Abstract
PURPOSE
Mandibular flexure is a crucial phenomenon that may affect the success of rigid bilateral mandibular prosthetic treatment. The aim of this study was to determine the amount of median mandibular flexure (MMF) that occurs during mouth opening from anterior to posterior mandible in seven different regions, in different age and gender groups of both dentulous and edentulous subjects, using an intraoral digital scanner.
MATERIALS AND METHODS
In this study, the mandibular arch of 56 dentulous and 35 edentulous individuals were scanned with an intraoral scanner at both the minimum mouth opening (MnMO) and the maximum mouth opening (MxMO). MMF values were calculated by subtracting the distance value at the MxMO from the distance between the reference points at the MnMO at seven different mandibular regions of dentulous and edentulous subjects. In addition, the left and right side MMF values were measured. All data were analyzed statistically (α = .05).
RESULTS
MMF value increased linearly from anterior to posterior mandible in both dentulous and edentulous individuals. The differences in MMF values were not statistically significant according to side (left/right), age, or gender (P > .05). No significant differences were found between the mean MMF values of the same region in both dentulous and edentulous individuals (P > .05).
CONCLUSION
MMF was seen in different regions of the mandibles of both edentulous and dentulous individuals measured at the MxMO. Mandibular flexure should be considered for the success and prognosis of the long-span and rigid prostheses.
Keywords: Deformation, Flexion, Lateral pterygoid muscle, Mandibular flexure, Mouth opening
INTRODUCTION
Mandibular flexure is a multifactorial phenomenon that occurs immediately and simultaneously with mandibular movements and causes changes in the shape of the mandible.1 Researchers have shown that the lateral pterygoid muscles (LPMs) contract and the condyles are pulled towards each other during the opening and protrusion movements of the mandible.2,3 Apart from the LPMs, the mylohyoid, platysma and superior constrictor pharyngeal muscles, which are the secondary auxiliary muscles, are also responsible for the medial movement of the condyles.4 During the opening movements of the mandible, the LPMs on both sides and the muscles of the floor of the mouth exert a force of contraction on the mandible. Mandibular flexion is also observed during clenching, occlusion or biting in the mandible.2,4,5
The deformation of the mandible during flexure is very small, so by some clinicians, it is often disregarded and considered to be of no practical importance. However, mandibular flexure may cause various problems in both conventional and implant-supported prostheses when rigid and long-span connections are planned extending to the posterior regions of the mandible. Previous clinical and experimental studies reported that this deformation may be associated with increased stress in fixed dental prostheses and implant abutments, poor fit of fixed and partial removable prostheses, impression distortion, pain during function, screw and implant fracture, decementation of the prosthesis, and porcelain fracture.4,6,7,8,9,10,11 Therefore, it is crucial to minimize the effect of flexure movement and adopt the correct technique during any mandibular prosthetic rehabilitation.
It was suggested that there are four patterns of jaw deformation during mandibular flexure: symphyseal bending, dorsoventral shear, corporal rotation, and antero-posterior shear.12 The most critical factor that cause mandibular deformation is the contraction of the LPMs during the opening and protrusion movement of the mandible in the frontal plane.4
The bending force is mainly exerted by the medial component of the obliquely located LPMs.12 However, although it is claimed that the function of the LPMs and the convergence of the condyles towards the middle of mandible are around the mental symphysis,2,3 according to authors’ knowledge, there is no detailed study showing exactly which part of the mandible stretches in the medial direction.
The aim of this study was to determine the amount of median mandibular flexure (MMF) that occurs during mouth opening from anterior to posterior mandible in seven different regions, in different age and gender groups of both dentulous and edentulous subjects, using an intraoral digital scanner. MMF amounts were evaluated and patterns were schematized. The null hypotheses were that: (1) the amount of MMF would not differ at different mandibular regions; (2) the right and left side mandibular flexure values would not differ from each other; (3) age and gender would not affect the amount of MMF; (4) there would be no difference between the MMFs of dentulous and edentulous subjects.
MATERIALS AND METHODS
A total of 91 volunteers, 56 dentulous and 35 edentulous individuals (50 males, 41 females), participated in the study. This study was approved by the Clinical Research Ethics Committee of Faculty of Medicine Süleyman Demirel University (12.07.2018-No: 158). After an informed consent was obtained from all individuals, they were subjected to clinical and radiological examinations. Individuals with temporomandibular joint disease, mandibular trauma, maxillofacial surgery and neuromuscular disease history, and who received orthodontic treatment in the last five years, and individuals with labile crests were not included in the study.
The mandibular arches were scanned with an intraoral scanning system (TRIOS; 3Shape, Copenhagen, Denmark) and digital images were obtained. Before the scanning process, incisal tips of canine teeth, buccal cusp tips of 1st premolar and 2nd premolar teeth, mesiobuccal and distobuccal cusp tips of 1st molar and 2nd molar teeth were determined as reference points bilaterally, and marked with a black marker pen (0.1 mm Faber-Castell; A. W. Faber-Castel Cosmetics GmbH, Stein, Germany) in dentulous individuals. The center of 0.1 mm-thick pen mark was used as the reference center.
In edentulous arches, three reference points were determined: (1) the top of the right retromolar pad, (2) the top of left retromolar pad, and (3) the midline corresponding to the lingual frenulum. Before scanning, occlusal surfaces of the mandibular teeth in dentulous individuals and mandibular alveolar mucosa of the edentulous individuals were air-dried. Intraoral scans were performed twice in all individuals, at the minimum mouth opening (MnMO) sufficient for insertion of the scanner tip height (18 mm) and at the maximum mouth opening (MxMO), at the same appointment, respectively.
In dentulous individuals with relatively less mouth opening (If 28% of the measured MxMO of an individual was less than 18 mm), only the buccal cusps of the premolar and molar teeth and the incisal surfaces of the anterior teeth with reference points were scanned. Lingual and remaining occlusal areas of teeth were not scanned. All digital occlusal images were recorded automatically and were transferred to the digital software program (Sketch-up Pro2017; Trimble Inc., Sunnyvale, CA, USA) using the “top view” option in the system.
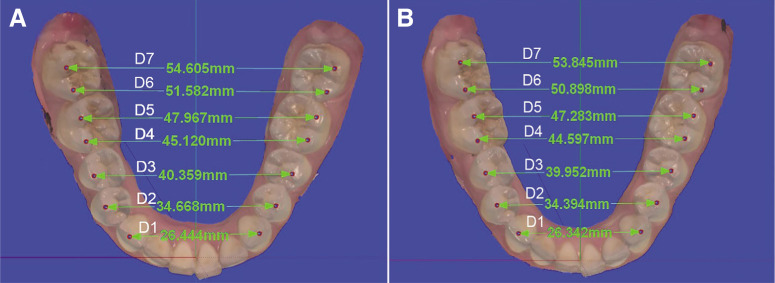
All measurements and evaluations were made independently by two observers. On digital images, the lines connecting the incisal tips and cusp tips on the right and left sides, marked in dentulous arches, were coded as D1, D2, D3, D4, D5, D6, D7 from anterior to posterior mandible (Fig. 1).
Fig. 1. Measurement of the distance between reference points on the digital image obtained at MnMO (A) and MxMO (B) in dentulous individuals.
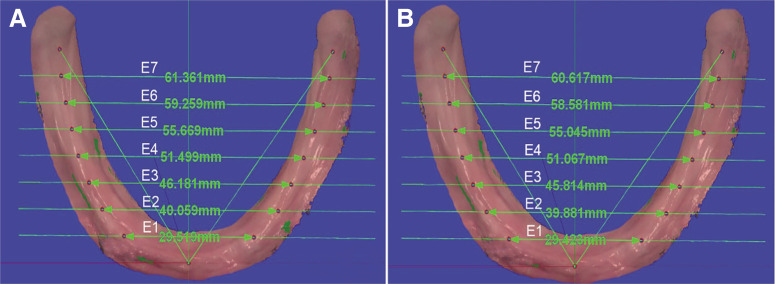
In edentulous individuals, two lines were drawn from the reference point on the midline to the right and left tops of the retromolar pad. The area between the tips of the canine teeth and the retromolar pads was divided into eight equal parts. New reference points were determined in order to measure the distance in seven regions where these lines intersect the top of the mandibular crest. The lines connecting the right and left reference points determined on the edentulous crest were coded as E1, E2, E3, E4, E5, E6, and E7 from anterior to posterior, respectively (Fig. 2).
Fig. 2. Measurement of the distance between reference points on the digital image obtained at MnMO (A) and MxMO (B) in edentulous individuals.
In dentulous individuals, it was seen that the incisal tips of the canine teeth almost corresponded to E1, when the lines between anterior crest tips and the retromolar pad were divided into eight equal parts as in the edentulous mandible. For this reason, it was assumed that E1 passes through the incisal tips of the canine teeth in the edentulous arcs. Thus, it was ensured that the reference points on the dentulous and edentulous crests were consistent with each other from anterior to posterior.
The distances between the right and left reference points (in dentulous individuals D and in edentulous individuals E lines) determined on the images were measured after scanning at the MnMO position. These measurements made in the MnMO position for each mandibular arch were also made for the images obtained at the MxMO in the same session. To ensure the precision of the measurements, the images were analyzed at 3X magnification on 17-inch screen. The MMF value was calculated by subtracting the distance measured between reference points at the MxMO from that of the distance between reference points measured at the MnMO position (Fig. 1 and Fig. 2).
An arc curve was drawn by combining reference points on all images obtained. The incisal contact point of the central incisor teeth in the dentulous arch, and the reference point at the predetermined midline in the edentulous arch were used as the anterior reference points.
The anterior reference point of the arc curve obtained at the MxMO of each individual was overlapped with the anterior reference point of the arc curve obtained from the MnMO position.
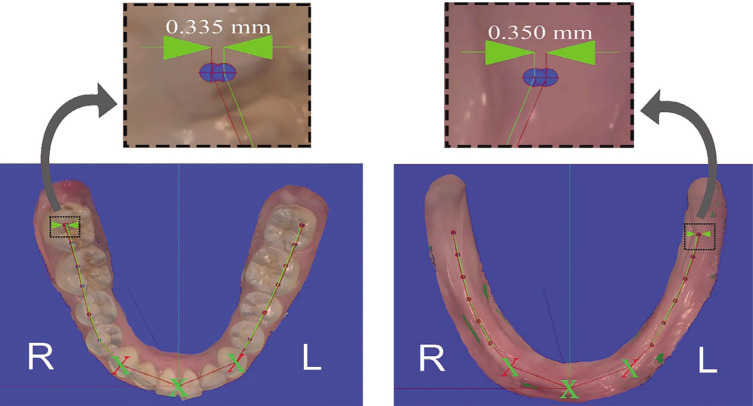
The canine reference point on the arc curve determined at the MxMO was located a little medial to that of the curve obtained at the MnMO due to MMF. Therefore, the curves were fixed so that the amount of MMF between the two curves in the canine region remained equal on both sides. The purpose of overlapping the anterior reference points and fixing the canine reference points as standard was to determine how the part of the arch posterior to the canine was shaped at right and left at the MxMO. The distance between the reference points of each region was measured on the two overlapped arcs. Thus, the flexure values on the right and left sides were calculated (Fig. 3).
Fig. 3. Measurement of right (R) and left (L) side MMF values in dentulous and edentulous individuals. Arrows indicate the MMF values calculated at the last reference points.
The statistical analyses were performed using a statistical software program (SPSS Statistics 25.0; IBM Corp., Armonk, NY, USA). The data were analyzed using the repeated measures analysis of variance (ANOVA) in factorial order.
In the present study, there were seven levels of the region factor where the measurements were made, two levels of the gender factor as male and female, and two levels of factors as the dentulous and edentulous subjects. Repeated measurements were carried out at the levels of the region factor. Tukey’s test was used to determine the differences between the mean levels of the factors.
In addition, in order to see how the amount of MMF is affected with gender and right or left in terms of direction, 3-factor repeated measures of ANOVA was used in seven regions in factorial order. Repeated measurements were carried out at the levels of the region and direction factor. In the study, the age variable was considered as a covariant in all variance analyses.
RESULTS
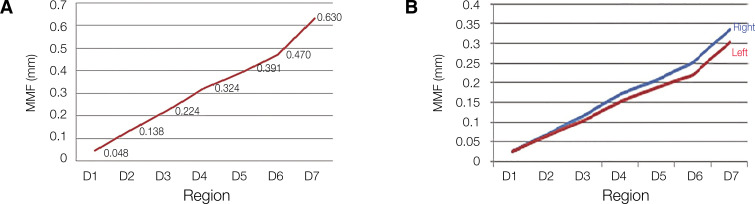
Mean MMF values from anterior to posterior were 0.048 mm in the D1 region (canine region), 0.138 mm in the D2 region, 0.224 mm in the D3 region, 0.324 mm in the D4 region, 0.391 mm to the D5 region, 0.470 mm in the D6 region and 0.630 mm in the D7 region (2nd molar tooth distal cusp region), respectively. Mean and standard deviation of MMF values of all regions according to gender are given in Table 1. MMF values increased linearly from anterior to posterior region (Fig. 4A).
Table 1. Mean and standard deviation (SD) MMF values measured at D1-D7 regions and results of repeated measures of ANOVA analyses in dentulous individuals.
| Total MMF ± SD (mm) | F | P | |||
|---|---|---|---|---|---|
| Region | 22.079 | < .001* | |||
| D1 | 0.048Ga ± 0.006 | ||||
| D2 | 0.138Fa ± 0.009 | ||||
| D3 | 0.224Ea ± 0.013 | ||||
| D4 | 0.324Da ± 0.017 | ||||
| D5 | 0.391Ca ± 0.018 | ||||
| D6 | 0.470Ba ± 0.023 | ||||
| D7 | 0.630Aa ± 0.025 | ||||
| Region × Gender | 1.833 | .159 | |||
| Male | Female | ||||
| D1 | 0.045a ± 0.008 | 0.052a ± 0.009 | |||
| D2 | 0.142a ± 0.013 | 0.135a ± 0.014 | |||
| D3 | 0.232a ± 0.017 | 0.216a ± 0.019 | |||
| D4 | 0.328a ± 0.023 | 0.320a ± 0.025 | |||
| D5 | 0.413a ± 0.025 | 0.369a ± 0.027 | |||
| D6 | 0.507a ± 0.031 | 0.434a ± 0.034 | |||
| D7 | 0.663a ± 0.034 | 0.597a ± 0.036 | |||
| Region × Age | 0.576 | .556 |
*P < .01
Different capital letters indicate statistically significant difference between regions for each gender.
The superscript letter “a” indicates that age is taken as a covariant. Mean age: 31.214.
Fig. 4. (A) Mean MMF values of dentulous individuals, (B) Mean right and left side MMF values of dentulous individuals.
MMF values increase linearly from anterior to posterior mandible on both the right and left sides in dentulous patients (Fig. 4B). As a result of the repeated measures of ANOVA, it was determined that there was no statistically significant difference between the mean MMF values of the right and left sides for each region (P > .05) (Table 2). D1 region was accepted as a reference point.
Table 2. Repeated measures of ANOVA in dentulous individuals.
| Right MMF ± SD (mm) | Left MMF ± SD (mm) | F | P | ||
|---|---|---|---|---|---|
| Direction × Region | 0.494 | .614 | |||
| D1 (ref) | 0.024a ± 0.003 | 0.024a ± 0.003 | |||
| D2 | 0.071a ± 0.005 | 0.067a ± 0.005 | |||
| D3 | 0.118a ± 0.007 | 0.106a ± 0.007 | |||
| D4 | 0.170a ± 0.010 | 0.153a ± 0.009 | |||
| D5 | 0.205a ± 0.010 | 0.186a ± 0.010 | |||
| D6 | 0.250a ± 0.012 | 0.220a ± 0.012 | |||
| D7 | 0.335a ± 0.014 | 0.302a ± 0.014 |
*P < .01
The superscript letter “a” indicates that age is taken as a covariant.
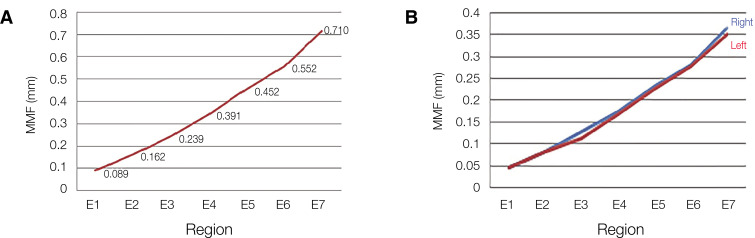
In edentulous individuals, mean and standard deviation (SD) of MMF values in all regions and also MMF values according to gender variable are given in Table 3. MMF values increased linearly from anterior to posterior mandibular region (Fig. 5A).
Table 3. Mean and standard deviation (SD) MMF values measured at E1-E7 regions and results of repeated measures of ANOVA analyses in edentulous individuals.
| Total MMF ± SD (mm) | F | P | |||
|---|---|---|---|---|---|
| Region | 7.304 | .002* | |||
| E1 | 0.089Ea ± 0.013 | ||||
| E2 | 0.162DEa ± 0.022 | ||||
| E3 | 0.239CDa ± 0.030 | ||||
| E4 | 0.343Ca ± 0.049 | ||||
| E5 | 0.452Ba ± 0.056 | ||||
| E6 | 0.552Ba ± 0.060 | ||||
| E7 | 0.710Aa ± 0.062 | ||||
| Region × Gender | 0.200 | .809 | |||
| Male | Female | ||||
| E1 | 0.103a ± 0.017 | 0.075a ± 0.019 | |||
| E2 | 0.177a ± 0.029 | 0.146a ± 0.034 | |||
| E3 | 0.264a ± 0.039 | 0.215a ± 0.046 | |||
| E4 | 0.347a ± 0.064 | 0.339a ± 0.074 | |||
| E5 | 0.477a ± 0.073 | 0.427a ± 0.085 | |||
| E6 | 0.572a ± 0.079 | 0.532a ± 0.092 | |||
| E7 | 0.751a ± 0.081 | 0.670a ± 0.094 | |||
| Region × Age | 1.996 | .147 |
*P < .01
Different capital letters indicate statistically significant difference between regions for each gender.
The superscript letter “a” indicates that age is taken as a covariant. Mean age: 62.286.
Fig. 5. (A) Mean MMF values of edentulous individuals, (B) Mean right and left side MMF values of edentulous individuals.
MMF values of edentulous individuals are listed in Table 4. No statistically significant difference was found between the mean MMF values of right and left sides (Table 4). It was seen that the MMF values increased linearly from anterior to posterior mandible in both the right and left sides (Fig. 5B).
Table 4. The results of the repeated measures of ANOVA in edentulous individuals.
| Right MMF ± SD (mm) | Left MMF ± SD (mm) | F | P | ||
|---|---|---|---|---|---|
| Direction × Region | 7.238 | .002* | |||
| E1 (Ref.) | 0.044Daa ± 0.007 | 0.044Daa ± 0.007 | |||
| E2 | 0.080Daa ± 0.011 | 0.081Daa ± 0.012 | |||
| E3 | 0.125CDaa ± 0.017 | 0.114CDaa ± 0.015 | |||
| E4 | 0.173BCaa ± 0.023 | 0.170BCaa ± 0.028 | |||
| E5 | 0.227BCaa ± 0.026 | 0.225BCaa ± 0.033 | |||
| E6 | 0.275ABaa ± 0.028 | 0.277ABaa ± 0.035 | |||
| E7 | 0.361Aaa ± 0.030 | 0.350Aaa ± 0.036 |
*P < .01
Capital letters indicate the difference between regions in each side, lower letters show the difference between sides in each region.
The superscript letter “a” indicates that age is taken as a covariant.
No statistically significant difference was found between mean MMF values of males and females in both dentulous and edentulous individuals (P > .05). Also, there was no statistically significant difference between mean MMF values of the right and left side in both dentulous and edentulous individuals (P > .05).
As a result, there were no statistically significant differences between the mean MMF values of D1 and E1, D2 and E2, D3 and E3, D4 and E4, D5 and E5, D6 and E6, and D7 and E7 regions, when comparing the dentulous and edentulous groups (P > .05).
DISCUSSION
Evaluation of mechanical properties in the mandible is difficult because of large variations in mandibular size and bone density in the population. In previous studies, in vivo intraoral and extraoral measurement methods were used to examine the amount of mandibular flexure. Traditional intraoral measurements were made using calipers, transducers fixed to tooth surfaces or implants, and strain gauge.2,3,5,7,10,12,13,14,15,16 Extraoral measurements were usually made on diagnostic models obtained from impressions taken at various openings of the mandible.2,17,18 In vitro studies on stress distribution in the corpus of the mandible were performed using photoelastic technique and FEA models.10 In this study, in the evaluation of MMF, 3-D digital models of the mandible were carried out by using an intraoral scanner. Occlusal images of these 3-D models were transferred to Sketch-up Pro2017 (Trimble Inc.) program and measurements were made on two-dimensional images.
In previous studies, mandibular deformation data ranging from a few micrometers to around 1 mm were measured.10,15,16,18,19,20 These differences may have occurred due to individual factors such as muscle strength, facial geometry, bone density, as well as differences in the measured regions.7,12,17 Additionally, the inadequacy and difficulties of the measurement methods used may have caused different results. In the strain gauge method, precise deformation values can be obtained only at the points where the strain gauge is placed.21 The photoelastic stress analysis method, on the other hand, provides qualitative information about stress distribution and concentration, but it has limitations in numerical data.21 In FEA, in order to obtain the most accurate results, the modeling should be done correctly and close to real structure.22 Moreover, there are some limitations and difficulties in modeling biological tissues in this method.23 Furthermore, bone structure may differ within itself and between individuals.
In some of the studies, digital models created by scanning conventional impressions were used to measure intermolar distance and MMF.19,24,25,26 Direct intraoral scanning eliminates errors that may result from distortion of the impression material and improper water/powder ratio of plaster material.27 The dimensional accuracy of digital models obtained by intraoral scanning was found to be higher compared to models obtained by scanning conventional impressions.28,29 Besides, the pressure applied to the mandible during impression taking with traditional methods may affect the amount of flexure.19 In this study, the disadvantages of different methods used to obtain study models in previous studies were eliminated by using an intraoral scanner.
It is stated that digital measurements are more controlled, safer and more precise than mechanical measurements.30 In this study, computer-assisted measurement method was applied. It is a reproducible method that is not affected by the person performing the measurement.
In conventional plaster model and indirect digital scanning method, in order to measure MMF quantity on both the plaster model and the digital model obtained by indirect scanning, two different models prepared in the minimum and maximum mouth opening are required. It is likely that deviations will occur in the identification and marking of reference points on two separate models. In this study, reference points were determined and marked on the mandibular arcs, intraorally. Marking these points before scanning allowed them to remain constant on the two images taken at the MnMO and immediately after the MxMO. Marking the reference points before scanning and obtaining a color digital image provided more precise measurements.
In dentulous individuals, the buccal cusp tips were chosen as the reference point, as in previous studies.11,26 Using the buccal cusps of the teeth as a reference allowed the minimum amount of mouth opening required for insertion of the intraoral scanner tip. When making the impression of mandibular full arch, it is recommended to perform it in the most closed position possible to minimize flexure. However, it was reported that there was no change in mandible width up to 28% of the MxMO, and the change in width is directly related to the size of the mouth opening.3 In the present study, MxMO was measured from the incisal edges of the central incisor teeth. The height of the scanner tip of the TRIOS (3Shape) intraoral scanner used was 18 mm. The intraoral scannings were made in a way that the minimum amount of mouth opening required for insertion of the scanner tip that would not risk mouth opening up to 28% of the MxMO at which mandibular flexure began. However, in individuals with naturally less amount of MnMO, the scanning included only the buccal cusps for premolar and molar teeth. Lingual sides of these teeth were not scanned in these individuals.3 Thus, the scanning was completed without increasing the interocclusal distance that could cause mandibular flexure at mouth opening.
Shinkai et al.11 performed digital scanning of plaster models to measure intermolar distance and MMF values on obtained images. According to the repeated measurements made by two researchers for each patient, the flexure amount was found to be between 0 and 0.36 mm.
Asadzadeh et al.15 measured the amount of mandibular deformation on 35 dentulous female individuals in the canine and 2nd molar region using digital calipers. The deformation in the MxMO was recorded as an average of 0.1671 mm in the canine region and 0.1894 mm in the second molar region. Ebadian et al.18 evaluated the relationship between MMF and maximum occlusal force in males and females. Impressions were taken with polyvinylsiloxane in each individual with the closed-mouth technique and at the MxMO. In the plaster models obtained from these impressions, the distance between the 1st molar teeth was measured with a digital caliper. The mean flexure value was found to be 0.62 mm in males and 0.72 mm in females.
Schmidt et al.31 evaluated a possible deformation of the mandible during mouth opening using an intraoral scanner and a conventional impression technique. Two digital impressions, at maximum mouth opening and at small mouth opening, and a conventional impression at small mouth opening were taken. During mouth opening, no mandibular deformation was detected according to digital measurements and no mandibular deformation was observed at the previously assumed level.
In this study, the MMF was measured in seven different regions from anterior to posterior in dentulous individuals. The flexure graph of the mandible was drawn with the data obtained. Accordingly, it was seen that the symphysis area was the center of rotation and the MMF was very low (0.048 mm) in the canine region. A linear increase was observed in the amount of flexure from the anterior to the posterior region as 0.048 mm, 0.138 mm, 0.224 mm, 0.324 mm, 0.391 mm, 0.470 mm, and 0.630 mm, respectively. However, it was observed that the mean MMF values increased a little more from D6 to D7 transition region in the posterior mandible. This increase in MMF values in posterior region may be caused by the direct force application of the LPMs, whose insertion is located at the posterior of the mandible. In previous studies, the MMF is frequently measured in the 1st molar and 2nd molar tooth regions.2,3,4,5,6,16,17,18,24,25 When comparing the results of this study with that of these studies in which the 1st molar and 2nd molar teeth were taken as references, it was seen that the MMF values measured were higher than those stated by some researchers2,4,5,6,17,25 and lower than those of the others.3,16,18,24 These differences may arise from the testing of different individual groups and the sensitivity variations of the measurement methods. At the same time, differences in bone structure between individuals may have caused diversity.
Most of the studies on edentulous mandibular arches focused on measuring the amount of strain that develops in the mandible during different jaw movements.32,33,34 In other studies, the amount of displacement between dental implants was evaluated using a transducer.7,8 Horiuchi et al.8 measured the position between two dental implants in the first molar region using a magnetic sensor system during jaw opening and protrusion movements. The displacement of the two implants at MxMO and the displacement during protrusion were found to be between 8 - 25 µm and 10 - 37 µm, respectively.
In a 3-D FEA study, Choi found the mean MMF values of 0.1685 mm in the 1st molar region and 0.256 mm in the 2nd molar region.33
Madani et al.16 performed measurements in transversal plane in 70 edentulous (experimental group) and 50 dentulous (control group) patients using a special measuring device between the bilateral canine and 2nd molar regions at the MxMO and closed positions. The mean amount of reduction in transversal plane was found as -0.0787 mm in edentulous patients in the 2nd molar region, while it was 0.7512 mm in dentulous patients. In the canine region, it was measured as 0.3069 mm in edentulous patients and 0.2254 mm in dentulous patients.
In the present study, MMF values were quantitatively measured on images obtained using an intraoral scanner in edentulous mandibles. In order to measure the MMF in different regions of the mandible and to evaluate the changes in the mandibular arch from the anterior to the posterior region, measurements were made in seven different regions. According to the authors’ knowledge, there is no study in the literature that measures the MMF in edentulous patients by using intraoral scanner as well as in seven different regions.
In edentulous arches, it is difficult to find any other acceptable reference points other than the crest tip corresponding to the lingual frenulum and retromolar pads. Therefore, the reference points of dentulous individuals were used for verification and standardization of reference point of edentulous arches. Accordingly, when the anterior crest tips in the dentulous individuals was divided into 8 equal parts between canine cusp tips and retromolar pads, it was observed that the incisal cusp tips of the canine teeth almost coincided with the E1 reference point when the line was drawn in the edentulous mandible starting from lingual frenulum to the retromolar pads. For this reason, it was assumed that E1 passes through the cusp tips of the canine teeth in edentulous arcs. Thus, the reference points in the dentulous and edentulous crests were consistent with each other from anterior to posterior.
In this study, the MMF values were measured in seven different regions from anterior to posterior in edentulous individuals. The MMF graph of the mandible was drawn with the data obtained. The symphysis area was the center of rotation and the mean MMF in the canine region was 0.091 mm. A linear increase was observed in the values of mean MMF as 0.089 mm, 0.162 mm, 0.239 mm, 0.343 mm, 0.452 mm, 0.552 mm and 0.710 mm from the anterior to the posterior region, respectively. As in dentulous patients, it was seen that the mean MMF values increased a little more from D6 to posterior D7 region. According to the results, the first null hypothesis that the amount of MMF would not differ at different mandibular regions was rejected. The alternative hypothesis that the amount of MMF differs at different mandibular regions was accepted.
The mandibular arches come towards the mid-sagittal plane with the mouth opening, and the total amount of this motion indicates the amount of MMF. However, the distance of the right or left side of the mandibular arch from the mid-sagittal plane cannot be determined if only the total amount of MMF is considered. Therefore, the anterior and canine reference points of the arches obtained at the MnMO and MxMO were overlapped. The amount of the flexure in the parts of the arches posterior to the canine teeth was found in the right and left sides at the MxMO. In this study, the highest MMF values in dentulous individuals were found in the right D7 region (0.357 mm) in males and in the right D7 region (0.313 mm) in females. The lowest MMF values were found in the left D2 region (0.065 mm) in females and in the left D2 region (0.069 mm) in males. The highest MMF values in edentulous individuals were found in the right E7 region (0.394 mm) in males and in the left E7 region (0.342 mm) in females. The lowest MMF values were found in the right E2 region (0.065 mm) in females and in the left E2 region (0.082 mm) in males. When the MMF values of the right side of dentulous individuals were analyzed, it was observed that the MMF values were slightly higher than those of the left side. However, there was no statistically significant difference between the MMF values on the right and left sides in both dentulous and edentulous individuals (P > .05). Therefore, the second hypothesis that the right and left side mandibular flexure values would not differ from each other was accepted.
In the indirect digital model study by Wolf et al.,19 the models were overlapped and the MMF was measured separately for each tooth on the right and left sides. The highest mean MMF value in females was 0.232 mm and it was observed in the right 1st molar and 2nd molar regions. The lowest mean MMF value was measured in the right canine region as 0.020 mm. In male patients, the highest mean MMF value was 0.184 mm and was observed in the right 1st molar and 2nd molar tooth regions, and the lowest mean MMF value was 0.011 mm and was observed in the right canine region. In the study of Wolf et al.,19 the mean MMF on the right side was found to be higher in dentulous patients, which was in line with our study. The reason for this might be the effect of individuals’ unilateral chewing preferences on muscles and bones.35 Unfortunately, there is no other study in the literature that measures the right and left MMF values of edentulous individuals.
In the current study, the mean age of edentulous individuals was 63 and the mean age of dentulous individuals was 29. There was no significant difference in terms of age within the group in both edentulous and dentulous individuals (P > .05). So, the third hypothesis that age and gender would not affect the amount of MMF was accepted for age parameter.
In this study, the mean MMF values were generally higher in edentulous individuals. However, no statistically significant differences were found between the mean MMF values of the same region in both dentulous and edentulous individuals (P > .05). Therefore, the fourth hypothesis that there would be no difference between the MMF of dentulous and edentulous subjects was accepted. The rigidity of the mandible depends on the cross-sectional area of the mandible, the cortical thickness, the structure of the cancellous bone, the characteristics of the bone and the shape of the mandible.12 Following the loss of teeth, alveolar bone loss and resorption are seen in the mandible with age.36 Age-related bone loss is associated with reduced density and mineral content of cortical and trabecular bone. With increasing age, the bone becomes more porous. With poor bone density, the mandible is more prone to flexure. Moreover, the mandibles, which have smaller symphysis areas and more porous bone structure, are more prone to flexure.10,37 On the contrary, with age, the flexibility of bone tissue decreases due to the decrease in the proportion of collagen fibers responsible for bone elasticity.38 However, it should be considered that stronger muscles may be associated with more mandibular flexure.4 Considering these reasons, it can be concluded that the amount of MMF in dentulous and edentulous individuals is in balance and will not change with age considerably.
In the present study, no statistically significant difference was found between genders in terms of MMF values in both groups of dentulous and edentulous individuals (P > .05). So, as stated before for age parameter, the third hypothesis was also accepted for gender parameter. The results are in accordance with the other studies.16,24 Nevertheless, the mean MMF values were slightly higher in males. This finding might be due to the larger and more voluminous mandible in males. Additionally, factors such as the mechanical properties of the bone, muscle strength and MxMO might also affect the amount of flexure.11,13,26,37,39 Generally, the decrease in the mineral density of the trabecular bone is more pronounced in females than in males. Specifically, bone resorption in postmenopausal women was noted to be three times than that of men.40
Splinting of dental implants and fixed dental prostheses create a rigid joint in the flexing mandible. Although there is a small amount of flexure in the mandible, stress areas may occur in the bone when rigid and long-span fixed dental prostheses and implants are used. Design of the implant-supported prostheses should allow mandibular flexure without generating stresses at the bone-implant interface.41 In mandible, when a dental restoration is planned by using multiunit (one piece) mandibular fixed dental prostheses or implant-supported fixed dental prostheses in completely edentulous mandible, mandibular flexure should be taken into account and prostheses should be fabricated as independent short pieces as possible.32,41,42 Additionally, during digital denture making based on intraoral scanning, the MMF should also be taken into consideration and scanning should be done at MnMO as possible.
On the other hand, the mechanical properties of prosthetic materials may also require changes in the design of prostheses.43 The modulus of elasticity of the supra-structure material used should also allow a relative degree of flexure compatible with that of the mandible. Otherwise, as a result of flexure caused by mandibular movement, failures such as fracture in the ceramic material or decementation of the fixed dental prostheses may be encountered. When planning mandibular long-span one-piece fixed or removable prostheses, mandibular flexion should be taken into account for patient satisfaction in the short term and for success of the prostheses and survival of teeth and implants in the long term.
Mandibular flexure occurs in 3D direction. In this study, the mandibular flexure in horizontal plane was considered when MMF was calculated. In further studies, mandibular flexure should be measured in 3D direction using digital scanning methods.
CONCLUSION
The results of this study revealed that MMF is seen in all regions of both edentulous and dentulous individuals measured at the MxMO. A linear increase was observed in the MMF values from the anterior to the posterior mandibular regions. The amount of flexure on the right side of dentulous individuals was slightly higher, but there was no significant difference between the right and left mandibular flexure amounts of all individuals. Gender and age did not show a significant difference in terms of MMF values in both groups of edentulous and dentulous individuals.
When a rigid long-span bilateral mandibular fixed dental prosthesis is planned, especially extending to the posterior region of the mandible, the phenomenon of mandibular flexure should be considered for the success and prognosis of a dental prosthesis.
References
- 1.Al-Sukhun J, Helenius M, Lindqvist C, Kelleway J. Biomechanics of the mandible part I: measurement of mandibular functional deformation using custom-fabricated displacement transducers. J Oral Maxillofac Surg. 2006;64:1015–1022. doi: 10.1016/j.joms.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 2.Regli CP, Kelly EK. The phenomenon of decreased mandibular arch width in opening movements. J Prosthet Dent. 1967;17:49–53. doi: 10.1016/0022-3913(67)90050-9. [DOI] [PubMed] [Google Scholar]
- 3.De Marco TJ, Paine S. Mandibular dimensional change. J Prosthet Dent. 1974;31:482–485. doi: 10.1016/0022-3913(74)90169-3. [DOI] [PubMed] [Google Scholar]
- 4.Omar R, Wise MD. Mandibular flexure associated with muscle force applied in the retruded axis position. J Oral Rehabil. 1981;8:209–221. doi: 10.1111/j.1365-2842.1981.tb00495.x. [DOI] [PubMed] [Google Scholar]
- 5.Goodkind RJ, Heringlake CB. Mandibular flexure in opening and closing movements. J Prosthet Dent. 1973;30:134–138. doi: 10.1016/0022-3913(73)90046-2. [DOI] [PubMed] [Google Scholar]
- 6.Gates GN, Nicholls JI. Evaluation of mandibular arch width change. J Prosthet Dent. 1981;46:385–392. doi: 10.1016/0022-3913(81)90443-1. [DOI] [PubMed] [Google Scholar]
- 7.Hobkirk JA, Schwab J. Mandibular deformation in subjects with osseointegrated implants. Int J Oral Maxillofac Implants. 1991;6:319–328. [PubMed] [Google Scholar]
- 8.Horiuchi M, Ichikawa T, Noda M, Matsumoto N. Use of interimplant displacement to measure mandibular distortion during jaw movements in humans. Arch Oral Biol. 1997;42:185–188. doi: 10.1016/s0003-9969(96)00101-x. [DOI] [PubMed] [Google Scholar]
- 9.Paez CY, Barco T, Roushdy S, Andres C. Split-frame implant prosthesis designed to compensate for mandibular flexure: a clinical report. J Prosthet Dent. 2003;89:341–343. doi: 10.1067/mpr.2003.57. [DOI] [PubMed] [Google Scholar]
- 10.Sivaraman K, Chopra A, Venkatesh SB. Clinical importance of median mandibular flexure in oral rehabilitation: a review. J Oral Rehabil. 2016;43:215–225. doi: 10.1111/joor.12361. [DOI] [PubMed] [Google Scholar]
- 11.Shinkai RS, Canabarro Sde A, Schmidt CB, Sartori EA. Reliability of a digital image method for measuring medial mandibular flexure in dentate subjects. J Appl Oral Sci. 2004;12:358–362. doi: 10.1590/s1678-77572004000400020. [DOI] [PubMed] [Google Scholar]
- 12.Hylander WL. Stress and strain in the mandibular symphysis of primates: a test of competing hypotheses. Am J Phys Anthropol. 1984;64:1–46. doi: 10.1002/ajpa.1330640102. [DOI] [PubMed] [Google Scholar]
- 13.McDowell JA, Regli CP. A quantitative analysis of the decrease in width of the mandibular arch during forced movements of the mandible. J Dent Res. 1961;40:1183–1185. [Google Scholar]
- 14.Burch JG. Patterns of change in human mandibular arch width during jaw excursions. Arch Oral Biol. 1972;17:623–631. doi: 10.1016/0003-9969(72)90189-6. [DOI] [PubMed] [Google Scholar]
- 15.Asadzadeh N, Madani AS, Mirmortazavi A, Sabooni MR, Shibani V. Mandibular width and length deformation during mouth opening in female dental students. J Appl Sci. 2012;12:1865–1868. [Google Scholar]
- 16.Madani AS, Asadzadeh N, Hosseini SH. Mandibular flexure in anterior-posterior and transverse plane on edentulous patients in mashhad faculty of dentistry. J Dent Mater Tech. 2013;1:24–28. [Google Scholar]
- 17.Chen DC, Lai YL, Chi LY, Lee SY. Contributing factors of mandibular deformation during mouth opening. J Dent. 2000;28:583–588. doi: 10.1016/s0300-5712(00)00041-5. [DOI] [PubMed] [Google Scholar]
- 18.Ebadian B, Abolhasani M, Heidarpour A, Ziaei M, Jowkar M. Assessment of the relationship between maximum occlusal force and median mandibular flexure in adults: a clinical trial study. J Indian Prosthodont Soc. 2020;20:76–82. doi: 10.4103/jips.jips_282_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wolf L, Bergauer B, Adler W, Wichmann M, Matta RE. Three-dimensional evaluation of mandibular deformation during mouth opening. Int J Comput Dent. 2019;22:21–27. [PubMed] [Google Scholar]
- 20.Choi AH, Conway RC, Taraschi V, Ben-Nissan B. Biomechanics and functional distortion of the human mandible. J Investig Clin Dent. 2015;6:241–251. doi: 10.1111/jicd.12112. [DOI] [PubMed] [Google Scholar]
- 21.Clelland NL, Lee JK, Bimbenet OC, Brantley WA. A three-dimensional finite element stress analysis of angled abutments for an implant placed in the anterior maxilla. J Prosthodont. 1995;4:95–100. doi: 10.1111/j.1532-849x.1995.tb00323.x. [DOI] [PubMed] [Google Scholar]
- 22.Brunski JB, Puleo DA, Nanci A. Biomaterials and biomechanics of oral and maxillofacial implants: current status and future developments. Int J Oral Maxillofac Implants. 2000;15:15–46. [PubMed] [Google Scholar]
- 23.Cochran DL. The scientific basis for and clinical experiences with Straumann implants including the ITI Dental Implant System: a consensus report. Clin Oral Implants Res. 2000;11:33–58. doi: 10.1034/j.1600-0501.2000.011s1033.x. [DOI] [PubMed] [Google Scholar]
- 24.Prasad M, Hussain MZ, Shetty SK, Kumar TA, Khaur M, George SA, Dalwai S. Median mandibular flexure at different mouth opening and its relation to different facial types: a prospective clinical study. J Nat Sci Biol Med. 2013;4:426–430. doi: 10.4103/0976-9668.117028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Canabarro Sde A, Shinkai RS. Medial mandibular flexure and maximum occlusal force in dentate adults. Int J Prosthodont. 2006;19:177–182. [PubMed] [Google Scholar]
- 26.Custodio W, Gomes SG, Faot F, Garcia RC, Del Bel Cury AA. Occlusal force, electromyographic activity of masticatory muscles and mandibular flexure of subjects with different facial types. J Appl Oral Sci. 2011;19:343–349. doi: 10.1590/S1678-77572011005000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quaas S, Rudolph H, Luthardt RG. Direct mechanical data acquisition of dental impressions for the manufacturing of CAD/CAM restorations. J Dent. 2007;35:903–908. doi: 10.1016/j.jdent.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 28.Flügge TV, Schlager S, Nelson K, Nahles S, Metzger MC. Precision of intraoral digital dental impressions with iTero and extraoral digitization with the iTero and a model scanner. Am J Orthod Dentofacial Orthop. 2013;144:471–478. doi: 10.1016/j.ajodo.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 29.Anh JW, Park JM, Chun YS, Kim M, Kim M. A comparison of the precision of three-dimensional images acquired by 2 digital intraoral scanners: effects of tooth irregularity and scanning direction. Korean J Orthod. 2016;46:3–12. doi: 10.4041/kjod.2016.46.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jemt T, Hjalmarsson L. In vitro measurements of precision of fit of implant-supported frameworks. A comparison between “virtual” and “physical” assessments of fit using two different techniques of measurements. Clin Implant Dent Relat Res. 2012;14:e175–e182. doi: 10.1111/j.1708-8208.2011.00416.x. [DOI] [PubMed] [Google Scholar]
- 31.Schmidt A, Klussmann L, Schlenz MA, Wöstmann B. Elastic deformation of the mandibular jaw revisited-a clinical comparison between digital and conventional impressions using a reference. Clin Oral Investig. 2021;25:4635–4642. doi: 10.1007/s00784-021-03777-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Law C, Bennani V, Lyons K, Swain M. Mandibular flexure and its significance on implant fixed prostheses: a review. J Prosthodont. 2012;21:219–224. doi: 10.1111/j.1532-849X.2011.00798.x. [DOI] [PubMed] [Google Scholar]
- 33.Choi AH. Finite element modeling of the mandible and ceramic dental implants. Dissertation. Sydney, Australia: University of Technology; 2004. [Google Scholar]
- 34.Ben-Nissan B. Three-dimensional modelling and finite element distortion analysis of the mandible, Dissertation. Sydney, Australia: University of New South Wales; 1987. [Google Scholar]
- 35.Balcioglu HA, Uyanikgil Y, Yuruker S, Tuna HS, Karacayli U. Volumetric assessment of lateral pterygoid muscle in unilateral chewing: a stereologic study. J Craniofac Surg. 2009;20:1364–1366. doi: 10.1097/SCS.0b013e3181ae41e9. [DOI] [PubMed] [Google Scholar]
- 36.Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers: a mixed-longitudinal study covering 25 years. J Prosthet Dent. 1972;27:120–132. doi: 10.1016/0022-3913(72)90188-6. [DOI] [PubMed] [Google Scholar]
- 37.Burch JG, Borchers G. Method for study of mandibular arch width change. J Dent Res. 1970;49:463. doi: 10.1177/00220345700490025101. [DOI] [PubMed] [Google Scholar]
- 38.Atkinson PJ, Woodhead C. Changes in human mandibular structure with age. Arch Oral Biol. 1968;13:1453–1464. doi: 10.1016/0003-9969(68)90027-7. [DOI] [PubMed] [Google Scholar]
- 39.Novak CA. Mandibular dimensional change in the various jaw positions and its effect upon prosthetic appliances. Dent Stud. 1972;50:19–21. [PubMed] [Google Scholar]
- 40.Gulsahi A, Yüzügüllü B, Imirzalioglu P, Genç Y. Assessment of panoramic radiomorphometric indices in Turkish patients of different age groups, gender and dental status. Dentomaxillofac Radiol. 2008;37:288–292. doi: 10.1259/dmfr/19491030. [DOI] [PubMed] [Google Scholar]
- 41.Zarone F, Apicella A, Nicolais L, Aversa R, Sorrentino R. Mandibular flexure and stress build-up in mandibular full-arch fixed prostheses supported by osseointegrated implants. Clin Oral Implants Res. 2003;14:103–114. doi: 10.1034/j.1600-0501.2003.140114.x. [DOI] [PubMed] [Google Scholar]
- 42.Misch CE. Dental implant prosthetics. 3rd ed. Mosby Elsevier; 2008. pp. 316–320. [Google Scholar]
- 43.Flanagan D. Complete artificial dentition supported by endosseous implants: a case report of total in-office treatment. J Oral Implantol. 2005;31:91–97. doi: 10.1563/0-726.1. [DOI] [PubMed] [Google Scholar]