Abstract
Background
Most cancers are due to modifiable lifestyle and environmental risk factors, and are potentially preventable. No studies have provided a systematic quantitative assessment of the burden of cancer mortality and incidence attributable to known risk factors in China.
Methods
We calculated the proportions of cancer deaths and new cases attributable to known risk factors in China, based on the prevalence of exposure around 1990 and national data on cancer mortality and incidence for the year 2005.
Results
Chronic infection is the main risk factor for cancer in China, accounting for 29.4% of cancer deaths (31.7% in men and 25.3% in women), followed by tobacco smoking (22.6% with 32.7% in men and 5.0% in women), low fruit intake (13.0%), alcohol drinking (4.4%), low vegetable intake (3.6%) and occupational exposures (2.7%). The remaining factors, including environmental agents, physical inactivity, the use of exogenous hormones and reproductive factors are each responsible for <1.0%.
Conclusions
Modifiable risk factors explain nearly 60% of cancer deaths in China, with a predominant role of chronic infection and tobacco smoking. Our findings could provide a basis for cancer prevention and control programs aimed at reducing cancer risk in other developing countries.
Keywords: cancer, modifiable risk factors, population attributable fraction, China
introduction
Cancer remains a major cause of mortality worldwide. Developed countries have made strides in prevention of some cancers, such as tumors caused by smoking and chronic infections, the incidence of these cancers are on the rise in developing countries. Exposure to lifestyle and environmental risk factors, however, are large differences in developing versus developed countries. China has a population of about 1.4 billion, accounting for 20% of the world's population. The age-adjusted cancer mortality in 2005 was 11.9 per million in men and 6.4 per million in women [1]. Cancer is the leading cause of death in China, cancer mortality is projected to increase significantly over the next 20–30 years. Developing effective cancer prevention and control programs in China require overcoming unique challenges. A necessary starting point, however, is to identify the proportion of cancer incidence and mortality caused by modifiable risk factors in the country. Previous studies of comprehensive assessments on the cancer burden in China have been limited, often restricting to one risk factor, one single cancer type or subpopulation [2–4].
Therefore, this report is to provide for the first time a systematic assessment of the number of cancer cases and deaths attributable to demonstrated carcinogens in China. Findings from our report should provide a rationale for prioritizing public health and research efforts in the future. Furthermore, our results would be informative for other countries in the region, with similar risk factor and cancer profiles.
methods
Our project is to estimate the contribution of known risk factors of cancer, including tobacco smoking [5], alcohol drinking [6], chronic infections [7], diet [8], overweight and obesity [9], occupational and environmental factors [10], exogenous hormones [11], to the burden of the disease through the calculation of proportion of specific cancers occurring in China in 2005 attributable to specific risk factors. As several project-related articles have already been published, this article focuses on the joint effects of modifiable risk factors on cancer and comparing these joint effects with those found in other similar studies. The proportion of cancer in the total population that can be attributable to a risk factor is defined as population attributable fraction (PAF). For avoidable risk factors, PAF is the proportion of cancer that would not have occurred had the exposure not taken place. For others, zero exposure is inappropriate, PAF is the fraction of cancer that would not occur with an alternative scenario of level or frequency of exposure, in general based on public health recommendations. We used systematic review and meta-analyses evidence on risk exposure and relative risk (RR) from the published data to estimate the population attributable fractions (PAFs). For every risk factor, a working group undertook comprehensive assessments of published studies and other sources to acquire data of exposure rate and RR.
definition of exposure
We selected the risk factors of cancer based on the including criteria:
Agents that have sufficient evidence as human carcinogens according to International Agency for Research on Cancer (IARC) Monographs [12].
Agents are causally associated with a reduced risk of cancer, according to IARC Cancer Prevention Handbook [13].
Agents that have never been evaluated by IARC, but with strong evidence for a causal association with cancer risk (e.g. reproductive factors and breast cancer risk) [14].
The risk factors included in our study are listed in Table 1. Some risk factors were excluded, because of a lack of available data at the national level, such as use of smokeless tobacco products, ionizing radiation, some occupational and infectious agents. The current health effects of cancer reflect the past patterns of exposure [15]. We selected a latency time of 15 years for exposures and cancer occurrence as a compromise [16]. Therefore, priority was given to exposure prevalence data referring to around 1990. For exogenous hormones, we assumed that no lag-time between hormone replacement therapy (HRT), oral contraceptives (OCs) and breast/ovarian cancer; we, therefore, used recent exposure data for HRT and OCs. For reproductive factors, we used data for 2001 (5-year latency).
Table 1.
Risk factors of cancer included in the study
| Risk factors | Specific exposures | Comments |
|---|---|---|
| Tobacco smoking | Ever-smoking | – |
| Alcohol drinking | Ever-drinking | – |
| Infectious agents | Human papillomavirus, Hepatitis B virus, Hepatitis C virus, Helicobacter pylori, Epstein–Barr virus | Excluded: human immunodeficiency virus, human T-cell lymphotropic virus-I, human herpes virus-8, Schistosoma hematobium, Clonorchis sinensis |
| Diet | Low vegetable and fruit intake | – |
| Occupational agents | Asbestos, silica, coke oven emissions, chromate, benzene, benzidine, arsenic, wood dust, leather dust, rubber industry | Several known carcinogens excluded painters, cadmium, aromatic amines, polycyclic aromatic hydrocarbons, ionizing radiation |
| Environmental agents | Indoor radon, passive smoking | – |
| Overweight and obesity | Body mass index over 25 and 30 kg/m2 | – |
| Physical inactivity | Lack of physical activity | – |
| Exogenous hormones | Hormone replacement therapy, oral contraceptives | Use of recent data on exposure frequency |
| Reproductive factors | Nulliparity, number of children, age at first birth, breast-feeding | Comparison with ideal exposure patterna |
aIdeal exposure pattern is zero nulliparity, none of women giving first birth after 30, two children per woman and 12 months of breast-feeding.
relative risks
Data on relative risks (RRs) were obtained from the studies identified from different sources, including PubMed, Websites, VIP Information, China National Knowledge Infrastructure and other databases (such as Springer). The search words involved ‘meta-analysis’, ‘case-control study’, ‘cohort study’, the name of specific risk factors and specific cancers. The studies retained for estimate should contain information of RRs or odds ratios and corresponding 95% confidence intervals and publish in the last 20 years; the languages covered in English and Chinese; the highest priority was given to meta-analyses and large-scale surveys of representative samples in China, followed by nonrepresentative samples of Chinese populations, meta-analysis from other Asian countries and finally meta-analysis from non-Asian countries (supplementary Table S1, available at Annals of Oncology online).
cancer mortality and incidence data
The Third National Death Cause Survey in China has been described in detail elsewhere [17]. Briefly, this was a retrospective survey, conducted in 160 randomized counties and 53 cancer high-risk areas from 2004 to 2005. In China, cancer mortality rate was 135.9/100 000 and age-adjusted mortality rate was 91.2/100 000 using the third census data. The cancer mortality data, used in the calculation of cancer deaths attributed to selected risk factors, were derived from that survey.
Cancer incidence data were estimated by applying mortality-to-incidence (M/I) ratio to the data on cancer deaths. M/I ratio [17] was derived from the data of 32 regional population-based cancer registries from 2003 to 2004 and calculated using Poisson regression adjusting for age, gender and sites (supplementary Table S2, available at Annals of Oncology online).
statistical methods
PAF was calculated based on the RR and frequency of population exposure to the risk factor [18].
RR is relative risk of a risk factor and a specific cancer, while P is the prevalence of exposure to the risk factor in the total population.
For continuous variables in risk factors such as number of children, PAF was obtained by multiplying the RR for unit exposure (RRi, e.g. RR for having one child) and the average exposure level (d), shown in the following formula, assuming a log-linear relationship between exposure and cancer risk.
Because most cancers are caused by multiple risk factors, PAF for individual risk factors for the same cancer sites can overlap and add to over 100%. In our study, we take into account the degree of overlap of PAF, assuming the independence between exposure and risk. Combined PAF for exposure to two risk factors A and B can be calculated by the following formula [19]:
This formula can also be extended to more than two risk factors.
We estimated the number of attributable deaths and incident cases of cancer by applying the estimated PAFs to the number of cancer deaths and new cases. The fraction of cancer mortality and incidence attributable to one specific risk factor was calculated by summing the attributable deaths and new cases of each kind of cancer, then dividing by the total cancer deaths and incident cases. We also calculated the fraction of deaths and new cases of individual cancers attributable to selected risk factors by applying the combined PAF estimates to that cancer incidence and mortality data.
results
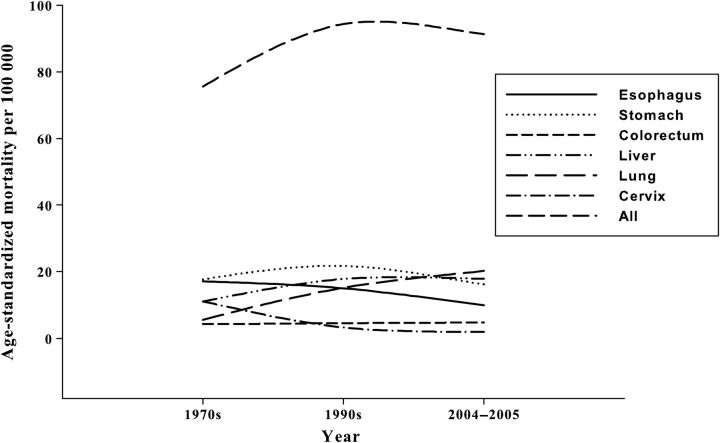
Time trends in cancer mortality in China are shown in Figure 1. The five common cancer sites are lung, stomach, liver, esophagus and colorectum. For lung and liver cancers, mortality has increased rapidly since 1970s, mainly due to the increasing exposure of smoking and hepatitis B virus (HBV)/hepatitis C virus (HCV) infection. In 2005, age-standardized mortality of lung cancer was 20.2/100 000. In contrast, mortality of stomach, esophageal and cervical cancers have slowly decreased since 1970s. In 2005, age-standardized mortality of stomach cancer was 16.2/100 000, decreased by 8.7% compared with the value in 1970s. Colorectal cancer mortality was relatively stable, with the rate of around 5.0/100 000.
Figure 1.
Temporal trends in cancer mortality in China from 1970 to 2005, by cancer sites (age standardized mortality rate based on Chinese population).
The estimated PAFs are summarized in Table 2. Chronic infection and tobacco smoking were the two main cancer risk factors in China, and were responsible for 29.4 and 22.6% of cancer deaths in China, respectively. Corresponding PAF for low fruit intake was 13.0%. Alcohol drinking, low vegetable intake and occupational agents were responsible for 2.7–4.4% of cancer deaths. The remaining factors accounted for <1.0% of cancer deaths, including environmental factors, overweight and obesity, physical inactivity, reproductive factors, OCs and HRT. In general, the fraction of cancer deaths in men and women attributable to the selected modifiable risk factors was 65.9 and 42.8%, respectively. Corresponding PAFs for cancer incidence are similar with the ones for cancer mortality (supplementary Figure S3, available at Annals of Oncology online).
Table 2.
Cancer deaths attributable to selected risk factors in China in 2005
| Risk factors | Men |
Women |
Total |
|||
|---|---|---|---|---|---|---|
| PAF% | N | PAF% | N | PAF% | N | |
| Infectious agents | 31.70 | 360 673 | 25.30 | 165 895 | 29.39 | 526 568 |
| Tobacco smoking | 32.74 | 372 264 | 5.02 | 32 848 | 22.61 | 405 112 |
| Low fruit intake | 13.70 | 155 983 | 11.70 | 76 858 | 13.00 | 232 841 |
| Alcohol drinking | 6.69 | 76 109 | 0.42 | 2774 | 4.40 | 78 883 |
| Low vegetable intake | 3.90 | 44 083 | 3.10 | 20 413 | 3.60 | 64 496 |
| Occupational agents | 3.08 | 34 795 | 2.07 | 13 536 | 2.70 | 48 331 |
| Environmental agents | 0.04 | 429 | 1.79 | 11 709 | 0.68 | 12 138 |
| Overweight and obesity | 0.06 | 671 | 0.78 | 5111 | 0.32 | 5782 |
| Physical inactivity | 0.31 | 3513 | 0.21 | 1350 | 0.27 | 4863 |
| Reproductive factorsa | – | – | 0.47 | 3065 | 0.17 | 3065 |
| Oral contraceptives and hormone replacement therapy | – | – | 0.03 | 175 | 0.01 | 175 |
| All the above | 65.88 | 748 944 | 42.80 | 280 227 | 57.44 | 1 029 171 |
PAF, population attributable fraction.
aNulliparity, parity, % with age at first birth ≥30 years, and number of months breast-feeding.
Summary results for individual cancers are reported in Table 3. PAFs for nasopharyngeal and cervical cancers were explained 100% by Epstein–Barr virus (EBV) and human papillomavirus (HPV) infection, respectively. Very large PAFs ≥70% were observed for cancers strongly associated with smoking, alcohol drinking, chronic infection and low vegetable and fruit intake (e.g. oral cavity and pharyngeal, noncardia gastric and liver cancers). For lung and cardia gastric cancers, PAFs were 60–70%. PAFs in the range of 20–60% were observed for cancers with one or more important, but not dominant, risk factors (e.g. esophageal, bladder, pancreatic cancers, Hodgkin's disease). For mesothelioma, breast, colon cancers and leukemia, PAFs were 10–20%. PAFs <10% were seen for Non-Hodgkin's lymphoma, rectum and kidney cancers whose etiology is largely unidentified. Discrepancies in cancer-specific PAF between men and women were explained by the different frequency of exposure to important risk factors, such as smoking, alcohol drinking and chronic infection.
Table 3.
Summary of population attributable fractions of cancer deaths (%) by cancer sites in China in 2005
| Cancer sites | Men |
Women |
Total |
|||
|---|---|---|---|---|---|---|
| PAF (%) | N | PAF (%) | N | PAF (%) | N | |
| Nasopharynx | 100.0 | 13 799 | 100.0 | 5438 | 100.0 | 19 237 |
| Cervix uteri | – | – | 100.0 | 18 484 | 100.0 | 18 484 |
| Gastric noncardia | 87.0 | 148 164 | 82.1 | 75 602 | 85.3 | 223 766 |
| Liver | 84.6 | 208 709 | 71.2 | 65 887 | 80.9 | 274 596 |
| Pharynx | 83.3 | 2094 | 69.5 | 605 | 79.7 | 2699 |
| Oral cavity | 80.7 | 3902 | 64.7 | 1503 | 75.5 | 5405 |
| Gastric cardia | 71.6 | 30 460 | 60.7 | 8359 | 68.9 | 38 819 |
| Lung | 80.5 | 229 990 | 41.1 | 55 314 | 67.9 | 285 304 |
| Esophagus | 51.4 | 67 647 | 33.1 | 19 381 | 45.8 | 87 028 |
| Urinary bladder | 43.5 | 6471 | 14.6 | 663 | 36.7 | 7134 |
| Hodgkin's disease | 24.7 | 389 | 24.7 | 243 | 24.7 | 632 |
| Pancreas | 36.0 | 7643 | 9.8 | 1599 | 24.6 | 9242 |
| Larynx | 30.5 | 2721 | 3.4 | 88 | 24.3 | 2809 |
| Burkitt's lymphoma | 24.0 | 66 | 24.0 | 33 | 24.0 | 99 |
| Mesothelioma | 18.6 | 125 | 18.8 | 93 | 18.5 | 218 |
| Breast | – | – | 14.8 | 5943 | 14.8 | 5943 |
| Endometrium | – | – | 14.7 | 1547 | 14.7 | 1547 |
| Colon | 19.7 | 4046 | 8.3 | 1373 | 14.6 | 5419 |
| Ovary | – | – | 12.4 | 1296 | 12.4 | 1296 |
| Leukemia | 9.9 | 2838 | 15.4 | 3429 | 12.3 | 6267 |
| Non-Hodgkin's lymphoma | 4.4 | 467 | 4.7 | 305 | 4.5 | 772 |
| Sinonasal | 3.7 | 51 | 2.8 | 22 | 3.4 | 73 |
| Rectum | 2.5 | 914 | 1.7 | 428 | 2.2 | 1342 |
| Kidney | 1.4 | 91 | – | – | 1.4 | 91 |
Abbreviation: PAF, population attributable fraction.
discussion
This is the first systematic assessment of the burden of modifiable risk factors-related cancer incidence and mortality in China. In 2005, age-adjusted cancer mortality in China increased by 20.7% compared with that in 1970s. There was no significant difference between urban and rural areas for age-adjusted cancer mortality. Cancer mortality for lung and liver has dramatically increased since 1970s, whereas it has decreased for cancers of cervix and esophagus. China is now undergoing a rapid industrialization and socioeconomic transition, leading to changes in cancer risk factors. Infection and smoking are the two common cancer risk factors in China.
Chronic infection was the main cancer risk factor in China. Over one-quarter of cancers were attributable to infection and the most common carcinogenic infections were HBV/HCV and Helicobacter pylori. Our findings were consistent with the results from a previous global analysis [20], which was 26.3% of total cancers in developing countries. The PAF values in our study varied from 100% of cervical and nasopharyngeal cancers (HPV and EBV, respectively) to 3.8% of oral cancer (HPV). Some rather minor differences between our estimates and those published by Parkin [20] are explained by the fact that we used data specific for China versus more global data used by Parkin, and the exclusion of some relatively minor oncogenic infections such as human immunodeficiency virus, human herpes virus 8, liver flukes and schistosomes from our estimate. However, the three cancer types (stomach, liver and cervix) accounted for the largest proportion of infection-related cancers both in the Parkin's and our studies. Our estimate of the role of chronic infections in cancer was comparable with those recently made for Japan (21.7%) [21] and Korea (24.7%) [22].
Tobacco smoking was the predominant cancer cause among men in China. The smoking-related cancer deaths in men represent ∼9% of all global cancer deaths among men [23] and 25% of smoking-related cancer deaths worldwide [24]. Furthermore, involuntary smoking is a relatively important cause of cancer in China, causing 11% of lung cancer deaths among nonsmoking women. Our results were consistent with the previous Chinese study based on the similar methodology [25–27] and the estimates by Peto [28] (Asia men: 34% of cancer deaths, Asia women: 4%). Our estimates, however, is likely to represent a conservative evaluation of the burden of tobacco-related cancer in China because of excluding a few rare cancers. The discrepancy of the results underlined the uncertainty of our PAF estimate for smoking whose impact did not reach full maturity. Smoking prevalence in China is slowly decreasing, but the burden of tobacco-related cancer will increase in the future.
Diet was the third risk factor of cancer in China, responsible for ∼16% of all cancer deaths. Data from Comparative Risk Assessment project [24] have illustrated that low fruit and vegetable intake explains 5% of cancer deaths worldwide, with 6% in low- and middle-income countries and 3% in high-income countries. Our results indicated a higher PAF for low vegetable and fruit intake than the previous estimate in low- and middle-income countries. Recently, the insufficient intake of fruit and vegetable is estimated to cause around 14% of gastrointestinal cancer deaths worldwide [29], i.e. close to ours. One limitation in this report is that RRs for low vegetable and fruit intake are originated from the global meta-analysis, but not from the studies in the Chinese population (not available). Other dietary factors (such as meat and fish intake) potentially associated with cancer were excluded in our study.
Alcohol drinking accounted for 4.4% of cancer deaths and 3.6% of cancer new cases in China. Alcohol drinking has considerably increased in China over the recent decades [30]. Our results were comparable with the previous global studies, which were 3–5% of cancer deaths caused by alcohol drinking worldwide [24, 31]. In our study, the stomach, breast, and pancreatic cancers were excluded because of the inconsistent evidence in Asian populations [32–34]. More research needs to elucidate whether their association is causal or is instead due to biases.
The other risk factors, including occupational and environmental agents, overweight/obesity, physical inactivity, reproductive factors, OCs and HRT, played a relatively limited role in our study. For these factors, our estimates are likely to be conservative evaluations. More than 30 occupational agents have been identified as carcinogens by IARC, but 10 agents included in our estimates. Exposure data on several agents were not available at the national level, such as vinyl chloride (causing liver angiosarcoma) and occupation as a painter (causing lung and bladder cancers). The effect of outdoor air pollution was excluded in our analysis. A previous similar study in France indicated that the proportion of cancer deaths attributable to air pollution was <1% [35]. The corresponding figure in the lung cancer deaths was 5% [36]. Our estimate for overweight/obesity was much lower than that in high-income countries. The possible explanation was the low prevalence used in our report. A rapid increase of the prevalence was observed during the past decade with an increase from 14.6% in 1992 to 21.8% in 2002 [37]. We projected the PAF based on the prevalence in 2002 and observed that the contribution of overweight/obesity to the cancer burden will increase in the future [9]. Other factors, such as ionizing radiation, drugs etc., are not studied in this article. Most of ionizing radiation originates from medical X-rays, cosmic and terrestrial radiations. Carcinogenic effects of high and middle doses of ionizing radiation are well demonstrated, but no direct observational epidemiological data support an association between exposure to low doses of ionizing radiation and cancer occurrence. Another argument is that medical X-rays are not ‘avoidable’ in the same sense as environmental factors. Aspirin and other nonsteroidal anti-inflammatory drugs have been considered as chemopreventive agents due to their anti-inflammatory properties. Previous studies have indicated the conflicting epidemiology evidence on their associations with cancer risk [38, 39]. The main argument for not including them is that benefits are expected to overcome risks, so these exposures are not avoidable as for environmental factors. The main issue with drugs is the increased risk of secondary cancer following chemotherapy.
The causes of a large number of types of cancer are largely unknown. For several important cancers, such as non-Hodgkin's lymphoma and kidney, brain and prostate cancers, we were able to attribute <5% of cases or death to known causes. About 46% of esophageal cancer deaths were attributable to smoking, alcohol drinking and low fruit and vegetable intake. We did not evaluate other known risk factors of esophageal cancer, including pickled vegetable consumption, poor oral health, hot drink consumption and low socioeconomic status, due to a lack of available data at the national level. Moreover, these high-risk circumstances represent special cases and have little impact on the overall PAF estimates. This fact stresses the need for further research in the modifiable causes of human cancer, in particular in countries undergoing a rapid transition in cancer risk such as China.
We compared our estimates of the combined PAFs with similar previous studies in different countries (Table 4). PAFs in our analysis were higher than the corresponding figures in Japan [21], France [16], the UK [40], Nordic countries [41] and the world [24], because of the predominant role of chronic infection on cancer in China. In China, chronic infection and smoking accounted for ∼45% of cancer deaths. In the western populations, on the other hand, chronic infection is a less important risk factor for cancer.
Table 4.
Comparison of the PAF (%) of cancer deaths or incident cases attributable to the combined effects of modifiable risk factors in various studies
| Studies | Men | Women | Total |
|---|---|---|---|
| Our studya | 65.9 | 42.8 | 57.4 |
| Worldwide study [24]b | – | – | 35.0 |
| Low- and middle-income countriesb | – | – | 34.0 |
| High-income countriesb | – | – | 37.0 |
| Japan study [21]c | 56.9 | 29.9 | 46.2 |
| French study [16]d | 42.5 | 23.6 | 35.0 |
| Nordic study [41]e | 33.0 | 20.0 | 17.5 |
| UK study [40]f | 45.3 | 40.1 | 42.7 |
PAF, population attributable fraction.
aPAF of cancer mortality was calculated for the combined effects of chronic infection, smoking, alcohol drinking, low vegetable and fruit intake, overweight/obesity, physical inactivity, occupational and environmental agents, reproductive factors and exogenous hormones.
bPAF of cancer mortality was calculated for the combined effects of smoking, alcohol drinking, low vegetable and fruit intake, overweight/obesity, physical inactivity, indoor smoke from household use of solid fuels, urban air pollution, contaminated injections in health-care settings and unsafe sex.
cPAF of cancer mortality was calculated for the combined effects of chronic infection, smoking, passive smoking, alcohol drinking, low vegetable and fruit intake, overweight/obesity, physical inactivity, salt intake and exogenous hormones.
dPAF of cancer mortality was calculated for the combined effects of chronic infection, smoking, alcohol drinking, overweight/obesity, physical inactivity, occupational agents, ultraviolet light, pollutants and exogenous hormones.
ePAF of cancer incidence was calculated for the combined effects of chronic infection, smoking, passive smoking, alcohol drinking, overweight/obesity, occupational agents, radon, solar radiation and man-made ionizing radiation.
fPAF of cancer incidence was calculated for the combined effects of chronic infection, smoking, alcohol drinking, consumption of vegetable, fruit, meat, fiber and salt, overweight/obesity, physical inactivity, occupational agents, radiation (ionizing and solar) and exogenous hormones and breast-feeding.
The strengths of our study include first systematic assessment of cancer causes, exposure data from a large-scale representative of the Chinese population, RRs from meta-analysis and large-scale studies, new national data on cancer mortality and incidence. However, there were several sources of uncertainty in the PAF estimates. First, data on exposure prevalence of some infectious agents were not obtained from mainland Chinese population, such as EBV. Secondly, RRs can vary from one population to another because of the impact of other risk factors and the interaction with environmental and genetics factors, which may be difficult to evaluate the direction and magnitude of this potential bias. For some risk factors, RRs from China were not available and were obtained from large sample size, high-quality and non-Chinese population studies. Thirdly, some risk factors, such as outdoor air pollutants, were excluded because they are not currently recognized as an established cause of cancer by IARC. Finally, cancer incidence was lacking, and was estimated from mortality data using M/I ratio.
Our estimates provide a systematic assessment of the burden of cancer incidence and mortality attributable to modifiable risk factors in China. Generally, nearly 60% of cancers in China can be avoidable. The effect of unselected risk factors on cancer in the whole Chinese population is still unknown. It is needed to continue more fundamental research on other lifestyle and genetic factors to illuminate the questions. This report reinforces the notion that the control of oncogenic infections and smoking are by far the main avenues for reducing the burden of cancer in China, but other risk factors, including alcohol drinking and diet, should not be neglected.
authors’ contribution
J.B.W., Y.L.Q., and P.B. had all access to the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Y.L.Q., W.Q.W., and P.B. contributed to study the concept and design. J.B.W., Y.J., H.L., P.L., H.J.X., J.J., W.X., J.F.S., Y.G.F., L.L., D.W., S.S.D., and W.Q.C. obtained and analyzed the data. J.B.W. drafted the report, which was edited by Y.L.Q. and P.B. All authors have reviewed and approved the final version.
funding
International Agency for Research on Cancer (Lyon, France; Grant number: CRA No GEE/08/19) and Cancer Institute, Chinese Academy of Medical Sciences (Beijing, China; Grant number: JK2011B19). The sponsor of the study had no role in study design, data collection, data analysis, data interpretation, decision to publish or preparation of the manuscript.
disclosures
The authors have declared no conflicts of interest.
Supplementary Material
references
- 1.Ministry of Health of the people's republic of China. Beijing, China: Chinese Academy of Medical Sciences and Peking Union Medical College Press; 2008. Report on the Third National Retrospective Survey of Death causes in China. [Google Scholar]
- 2.Lam TH, He Y, Li LS, et al. Mortality attributable to cigarette smoking in China. JAMA. 1997;278:1505–1508. doi: 10.1001/jama.1997.03550180055037. [DOI] [PubMed] [Google Scholar]
- 3.Shen XB, Wang GX, Huang YZ, et al. Analysis and estimates of attributable risk factors for lung cancer in Nanjing, China. Lung Cancer. 1996;14(Suppl 1):S107–S112. doi: 10.1016/s0169-5002(96)90216-0. [DOI] [PubMed] [Google Scholar]
- 4.Wu M, Van't Veer P, Zhang ZF, et al. A large proportion of esophageal cancer cases and the incidence difference between regions are attributable to lifestyle risk factors in China. Cancer Lett. 2011;308:189–196. doi: 10.1016/j.canlet.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Wang JB, Jiang Y, Wei WQ, et al. Estimation of cancer incidence and mortality attributable to smoking in China. Cancer Causes Control. 2010;21:959–965. doi: 10.1007/s10552-010-9523-8. [DOI] [PubMed] [Google Scholar]
- 6.Liang H, Wang JB, Xiao HJ, et al. Estimation of cancer incidence and mortality attributable to alcohol drinking in China. BMC Public Health. 2010;10:730. doi: 10.1186/1471-2458-10-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xiang W, Shi JF, Li P, et al. Estimation of cancer cases and deaths attributable to infection in China. Cancer Causes Control. 2011;22:1153–1161. doi: 10.1007/s10552-011-9791-y. [DOI] [PubMed] [Google Scholar]
- 8.Xiao HJ, Liang H, Wang JB, et al. Attributable causes of cancer in china: fruit and vegetable. Chin J Cancer Res. 2011;23:171–176. doi: 10.1007/s11670-011-0171-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang D, Zheng W, Wang SM, et al. Estimation of cancer incidence and mortality attributable to overweight, obesity, and physical inactivity in China. Nutr Cancer. 2012;64:48–56. doi: 10.1080/01635581.2012.630166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li P, Deng SS, Wang JB, et al. Occupational and environmental cancer incidence and mortality in China. Occup Med (Lond) 2012 doi: 10.1093/occmed/kqs016. [DOI] [PubMed] [Google Scholar]
- 11.Li L, Ji J, Wang JB, et al. Attributable causes of breast cancer and ovarian cancer in China: reproductive factors, oral contraceptives and hormone replacement therapy. Chin J Cancer Res. 2012;24:9–17. doi: 10.1007/s11670-012-0009-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Vol. 1–91. Lyon, France: IARC; 1972. [PMC free article] [PubMed] [Google Scholar]
- 13.International Agency for Research on Cancer. IARC Handbooks of Cancer Prevention. Vol. 1–11. Lyon, France: IARC; pp. 1997–2007. [Google Scholar]
- 14.Kelsey JL, Gammon MD, John EM. Reproductive factors and breast cancer. Epidemiol Rev. 1993;15:36–47. doi: 10.1093/oxfordjournals.epirev.a036115. [DOI] [PubMed] [Google Scholar]
- 15.Doll R, Peto R, Wheatley K, et al. Mortality in relation to smoking: 40 years’ observations on male British doctors. BMJ. 1994;309:901–911. doi: 10.1136/bmj.309.6959.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boffetta P, Tubiana M, Hill C, et al. The causes of cancer in France. Ann Oncol. 2009;20:550–555. doi: 10.1093/annonc/mdn597. [DOI] [PubMed] [Google Scholar]
- 17.Chen WQ. Estimation of cancer incidence and mortality in China in 2004–2005. Chin J Oncol. 2009;31:664–668. [PubMed] [Google Scholar]
- 18.Levin ML. The occurrence of lung cancer in man. Acta Unio Int Contra Cancrum. 1953;9:531–541. [PubMed] [Google Scholar]
- 19.Ezzati M, Hoorn SV, Rodgers A, et al. Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet. 2003;362:271–280. doi: 10.1016/S0140-6736(03)13968-2. [DOI] [PubMed] [Google Scholar]
- 20.Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer. 2006;118:3030–3044. doi: 10.1002/ijc.21731. [DOI] [PubMed] [Google Scholar]
- 21.Inoue M, Sawada N, Matsuda T, et al. Attributable causes of cancer in Japan in 2005—systematic assessment to estimate current burden of cancer attributable to known preventable risk factors in Japan. Ann Oncol. 2012;23:1362–1369. doi: 10.1093/annonc/mdr437. [DOI] [PubMed] [Google Scholar]
- 22.Shin A, Park S, Shin HR, et al. Population attributable fraction of infection-related cancers in Korea. Ann Oncol. 2011;22:1435–1442. doi: 10.1093/annonc/mdq592. [DOI] [PubMed] [Google Scholar]
- 23.Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 24.Danaei G, Vander Hoorn S, Lopez AD, et al. Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors. Lancet. 2005;366:1784–1793. doi: 10.1016/S0140-6736(05)67725-2. [DOI] [PubMed] [Google Scholar]
- 25.Niu SR, Yang GH, Chen ZM, et al. Emerging tobacco hazards in China: 2. Early mortality results from a prospective study. BMJ. 1998;317:1423–1424. doi: 10.1136/bmj.317.7170.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu BQ, Peto R, Chen ZM, et al. Emerging tobacco hazards in China: 1. Retrospective proportional mortality study of one million deaths. BMJ. 1998;317:1411–1422. doi: 10.1136/bmj.317.7170.1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gu DF, Kelly TN, Wu XG, et al. Mortality attributable to smoking in China. N Engl J Med. 2009;360:150–159. doi: 10.1056/NEJMsa0802902. [DOI] [PubMed] [Google Scholar]
- 28.Peto R, Lopez AD, Boreham J, et al. Mortality from Smoking in Developed Countries 1950–2000. Oxford, UK: Oxford University Press; 1994. [Google Scholar]
- 29.Promoting Fruit and Vegetable Consumption Around the World. http://www.who.int/dietphysicalactivity/fruit/en/index2.html. (8 September 2011, date last accessed)
- 30.Ma GS. The Nutrition and Health Status of the Chinese People: Behaviors and Lifestyle in 2002. Beijing, China: People Health Press,; 2006. [Google Scholar]
- 31.Boffetta P, Hashibe M, La Vecchia C, et al. The burden of cancer attributable to alcohol drinking. Int J Cancer. 2006;119:884–887. doi: 10.1002/ijc.21903. [DOI] [PubMed] [Google Scholar]
- 32.Rao KQ, Li LD. Research Report on Risk Factor of Cancer in China. Beijing, China: Peking Union Medical College Press,; 2003. [Google Scholar]
- 33.Shimazu T, Tsuji I, Inoue M, et al. Alcohol drinking and gastric cancer risk: an evaluation based on a systematic review of epidemiologic evidence among the Japanese population. Jpn J Clin Oncol. 2008;38:8–25. doi: 10.1093/jjco/hym152. [DOI] [PubMed] [Google Scholar]
- 34.Tramacere I, Scotti L, Jenab M, et al. Alcohol drinking and pancreatic cancer risk: a meta-analysis of the dose-risk relation. Int J Cancer. 2010;126:1474–1486. doi: 10.1002/ijc.24936. [DOI] [PubMed] [Google Scholar]
- 35.International Agency for Research on Cancer. Académie des Sciences–Institut de France, Académie de Médecine, Fédération Nationale des Centres de Lutte contre le Cancer. IARC working group reports, Vol 3, attributable causes of cancer in France in the year 2000. Lyon, France: IARC Press; 2007. [Google Scholar]
- 36.World Health Organization. Geneva, Switzerland: World Health Organization; 2002. The World Health Report 2002: Reducing Risks, Promoting Healthy Life. [Google Scholar]
- 37.Wang Y, Mi J, Shan XY, et al. Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes (Lond) 2007;31:177–188. doi: 10.1038/sj.ijo.0803354. [DOI] [PubMed] [Google Scholar]
- 38.Bardia A, Ebbert JO, Vierkant RA, et al. Association of aspirin and nonaspirin nonsteroidal anti-inflammatory drugs with cancer incidence and mortality. J Natl Cancer Inst. 2007;99:881–889. doi: 10.1093/jnci/djk200. [DOI] [PubMed] [Google Scholar]
- 39.Daugherty SE, Pfeiffer RM, Sigurdson AJ, et al. Nonsteroidal anti-inflammatory drugs and bladder cancer: a pooled analysis. Am J Epidemiol. 2011;173:721–730. doi: 10.1093/aje/kwq437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parkin DM, Boyd L, Walker LC. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br J Cancer. 2011;105(Suppl 2):S77–S81. doi: 10.1038/bjc.2011.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Olsen JH, Andersen A, Dreyer L, et al. Summary of avoidable cancers in the Nordic countries. APMIS. 1997;76(Suppl):141–146. doi: 10.1111/j.1600-0463.1997.tb05617.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.