Abstract
Airborne transmission of aerosols contributes to a large portion of the SARS-CoV-2 spread indoors. This study develops a real-time interactive web-based platform for the public to compare various strategies to curb indoor airborne transmission of COVID-19 in different archetype buildings at a city scale. Although many countries have started vaccination and a gradual re-opening, because of emerging new variants of the virus and the possibility of future pandemics, a lively updated tool for monitoring and mitigation of infection risk is essential. As a demonstration, we evaluated the impacts of six mitigation measures on the infection risks in various building types in a city. It shows that the same strategy could perform quite differently, depending on building types and properties. All strategies are shown to reduce the infection risk but wearing a mask and reducing exposure time are the most effective strategies in many buildings, with around 60% reduction. Doubling the minimum required outdoor air ventilation rate is not as effective as other strategies to reduce the risk. It also causes considerable penalties on energy consumption. Therefore, new building ventilation standards, control actions, and design criteria should be considered to mitigate the infection risk and save energy.
Keywords: COVID-19, Airborne transmission, Indoor environment, Urban scale, Infection risk, Energy saving
1. Introduction
A novel coronavirus disease, later named SARS-CoV-2 or COVID-19, rapidly spread throughout the world and was announced as a pandemic on March 11, 2020 (World Health Organization, 2020). As of June 03, 2021, the total number of COVID-19 cases exceeded 172.8 million worldwide, with a confirmed 3716,615 total deaths (WHO, 2020). Latest research findings show that aerosols' airborne transmission is a large portion of the spread of COVID-19 disease, especially in indoor spaces with poor ventilation conditions, large gatherings, and long-duration exposure to high concentration aerosols (Anderson, Turnham, Griffin & Clarke, 2020; Asadi, Bouvier, Wexler & Ristenpart, 2020; Li et al., 2021; Miller et al., 2020; Morawska & Cao, 2020; Tang et al., 2020). Several studies show that improving the ventilation condition and air cleaning, wearing a face mask, avoid overcrowding, and shortening the event time (exposure time) can significantly reduce the airborne infection risk in indoor environments (Agarwal et al., 2021; Kohanski, Lo & Waring, 2020; Morawska et al., 2020; R Zhang, Li, Zhang, Wang & Molina, 2020.) Buonanno et al. (2020b) evaluated the number of people infected by asymptomatic SARS-CoV-2 subjects in indoor environments. The results show the great importance of proper ventilation in the containment of the virus in indoor environments. Curtius, Granzin and Schrod (2020) tested the efficiency of operating four air purifiers equipped with HEPA filters and the total air exchange rate of in a high school classroom. The aerosol concentration was reduced by more than 90% within less than 30 mins after running the purifiers. Some other researchers evaluated the reduced infection risk using other strategies. For example, Dai and Zhao (2020) calculated the required ventilation rate to ensure a probability of less than 1% infection for different exposure times using the Wells-Riley model (Riley, Murphy & Riley, 1978). They modeled some typical scenarios and concluded that the minimum required ventilation rate can be reduced to a quarter by wearing the mask, which normal ventilation can achieve. Lelieveld et al. (2020) estimated the infection risk in several indoor environments and compared the infection risk between different scenarios. Active room ventilation and wearing face masks by all subjects could reduce the individual infection risk by five to ten, similar to a high-volume HEPA air purifier. Zhang (2020) calculated the reduced infection risk by integrating different air quality strategies, including source control, ventilation, and air cleaning strategies. They modeled classrooms and offices because of their large occupant density. Integration of strategies can reduce the infection risk by a factor of 8.5 to 500. Sun and Zhai (2020) modified the Wells-Riley model by introducing two indices for social distancing and ventilation effectiveness. It was shown that half occupancy density could reduce the infection risk by 20–40% in the first 30 min of the event. The combination of proper social distance and high ventilation effectiveness can reduce the required ventilation rate for a safe indoor environment. A comprehensive study on the ventilation standards and controlling the risk of airborne respiratory infection shows that current standards cannot prevent infection. Ventilation standards must be improved to explicitly consider infection control in their definitions (Morawska et al., 2021). Shen et al. used a systematic approach for evaluating the IAQ control strategies in mitigating the infection risk in different indoor environments (Shen, Kong, Dong, Birnkrant & Zhang, 2021). Integrated mitigation strategies such as doubling supply air, HEPA filter, displacement ventilation, etc., are recommended for different indoor spaces to mitigate the infection risk to the target level. Enhanced ventilation is an effective strategy to mitigate the risk, but it also comes with higher costs because of increased heating or cooling energy consumption. Therefore, new ventilation strategies and standards must be introduced, such as flexible demand-controlled ventilation systems and personalized ventilation, to reduce the infection risk and save energy. Combining dilution ventilation (DV) and Ventilative cooling (VC) is a proposed strategy to minimize the cooling related energy consumption and reduce COVID-19 airborne transmission in high-rise buildings (Sha, Zhang & Qi, 2021). Using air cleaning systems is another effective solution for indoor airborne control of COVID-19. Traditional air cleaning systems have some operational process risks. To aovid them, Feng et al. proposed a new UV+Filter system with lower risk and higher energy consumption compared to the Fibrous-filter, ESP (electrostatic precipitator), and HEFS (hybrid electrostatic filtration system) (Feng, Cao & Haghighat, 2021).
While these previous studies focused on a few building types, some other studies investigated more buildings or developed general tools for all types. Jiminez et al. (2020) developed a public data spreadsheet known as “COVID-19 Aerosol Transmission Estimator” (COVID-19 Estimator or ATE hereafter). Users are allowed to input the prevalence rate in the region of study and other building-specific information. Their tool provides much information on key input parameters based on the most recent COVID-19 studies and makes it possible to evaluate infection risks and mitigation strategies. Some other tools have been developed for the assessment and mitigation of COVID-19 airborne infection risk. MyCOVIDRisk (Goldberg, Bingaman, Perera & Ranney, 2021) is an online tool developed by Brown University, walking through a series of questions about the event a person plans to attend. Based on those factors, it calculates the infection risk and provides a series of suggestions to reduce it. SAFEAIRSPACES COVID-19 Aerosol Relative Risk Estimator (Parhizkar, Van Den Wymelenberg1, Haas & Corsi, 2020) is another online tool that calculates the airborne infection risk in a room based on user input data and presents risk levels that correspond to higher ventilation rates. Airborne.cam (University of Cambridge, 2020) is an online application that helps users understand how to mitigate indoor airborne transmission of the SARS-CoV-2 virus. They provide time series infection risk based on the user input data. Kasibhatla et al. developed the “COVID exposure modeler” (P. Kasibhatla, Jimenez, Fay, Albright & Pan, 2020), an online tool for estimating COVID-19 airborne infection risk in classrooms as an offshoot of the COVID-19 Estimator tool. They calculate the probability of infection risk in a classroom based on the uncertainty in the input data.
However, most of the existing tools are limited by: user-friendliness; with a static prevalence rate: Eeach city or state has its unique COVID-19 prevalence with daily variations, e.g., the top five most infected state prevalence rate varies from 3.5%−5% in the U.S. and 0.6%−1.3% in Canada on December 29, 2021 (Wang, Katal & Albettar, 2020; lack of data; standalone building or building type not on a large scale such as urban, contourite, or continent-scale for real-time infection risk; serving only research community, not the general public; Besides the variations of the prevalence rates, the infection risk model often has other key input parameters, often related to cities, buildings, and occupancies, e.g., lockdown dates and rates, occupancy levels, age, sex, and exposure time. Building system-specific parameters are also important, including floor area or room size, outdoor air ventilation, recirculation rates, duct filter types, with/without air cleaners and their capacities, and mask types. So, the information cannot be readily transferred to the public.
While COVID-19 has been showing it could linger longer because of its emerging new variants or become permanent with the human being, also the possibility of future pandemics, it is essential to increase public awareness and knowledge about the indoor airborne risks. While research results or publications data often take time to reach the crowd, a well-calibrated and interactive tool will be beneficial to unravel the myth of the risk and develop mitigation strategies. The public have not been well aware of the risk and still baffled about the COVID-19 and mitigation measures: for example, a large number of people have taken to the streets in various countries, such as the US, UK, Australia, Italy, and Canada, to protest the mandatory use of face masks and other lockdown rules. A recent study on the COVID-19 prevalence in Chicago shows that the population density was not significantly related to the prevalence, and areas with low educational attainment experienced higher case rates (Kashem, Baker, González & Lee, 2021). Therefore, public awareness can play a major role in preventing future outbreaks. Another study on the real-time data in the 276 prefecture-level cities in China also showed that a city with a high-level of information technologies, e.g., real-time urban-scale data available from the “smart city infrastructure”, could contribute significantly to the pandemic preventions and controls (Chu, Cheng & Song, 2021). A similar conclusion was reached by another study of using anonymized mobile phone data to cluster mobility information and develop isolaton strategies in Brazil (Silva et al., 2021). A statistical study on the city management during crisis situations also found that starting in 2020, the research focus has turned primarily towards using information and communication technologies for crisis prevention and control (Machado, Melina Nassif Mantovani Ribeiro & Backx Noronha Viana, 2021). Much information may be well known by the research community, but most often not by the public; when the public has been aware of the risk and measures from the scientific publication as a source, it could be already late.
To address the generality problem based on building type information, acquiring all this information at the urban scale may be achieved in two ways. One is to develop an archetype building library based on publicly available data, such as building standards and codes and statistics databases. Because an archetype building is specific to a building type, the results of urban-scale infection risk and mitigation strategies can be compared statistically among various building types and total numbers in a city. Although actual building information may deviate from the archetype-based database, it is reasonable to consider that most buildings of the same type tend to follow similar standards, codes, and statistics. So, the infection risk and mitigation evaluations are substantiated at the urban scale. A similar method has been widely applied to urban-level building energy analysis: archetype libraries were developed to characterize the properties necessary for building energy analysis, but it is challenging to collect them for all buildings in a city. The use of ideal or archetype building also was applied by previous researchers. Gao, Li and Leung (2009) developed a model for calculating indoor airborne infection risk at a community level and estimated the impact of control strategies such as ventilation rate on the infection risk. They concluded that the current ventilation rate in Hong Kong offices and the recommended value by ASHRAE are pretty low to control airborne infectious diseases in indoor environments. Gao et al. (2016) designed an indoor transmission network model for an ideal city to estimate the infection risk and disease spread in their other work. They evaluated the effectiveness of using ventilation strategy in controlling the disease spread and compared it with other intervention strategies. They concluded that the ventilation rate in homes, classrooms, and offices could reach up to 5 ACH by opening the windows. Its impact is the same as isolating 12% of the population or mass vaccination. They did not model all buildings in a city and used some actual censuses, social behavior surveys, and building surveys, etc., for community-scale analysis.
On the other hand, as noted previously, archetype buildings could deviate from actual buildings in reality, so it is still preferable to obtain the actual building information. To address the building-specific problem: the impact of mitigation strategies should be studied separately for each building to find the best strategy depending on the building condition. Also, to update the current ventilation standards, the required minimum ventilation rate to control the airborne infection risk should be investigated for each building type. However, many of the required data should be provided by building owners or others with access to the data, and the information is often private or proprietary. A solution to this dilemma could be creating an anonymous and user-friendly web tool so that a building owner, manager, and engineer can provide the information required, assess the infection risk, and evaluate the mitigation strategies specific to his/her building. Meanwhile, all the input information will be lost once the secure web browser is closed to maintain privacy.
In this study, we tried to achieve solutions for both problems. First, we developed an archetype library based on different standards and codes to estimate the parameters we need to calculate infection risk in buildings. For example, a building's minimum required ventilation rate is based on ASHRAE Standard 62.1 (ANSI/ASHRAE, 2019). This work aims to evaluate the probability of infection in buildings based on the current standards and then reduce the infection risk by comparing different mitigation strategies. We developed a user-friendly web-based and 3D-city portal, the City Reduced Probability of Infection for Indoor Airborne Transmission of COVID-19 (https://concordia-cityrpi.web.app/) for North America. The website facilitates any layperson to use the service without prior technical knowledge from his/her mobile devices or computers. All the archetype library data are based on publicly available data. All the confidential input parameters are not collected and discarded at the client-side after an active web session. Since its launch in July 2020, the CityRPI website has been used extensively with visits across North America and Europe and many media coverages from both academic research (Dupuis, 2020) and the public (Cook, 2020; Crockett, 2020; Rainville, 2020). This paper summarizes the background and fundamentals of the website. Second, to investigate the required ventilation rate in controlling the infection risk, we studied the impact of different ventilation rates on infection risk and energy consumption at the urban scale. It was achieved by integrating CityRPI, which calculates the airborne infection risk of COVID-19 in all buildings, with CityBEM (City Building Energy Model) (Katal, Mortezazadeh & Wang, 2019; ), which calculates the impact of different strategies on the buildings' peak energy demand. This study can reveal the weaknesses of current ventilation standards in preventing the infection risk and their associated energy impacts.
2. Methodology
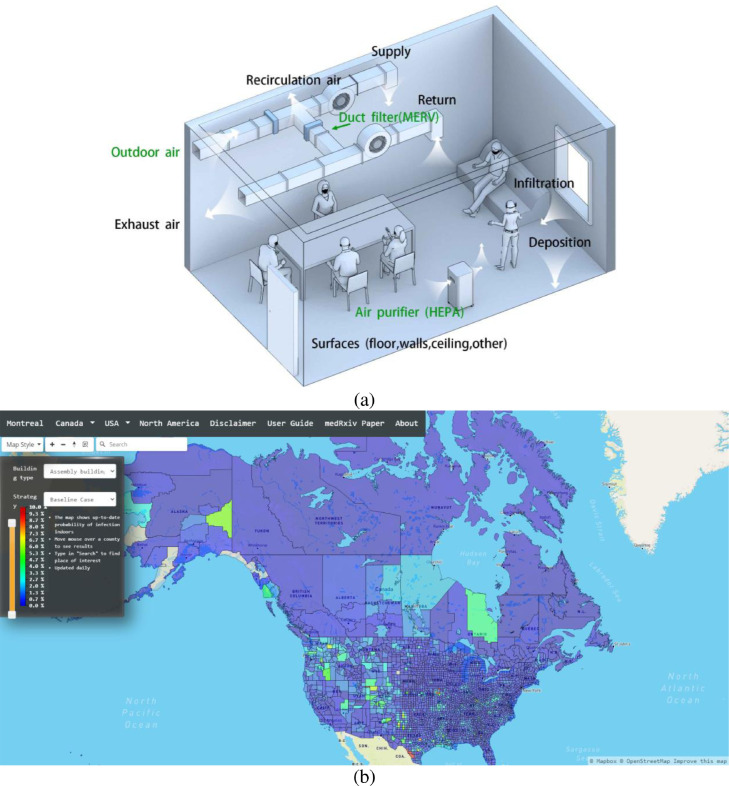
Fig. 1a shows the CityRPI model explained in detail in the following sections. To provide real-time data on airborne infection risk in North American cities, we developed an interactive website for the CityRPI model (https://concordia-cityrpi.web.app/). The purpose is to calculate the airborne infection risk in all city buildings and evaluate the impact of different mitigation measures on reducing the risk. The interactive website helps individuals find the best strategies for reducing the airborne infection risk in their buildings. The number of daily new infected cases in U.S. and Canadian cities are obtained from a GitHub page created by the New York Times (New York Times, 2020) and a GIS Hub provided by Esri Canada (Esri Canada, 2020). We calculate a baseline infection risk for each building based on the normal condition, then calculate the reduced probability of infection (RPI) using seven different mitigation measures. The result is plotted for all North American cities on the map (Fig. 1b). Users can select a building type and desired strategy to see the distribution of infection risk in all cities. More information can be found by moving the cursor on cities.
Fig. 1.
a) Schematic of the CityRPI model, b) CityRPI website: the probability of infection in North American cities.
2.1. CityRPI for assessing aerosol infection risks and mitigation strategies
The aerosol infection risk calculation is based on the modified Wells-Riley formulation (Gammaitoni & Nucci, 1997; Nicas, Nazaroff & Hubbard, 2005). The following theory was based on the original work of the COVID-19 Aerosol Transmission Estimator” by Jiminez et al. (2020) while this study extended the work to various building types at a whole-city scale for North America, investigating various mitigation strategies and their energy impacts, which have not been addressed previously. The estimator is based on five assumptions: i) one infector in a space with a constant SARS-CoV-2 quanta generation rate, ii) zero initial quanta in the space, iii) latent period of the disease is longer than the time duration of the event, iv) indoor environment is well-mixed, and v) the infectious quanta removal is a first-order process. Two types of P.I. are calculated: conditional P.I. and absolute P.I. The conditional probability of infection calculates the probability of another person getting infected, under the condition that there is one infector in the room. It is calculated based on the assumed number of infected people inside the room, and the prevalence rate of the disease in the studied area is not considered in the calculation of the conditional probability. The absolute probability of infection is calculated based on the and considering the prevalence rate of the disease in a community/city/region.
2.1.1. Conditional probability of infection
The conditional probability of infection is calculated by Eq. (1):
| (1) |
where is the number of quanta inhaled by a susceptible. Consider a susceptible in the room who inhales at rate B and is present for T hours. The expected number of quanta inhaled is calculated by Eq. (2):
| (2) |
is the time-average quanta concentration ; is the fraction of people in the room who wears the mask, and is the inhalation mask efficiency. By solving the well-mixed contaminant balance equation for the room (Eq. (3)), is calculated using Eq. (4).
| (3) |
| (4) |
is the volume of the room ; is the first-order loss rate coefficient for quanta ; and is the net quanta emission rate . is calculated based on the number of infected people in the room , the fraction of people in the room with the mask , exhalation mask efficiency , and quanta emission rate by one infected individual (Eq. (5)).
| (5) |
Buonanno et al. (2020a) estimated the quanta emission rate of SARS-CoV-2 for different combinations of expiratory activities (oral breathing, speaking, and singing or loudly speaking) and activity levels (resting, light activity, and heavy exercise). The values are based on the original variant of the virus, and the studied period in this work is the same period of the original variant. The must be updated by emerging new variants of the virus.
2.1.2. First-order loss rate coefficient
The infectious quanta could be removed from room air by first-order processes reflecting several mechanisms: outdoor air ventilation , filtration , deposition on surfaces , and airborne inactivation .
| (6) |
First, infectious quanta are removed with a first-order rate constant equal to the air change of outdoor air per hour supplied to the room by the HVAC system or by opening the windows. Second, the in-room air filtration using portable air purifiers and/or duct filters in HVAC systems can remove infectious quanta with a rate constant . Third, infectious quanta are removed by gravitational settling with a first-order rate constant . The deposition rate is calculated by Buonanno et al. (2020a) and is equal to 0.24 . Finally, infectious quanta are inactivated with a first-order rate constant . The quanta inactivation was evaluated based on the SARS-CoV-2 half-life (1.1 h) and is equal to 0.63 (Van Doremalen et al., 2020).
2.1.3. Absolute probability of infection
For the estimation of infection risk in city-scale where the number of infected individuals in each building is not known, the prevalence of the disease in the community is used to estimate the chance that a person is infective and the absolute probability of infection is calculated based on estimated infected individuals (Jimenez & Peng, 2020).
As described in the previous section, estimates the probability of a person getting infected under the “condition” that an infective person is in the same room. To evaluate the probability one healthy person gets infected in a room with a total number of Ntot people (including the healthy person him/herself), the chance that each of the rest of Ntot – 1 independent people is an infector equals to the disease prevalence rate , showing the probability of any person being infected in a city that depends on the state of the pandemic in the region of study and the period of the disease. Therefore calculates the probability of that healthy person of interest getting infected by any individual of the Ntot – 1 people in the room. Then, calculates the probability of the healthy person not being infected by another individual (the person of interest survives on the 1:1 basis), and estimates the probability that none of the Ntot – 1 will infect the healthy person of interest (i.e., the person survives on the 1: (Ntot – 1) basis). Finally, shows the chance that the healthy person of interest may get infected by one or multiple people in the same room, which is called the absolute probability of infection by Jimenez and Peng (2020).
| (7) |
| (8) |
and are the number of daily new cases and the population of the studied region, respectively. is the fraction of unreported cases. A study on ten diverse geographical sites in the U.S. shows that the estimated number of infections was much greater (6 to 24 times) than the number of reported cases in all sites (Havers et al., 2020). is the duration of the infectious period of SARS-CoV-2 (Byrne et al., 2020). Many studies only used the conditional probability of infection in their works, and few of them used the absolute probability of infection as the infection risk metric. The explanations of the conditional and absolute probabilities are based on recent publications, including Peng and Jimenez ( Peng & Jimenez, 2021) and Peng et al. (Peng et al., 2022.). The detailed formulations can be found in their “COVID-19 Aerosol Transmission Estimator” (Jimenez & Peng, 2020).
2.2. Building archetypes for airborne transmission risk analysis
Airborne infection risk calculation using the equations of Section 2.1 is a function of several buildings related parameters such as floor area, ceiling height, average stay time, the average age of occupants, occupant density, outdoor airflow rate, etc. Also, some building geometrical and non-geometrical properties are required for the calculation of buildings’ energy performance. Building geometry is obtained from open data sources such as OpenStreetMap (OSM) (Weber & Haklay, 2008), Microsoft building footprint (Microsoft, 2019a, 2019b), and Google Earth (G.E.) API (Gorelick et al., 2017) as described by Katal, Mortezazadeh and Wang (2020). It is almost impossible to access other parameters for all buildings in a city. Parameters necessary for building energy performance calculation are obtained from an archetype library developed by Katal et al. (2019). We developed a new archetype library to estimate the necessary parameters for the P.I. calculation in this work. In this library, we classified buildings into twenty-nine different usage types. Then, we assigned the required parameters to each class. The usage type of buildings for the City of Montreal studied in this work is obtained from the shapefiles of boundaries of the property assessment units (PAU) (City of Montreal, 2020).
We used several standards, codes, and references to collect the information for creating the archetype library. The numbers of occupants and outdoor ventilation rate were estimated based on ASHRAE Standard 62.1-Table 6.2.2.1 (ANSI/ASHRAE, 2019). The table provides occupant density (, outdoor airflow rate required per person , and outdoor airflow rate required per unit area for different occupancy categories (building type). Table 1 includes the information required from Table 6–1 of ASHRAE 62.1, such as the occupancy and ventilation rate, which have been doubled checked for consistency. It also includes other parameters for the calculation of infection risk, such as quanta generation rates, floor heights, which are used for the calculation of room volume of each building type based on the floor area, when we developed the archetype building models based on the Montreal building datasets. Using these parameters and the floor area of the building , total number of occupants and air change of outdoor air per hour is estimated by Eqs. (9) and (10). Note that CityRPI allows a user to input their own building geometrical and system information including floor height, area, occupancy density/number of people so that he/she can use it for a specific building or space.
| (9) |
| (10) |
Table 1.
Buildings archetype library for calculation of airborne infection risk.
| Building | Hf (m) | Rp (cfm/person) | Ra (cfm/ft2) | Occupant density (#/100m2) | Stay time (h) | |
|---|---|---|---|---|---|---|
| Apartment | 3.3 | 5 | 0.06 | 4 | 10 | 5.70 |
| Assembly | 5 | 5 | 0.06 | 150 | 3 | 15.95 |
| Bank | 3.2 | 7.5 | 0.06 | 15 | 1 | 6.85 |
| Cottage | 2.5 | 5 | 0.06 | 3 | 10 | 5.70 |
| Courthouse | 4.8 | 5 | 0.06 | 70 | 3 | 6.85 |
| Daycare | 2.5 | 10 | 0.18 | 25 | 6 | 15.95 |
| Hospital | 3 | 7.5 | 0.18 | 20 | 2 | 6.85 |
| Hotel | 3.6 | 5 | 0.06 | 10 | 2 | 6.85 |
| House | 2.5 | 5 | 0.06 | 3 | 10 | 5.70 |
| Industrial | 9 | 10 | 0.18 | 7 | 4 | 15.95 |
| Library | 4.5 | 5 | 0.12 | 10 | 3 | 6.85 |
| Museum | 6.5 | 7.5 | 0.06 | 40 | 3 | 15.95 |
| Nursing home | 2.5 | 5 | 0.12 | 25 | 2 | 5.70 |
| Office | 4 | 5 | 0.06 | 5 | 4 | 6.85 |
| Parking | 2 | 5 | 0.06 | 25 | 0.5 | 15.95 |
| Personal service | 3 | 7.5 | 0.06 | 25 | 1 | 6.85 |
| Public service | 2.5 | 5 | 0.06 | 30 | 1 | 15.95 |
| Restaurant | 3 | 7.5 | 0.18 | 70 | 1.5 | 6.85 |
| Retail store | 4.5 | 7.5 | 0.06 | 40 | 1 | 15.95 |
| Retirement house | 2.5 | 5 | 0.06 | 10 | 2 | 5.70 |
| School | 3 | 5 | 0.12 | 35 | 6 | 6.85 |
| Shared house | 2.5 | 5 | 0.06 | 10 | 2 | 5.70 |
| Shopping center | 2.4 | 7.5 | 0.06 | 40 | 2 | 15.95 |
| Sport center | 6 | 20 | 0.18 | 7 | 2 | 38.30 |
| Student house | 2.5 | 5 | 0.06 | 10 | 2 | 5.70 |
| Studio | 2.5 | 5 | 0.12 | 10 | 4 | 6.85 |
| Transport | 2.5 | 7.5 | 0.06 | 100 | 0.5 | 6.85 |
| University | 3 | 10 | 0.18 | 25 | 2 | 6.85 |
| Warehouse | 6 | 10 | 0.06 | 4 | 1 | 15.95 |
The susceptible person's breath rate in the room is estimated using US EPA Exposure Factors Handbook (Chapter 6) (U.S. Environmental Protection Agency, 2011). The breath rate depends on age and activity level. A typical activity type and average age are defined for each building type to assign the building breath rate. The quanta emission rate by an infective person in the room depends on the activity level. We used the recommended quanta emission rate by Buonanno et al. (2020a and 2020b), and standard activity levels to estimate each building type's quanta emission rate. The ceiling height and stay time are obtained based on the standard values of different building types. Therefore, we assumed that all buildings are designed and operating based on the available standards to calculate the indoor airborne infection risk and energy consumption in this work. Table 1shows some key input parameters of the archetype library assigned to each building type.
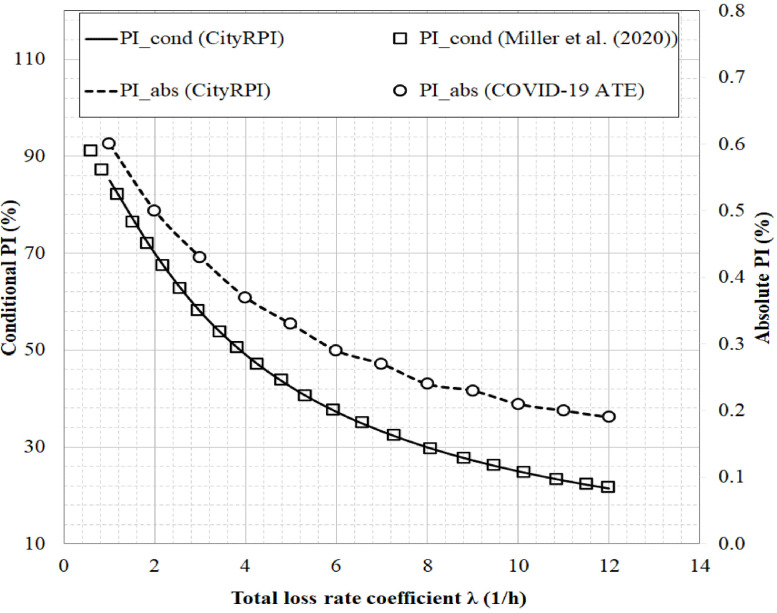
3. Verification based on a super-spreading event
We modeled a real super spreading event (SSE) in Skagit Valley, Washington, USA, to verify the CityRPI source code written for calculation of airborne infection risk. One symptomatic case attended the Skagit Valley Chorale (SVC) weekly rehearsal on March 10, 2020. Among the 61 attendees at the event, 53 cases were subsequently infected. Detailed analysis of evidence and reports by Miller et al. (2020) shows that respiratory aerosols' airborne transmission was the leading mode of transmission in this event. Miller et al. (2020) estimated the average quanta emission rate based on the available information and calculated the conditional P.I. for different scenarios. Jimenez (2020) extended the previous work by Miller et al. (2020). He developed the COVID-19 Aerosol Transmission Estimator (COVID-19 ATE) to calculate conditional and absolute airborne infection risk in several indoor environments. He evaluated the disease prevalence rate at the Skagit Valley and calculated the event's absolute P.I. In this section, we modeled the SVC event by the CityRPI and compared the conditional and absolute P.I. with the results by Miller et al. (2020) and Jimenez (2020). Table 2 shows the simulation settings of the SVC event. Conditional and absolute probabilities of infections are calculated as a function of loss rate and results are shown in Fig. 2 . Infection risks calculated by CityRPI are the same as Miller et al. (2020) and COVID-19 ATE (Jimenez and Peng, 2020), which shows that the airborne infection risk calculation by CityRPI is verified.
Table 2.
Parameters used for the simulation of SVC super spreading event.
| Parameter | Symbol | Unit | Value |
|---|---|---|---|
| Volume | 810 | ||
| Duration of event | hour | 2.5 | |
| Volumetric breathing rate | 1.0 | ||
| Quanta emission rate | 970 | ||
| Fraction of population with immunity | – | 0 | |
| Fraction of people with mask | – | 0 | |
| Total number of people in the room | – | 61 | |
| Number of infective people | – | 1 | |
| Disease prevalence rate | % | 0.011 |
Fig. 2.
Comparison of and at different loss rate coefficients for SVC super spreading event calculated by CityRPI, COVID-19 ATE from Jimenez (2020), and by Miller et al. (2020).
4. Risk assessments and energy impacts
According to Eqs. (1)-(8), the indoor aerosol infection risk is a function of several parameters. Some of them, such as the number of occupants, ventilation rate, stay time, and breathing rate, depend on the building usage type. Therefore, infection risk and the effectiveness of mitigation measures can change by building type. This section modeled the Montreal City by CityRPI and studied the impact of six mitigation strategies on indoor aerosol infection risk. Increasing the outdoor air ventilation rate by opening the windows or more outdoor air from the HVAC intakes can improve the room ventilation condition and reduce infection risk. However, it can also significantly increase building energy consumption in the winter. Therefore, finding the most effective strategy considering both the reduced probability of infection and the building energy consumption is essential. For this purpose, we conducted the simulation over Montreal from February 12–21, 2020, which was the coldest period of winter 2019, and the effectiveness of three mitigation strategies for improving the indoor ventilation condition (more outdoor air, upgrading duct filter, portable air cleaner) are compared. Note that all calculations were done based on assuming one infective in the room.
4.1. Results
In this section, first, we study the conditional and absolute P.I. of buildings at baseline conditions (e.g., minimum design ventilation rate by default). We assumed that all buildings operate under the normal condition with full occupancy during the whole study period. We compare the infection risk between different building types to find the most vulnerable buildings against the airborne infection risk of COVID-19. We also study the daily variation of to investigate its change with the prevalence rate of the disease. Then, to reduce the infection risk in buildings, we designed several scenarios using different mitigation measures. Finally, we applied the mitigation measures to all buildings in the city to find the most effective strategies for each building type. Some strategies also affect building energy consumption. Therefore, we calculated the increased peak demands for all buildings and identified the recommended strategies for risk reduction and energy consumption.
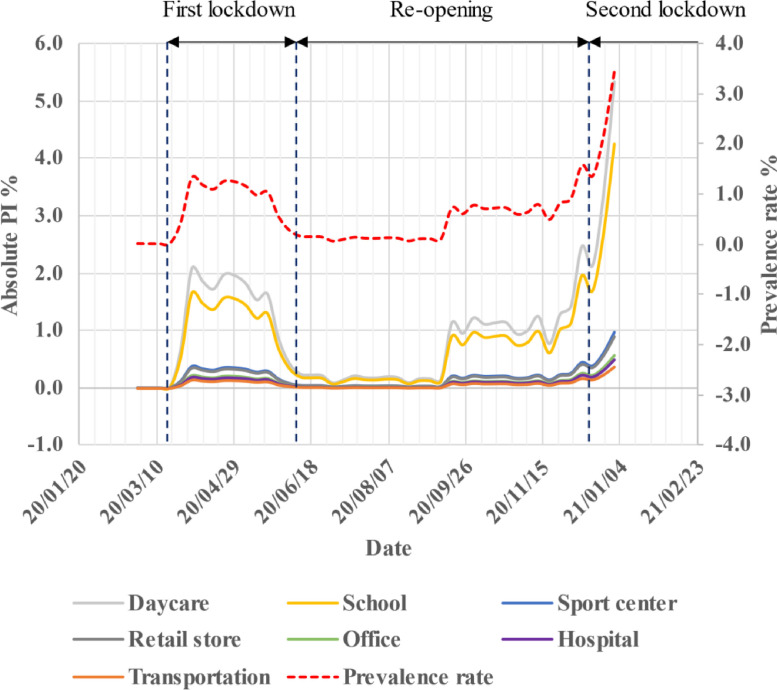
4.1.1. Probability of infection and prevalence rate
To demonstrate the P.I. variation with the city's prevalence rate, we calculated all buildings' historical P.I. from the start of the pandemic in Montreal until January 6, 2021. The first wave of the COVID-19 pandemic started on February 25, 2020, and the complete lockdown measures began on March 18, 2020. By reducing the number of daily cases, the re-opening gradually started from May 2, 2020, with re-opening schools and daycares around January 1, 2021. The second wave of the pandemic begun around the middle of September 2020. The Quebec government reimposed a partial lockdown on December 25, 2020 that continued until February 8, 2021. The red dot-line in Fig. 3 shows the weekly prevalence rate of the COVID-19 in Montreal. The highest prevalence rate is around 4%, which means that one person could be infected among 25 persons averaged over the whole population. It includes both symptomatic and asymptomatic cases. The historical of seven building types are plotted and compared in Fig. 3. We calculated the of all 29 building types, but to compare the variation of relative with time, the result is plotted for seven buildings with the most usage and importance during the pandemic. We did not plot the of buildings because it is not a function of the prevalence rate and is constant with time. According to Fig. 3, even though the varies with the prevalence rate but the relative infection risk of buildings is the same; for example, daycare remains with the high among selected buildings.
Fig. 3.
The historical prevalence rate of COVID-19 in Montreal and of seven selected building types.
To compare the P.I. between all twenty-nine building types, we calculated the conditional and absolute P.I. of buildings on the worst day (May 3, 2020) with the largest daily new cases and prevalence rate. The number of daily new cases, total number of confirmed cases, total number of deaths, and the total number of recovered patients were 1652, 16,251, 1365, and 9123. The prevalence rate of the disease was around 4.03%. Fig. 3 shows the weekly prevalence rate, and this specific day is not plotted in this figure, but as it can be seen, the number of daily new cases is still increasing during the second wave and arrives close to the worst case.
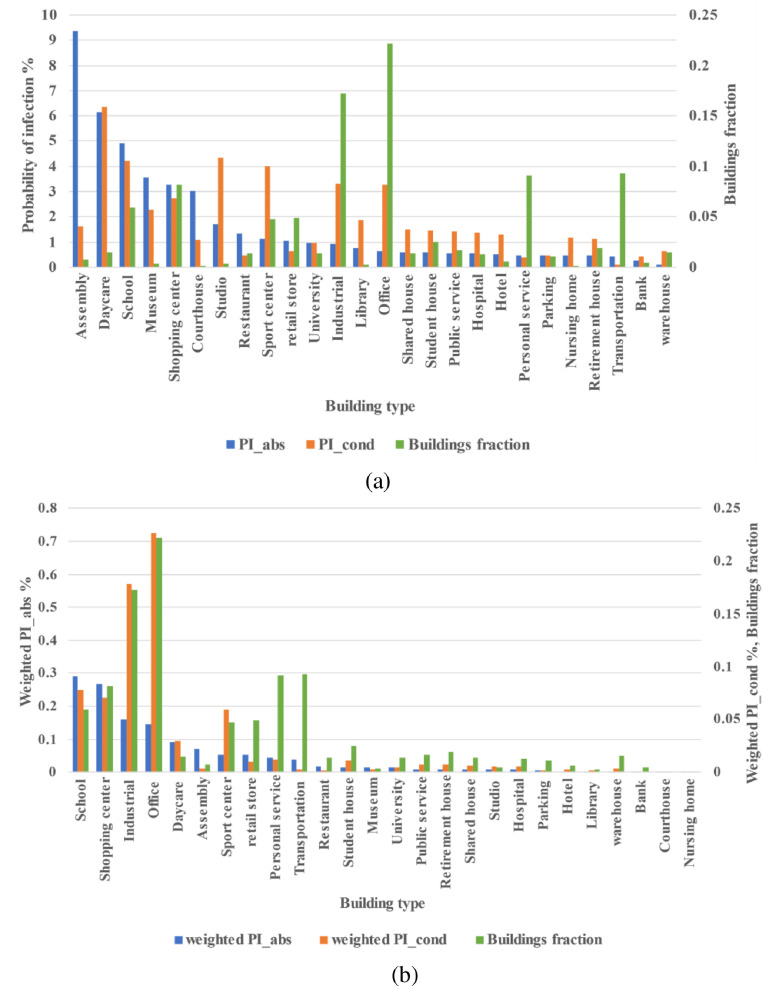
4.1.2. City-scale probability of infection of buildings
Fig. 4a shows the , , and the number of buildings in each type per total number of buildings. This figure could provide the information to find the vulnerable buildings to the COVID-19 airborne transmission. Buildings are sorted based on the value. The daycare, classroom, studio, sports center, industrial building, and office room are six buildings with the largest . All these buildings except the sports center are buildings with a long exposure time (> 4 h). Sports center shows high because of the increased quanta emission rate from heavy activities, exposure time and quanta emission rate are two dominant parameters for aerosol transmissions indoors.
Fig. 4.
a) Conditional and absolute P.I. of all building types on the worst day of the pandemic, b) weighted conditional and absolute P.I., and building type fraction on the worst day.
The is a function of the , the number of susceptible, and the prevalence rate. In this case, the prevalence rate is the same for all buildings. The number of susceptible people depends on the number of occupants in the room. Unlike the conditional P.I., an assembly building shows the highest because of the highest occupant density and susceptible people. Daycare, school, museum, shopping center, and courthouse are other buildings with large , due to high occupant density and .
The number of buildings per type is another important parameter when comparing different buildings. One building type can have a large , but if there are few buildings of this type in a city or urban area, it may not affect the city-scale risk. To consider its impact, we calculated the weighted probability of infection, which is the probability of infection multiplied by building type fraction, , which is the number of buildings with a specific type and is the total number of studied buildings. Most of the city buildings are residential buildings, but because our focus is on public buildings, residential buildings are removed from the analysis Fig. 4b shows the weighted conditional and absolute P.I. The school buildings offer the largest weighted because of large and building fraction. Shopping centers, industrial buildings, offices, and daycares are the next vulnerable buildings. Regarding the weighted , which is “person to person” transmission without considering the prevalence rate, office, industrial building, school, shopping center, sports center, and daycare are the most vulnerable buildings. The office building was the 6th vulnerable building considering only the , however, it is the most vulnerable building at the city scale because of the large number of office buildings in the city. Therefore, it is essential to focus on the buildings with the largest weighted P.I. to reduce the airborne infection risk.
As mentioned previously, airborne infection risk depends on building properties. The in Fig. 4b changes from 9.4% for an assembly room to 0.4% for a warehouse. Each person should determine the tolerable infection risk for himself/herself based on the situation, but some researchers have suggested a 0.1% infection risk as to the acceptable risk level (Jimenez & Peng, 2020). Results show that the probability of infection in all buildings on the worst day of the pandemic is higher than the tolerable risk level. Therefore, the existing standards, such as the required ventilation rate recommended by ASHRAE Standard 62.1., occupant density, and stay time, cannot provide a safe indoor environment. Therefore, one or several mitigation strategies should be applied to reduce the COVID-19 airborne infection risk for indoor spaces.
4.1.3. Reduced probability of infection and prevalence rate
Six different mitigation measures are studied for their impact on all building airborne infection risk, including wearing a face mask, reducing the stay time, reducing the number of people, using more outdoor air ventilation, upgrading the duct filter in the HVAC system, and using a portable air cleaner in the room. The baseline measure for comparison is no mask usage, minimum outdoor air ventilation, no duct filter and air cleaner, full occupancy, and standard stay time.
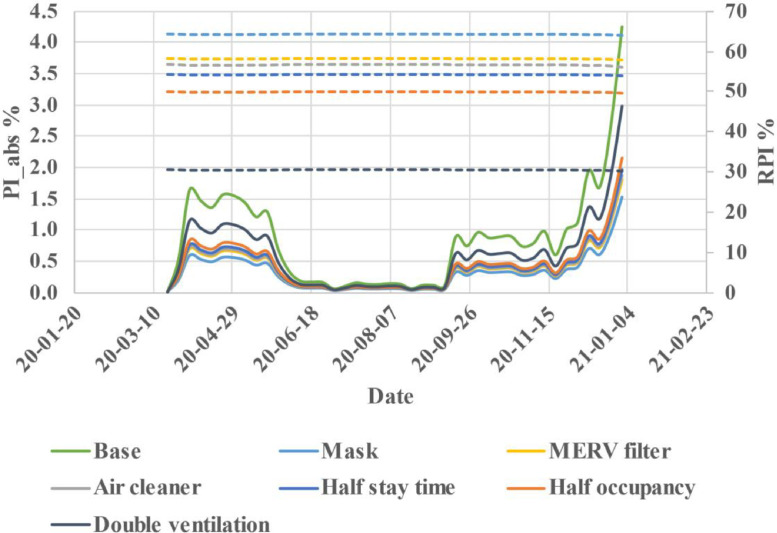
Before analyzing the impact of scenarios on all buildings, studying the RPI change with the prevalence rate is crucial. For this purpose, we calculated the classroom daily RPI from the beginning of the pandemic until January 6, 2021 (Fig. 5 ) at the city scale. We selected the school building because it is the most vulnerable building based on Fig. 4b. Results show that all strategies' effectiveness is almost constant with time and is independent of the prevalence rate. For a classroom, wearing a face mask by all occupants is the most effective strategy with 64% RPI. The next effective strategies are upgrading the duct filter to the MERV-13 filter, using a portable air cleaner with 480 CFM flow rate, half stay time, and half occupancy with 50%−58% RPI. Finally, doubling the outdoor air ventilation rate seems the least effective strategy with only 31% RPI.
Fig. 5.
Variation of PIabs (solid lines) and RPI (dashed lines) of school classroom for mitigation measures.
It should be noted that the duct filter RPI is the median of all school buildings in the city because the HVAC system airflow rate depends on the design condition and building properties. A study by Curtius et al. (2020) on using portable air cleaners in the classrooms show that a total air exchange rate of 5.7 h −1 reduces the airborne transmission by 80%, the equivalent air exchange rate of air cleaner modeled in this work is around 2.7 h −1, and the reduced infection risk is 53%. By using more air cleaners in the room, we can get more reduction. The conditional P.I. is not plotted in this figure because it is independent of the prevalence rate.
According to Fig. 5, the relative effectiveness, RPI, of all strategies seems independent of the prevalence rate. Therefore, to study the impact of mitigation measures on all building infection risk reduction, we calculated the RPI on the worst pandemic day. Energy impact is another important factor that must be considered. Some of the strategies can increase building energy consumption while reducing the infection risk. For example, more outdoor air ventilation rate in the winter needs more pre-heating and thus more energy. Upgrading duct filters with higher efficiency may increase fan power consumption, and a portable air cleaner also adds extra electricity usage. The number of daily cases in Montreal is rising during the winter; therefore, we calculated the increased building peak energy demand for the coldest period of winter 2019 by assuming the winter of 2020 would have similar weather.
4.1.4. Effectiveness of mitigation measures and energy impacts
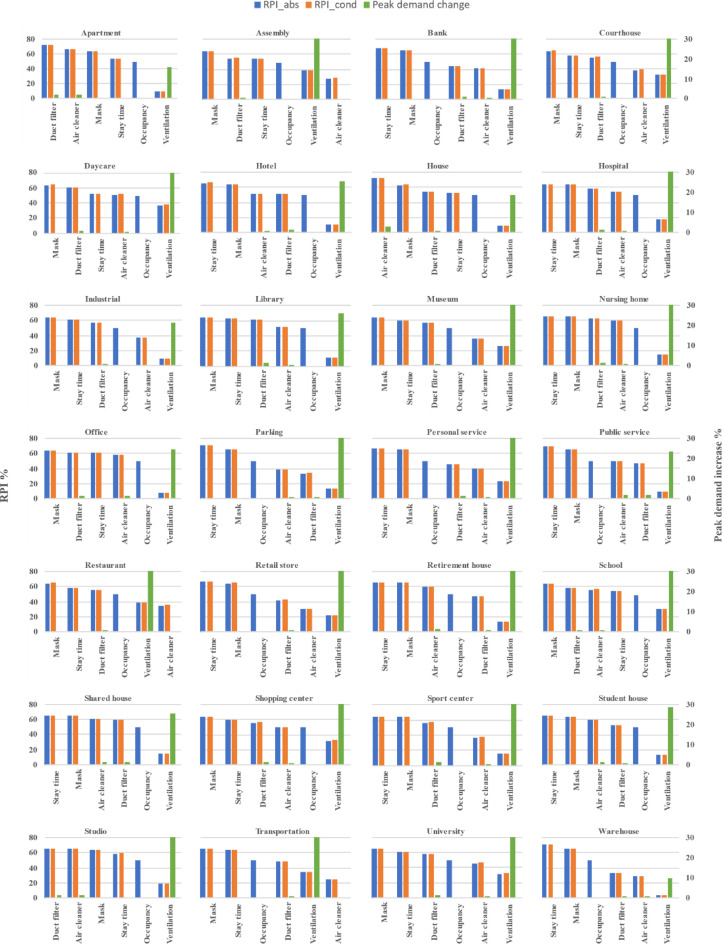
Fig. 6 represents the reduced conditional and absolute P.I.s and peak energy demands of all building types obtained by different mitigation measures. Strategies are sorted based on the effectiveness of reducing the of each building type. Comparing the reduced percentage of conditional and absolute infection risks shows that the reduction is around the same range for both P.I.s except for the half occupancy strategy.
Fig. 6.
Conditional and absolute RPI and peak load increase of strategies by building type.
Wearing a face mask or half stay time is the most effective strategy for reducing the infection risk in most buildings, except studio and residential buildings. The duct filter or using a portable air cleaner can be the most effective strategy in these buildings. On the other hand, double outdoor air ventilation rate is the least effective strategy in almost all the buildings except the assembly room, restaurant, and transportation environment. Using a portable air cleaner (480 CFM by default) is the least effective strategy in these three building types. Proper outdoor air ventilation by opening the windows or air intakes can reduce COVID-19 aerosol particle concentration and minimize infection risk. The existing ASHRAE recommended minimum outdoor air ventilation rate for indoor air quality purposes is not enough for providing a safe indoor space regarding the airborne transmission of COVID-19 aerosol respiratory. ASHRAE recommended increasing the outdoor air and reducing the HVAC system recirculation air to reduce the infection risk. Fig. 6 shows that a 100% increase in outdoor air ventilation rate is not as effective as the other strategies.
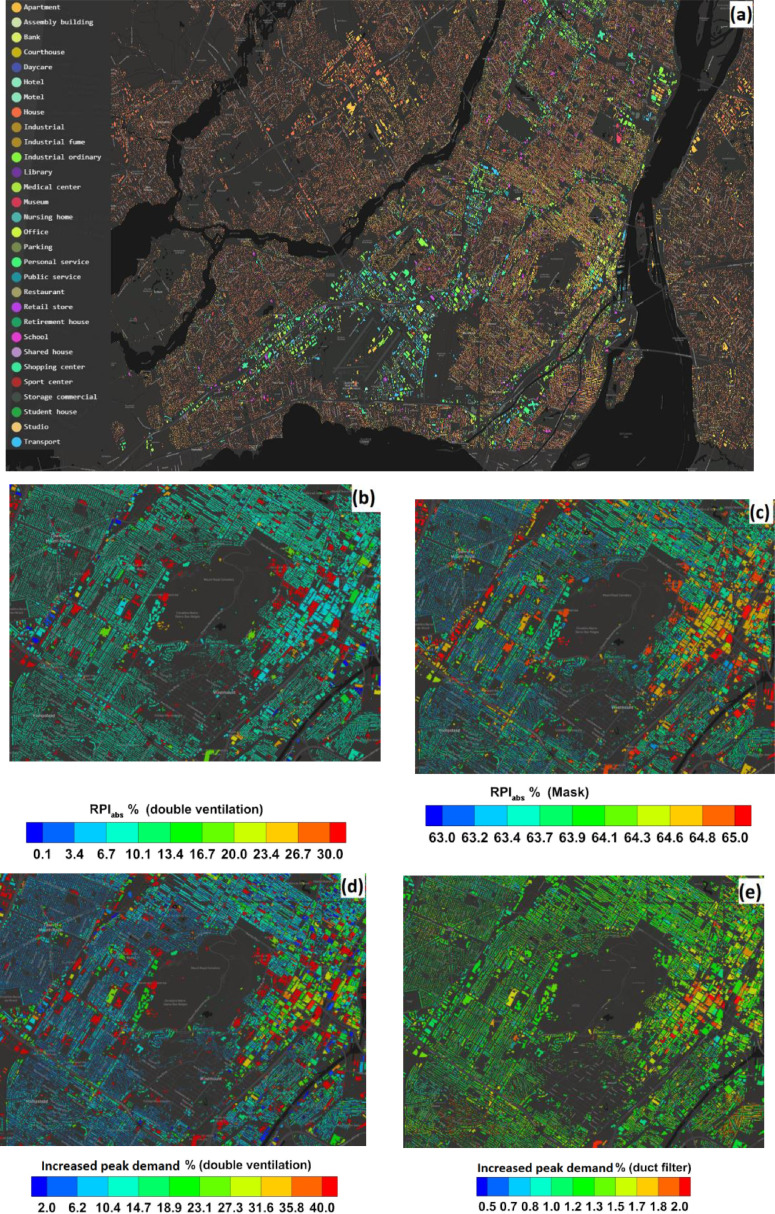
The distribution of buildings by usage type is plotted in Fig. 7 a. We plotted the of all downtown buildings for double outdoor air ventilation rate and wearing a face mask in Figs. 7b and 7c. This region includes diverse building types and covers almost all building types studied in this work. The RPI range for double outdoor ventilation rates is between 0.1%−35%, but wearing a face mask is always greater than 60%. Our analysis shows that four times outdoor air ventilation rate could provide a similar level reduction of infection risk as wearing a face mask in many cases, consistent with the result presented by Dai and Zhao (2020).
Fig. 7.
a) building distribution by type, b, c) RPI by doubling the minimum required outdoor air ventilation rate and wearing a face mask, d,e) Increased peak energy demand by double outdoor air ventilation and upgrading the duct filter.
The energy impacts were investigated by modeling the coldest period of Winter 2019 in the City of Montreal, Canada. The weather data are obtained from the High-Resolution Deterministic Prediction System (HRDPS) developed by environment and climate changa canada (ECCC) (Milbrandt et al., 2016). The integrated model of CityRPI and CityBEM could be potentially used for short-term forecasting of infection risk and energy consumption of buildings in the upcoming winters. CityBEM (Katal et al., 2019; ) is an urban building energy model covering all essential heat and mass transfer mechanisms for the calculations of building heating/cooling loads, energy consumption, and indoor air and buildings’ surface temperature. CityBEM solves transient heat balance equations for indoor air, wall, floor, roof, thermal mass, and windows and calculates each element's temperature. CityBEM models a Constant Air Volume (CAV) system for both heating and cooling. Heating/cooling energy consumption is estimated by calculating the building's heating/cooling load and modeling the HVAC system. This paper does not include the CityBEM model details for brevity, which can be found in the supplementary material to the submission.
The energy analysis shows that the increased peak energy demand for double outdoor air ventilation varies between 10%−60% depending on the building type. At the same time, it is less than 2% for upgrading duct filters (MERV 13) or using a portable air cleaner, and other strategies do not have an energy penalty. The results are plotted in Figs. 7d and 7e. The energy penalty using double outdoor air ventilation rate is between 2%−70% for all buildings while it is less than 2% for upgrading the duct filter. Considering both reduced infection risk and increased peak demand, we may conclude that double outdoor air ventilation is the least effective strategy. To get the same RPI as other strategies, such as wearing a face mask or half stay time, we need to increase the outdoor air ventilation rate further while unavoidably increasing the heating demand. As a result, this could build excessive pressures on the electricity grid and increase the chance of power outages in the city.
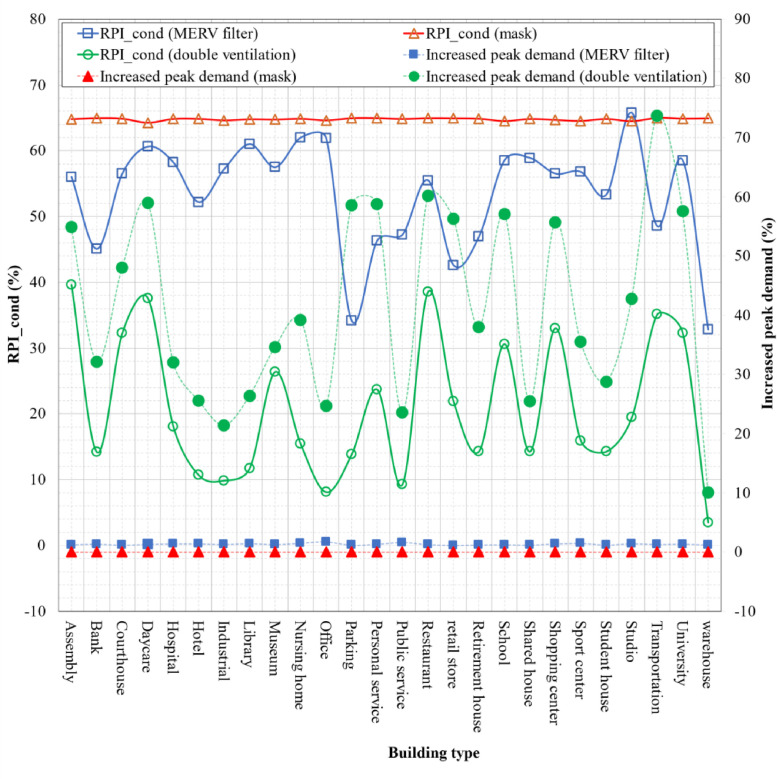
To summarize the result, the reduced and increased peak demand by the three most significant strategies, i.e., the double minimum required ventilation rate, wearing a face mask, and upgrading MERV filter in ducts are compared in Fig. 8 for all building types. According to the result, reduced infection risk obtained from wearing a face mask by all occupants is larger than two other strategies in all building types. It is also with minimum energy penalty, making it the most efficient strategy considering both infection risk and energy penalty. Furthermore, the upgrading duct filter in the HVAC system provides a larger RPI and lower increased peak demand in all buildings than the double outdoor air ventilation rate. Therefore, to reduce the infection risk and improve the ventilation condition, upgrading the duct filter is more effective than doubling the minimum required outdoor air ventilation rate.
Fig. 8.
Comparison of reduced and increased peak demand in all buildings obtained by doubling the minimum required outdoor air ventilation rate, upgrading the MERV filter in the HVAC system, and wearing a face mask by all occupants.
In conclusion, all studied measures can contribute to reducing the indoor aerosol infection risk of COVID-19. The effectiveness of these measures depends on building types and properties. Several strategies can be used together for more reduction in the risk and providing a safer indoor environment. We recommend wearing a face mask or reducing half of the stay time as the first and most effective strategy in all buildings based on the presented results. Reducing the stay time and occupant number can significantly reduce the risk, especially in crowded spaces and buildings where people often linger for a while. Regarding improving ventilation conditions to reduce infection risk, upgrading the duct filter of HVAC systems and using a portable air cleaner are more effective than merely increasing outdoor air ventilation rates. The former measures also have a lower energy penalty than the increased outdoor ventilation rate. On the other hand, air cleaners can be supplemental measures, but they cannot replace the ventilation required to maintain a healthy indoor environment. Keeping the required ventilation rate (e.g., some buildings operate at a “Pandemic Mode” by increasing ventilation rates while balancing energy costs) and applying supplemental measures, such as air purifiers, should be considered.
5. Conclusion and future work
This study developed CityRPI, a real-time web tool to monitor the current COVID-19 prevalence rate and evaluate building-specific mitigation measures in a city. We developed an archetype library based on standards and references to estimate different parameters for calculating building infection risk. For demonstration, we modeled Montreal City, calculated the infection risk of different building types in the city, and evaluated the impact of six mitigation strategies on reducing infection risk. Some strategies impact the energy consumption of a building, especially in the winter. We integrated CityRPI with the CityBEM model to calculate all building peak energy demand. The main conclusions are as follows:
-
1
On the day with the highest infection rate, the probability of infection in all buildings was higher than the tolerable infection risk. It shows that building standard operating conditions, such as the minimum ventilation rate recommended by ASHRAE, occupant density, and stay time, may not be sufficient. Stay time and quanta emission rate are the two dominant factors regarding the infection risk in buildings.
-
2
The weighted probability of infection shows that, on a whole city scale, school buildings are the most vulnerable in the city currently, considering the absolute P.I. Offices are the most vulnerable buildings, considering the conditional P.I., which is the “person-to-person” airborne transmission.
-
3
The mitigation study shows that wearing a face mask and half stay time are the most effective strategies for most buildings. Conversely, double outdoor air ventilation rate is the least effective strategy in many buildings, and the corresponding RPI is much lower than other strategies.
-
4
Double outdoor ventilation rate also significantly increases building peak heating demand in the winter. Therefore, this strategy may not be as effective as other strategies considering the infection risk and electricity consumption in the winter. Existing ventilation standards could be improved considering the airborne infection risk criteria for possible future pandemics.
-
5
The CityRPI website provides separate infection risk calculations and most to the least effective strategies for each building in the city. A user can change the input parameters and properties of his/her building to improve the calculation accuracy and get a more detailed analysis.
The calculation of infection risk involves many input parameters, and the results could be subject to the uncertainties of these parameters. Therefore, users are advised to focus on the relative values of the Reduction of Probability of Infection (RPI) and the limitations of the current study should be noted. The quanta emission rate is one of the major uncertain parameters in this work. This parameter depends on the activity type and other conditions. Also, the quanta emission rate can be significantly different in new variants of the virus. It is possible to add it as an input so that the generation rates of the different variants can be evaluated and the infection risk can be based on the most recent variant. Meanwhile, the ventilation rate is another critical parameter for estimating the risk levels, so it should be provided as accurately as possible by the user. The proposed tool is also based on the assumption that there is only one infector in the building, which may not be the case in reality. Once again, the estimated risk levels should always be interpreated on a relative basis, considering the uncertainties involved, such as the ventilation rates and the quanta generation rates. Any user should not use the proposed tool for the required mitigation measures to reach the desired level of risk, but instead, a relative reduction of the probability of infection should be used. As future work, a sensitivity analysis of the infection risk model becomes necessary to quantify these uncertainties' impacts on the results. It will help to determine which parameters are dominant and understand the uncertainties of the estimated values. On the other hand, although the COVID-19 Aerosol Transmission Estimator by Jimenez et al. (Jimenez, 2020) has been known for many researchers with multiple media coverages, such as National Geographic (Wei-Haas & K Elliott, 2020), the original study has not been published. The conditional probability in the work of Jimenez et al. (Jimenez, 2020) is the same as other studies of using the Well-Riley approach with one infector in the space, whereas we have derived their absolute probability and confirmed the mathematics, although it is not officially published yet. The same approach has been implemented in a new publication by the Canadian Committee on Indoor Air Quality for Addressing COVID-19 in Buildings (Sears, Wang & Katal, 2021), which have been peer-reviewed by the committee members including health and building experts and researchers. Meanwhile, the current infection risk model could underestimate the risk, especially for an event with many occupants and a high prevalence rate in a city. The conditional probability is based on the scenario that there is only one infector present in a room. With more people and higher prevalence, the chance of more than one infector in the same room could become high, which could be considered in a future study.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The research is supported by the Natural Sciences and Engineering Research Council (NSERC) of Canada through the Discovery Grants Program [#RGPIN-2018–06734] and the Advancing Climate Change Science in Canada Program [#ACCPJ 535986–18]. The authors acknowledged the valuable discussions with Dr. Zhe Peng at the University of Colorado Boulder, USA.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.scs.2022.103810.
Appendix. Supplementary materials
References
- Agarwal N., Meena C.S., Raj B.P., Saini L., Kumar A., Gopalakrishnan N., et al. Indoor air quality improvement in COVID-19 pandemic: Review. Sustainable Cities and Society. 2021;70 doi: 10.1016/J.SCS.2021.102942. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson E.L., Turnham P., Griffin J.R., Clarke C.C. Consideration of the aerosol transmission for COVID-19 and public health. Risk Analysis. 2020 doi: 10.1111/risa.13500. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- ANSI/ASHRAE . ASHRAE. 2019. ANSI/ASHRAE standard 62.1-2019, ventilation for acceptable indoor air quality. [Google Scholar]
- Asadi S., Bouvier N., Wexler A.S., Ristenpart W.D. Aerosol Science and Technology. 2020. The coronavirus pandemic and aerosols: Does COVID-19 transmit via expiratory particles? https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonanno, G., Morawska, L., & Stabile, L. (2020). Quantitative assessment of the risk of airborne transmission of SARS-CoV-2 infection: Prospective and retrospective applications. 145, 106112. [DOI] [PMC free article] [PubMed]
- Buonanno G., Stabile L., Morawska L. Estimation of airborne viral emission: Quanta emission rate of SARS-CoV-2 for infection risk assessment. Environment International. 2020;141 doi: 10.1016/j.envint.2020.105794. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne A.W., McEvoy D., Collins A.B., Hunt K., Casey M., Barber A., et al. BMJ open. 2020. Inferred duration of infectious period of SARS-CoV-2: Rapid scoping review and analysis of available evidence for asymptomatic and symptomatic COVID-19 cases. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu Z., Cheng M., Song M. What determines urban resilience against COVID-19: City size or governance capacity? Sustainable Cities and Society. 2021;75 doi: 10.1016/J.SCS.2021.103304. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- City of Montreal. (2020). Unités d’évaluation foncière - Jeu de données.
- Cook, B. (2020). Concordia web application suggests ways to reduce indoor coronavirus transmission - Montreal | Globalnews.ca.
- Crockett, D. (2020). New web tool assesses air quality in Montreal buildings to reduce spread of COVID-19 | CTV News.
- Curtius, J., Granzin, M., & Schrod, J. (2020). Testing mobile air purifiers in a school classroom: Reducing the airborne transmission risk for SARS-CoV-2. MedRxiv. https://doi.org/ 10.1101/2020.10.02.20205633.
- Dai H., Zhao B. Association of the infection probability of COVID-19 with ventilation rates in confined spaces. Building Simulation. 2020 doi: 10.1007/s12273-020-0703-5. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupuis, J. (2020). Concordia researchers build web-based tool to reduce risk of indoor SARS-CoV-2 transmission.
- Esri Canada. (2020). COVID-19 Canada.
- Feng Z., Cao S.J., Haghighat F. Removal of SARS-CoV-2 using UV+Filter in built environment. Sustainable Cities and Society. 2021;74 doi: 10.1016/J.SCS.2021.103226. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gammaitoni L., Nucci M.C. Using a mathematical model to evaluate the efficacy of TB control measures. Emerging Infectious Diseases. 1997 doi: 10.3201/eid0303.970310. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao X., Li Y., Leung G.M. Ventilation control of indoor transmission of airborne diseases in an urban community. Indoor and Built Environment. 2009 doi: 10.1177/1420326X09104141. [DOI] [Google Scholar]
- Gao X., Wei J., Li H., Xu P., Cowling B.J., Li Y. Building ventilation as an effective disease intervention strategy in a dense indoor contact network in an Ideal City. PLoS ONE. 2016;11(9):e0162481. doi: 10.1371/journal.pone.0162481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg E.M., Bingaman C.S., Perera S., Ranney M.L. MyCOVIDRisk app: Development and utilisation of a COVID-19 risk assessment and mitigation application. BMJ Innovations. 2021;7(2):363–367. doi: 10.1136/bmjinnov-2021-000672. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorelick N., Hancher M., Dixon M., Ilyushchenko S., Thau D., Moore R. Google earth engine: Planetary-scale geospatial analysis for everyone. Remote Sensing of Environment. 2017 doi: 10.1016/j.rse.2017.06.031. https://doi.org/ [DOI] [Google Scholar]
- Havers F.P., Reed C., Lim T., Montgomery J.M., Klena J.D., Hall A.J., et al. Seroprevalence of Antibodies to SARS-CoV-2 in 10 sites in the United States, March 23-May 12, 2020. JAMA Internal Medicine. 2020 doi: 10.1001/jamainternmed.2020.4130. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Jimenez J. Cooperative Institute for Research in Environmental Sciences at the University of Colorado Boulder; Boulder, CO: 2020. COVID-19 airborne transmission tool.https://cires.colorado.edu/news/covid-19-airborne-transmission-tool-available [Google Scholar]
- Jimenez, J., & Peng, Z. (2020). 2020_COVID-19_Aerosol_Transmission_Estimator - Google Sheets. https://tinyurl.com/covid-estimator.
- Kashem S.Bin, Baker D.M., González S.R., Lee C.A. Exploring the nexus between social vulnerability, built environment, and the prevalence of COVID-19: A case study of Chicago. Sustainable Cities and Society. 2021;75 doi: 10.1016/J.SCS.2021.103261. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasibhatla, P., Jimenez, J., Fay, J., Albright, E., & Pan, W. (2020). COVID Exposure Modeler.
- Katal A., Mortezazadeh M., Wang L.(Leon) Modeling building resilience against extreme weather by integrated CityFFD and CityBEM simulations. Applied Energy. 2019;250:1402–1417. doi: 10.1016/j.apenergy.2019.04.192. https://doi.org/ [DOI] [Google Scholar]
- Katal A., Mortezazadeh M., Wang L.(Leon) Urban microclimate and building thermal/energy modelling – from 3D city generation to dynamic urban simulations. Energy. 2020 (Manuscript submitted for publication) [Google Scholar]
- Kohanski M.A., Lo L.J., Waring M.S. Review of indoor aerosol generation, transport, and control in the context of COVID-19. International Forum of Allergy and Rhinology. 2020 doi: 10.1002/alr.22661. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lelieveld, J., Helleis, F., Borrmann, S., Cheng, Y., Drewnick, F., Haug, G. et al. (2020). Model Calculations of Aerosol Transmission and Infection Risk of COVID-19 in Indoor Environments. MedRxiv. https://doi.org/ 10.1101/2020.09.22.20199489. [DOI] [PMC free article] [PubMed]
- Li Y., Qian H., Hang J., Chen X., Cheng P., Ling H., et al. Probable airborne transmission of SARS-CoV-2 in a poorly ventilated restaurant. Building and Environment. 2021 doi: 10.1016/j.buildenv.2021.107788. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machado C., Melina Nassif Mantovani Ribeiro D., Backx Noronha Viana A. Public health in times of crisis: An overlooked variable in city management theories? Sustainable Cities and Society. 2021;66 doi: 10.1016/J.SCS.2020.102671. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Microsoft. (2019a). Computer generated building footprints for the United States: Microsoft/USBuildingFootprints.
- Microsoft. (2019b). GitHub - microsoft/CanadianBuildingFootprints: Computer generated building footprints for Canada.
- Milbrandt J.A., Bélair S., Faucher M., Vallée M., Carrera M.L., Glazer A. The pan-canadian high resolution (2.5 km) deterministic prediction system. Weather and Forecasting. 2016 doi: 10.1175/WAF-d-16-0035.1. https://doi.org/ [DOI] [Google Scholar]
- Miller, S.L., .Nazaroff, W.W., .Jimenez, J.L., .Boerstra, A., Buonanno, G., Dancer, S.J. et al. (2020). Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. MedRxiv. https://doi.org/ 10.1101/2020.06.15.20132027. [DOI] [PMC free article] [PubMed]
- Morawska L., Allen J., Bahnfleth W., Bluyssen P.M., Boerstra A., Buonanno G., et al. A paradigm shift to combat indoor respiratory infection. Science (New York, N.Y.) 2021;372(Issue 6543):689–691. doi: 10.1126/science.abg2025. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Morawska L., Cao J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environment International. 2020 doi: 10.1016/j.envint.2020.105730. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Tang J.W., Bahnfleth W., Bluyssen P.M., Boerstra A., Buonanno G., et al. How can airborne transmission of COVID-19 indoors be minimised? Environment International. 2020 doi: 10.1016/j.envint.2020.105832. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York Times. (2020). GitHub - nytimes/covid-19-data: An ongoing repository of data on coronavirus cases and deaths in the U.S..
- Nicas M., Nazaroff W.W., Hubbard A. Toward understanding the risk of secondary airborne infection: Emission of respirable pathogens. Journal of Occupational and Environmental Hygiene. 2005 doi: 10.1080/15459620590918466. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parhizkar, H., Van Den Wymelenberg1, K., Haas, C., & Corsi, R. (2020). SAFEAIRSPACES ESTIMATOR | Safeairspaces.
- Peng Z., Rojas A.L.P., Kropff E., Bahnfleth W., Buonanno G., Dancer S.J., et al. Practical Indicators for Risk of Airborne Transmission in Shared Indoor Environments and Their Application to COVID-19 Outbreaks. Environmental Science & Technology. 2022;56(2):1125–1137. doi: 10.1021/acs.est.1c06531. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Peng Zhe, Jimenez J.L. Exhaled CO2as a COVID-19 infection risk proxy for different indoor environments and activities. Environmental Science and Technology Letters. 2021;8(5):392–397. doi: 10.1021/acs.estlett.1c00183. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Rainville, S. (2020). Reducing the risk of COVID-19 indoor transmission.
- Riley E.C., Murphy G., Riley R.L. Airborne spread of measles in a suburban elementary school. American Journal of Epidemiology. 1978 doi: 10.1093/oxfordjournals.aje.a112560. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Sears, M., Wang, L.(Leon), & Katal, A. (2021). Addressing COVID-19 in Buildings | Module 15 | iaqresource.ca.
- Sha H., Zhang X., Qi D. Optimal control of high-rise building mechanical ventilation system for achieving low risk of COVID-19 transmission and ventilative cooling. Sustainable Cities and Society. 2021;74 doi: 10.1016/J.SCS.2021.103256. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen J., Kong M., Dong B., Birnkrant M.J., Zhang J. A systematic approach to estimating the effectiveness of multi-scale IAQ strategies for reducing the risk of airborne infection of SARS-CoV-2. Building and Environment. 2021;200 doi: 10.1016/j.buildenv.2021.107926. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva J.C.S., de Lima Silva D.F., Delgado Neto A.de S., Ferraz A., Melo J.L., Ferreira Júnior N.R., et al. A city cluster risk-based approach for Sars-CoV-2 and isolation barriers based on anonymized mobile phone users’ location data. Sustainable Cities and Society. 2021;65 doi: 10.1016/J.SCS.2020.102574. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun C., Zhai Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustainable Cities and Society. 2020;62 doi: 10.1016/j.scs.2020.102390. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang S., Mao Y., Jones R.M., Tan Q., Ji J.S., Li N., et al. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environmental International. 2020 doi: 10.1016/j.envint.2020.106039. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- University of Cambridge. (2020). Airborne.cam - evaluate COVID-19 risk of infection from airborne transmission.
- US Environmental Protection Agency . U.S. Environmental Protection Agency; 2011. Exposure factors handbook: 2011 edition. http://doi.org/EPA/600/R-090/052F. [Google Scholar]
- Van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. New England Journal of Medicine. 2020;382(16):1564–1567. doi: 10.1056/nejmc2004973. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, L.(Leon), Katal, A., & Albettar, M. (2020). CityRPI for Indoor Airborne Transmission.
- Weber P., Haklay M.(Muki). OpenStreetMap: User-Generated Street Maps. IEEE Pervasive Computing. 2008 doi: 10.1109/MPRV.2008.80. https://doi.org/ [DOI] [Google Scholar]
- Wei-Haas M., Elliott K. Measure the risk of airborne COVID-19 in your office, classroom, or bus ride. National Geographic. 2020 https://www.nationalgeographic.com/science/article/how-to-measure-risk-airborne-coronavirus-your-office-classroom-bus-ride-cvd [Google Scholar]
- WHO. (2020). Coronavirus disease (COVID-19).
- World Health Organization, W. (2020). Coronavirus (COVID-19) events as they happen. https://Www.Who.Int/Emergencies/Diseases/Novel-Coronavirus-2019/Events-As-They-Happen.
- Zhang J. Integrating IAQ control strategies to reduce the risk of asymptomatic SARS CoV-2 infections in classrooms and open plan offices. Science and Technology for the Built Environment. 2020 doi: 10.1080/23744731.2020.1794499. https://doi.org/ [DOI] [Google Scholar]
- Zhang R., Li Y., Zhang A.L., Wang Y., Molina M.J. Proceedings of the National Academy of Sciences of the United States of America. 2020. Identifying airborne transmission as the dominant route for the spread of COVID-19. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.