Abstract
Introduction
Different groups of neoplastic and non-neoplastic conditions can involve the ovaries and the epithelial tumors such as mucinous and Brenner tumors are the most common neoplastic category.
Presentation of case
This is a case report of a huge mucinous cystadenoma associated with benign Brenner tumor in 56 years old postmenopausal woman, who presented with a fast-growing abdominopelvic mass, and also review the reported articles about this rare occurrence.
Discussion
Mucinous neoplasms of the ovary represent 10%–15% of ovarian neoplasms and about 80% of them are benign. Brenner tumors are a relatively rare epithelial neoplasm of the ovary that usually affect postmenopausal women and most of them are benign. Coexistence of Mucinous cystadenoma with Brenner tumor is a rare mixed epithelial tumor of the ovary.
Conclusion
This case report and review of article create awareness among the surgeons and pathologists about rare occurrence of combination of ovarian mucinous cystadenoma and benign Brenner tumor.
Keywords: Mucinous cystadenoma, Brenner tumor, Ovarian tumor, Case report
Highlights
-
•
Different groups of neoplastic and non-neoplastic conditions can involve the ovaries --- epithelial tumors such as mucinous and Brenner tumors are the most common neoplastic category.
-
•
Coexistence of Mucinous cystadenoma with Brenner tumor is a rare mixed epithelial tumor of the ovary.
-
•
This article create awareness among the surgeons and pathologists about rare occurrence of this combination
1. Introduction
The ovary can be involved by a different group of neoplastic and nonneoplastic conditions. The World Health Organization (WHO) classifies ovarian neoplasms into 13 distinct categories. Epithelial tumors are the most common category and include a heterogeneous collection of neoplasms such as mucinous and Brenner tumors [1].
Mucinous neoplasms of the ovary represent 10%–15% of ovarian neoplasms and are divided into benign, borderline, and malignant groups. Benign mucinous neoplasms include mucinous cystadenoma and mucinous adenofibroma and account for 80% of cases [2].
Brenner tumors are a relatively rare epithelial neoplasm of the ovary, accounting for 1.4–2.5% of all ovarian tumors and they usually affect postmenopausal women, and most (about 99%) are benign [3].
Mixtures of epithelial tumors are common. Minor foci of another tumor other than the predominant one can be ignored, but when significant amounts (>10%) of several tumor types are present, the tumor is best classified as a mixed epithelial tumor. Mucinous cystadenoma occasionally contains a component of Brenner tumor, with reported incidence of 1.3% of ovarian mucinous neoplasms ranging up to 4% [4].
In this article we report a case of mixed mucinous cystadenoma with Brenner tumor.
2. Case presentation
A 56 years old postmenopausal woman presented to our center with a three month of progressively worsening abdominal discomfort and distention. She had no weight loss or vaginal bleeding. She was not hypertensive nor diabetic.
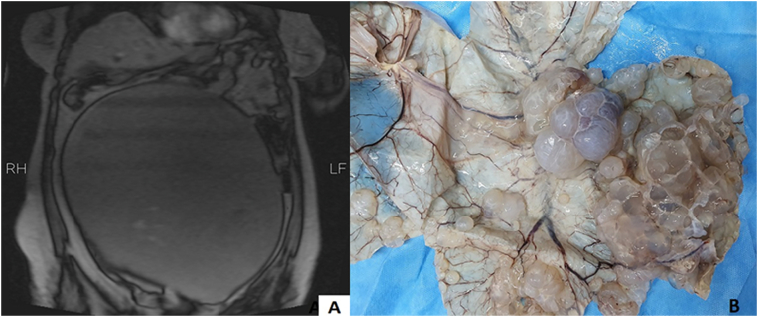
Abdominopelvic sonography detected a huge cyst involving total abdominopelvic cavity and for further evaluation of its features abdominopelvic MRI with and without contrast was performed. This demonstrated a 270 × 255 × 150 mm cystic mass with septation and daughter cysts at abdominopelvic cavity with enhancement of septation's walls originating from left ovary most compatible with ovarian mucinous cystadenoma (Fig. 1A). Other pelvic organs were unremarkable and no LAP was detected in pelvic cavity.
Fig. 1.
A, abdominopelvic MRI showed a 270 × 255 × 150 mm cystic mass at abdominopelvic cavity; B, huge opened multilocular cystic mass filled with mucoid material.
Tumor markers (CA125, AFP, BHCG, LDH and HE4) were in normal limits and Roma index was 1.9. Other lab data had normal findings.
Exploratory laparotomy was done for the patient and the massive tumor was carefully dissected and it was traced to the left adnexa and total hysterectomy and bilateral salpingo-oophorectomy was performed.
Pathological gross evaluation identified a separate huge 30 × 23 × 17 cm multilocular cystic mass filled with mucoid material attached to the remanent fallopian tube. Uterus and attached right adnexa were unremarkable (Fig. 1B).
In histological sections of left ovarian cyst there were medium to large sized cysts lined by tall columnar epithelium with basally located nuclei and intracellular pale staining mucin. There were also nests and islands of epithelial cells of transitional cell types that were round to polygonal with oval nuclei, prominent nucleoli and clear to eosinophilic cytoplasm in dense fibroblastic stroma in more than 10% of the embedded areas. By considering these histological features the final diagnosis of benign mucinous cystadenoma with benign Brenner tumor components was assigned (Fig. 2A, B).
Fig. 2.
A, cyst wall lined by tall columnar epithelium with basally located nuclei and intracellular pale staining mucin (×200); B, nests and islands of epithelial cells of transitional cell types in dense fibroblastic stroma (×200).
3. Discussion
Epithelial tumors, numerically the most important group of neoplasms, have traditionally been thought to derive from the ovarian surface epithelium (OSE) and were thus referred to as surface epithelial tumors. It is now appreciated that the epithelial tumors of the ovary are of diverse origins, histogenetically. Epithelial ovarian tumors are subclassified based on cell type as serous, endometrioid, clear cell, mucinous, seromucinous, or transitional (Brenner) [5].
Ovarian mucinous neoplasms consist of a lower percentage of epithelial tumors than serous neoplasms, representing approximately 10–15% of all ovarian tumors and about 80% of these lesions are benign [6].
Brenner tumors are rare epithelial tumors accounting for around 2–3% of ovarian tumors and are rarely malignant. Brenner tumors are frequently identified incidentally following resection of other lesions, with as many as 30% of Brenner tumors identified as combined lesions. The lesions frequently present in postmenopausal patients with a mean age around 60 years [7].
Although the relationship between ovarian mucinous tumor and Brenner tumor is well known, there are few reported cases of the coexistence of these two types of ovarian tumors in the literature [4].
Here we review 6 case reports of mixed mucinous cystadenoma with Brenner tumor. The clinicopathological features of these cases as well as our case are summarized in Table 1.
Table 1.
Clinicopathological characteristics of reported cases.
| Sridevi et al. [4] | Abbas et al. [8] | Pradhan et al. [9] | Anoedward et al. [10] | Duogherty et al. [11] | Nazari et al. [12] | Our case | |
|---|---|---|---|---|---|---|---|
| Year | 2015 | 2015 | 2017 | 2017 | 2018 | 2020 | 2021 |
| Age | 52 | 70 | 52 | 59 | 57 | 58 | 56 |
| Clinical presentation | Pelvic discomfort | Progressive abdominal pain | Abdominal pain | Abdominal distention | Progressive abdominal discomfort | Abdominal pain and distention | Progressive abdominal discomfort and distention |
| Course duration | 1 month | 2 months | 6 months | 3 months | 3 months | 6 months | 3 months |
| Location | Left ovary | Right ovary | Right ovary | Right ovary | Left ovary | Right ovary | Left ovary |
| Size | 8 × 7 × 5 cm | 52 × 41 × 36 cm | 25 × 20 × 18 cm | 25 × 15 cm | 40 × 22 × 27 cm | 20 × 13 cm | 30 × 23 × 17 cm |
| Surgical treatment | TAH-BSO | TAH-BSO | TAH-BSO | TAH-BSO | TAH-BSO | TAH-BSO | TAH-BSO |
All the presented patients were postmenopausal women with progressive abdominopelvic discomfort. The disease course was less than 6 months in all cases. All the ovarian masses were unilateral and five of them were huge mass (more than 20 cm) and only in one case the mass was less than 10 cm. There was no side preference and the masses had involved right or left ovaries equally. All the patients underwent TAH-BSO for treatment because of menopausal status and possibility of malignancy [4], [8], [9], [10], [11], [12].
Our patient was also a post-menopausal woman with history of 3-month progressive abdominal pain and distention with huge 30 × 23 × 17 cm left ovarian mass which underwent TAH-BSO and pathological diagnosis of mucinous cystadenoma associated with benign Brenner tumor was made.
Ovarian mucinous tumors have been divided into benign (mucinous cystadenoma), borderline, and malignant (mucinous carcinoma); most mucinous tumors are benign or borderline. Grossly, they tend to grow larger than the serous types and are partially or completely cystic, often multiloculated and have a smooth surface. A fluid to viscous material of mucoid nature is present in the lumen. The epithelium is referred to as intestinal and is characterized by an epithelial lining with a picket fence appearance, goblet cells, Paneth cells and endocrine cells. The distinction between benign and borderline mucinous tumor is based on the presence of cytologic atypia and stratification which is present in borderline type [5].
Brenner tumors consist of solid and cystic nests of epithelial cells resembling transitional epithelium (urothelium) surrounded by an abundant stromal component of dense, fibroblastic nature microscopically. The epithelial cells have sharply defined outlines with oval nucleus and a small but distinct nucleolus and longitudinal grooves with clear cytoplasm [5].
The work has been reported in line with the SCARE 2020 criteria [13].
This case report and review of literature creating awareness among the pathologists and surgeons about occurrence of combination of ovarian mucinous cystadenoma and Brenner tumor.
Sources of funding
No source of funding.
Ethical approval
Not applicable.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Maryam Maghbool, MD: study concept and design, data interpretation, manuscript writing.
Babak Samizadeh, MD: data interpretation, manuscript writing.
Research registration
Not applicable.
Guarantor
Dr. Maryam Maghbool.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
None.
References
- 1.Kurman R.J., Carcangiu M.L., Herrington S., Young R.H. 4th ed. IARC; Lyon, France: 2014. World Health Organization Classification of Tumours of the Female Reproductive Organs. [Google Scholar]
- 2.Marko J., Marko K.I., Pachigolla S.L., Crothers B.A., Mattu R., Wolfman D.J. Mucinous neoplasms of the ovary: radiologic-pathologic correlation. Radiographics. 2019;39(4):982–997. doi: 10.1148/rg.2019180221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Turgay B., Koyuncu K., Taşkın S., Ortaç U.F. Features of ovarian brenner tumors: experience of a single tertiary center. Turk. J. Obstet. Gynecol. 2017;14(2):133–137. doi: 10.4274/tjod.98216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sridevi S., Manmadha Rao V., Satish Kumar S., Bhagyalakshmi A. Mucinous cystadenoma with brenner tumor: a case report. J. Evid.-based Med. Healthc. 2015;2(4):455–458. [Google Scholar]
- 5.Rosai Juan. Rosai and Ackerman’s Surgical Pathology. 11th edition. Mosby; Edinburgh: 2017. Female reproductive system; pp. 1374–1390. [Google Scholar]
- 6.Kato H., Kanematsu M., Furui T., Morishige K., Hirose Y. Ovarian mucinous cystadenoma coexisting with benign brenner tumor:MR imaging findings. Abdom. Imaging. 2013;38:412–416. doi: 10.1007/s00261-012-9887-1. [DOI] [PubMed] [Google Scholar]
- 7.Jung S.E., Lee J.M., Rha S.E., Byun J.Y., Jung J.I., Hahn S.T. CT and MR imaging of ovarian tumors with emphasis on differential diagnosis. Radiographics. 2002;22:1305–1325. doi: 10.1148/rg.226025033. [DOI] [PubMed] [Google Scholar]
- 8.Abbas A.M., Amin M.T. Brenner's tumor associated with ovarian mucinous cystadenoma reaching a huge size in postmenopausal woman. J. Cancer Res. Ther. 2015;11(4):1030. doi: 10.4103/0973-1482.151858. [DOI] [PubMed] [Google Scholar]
- 9.Pradhan P., Mohanty L., Pradhan D., Pujari S., Kar A. Benign brenner tumor of ovary with mucinous cystadenoma: a case report. Asia J. Pharm. Health Sci. 2017;7:1643–1646. [Google Scholar]
- 10.Henry AKO Anoedward G., James Adeshina S., Omolade Adegoke O., Olufemi Awotunde T., Eniola Lasisi M., Olurotimi Jooda K. Mucinous cystadenomacoexisting with Brenner tumour: a case report. Sudan Med. J. 2017;11(5563):1–3. [Google Scholar]
- 11.Dougherty D., Onyemkpa C., Engel M., Oyasiji T. A case report of an incidental brenner tumor found after resection of a large ovarian mucinous neoplasm. Int. J. Surg. Case Rep. 2018;49:40–43. doi: 10.1016/j.ijscr.2018.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nazari F., Dehghani Z. Coexistence of benign brenner tumor with mucinous cystadenoma in an ovarian mass. Iran. J. Pathol. 2020;15(4):334–337. doi: 10.30699/ijp.2020.104017.2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]