Abstract
PURPOSE
The aim of this study was to investigate shade changes in fully- and pre-crystalized CAD-CAM lithium disilicate crowns after the required and additional firing processes.
MATERIALS AND METHODS
One hundred and five crowns of shade A1 with high translucency were milled out of CAD-CAM lithium disilicate blocks and categorized as follows (n = 15): (1) restorations fabricated from Straumann n!ce with no additional sintering process; (2) restorations fabricated from Straumann n!ce with one additional sintering process; (3) restorations fabricated from Straumann n!ce with two additional sintering processes; (4) restorations fabricated from Amber Mill with one sintering process; (5) restorations fabricated from Amber Mill with two sintering processes; (6) restorations fabricated from IPS e.max CAD with one sintering process; (7) restorations fabricated from IPS e.max CAD with two sintering processes. All restorations were evaluated with a color imaging spectrophotometer.
RESULTS
All restorations presented some color alteration from the original shade both after a single and after two firing processes.
CONCLUSION
The required and additional sintering processes for restorations fabricated with chairside CAD-CAM lithium disilicate blocks cause an alteration of the original shade selected. Shade A1 high translucency restorations tend to change to a more yellowish B1 shade after a sintering process.
Keywords: Prosthodontics, Ceramics, Crowns, Dentistry, Esthetics
INTRODUCTION
The use of computer-aided design and computer-aided manufacturing (CAD-CAM) technologies in dentistry has greatly increased during the last decade because they allow the clinician to fabricate high-quality restorations accurately, efficiently, and without errors, unlike conventional methods.1 Currently, CAD-CAM technology is available in chairside systems for clinics, which makes it possible to fabricate the final restoration in a single visit, saving the time and effort required to take conventional impressions and fabricate provisional restorations.2
A report in 2014 by one of the largest dental laboratories in the US reported that 80.2% of restorations were all-ceramic, compared to 23.9% in 2008.3 A practice-based research study in 2016 reported that 52% of clinicians would choose all-ceramic restorations, with 32% choosing zirconia and 21% reinforced ceramic materials, such as lithium disilicate, even for posterior teeth.4 Lithium disilicate is now a popular material, but it was first introduced as a core material in the late 1990s and the first version was obtained by heat-pressing ingots, similar to the lost-wax technique used for restorations fabricated from metal alloys.5 Lithium disilicate for CAD-CAM systems was introduced in 2006 as pre-crystallized ceramic blocks (IPS e.max CAD, Ivoclar Vivadent, Schaan, Liechtestein), and since then other manufacturers have marketed similar materials with unique additional characteristics, such as the ability to vary their translucency within a single block through different firing temperatures (Amber Mill; Hass Bio, Gangwon-do, Korea).6 Those materials are milled in a pre-crystalized state and the restoration becomes fully-crystalized after the firing process.7 A fully-crystallized lithium disilicate (Straumann n!ce; Straumann, Basel, Switzerland) was recently introduced, and this material is innovative because the conventional in-office sintering process is not mandatory, although extra firing processes are possible.8
Although manufacturers fabricating lithium disilicate claim that it has excellent optical properties after only milling and polishing, or the required firing process, some adjustments such as staining or adding material in contact areas may be necessary prior to final cementation, and those adjustments necessitate additional firing processes in the clinic.9 However, no studies have evaluated shade variation due to such additional firing processes in fully- and pre-crystalized CAD-CAM lithium disilicate restorations. Therefore, the aim of this study is to evaluate the color stability of fully- and pre-crystalized CAD-CAM lithium disilicate anterior crowns after required and additional sintering processes. The first null hypothesis is that the shade of pre- and fully-crystallized chairside CAD-CAM lithium disilicate restorations will not differ from the original shade A1 after firing. The second null hypothesis is that restorations made with fully-crystallized lithium disilicate (Straumann® n!ce®) will show no difference from the original shade before undergoing any sintering process and after undergoing one or two optional sintering processes. The third null hypothesis is that crowns fabricated with the novel pre-crystallized lithium disilicate (Amber® Mill) will show no difference from the original shade A1 after undergoing one or two sintering processes. The fourth null hypothesis is that crowns manufactured with the conventional pre-sintered lithium disilicate (IPS e.max CAD) will show no difference from the original shade A1 after undergoing one or two sintering processes.
MATERIALS AND METHODS
A typodont (1560 Dentoform; Columbia Dentoform, Lancaster, PA, USA) maxillary left central incisor in ivory color was prepared for an all-ceramic crown with 1.5 mm incisal reduction and 1.0 mm chamfer. The prepared tooth and the typodont were scanned with a chair-side intra-oral scanner (Primescan; Dentsply Sirona, Charlotte, NC, USA) and a digital crown design with ideal contours was provided by the software. A total of 105 crowns were milled out (MCXL Milling Unit; Dentsply Sirona, Charlotte, NC, USA) of different brands of lithium disilicate blocks (shade: A1 high translucency) as follows: (1) restorations fabricated from Straumann n!ce (fully-crystallized block) with no additional sintering process (n!0); (2) restorations fabricated from Straumann n!ce with one additional sintering process (n!1); (3) restorations fabricated from Straumann n!ce with two additional sintering processes (n!2); (4) restorations fabricated from Amber Mill (pre-crystalized block) with one sintering process (Am1); (5) restorations fabricated from Amber Mill with two sintering processes (Am2); (6) restorations fabricated from IPS e.max CAD (pre-crystallized block) with one sintering process (Em1); and (7) restorations fabricated from IPS e.max CAD with two sintering processes (Em2).
The sintering process for all ceramics was carried out with a ceramic and crystallization furnace for dentistry (Programat CS2; Ivoclar Vivadent) with the firing process recommended by each manufacturer: for IPS e.max CAD, the standard cycle (P1 Cycle) at 403℃ standby temperature for 24 minutes; for Amber Mill, a customized sintering cycle was used following the manufacturer’s recommendation with Standard Mode at 400℃ for 30 minutes; and Straumann n!ce was also sintered with a customized sintering cycle following the manufacturer’s recommendation at 450℃ base temperature for 25 minutes. All restorations were polished with a lithium polishing system (IPS e.max Chairside Adjustment & Polishing System; Brasseler, Savannah, GA, USA).
Each of the restorations was seated on the typodont tooth without any resin cement or trying-paste and then a color imaging spectrophotometer (Spectroshade Micro II; Oxnard, CA, USA) was used to obtain one frontal image of the restoration. The outline of the facial surface was delimited following the borders but held 1.0 mm away from the gingiva as required by the software, and a map of the shades was obtained for each restoration (Fig. 1). The shade map for each crown was evaluated with a software (The Image Color Extract PHP; Kepler Gelotte) and the percentage of every shade present was obtained. Statistical analysis was performed with a non-parametric test to analyze shade differences among the groups. The Kruskal-Wallis test was performed to evaluate the distribution of shades across the groups.
Fig. 1. The shades displayed in each group.
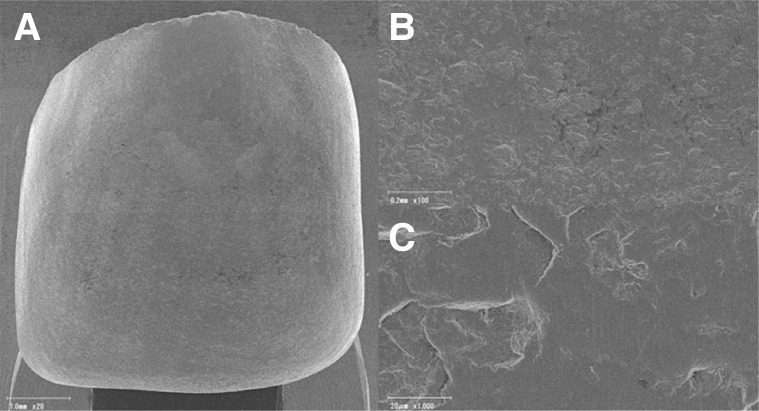
The restorations were observed with field-emission scanning electron microscopy (ERA 8800FE; Elionix, Tokyo, Japan). A thin coat of gold was applied to the specimens in a sputter coater (Quick Coater Type SC-701; Sanyu Electron, Tokyo, Japan) to provide electrical conductivity.
RESULTS
All the crowns showed a certain amount of shade modification. The initial shade A1 is reddish-brown, but digital images revealed a significant presence of shade B1 or B2, both of which are more reddish-yellow. The results are presented in Figure 1, and representative images are shown in Figure 2.
Fig. 2. Representative spectrophotometer images showing the shades visible on the crowns.
Most of the groups showed some percentage of B1 shade, except for group 1 (n!0), which showed some percentage of B2 shade. Group 5 (Am2) showed the highest amount of B1, followed by group 4 (Am1) and group 2 (n!1). Group 1 (n!0) maintained the largest area of A1 shade in the restoration. Group 2 (n!1) and Group 3 (n!2) showed a statistically significant difference from the original shade after undergoing one and two optional firing processes. Group 6 (Em1) and 7 (Em2) were very similar, with a high amount of A1 shade. Group 5 (Am2) showed the highest statistically significant difference from the original shade A1.
Representative SEM observations of the surfaces of the prepared restorations at different magnifications (a: ×20, b: ×100 and c: ×1,000) are shown in Figures 3, 4, 5, 6, 7, 8, and 9. SEM observation of Group 1 (n!0) showed an irregular surface with some scratches. The surfaces of Group 2 (n!1) and Group 3 (n!2) were clearly different from Group 1, and the surfaces appeared quite smooth at low magnifications (×20). In addition, some voids were observed in Group 2 in the higher magnification images, but the number of voids in Group 3 were clearly reduced by the second additional sintering. In Groups 4 (Am1) and 5 (Am2), smooth surfaces were observed in both groups at lower magnifications, but the characteristics of the surface were different. In the higher magnification images, smaller pores were observed in Group 4 than in Group 5. In Groups 6 (Em1) and 7 (Em2), although some voids were observed in both groups, similar smooth surfaces were observed.
Fig. 3. SEM image of surface of restoration fabricated with Straumann n!ce with no additional sintering process. (A) 20× magnification, (B) 100× magnification and (C) 1000× magnification.
Fig. 4. SEM images of surface of restoration fabricated with Straumann n!ce with one additional sintering process. (A) 20× magnification, (B) 100× magnification and (C) 1000× magnification.
Fig. 5. SEM image of surface of restoration fabricated with Straumann n!ce with two additional sintering processes. (A) 20× magnification, (B) 100× magnification and (C) 1000× magnification.
Fig. 6. SEM image of surface of restoration fabricated with Amber Mill with one sintering process. (A) 20× magnification, (B) 100× magnification and (C) 1000× magnification.
Fig. 7. SEM image of surface of restoration fabricated with Amber Mill with two sintering processes. (A) 20× magnification, (B) 100× magnification and (C) 1000× magnification.
Fig. 8. SEM image of surface of restoration fabricated with IPS e.max CAD with one sintering process. (A) 20× magnification, (B) 100× magnification and (C) 1000× magnification.
Fig. 9. SEM image of surface of restoration fabricated with IPS e.max CAD with two sintering processes. (A) 20× magnification, (B) 100× magnification and (C) 1000× magnification.
DISCUSSION
A dentist usually faces the challenge of replicating the color of natural teeth, and the goal for restorations in the esthetic zone is to achieve optical, biological, and morphological esthetic results that are accepted by patients.10 Color replication is a considered process that includes shade selection followed by shade duplication. Shade can be chosen through visual assessment or by using digital devices.11 Although clinicians usually perform a visual assessment of color using a prefabricated shade guide, this process has been reported in the literature to be inconsistent and unreliable.12 It can be influenced by the clinician’s interpretation and environmental factors such as lighting conditions, level of experience, fatigue of the human eye, aging and emotion.13 Therefore, novel technology can help secure more consistent and accurate shade selection. Spectrophotometers have been demonstrated to be very accurate for tooth color matching.14 However, there are few spectrophotometers for dentistry available on the market and they evaluate the shade of teeth or ceramic in the gingival, middle, and incisal thirds, and have black and white displays. However, the spectrophotometer used in this study provides high digital resolution colored images that evaluate every area of the tooth or prosthesis to obtain a full shade map.
Previous studies evaluating lithium disilicate restorations have found acceptable color stability after aging and coffee staining processes.15 Unfortunately, color modification after the sintering process has been little investigated to date. One study evaluated the effect of the sintering process of a conventional CAD-CAM lithium disilicate (IPS e.max CAD) on veneer restorations over the course of 3 sintering processes, and it was found that repeated sintering processes significantly influenced the color.16 That study was, however, limited by the use of a traditional non-color spectrophotometer that splits the restoration into three areas for measurement; the shade of thin restorations such as veneer may be strongly affected by factors such as the color of the background holding the veneer and the type and amount of ambient light. As noted earlier, this study used a novel color digital spectrophotometer that can produce a shade map of the entire surface, and the restoration was a traditional full coverage crown with 1.5 mm incisal thickness and 1.0 mm chamfer, thus avoiding any issues due to the thinness of restorations. We also evaluated a conventional (IPS e.max CAD) and two novel fully- and pre-crystalized materials (Straumann n!ce and Amber Mill), meaning that the results of the present study should be more broadly informative. For this study, the thickness on the facial surface of the crown was 1.0 mm. Previous studies have shown that ceramic restorations with thicknesses of 1.0 mm show no clinically perceptible color changes when used with different shades of cement, so it was not necessary to measure the interaction of cement shade and restoration shade.17,18,19
If the shade of chair-side CAD-CAM lithium disilicate remained stable through the fabrication process, the clinician might be able to produce more predictable esthetic restorations. However, the color deviation from A1 was significant among all the brands tested, except for the fully-crystalized lithium disilicate (Straumann n!ce) when it is not sintered in the clinic, so the first null hypothesis can be partially rejected. In the majority of the groups, a considerable amount of shade B1 appeared in the spectrophotometer image, except for Group 1 (n!0), which is a fully-crystalized material and was not sintered during the experiment. The restorations fabricated from fully-crystalized lithium disilicate presented a small amount of shade B2, but after one sintering process, shade B1 became the major shade, and after the second optional sintering process, A1 shade became the more prevalent shade, followed by B1. Therefore, the second null hypothesis can be rejected. The novel pre-crystalized lithium disilicate (Amber Mill) saw a considerable reduction in the amount of shade A1, leaving shade B1 covering the majority of the surface, after both one and two firing processes, and thus the third null hypothesis can also be rejected. The results of SEM observations of Groups 2-5 suggest that the increase of the amount of B1 shade may be related to the bigger voids and pores. Those defects may induce light scattering, which would alter the shade. The conventional pre-crystalized lithium disilicate (IPS e.max CAD) showed no statistically significant difference from the original shade A1 after undergoing one or two sintering processes, and SEM images of Group 6 and 7 were quite similar, thus the fourth null hypothesis was not rejected. The resulting SEM images concur with a previous study evaluating the mechanical properties of lithium disilicate after multiple firing processes, in which the SEM images showed that repeated firing process for IPS e.max CAD cause the complex mesh structure to disappear and be replaced by a dense and porous surface.20 Our SEM images also displayed more porosities for IPS e.max CAD, Amber Mill, and Straumann n!ce after repeating firing processes.
Further studies might include using a color digital spectrophotometer to evaluate the color changes in a ceramic crown after several sintering process in comparison with a natural tooth. Our study did not evaluate color stability on sintering crowns that had received stains, which may be an interesting topic for future studies. Additionally, it would be valuable to evaluate other chair-side CAD-CAM materials in the same way.
CONCLUSION
Spectrophotometer evaluation demonstrated that additional sintering processes cause significant changes in shade for restorations fabricated from fully-sintered and novel pre-crystalized CAD-CAM lithium disilicate, unlike the conventional pre-crystalized equivalent. Restorations fabricated with shade A1 shifted towards shade B1 after one or two sintering processes. Restorations fabricated from fully-crystalized lithium disilicate blocks without a sintering process displayed mainly A1 shade, but some areas showed B2 shade.
ACKNOWLEDGEMENTS
Authors would like to thank Darcy Lanz DT for her laboratory support, Dr. Curt Bay for the statistical analysis support and Dr. Ann Spolarich for her guidance.
Footnotes
This research was supported by the ATSU Warner/Fermaturo Research Grant (#560-745).
References
- 1.Tsujimoto A, Barkmeier WW, Takamizawa T, Latta MA, Miyazaki M. Influence of thermal cycling on flexural properties and simulated wear of computer-aided design/computer-aided manufacturing resin composites. Oper Dent. 2017;42:101–110. doi: 10.2341/16-046-L. [DOI] [PubMed] [Google Scholar]
- 2.Jurado CA, Tsujimoto A, Watanabe H, Villalobos-Tinoco J, Garaicoa JL, Markham MD, Barkmeier WW, Latta MA. Chair-side CAD/CAM fabrication of a single-retainer resin bonded fixed dental prosthesis: a case report. Restor Dent Endod. 2020;45:e15. doi: 10.5395/rde.2020.45.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christensen GJ. Is the rush to all-ceramic crowns justified? J Am Dent Assoc. 2014;145:192–194. doi: 10.14219/jada.2013.19. [DOI] [PubMed] [Google Scholar]
- 4.Makhija SK, Lawson NC, Gilbert GH, Litaker MS, McClelland JA, Louis DR, Gordan VV, Pihlstrom DJ, Meyerowitz C, Mungia R, McCracken MS National Dental PBRN Collaborative Group. Dentist material selection for single-unit crowns: findings from the National Dental Practice-Based Research Network. J Dent. 2016;55:40–47. doi: 10.1016/j.jdent.2016.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Albakry M, Guazzato M, Swain MV. Influence of hot pressing on the microstructure and fracture toughness of two pressable dental glass-ceramics. J Biomed Mater Res B Appl Biomater. 2004;71:99–107. doi: 10.1002/jbm.b.30066. [DOI] [PubMed] [Google Scholar]
- 6.Yin R, Jang YS, Lee MH, Bae TS. Comparative evaluation of mechanical properties and wear ability of five CAD/CAM dental blocks. Materials (Basel) 2019;12:2252. doi: 10.3390/ma12142252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stawarczyk B, Mandl A, Liebermann A. Modern CAD/CAM silicate ceramics, their translucency level and impact of hydrothermal aging on translucency, Martens hardness, biaxial flexural strength and their reliability. J Mech Behav Biomed Mater. 2021;118:104456. doi: 10.1016/j.jmbbm.2021.104456. in press. [DOI] [PubMed] [Google Scholar]
- 8.Preis V, Hahnel S, Behr M, Rosentritt M. In vitro performance and fracture resistance of novel CAD/CAM ceramic molar crowns loaded on implants and human teeth. J Adv Prosthodont. 2018;10:300–307. doi: 10.4047/jap.2018.10.4.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kanat-Ertürk B. Color stability of CAD/CAM ceramics prepared with different surface finishing procedures. J Prosthodont. 2020;29:166–172. doi: 10.1111/jopr.13019. [DOI] [PubMed] [Google Scholar]
- 10.Kurt M, Bankoğ lu Güngör M, Karakoca Nemli S, Turhan Bal B. Effects of glazing methods on the optical and surface properties of silicate ceramics. J Prosthodont Res. 2020;64:202–209. doi: 10.1016/j.jpor.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 11.Wee AG. Description of color, color replication process and esthetics. Contemporary Fixed Prosthodontics. 4th ed. St. Louis, MO: Mosby; 2006. pp. 709–732. [Google Scholar]
- 12.Cal E, Sonugelen M, Guneri P, Kesercioglu A, Kose T. Application of a digital technique in evaluating the reliability of shade guides. J Oral Rehabil. 2004;31:483–491. doi: 10.1111/j.1365-2842.2004.01197.x. [DOI] [PubMed] [Google Scholar]
- 13.Berns RS, Billmeyer FW, Saltzman M. Billmeyer and Saltzman’s principles of color technology. 4th ed. Hoboken, NJ: John Wiley & Sons; 2019. pp. 13–20. [Google Scholar]
- 14.Paul SJ, Peter A, Rodoni L, Pietrobon N. Conventional visual vs spectrophotometric shade taking for porcelain-fused-to-metal crowns: a clinical comparison. Int J Periodontics Restorative Dent. 2004;24:222–231. [PubMed] [Google Scholar]
- 15.Acar O, Yilmaz B, Altintas SH, Chandrasekaran I, Johnston WM. Color stainability of CAD/CAM and nanocomposite resin materials. J Prosthet Dent. 2016;115:71–75. doi: 10.1016/j.prosdent.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 16.Cui H, Jia Y, Shaofeng M, Biyun G. Effect of repeated sintering and variations in thickness on the color and microstructure of dental lithium disilicate-based glass ceramic veneers. West China J Stomatol. 2017;35:389–393. doi: 10.7518/hxkq.2017.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turgut S, Bagis B. Effect of resin cement and ceramic thickness on final color of laminate veneers: an in vitro study. J Prosthet Dent. 2013;109:179–186. doi: 10.1016/S0022-3913(13)60039-6. [DOI] [PubMed] [Google Scholar]
- 18.Kim SJ, Woo JM, Jo CW, Park JH, Kim SK, Kahm SH. Color changes of ceramic veneers following glazing with respect to their composition. J Adv Prosthodont. 2019;11:16–22. doi: 10.4047/jap.2019.11.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Q. Effects of Luting Composites on the Resultant Colors of Ceramic Veneers to Intended Shade Tab. J Prosthodont. 2019;28:327–331. doi: 10.1111/jopr.12585. [DOI] [PubMed] [Google Scholar]
- 20.Ozdogan A, Ozdemir H. Effects of multiple firing processes on the mechanical properties of lithium disilicate glass-ceramics produced by two different production techniques. J Prosthet Dent. 2021;125:527.e1–527.e7. doi: 10.1016/j.prosdent.2020.10.016. [DOI] [PubMed] [Google Scholar]