Abstract
Context/Objective
The risk of lower extremity (LE) fractures in persons with spinal cord injury or disorders (SCI/D) is double that of the able-bodied population. LE fractures are the most common fracture location in SCI/D. Physical therapists (PTs) and occupational therapists (OTs) play an important role in rehabilitating LE fractures in Veterans with SCI/D. This paper describes their role in assisting persons with SCI/D and LE fractures to return to previous function and levels of participation.
Design
Cross-sectional semi-structured interviews were conducted by telephone. Setting: VA SCI centers
Participants
Purposive sample of therapists (PTs and OTs) experienced in LE fracture rehabilitation in SCI/D Interventions: NA.
Outcome Measures
Coding of responses used a data-driven thematic and deductive approach, dictated by a semi-structured interview guide addressing the entire treatment process.
Results
Participants strongly advocated for early PT/OT involvement in post-fracture rehabilitation in order to recommend braces and devices to minimize skin breakdown, and needs for patient equipment, skills training and/or caregiver assistance resulting from post-fracture mobility changes. Seating specialists should be involved in post-fracture seating assessments in wheelchair users to address changes in alignment, deformities, limb length discrepancies and/or seating posture during and following fracture management.
Conclusion
PTs and OTs are critical in rehabilitating LE fractures in persons with SCI/D and LE fractures, bringing expertise in patient function, ambulatory status, transfer strategies, mobility equipment, spasticity, lifestyle, and home and caregiver support. Involving them early in the rehabilitation process, along with orthopedic surgeons, physiatrists and other SCI clinicians can address the multiple and often unique issues that occur in managing fractures in this population.
Keywords: Spinal cord injury, Fracture, Osteoporosis, Physical therapy, Occupational therapy
Introduction
The National Spinal Cord Injury Statistical Center estimates that there are approximately 291,000 persons in the United States living with a Spinal Cord Injury or disorder (SCI/D).1 The Department of Veterans’ Affairs (VA) SCI/D System of Care provides comprehensive, life-long care to over 27,000 Veterans with SCI/D across 25 hub (Centers) and 130 spoke facilities.2
Approximately 80% of Veterans with SCI/D develop either osteopenia or osteoporosis, with approximately 50 to 70% sublesional loss of bone mineral density (BMD).3–6 Low BMD in individuals with SCI/D is associated with increased fracture risk.7 Persons with SCI have a 25–34% lifetime incidence of sustaining a lower extremity (LE) fracture,7,8 and LE fracture risk in persons with SCI/D is twice that of the able-bodied population.9–11
LE fractures constitute more than 80% of fractures in persons with SCI/D, with the most common location being the distal femur and proximal tibia.12–14 Complications, including non-/mal- unions, amputations, pressure injuries, etc., are common sequelae following LE fracture. However, currently, there are no guidelines for fracture management in SCI/D. As a result, management of LE fractures in persons with SCI/D is largely determined on a case-by-case basis, through discussions with patients, medical and surgical (orthopaedic) teams and therapists.15
Non-operative (“conservative”) LE fracture management has been the traditional treatment modality used; however, surgical management is increasing.6,16 Conservative management frequently begins with immobilization of the fracture site, and a period of range-of-motion (ROM) limitation in the affected joint(s). In some cases, a new wheelchair prescription or modifications to the existing seating plan are needed.4
LE fractures are infrequent but potentially devastating events in the lives of persons with SCI.17,18 Even in the simplest scenario, healing a LE fracture requires a significant amount of time as well as restrictions to the individual’s ability to participate in daily activities. There is little empirical evidence available on how best to prevent and/or treat osteoporosis and/or manage osteoporotic fractures in SCI. The goal of this paper was to obtain feedback from experienced PTs/OTs to better understand their insights and recommendations on best practices to improve the fracture treatment process for Veterans with SCI.
Methods
Focus groups and semi-structured interviews were conducted with a purposive sample of PTs and OTs from VA SCI Centers in February–March 2020. Letters describing the study were emailed to the VA SCI centers directors asking that they inform PTs and OTs about the study and provide release time to participate. Information letters were also emailed to SCI therapists with experience in rehabilitation of LE fractures inviting them to participate in the study. The letter described the study purpose, topics to be discussed, that participation was voluntary, and responses were confidential. Reminders were sent via email, telephone and VA’s internal instant messaging service.
Eligibility to participate in the study included having treated at least one surgically managed acute LE fracture in the past 3 years and/or 2 conservatively (medically) managed acute LE fractures in the past year. Interviews and focus groups were conducted by telephone. Interview audio-recordings and notes were uploaded to a secure server for coding.
Prior to participating in the interviews, individuals completed a short background survey asking whether they worked at a VA SCI center or a spoke site, years working with SCI patients, number of patients with LE fractures and LE fractures surgically managed by them or at their site per year, and factors affecting their therapy management plan. Verbal consent was obtained prior to each interview using a standardized script.
The interview guide was developed by research and clinical team members with expertise in health services research and qualitative analysis (MLG, FW) and bone health (LC). Clinical collaborators also included experts in SCI medicine (KR) and PT (TC). The interview included semi-structured questions focusing on common experiences of PTs/OT in managing LE fracture patients.
The initial interview guide was pilot-tested and refined using feedback from two SCI physicians and a PT at the VA SCI center with the highest LE fracture incidence. The final version of the interview guide included questions about medical vs. surgical management of LE fractures, information typically received from orthopaedic surgeons about patients with LE fractures, and how fracture location, SCI- specific and co-morbid medical conditions affected rehabilitation decisions. Interviews also addressed interdisciplinary team member involved in fracture rehabilitation and whether formal recommendations, guidelines or protocols for LE fracture rehabilitation would be beneficial.
We conducted a total of four focus groups (with varying attendance, n = 6, 3, 2, and 2) and two 1:1 interviews. For logistical reasons, interviews included PTs and OTs and were scheduled around their clinical responsibilities. Detailed notes were collected during phone interviews, and audio-recordings were consulted as needed. Coding of responses was completed using a data-driven thematic and deductive approach, in large part dictated by the semi-structured interview guide that addressed the entire treatment process.19–21 The coding team included an experienced qualitative researcher (MG), an SCI physician (KR) and a physical therapist (TC). An initial coding scheme was developed based on the interview topics and further refined during coding of the first 2 interviews in Excel software. The remaining focus groups and interviews were reviewed by each coder independently to identify prominent themes/quotes. Coders subsequently met as a group to review all interview responses.
Participant responses about specific aspects of the treatment process were generally consistent, with the coding activities focused on selecting the most representative response(s) for each question.
Discrepancies between coders were discussed until 100% agreement was reached.22,23 The study was approved by the Institutional Review Board of the Edward Hines Jr. VA Hospital.
Results
A total of 15 therapists, including 10 PTs (one kinesiotherapist, KT) and five OTs from ten (of 25) VA SCI centers, participated in the study (see Table 1). All therapists had experience in rehabilitating LE fractures in Veterans with SCI/D at VA SCI centers. Participants were female (80%). PTs described working in SCI/D for 13.3 vs. 9.7 years for OTs. All participants described providing rehabilitation for LE fractures (PT = 9.35 vs. OT = 9.5 annually), a subset of which received surgical management (annual mean: PT = 2.8 vs. OT = 4.8).
Table 1.
Participant demographic and background characteristics.
| PhysicalTherapists(N = 10)a | OccupationalTherapists(N = 5) | All(N = 15) | |
|---|---|---|---|
| # of years working with SCI/Dpatients | |||
| M (SD) | 13.20 (9.2) | 9.7 (8.3) | 12.03 (8.7) |
| Range | 3–30 | 1.5–20 | 1.5–30 |
| # currently working at an SCI/D Center | |||
| n (%) | 10 (100.0%) | 5 (100.0%) | 15 (100.0%) |
| # of PTs who work with SCI/Dpatients with LE fractures at participant’s siteb | |||
| M (SD) | 6.3 (2.5) | 4.5 (1.7) | 5.79 (2.4) |
| Range | 4–12 | 3–7 | 3–12 |
| Approximate # of patients with LE fracture participant manages per year | |||
| M (SD) | 9.35 (9.5) | 9.50 (5.0) | 9.4 (8.1) |
| Range | 1–24 | 1.5–15 | 1–24 |
| Approximate # of surgicallymanaged LE fractures at participant’s site per yearc | |||
| M (SD) | 2.8 (2.2) | 4.8 (3.3) | 3.5 (2.7) |
| Range | 1–7.5 | 1.5–8 | 1–8 |
| When participants usually see a patient with an LE fracture n (%): | |||
| • Before fracture treatment | 7 (70.0%) | 4 (80.0%) | 11 (73.3%) |
| • During fracture treatment | 6 (60.0%) | 4 (80.0%) | 10 (67.7%) |
| • After fracture treatment | 7 (70.0%) | 4 (80.0%) | 11 (73.3%) |
| Characteristics by which the physical therapist management plan differs, n (%): | |||
| • Surgical vs. medical treatment of LE fracture | 9 (90.0%) | 5 (100.0%) | 14 (93.3%) |
| • Duration of patient injury | 9 (90.0%) | 2 (40.0%) | 11 (73.3%) |
| • Level of patient injury | 8 (80.0%) | 5 (100.0%) | 13 (86.7%) |
| • Caregiver support in the home | 9 (90.0%) | 5 (100.0%) | 14 (93.3%) |
| Gender, n (%): | |||
| Male | 2 (20.0%) | 1 (20.0%) | 3 (20.0%) |
| Female | 8 (80.0%) | 4 (80.0%) | 12 (80.0%) |
Includes one Kinesiotherapist (“Kinesiotherapist” was not an option in the background questionnaire).
Missing: n = 1.
Missing: n = 2.
Medical vs. surgical management of LE fractures
Participants were asked to describe their perceptions of the proportion of patients with SCI/D whose LE fractures were medically (vs. surgically) managed:
[The] vast majority [of our patients with LE fractures] are medically managed. We haven’t had a lot of LE fractures, [maybe] 8 in the past 10 years? (3/11, D12)
The surgeon is [typically] driving [the treatment decision] based on the [patient's overall anticipated] functional recovery. (3/11, F12)
If [the patient was] ambulatory before [their] fracture, [we] may push more for surgery. … Unless it’s going to greatly change [the patient’s] functional status, surgeons won’t operate. (3/9, line 77–80)
Information exchange with orthopaedic surgeons
Participants were asked to describe the kinds of information they routinely receive from the orthopaedic surgeons regarding fracture patients:
The surgical team will [typically] give us [information] about weight-bearing, transfer, equipment … The SCI [physicians provide] level of injury, etiology – anything that might limit … [their return to prior function]. (3/9, lines 130–132)
Several therapists indicated that patients might benefit from an interdisciplinary consultation to ensure comprehensive rehabilitation:
[I] wish I could be a part of [the early mobilization] decision more often, to bring [the therapy perspective] back to orthopaedics, [that] even though [the patient is] not ambulatory – we need to be on the same page with orthopaedics. (2/26, D43)
It would be amazing if we could be in the room … if the orthopedist, SCI [physician] and therapist can come together to determine the plan of care. (2/26, F28)
Another participant indicated that patients may benefit from being involved in the treatment decision:
[It’s so] important to have … conversations between the patient and the surgeons and SCI physicians because [LE fractures] take so much longer to heal than for an able-bodied individual, [and] the impact is that much longer. (2/26, G28)
Need for additional information from surgical team
Therapists often described needing additional information regarding how best to rehabilitate the fracture.
The [information provided by orthopaedics in the] initial consult is [often] minimal [with respect to] activity [and] range of motion restrictions … we [almost] never get [information] about the types of transfer techniques that would be allowed. (3/11, E25)
Our SCI providers will go back to [the surgeons and] ask “can we flex the knee 90 degrees?” We [might also] ask for orders to … [get] them [up] in the chair. (2/26, D25)
Participants described orthopaedic surgeons as having knowledge gaps due to limited experience with LE fractures in SCI/D:
Sometimes ortho gives precautions that are not feasible in SCI, so we’ll go back to them for Plan B … . I don’t think [the orthopaedic surgeon] had any idea of what the [patient’s] transfer process [entails], what the modifications [to enable] driving would be … [SCI patients often] can’t get close enough to the hand controls if their knee is extended– it is not as simple as unlocking the knee. (3/11, E24)
If they’re in a brace, if you try to send them home, [sometimes] they can’t [fit their wheelchair] down the hallway. (3/10, F40)
This lack of experience with SCI/D can have significant consequences:
[Some orthopaedic surgeons], based on how long they’ve been practicing or how many surgeries they’ve done, they might stick with their guns and say 6–8 weeks of bedrest [even if it negatively affects patient function]. (3/11, E32)
Therapists participation in the treatment decision
Participants described a desire for earlier involvement and their advocacy role in assisting patient return to their previous level of function:
Therapists can also have a big impact on selection of bracing initially … We usually change the brace ortho chose because they’re not cognitive of SCI issues (skin, muscle issues). Off-the-shelf braces for [the general population] don’t fit SCI well [and] can cause more secondary complications. (2/26, I–28)
In rehabilitating fractures in persons with SCI/D, surgeons may lack knowledge or expertise in promote healing and safe transfers:
It’s up to [the] therapists to advocate for [ROM] and returning [Veterans] to their wheelchairs, [to] have [their] leg returned to regular position rather than sticking straight out. [This can be] … daunting for patients because they have to stay in [the] hospital, [they] can’t drive or get in a car or return home due to transfer restrictions. (2/26, H25)
Facilitating safe transfers after LE fracture
Completing safe transfers in SCI/D can require extensive use of a person’s legs:
Ortho also often doesn’t seem to understand that [while transferring], people [with SCI routinely] shift [their] weight from one leg to another … they can [inadvertently] twist [their] fractured leg, which isn’t what we want. (3/10, D 25)
PT considerations during rehabilitation
Monitoring for secondary complications is a routine part of post-fracture rehabilitation.
Participants reported routinely using a variety of rehabilitation modalities and monitoring patients for various post-fracture complications. All participants also described doing routine assessment for pain and autonomic dysreflexia and concurrent management with physiatry/SCI physicians.
Early mobilization
Early mobilization is an important aspect of post-fracture rehabilitation that includes stretching and exercises to preserve patient joint range-of-motion and prevent contracture, proper posture and positioning in wheelchairs or in bed, orthotics and other regimens (cryotherapy, nerve blocks and chemodenervation) to minimize muscle spasms:
[Early mobilization does not depend] on [fracture] location – it just takes longer for SCI to … heal. There's often an extended period … before [SCI patients] can do [ROM and the] nonunion rate [is] high. (3/10, E 43)
Spasticity
Many individuals with SCI/D also experience spasticity, which can lead to muscle stiffening or contractions:
In terms of … [severe spasticity for] tib/fib [fractures], that would sometimes cause them to break ROM] precautions, … so we would add [an] extra brace [or] meds to [prevent that]. (3/11, D 36)
Seating assessment
Individuals with SCI/D commonly experience fractures due to accidents (e.g. falling or colliding with objects). Seating assessments can address changes in alignment following fracture regardless of anatomic location. Pressure mapping may also be indicated to guide cushion selection:
Everyone [with an LE fracture] has a seating assessment, [not necessarily] pressure mapping. (2/26, H34)
We [sometimes] use pressure mapping for education, if the patient is not understanding our concern regarding the fracture. (2/26, D39)
[We might] have [provide] a completely different wheelchair. (3/10, E 39)
Patient characteristics affecting post-fracture care
Participants acknowledged that many patient characteristics can affect post-fracture care include age, medical history, comorbidities and wounds:
The more comorbidities patients have, the less likely … [their fracture is to be] surgically managed. (2/26, G40)
[We work closely together] to manage [co-morbid] symptoms – extra precautions with the splinting and skin care … seating [adjustments], … reviewing their [transfer] techniques. (3/9, lines 87–90)
Respondents indicated that SCI factors (e.g. duration of injury, level of injury, completeness of injury, ambulatory status) have the potential to affect post-fracture rehabilitation:
[SCI] duration [matters]. The longer they’ve been sitting, the more osteoporotic they are – just trying to stabilize that, … getting them back to their activities [is more challenging]. (2/26, F57)
[Orthopaedics typically isn't] considering … use … [of a] standing wheelchair [or a] standing frame … We may advocate for surgical fixation for patients who are able to weight bear. (3/13, D62)
Benefits of guidelines for management of lower extremity fractures
Respondents pointed out that some surgeons may not have treated many LE fractures in individuals with SCI because of their low incidence. Participants agreed that a guideline would be beneficial:
[A guideline can educate] orthopaedic surgeons … so they know where [therapists] come from, [it can be] beneficial for the whole team. (2/26, D64)
Recommendations and guidelines would be helpful for [providers in] community and non-SCI- Center [settings]. We will see [fracture] patients with seating [problems who] did not have any bracing yet, or … are not out of bed because no one ordered them a leg rest [for their wheelchair]. (2/26, G59)
Involvement of other disciplines in post-fracture rehabilitation
Respondents stated their belief that an interdisciplinary care team of providers (e.g. surgeons, SCI clinicians, PTs, nurses, social workers) should be involved in post-fracture rehabilitation from the beginning. In particular, respondents identified the critical role of social work:
[At our site, the] entire team … [is] … working on discharge planning from Day 1. [For outpatients with delayed] healing, [we] might look into home health aides or a visiting nursing to assist with making sure they make appointments [and] follow up with orthopaedics. (3/11, D66)
[Other disciplines get involved] if [the patient] can’t go back … home based on [their] current level of function or style of home, or if they need a caregiver but [are ineligible for a] service- connected [disability pension]. (3/11, E 66)
[If the patient’s] level of assistance changes, they may now need help with bowel and bladder care. Because of [the fracture] position, [they often] can’t fit into hallways … [We’re] looking for how to manage that. (3/11, D 67)
Discussion
The World Health Organization (WHO) released the “International Classification of Functioning, Disability, and Health” (ICF) framework in 2001 to address necessary components of health and well- being for disabled individuals.24 ICF components include: (1) Body Functions and Structures; and (2) Activities and Participation and can be applied to any health condition to unify/standardize patient- oriented therapies. Applying the ICF framework to complex medical conditions such as LE fractures in individuals with SCI requires a comprehensive therapeutic approach. Focusing on simply healing an individual’s fracture is wholly inadequate. To ensure that individuals fully recover and can return to baseline post-fracture an interdisciplinary care team (e.g. surgeons, SCI clinicians, PTs, OTs, nurses, social workers) must consider all aspects of the ICF framework at the very beginning of the fracture management. To fully address the health care needs of an individual with SCI who sustains a LE fracture the team must consider their lifestyle, medication use, mental status, motivation and return to his/her environment (e.g. living condition, wheelchair, work, family relations). Understanding the variability in individual functioning during everyday situations and how each component of the ICF framework affects the others, as well as designing interventions that remove barriers preventing individuals from returning to their previous level of functioning is a vital part of rehabilitation planning.25
Our findings indicate that PTs and OTs feel strongly that they should be involved in post-fracture rehabilitation as soon as possible. Therapists work closely with prosthetics professionals to recommend customized braces and devices to minimize adverse events (e.g. skin breakdown). Therapists can assess patient equipment needs, need for skills training and/or caregiver assistance resulting from post- fracture mobility changes. A wheelchair seating specialist should be involved in post-fracture care for seating assessments in wheelchair users to address changes in alignment, deformities, limb length discrepancies and/or seating posture during and following fracture management.
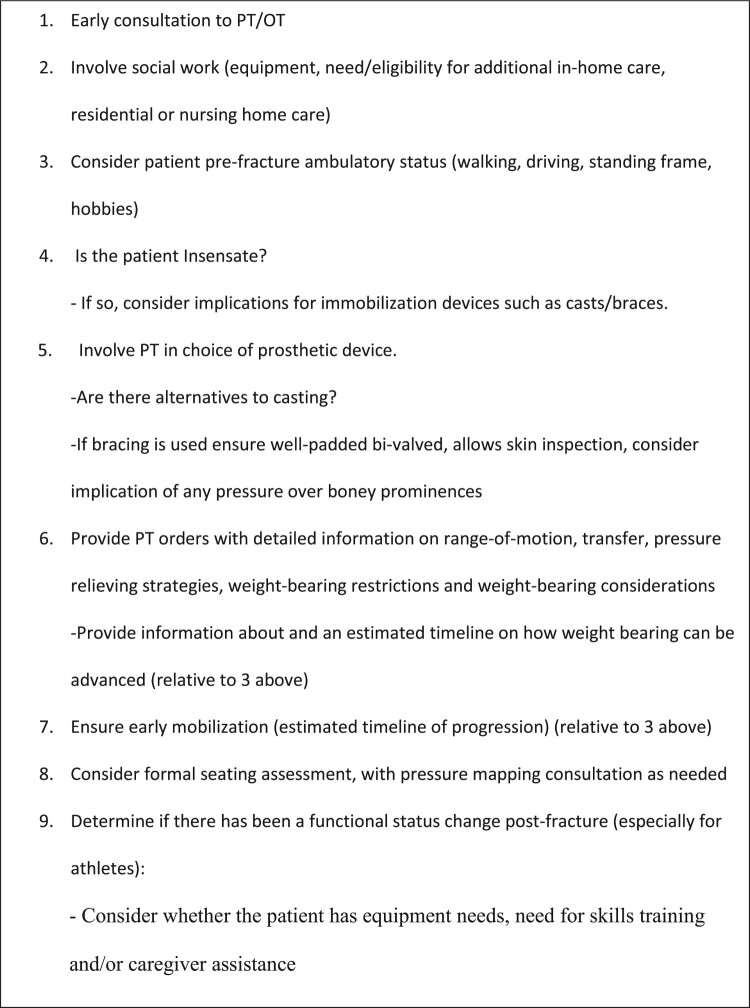
To ensure that post-fracture rehabilitation be individualized to accomplish patient goals, as shown in Fig. 1, orthopaedic surgeons should also consider involving PTs and OTs and social workers as early in the fracture management process as is feasible to address patient need for: new and/or modified equipment during or after fracture treatment and to ensure that the discharge plan includes patient skills training and/or caregiver assistance due to change in mobility from fracture. We recommend that orthopaedic surgeons also provide PTs and OTs with detailed instructions on ROM and weight-bearing restrictions including transfer restrictions immediately post-fracture. These instructions should be updated on a regular basis to let PTs/OTs know when rehabilitation can be progressed.
Figure 1.
Therapy considerations for orthopedic surgeons treating patients with SCI/D and LE fractures.
Although caregivers are extremely important stakeholders in the post-fracture management process, our impression was that PTs/OTs dealt primarily with patients. Therefore, we included no specific questions about the impact of LE fractures on caregivers of persons with SCI and did not code for it. It is therefore noteworthy that a number of participants brought this topic up independently.
Limitations
There were a number of limitations to this study. The low incidence of LE fractures in this population, along with our eligibility criteria requiring participants to have treated at least one surgically managed acute LE fracture in the past 3 years and/or 2 conservatively (medically) managed acute LE fractures in the past year necessarily limited our sample. Although small, our sample represents clinical practices at 40% of VA SCI centers.
The small number of OTs in our sample precluded doing any formal comparisons, however, anecdotally, no differences between PTs/OTs were observed.
Our focus on PT/OT post-fracture management also precluded the direct participation of orthopedic surgeons. We attempted to mitigate this concern by including an orthopedic surgeon (CS) as a co-author.
Future studies could provide a more comprehensive picture of the fracture treatment process by including input from patients with SCI, informal caregivers and additional orthopedic surgeons.
Conclusion
PTs and OTs play a critical role in helping persons with SCI/D and LE fractures to return to previous function and levels of participation. There is a well-documented relationship between surgical volume and treatment outcomes.26–29 Given its low incidence, it is likely that PTs/OTs in our study have seen a higher volume of LE fractures in SCI/D than the average orthopedic surgeon. Early involvement of PTs and OTs can help patients to avoid adverse outcomes. They bring a wealth of knowledge about patient function and ambulatory status, transfer strategies, mobility equipment, spasticity, lifestyle, home and caregiver support that may be relevant in determining the best plan.
Involving them early and often in the rehabilitation process, along with the orthopedic surgeon, physiatrists and other SCI clinicians can address the multiple and often unique issues that occur in managing fractures in this population.
Abbreviations
- BMD
bone mineral density
- ICF
International Classification of Functioning, Disability, and Health framework
- LE
lower extremity
- PTs
physical therapists
- OTs
occupational therapists
- ROM
range-of-motion
- SCI/D
spinal cord injury or disorder
- VA
US Department of Veterans Affairs
- WHO
World Health Organization
Acknowledgements
This study was supported by the US Department of Defense (W81XWH-16-1-0413) and US Department of Veterans Affairs, Office of Research and Development, Health Services Research and Development Service (IIR 15-294). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the United States government. This paper would not have been possible without the exceptional support of the VA physical and occupational therapists who participating in the interviews described in this manuscript.
Funding Statement
This work was supported by U.S. Department of Defense [grant number W81XWH-16-1-0413]; U.S. Department of Veterans Affairs [grant number IIR 15-294].
Disclaimer statements
Contributors None.
Conflicts of interest Authors have no conflict of interests to declare.
References
- 1.National SCI Statistical Center . [cited 2020 June 21]. Available from https://www.sci-info-pages.com/wp-content/media/NSCISC-2019-Spinal-Cord-Injury-Facts-and-Figures-at-a-Glance.pdf.
- 2.VA's Spinal Cord Injuries and Disorders System of Care [cited 2020 June 21]. Available from https://www.sci.va.gov/VAs_SCID_System_of_Care.asp.
- 3.Akhigbe T, Chin AS, Svircev JN, Hoenig H, Burns SP, Weaver FM, et al. A retrospective review of lower extremity fracture care in patients with spinal cord injury. J Spinal Cord Med. 2015, Jan;38(1):2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bethel M, Bailey L, Weaver F, Harmon RL, Priebe MM, Le B, et al. A historical study of appendicular fractures in veterans with traumatic chronic spinal cord injury: 2002–2007. J Spinal Cord Med. 2016;39(6):686–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carbone LD, Chin AS, Burns SP, Svircev JN, Hoenig H, Heggeness M, et al. Mortality after lower extremity fractures in men with spinal cord injury. J Bone Miner Res. 2014;29(2):432–9. [DOI] [PubMed] [Google Scholar]
- 6.Grassner L, Klein B, Maier D, Buhren V, Vogel M.. Lower extremity fractures in patients with spinal cord injury characteristics, outcome and risk factors for non-unions. J Spinal Cord Med. 2018;41(6):676–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biering-Sorensen F, Bohr HH, Schaadt OP.. Longitudinal study of bone mineral content in the lumbar spine, the forearm and the lower extremities after spinal cord injury. Eur J Clin Invest. 1990;20:330–5. [DOI] [PubMed] [Google Scholar]
- 8.Eser P, Frotzler A, Zehnder Y, Wick L, Knecht H, Denoth J, et al. Relationship between the duration of paralysis and bone structure: a pQCT study of spinal cord injured individuals. Bone 2004;34:869–80. [DOI] [PubMed] [Google Scholar]
- 9.Zehnder Y, Luthi M, Michel D, Knecht H, Perrelet R, Neto I, et al. Long-term changes in bone metabolism, bone mineral density, quantitative ultrasound parameters, and fracture incidence after spinal cord injury: a cross- sectional observational study in 100 paraplegic men. Osteoporos Int. 2004;15:180–9. [DOI] [PubMed] [Google Scholar]
- 10.Vestergaard P, Krogh K, Rejnmark L, Mosekilde L.. Fracture rates and risk factors for fractures in patients with spinal cord injury. Spinal Cord. 1998;36:790–6. [DOI] [PubMed] [Google Scholar]
- 11.Eser P, Frotzler A, Zehnder Y, Denoth J.. Fracture threshold in the femur and tibia of people with spinal cord injury as determined by peripheral quantitative computed tomography. Arch Phys Med Rehabil. 2005;86:498–504. [DOI] [PubMed] [Google Scholar]
- 12.Frotzler A, Cheikh-Sarraf B, Pourtehrani M, Krebs J, Lippuner K.. Long-bone fractures in persons with spinal cord injury. Spinal Cord. 2015;53(9):701–4. [DOI] [PubMed] [Google Scholar]
- 13.Gifre L, Vidal J, Carrasco J, Portell E, Puig J, Monegal A, et al. Incidence of skeletal fractures after traumatic spinal cord injury: a 10-year follow-up study. Clin Rehabil. 2014;28(4):361–9. [DOI] [PubMed] [Google Scholar]
- 14.Anderson SD, Anderson DG, Vaccaro AR.. Skeletal fracture demographics in spinal cord-injured patients. Arch Orthop Trauma Surg. 2004;124(3):193–6. [DOI] [PubMed] [Google Scholar]
- 15.Perkins C, Buck JS, Karunakar MA.. Outcomes in the treatment of femur fractures in patients with pre-existing spinal cord injury. Bull Hosp Jt Dis. 2013, Sep;77(3):211–15. [PubMed] [Google Scholar]
- 16.Schulte LM, Scully RD, Kappa JE.. Management of lower extremity long-bone fractures in spinal cord injury patients. J Am Acad Orthop Surg. 2017, Sept;25(9):e204–e13. [DOI] [PubMed] [Google Scholar]
- 17.Wang L, Yao X, Xiao L, Tang X, Ding H, Zhang H, et al. The effects of spinal cord injury on bone healing in patients with femoral fractures. J Spinal Cord Med. 2014;37(4):414–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zleik N, Weaver F, Harmon RL, Le B, Radhakrishnan R, Jirau-Rosaly WD, et al. Prevention and management of osteoporosis and osteoporotic fractures in persons with a spinal cord injury or disorder: a systematic scoping review. J Spinal Cord Med. 2019;42(6):735–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beebe J. Rapid qualitative inquiry: a field guide to team-based assessment. 2nd ed. Lanham: Rowman & Littlefield; 2014. [Google Scholar]
- 20.Gale RC, Wu J, Erhardt T, Bounthavong M, Reardon CM, Damschroder LJ, et al. Comparison of rapid vs in-depth qualitative analytic methods from a process evaluation of academic detailing in the VHA. Implementation Sci. 2019;14(11). PMCID: PMC6359833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor B, Henshall C, Kenyon S, Litchfield I, Greenfield S. . Can rapid approaches to qualitative analysis deliver timely, valid findings to clinical leaders? BMJ Open. 2018;8(10):e019993. PMCID: PMC6194404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gisev N, Bell JS, Chen T.. Interrater agreement and interrater reliability: key concepts, approaches, and applications. Res Social Adm Pharm. 2013;9(3):330–8. [DOI] [PubMed] [Google Scholar]
- 23.Holdford D. Content analysis methods for conducting research in social and administrative pharmacy. Res Social Adm Pharm. 2008;4(2):173–81. [DOI] [PubMed] [Google Scholar]
- 24.International Classification of Functioning, Disability, and Health (ICF). ICF full version. Geneva, Switzerland: World Health Organization; 2001. [cited 2020 June 21]. Available from https://apps.who.int/iris/bitstream/handle/10665/42407/9241545429.pdf.
- 25.Madden RH, Bundy A.. The ICF has made a difference to functioning and disability measurement and statistics. Disabil Rehabil. 2019;41(12):1450–62. [DOI] [PubMed] [Google Scholar]
- 26.Critchley RJ, Baker PN, Deehan DJ.. Does surgical volume affect outcome after primary and revision knee arthroplasty? A systematic review of the literature. Knee 2012 Oct;19(5):513–18. [DOI] [PubMed] [Google Scholar]
- 27.Yoo S, Jang EJ, Jo J, Jo JG, Nam S, Kim H, et al. The association between hospital case volume and in- hospital and one-year mortality after hip fracture surgery. Bone Joint J 2020 Oct;102-B(10):1384–91. [DOI] [PubMed] [Google Scholar]
- 28.Koltsov JCB, Marx RG, Bachner E, McLawhorn AS, Lyman S.. Risk-based hospital and surgeon-volume categories for total hip arthroplasty. J Bone Jt Surg. 2018;100:1203–8. [DOI] [PubMed] [Google Scholar]
- 29.Shervin N, Rubash HE, Katz JN.. Orthopaedic procedure volume and patient outcomes: A systematic literature review. Clin Orthop Relat Res. 2007;457:35–41. [DOI] [PubMed] [Google Scholar]