 2020;31:3124–3131. doi: 10.1111/jce.14781. [DOI] [PubMed] [Google Scholar]
- 62.Verma A., et al. Discerning the incidence of symptomatic and asymptomatic episodes of atrial fibrillation before and after catheter ablation (DISCERN AF): a prospective, multicenter study. JAMA Intern Med. 2013;173:149–156. doi: 10.1001/jamainternmed.2013.1561. [DOI] [PubMed] [Google Scholar]
- 63.Noseworthy P.A., et al. Patterns of anticoagulation use and cardioembolic risk after catheter ablation for atrial fibrillation. J Am Heart Assoc. 2015;4 doi: 10.1161/JAHA.115.002597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Giudicessi J.R., et al. Artificial intelligence-enabled assessment of the heart rate corrected qt interval using a mobile electrocardiogram device. Circulation. 2021;143:1274–1286. doi: 10.1161/CIRCULATIONAHA.120.050231. [DOI] [PubMed] [Google Scholar]
- 65.Chung E.H., Guise K.D. QTC intervals can be assessed with the AliveCor heart monitor in patients on dofetilide for atrial fibrillation. J Electrocardiol. 2015;48:8–9. doi: 10.1016/j.jelectrocard.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 66.Samol A., et al. Single-lead ECG recordings including Einthoven and Wilson leads by a smartwatch: a new era of patient directed early ECG differential diagnosis of cardiac diseases? Sensors (Basel) 2019;19:4377. doi: 10.3390/s19204377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Strik M., et al. Validating QT-interval measurement using the Apple Watch ECG to enable remote monitoring during the COVID-19 pandemic. Circulation. 2020;142:416–418. doi: 10.1161/CIRCULATIONAHA.120.048253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Maille B., et al. Smartwatch electrocardiogram and artificial intelligence for assessing cardiac-rhythm safety of drug therapy in the COVID-19 pandemic. The QT-logs study. Int J Cardiol. 2021;331:333–339. doi: 10.1016/j.ijcard.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Aroganam G., Manivannan N., Harrison D. Review on wearable technology sensors used in consumer sport applications. Sensors (Basel) 2019;19:1983. doi: 10.3390/s19091983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li R.T., Kling S.R., Salata M.J., Cupp S.A., Sheehan J., Voos J.E. Wearable performance devices in sports medicine. Sports Health. 2016;8:74–78. doi: 10.1177/1941738115616917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Seshadri D.R., et al. Wearable sensors for monitoring the internal and external workload of the athlete. NPJ Digit Med. 2019;2:71. doi: 10.1038/s41746-019-0149-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Moore I.S., Willy R.W. Use of wearables: tracking and retraining in endurance runners. Curr Sports Med Rep. 2019;18:437–444. doi: 10.1249/JSR.0000000000000667. [DOI] [PubMed] [Google Scholar]
- 73.Seshadri D.R., et al. Wearable sensors for monitoring the physiological and biochemical profile of the athlete. NPJ Digit Med. 2019;2:72. doi: 10.1038/s41746-019-0150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Foster C., Rodriguez-Marroyo J.A., de Koning J.J. Monitoring training loads: the past, the present, and the future. Int J Sports Physiol Perform. 2017;12:S22–S28. doi: 10.1123/ijspp.2016-0388. [DOI] [PubMed] [Google Scholar]
- 75.Gajda R., Biernacka E.K., Drygas W. Are heart rate monitors valuable tools for diagnosing arrhythmias in endurance athletes? Scand J Med Sci Sports. 2018;28:496–516. doi: 10.1111/sms.12917. [DOI] [PubMed] [Google Scholar]
- 76.Drager L.F., et al. Sleep apnea and cardiovascular disease: lessons from recent trials and need for team science. Circulation. 2017;136:1840–1850. doi: 10.1161/CIRCULATIONAHA.117.029400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shelgikar A.V., Anderson P.F., Stephens M.R. Sleep tracking, wearable technology, and opportunities for research and clinical care. Chest. 2016;150:732–743. doi: 10.1016/j.chest.2016.04.016. [DOI] [PubMed] [Google Scholar]
- 78.Tiron R., et al. Screening for obstructive sleep apnea with novel hybrid acoustic smartphone app technology. J Thorac Dis. 2020;12:4476–4495. doi: 10.21037/jtd-20-804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Moreno-Pino F., Porras-Segovia A., Lopez-Esteban P., Artes A., Baca-Garcia E. Validation of Fitbit Charge 2 and Fitbit Alta HR against polysomnography for assessing sleep in adults with obstructive sleep apnea. J Clin Sleep Med. 2019;15:1645–1653. doi: 10.5664/jcsm.8032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Faust L., Feldman K., Mattingly S.M., Hachen D., Chawla N.V. Deviations from normal bedtimes are associated with short-term increases in resting heart rate. NPJ Digit Med. 2020;3:39. doi: 10.1038/s41746-020-0250-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chaudhry F.F., et al. Sleep in the natural environment: a pilot study. Sensors (Basel) 2020;20:1378. doi: 10.3390/s20051378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Huynh P., et al. Heart rate measurements in patients with obstructive sleep apnea and atrial fibrillation: prospective pilot study assessing Apple Watch's agreement with telemetry data. JMIR Cardio. 2021;5 doi: 10.2196/18050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yeung C., et al. Extended cardiac monitoring in patients with severe sleep apnea and no history of atrial fibrillation (the Reveal XT-SA study) Am J Cardiol. 2018;122:1885–1889. doi: 10.1016/j.amjcard.2018.08.032. [DOI] [PubMed] [Google Scholar]
- 84.de Zambotti M., Cellini N., Goldstone A., Colrain I.M., Baker F.C. Wearable sleep technology in clinical and research settings. Med Sci Sports Exerc. 2019;51:1538–1557. doi: 10.1249/MSS.0000000000001947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Stone J.D., et al. Evaluations of commercial sleep technologies for objective monitoring during routine sleeping conditions. Nat Sci Sleep. 2020;12:821–842. doi: 10.2147/NSS.S270705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ayas N.T., Pittman S., MacDonald N., White D.P. Assessment of a wrist-worn device in the detection of obstructive sleep apnea. Sleep Med. 2003;4:435–442. doi: 10.1016/s1389-9457(03)00111-4. [DOI] [PubMed] [Google Scholar]
- 87.Perez-Pozuelo I., et al. The future of sleep health: a data-driven revolution in sleep science and medicine. NPJ Digit Med. 2020;3:42. doi: 10.1038/s41746-020-0244-4. [DOI] [PMC free article] [PubMed] [Google Scholar]