Abstract
Background
Understanding COVID-19 epidemiology is crucial to clinical care and to clinical trial design and interpretation.
Objective
To describe characteristics, treatment, and outcomes among patients hospitalized with COVID-19 early in the pandemic.
Methods
A retrospective cohort study of consecutive adult patients with laboratory-confirmed, symptomatic SARS-CoV-2 infection admitted to 57 US hospitals from March 1 to April 1, 2020.
Results
Of 1480 inpatients with COVID-19, median (IQR) age was 62.0 (49.4–72.9) years, 649 (43.9%) were female, and 822 of 1338 (61.4%) were non-White or Hispanic/Latino. Intensive care unit admission occurred in 575 patients (38.9%), mostly within 4 days of hospital presentation. Respiratory failure affected 583 patients (39.4%), including 284 (19.2%) within 24 hours of hospital presentation and 413 (27.9%) who received invasive mechanical ventilation. Median (IQR) hospital stay was 8 (5–15) days overall and 15 (9–24) days among intensive care unit patients. Hospital mortality was 17.7% (n = 262). Risk factors for hospital death identified by penalized multivariable regression included older age; male sex; comorbidity burden; symptoms-to-admission interval; hypotension; hypoxemia; and higher white blood cell count, creatinine level, respiratory rate, and heart rate. Of 1218 survivors, 221 (18.1%) required new respiratory support at discharge and 259 of 1153 (22.5%) admitted from home required new health care services.
Conclusions
In a geographically diverse early-pandemic COVID-19 cohort with complete hospital folllow-up, hospital mortality was associated with older age, comorbidity burden, and male sex. Intensive care unit admissions occurred early and were associated with protracted hospital stays. Survivors often required new health care services or respiratory support at discharge.
Initial investigations have yielded a consensus understanding of the most common phenotypes and transmission dynamics of COVID-19 as well as preliminary identification of factors associated with adverse outcomes.1–6 Many studies, however, have been constrained by short observation periods and scarce data on hospital trajectory. Additionally, few well-designed analyses of risk factors for adverse outcomes have been conducted in diverse, multicenter patient populations.
A more granular and geographically diverse nationwide analysis of the epidemiology, clinical trajectory, and heterogeneity of patients with COVID-19 is necessary to aid clinical decision-making, help clinicians situate specific cases relative to expected variation, inform clinical trial design and interpretation, and enhance health system planning.
To address these issues, we leveraged a nationwide acute care trials network to conduct an observational study of adult patients with symptomatic SARS-CoV-2 infection admitted to 57 geographically diverse US hospitals. We used high-fidelity clinical data collected during the entire hospital course (from admission to hospital discharge) to identify risk factors for in-hospital mortality and for early and late respiratory failure. We also describe patients’ illness trajectory, patterns of organ failure, therapies, and the distribution of several clinical outcomes meaningful to patients, clinicians, health system planners, and researchers.
Methods
Design and Setting
We conducted a retrospective, multicenter cohort study of adult patients admitted to US hospitals with laboratory-confirmed SARS-CoV-2 infection and symptomatic COVID-19. Participating hospitals were members of the National Heart, Lung, and Blood Institute Prevention and Early Treatment of Acute Lung Injury (PETAL) Network and included 57 geographically diverse US hospitals organized within 12 clinical centers (Figure 1). The PETAL Network central institutional review board at Vanderbilt University and the institutional review boards at each participating hospital approved the study or determined that the study was exempt from review.
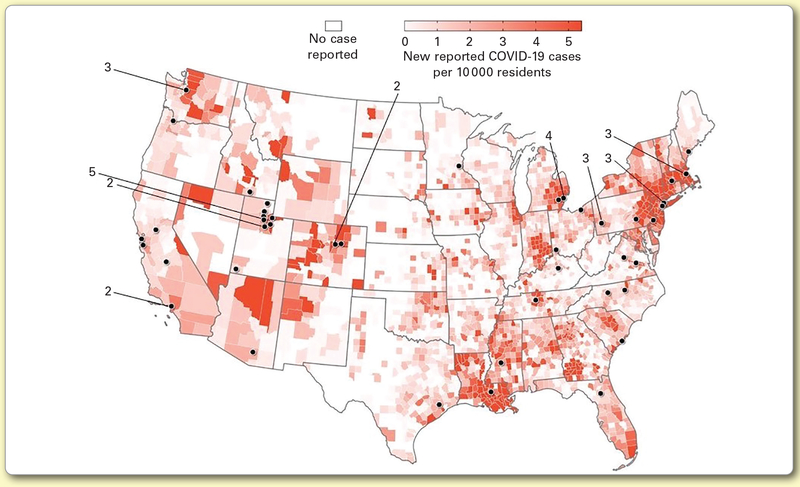
Figure 1.
Map of contributing hospitals with associated county-level COVID-19 incidence during cohort eligibility. Choropleth map illustrates spatial variation in county-level COVID-19 incidence rate (cases per 10 000 residents) during the third week of March 2020 (see Supplement 1). Dots represent contributing hospitals. For closely adjacent hospitals, a single dot indicates the location of multiple hospitals and is labeled with the number of contributing sites represented.
Participants
Patients aged 18 years or older admitted to a study hospital from March 1 to April 1, 2020, were eligible for inclusion if they had a positive polymerase chain reaction test result for SARS-CoV-2 during their admission or within the preceding 14 days and infection (including fever, cough, dyspnea, hypoxemia, or bilateral airspace opacities). We excluded prisoners and patients with prior hospital admission for COVID-19. Each clinical center contributed data from up to 125 consecutive patients drawn from that center’s contributing hospitals. Because some clinical centers admitted fewer than 125 eligible patients during the study period, clinical centers with excess eligible patients contributed additional participants toward a total study inclusion target of 1500 patients.
Data Collection
Trained personnel obtained data on demographic and clinical characteristics, interventions, and outcomes by manual review of medical records according to a standardized protocol. Abstracted data were entered into a structured data capture interface with integrated real-time data validation.7 Manual medical record review was supplemented at some sites by electronic data abstraction. Patients were followed until hospital discharge. Additional assessments were performed on hospital days 1, 4, 8, 15, 21, and 28 and (if applicable) on day 1 in the intensive care unit (ICU). Each site was also asked to provide counts and basic demographics of all patients hospitalized with COVID-19 during the study window.
To quantify illness severity, we adapted an 8-point ordinal outcomes scale recommended by the World Health Organization (Supplemental Table 1, available online only at ajcconline.org).8 Scale values used the worst available value for the calendar day or, if data were missing, from an adjacent day. Sequential Organ Failure Assessment score calculation did not incorporate urine output but otherwise used standard methods, including assigning component scores of 0 when data were missing.9 Respiratory support was defined by treatment with supplemental oxygen or positive pressure ventilation. When Pao2 data were unavailable, values were estimated from peripheral oxygen saturation (Spo2) values using a validated nonlinear formula.10 For patients receiving oxygen by nasal cannula or face mask, the fraction of inspired oxygen (Fio2) was estimated using the formula Fio2 = 0.21 + (0.03 × [oxygen flow rate in liters per minute]). Comorbidities, symptoms and their duration, and complications were obtained from clinical documentation.
Outcomes
The primary outcome was hospital mortality. Prespecified secondary outcomes included respiratory failure (defined as treatment with oxygen at ≥11 L/min delivered by face mask, high-flow nasal cannula, noninvasive positive pressure ventilation, or invasive mechanical ventilation) occurring early (≤24 hours) or late (>24 hours) after hospital presentation. Other secondary outcomes included 7-, 14-, and 28-day hospital mortality; COVID-19 ordinal outcome scale values on hospital days 4, 8, 15, and 28; length of hospital stay; respiratory, cardiovascular, and renal support therapies; and survivors’ discharge health status.
Statistical Analysis
Continuous data are reported as medians and interquartile ranges (IQRs). Categorical data are reported as numbers and percentages. For descriptive analyses, we did not perform statistical hypothesis testing.
We employed L1 (lasso)–penalized logistic mixed-effects regression11,12 to identify risk factors for mortality, early-onset respiratory failure, and late-onset respiratory failure from outcome-specific sets of candidate risk factors identified a priori by a team of experienced epidemiologists and clinical researchers on the basis of previously reported association, plausibility, clinical utility, and data availability. To manage missingness among candidate risk factors, we performed penalized regression after multiple imputation of missing data using chained equations.13 Adjusted effect sizes for selected risk factors were estimated in the multiply imputed data using multivariable mixed-effects logistic regression and combined coefficients using Rubin’s rules.13–16 To account for site-level clustering of patient characteristics, care practices, and outcomes as well as between-site variation in resource strain,17 we employed a random effect for study site during both penalized regression18 and multivariable logistic regression model refitting for effect size estimation. Additional details are available in Supplement 1 (available online only).
We assessed our findings’ robustness in prespecified sensitivity analyses by reestimating effect sizes after (1) reclassifying patients discharged with hospice services as having the primary outcome (in-hospital mortality); (2) excluding patients who died without respiratory failure from the secondary analysis of late respiratory failure; and (3) excluding support with oxygen by face mask from the definition of respiratory failure. As an additional measure of variable importance, we also report the percentage of models in which each candidate variable was ultimately selected during cross-validation.19 Analyses were performed with R, version 4.0.3 (R Foundation for Statistical Computing); Stata, version 16.1 (StataCorp); and SAS, version 9.4 (SAS Institute Inc).
Results
Among the 1480 patients included in our cohort, the median (IQR) age was 62.0 (49.4–72.9)years, 649 patients (43.9%) were female, and 822 of 1338 (61.4%) patients with known race/ethnicity were Hispanic/Latino or non-White (Table 1; Supplemental Table 2, available online only). The demographic profile of included patients was similar to that of the source population of all patients with COVID-19 admitted to study hospitals from March 1 to April 1, 2020 (Supplemental Table 3, available online only). Each of the 57 enrolling hospitals contributed a median (IQR) of 21 (8–41) patients. Most patients had at least 1 comorbidity included in the Charlson Comorbidity Index (n = 843; 57.0%). The median (IQR) preadmission symptom duration was 6 (3–9) days and was longer in survivors than in patients who died in the hospital (median [IQR], 7 [4–9] days vs 4 [2–7] days). The first-available Pao2 to Fio2 ratio was less than 300 in 514 of 1452 patients (35.4%) with available data, and most patients (n = 1203; 81.3%) had a Sequential Organ Failure Assessment score of 2 or greater within 24 hours of hospital arrival (Supplemental Table 4, available online only).
Table 1.
Patient demographic and clinical characteristics within 24 hours of hospital arrivala
| Characteristic | Overall (N = 1480) | Hospital outcome |
|
|---|---|---|---|
| Discharged alive (n = 1218) | Died (n = 262) | ||
| Age, y | 62.0 (49.4–72.9) | 59.3 (46.9–70.2) | 72.3 (62.8–81.2) |
|
| |||
| Female sex | 649 (43.9) | 560 (46.0) | 89 (34.0) |
|
| |||
| Race/ethnicity | |||
| Hispanic or Latino | 272 (18.4) | 247 (20.3) | 25 (9.5) |
| Non-Hispanic Black | 460 (31.1) | 367 (30.1) | 93 (35.5) |
| Non-Hispanic White | 539 (36.4) | 433 (35.6) | 106 (40.5) |
| Other/unknown | 209 (14.1) | 171 (14.0) | 38 (14.5) |
|
| |||
| Body mass indexb (n = 1382) | 30.2 (26.0–35.6) | 30.4 (26.2–35.9) | 29.2 (25.0–34.9) |
|
| |||
| Charlson Comorbidity Index | 3 (1–5) | 2 (1–4) | 5 (3–7) |
|
| |||
| Comorbidities | |||
| Chronic pulmonary disease | 351 (23.7) | 279 (22.9) | 72 (275) |
| Cardiovascular disease | 238 (16.1) | 162 (13.3) | 76 (29.0) |
| Chronic renal failure | 154 (10.4) | 111 (9.1) | 43 (16.4) |
| Hypertension | 845 (571) | 653 (53.6) | 192 (73.3) |
| Diabetes | 473 (32.0) | 337 (277) | 136 (51.9) |
|
| |||
| Admitted from care facility | 120/1475 (8.1) | 70/1214 (5.8) | 50/261 (19.2) |
|
| |||
| Home medications | |||
| ACE inhibitor | 266 (18.0) | 200 (16.4) | 66 (25.2) |
| Angiotensin receptor blocker | 192 (13.0) | 146 (12.0) | 46 (176) |
| Systemic corticosteroids | 92 (6.2) | 67 (5.5) | 25 (9.5) |
|
| |||
| Symptoms | |||
| Duration, d (n = 1217) | 6 (3–9) | 7 (4–9) | 4 (2–7) |
| Fever or chills | 1288 (870) | 1082 (88.8) | 206 (78.6) |
| Cough | 1253 (84.7) | 1058 (86.9) | 195 (74.4) |
| Dyspnea | 1181 (79.8) | 984 (80.8) | 197 (75.2) |
| Confusion | 148 (10.0) | 78 (6.4) | 70 (26.7) |
| Gastrointestinal symptoms | 626 (42.3) | 540 (44.3) | 86 (32.8) |
|
| |||
| Sequential Organ Failure Assessment score | 3 (2–4) | 2 (2–4) | 5 (3–9) |
|
| |||
| COVID-19 Ordinal Outcome Scale | 4 (3–4) | 4(3–4) | 4 (4–7) |
|
| |||
| Initial vital signs | |||
| Heart rate, beats per minute (n = 1474) | 94 (82–106) | 94 (82–106) | 92 (80–105) |
| Systolic blood pressure, mm Hg (n = 1474) | 131 (117–145) | 131 (118–145) | 132 (114–146) |
| Respiratory rate, breaths per minute (n = 1478) | 20 (18–23) | 20 (18–22) | 20 (18–25) |
| Glasgow Coma Scale score <15 | 189/1462 (12.9) | 103/1204 (8.6) | 86/258 (33.3) |
| Pao2 to Fio2 ratio (n = 1452) | 338 (260–431) | 337 (279–431) | 267 (174–360) |
|
| |||
| Bilateral opacities on initial chest imagingc | 980 (66.2) | 786 (64.5) | 194 (74.1) |
|
| |||
| Initial laboratory results | |||
| White blood cell count, ×1000/μL (n = 1468) | 6.1 (4.7–8.1) | 5.9 (4.6–77) | 70 (5.2–10.3) |
| Lymphocyte count, ×1000/μL (n = 1271) | 0.9 (0.7–1.3) | 1.0 (0.7–1.3) | 0.8 (0.6–1.2) |
| Lactate >2 mmol/L | 177/948 (18.7) | 113/753 (15.0) | 64/195 (32.8) |
| Creatinine, mg/dL (n = 1459) | 1.0 (0.8–1.3) | 1.0 (0.8–1.2) | 1.3 (0.9–2.1) |
| Aspartate aminotransferase, U/L (n = 1198) | 39 (27–59) | 38 (275–57) | 40 (27–68) |
| Ferritin, ng/mL (n = 568) | 548 (266–1117) | 522 (238–1026) | 805 (433–1608) |
| d-dimer, μg/mL (n = 438) | 0.8 (0.5–1.4) | 0.7 (0.5–1.2) | 1.5 (0.8–3.9) |
Abbreviations: ACE, angiotensin-converting enzyme; AST, aspartate aminotransferase; Fio2, fraction of inspired oxygen.
Values are reported as number (percentage) or median (IQR). Where 1 or more patients had missing data, the number of patients with nonmissing data is shown.
Calculated as weight in kilograms divided by height in meters squared.
Bilateral airspace opacities noted in radiologisťs interpretation of patienťs first-available chest radiograph and/or computed tomography scan.
Common pharmacologic treatments included hydroxychloroquine (54.3% of patients), azithromycin (65.4%), other antibiotics (78.6%), and therapeutic anticoagulation (23.6%) (Table 2). Systemic corticosteroid therapy was relatively rare (13.9%). Clinically diagnosed acute respiratory distress syndrome was the most common complication, affecting 483 patients (32.6%), including 200 of the 262 (76.3%) patients who died in the hospital (Supplemental Table 5, available online only). Among patients not receiving dialysis before admission, acute renal failure was also more common in nonsurvivors (148 of 249 patients; 59.4%) than in survivors (173 of 1188 patients; 14.6%). Venous thromboembolism was diagnosed in 46 patients (3.1%).
Table 2.
Clinical management and outcomesa
| Feature | Overall (N = 1480) |
|---|---|
|
| |
| Admitted to intensive care unit | 575 (38.9) |
|
Respiratory support modalities | |
| Nasal cannula or face mask | 1156 (78.1) |
| High-flow nasal cannula | 254 (172) |
| Noninvasive positive pressure ventilation | 129 (8.7) |
| Mechanical ventilation | 413 (279) |
|
| |
| Prone positioning | 162 (10.9) |
|
| |
| Inhaled pulmonary vasodilator | 55 (3.7) |
|
| |
| Extracorporeal membrane oxygenation | 8 (0.5) |
|
| |
| Vasopressors or inotropes | 366 (24.7) |
|
| |
| Renal replacement therapy | 131 (8.9) |
|
Pharmacologic therapy administered | |
| Azithromycin | 968 (65.4) |
| Other antibiotics | 1164 (78.6) |
| Therapeutic anticoagulation | 350 (23.6) |
| Hydroxychloroquine or chloroquine | 804 (54.3) |
| Interleukin 6 receptor antagonist | 106 (72) |
| Enteric or intravenous corticosteroids | 205 (13.9) |
| Remdesivir | 88 (5.9) |
| Lopinavir/ritonavir | 59 (4.0) |
|
Score on COVID-19 Ordinal Outcome Scale | |
| Day 4 | 4 (3–5) |
| Day 8 | 3 (1–6) |
| Day 15 | 1 (1–5) |
| Day 28 | 1 (1–2) |
|
| |
| Respiratory failure during hospitalization | 583 (39.4) |
|
Hospital disposition | |
| Died | 262 (177) |
| Discharged with hospice | 12 (0.8) |
| Discharged to home | 1044 (70.5) |
| Discharged to home with in-home health care | 156/1044 (14.9) |
| Skilled nursing facility | 66 (4.5) |
| Long-term acute care hospital | 22 (1.5) |
| Inpatient rehabilitation facility | 57 (3.9) |
| Transfer to another acute care hospital | 17 (1.1) |
|
| |
| Hospital length of stay, d | 8 (5–15) |
|
| |
| Hospital mortality | |
| 7-day | 66 (4.5) |
| 14-day | 179 (12.1) |
| 28-day | 249 (16.8) |
|
Organ support at discharge among survivors (n = 1218) | |
| New respiratory support (any) | 221 (18.1) |
| New home oxygen | 202 (16.6) |
| Noninvasive ventilation | 6 (0.5) |
| Ventilator | 7 (0.6) |
| Tracheotomy | 14 (1.2) |
| New dialysis | 10 (0.8) |
Values are reported as number (percentage) or median (IQR).
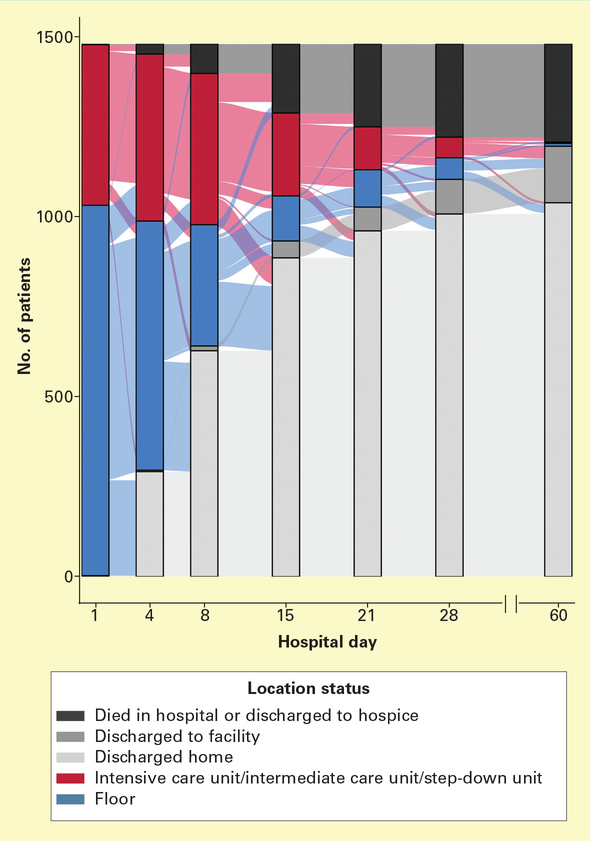
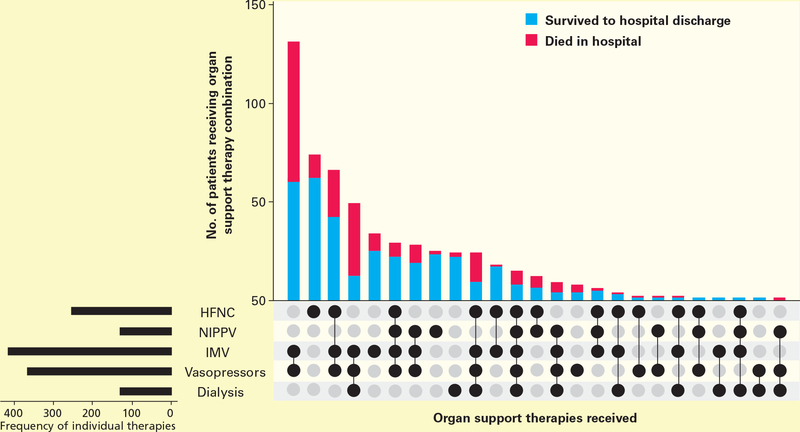
Overall, 575 patients (38.9%) received care in an ICU during their hospitalization. Of these, 369 (64.2%) were admitted to the ICU within 24 hours of hospital arrival (Supplemental Table 6, available online only). Most of the remaining ICU admissions occurred by hospital day 4 (Figure 2). More than four-fifths of patients (n = 1203; 81.3%) required some form of respiratory support during their hospital stay and 583 (39.4%) developed respiratory failure, including 413 (27.9%) who received invasive mechanical ventilation, 129 (8.7%) who received noninvasive positive pressure ventilation, and 254 (17.2%) who were treated with high-flow nasal cannula (Table 2). Respiratory failure occurred in 284 patients (19.2%) within 24 hours of hospital arrival. Among the 567 (38.3%) patients who required advanced organ-support therapies (high-flow nasal cannula, positive pressure ventilation, renal replacement therapy, and/or vasopressors), mechanical ventilation plus vasopressor support was the most common combination (23.1%, Figure 3). The vast majority (85.0%) of patients who received invasive mechanical ventilation were also treated with vasopressors during their hospitalization.
Figure 2.
Hospital level of care from arrival at study hospital through discharge or hospital day 60. Alluvial diagram depicts patients’ transitions between treatment intensity levels during their hospitalization and ends on study hospital discharge. Because patients were not followed up beyond hospital discharge, patients do not transition out of postdischarge status of home or facility.
Figure 3.
Organ support therapy combinations and associated hospital mortality among patients requiring organ support therapy. Includes 567 patients receiving at least 1 advanced organ support therapy.
Abbreviations: HFNC, high-flow nasal cannula; IMV, invasive mechanical ventilation; NIPPV, noninvasive positive pressure ventilation.
Many patients experienced prolonged hospitalization, with median (IQR) hospital stays of 8 (5–15) days (Supplemental Figure 2, available online only). On day 15 of hospitalization, 355 (24.0%) patients remained admitted; 117 (7.9%) patients remained admitted on hospital day 28. Hospitalizations were longer for patients admitted to an ICU than for patients not admitted to an ICU (median [IQR], 15 [9–24] days vs 6 [4–9] days).
Hospital mortality was 17.7% (n = 262, Table 2). Mortality was higher among patients admitted to an ICU (35.5%) than among patients never admitted to an ICU (5.3%). Mortality correlated with the number of organ failures, occurring in 11 of 58 (19.0%) patients who received mechanical ventilation and had isolated respiratory failure, 111 of 254 (43.7%) intubated patients who also required vasopressor support, and 64 of 97 (66.0%) intubated patients who required both vasopressors and renal replacement therapy. Unadjusted hospital mortality was higher in older patients; men; patients with hypertension, diabetes, cancer, or chronic cardiovascular disease; and individuals admitted from a long-term care facility (Table 1; Supplemental Figure 3, available online only).
Penalized regression identified the following risk factors for mortality: older age, shorter reported interval from symptom onset to hospitalization, male sex, comorbidity burden, tachycardia, tachypnea, hypotension, abnormal mental status, hypoxemia, higher first-available creatinine level, and higher first-available white blood cell count (Table 3). Race/ethnicity was among the 4 candidate variables not identified as contributing risk factors for mortality. After multivariable regression, the risk of mortality increased exponentially with age, reaching an adjusted odds ratio of 30.7 (95% CI, 8.8–107.0) in patients 80 years and older compared with patients younger than 40 years. Adjusted odds ratios were similar in the sensitivity analysis reclassifying 12 patients discharged with hospice services as having the mortality outcome.
Table 3.
Risk factors for hospital mortalitya
| Risk factor | Percentage of cross-validation models including variable | Candidate risk factor included in final model? | Odds ratio (95% CI) |
|---|---|---|---|
| Days from symptom onset | 100 | Yes | 0.92 (0.87–0.96) |
|
| |||
| Female sex | 72.2 | Yes | 0.53 (0.37–0.76) |
|
| |||
| Age, y | 98.1 | Yes | |
| <40 | Reference | ||
| 40–49 | 3.73 (0.98–14.22) | ||
| 50–59 | 766 (2.19–26.77) | ||
| 60–69 | 10.63 (3.11–36.35) | ||
| 70–79 | 14.76 (4.28–50.93) | ||
| ≥80 | 30.68 (8.80–106.95) | ||
|
| |||
| Charlson Comorbidity Indexb | 100 | Yes | 1.15 (1.06–1.25) |
|
| |||
| Long-term care facility resident | 99.8 | Yes | 1.17 (0.66–2.05) |
|
| |||
| Highest heart rate (per increase of 10 beats per minute)c | 68.4 | Yes | 1.05 (1.04–1.06) |
|
| |||
| Lowest systolic blood pressure,c mm Hg | 96.2 | Yes | |
| ≥110 | Reference | ||
| 100–109 | 0.93 (0.58–1.48) | ||
| 90–99 | 0.63 (0.38–1.06) | ||
| <90 | 1.74 (1.07–2.86) | ||
|
| |||
| Highest respiratory rate,c breaths per minute | 100 | Yes | 1.05 (1.02–1.07) |
|
| |||
| First-available Glasgow Coma Scale score <15c | 100 | Yes | 1.89 (1.21–2.80) |
|
| |||
| First-available Pao2 to Fio2 ratioc | 99.8 | Yes | |
| ≥300 | Reference | ||
| 200–299 | 1.84 (1.21–2.80) | ||
| 100–199 | 2.41 (1.41–4.11) | ||
| <100 | 4.20 (1.87–9.40) | ||
|
| |||
| First-available serum creatinine level, mg/dL | 99.2 | Yes | 1.11 (1.02–1.21) |
|
| |||
| First-available white blood cell count, ×1000/μL | 100 | Yes | 1.05 (1.02–1.09) |
|
| |||
| Race/ethnicity | 378 | No | – |
|
| |||
| Dyspnea | 377 | No | – |
|
| |||
| Body temperatured | 35.0 | No | – |
|
| |||
| First-available serum level of aspartate aminotransferase >40 U/Lc | 18.1 | No | – |
Analysis includes 1470 patients surviving >24 hours from hospital arrival.
Weighted Charlson Comorbidity Index calculated excluding age component.
Value obtained within 24 hours of hospital arrival.
Temperature most different from 37 °C in the first 24 hours after arrival at the study hospital.
Fewer risk factors were identified for early respiratory failure. These risk factors included body mass index, dyspnea on presentation, initial respiratory rate, abnormal mental status, higher first-available creatinine level, higher first-available white blood cell count, and elevated first-available aspartate aminotransferase level (Supplemental Table 7, available online only). The adjusted odds of early respiratory failure were more than 4 times higher if the first-available Glasgow Coma Scale score was less than 15 (odds ratio, 4.69; 95% CI, 3.07–7.16). In contrast, risk factors identified for late respiratory failure and the magnitudes of the observed associations were similar to those identified for mortality (Supplemental Table 8, available online only). Chronic pulmonary disease was not identified as a risk factor for either early or late respiratory failure. Sensitivity analyses that excluded patients who died without meeting respiratory failure criteria or excluded face mask oxygen support from the definition of respiratory failure yielded similar results.
Among the 1218 survivors, the 221 (18.1%) patients who were prescribed at least 1 form of new respiratory support were older and experienced a higher incidence of respiratory failure during their hospitalization than did patients who did not receive new respiratory support (Supplemental Table 9, available online only). Discharge with new home-based or facility-based health care services occurred in 259 of the 1153 (22.5%) survivors initially admitted from home. Compared with survivors who were not discharged with new health care services, these patients were older and had more severe illness and longer hospitalizations (Supplemental Table 10, available online only). Ten of the 34 (29%) survivors who required new renal replacement therapy during their admission continued dialysis after discharge.
Discussion
In this large US cohort of inpatients with COVID-19 followed to hospital discharge, we observed prolonged hospital stays and 17.7% hospital mortality during the first pandemic wave. Most patients developing critical illness were admitted to the ICU by hospital day 4, and mortality increased substantially when respiratory failure was complicated by shock or the need for dialysis. Increasing age had an exponential association with mortality. Male sex, comorbidity burden, hypoxemia, and abnormalities of vital signs and laboratory test results on hospital day 1 were also associated with increased odds of dying. Among survivors, 18.1% were discharged with respiratory support that was new or higher in intensity than at baseline. Nearly 1 in 4 survivors admitted from home received new at-home or facility-based health care services at discharge.
Hospital mortality in our cohort was lower than in some contemporaneous cohorts in China2 and the United States1,20,21 but higher than the 10% mortality observed in a systematic review of studies performed through April 20, 2020.22 Heterogeneous mortality rates across studies may be due to differing follow-up duration as well as between-hospital differences in admission thresholds, patient mix, management strategies, resource strain, and hospital-level operational modifications.5,6,23–25 We captured data through hospital discharge for all cohort patients, including the nearly 10% who remained in the hospital for more than 4 weeks, thus avoiding the potential for misestimation of hospital mortality.20,26 The geographic heterogeneity of this cohort should also mitigate the effects of regional-level and hospital-level variation, yielding a more generalizable estimate of COVID-19 hospital mortality early in the pandemic. However, current mortality rates may differ from our estimates in the face of shifting SARS-CoV-2 infection rates and COVID-19 treatment.27,28
Our data also highlight the high inpatient morbidity and prolonged hospitalizations experienced by patients with COVID-19. Shock and renal failure were common among nonsurvivors, corroborating reports suggesting that COVID-19–related critical illness and death often result from multiorgan dysfunction rather than isolated respiratory failure.5,29,30 Adding to this prior work, we found that ICU admission, when required, was likely to occur early in the hospitalization. Together, these findings suggest that efforts to reduce the incidence of COVID-19 critical illness should consider the multiorgan effects of SARS-CoV-2 infection and focus on the prehospital and early hospital settings.
The number of patients who received new postdischarge health care services or respiratory support suggests that substantial impairment relative to baseline health status and function is common among survivors of a hospitalization related to COVID-19. However, characterization of the severity, patterns, and duration of symptoms and disability after outpatient SARS-CoV-2 infection and hospitalization for COVID-19 remains preliminary.31–34 Future studies are needed to better characterize the posthospital trajectory in COVID-19 survivors as well as predictors, mechanisms, trajectory, management, and prevention of persistent impairment in this population.
We evaluated a comprehensive and generalizable array of demographic and clinical characteristics as potential risk factors for COVID-19 mortality and respiratory failure. Men made up a disproportionately large fraction of hospitalized patients with COVID-19 and experienced poorer outcomes than women, confirming the results of prior studies.3,5,35,36 Drivers of sex-based disparities in clinical outcomes warrant further study and may include differences in angiotensin-converting enzyme 2 receptor expression, immune response, and other mechanisms.37,38 However, as with any other multivariable analysis, the parameters chosen and their estimated effect sizes are conditional on the other variables in the model. This is particularly important when interpreting our data suggesting that, for a given level of demographic and clinical risk at a given hospital, COVID-19 outcomes in our cohort were similar across race/ethnicity categories once patients were hospitalized. This finding is consistent with prior reports39 and suggests that higher COVID-19 mortality among minority patients does not indicate a biological difference in risk but rather reflects underlying health disparities leading to worse baseline health status, higher illness severity on presentation, and delayed hospital presentation combined with disparities in SARS-CoV-2 infection rates,40–43 admission thresholds, and potentially differences in care quality at hospitals treating a greater proportion of minority patients.44,45
Our study has important strengths and several notable limitations. Leveraging the resources and personnel of an experienced clinical trials network, we collected a rich body of carefully curated data for a cohort representative of the underlying population of all patients with COVID-19 hospitalized early in the pandemic at 57 geographically diverse US hospitals. Follow-up to hospital discharge and identification of new health support needs among survivors yielded a comprehensive portrait of the sickest patients’ hospital trajectories. Our patient cohort was enrolled early in the COVID-19 pandemic, allowing us to contribute to collaborative international efforts46 to describe and study the epidemiology of COVID-19 and substantively inform clinical trial design for national and international efforts such as Operation Warp Speed’s ACTIV-3 studies.47 Pharmacologic and organ support management strategies, however, have continued to evolve with emerging evidence, new therapeutic options, and clinicians’ increasing experience managing this disease. For instance, treatment with repurposed drugs (hydroxychloroquine and azithromycin) shown in subsequent trials to lack efficacy was common in our cohort,48–52 although corticosteroids—which now appear beneficial—were rarely used.53,54 Our definition of respiratory failure included receipt of high-flow oxygen therapy as well as invasive or noninvasive positive pressure ventilation, increasing the likelihood that identified risk factors are unaffected by shifting management practices. However, additional studies are needed to validate the risk factors we identified and evaluate how new therapeutic strategies affect the observed associations.
Our study has several additional limitations. First, our data do not include deaths or readmissions occurring after study hospital discharge. Second, although collection of patients’ clinical histories (including symptoms) by manual review of clinical documentation has advantages over claims-based or automated analyses, our findings may be vulnerable to recall bias, underreporting dependent on patients’ illness severity, and incomplete clinician documentation in times of strain. Third, most study sites were academic referral hospitals, so complex, severely ill patients with COVID-19 may be overrepresented relative to a population-based sample. Fourth, our analysis did not directly evaluate potential effects on patient management and outcomes due to variations in patient volumes and resource strain between hospitals and across the enrollment period. Inclusion of a site-level random effect in our risk factor analyses mitigated the effect of such differences. Finally, because of the selection procedure used to identify important risk factors, reported CIs may underestimate the imprecision for the effect size estimates.55 The impact of this selective inference is substantially mitigated by the relatively small collection of candidate variables and the relatively strong prognostic value of the included risk factors.
Conclusions
Among patients hospitalized with COVID-19 early in the pandemic at a geographically diverse network of US hospitals, mortality was 17.7% and was associated with comorbidity burden, male sex, and advancing age. Admission to the ICU, when required, usually occurred within 4 days of hospital arrival. Patients experienced prolonged hospital stays, and a substantial proportion of survivors received new facility-based or home-based health care services or new respiratory support at discharge.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Dr Angela Presson for input regarding statistical analyses and Alison Pollock, Xiaoqi Bao, and Dr Bo Zhao for assistance creating data visualizations. See the list of PETAL Network contributors in Supplement 2 (available online only).
FINANCIAL DISCLOSURES
This work was supported by the National Heart, Lung, and Blood Institute (NHLBI)(3U01HL123009-06S2, U01HL123009, U01HL122998, U01HL123018, U01HL123023, U01HL123008, U01HL123031, U01HL123004, U01HL123027, U01HL123010, U01HL123033, U01HL122989, U01HL123022, and U01HL123020) and the National Institutes of Health (UL1RR025758). This work does not necessarily reflect the view of the US Government, National Institutes of Health, or Department of Veterans Affairs.
Contributor Information
Ithan D. Peltan, assistant professor, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Intermountain Medical Center, Murray, Utah, and an adjunct assistant professor, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, University of Utah School of Medicine, Salt Lake City.
Ellen Caldwell, data analyst/biostatistician, Division of Pulmonary, Critical Care and Sleep Medicine, Department of Medicine, University of Washington, Seattle.
Andrew J. Admon, clinical instructor, Division of Pulmonary and Critical Care Medicine, Department of Medicine, University of Michigan School of Medicine, Ann Arbor.
Engi F. Attia, assistant professor, Division of Pulmonary, Critical Care and Sleep Medicine, Department of Medicine, University of Washington.
Stephanie J. Gundel, research coordinator, Division of Pulmonary, Critical Care and Sleep Medicine, Department of Medicine, University of Washington.
Kusum S. Mathews, assistant professor, Division of Pulmonary and Critical Care Medicine, Department of Medicine and Department of Emergency Medicine, Icahn School of Medicine at Mount Sinai, New York, New York.
Alexander Nagrebetsky, assistant professor, Department of Anesthesia, Critical Care and Pain Medicine, Massachusetts General Hospital and Harvard Medical School, Boston, Massachusetts.
Sarina K. Sahetya, assistant professor, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland.
Christine Ulysse, statistician, Division of Biostatistics, Department of Medicine, Massachusetts General Hospital.
Samuel M. Brown, professor, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Intermountain Medical Center, and Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, University of Utah School of Medicine.
Steven Y. Chang, professor, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Ronald Reagan UCLA Medical Center, David Geffen School of Medicine at University of California, Los Angeles (UCLA).
Andrew J. Goodwin, professor, Division of Pulmonary, Critical Care, Allergy, and Sleep Medicine, Department of Medicine, Medical University of South Carolina, Charleston.
Aluko A. Hope, associate professor, Division of Critical Care Medicine, Department of Medicine, Montefiore Medical Center and Albert Einstein School of Medicine, Bronx, New York.
Theodore J. Iwashyna, professor, Division of Pulmonary and Critical Care Medicine, Department of Medicine, University of Michigan School of Medicine, and Veterans Affairs (VA) Center for Clinical Management Research, VA Ann Arbor Healthcare System, Ann Arbor, Michigan.
Nicholas J. Johnson, associate professor, Division of Pulmonary, Critical Care and Sleep Medicine, Department of Medicine, University of Washington, and Department of Emergency Medicine, University of Washington.
Michael J. Lanspa, associate professor, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Intermountain Medical Center, and Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, University of Utah School of Medicine.
Lynne D. Richardson, professor, Departments of Emergency Medicine and Population Health Sciences, and codirector, Institute for Health Equity Research, Icahn School of Medicine at Mount Sinai.
Kelly C. Vranas, assistant professor, Center to Improve Veteran Involvement in Care, VA Portland Health Care System, Portland, Oregon, and Division of Pulmonary and Critical Care Medicine, Department of Medicine, Oregon Health and Science University, Portland.
Derek C. Angus, professor and chair, Department of Critical Care Medicine, University of Pittsburgh Medical Center and University of Pittsburgh Schools of the Health Sciences, Pittsburgh, Pennsylvania.
Rebecca M. Baron, associate professor, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston.
Benjamin A. Haaland, associate professor, Department of Population Health Sciences, University of Utah School of Medicine.
Douglas L. Hayden, assistant professor, Division of Biostatistics, Department of Medicine, Massachusetts General Hospital.
B. Taylor Thompson, professor, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Massachusetts General Hospital and Harvard Medical School.
Todd W. Rice, associate professor, Division of Allergy, Pulmonary, and Critical Care Medicine, Department of Medicine, Vanderbilt University School of Medicine, Nashville, Tennessee.
Catherine L. Hough, professor and chief, Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Medicine, Oregon Health and Science University.
REFERENCES
- 1.Lewnard JA, Liu VX, Jackson ML, et al. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ. 2020;369:m1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anesi GL, Jablonski J, Harhay MO, et al. Characteristics, outcomes, and trends of patients with COVID-19–related critical illness at a learning health system in the United States. Ann Intern Med. 2021;174(5):613–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Docherty AB, Harrison EM, Green CA, et al. ; ISARIC4C investigators. Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta S, Hayek SS, Wang W, et al. ; STOP-COVID Investigators. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. 2020;180(11):1436–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Domecq JP, Lal A, Sheldrick CR, et al. ; Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study (VIRUS): COVID-19 Registry Investigator Group. Outcomes of patients with coronavirus disease 2019 receiving organ support therapies: the international Viral Infection and Respiratory Illness Universal Study registry. Crit Care Med. 2021;49(3):437–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO Working Group on the Clinical Characterisation and Management of COVID-19 infection. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis. 2020;20(8):e192–e197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-Related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22(7):707–710. [DOI] [PubMed] [Google Scholar]
- 10.Brown SM, Grissom CK, Moss M, et al. ; NIH/NHLBI PETAL Network Collaborators. Nonlinear imputation of Pao2/Fio2 from Spo2/Fio2 among patients with acute respiratory distress syndrome. Chest. 2016;150(2):307–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Efron B, Hastie T, Johnstone I, Tibshirani R. Least angle regression. Ann Statistics. 2004;32(2):407–499. [Google Scholar]
- 12.Zou H, Hastie T. Regularization and variable selection via the elastic net. J R Stat Soc Series B Stat Methodol. 2005; 67(2):301–320. [Google Scholar]
- 13.Rubin DB. Multiple Imputation for Nonresponse in Surveys. Wiley; 1987. [Google Scholar]
- 14.van der Heijden GJ, Donders AR, Stijnen T, Moons KG. Imputation of missing values is superior to complete case analysis and the missing-indicator method in multivariable diagnostic research: a clinical example. J Clin Epidemiol. 2006;59(10):1102–1109. [DOI] [PubMed] [Google Scholar]
- 15.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2010;30(4):377–399. [DOI] [PubMed] [Google Scholar]
- 16.van Buuren S, Groothuis-Oudshoorn K. MICE: multivariate imputation by chained equations in R. J Stat Software. 2011;45(3):1–67. [Google Scholar]
- 17.Localio AR, Berlin JA, Ten Have TR, Kimmel SE. Adjustments for center in multicenter studies: an overview. Ann Intern Med. 2001;135(2):112–123. [DOI] [PubMed] [Google Scholar]
- 18.Schelldorfer J, Meier L, Bühlmann P. GLMMLasso: an algorithm for high-dimensional generalized linear mixed models using L1-penalization. J Computational Graphical Statistics. 2014;23(2):460–477. [Google Scholar]
- 19.Vergouwe Y, Royston P, Moons KG, Altman DG. Development and validation of a prediction model with missing predictor data: a practical approach. J Clin Epidemiol. 2010; 63(2):205–214. [DOI] [PubMed] [Google Scholar]
- 20.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Argenziano MG, Bruce SL, Slater CL, et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ. 2020;369:m1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Potere N, Valeriani E, Candeloro M, et al. Acute complications and mortality in hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Crit Care. 2020;24(1):389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wadhera RK, Wadhera P, Gaba P, et al. Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA. 2020;323(21):2192–2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bravata DM, Perkins AJ, Myers LJ, et al. Association of intensive care unit patient load and demand with mortality rates in US Department of Veterans Affairs hospitals during the COVID-19 pandemic. JAMA Netw Open. 2021;4(1): e2034266. doi: 10.1001/jamanetworkopen.2020.34266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mathews KS, Seitz KP, Vranas KC, et al. ; National Heart, Lung, and Blood Institute Prevention and Early Treatment of Acute Lung Injury (PETAL) Clinical Trials Network. Variation in initial U.S. hospital responses to the coronavirus disease 2019 pandemic. Crit Care Med. 2021;49(7):1038–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jung RG, Di Santo P, Clifford C, et al. Methodological quality of COVID-19 clinical research. Nat Commun. 2021;12(1):943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Asch DA, Sheils NE, Islam MN, et al. Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 months of the pandemic. JAMA Intern Med. 2021; 181(4):471–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Monod M, Blenkinsop A, Xi X, et al. ; Imperial College COVID-19 Response Team. Age groups that sustain resurging COVID-19 epidemics in the United States. Science. 2021;371(6536): eabe8372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang Y, Lu X, Li Y, et al. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med. 2020;201(11):1430–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Richards-Belle A, Orzechowska I, Gould DW, et al. ; ICNARC COVID-19 Team. COVID-19 in critical care: epidemiology of the first epidemic wave across England, Wales and Northern Ireland. Intensive Care Med. 2020;46(11):2035–2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tenforde MW, Kim SS, Lindsell CJ, et al. ; IVY Network Investigators; CDC COVID-19 Response Team; IVY Network Investigators. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(30):993–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chopra V, Flanders SA, O’Malley M, Malani AN, Prescott HC. Sixty-day outcomes among patients hospitalized with COVID-19. Ann Intern Med. 2021:174(4):576–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCue C, Cowan R, Quasim T, Puxty K, McPeake J. Long term outcomes of critically ill COVID-19 pneumonia patients: early learning. Intensive Care Med. 2021;47(2):240–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Taboada M, Cariñena A, Moreno E, et al. Post-COVID-19 functional status six-months after hospitalization. J Infect. 2021;82(4):e31–e33. doi: 10.1016/j.jinf.2020.12.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Myers LC, Parodi SM, Escobar GJ, Liu VX. Characteristics of hospitalized adults with COVID-19 in an integrated health care system in California. JAMA. 2020;323(21):2195–2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020;81(2):e16–e25. doi: 10.1016/j.jinf.2020.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Takahashi T, Ellingson MK, Wong P, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020;588(7837):315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Griffith DM, Sharma G, Holliday CS, et al. Men and COVID-19: a biopsychosocial approach to understanding sex differences in mortality and recommendations for practice and policy interventions. Prev Chronic Dis. 2020;17:E63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with Covid-19. N Engl J Med. 2020;382(26):2534–2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Introduction to COVID-19 racial and ethnic health disparities. Centers for Disease Control and Prevention. Updated December 10, 2020. Accessed February 22, 2021. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/index.html
- 41.Adegunsoye A, Ventura IB, Liarski VM. Association of Black race with outcomes in COVID-19 disease: a retrospective cohort study. Ann Am Thorac Soc 2020;17(10):1336–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bui DP, McCaffrey K, Friedrichs M, et al. Racial and ethnic disparities among COVID-19 cases in workplace outbreaks by industry sector—Utah, March 6-June 5, 2020. MMWR Morb Mort Wkly Rep. 2020;69(33):1133–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood). 2020;39(7):1253–1262. [DOI] [PubMed] [Google Scholar]
- 44.Corl K, Levy M, Phillips G, Terry K, Friedrich M, Trivedi AN. Racial and ethnic disparities in care following the New York State Sepsis Initiative. Health Aff (Millwood). 2019;38(7):1119–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jones JM, Fingar KR, Miller MA, et al. Racial disparities in sepsis-related in-hospital mortality: using a broad case capture method and multivariate controls for clinical and hospital variables, 2004–2013. Crit Care Med. 2017;45(12): e1209–e1217. doi: 10.1097/CCM.0000000000002699 [DOI] [PubMed] [Google Scholar]
- 46.COVID-19 clinical research resources. ISARIC. Accessed February 4, 2021. https://isaric.org/research/covid-19-clinical-research-resources/ [Google Scholar]
- 47.ACTIV-3/TICO LY-CoV555 Study Group, Lundgren JD, Grund B, et al. A neutralizing monoclonal antibody for hospitalized patients with Covid-19. N Engl J Med. 2021;384(10):905–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Self WH, Semler MW, Leither LM, et al. Effect of hydroxychloroquine on clinical status at 14 days in hospitalized patients with COVID-19: a randomized clinical trial. JAMA. 2020;324(21):2165–2176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brown SM, Peltan I, Kumar N, et al. Hydroxychloroquine vs. azithromycin for hospitalized patients with COVID-19 (HAHPS): results of a randomized, active comparator trial. Ann Am Thorac Soc. 2020;18(4):590–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.WHO Solidarity Trial Consortium, Pan H, Peto R, et al. Repurposed antiviral drugs for Covid-19 — interim WHO Solidarity Trial results. N Engl J Med. 2021;384(6):497–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Furtado RHM, Berwanger O, Fonseca HA, et al. ; COALITION COVID-19 Brazil II Investigators. Azithromycin in addition to standard of care versus standard of care alone in the treatment of patients admitted to the hospital with severe COVID-19 in Brazil (COALITION II): a randomised clinical trial. Lancet. 2020;396(10256):959–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.RECOVERY Collaborative Group. Azithromycin in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021;397(10274): 605–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Sterne JAC, Murthy S, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324(13):1330–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Taylor J, Tibshirani RJ. Statistical learning and selective inference. Proc Natl Acad Sci USA. 2015;112(25):7629–7634. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.