Abstract
Background
Achieving appropriate leg length after surgery remains a concern for surgeons performing total hip arthroplasty (THA). The focus of surgeons trying to equalize leg length has been primarily on positioning of the femoral implant. This study evaluates the impact of acetabular height on leg length and its impact on femoral component choices during THA.
Methods
We reviewed standing pelvic radiographs of 100 patients who underwent staged bilateral THA by a single surgeon from 2016 to 2019. Leg length discrepancies and acetabular heights were determined from preoperative and postoperative radiographs. The difference between the first and second operative hips was compared at each stage of the procedures. Results were analyzed using paired t-tests.
Results
There is a significant increase in mean leg length and acetabular height after both the first and second stages of the procedure. Although there was a small change in average acetabular height for each procedure, height increased or decreased by greater than 5 mm in 44 of 200 cases. Comparing left to right hips after the second surgery disclosed no statistically significant differences in acetabular height or leg length.
Conclusion
Acetabular height and leg length changes with each stage of the procedure in sequential bilateral THA. In almost 25% of cases, the acetabular height changed by more than 5 mm. This has significant implications and needs to be considered during preoperative planning as well as operative decision-making. To account for these differences, a THA may require intraoperative acetabular assessment and changes in femoral positioning and sizing to achieve the optimal leg length.
Keywords: Acetabular height, Total hip arthroplasty, Limb length discrepancy, Femoral component
Introduction
Total hip arthroplasty (THA) is a revolutionary procedure that was introduced in the 1960s for the management of patients with arthritis, and it continues to be one of the most successful and cost-effective procedures showing exceptional long-term outcomes [1,2]. Although arthroplasty techniques have evolved significantly over the years, achieving equal and satisfactory leg lengths can sometimes be elusive [3]. In most series, the operative limb is lengthened which, although desirable in a shortened arthritic extremity, can lead to difficulties in cases where there is a persisting inequality [4,5]. Even with substantial pain relief, patients with leg length discrepancy (LLD) report dissatisfaction with surgery [[5], [6], [7], [8], [9], [10], [11], [12], [13], [14]].
Surgeons commonly use a variety of techniques to measure and adjust leg length during THA. This includes advanced techniques such as robotics, navigation, and fluoroscopic guidance, where the actual limb length can be directly measured [[15], [16], [17], [18], [19], [20]]. However, many surgeons still rely on manual techniques and preoperative templating. The focus in the literature has been to adjust the location of the femoral neck cut along with choice and size of femoral implant to optimize the length of the extremity [21]. However, positioning of the acetabulum can significantly influence length as well [[22], [23], [24]]. Previous authors have reported on LLD outcomes associated with unilateral replacements. Staged bilateral hip replacements provide a unique opportunity to study the effects of surgery on acetabular position and LLD with the potential to magnify its impact through two separate surgical procedures.
The purpose of this study is to evaluate the change in position that occurs in the acetabulum during sequential bilateral hip replacement to illustrate the effects that these changes have on femoral prosthesis placement and ultimate leg length. The hypothesis is that acetabular position can significantly change during THA and needs to be accounted for during THA to maintain appropriate leg length.
Material and methods
After obtaininig institutional review board approval, we retrospectively reviewed postoperative standing radiographs of all patients who had undergone staged bilateral primary THA by a single surgeon from 2016 to 2019. THAs were performed by the direct anterior approach on a fracture table (HANA, Mizuho OSI, Union City, CA) using radiographic guidance. Only patients who had staged bilateral THAs with preoperative and postoperative radiographs were included in the study. Patients who underwent simultaneous bilateral THA were excluded from the study.
Using preoperative and postoperative standing pelvic AP radiographs, the LLD and acetabular height were measured on the preoperative and postoperative limbs at each stage of the sequential bilateral THA using a PACS system (Sectra IDS7, Linköping , Sweden). The LLD was measured by using the vertical distance from the most prominent points of the lesser trochanters bilaterally to the interteardrop line (Fig. 1). The difference between the 2 distances was recorded as the LLD. The acetabular height difference was measured from the center of rotation to the interteardrop line (Fig. 2). All measurements were made by one orthopedic surgery resident physician. We did not adjust for magnification. Results were analyzed using paired t-tests.
Figure 1.
The leg lengths are measured from the interteardrop line to the most prominent aspect of the lesser trochanter. In this patient, the postoperative right lower extremity is longer than the left lower extremity.
Figure 2.
The acetabular height is measured from the interteardrop line to the acetabular center of rotation. In this patient, the acetabular height for the right hip is 13 mm, while the acetabular height for the left hip is 12 mm.
Results
A total of 129 consecutive patients were identified. Twenty-seven patients were eliminated because they did not have preoperative films, and 2 patients did not have radiographs obtained after the second THA. Therefore, a total of 100 patients were included for the analysis for a total of 200 THA procedures. Average age was 65.2 years. Sixty-three patients were female, and 37 were male.
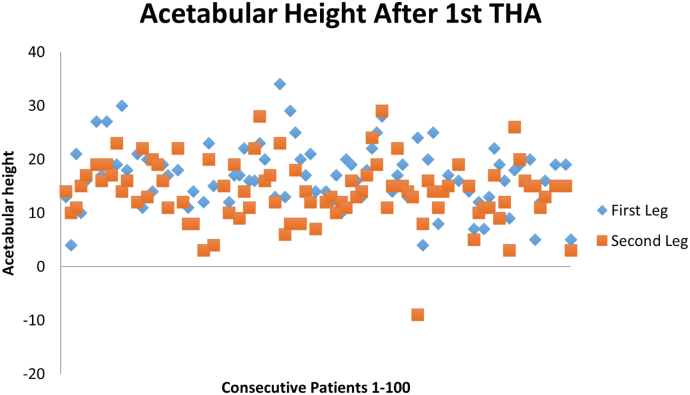
Preoperatively, there was no significant difference in the average acetabular height between the two extremities (P = .08). This is despite a statistically significant difference in preoperative leg length (P = .003). Measurement of acetabular height after the first procedure showed a significant mean increase of 1.22 mm (−10 to +16; P = .003). Similarly, the second operative hip showed a significant increase in acetabular height comparing preoperative values to postoperative ones with a mean of 1.44 mm (−16 to +26; P = .018). The mean acetabular height of both extremities statistically significantly increased irrespective of whether it was the first or second procedure. After the first THA, the acetabular heights for the two sides differed significantly (P < .001). This difference disappeared after both extremities had undergone THAs (P = .50). Average measurements and comparisons of acetabular height are depicted in Table 1, Table 2, respectively. The changes are illustrated in the scatterplots showing the changes for each patient (Figure 3, Figure 4, Figure 5, Figure 6).
Table 1.
Mean acetabular height.
| Stage | Operative hip | Mean acetabular height (mm) |
|---|---|---|
| Preoperative | First operative hip | 15.500 |
| Second operative hip | 14.700 | |
| After first THA | First operative hip (postop) | 16.722 |
| Second operative hip (preop) | 14.000 | |
| After second THA | First operative hip | 16.510 |
| Second operative hip | 16.140 |
Table 2.
Comparison of acetabular heights of hips in various stages.
| Operativehip | Comparison of acetabular height between stages | P values | |
|---|---|---|---|
| First operative hip | Preoperative | After first stage (postop) | |
| 15.500 mm | 16.722 mm | .003 | |
| Preoperative | After second stage (postop) | ||
| 15.500 mm | 16.510 mm | .034 | |
| After first stage (postop) | After second stage (postop) | ||
| 16.722 mm | 16.510 mm | .155 | |
| Second operative hip |
Preoperative | After first stage (preop) | |
| 14.700 mm | 14.000 mm | .404 | |
| Preoperative | After second stage (postop) | ||
| 14.700 mm | 16.140 mm | .018 | |
| After first stage (preop) | After second stage (postop) | ||
| 14.000 mm |
16.140 mm |
.002 |
|
| Stage |
Comparison of acetabular height between hips |
P values |
|
| Preoperative | First operative hip | Second operative hip | |
| 15.500 mm | 14.700 mm | .085 | |
| After first stage | First operative hip (preop) | Second operative hip (postop) | |
| 16.722 mm | 14.000 mm | <.001 | |
| After second stage | First operative hip (postop) | Second operative hip (postop) | |
| 16.510 mm | 16.140 mm | .503 | |
P-values <.05 depicted in bold.
Figure 3.
Acetabular height after the first THA. Scatter plot of first operative limb (postoperative) vs second operative limb (preoperative).
Figure 4.
Differences in acetabular height between first operative limb (postoperative) and second operative limb (preoperative) after the first THA.
Figure 5.
Scatter plot of acetabular height of first operative limb. Before and after the first THA (postoperative).
Figure 6.
Scatter plot of acetabular height of second operative limb. Before the first THA (preoperative) and after the second THA (postoperative).
Similar to increases in acetabular height, the leg length also increased after each stage of THA. Preoperatively, the first operative limb was significantly shorter by an average of 1.74 mm (−20 to +18; P = .003). There was a significant increase in leg length after the first procedure (P < .001), resulting in the operative limb being significantly longer by an average of 2.70 mm (−14 to +32; P < .001). There was a similar significant increase in leg length during the second operative limb after THA as well (P = .001). The LLD preoperatively significantly improved after bilateral THA, from 1.74 mm to 0.38 mm (P = .01). The LLD after bilateral THA was negligible (P = .334). Average measurements and comparisons of LLD are depicted in Table 3, Table 4, respectively.
Table 3.
LLD at various stages of THA.
| LLD at various stages of THA | ||
|---|---|---|
| Stage | Mean (mm) | P values |
| Preoperative | −1.74 | .003 |
| After first THA (preop vs postop) | 2.70 | <.001 |
| After second THA | 0.38 | .334 |
Positive value depicts the first operative extremity is longer. Negative value depicts the first operative extremity is shorter.
P-values <.05 depicted in bold.
Table 4.
Comparison of LLD between various stages of THA.
| Comparison of LLD between various stages of THA | P values |
|---|---|
| Before vs after first THA | <.001 |
| Before vs after second THA | .011 |
| After first THA vs after second THA | .001 |
There is a significant change in LLD in every stage of the procedure.
P-values <.05 depicted in bold.
The study design offered an opportunity to evaluate internal consistency of the measurement technique. Each hip was measured twice without an intervention. For the first hip, this comprised the postoperative measurement of acetabular height, which was measured before and after the second procedure (16.72 mm and 16.51 mm, respectively, P = .16). For the second hip, this included the measurement of acetabular height, which should have shown no change before and after the first procedure (14.70 mm and 14.00 mm, respectively, P = .40). In all cases, the outcomes did not change between the sets of presumed equal measurements (Table 2).
Discussion
The results of this study indicate that the position of the acetabulum has the potential to significantly change during each stage of the procedure with implications for leg length and femoral implant choice. Reviewing sequential bilateral total hip replacements provided a unique opportunity to study the changes that can occur in acetabular position. Moreover, although the mean was statistically significant, the range of changes (as much as 42 mm) after each procedure is even more dramatic, emphasizing that these changes need to be considered during preoperative planning and operative execution. In this series of patients whose leg length was measured with fluoroscopic guidance, these changes were accounted for during the second procedure resulting in an improved LLD after the second procedure.
The goals of THA are to not only relieve pain but also restore normal leg length to optimize gait and function. LLD is a common complication of THA and is perceived by 6% [25] to 32% [26] of patients, especially when shortening and lengthening exceeds 10 mm and 6 mm, respectively [27]. LLD of more than 20 mm has been reported to cause social problems [5]. Even with pain relief and good range of motion in the hip after the surgery, LLD after THA is a major concern and has been associated with low back pain [6,11], abnormal gait [7,12], peroneal and sciatic nerve palsies [28,29], dislocation [9], and early component loosening [8], which can lead to patient dissatisfaction and possible revision surgery [22]. Patient dissatisfaction with LLD is the most common reason for litigation after THA [10,13].
Although this series was performed on patients with bilateral THA, it highlights the difficulty of predicting acetabular height and position during planning and execution for even unilateral THA. The ideal situation after any THA is to have symmetrical left and right limbs after surgery. For surgeons who template preoperatively, based upon these data, it is not possible to assume that the acetabular center of rotation will not change as a result of surgery. This adds an additional variable which may be difficult to account. Traditionally, many arthroplasty surgeons focus on the positioning of the femoral implant when adjusting leg lengths during THA assuming that the center of rotation remains fixed in most cases. Femoral templating allows the surgeon to measure the level of femoral neck resection as well as the size and position of the femoral implant, which influence leg length [21]. Femoral neck resection height is relatively accessible to the surgeon during the procedure; whereas acetabular position and height are more difficult to measure intraoperatively without advanced techniques such as navigation and robotics. Ignoring the impact of unrecognized acetabular position variability on these measurements can lead to unacceptable outcomes, assuming that this series is generalizable to other surgeons.
Intraoperative techniques used by surgeons to equalize leg lengths during THA are variable. Advanced technology such as robotics [16,17,19], navigation [18,20], and fluoroscopic guidance [15,16] are claimed to have the potential to create a reproducible result, with the outcomes in this particular series of patients by a single surgeon potentially supporting this claim. Without a comparison group, we are unable to make the claim that the technology was a critical factor. All patients in our study underwent THA performed via the direct anterior approach with the use of fluoroscopy, and based on the data, equalizing leg length was achieved with this technique. Intraoperative imaging can be used to evaluate acetabular position as well as leg lengths and may account for the high reliability in preventing significant LLD in this study. However, the use of fluoroscopy has not been shown to decrease LLD by previous authors [15,16].
Surgeons also use mechanical means including intraoperative markers as well as preoperative templating to try to equalize leg lengths during surgery. Intraoperative mechanical methods have the potential to be more reliable at adjusting leg lengths than preoperative templating, particularly if they span both components [30,31]. Most commonly, a stable reference point is marked on the pelvis, and a variable reference point is marked on the greater trochanter [30]. The distance between reference points may be measured with screws and screwdrivers [32], guidewires [33], Steinman pins [4,34,35], calipers [36], sutures [37], or rulers [38]. By including a reference point above both components and a reference point below, the issue of acetabular height changes is theoretically eliminated. What is clear from the data presented is that the position of the acetabulum can change and is a variable that needs to be considered during planning and execution of THA. Adjunctive mechanical or advanced technology methods are attractive to minimize LLD, and this study suggests that the authors were able to achieve excellent leg lengths using fluoroscopy. However, the role of these techniques remains to be proven in comparative studies.
For bilateral staged THA, the chances for acetabular changes to affect leg length could be potentially increased. This may be even more significant if each stage of the procedure is performed by a different surgeon using different techniques. Although the data showed a consistent increase in the mean acetabular height for the first and second procedures, more concerning is that the range included significant positive and negative changes (−16 mm to +26 mm), even with the use of fluoroscopy. In our study, THA performed for severe osteoarthritis and avascular necrosis tended to have a positive change in acetabular height, whereas THA performed for severe hip dysplasia tended to have a negative change in acetabular height. By its nature, the outcome expressed as a mean of differences (+1.08 mm) is likely to underrepresent the variability of the potential outcomes as the negative values offset the positive. The overall change in mean acetabular height and leg length for these procedures would seem to be small and potentially insignificant. However, it is more important to consider both the positive and negative fluctuations by taking the absolute values of these differences. When evaluating these differences by the absolute values, the mean change of acetabular height was 3.97 mm. During the 200 procedures, the acetabular height varied by more than 5 mm in 44 cases. For the unsuspecting surgeon, these changes could be additive with one side being potentially higher and one lower leading to a significant discrepancy if not accounted for on the femoral side.
In our study, there was a tendency to overlengthen the leg during the first THA and then equalize the leg lengths during the second. For a patient where a contralateral hip replacement is contemplated, some degree of lengthening may be acceptable with a plan to correct the discrepancy during the subsequent procedure. Although this change in leg lengths is statistically significant, it may not be clinically significant to the patient. It is still important to counsel the patients that their shorter leg will likely be overcorrected, making it the longer leg postoperatively, and that their leg lengths should improve after the second THA.
The major limitations of this study include its retrospective design and surgery performed by one surgeon using one specific surgical approach. Conducting a prospective study would further enhance the level of evidence in evaluating changes in acetabular height and leg lengths. Moreover, all the procedures were performed with intraoperative fluoroscopic guidance, which is not universally adopted by surgeons, and a surgeon who uses different techniques may have different outcomes. Although prior authors have indicated THA fluoroscopic guidance did not prevent LLD, our study would seem to indicate the opposite is true. A study with multiple surgeons or a multicentered study involving THAs with various approaches or implants would increase the validity of our findings. Similarly, because our radiographic measurements may carry some intraobserver variability, having multiple reviewers taking measurements would increase the validity of our results. The study used standard radiographic measurements for LLD including the teardrop and lesser trochanter. However, there are many ways to measure leg length, and there is no way to know which is the optimum anatomic method. We did not use magnification correction for this study. Although we do not think magnification would have affected the results when comparing both hips at the same stage of the procedure, correcting for magnification could have increased the validity of our findings when comparing data from different stages.
Conclusion
Acetabular heights and leg lengths change at each stage in sequential bilateral THAs. Although surgeons primarily focus on the femoral neck resection and femoral implant size and positioning to optimize leg lengths, unanticipated changes in acetabular height must also be considered before and during the surgery. Overlooking expected changes in acetabular height in THA can result in significant LLD leading to patient dissatisfaction. Bilateral staged total hip replacement has the potential to magnify this effect. Studies are necessary to evaluate the effects of advanced techniques such as navigation, robotics, and intraoperative radiography in comparison to standard mechanical methods.
Conflicts of interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: A. Saxena is a paid consultant for Corin USA; has stock or stock options in Parvizi Surgical Innovation; receives research support from Halyard and United Orthopaedics; is in the editorial or governing board of JOA, JBJS, Journal of Surgical Orthopaedic Advances, and JAAOS; is a board member of AAOS, AAHKS, American Board of Oethopaedic Surgery, and EOA. A. Star is in the speakers' bureau or gave paid presentations for and is a paid consulant for DePuy and Stryker; has stock or stock options in Radlink; and is a board member in AAOS. All other authors declare no conflicts to disclose.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2022.01.026.
Appendix A. Supplementary data
References
- 1.Learmonth I.D., Young C., Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370(9597):1508. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 2.Jenkins P., Clement N., Hamilton D., Gaston P., Patton J., Howie C. Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis. Bone Joint J. 2013;95(1):115. doi: 10.1302/0301-620X.95B1.29835. [DOI] [PubMed] [Google Scholar]
- 3.Rubash H.E., Parvataneni H.K. The pants too short, the leg too long: leg length inequality after THA. Orthopedics. 2007;30(9):764. doi: 10.3928/01477447-20070901-30. [DOI] [PubMed] [Google Scholar]
- 4.Ranawat C.S., Rao R.R., Rodriguez J.A., Bhende H.S. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty. 2001;16(6):715. doi: 10.1054/arth.2001.24442. [DOI] [PubMed] [Google Scholar]
- 5.Jasty M., Webster W., Harris W. Management of limb length inequality during total hip replacement. Clin Orthop Relat Res. 1996;(333):165. [PubMed] [Google Scholar]
- 6.Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine. 1983;8(6):643. doi: 10.1097/00007632-198309000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Rösler J., Perka C. The effect of anatomical positional relationships on kinetic parameters after total hip replacement. Int Orthop. 2000;24(1):23. doi: 10.1007/s002640050006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amstutz H.C., Ma S.M., Jinnah R.H., Mai L. Revision of aseptic loose total hip arthroplasties. Clin Orthop Relat Res. 1982;170(170):21. [PubMed] [Google Scholar]
- 9.Woo R.Y., Morrey B.F. Dislocations after total hip arthroplasty. JBJS. 1982;64(9):1295. [PubMed] [Google Scholar]
- 10.Hofmann A.A., Skrzynski M.C. Hip arthroplasty: headaches & migraines: leg-length inequality and nerve palsy in total hip arthroplasty: a lawyer awaits. Orthopedics. 2000;23(9):943. doi: 10.3928/0147-7447-20000901-20. [DOI] [PubMed] [Google Scholar]
- 11.Friberg O. Biomechanical significance of the correct length of lower limb prostheses: a clinical and radiological study. Prosthet Orthot Int. 1984;8(3):124. doi: 10.3109/03093648409146072. [DOI] [PubMed] [Google Scholar]
- 12.Lai K., Lin C., Jou I., Su F. Gait analysis after total hip arthroplasty with leg-length equalization in women with unilateral congenital complete dislocation of the hip–comparison with untreated patients. J Orthop Res. 2001;19(6):1147. doi: 10.1016/S0736-0266(01)00032-8. [DOI] [PubMed] [Google Scholar]
- 13.White A. AAOS committee on professional liability: study of 119 closed malpractice claims involving hip replacement. AAOS Bull. 1994 [Google Scholar]
- 14.Konyves A., Bannister G. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br. 2005;87(2):155. doi: 10.1302/0301-620x.87b2.14878. [DOI] [PubMed] [Google Scholar]
- 15.Bingham J.S., Spangehl M.J., Hines J.T., Taunton M.J., Schwartz A.J. Does intraoperative fluoroscopy improve limb-length discrepancy and acetabular component positioning during direct anterior total hip arthroplasty? J Arthroplasty. 2018;33(9):2927. doi: 10.1016/j.arth.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 16.El Bitar Y.F., Stone J.C., Jackson T.J., Lindner D., Stake C.E., Domb B.G. Leg-length discrepancy after total hip arthroplasty: comparison of robot-assisted posterior, fluoroscopy-guided anterior, and conventional posterior approaches. Am J Orthop. 2015;44:265. [PubMed] [Google Scholar]
- 17.Leg length discrepancy following total hip arthroplasty: comparing anterior, posterior, and MAKO-assisted posterior approaches. 2013. Orthopaedic Proceedings: The British Editorial Society of Bone & Joint Surgery. [Google Scholar]
- 18.Rajpaul J., Rasool M.N. Leg length correction in computer assisted primary total hip arthroplasty: a collective review of the literature. J Orthop. 2018;15(2):442. doi: 10.1016/j.jor.2018.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakamura N., Sugano N., Nishii T., Kakimoto A., Miki H. A comparison between robotic-assisted and manual implantation of cementless total hip arthroplasty. Clin Orthop Relat Res. 2010;468(4):1072. doi: 10.1007/s11999-009-1158-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wasterlain A.S., Buza J.A., III, Thakkar S.C., Schwarzkopf R., Vigdorchik J. Navigation and robotics in total hip arthroplasty. JBJS Rev. 2017;5(3):e2. doi: 10.2106/JBJS.RVW.16.00046. [DOI] [PubMed] [Google Scholar]
- 21.Woolson S.T., Hartford J.M., Sawyer A. Results of a method of leg-length equalization for patients undergoing primary total hip replacement. J Arthroplasty. 1999;14(2):159. doi: 10.1016/s0883-5403(99)90119-5. [DOI] [PubMed] [Google Scholar]
- 22.Frueh W.W., Hozack W.J. Seminars in Arthroplasty. WB Saunders; 2005. Management of limb length discrepancy after total hip arthroplasty; pp. 127–131. (Vol. 16, No. 2) [Google Scholar]
- 23.Bhaskar D., Rajpura A., Board T. Current concepts in acetabular positioning in total hip arthroplasty. Indian J Orthop. 2017;51:386. doi: 10.4103/ortho.IJOrtho_144_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parvizi J., Sharkey P.F., Bissett G.A., Rothman R.H., Hozack W.J. Surgical treatment of limb-length discrepancy following total hip arthroplasty. JBJS. 2003;85(12):2310. doi: 10.2106/00004623-200312000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Love B. Leg-length discrepancy after total hip replacement. J Bone Joint Surg Am. 1983;65:103. [Google Scholar]
- 26.Edeen J., Sharkey P.F., Alexander A.H. Clinical significance of leg-length inequality after total hip arthroplasty. Am J Orthop (Belle Mead NJ) 1995;24(4):347. [PubMed] [Google Scholar]
- 27.Sarangi P., Bannister G. Leg length discrepancy after total hip replacement. Hip Int. 1997;7(3):121. [Google Scholar]
- 28.Edwards B.N., Tullos H.S., Noble P.C. Contributory factors and etiology of sciatic nerve palsy in total hip arthroplasty. Clin Orthop Relat Res. 1987;(218):136. [PubMed] [Google Scholar]
- 29.Eggli S., Hankemayer S., Müller M. Nerve palsy after leg lengthening in total replacement arthroplasty for developmental dysplasia of the hip. J Bone Joint Surg Br. 1999;81(5):843. doi: 10.1302/0301-620x.81b5.9610. [DOI] [PubMed] [Google Scholar]
- 30.Desai A.S., Dramis A., Board T.N. Leg length discrepancy after total hip arthroplasty: a review of literature. Curr Rev Musculoskelet Med. 2013;6(4):336. doi: 10.1007/s12178-013-9180-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Knight J.L., Atwater R.D. Preoperative planning for total hip arthroplasty: quantitating its utility and precision. J Arthroplasty. 1992;7:403. doi: 10.1016/s0883-5403(07)80031-3. [DOI] [PubMed] [Google Scholar]
- 32.Mihalko W.M., Phillips M.J., Krackow K.A. Acute sciatic and femoral neuritis following total hip arthroplasty: a case report. JBJS. 2001;83(4):589. doi: 10.2106/00004623-200104000-00017. [DOI] [PubMed] [Google Scholar]
- 33.McGee H.M. A simple method of obtaining equal leg length in total hip arthroplasty. Clin Orthop Relat Res. 1985;(194):269. [PubMed] [Google Scholar]
- 34.A technique for comparison of leg lengths during total hip replacement. Am J Orthop (Belle Mead NJ) 1996;25(1):61. [PubMed] [Google Scholar]
- 35.Huddleston H.D. An accurate method for measuring leg length and hip offset in hip arthroplasty. Orthopedics. 1997;20(4):331. doi: 10.3928/0147-7447-19970401-10. [DOI] [PubMed] [Google Scholar]
- 36.Woolson S.T., Harris W.H. A method of intraoperative limb length measurement in total hip arthroplasty. Clin Orthop Relat Res. 1985;(194):207. [PubMed] [Google Scholar]
- 37.Hossain M., Sinha A. A technique to avoid leg-length discrepancy in total hip arthroplasty. Ann R Coll Surg. 2007;89(3):314. doi: 10.1308/003588407X179189c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matsuda K., Nakamura S., Matsushita T. A simple method to minimize limb-length discrepancy after hip arthroplasty. Acta Orthop. 2006;77(3):375. doi: 10.1080/17453670610046280. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.