Abstract
Introduction
Fully hydroxyapatite-coated titanium alloy double-tapered stems have been successful implant designs for THA. The Novation Element Stem (Exactech, Gainesville, FL) is one of several of these implants following a modified Corail design philosophy. Although a great deal is known about the results of the Corail stem, little is known about the more recent Corail-inspired implants. The authors evaluated the clinical outcomes, radiographic findings and survival statistics of the collarless version of the Element Stem when used routinely in a diverse patient population.
Methods
A retrospective review was performed for all primary THR cases from 2010 to 2018. Patient demographics and HHS/OHS/patient satisfaction scores were obtained. Radiographs were evaluated for stem subsidence, radiolucencies, and bone responses to the implant.
Results
One hundred and fifty seven Element Stems were implanted with greater than 2 years of radiographic follow-up, while 105 Element Stems implanted during the study period had a survival of 5 years or more. Average HHS was 91.7 and average OHS was 44.0. 54 of 157 hips had radiolucencies, all of which included a proximal zonal radiolucency. Average subsidence was 3.33 mm; 18 hips had subsidence > 4 mm. There were 8 revisions for: aseptic loosening (4), trauma-related peri-prosthetic fractures, and early proximal–medial fractures. At 5 years, the all-cause survival rate is 92.4%, 96.2% based only on aseptic loosening and 98.1% based only on proximal medial fractures.
Conclusion
Clinical outcomes using the collarless Novation Element Stem are good, but early proximal medial fracture is still a factor in patients with poor-quality bone. Proximal radiolucencies progressing to aseptic loosening post-operatively are also a concern. The 11.5% rate of subsidence is comparable to other fully HA-coated collarless stems. This study provides a thorough critical analysis of outcomes and midterm survival data of this dual tapered-wedge fully HA-coated collarless stem used routinely in a diverse patient population.
Keywords: HA coating, Cementless collarless femoral stem, Press fit femoral stem, Outcomes, Mid-term outcomes, Aseptic loosening
Introduction
Total hip arthroplasty (THA) continues to be one of the most common elective procedures performed worldwide as our current population continues to age [1]. Overtime, the use of un-cemented collarless stems in the United States has become common place [1–3]. The relative ease of insertion, proven implant survival, and reliable clinical outcomes have made them popular [4–6].
However, challenges, such as the precision of proximal femoral canal fit, reproducibility of final implant seating height, early proximal femoral fractures and stem subsidence, continue to be concerns for these cementless stems [7–9]. Several cementless stems, fully coated with hydroxyapatite (HA), have been designed that attempt to reduce some of these challenges [10–12]. These implants achieve initial stability by virtue of their overall shape, do not necessarily require tight proximal cortical contact, and achieve long-term fixation through osseo-integration of their full-length HA coatings [13–15]. They do not require prominent ingrowth surfaces which can prevent complete seating, and their proximal shape does not require proximal fit matching the contours of the femoral neck and calcar.
In 2009, the senior author chose to begin using a new collarless fully HA-coated hip stem in primary total hip arthroplasty cases. The rationale behind the choice being that the implant would be more universally applicable and more forgiving, compared to other collarless un-cemented stems that rely on proximal fit and proximal femoral ingrowth. To the authors’ knowledge, there is only one reported study regarding survivorship or complications of the Element Stem, with Godoy-Monzon et al. reporting a stem survival rate of 93% at 9 years. However, the authors presented little radiographic data, and for the patients that did have radiographic follow-up, radiolucencies were detected [16]. Magill et al. provided a recent analysis of the Corail stem with median 6-year follow-up including a collared and collarless variant, concluding that the presence of radiolucencies in zone 7 was the most prominent radiographic finding. Collarless femoral stems were found to have a much higher prevalence of radiolucencies compared to collared stems (23.6% vs. 2.6%, respectively), but a full comparison was unable to be performed due to heterogeneity [17]. The authors did not include revision cases in their cohort and thus could not provide any survival data. Therefore, we felt that a more critical analysis of outcomes regarding the Element collarless stem was necessary.
The current study was conducted to determine the clinical outcomes, patient satisfaction, incidence of subsidence, prevalence of early femoral fracture and the midterm implant survival rate using this collarless dual-tapered fully HA-coated stem at 5-year follow-up. We hypothesize that: 1) the radiographic clinical results and survival data using this stem would be comparable to those reported for other similar fully coated hydroxyapatite stems, and 2) that there would be a reduced rate of proximal femoral fractures compared to collarless cementless stems primarily relying on proximal fit and proximal osseo-integration.
Materials and methods
This is a retrospective cohort study, based on a prospective joint registry. All study patients were informed, consented, and entered into a hospital-based IRB approved total joint registry designed for joint arthroplasty follow-up studies. The majority of patient data were acquired and entered prospectively. A few cases predated the database, which were consented at the follow-up visits. Pre-operative demographics, radiographic data, and operative data for these early cases were obtained and entered retrospectively.
The Element Stem (Novation Element, Exactech, Inc. Gainesville, FL) is a fully hydroxyapatite (HA)-coated forged titanium alloy (TiAl6V4) dual-tapered implant, which borrows from the general design concepts of the Corail stem (DePuy Orthopaedics Inc., Warsaw, IN) or the older Furlong stem (JRI Orthopaedics, Inc. Sheffield, United Kingdom). Surface roughness beneath the HA coating in the Element Stem is Ra 6.9 microns Rt 30 microns, the bonding strength of the HA coating to the metal substrate is > 15 MPa, HA purity is 98%, and the crystallinity is 60–90%. There are many similarities between the Element and Corail implants, but some notable differences are present. Both stems have HA coatings applied to an underlying grit blast titanium alloy substrate using a plasma spray process. The differences are as follows: the thickness of the Element HA coating is 80 ± 20 microns rather than 155 ± 35 microns on the Corail, and both the Element Stem and Corail proximal cross sections are trapezoidal, (the Corail having the narrowest side medial with less acute edges, while the Element Stem has the narrowest side lateral with more acute edges, making the medial side of the Element Stem broader flatter and sharper). The neck lengths and offsets of the smaller-sized Element Stems (8–12) were reduced to fit smaller proximal femoral anatomies.
The senior author chose to use the collarless version of the Element Stem with a presumption that in a wedge-shaped cementless implant, small amounts of early subsidence would be desirable to achieve better initial implant stability. In part, this attitude evolved from previous experience implanting the CLS stem (Zimmer, Wausau, IN) [18, 19].
277 primary total hip arthroplasties were implanted by the senior author at a single institution from 5/10/10 to 3/1/2018 using the Element Stem. Pre-operative templating was performed in all cases. All surgeries were performed by or under the direct supervision of the senior author through a posterior lateral approach. A mini-posterior lateral approach was used in slender patients. Canal alignment was determined with a Charnley tapered reamer followed by impaction broaching.
Three different un-cemented ingrowth acetabular components with their associated polyethylenes were used during the study period. These polyethylenes were used in series based on the surgeon’s changing preference over time, Pinnacle – Marathon poly (DePuy Orthopaedics Inc., Warsaw, IN) 5/10/10–10/15/12, Novation InteGrip–Connection GXL poly (Exactech, Inc. Gainesville, FL) 2/13/12 – 11/29/16, and Trident or Tritanium–X-3 poly (Stryker Corp. Kalamazoo, MI) 12/27/16 to 3/1/18. Each socket was implanted according to the manufacturer’s recommendations.
Study protocol office visits included pre-operative, 6-week, 3-month, 1-year, and every 5 years after surgery. Clinical outcomes were measured using Harris Hip Scores (HHS), Oxford Hip Scores (OHS), Charnley ratings, and visual analog patient satisfaction scores which were acquired during routine office visits. Protocol radiographs were taken pre-operatively, in recovery room, 6-week, 1-year, and 5-year post-op. Many patient visits occurred at times other than those in the protocol. Hip scores and X-rays were therefore obtained at these other follow-up intervals. Patients who did not return for follow-up were contacted by phone and either asked to return or interviewed to acquire HHS, OHS, and patient satisfaction scores. Implant survival determinations were made by direct contact, reviewing any available imaging that revealed an intact implant, or review of medical records documenting continued survival of the implant. All radiographs were reviewed by two independent authors. Radiographs were evaluated for degree of subsidence with respect to the greater trochanter [8], signs of osteo-integration, such as spot welding, cortical hypertrophy, or proximal stress shielding, stem alignment, fixation type, such as distal potting or 3-point fixation, radiolucencies denoted by Gruen zones, and Dorr classification [20]. Any signs of fracture, osteolysis, or infection were noted.
Inclusion criteria included any patient that underwent a primary THA over the age of 18 with the Element stem from 5/10/10 to 3/1/18, due to primary or secondary osteoarthritis, dysplasia, post-traumatic arthritis, inflammatory arthritis or avascular necrosis. Patients undergoing revision THA or primary THA due to malignancy, severe dysplasia requiring a modular implant, or THA due to femoral neck fracture were excluded.
A total of 277 stems met these criteria. Exclusion criteria for the midterm survival cohort included: any patient that did not have a minimum 5-year follow-up either through: clinical assessment, telephonic visit, or radiographs obtained. This excluded 170 patients. Exclusion criteria for the radiographic and clinical follow-up cohorts included: any patients without adequate 2 year or greater radiographs or lack of HHS, OHS, or satisfaction scores more than 2 years after surgery. This excluded 118 patients in the radiographic cohort and a further 33 patients in the clinical cohort. A summary of the total number of patients included in each cohort is detailed in Table 1. A failure in this study was defined as any stem which was indicated for a revision.
Table 1.
Basic demographics
| Study population | Radiographic 2 + year F/U | Clinical 2 + year F/U | Survival 5 + years | Clinical + radiographic post-op and 2 + year F/U | P value |
|---|---|---|---|---|---|
| Total | 157 | 124 | 105 | 80 | |
| Age (years) |
58.2 ± 12.7 Range: (20–82) |
58.8 ± 11.9 Range: (25–82) |
56.9 ± 11.9 Range: (20–81) |
59.2 ± 11.1 Range: (31–82) |
0.57 |
| Gender |
Male: 87 Female: 70 |
Male: 69 Female: 55 |
Male: 58 Female: 47 |
Male: 36 Female: 31 |
0.99 |
| BMI |
28.7 ± 5.20 Range: (18.9–46.1) |
28.5 ± 5.00 Range: (18.9–46.1) |
29.2 ± 5.51 Range: (19.5–54.8) |
29.1 ± 5.15 Range: (21.3–46.1) |
0.47 |
| Follow-up (years) |
3.85 ± 1.81 Range: (2–10) |
4.81 ± 1.53 Range: (2–10) |
5.75 ± 1.68 Range: (5–10) |
4.65 ± 1.28 Range: (2–7) |
< 0.0001 |
| Diagnosis | 0.97 | ||||
| Degenerative Joint Disease | 108 (69%) | 92 (74.1%) | 73 (70.0%) | 59 (73.8%) | |
| Post-Traumatic Arthritis | 5 (3.2%) | 5 (4.03%) | 5 (4.76%) | 3 (3.75%) | |
| Avascular Necrosis | 34 (21.7%) | 22 (17.7%) | 22 (25.7%) | 14 (17.5%) | |
| Other | 10 (6.3%) | 5 (4.03%) | 5 (4.76%) | 4 (5%) | |
| Cup Implant | |||||
| Pinnacle | 53 | 34 | 51 | 16 | |
| Intergrip GXL | 92 | 85 | 53 | 60 | |
| Tritanium | 12 | 5 | 1 | 4 | |
| Stem Size | |||||
| 8 | 11 | 9 | 4 | 3 | |
| 9 | 25 | 14 | 17 | 11 | |
| 10 | 33 | 21 | 22 | 16 | |
| 11 | 37 | 30 | 25 | 19 | |
| 12 | 20 | 22 | 10 | 12 | |
| 13 | 14 | 12 | 13 | 8 | |
| 14 | 8 | 10 | 8 | 7 | |
| 15 | 6 | 4 | 5 | 3 | |
| 16 | 2 | 2 | 1 | 1 | |
| Stem offset | |||||
| Standard | 93 | 63 | 63 | 45 | |
| Extended | 64 | 61 | 42 | 35 | |
The bold signifies a P-value reaching statistical significance
Categorical Data: Chi-Squared. ANOVA for all other statistics
Comparisons of basic demographic data across our cohorts were performed with chi-squared analysis for categorical data and one-way ANOVA for numerical data. HHS and OHS scores in each group were tested for normality with the Shapiro–Wilk test and were subsequently found to be non-parametric, necessitating the use of the Kruskal–Wallis test for statistical interpretation. Kaplan–Meier survival curves were used to predict survival data. All statistical analyses were conducted with Microsoft Excel for Statistical Computing.
Results
Patient demographics
Data in regard to 3 separate cohorts are reported in this study. 2-year radiographic cohort: out of the 277 stems implanted, 3 separate cohorts were analyzed. 2-year radiographic cohort: 157 patients had a minimum of 2-year radiographic follow-up (Table 1), the rest were either lost to follow-up or deceased. 2-year clinical cohort: 124 stems had a minimum of 2-year clinical follow-up (Table 1). Mid-term survival cohort: 105 patients had either radiographic, clinical, or self-reported implant survival of 5 years or more (Table 1). Regardless of the cohort, the most common acetabular polyethylene used was the GXL polyethylene, followed by Marathon polyethylene. The most common stem sizes were 9–12, with similar distribution among all groups. Ninety-three were implanted with standard offset compared to only 64 implanted with extended offset.
Radiographic outcome
Radiographic outcomes for hips with ≥ 2-year radiographs are detailed in Tables 2 and 3.
Table 2.
Summary of radiographic findings
| Radiographic finding | Number of occurrences/total |
|---|---|
| Zone of Radiolucencies | Total: 54/157 34.4% |
| Z1 | 35 |
| Z2 | 2 |
| Z3 | 1 |
| Z4 | 0 |
| Z5 | 2 |
| Z6 | 3 |
| Z7 | 3 |
| Z8 | 36 |
| Z9 | 1 |
| Z10 | 0 |
| Z11 | 0 |
| Z12 | 1 |
| Z13 | 1 |
| Z14 | 6 |
| Spot welding | |
| Z3 | 23 |
| Z4 | 4 |
| Z5 | 8 |
| Z10 | 3 |
| Z11 | 5 |
| Z12 | 24 |
| Cortical hypertrophy | |
| Z4 | 1 |
| Z5 | 2 |
| Z12 | 1 |
| Stress shielding | 0 |
| Osteolysis of greater trochanter | 2 |
Table 3.
Additional radiographic findings
| Radiographic finding | Number of occurrences/total |
|---|---|
| Average greater trochanter subsidence |
3 ± 12 Range (0–95) |
| Greater trochanter subsidence > 4 mm | 18 |
| Dorr classification | |
| Type A | 8 |
| Type B | 144 |
| Type C | 5 |
| Type of initial fixation | |
| Distal potting | 47 |
| Point fixation | 106 |
| Suspension in cancellous bone | 4 |
| Alignment | |
| Stems in Varus Alignment | 102 |
| Average varus angulation (degrees) | 1 ± 1 |
| Stems in Valgus Alignment | 55 |
| Average valgus angulation (degrees) | 1 ± 1 |
Radiolucencies
Fifty-four of 157 hips had radiolucencies (34.4%), all of which included a proximal zonal radiolucency (Z1, 7, 8, or 14). Zone 8 and zone 1 were the most common, with 36 and 35 instances reported respectively. Only 7 patients had an isolated distal radiolucency reported (13%). Twenty-six of the 54 patients (48.1%) had multiple radiolucencies reported. When broken down by acetabular implant type, 24 Marathon, 27 Connection GXL, and 3 X-3 implants had radiolucencies present (Table 4). Ninety-one percent of the hips were Dorr B, 5.1% Dorr A and 3.2% Dorr C.
Table 4.
Polyethylene liner and radiolucencies
| Radiographic findings | Implant type | ||
|---|---|---|---|
| Pinnacle | Integrip GXL | Tritanium | |
| Zone of radiolucencies | |||
| Z1 | 18 | 16 | 1 |
| Z2 | 2 | ||
| Z3 | 1 | ||
| Z4 | |||
| Z5 | 2 | 1 | |
| Z6 | 2 | 1 | |
| Z7 | 3 | ||
| Z8 | 18 | 15 | 3 |
| Z9 | 1 | ||
| Z10 | |||
| Z11 | |||
| Z12 | 1 | ||
| Z13 | 1 | ||
| Z14 | 3 | 2 | 1 |
| Instances of aseptic loosening | 2 | 2 | |
Alignment and type of initial fixation
One hundred two were placed in a mild varus alignment with an average varus angulation of 1 degree (range 0–5). Fifty-five stems were placed in mild valgus alignment with an average valgus angulation of 1 degree (range 0–5). A total of 47 stems (29.9%) were seen to have achieved initial fixation stability through distal potting, 106 stems through (67.5%) point fixation and 4 (2.5%) through suspension in cancellous bone.
Subsidence
Average subsidence for all stems was 3.3 mm (0–95 mm), with 18 hips having subsidence of greater than 4 mm (average subsidence of that cohort 15.6 mm (4–95 mm). When addressing greater trochanteric subsidence in particular, in patients with subsidence greater than 4 mm, 17/18 hips were given a Dorr classification score of B and 1/18 Dorr C. In this group, no appreciable differences were seen when assessing stem size, polyethylene type, varus/valgus angulation, but distal potting was seen in 4 stems (22.2%).
Other findings
Two hips had osteolysis of the greater trochanter. One hip had a lytic cavity within the greater trochanter not in contact with the stem, while the other hip had wide lytic appearing radiolucency in zone 1 which ballooned out into the trochanter. Neither patient with osteolysis had any clinical symptoms of failure. Interestingly, both of these hips were implanted with GXL polyethylene. Two hips developed Brooker 3 heterotopic bone formation, but both patients remain asymptomatic.
Clinical outcomes
Average Harris Hip Score at latest follow-up was 91.7 (range 39–100), average Oxford Hip Score was 44.0 (range 13–48) and patient satisfaction score was 9.54 (range 5–10), at the most recent follow-up (Table 5).
Table 5.
Clinical outcomes
| Clinical score | Clinical survival 2 + year F/U | Clinical + radiographic post-op and 2 + year F/U | P value |
|---|---|---|---|
| HHS |
91.9 ± 12.7 Range: (39–100) |
91.9 ± 12.2 Range: (39–100) |
0.50 |
| OHS |
43.9 ± 6.98 Range: (13–48) |
43.7 ± 7.27 Range: (13–48) |
0.41 |
| Patient satisfaction (0–10) |
9.47 ± 1.12 Range: (5–10) |
9.48 ± 1.14 Range: (5–10) |
0.98 |
Failures leading to revision
There were 8 revisions: 4 for aseptic loosening, 2 for late trauma-related peri-prosthetic fractures, and 2 early proximal medial fractures (Table 6).
Table 6.
Causes for revision
| Complications | Occurrences |
|---|---|
| Aseptic Loosening | 4 |
| Peri-prosthetic Fracture-Proximal Medial | 2 |
| Peri-prosthetic Fracture-Late Traumatic | 2 |
In regard to aseptic loosening, 1 patient had traumatic dislocation of bilateral THA after motor vehicle accident. After initial closed reduction of both hips, the patient later presented with progressive radiolucencies around the left femoral stem. No revision of the stem was performed due to a complicated social situation. The other 3 cases developed progressive loosening without history of trauma. All 4 cases had Dorr B canals. 3 of the stems (75%) in this group had a standard offset and 3 of the stems (75%) were in a valgus alignment, with an average angulation of 1 ± 1 degrees (range: < 1–1 degrees), and 1 stem was in varus alignment of 1 degree. That being said, valgus angulation in this group was not significantly different compared to patients without aseptic loosening (1.2 ± 1 vs 1.11 ± 0.99, p = 0.47). In addition, distal potting was seen in one patient that underwent revision for aseptic loosening (25%). No statistically significant differences were seen with regard to stem size or polyethylene used between patients with or without aseptic loosening. Figure 1 shows radiographic progression of radiolucencies described from a stem within our cohort.
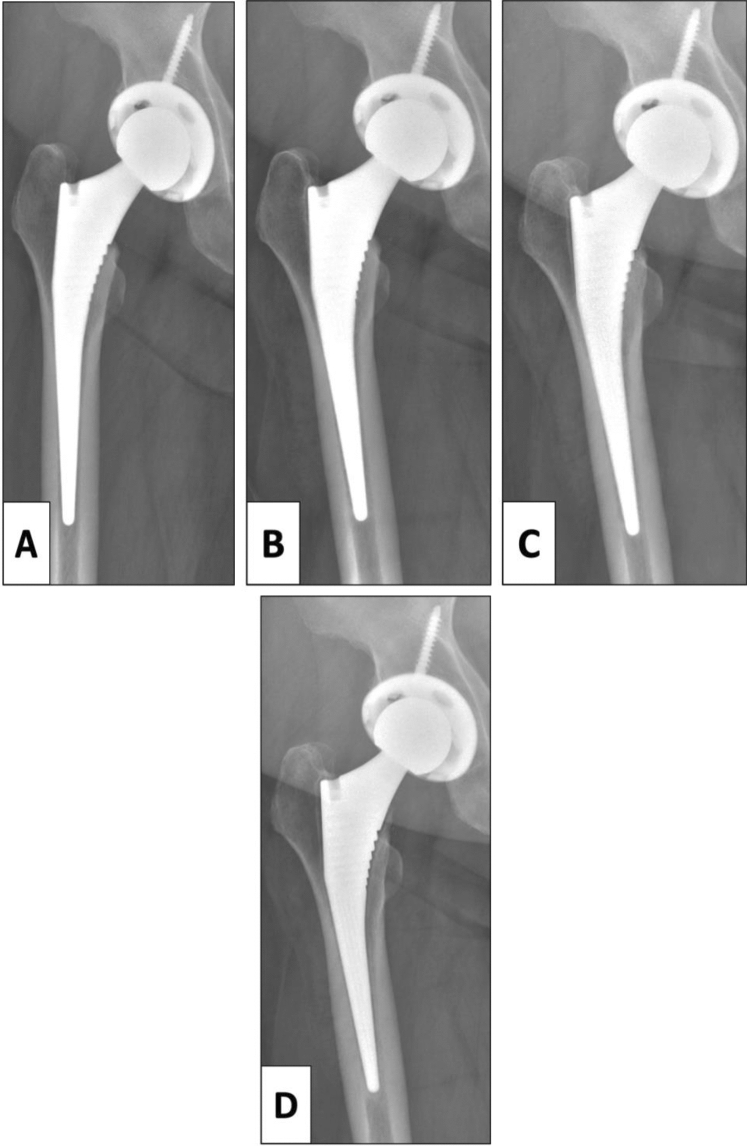
Fig. 1.
Progressive radiolucencies leading to aseptic loosening in a 53-year-old female. A Post-operative recovery room film demonstrating appropriate fit. B Film at 10 months already demonstrates radiolucency in Zone 1. C Film at 24 months demonstrating progressive radiolucencies in Zones 1 and 2. D Film taken 60 months after surgery demonstrating progressive radiolucencies in Zones, 1,2,3 and 7 with the beginning of shelf formation
Two hips had early proximal medial fractures and 2 had traumatic peri-prosthetic fractures requiring revision, all of which had a Dorr B classification. All patients with fractures had an extended offset, but no differences in stem size, polyethylene type, or varus/valgus angulation were seen. Two hips in this group had distal potting. The remaining failure was due to excessive polyethylene wear (implanted with GXL Poly).
Survival
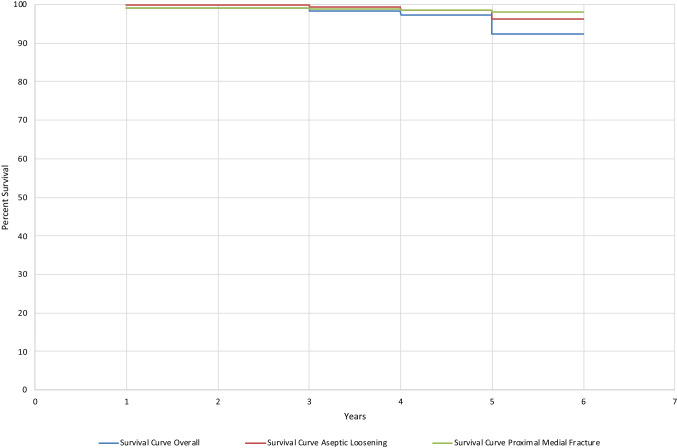
At 2 years with revision as end point, survival rate of this stem was 99%. The survival rate at 2 years with aseptic loosening as end point is 100%. At 5 years, survival rate with revision as end point is 92.4%, 96.2% with aseptic loosening as end point, and 98.1% with proximal medial fractures as end point. Figure 2 demonstrates the Kaplan–Meier survival curve for our cohort, further divided into overall survival versus patients with aseptic loosening versus proximal medial fractures.
Fig. 2.
Kaplan–Meier survival curve
Discussion
The original Corail and Furlong stems are examples of fully hydroxyapatite (HA)-coated traditional length implants that achieve initial stability by virtue of their shape and then acquire reliable long-term fixation by osseo-integration of their HA coatings [21, 22]. This philosophy of implant design has proven to be extremely successful [23, 24]. The original exclusivity of the Corail design expired, making it possible for several companies to market their own versions of the Corail-type design. The Element Stem was one such implant and acquired 510 K clearance in 2008. Although there have been many thorough reports of the clinical and radiographic success of the Corail and Furlong, little has been published about similar analyses of the Corail-inspired designs on the market today. Only two other stems have published survival rates. The survival rate for the Polarstem (Smith and Nephew, Inc Watford, UK) at 5 years is reported to be 99.6% and the Avenir stem (Zimmer-Biomet, Warsaw IN, USA) at 7 years is 98.9% [25, 26].
This dual tapered-wedge fully HA-coated stem was used by the senior author in all hips presenting for primary total hip arthroplasty. The only exceptions were hips with femoral canals requiring implant sizes smaller than the smallest implant or cases of extreme acetabular deficiencies or femoral rotational abnormalities better served by modular stems. The collared version of the implant was never used. Hips with inflammatory arthritis and poor bone quality were not excluded.
The survival rate of the Element Stem at 5 years with revision as an end point is 92.4%. This included aseptic loosening, late failures due to high-energy trauma, and early failures due to low-energy proximal medial fractures. Implant survival with aseptic loosening as an end point was 96.2% at 5 years which is lower than other fully HA-coated collarless stems. The patient population in this series was not selective, as this stem was the workhorse choice for the senior author. In regard to the Corail stem with revision for any cause as the end point, Hallan et al. reported a 10-year survival rate of 98% and Vidalain et al. reported a 23-year survival rate of 96.3% [21, 27]. For the Furlong stem with revision for any cause as the end point, Shetty et al. reported a 99% survival at 13 years and Gabbar et al. reported a 94.3% survival rate at 10 years [22, 28].
Eighteen (11.5%) of our subsided stems had a greater trochanteric subsidence of more than 4 mm (0–95 mm). However, these implants remained stable, asymptomatic, and unrevised. As reported by Al Najjim et al., the subsidence rate for the collarless tapered-wedge fully HA-coated stem at 1 year was 11% and 7.6% for the collared version [29]. Demey et al. reported that collared un-cemented stems have significantly greater immediate stability than collarless as they are able to withstand greater vertical and horizontal forces before the initiation of subsidence and subsequent fracture [30]. Another recent biomechanical analysis suggests that collared stems may offer a protective effect in torsional loading which translates to reduced risk of early peri-prosthetic fractures [31]. Second, all of our stems that sustained subsidence greater than 4 mm were found to have Dorr B and Dorr C type femur morphology. It is thought that adequate bone morphology and quality are necessary to decrease risk of subsidence with use of a tapered, cementless femoral stem. A recent study evaluated subsidence of HA-coated femoral stems with different Dorr type femoral morphology and demonstrated a 0.4 mm and 0.18 mm greater subsidence in Dorr C- and B-type femurs, respectively, when compared to Dorr Type A, although this was not statistically significant [32]. It might be advisable to consider the use of this dual tapered-wedge fully HA-coated stem in patients with poor bone quality and high BMIs, who theoretically might be more prone to subsidence or early peri-prosthetic fractures.
Two stems (1.9%) suffered early proximal medial fractures (Fig. 3). Both were in women who were diagnosed and under treatment for osteoporosis. This complication has been well reported by others using collarless un-cemented implants, such as the Accolade (3.7%), TriLock (4.9%), and Corail (5.4%.) [33]. Both of our early-fracture patients required open reduction internal fixation and stem revision. Although the rate of this complication was lower than that reported by others, the consequences can be great. It is not clear whether the flatter proximal medial surface, resulting in more acute-angled corners, of the dual tapered-wedge fully HA-coated stem might have played a role in these early fractures. The authors now consider using a proximal prophylactic cerclage cable, a collared Element Stem, or a cemented implant in advanced osteoporotic cases.
Fig. 3.
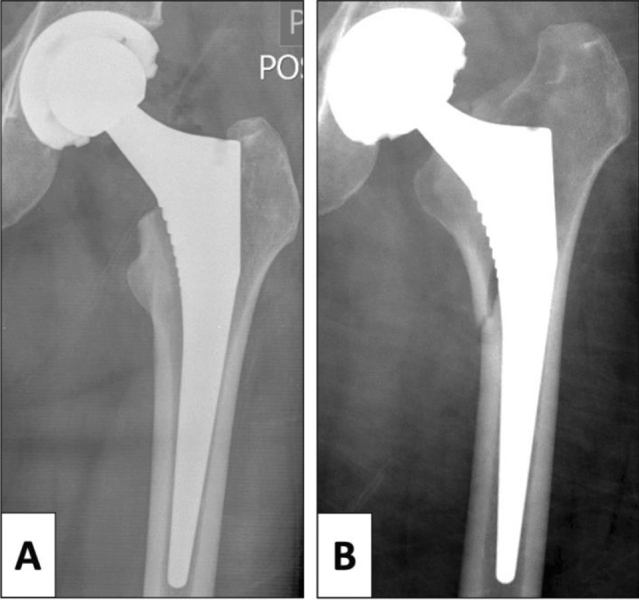
Proximal medial fracture in a 54-year-old female. A Post-operative recovery room films demonstrating stable fixation. B Proximal medial fracture necessitating revision less than 1 month after surgery
Two cases (1.9%) suffered late peri-prosthetic fractures as a result of traumatic injuries secondary to a fall at 58 months and 64 months. Both hips were silent clinically and radiographically prior to the traumatic event. These cases were treated with open reduction internal fixation and stem revision. Neither of these failures were felt to be attributable to the stem design.
Of the four stems (3.8%) that developed progressive radiolucencies and aseptic loosening, 3 stems displayed progressive aseptic loosening without histories of trauma. Each had uncomplicated operative and post-operative courses. One-year post-operative radiolucencies appeared proximally in zones 1 and 14. Clinically, they remained asymptomatic. Radiolucencies continued to progress into zone 8 and more distal into zones 2 and 3. Three to four years after surgery, the patients reported pain consistent with stem loosening. Infection work-ups including CRP, ESR, synovial fluid analysis, and cultures were negative. Two of these hips were revised allowing examination of the stems and the other has yet to be revised because of the coronavirus.
The cause of these late progressive radiolucencies leading to aseptic loosening is not clear. One possible explanation is polyethylene wear. All four cases had acetabular components with moderately crosslinked polyethylene liners (2 Connection GXL and 2 Marathon). The 4 liners showed 0.9, 1.5, 3.5 and 5 mm of asymmetry, respectively. Two other cases without stem loosening with GXL polyethylene liners had femoral osteolysis. There is a concern with potential early wear of GXL polyethylene as documented in the literature [34]. However, looking at our Element Stem data, there was no statistically significant difference in the incidence of radiolucencies or aseptic loosening between those cases performed with GXL polyethylene and Marathon or X-3 polyethylene at 2 years. Also, of note, no cases of stress shielding were seen with the radiographic evaluation of our cases.
Another explanation could be degradation or de-bonding of the HA coating. Resorption and de-bonding of HA has been reported in the early days of HA coatings [35–39]. Due to the concerns for this HA resorption and de-bonding, standards for HA coating were developed by the ISO and ASTM organizations. As per the makers, the stem evaluated in this study is in compliance with these standards, making the occurrence of degradation and de-bonding less likely. In our cohort, when the removed stems were examined, they showed a uniformed loss of HA coating in both a case of late peri-prosthetic fracture and aseptic loosening. This resorption, however, has been described in literature, along with accounts that thorough bonding of bone to the titanium stem was visualized even in cases of full resorption [40]. There was no evidence of de-bonding of HA coating among our retrieved stems (Fig. 4).
Fig. 4.

Retrieved element stem. A Element Stem prior to implantation. B Element stem retrieved after revision for aseptic loosening. Demonstrated is the uniform loss of hydroxyapatite coating, likely secondary to resorption and abrasion
Morphology of the proximal femur can affect the initial fit of the stem preventing the stability necessary for osseo-integration. One of the proposed fixation mechanisms with wedge-shaped implants is distal potting. Distal potting occurs when the diaphyseal aspect of the stem pots between thick cortical diaphyseal bones. This might leave the proximal portion of the stem less secure, resulting in motion responsible for later radiolucencies. The absence of stress shielding in our cases is consistent with proximal bone loading. However, in our cohort, no distal potting was seen for any of the stems with aseptic loosening, making this a less likely explanation for the loosening observed. All stems with aseptic loosening were Dorr B canals. There was no association between stem size or offset and aseptic loosening. There was also a concern that the use of the Charnley tapered reamer prior to broaching might have displaced bone beyond the dimensions of the smaller stems distally. However, smaller stems did not correlate with loosening in our series and we did not see any early distal radiolucencies in hips with small stem sizes (Size 8, 9).
The Element Stem has many design concepts similar to the Corail stem. The Corail stem is well documented in the literature, but little has been described of other more similar stems. Vidalain et al. prospectively evaluated long-term 20-year outcomes with use of the cementless Corail femoral stem and found a survival probability of 97.7% at 15 years and 96.3% at 23 years [21]. Buttaro et al. also described favorable long-term results, but described an uncommon complication of the stem, with a 2.1% metaphyseal de-bonding at mid-term follow-up, primarily in patients with Dorr B-type femurs and elevated BMI [41]. Due to the limited literature for similar stems, we elected to describe our mid-term outcomes with use of the Element Stem.
There are limitations associated with this study. First, there are inherent limitations due to the retrospective nature of this study, such as having incomplete data sets, with some necessary imaging and clinical scores not available for all patients. A relatively small samples size due to loss of follow-up is a concern, although sample size was comparable to some other critical analysis studies regarding total hip stem outcomes. This necessitated that 3 separate cohorts be reported for clinical, radiographic and survival data as it was important to report on the largest cohort of patients available regarding a specific variable. This study included various different polyethylene liners that were used during the study period, which may be confounding in nature for evaluating osteolysis and other radiographic measurements. Next, with only mid-term 5-year follow-up, further long-term studies are necessary to further elucidate survival of this femoral stem. Finally, though our clinical outcomes were overall positive, the lack of consistent pre-operative clinical scores does not allow us to demonstrate the extent to which our patients improved after surgery. Despite the mentioned limitations, a comprehensive report of the survival and outcome data regarding this stem was performed.
Conclusion
The 5-year survival rate of this dual tapered-wedge fully HA-coated stem with all revisions as an end point in this diverse patient population is 92.4% and with aseptic loosening as an end point is 96.2%. In patients with osteoporotic bone, early proximal medial fracture remains a concern with this implant. The use of a proximal prophylactic cerclage or a cemented stem might be considered in these cases. The phenomenon of proximal radiolucencies progressing to aseptic loosening post-operatively is unusual but concerning and will require further study. The 11.5% rate of subsidence is comparable to other fully HA-coated collarless stems and has been clinically asymptomatic. The rate might be lower with the use of the collared version of the stem. The clinical outcomes are good with high OHS, HSS, and satisfactions scores among most patients. Studies with larger sample sizes and longer follow-up are still necessary to more fully understand the performance of this implant.
Funding
One author has received financial support from Exactech Inc., Gainsvesille, FL for the purposes of this study (R.P.R). There was no company involvement in the results and creation of our manuscript.
Declarations
Conflict of interest
One author is a paid consultant for Exactech., Inc, and Stryker, Inc (Athens Michigan) (R.P.R.).
Ethical approval
IRB approval was obtained prior to beginning the study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ramakanth R. Yakkanti, Email: ramakanth.yakkanti@jhsmiami.org
Dylan N. Greif, Email: d.greif@med.miami.edu
Dennis J. Vanden Berge, Email: dennis.vandenberge@jhsmiami.org.
Raymond P. Robinson, Email: RRobinson5@med.miami.edu
References
- 1.Lehil MS, Bozic KJ. Trends in total hip arthroplasty implant utilization in the United States. J Arthroplasty. 2014;29(10):1915–1918. doi: 10.1016/j.arth.2014.05.017. [DOI] [PubMed] [Google Scholar]
- 2.Murray DW. Cemented femoral fixation: the North Atlantic divide. Bone Jt J. 2013;95:51–52. doi: 10.1302/0301-620X.95B11.32976. [DOI] [PubMed] [Google Scholar]
- 3.Hutt J, Hazlerigg A, Aneel A, Epie G, Dabis H, Twyman R, et al. The effect of a collar and surface finish on cemented femoral stems: a prospective randomised trial of four stem designs. Int Orthop. 2014;38(6):1131–1137. doi: 10.1007/s00264-013-2256-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Junnila M, Laaksonen I, Eskelinen A, et al. Implant survival of the most common cemented total hip devices from the Nordic Arthroplasty Register Association database. Acta Orthop. 2016;87(6):546–553. doi: 10.1080/17453674.2016.1222804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warth L, Callaghan J, Liu S, et al. Thirty-five-year results after Charnley total hip arthroplasty in patients less than fifty years old. A concise follow-up of previous reports. J Bone Jt Surg Am. 2014;96(21):1814–1819. doi: 10.2106/JBJS.M.01573. [DOI] [PubMed] [Google Scholar]
- 6.Wyatt M, Hooper G, Frampton C, Rothwell A. Survival outcomes of cemented compared to uncemented stems in primary total hip replacement. World J Orthop. 2014;5(5):591–596. doi: 10.5312/wjo.v5.i5.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Foster A, Thompson N, Wong J, Charlwood A. Periprosthetic femoral fractures–a comparison between cemented and uncemented hemiarthroplasties. Injury. 2005;36(3):424–429. doi: 10.1016/j.injury.2004.07.023. [DOI] [PubMed] [Google Scholar]
- 8.Ries C, Boese C, Dietrich F, Miehlke W, Heisel C. Femoral stem subsidence in cementless total hip arthroplasty: a retrospective single-centre study. Int Orthop. 2019;43(2):307–314. doi: 10.1007/s00264-018-4020-x. [DOI] [PubMed] [Google Scholar]
- 9.Gkagkalis G, Goetti P, Mai S, Meinecke I, Helmy N, Bosson D, et al. Cementless short-stem total hip arthroplasty in the elderly patient is it a safe option?: a prospective multicentre observational study. BMC Geriatr. 2019;19(1):112. doi: 10.1186/s12877-019-1123-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Willburger RE, Heukamp M, Lindenlaub P, Efe T, Peterlein CD, Schüttler KF. Excellent midterm survival and functional outcomes of a fully hydroxyapatite-coated cementless stem: first results of a prospective multicenter study. Arthroplast Today. 2020;6(2):201–205. doi: 10.1016/j.artd.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Critchley O, Callary S, Mercer G, Campbell D, Wilson C. Long-term migration characteristics of the corail hydroxyapatite-coated femoral stem: a 14-year radiostereometric analysis follow-up study. Arch Orthop Trauma Surg. 2020;140(1):121–127. doi: 10.1007/s00402-019-03291-8. [DOI] [PubMed] [Google Scholar]
- 12.Louboutin L, Viste A, Desmarchelier R, Fessy MH. Long-term survivorship of the Corail™ standard stem. Orthop Traumatol Surg Res. 2017;103(7):987–992. doi: 10.1016/j.otsr.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 13.Horváth T, Hanák L, Hegyi P, Butt E, Solymár M, Szűcs Á, et al. Hydroxyapatite-coated implants provide better fixation in total knee arthroplasty. A meta-analysis of randomized controlled trials. PLoS ONE. 2020;15(5):e0232378. doi: 10.1371/journal.pone.0232378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Castellini I, Andreani L, Parchi PD, Bonicoli E, Piolanti N, Risoli F, et al. Hydroxyapatite in total hip arthroplasty. Our experience with a plasma spray porous titanium alloy/hydroxyapatite double-coated cementless stem. Clin Cases Miner Bone Metab. 2016;13(3):221–227. doi: 10.11138/ccmbm/2016.13.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kelly SJ, Robbins CE, Bierbaum BE, Bono JV, Ward DM. Use of a hydroxyapatite-coated stem in patients with Dorr Type C femoral bone. Clin Orthop Relat Res. 2007;465:112–116. doi: 10.1097/BLO.0b013e318156bf96. [DOI] [PubMed] [Google Scholar]
- 16.Godoy-Monzon D, Sasaki S, Svarzchtein S (2019) 9 Years follow up of a fully covered hydroxyapatite femoral stem. J Orthop Muscular Syst Res
- 17.Magill P, Hill J, O'Brien S, Stevenson M, Machenaud A, Beverland D. Observed effect of femoral component undersizing and a collarless design in the development of radiolucent lines in cementless total hip arthroplasty. Arthroplast Today. 2020;6(1):99–103. doi: 10.1016/j.artd.2019.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robinson RP, Deysine GR, Green TM. Uncemented total hip arthroplasty using the CLS stem: a titanium alloy implant with a corundum blast finish. Results at a mean 6 years in a prospective study. J Arthroplasty. 1996;11(3):286–292. doi: 10.1016/S0883-5403(96)80080-5. [DOI] [PubMed] [Google Scholar]
- 19.Robinson RP, Lovell TP, Green TM. Hip arthroplasty using the cementless CLS stem. A 2–4-year experience. J Arthroplasty. 1994;9(2):177–192. doi: 10.1016/0883-5403(94)90067-1. [DOI] [PubMed] [Google Scholar]
- 20.Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993;14(3):231–242. doi: 10.1016/8756-3282(93)90146-2. [DOI] [PubMed] [Google Scholar]
- 21.Vidalain JP. Twenty-year results of the cementless Corail stem. Int Orthop. 2011;35(2):189–194. doi: 10.1007/s00264-010-1117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shetty AA, Slack R, Tindall A, James KD, Rand C. Results of a hydroxyapatite-coated (Furlong) total hip replacement: a 13- to 15-year follow-up. J Bone Jt Surg Br. 2005;87(8):1050–1054. doi: 10.1302/0301-620X.87B8.16011. [DOI] [PubMed] [Google Scholar]
- 23.Froimson MI, Garino J, Machenaud A, Vidalain JP. Minimum 10-year results of a tapered, titanium, hydroxyapatite-coated hip stem: an independent review. J Arthroplasty. 2007;22(1):1–7. doi: 10.1016/j.arth.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 24.Søballe K, Toksvig-Larsen S, Gelineck J, Fruensgaard S, Hansen ES, Ryd L, et al. Migration of hydroxyapatite coated femoral prostheses. A Roentgen Stereophotogrammetric study. J Bone Joint Surg Br. 1993;75(5):681–687. doi: 10.1302/0301-620X.75B5.8397213. [DOI] [PubMed] [Google Scholar]
- 25.Cypres A, Fiquet A, Girardin P, Fitch D, Bauchu P, Bonnard O, et al. Long-term outcomes of a dual-mobility cup and cementless triple-taper femoral stem combination in total hip replacement: a multicenter retrospective analysis. J Orthop Surg Res. 2019;14(1):376. doi: 10.1186/s13018-019-1436-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Erivan R, Villatte G, Brientini JM, Kreider D, Descamps S, Boisgard S. 7-year results of primary total hip arthroplasty with the uncemented Avenir stem. Hip Int. 2019;29(4):418–423. doi: 10.1177/1120700018810211. [DOI] [PubMed] [Google Scholar]
- 27.Hallan G, Lie SA, Furnes O, Engesaeter LB, Vollset SE, Havelin LI. Medium- and long-term performance of 11,516 uncemented primary femoral stems from the Norwegian arthroplasty register. J Bone Jt Surg Br. 2007;89(12):1574–1580. doi: 10.1302/0301-620X.89B12.18969. [DOI] [PubMed] [Google Scholar]
- 28.Gabbar OA, Rajan RA, Londhe S, Hyde ID. Ten- to twelve-year follow-up of the furlong hydroxyapatite-coated femoral stem and threaded acetabular cup in patients younger than 65 years. J Arthroplasty. 2008;23(3):413–417. doi: 10.1016/j.arth.2007.01.027. [DOI] [PubMed] [Google Scholar]
- 29.Al-Najjim M, Khattak U, Sim J, Chambers I. Differences in subsidence rate between alternative designs of a commonly used uncemented femoral stem. J Orthop. 2016;13(4):322–326. doi: 10.1016/j.jor.2016.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Demey G, Fary C, Lustig S, Neyret P, Tarik siSelmi P. Does a collar improve the immediate stability of uncemented femoral hip stems in total hip arthroplasty? A bilateral comparative cadaver study. J Arthroplasty. 2011;26(8):1549–1555. doi: 10.1016/j.arth.2011.03.030. [DOI] [PubMed] [Google Scholar]
- 31.Johnson AJ, Desai S, Zhang C, Koh K, Zhang LQ, Costales T, et al. A calcar collar is protective against early torsional/spiral periprosthetic femoral fracture: a paired cadaveric biomechanical Analysis. J Bone Jt Surg Am. 2020;102(16):1427–1433. doi: 10.2106/JBJS.19.01125. [DOI] [PubMed] [Google Scholar]
- 32.Rattanaprichavej P, Laoruengthana A, Chotanaphuti T, Khuangsirikul S, Phreethanutt C, Pongpirul K. Subsidence of hydroxyapatite-coated femoral stem in dorr type C proximal femoral morphology. J Arthroplasty. 2019;34(9):2011–2015. doi: 10.1016/j.arth.2019.05.017. [DOI] [PubMed] [Google Scholar]
- 33.Ponzio DY, Shahi A, Park AG, Purtill JJ. Intraoperative proximal femoral fracture in primary cementless total hip arthroplasty. J Arthroplasty. 2015;30(8):1418–1422. doi: 10.1016/j.arth.2015.02.043. [DOI] [PubMed] [Google Scholar]
- 34.Thomas WC, Parvataneni HK, Vlasak RG, Gray CF. Early polyethylene failure in a modern total hip prosthesis: a note of caution. J Arthroplasty. 2020;35(5):1297–1302. doi: 10.1016/j.arth.2019.12.043. [DOI] [PubMed] [Google Scholar]
- 35.Collier JP, Surprenant VA, Mayor MB, Wrona M, Jensen RE, Surprenant HP. Loss of hydroxyapatite coating on retrieved, total hip components. J Arthroplasty. 1993;8(4):389–393. doi: 10.1016/S0883-5403(06)80037-9. [DOI] [PubMed] [Google Scholar]
- 36.Tonino AJ, Thèrin M, Doyle C. Hydroxyapatite-coated femoral stems. Histology and histomorphometry around five components retrieved at post mortem. J Bone Jt Surg Br. 1999;81(1):148–154. doi: 10.1302/0301-620X.81B1.0810148. [DOI] [PubMed] [Google Scholar]
- 37.Tonino AJ, van der Wal BC, Heyligers IC, Grimm B. Bone remodeling and hydroxyapatite resorption in coated primary hip prostheses. Clin Orthop Relat Res. 2009;467(2):478–484. doi: 10.1007/s11999-008-0559-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jansen JA, van de Waerden JP, Wolke JG, de Groot K. Histologic evaluation of the osseous adaptation to titanium and hydroxyapatite-coated titanium implants. J Biomed Mater Res. 1991;25(8):973–989. doi: 10.1002/jbm.820250805. [DOI] [PubMed] [Google Scholar]
- 39.Svehla M, Morberg P, Bruce W, Zicat B, Walsh WR. The effect of substrate roughness and hydroxyapatite coating thickness on implant shear strength. J Arthroplasty. 2002;17(3):304–311. doi: 10.1054/arth.2002.30410. [DOI] [PubMed] [Google Scholar]
- 40.Aebli N, Krebs J, Schwenke D, Stich H, Schawalder P, Theis JC. Degradation of hydroxyapatite coating on a well-functioning femoral component. J Bone Jt Surg Br. 2003;85(4):499–503. doi: 10.1302/0301-620X.85B4.13605. [DOI] [PubMed] [Google Scholar]
- 41.Buttaro MA, Oñativia JI, Slullitel PA, Andreoli M, Comba F, Zanotti G, Piccaluga F. Metaphyseal debonding of the Corail collarless cementless stem: report of 18 cases and case-control study. Bone Jt J. 2017;99(11):1435–1441. doi: 10.1302/0301-620X.99B11.BJJ-2017-0431.R1. [DOI] [PubMed] [Google Scholar]