Abstract
The purpose of this study was to explore the association between psychological resilience and cognitive function in military veterans. We obtained public-use data from the Health and Retirement Study (HRS) for this cross-sectional study of military veterans aged 52 to 101 years (n = 150). We estimated a multivariable linear regression model in which cognitive function served as the dependent variable and psychological resilience served as the independent variable. After controlling for demographics, health conditions, and health behaviors, veterans who had higher psychological resilience scores had better cognitive function (b = 0.22, p = 0.03). Our findings suggest that psychological resilience may be associated with cognitive function among veterans. These findings highlight the importance of assessing psychological resilience in gerontological social work practice.
Keywords: neurocognitive disorders, psychological resilience, veterans health
Introduction
As the aging population grows, the global prevalence of dementia (e.g., Alzheimer’s, vascular, frontotemporal, and Lewy body) is expected to increase from 50 million to over 152 million by 2050 (World Health Organization [WHO], 2019). Cognitive decline can manifest as memory loss, executive dysfunction, and other neuropsychological symptoms (Rockford et al., 2019; WHO, 2019). Behavioral changes, like irritability, agitation, mood disturbances, aggression, as well as psychotic symptoms, such as delusions, hallucinations, and confusion can also occur. Risk of dementia is high among military veterans, especially, with an estimated prevalence of dementia among Veteran Affairs (VA) patients age 65 and older at 9.6% (Zhu & Sano, 2021).
Taylor et al. (2019) documented the importance of psychological resilience in later-life for older male veterans, and that veterans with higher levels of resilience may have less functional impairment compared to veterans with lower levels of resilience. According to the American Psychological Association (n.d.), resilience (also called psychological resilience) is defined as “the process and outcome of successfully adapting to difficult or challenging life experiences, especially through mental, emotional, and behavioral flexibility and adjustment to external and internal demands.”
Meredith et al. (2011) described psychological resilience as more than a personality trait, including personal experience, and the context of life surrounding the person. Reviewing theories of resilience, Fletcher and Sarkar (2013) categorized subareas of resilience that included protective factors, coping with stress and adversity, as well as motivational forces. Isaacs et al. (2017) conducted a prospective cohort analysis using data from the National Health and Resilience in Veterans Study and found that the majority (67.7%) of veterans had minimal-to-no current psychological distress and were deemed psychologically resilient.
Lyons and Bartolomucci (2020) suggested that chronic stress is a risk factor contributing to the onset and progression of Alzheimer’s disease. Yaffe et al. (2010) found that veterans diagnosed with post-traumatic stress disorder (PTSD) had an increased risk of dementia. The authors indicated that chronic stress may damage the hippocampus. Veterans with PTSD have been found to have smaller hippocampal volumes, a finding that may be associated with increased risk of dementia in elderly veterans. Utilizing a sample of approximately 180,000 older veterans 55 years and older, Meziab et al. (2014) found that those with a history of being a prisoner of war (POW) and PTSD had more than twice the risk of dementia than other veterans. The authors discussed how POW and PTSD altered hypothalamic–pituitary–adrenal functioning and increased cortisol levels and norepinephrine with cognitive deterioration. Elliott et al. (2015), who studied war veterans and the association of personality prototypes and adjustment, found that veterans characterized as resilient reported the lowest levels of PTSD and depression and were prospectively less likely to have PTSD and depression symptoms over time.
Reviewing a meta-analysis of studies across populations and countries, Günak et al. (2020) reported that individuals with PTSD were 1.61–1.99 times greater at risk for dementia then those without the diagnosis. Veterans with PTSD were found to have a lower risk than the general population with PTSD, and that PTSD is a potentially modifiable risk factor for all-cause dementia. This difference between veterans and non-veterans is possibly attributed to PTSD treatment interventions and resilience training provided by the military (Fletcher & Sarkar, 2013; Meredith et al., 2011). Fogle et al. (2020) in a review of the National Health and Resilience in Veterans Study described the protective psychosocial characteristics included in definitions of psychological resilience (e.g., mitigation of stress and other protective factors) in veterans. Protective factors, including resilience, as well as a sense of purpose, positive outlook, and conscientiousness, were shown to contribute to successful aging for veterans in the United States (Pietrzak et al., 2021).
Although some studies have examined the association between psychological resilience and functional activities of daily living (Manning et al., 2016; Taylor et al., 2019), a paucity of research has examined the association between psychological resilience and cognitive decline among older individuals. For example, Son et al.’s (2019) cross-sectional study of older Korean individuals found that those with higher levels of psychological resilience exhibited an enhanced orbitofrontal network (i.e., the region of the brain that mediates subjective well-being) compared to those with low levels of resilience. However, this study did not examine military veterans, who may be exposed to resilience training during military service. As such, the purpose of this study was to determine the relationship between psychological resilience and cognitive function among military veterans.
Materials and Methods
Data Source and Sample
We obtained public-use data files from the Health and Retirement Study (HRS) for this cross-sectional study (University of Michigan, 2020). The HRS, which began in 1992 with funding from the National Institute on Aging, is an interview-based study with follow-ups biennially for consenting participants and their spouses. Hispanics, Blacks, and residents of Florida are oversampled (Fisher & Ryan, 2018). HRS interviews solicit participant responses in the following domains: demographics, housing, family, household, finances and wealth, health status, health behaviors, cognitive status, and employment. For purposes of this study, we limited the sample to individuals who responded in the affirmative to the following question in 2018: “have you ever served in the active military of the United States?” Our sample included participants aged 52 to 101 years (n = 150) who had complete data on all covariates, including the military service status question, the psychological resilience items, and the cognitive decline module. An IRB considered the present study exempt from human subjects committee review.
Measures
Our dependent variable, cognitive performance, was operationalized as the number of correctly completed test domains within with the modified Telephone Interview of Cognitive Status (TICS), originally developed by Brandt and colleagues (1988) and modified (i.e., TICS-m) by Breitner and colleagues (1995). The TICS-m was designed to test cognitive performance in domains such as episodic, semantic, and working memory, as well as attention, orientation, and language. The TICS-m has been shown to be sensitive to the diagnosis of dementia and mild cognitive impairment and that there is little evidence for ceiling or practice effects (de Jaeger et al., 2003). Testing includes immediate and delayed recall of 10 words, naming of objects, dates, the current president and vice-president, and serial 7’s subtraction. Our analysis included scores ranging from 0 to 10, indicating the number of domains correctly specified during an interview—where a score of 0 would indicate all incorrect responses and a score of 10 would indicate all correct responses.
Our primary independent variable, psychological resilience, was measured using 12 items from the 2018 HRS leave behind questionnaires (Table 1), as in Manning and colleagues’ study (2016). Previous research has shown that the 12 items forming the HRS resilience scale are valid and reliable (Manning et al., 2016). Specially, the items have a Cronbach’s alpha of 0.84 and, in principal components analysis, produce a one-factor eigenvalue >4 (Manning et al., 2012). By dividing each participant’s single item score by the highest score on each item (e.g., 1/6 or 1/7), we determined that the minimum possible score on the scale was 1.93 (e.g., all ones, indicating the lowest possible amount of psychological resilience) and the maximum possible score was 75.00 (e.g., all sixes or sevens, indicating the highest possible amount of psychological resilience).
Table 1.
Health and Retirement Study Interview Items Included in the Composite Psychological Resilience Construct.
| Item | Question stem | Response options |
|---|---|---|
| 1 | I feel it is impossible for me to reach the goals that I would like to strive for | 1–6; Strongly disagree — Strongly agree |
| 2 | So far, I have gotten the important things I want in life | 1–7; Strongly disagree — Strongly agree |
| 3 | If something can go wrong for me, it will | 1–6; Strongly disagree — Strongly agree |
| 4 | I am satisfied with my life | 1–7; Strongly disagree – Strongly agree |
| 5 | What happens in my life is often beyond my control | 1–6; Strongly disagree — Strongly agree |
| 6 | I can do things that I want to do | 1–6; Strongly disagree — Strongly agree |
| 7 | The future seems hopeless to me and I can’t believe that things are changing for the better | 1–6; Strongly disagree — Strongly agree |
| 8 | When I really want to do something, I usually find a way to succeed at it | 1–6; Strongly disagree — Strongly agree |
| 9 | In most ways, my life is close to ideal | 1–7; Strongly disagree — Strongly agree |
| 10 | I can do just about anything I set my mind to | 1–6; Strongly disagree — Strongly agree |
| 11 | There is really no way I can solve the problems I have | 1–6; Strongly disagree — Strongly agree |
| 12 | I have a sense of direction and purpose in life | 1–6; Strongly disagree — Strongly agree |
Because previous studies have shown that many individual, social, and behavioral factors are associated with cognitive decline, we included several covariates in our analyses. Specifically, for each participant’s 2018 HRS survey, we obtained their age, race (i.e., White or non-White), sex (i.e., male or female), educational level (i.e., no bachelor’s degree or bachelor’s degree), marital status (i.e., married or not married), height and weight (i.e., for the purposes of calculating body mass index), diabetes diagnosis (i.e., yes or no), hypertension diagnosis (i.e., yes or no), number of times binge consumption of alcohol was reported in the past week, and engagement in moderate physical activity at least once per week (i.e., yes or no).
Data Analysis
All data were analyzed in R Studio version 4.0.4 for Windows. In order to address our research question, we fit a multivariable linear regression model to the data and calculated adjusted beta coefficients and 95% confidence intervals. The dependent variable in our model, cognitive performance, was regressed on the independent variable, psychological resilience. We controlled for age, race, sex, education, marital status, physical activity, diabetes, body mass index, hypertension, and binge drinking by including these variables in our multivariable model as independent variables, such that all beta coefficients in the model were adjusted for these factors.
Results
Univariate descriptive statistics for the study sample are presented in Table 2. The average age for the military veterans in this study was 76.87 years (Range = 52–101; SD = 7.37). The sample was primarily composed of males and individuals with a self-reported race of White. Approximately half of the individuals in the study completed a bachelor’s degree and most were married. Our analysis of the health behaviors of the sample revealed that 102 individuals did not engage in any binge consumption of alcohol, while 48 engaged in binge drinking with an average weekly engagement of 0.21 times. Most (80%) individuals engaged in moderate physical activity at least once per week. Hypertension was more prevalent (71%) than diabetes (23%).
Table 2.
Social, Demographic, Behavioral, and Cognitive Characteristics of the Study sample (n = 150).
| 2018 | |
|---|---|
| Variable | M (SE) |
| Age | 76.87 (0.60) |
| Body Mass Index | 27.60 (0.39) |
| Days of binge drinking/Week | 0.21 (0.07) |
| Resilience Score (1.93–75.00) | 10.06 (0.11) |
| Telephone interview of cognitive status items correct | 9.15 (0.14) |
| n (%) | |
| Race (White) | 141 (94.00) |
| Gender (male) | 148 (98.67) |
| Education (Bachelor’s degree) | 77 (51.33) |
| Married | 118 (78.67) |
| Diabetes | 34 (22.67) |
| Moderate PA > 0 times/Week | 120 (80.00) |
| Hypertension | 106 (70.67) |
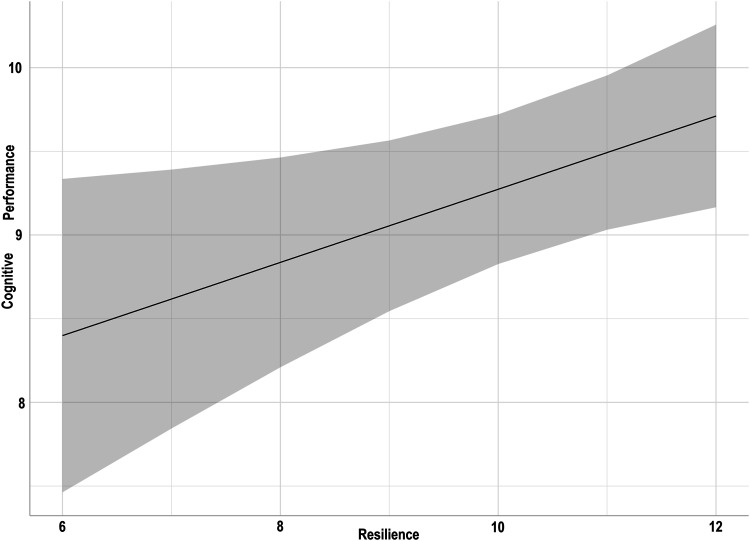
Results showed that, in the aggregate, military veterans averaged 9.15 out of 10 on the cognitive performance measure. Resilience scores, in the aggregate, were 10.06 out of 75.00. The results of our multivariable linear regression model, in which cognitive performance was regressed on psychological resilience scores, are shown in Table 3 and Figure 1. Overall, the model provided adequate fit to the data (Adjusted R2 = 0.22; F = 4.82, p < 0.001). First, males had higher cognition scores than females (b = 7.25, p < 0.001). Second, individuals with higher psychological resilience scores had significantly higher cognitive performance scores (b = 0.22, p = 0.03). In particular, as shown in Figure 1, for every five-point increase in resilience, there was a corresponding 1.10 point increase in cognitive performance [which is evident from the beta coefficient for psychological resilience (b = 0.22 *5 = 1.10)].
Table 3.
Factors Associated with Cognitive Performance Among Military Veterans.
| Variable | b (SE) a | p b | 95% CI c |
|---|---|---|---|
| Intercept | −2.75 (2.29) | 0.23 | −7.28, 1.77 |
| Age | 0.02 (0.02) | 0.23 | −0.02, 0.06 |
| Sex (male) | 7.25 (1.19) | <0.001 | 4.88, 9.61 |
| Race (White) | 0.65 (0.55) | 0.24 | −0.43, 1.74 |
| Married | −0.13 (0.32) | 0.69 | −0.77, 0.51 |
| Bachelor’s degree | 0.14 (0.28) | 0.60 | −0.40, 0.69 |
| Moderate physical activity | 0.23 (0.36) | 0.52 | −0.48, 0.94 |
| Diabetes | 0.13 (0.31) | 0.68 | −0.50, 0.79 |
| Body Mass Index | −0.01 (0.03) | 0.90 | −0.06, 0.05 |
| Hypertension | −0.17 (0.29) | 0.56 | −0.74, 0.41 |
| Binge drinking | 0.23 (0.16) | 0.15 | −0.08, 0.54 |
| Psychological resilience | 0.22 (0.10) | 0.03 | 0.03, 0.41 |
aUnstandardized, adjusted beta coefficient and standard error.
bp-value for t-statistic associated with each beta coefficient.
c95% confidence interval for the beta coefficient.
Figure 1.
This figure provides a plot of predicted values for each participant pertaining to the relationship between psychological resilience and cognitive performance (n = 150).
Discussion
The current study examined the relationship between psychological resilience and cognitive performance among military veterans aged >50 years. Our analysis revealed significant associations between cognitive performance and higher levels of resilience, after adjusting for potential confounding factors. Specifically, our analysis showed that veterans who had increasing psychological resilience scores had significantly higher cognitive performance scores (i.e., for every five-point increase in resilience scores there was a corresponding 1.10 increase in cognitive performance scores). Whether resilience leads to better cognition remains unclear, as this study was cross-sectional in nature. So far, one study has provided evidence to suggest that resilience may be associated with cognition (Son et al., 2019), with this study lending additional empirical support.
Limitations
This study is not without limitations. First, our study relied on self-report measures and may be biased by confounding factors not controlled for in this analysis, such as PTSD symptoms or traumatic brain injury. Second, the majority of participants were male, and most were White, thus limiting the generalization of the findings among more diverse samples, including female and racial minority veterans. Third, due to the lack of an randomized experimental design, we cannot determine causality in the relationship between cognitive decline and resilience; no conclusions can be drawn as to whether psychological resilience leads to lower levels of cognitive decline. Future studies investigating the causal/directional pathways underlying these relationships are needed and may elucidate novel interventional strategies to slow cognitive decline.
Implications
Our findings provide supporting evidence of an association between psychological resilience and cognitive performance, with results consistent with findings from previous studies that showed a relationship between resilience and cognitive function. For instance, Taylor et al. (2019) found that psychological resilience moderates the association between functional limitations and early-life service-related exposures (SREs) to death in military veterans, and that maintaining higher levels of resilience in the face of adverse exposures can considerably lessen functional impairment over time. Likewise, Elliott et al. (2015) observed that a resilient prototype was directly associated with lower PTSD, depression, functional disability, and higher quality of life compared with a non-resilient personality prototype. In a similar vein, Wingo et al. (2017) demonstrated an association between higher resilience and more intact social functioning regardless of the severity of PTSD and depression.
From a mental health prevention and treatment perspective, psychological resilience may be considered a protective factor against cognitive decline in the future, helping to buffer veterans from dementia/Alzheimer’s disease and supporting the enhanced mental health of older veterans. According to American Psychological Association (n.d.), cognitive resilience includes ways in which individuals view and engage with the world, the availability and quality of social resources, and specific coping strategies. Public health and Veterans Affairs professionals can aim to promote and foster cognitive resilience among veterans by ensuring access to quality social resources and cultivating coping strategies through veteran-centered interventions. Additionally, public health and Veterans Affairs providers can seek to identify motivational forces within veterans’ lives to increase the preventive factors against cognitive decline. One resource that could be helpful to state and local public health practitioners is the Healthy Brain Initiative, a collaboration between the Centers for Disease Control and National Institute on Aging within the National Institutes for Health. Resources on this page highlight factors (social engagement, diet, and physical exercise) for healthy brain aging that can help determine how to approach cognitive resilience within communities and specifically for veterans.
Conclusion
Research suggests, therefore, that increased resilience has a positive impact on functionality, mental health, and cognition. However, this association is still not well understood, and additional research is needed to draw conclusions about the complex interplay between resilience and cognitive function.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Data Availabity: Data are available here: https://hrs.isr.umich.edu/
ORCID iDs
Justin McDaniel https://orcid.org/0000-0001-8008-1645
David L. Albright https://orcid.org/0000-0002-5901-9393
References
- American Psychological Association (2020). Resilience. In APA dictionary of psychology. https://dictionary.apa.org/resilience. [Google Scholar]
- Brandt J., Spencer M., Folstein M. (1988). The telephone interview for cognitive status. Cognitive and Behavioral Neurology, 1(2), 111–117. [Google Scholar]
- Breitner J. C., Welsh K. A., Gau B. A., McDonald W. M., Steffens D. C., Saunders A. M., Magruder K. M., Helms M. J., Plassman B. L., Folstein M. F. (1995). Alzheimer’s disease in the National Academy of Sciences-National Research Council Registry of Aging Twin Veterans. III. Detection of cases, longitudinal results, and observations on twin concordance. Archive of Neurology, 52(8), 763–771. 10.1001/archneur.1995.00540320035011 [DOI] [PubMed] [Google Scholar]
- de Jager C.A., Budge M. M., Clarke R. (2003). Utility of TICS-M for the assessment of cognitive function in older adults. International Journal of Geriatric Psychiatry, 18(4), 318–324. 10.1002/gps.830 [DOI] [PubMed] [Google Scholar]
- Elliott T. R., Hsiao Y. Y., Kimbrel N. A., Meyer E. C., DeBeer B. B., Gulliver S. B., Kwok O. M., Morissette S. B. (2015). Resilience, traumatic brain injury, depression, and posttraumatic stress among Iraq/Afghanistan war veterans. Rehabilitation Psychology, 60(3), 263–276. 10.1037/rep0000050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher G. G., Ryan L. H. (2018). Overview of the health and retirement study and introduction to the special issue. Work, Aging, and Retirement, 4(1), 1–9. 10.1093/workar/wax032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher D., Sarkar M. (2013). Psychological resilience: A review and critique of definitions, concepts, and theory. European Psychologist, 18(1), 12–23. 10.1027/1016-9040/a000124 [DOI] [Google Scholar]
- Günak M. M., Billings J., Carratu E., Marchant N. L., Favarato G., Orgeta V. (2020). Post- traumatic stress disorder as a risk factor for dementia: Systematic review and meta-analysis. The British Journal of Psychiatry, 217(5), 600–608. 10.1192/bjp.2020.150 [DOI] [PubMed] [Google Scholar]
- Isaacs K., Mota N. P., Tsai J., Harpaz-Rotem I., Cook J. M., Kirwin P. D., Krystal J. H., Southwick S. M., Pietrzak R. H. (2017). Psychological resilience in U.S. military veterans: A 2-yr, nationally representative prospective cohort study. Journal of Psychiatric Research, 84, 301–309. 10.1016/j.jpsychires.2016.10.017 [DOI] [PubMed] [Google Scholar]
- Lyons C. E., Bartolomucci A. (2020). Stress and Alzheimer’s disease: A senescence link? Neuroscience and Biobehavioral Reviews, 115, 285-298. 10.1016/j.neubiorev.2020.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning L. K., Carr D. C., Kail B. L. (2016). Do higher levels of resilience buffer the deleterious impact of chronic illness on disability in later life? Gerontologist, 56(3), 514–524. 10.1093/geront/gnu068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith L. S., Sherbourne C. D., Gaillot S. J., Hansell L., Ritschard H. V., Parker A. M., Wrenn G. (2011). Promoting psychological resilience in the U.S. Military. Rand Health Quarterly, 1(2), 2. [PMC free article] [PubMed] [Google Scholar]
- Meziab O., Kirby K. A., Williams B., Yaffe K., Byers A. L., Barnes D. E. (2014). Prisoner of war status, posttraumatic stress disorder, and dementia in older veterans. Alzheimer’s & Dementia, 10(3), S236–S241. 10.1016/j.jalz.2014.04.004 [DOI] [PubMed] [Google Scholar]
- Pietrzak R. H., Levy B. R., Tsai J., Southwick S. M. (2021). Successful aging in older us veterans: Results from the national health and resilience in veterans study. Am J of Geriatric Psychiatry, 29(3), 251–256. 10.1016/j.jagp.2020.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockwood K., Sanon Aigbogun M., Stanley J., Wong H., Dunn T., Chapman C. A. T., Howlett S. E., Miguelez M., McGarrigle L., Baker R. A. (2019). The symptoms targeted for monitoring in a web-based tracking tool by caregivers of people with dementia and agitation: Cross-sectional study. Journal of Medical Internet Research, 21(6), e13360. 10.2196/13360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son S. J., Park B., Choi J. W., Roh H. W., Kim N. R., Sin J. E., Kim H., Lim H. K., Hong C. H. (2019). Psychological resilience enhances the orbitofrontal network in the elderly with mild cognitive impairment. Frontiers in Psychology, 10, 615. 10.3389/fpsyt.2019.00615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor M. G., Ureña S., Carr D. C., Min S. (2019). Early-life military exposures and functional impairment trajectories among older male veterans. The buffering effect of psychological resilience. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 74(5), 832–841. 10.1093/geronb/gby029 [DOI] [PubMed] [Google Scholar]
- University of Michigan . (2020). Health and retirement study: HRS data products [2010, 2018]. https://hrs.isr.umich.edu/data-products [Google Scholar]
- Wingo A. P., Briscione M., Norrholm S. D., Jovanovic T., McCullough S. A., Skelton K., Bradley B. (2017). Psychological resilience is associated with more intact social functioning in veterans with post-traumatic stress disorder and depression. Psychiatry Research, 249, 206-211. 10.1016/j.psychres.2017.01.022 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2019). Risk of reduction of cognitive decline and dementia: WHO guidelines. https://apps.who.int/iris/bitstream/handle/10665/312180/9789241550543-eng.pdf?ua=1&ua=1&dom=prime&src=syn [PubMed] [Google Scholar]
- Zhu C. W., Sano M. (2021). Demographic, health, and exposure risks associated with cognitive loss, Alzheimer’s disease and other dementias in US military veterans. Frontiers in Psychiatry, 12, 610334. 10.3389/fpsyt.2021.610334 [DOI] [PMC free article] [PubMed] [Google Scholar]