Abstract
Objective
To investigate the use of custom-made knee-ankle-foot orthoses in daily life and differences in usability factors of knee-ankle-foot orthoses between users and discontinued users.
Design
Cross-sectional survey study.
Subjects
A total of 163 polio survivors provided with a knee-ankle-foot orthosis at an outpatient clinic of a university hospital.
Methods
Use and usability of knee-ankle-foot orthoses in daily life were assessed with a postal questionnaire. Usability factors were formulated using the International Organization for Standardization (ISO) 9241-11 standard.
Results
A total of 106 respondents (65%) returned the questionnaire. Of these, 98 were eligible for analysis. Seventy-four respondents (76%) reported using their knee-ankle-foot orthosis. Compared with discontinued users (24%), users experienced more limitations when walking without an orthosis (p = 0.001), were more often experienced with wearing a previous orthosis (p < 0.001) and were more often prescribed with a locked rather than a stance-control knee-ankle-foot orthosis (p = 0.015). Furthermore, users reported better effectiveness of their knee-ankle-foot orthosis (p < 0.001), more satisfaction with goals of use and knee-ankle-foot orthosis-related aspects (p < 0.001).
Conclusion
The majority of polio survivors used their custom-made knee-ankle-foot orthoses in daily life. Factors related to continued use, such as walking ability without orthosis, expectations of the orthosis, previous orthosis experience and type of knee-ankle-foot orthosis provided, should be considered and discussed when prescribing a knee-ankle-foot orthosis in polio survivors.
LAY ABSTRACT
Knee-ankle-foot orthoses for knee instability are commonly prescribed in polio survivors to enhance safe ambulation. This survey investigated the use of knee-ankle-foot orthoses in daily life and differences in factors of usability between users and discontinued users. Seventy-six percent of polio survivors used their custom-made knee-ankle-foot orthosis in daily life. Important usability factors that were related to continued use of knee-ankle-foot orthoses were low perceived walking ability status without orthosis, previous orthosis experience, high perceived effectiveness and satisfaction when standing and walking with a knee-ankle-foot orthoses. When prescribing a custom-made knee-ankle-foot orthoses it is important to consider these factors and discuss goals of use and expected benefits of the knee-ankle-foot orthoses with the patient, especially in relation to perceived walking limitations and activities in daily life.
Key words: poliomyelitis, leg muscle weakness, knee-anklefoot orthoses, usability, physical mobility, rehabilitation
Neuromuscular diseases, such as poliomyelitis, can leave individuals with permanent lower extremity muscle weakness, often including the quadriceps among other proximal lower limb muscles (1). This may cause knee instability during standing and walking, increasing the risk of falling (2, 3). Compensatory actions to prevent falling, such as excessive knee-(hyper)extension and forward trunk lean, may lead to knee and/or back pain (3) and to fatigue due to the increased energy cost of walking (4, 5). These commonly reported mobility problems in polio survivors (1, 6) may negatively affect functioning in daily life (5, 7, 8).
Knee-ankle-foot orthoses (KAFOs) are intended to enhance safe ambulation (3) by ensuring stability during standing and walking, while also reducing walking energy cost (9). The most frequently prescribed KAFOs are locked KAFOs and stance-control KAFOs (SC-KAFOs). Locked KAFOs feature a knee joint that is locked during both the stance and swing phase of gait, while SC-KAFOs are equipped with a stance-control knee joint that locks during the stance phase, but permits knee flexion during swing (10, 11). These KAFOs often need to be custom-made, as, along with lower extremity muscle weakness, many polio survivors have contractures and misalignments of joints.
While (custom-made) KAFOs are commonly applied in rehabilitation treatment of polio survivors for lower extremity muscle weakness with knee instability, little research has been done on the use and usability of these orthotic devices. Studies addressing orthosis use in individuals with polio residuals have focused mainly on ankle-foot orthoses (AFOs) (12, 13), results that cannot be generalized to the use of KAFOs. It is therefore still unclear which usability factors influence an individual’s decision to use their KAFO, usability in this context being defined as “the extent to which a product can be used by specified users to achieve specified goals with effectiveness, efficiency and satisfaction in a specified context of use” (14). A recent qualitative study in a relatively small sample of KAFO users indicated that several usability factors, including perceived effectiveness and satisfaction, correlated with participants’ reports of KAFO use or discontinued use (15), but no study to date has addressed differences in these factors between users and discontinued users. A better understanding of factors of usability and their relation to KAFO use would help to further improve KAFO applications in clinical practice. We therefore conducted a cross-sectional survey among polio survivors to retrospectively evaluate the use and usability of custom-made KAFOs provided in clinical practice. Our specific research questions were: (i) What is the use of custom-made KAFOs in daily life?, and (ii) How do users and discontinued users differ in terms of usability factors, such as context of use, perceived effectiveness and satisfaction with the prescribed KAFO?
METHODS
Participants
In this cross-sectional survey, reporting was in accordance with Strengthening Reporting of Observational Studies in Epidemiology (STROBE) recommendations (16). Participation in the survey was by invitation and included all adult polio survivors provided with a custom-made KAFO (both newly prescribed KAFOs and repeat prescriptions) between January 2004 and November 2015 at our outpatient polio and orthotic expert clinic at the Amsterdam UMC, location Academic Medical Centre, Amsterdam, the Netherlands. Polio survivors for whom the KAFO indication had changed (as retrieved from the medical records) due to an altered medical condition were ineligible. Study information, the use and usability questionnaire and a stamped addressed return envelope were posted to all potentially eligible individuals. As the study concerned a survey and participants were not subjected to any burdensome tests or behavioural obligations, the study did not fall under the Medical Research Involving Human Subjects Act (Article 21 paragraph 1 sub b) and the requirement for ethical review of the study was waived by the local ethics committee on 25 August 2015.
Description of the intervention
The KAFOs used by participants in this study were prescribed in a polio and orthosis expert centre. All KAFOs were fabricated of carbon composite and custom-made by the same orthosis company (OIM Orthopedie, Noordwijkerhout, the Netherlands). The choice for KAFO type (locked KAFO vs SC-KAFO) was made by a rehabilitation physician together with a senior orthotist, following a standardized intake, physical examination and 3D gait analysis (11). Based on the outcomes, the required orthotic functions to reach the desired goals of the patient were determined. For a SC-KAFO, contraindications, such as knee flexion contractures (>10–15°), non-correctable varus/valgus deformities, cognitive disorders or ischial weight-bearing (17, 18) were checked to ensure that prescription of a SC-KAFO was suitable. A knee joint with bale lock (Otto Bock Healthcare, GmbH, Duderstadt, Germany) was used for locked KAFOs, and the following knee joints were used for SC-KAFOs: Swing Phase Lock (Basko Healthcare B.V., Zaandam, the Netherlands), E-MAG Active (Otto Bock Healthcare, GmbH, Duderstadt, Germany), and NEURO MATIC and NEURO TRONIC (Fior & Gentz, GmbH, Lüneburg, Germany).
Questionnaire
The international ISO 9241-11 standard “Guidance of usability” (14) was used to identify factors relevant to the measurement of use and usability, which included orthosis use in daily life, goals of use, context of use, perceived effectiveness on goals of use and satisfaction. To evaluate usability factors, a validated questionnaire was supplemented with custom-designed questions related to perceived effectiveness and satisfaction concerning goals of use. Individuals were asked to respond to questions based on their most recently delivered KAFO. Individuals who did not return the questionnaire within 2 months received a reminder together with a new questionnaire. When the questionnaire was still not returned following the reminder, individuals were contacted by phone to ask if the questionnaire had been received and whether they would be willing to complete and return it. Individuals who still did not return a completed questionnaire after the call were considered non-respondents. Socio-demographic data (e.g. age, sex, ethnicity) on both the respondents and non-respondents were retrieved from the patients’ medical records and used for comparison.
Orthosis use
Individuals were asked if they used their KAFO in daily life (yes/no). If the answer was no, 8 predefined reasons for discontinued use were offered, from which multiple reasons could be selected, together with the opportunity to provide an open answer. If the KAFO was being used, frequency of use (in days per week) and daily wearing time (in h) were noted. Mean daily wearing time (in h per day) was calculated based on daily wearing time multiplied by the reported number of days per week the KAFO was worn, divided by 7 (days).
Goals of use
Goals of using the KAFO were inventoried by 11 predefined possible answers concerning standing and walking-related problems, along with an open-answer option to describe additional goals of use, where applicable. Multiple answers were allowed.
Context of use
Context of use refers to a description of user characteristics, tasks, equipment and the environment in which the orthosis is used (14). Regarding “user characteristics”, questions concerning socio-demographics, walking ability status and health status were asked. Walking ability status was described as self-reported functional ambulation when walking without orthosis and classified as 1 of 3 levels (inside and around the house only; rarely more than 1 km; often more than 1 km (19)), and by the experience of goals of use when standing/walking without orthosis (7-point Likert Scale, ranging from very badly [1] to very well [7]). Health status was measured with the Dutch version of the Short Form Health Survey physical functioning and mental functioning (with scores ranging from 0 to 100, with 100 being the maximal score) (20).
“Tasks” were inventoried based on questions covering whether this was the participant’s first-ever orthosis and the duration of orthosis use (in years). “Equipment” and “environment” were defined as the participants most recently received KAFO type (locked KAFO or SC-KAFO) and how often the KAFO was used indoors and outdoors, respectively.
Perceived effectiveness
Perceived effectiveness was expressed as the score for goals of use when standing/walking with the KAFO minus the score with out the KAFO. In addition, an overall perceived effectiveness score was calculated based on the mean score of all goals of use.
Satisfaction
Satisfaction was measured with the Dutch version of the Quebec User Evaluation of Satisfaction with Assistive Technology (D-QUEST), which has good reliability (21). For analysis, the mean scores of the 2 sub-scales (satisfaction related to orthosis aspects and satisfaction with provided services) were calculated (21). In addition, self-designed multiple-choice questions were posed regarding satisfaction with the KAFO in terms of goals of use.
Statistical analysis
Statistical analyses were carried out in SPSS version 24 (IBM Company, Armonk, NY, USA). Data were not normally distributed. Missing values were not imputed and individuals with missing data were not discarded. For each specific analysis, tables. Descriptive statistics (numbers, percentages, medians [interquartile range (IRQ)] were used to describe the study population, orthosis use, goals of use, context of use, perceived effectiveness and satisfaction. Differences in context of use, perceived effectiveness and satisfaction with the D-QUEST between users and discontinued users were tested for categorical data with a Fisher’s exact test and for continuous data with a Mann–Whitney U test. Perceived effectiveness (per goal of use and overall) between walking with and without KAFO among users and discontinued users was analysed with a Wilcoxon signed-rank test. The level of statistical significance was set at p < 0.05.
RESULTS
Participants
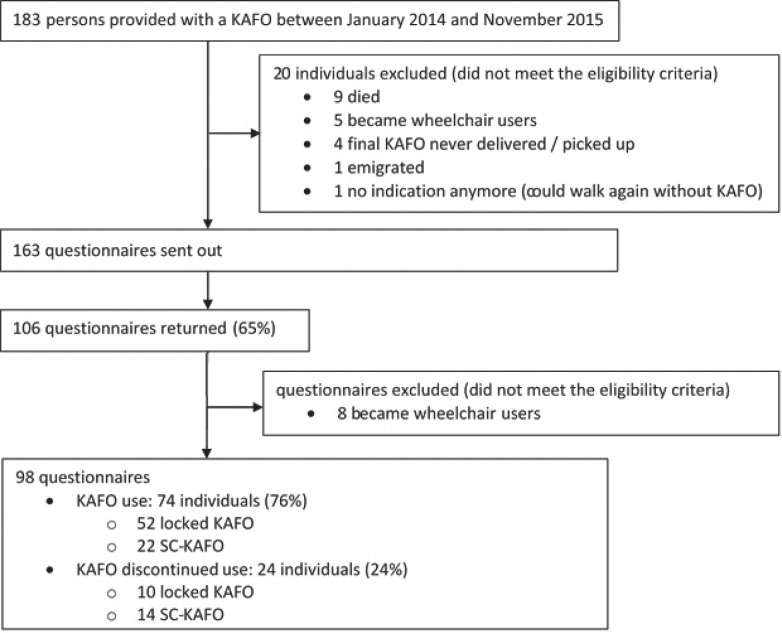
Between January 2004 and November 2015, a custom-made KAFO was provided to 183 polio survivors, of whom 9 individuals were now deceased and 11 individuals failed to meet the eligibility criteria for a variety of reasons (Fig. 1). The remaining 163 individuals were sent a questionnaire and 106 returned the questionnaire (response rate: 65%). Respondents were significantly older than non-respondents (mean (standard deviation; SD) age: 63.3 (12.4) vs 52.0 (12.4) years, p = 0.011) and more often Caucasian (78% vs 39%, p < 0.001). Eight respondents, who had become wheelchair dependent and had therefore discontinued using their KAFO were excluded, leaving 98 respon dents in the final analysis. The median [interquartile range; IQR] time elapsed between most recent KAFO delivery and completion of the questionnaire was 2.6 [1.7–3.8] years for KAFO users and 3.3 [2.0–7.3] years (p = 0.049) years for discontinued users.
Fig. 1.
Flow-cart of the study population and information on use. KAFO: knee-ankle-foot orthosis, SC: stance-control.
Orthosis use
Seventy-four individuals (76%) used their KAFO, with a median [IQR] wearing time of 13 [9.3–13.0] h per day. Twenty-four individuals (24%) reported not using their KAFO (Table I).
Table I.
Characteristics of users vs discontinued users
| Users (n = 74) | Discontinued users (n = 24) | p– value | |
|---|---|---|---|
| Age, years | 64 [60–75] | 64 [54–68] | 0.313 |
| Polio at age, years | 2 [1–4]g | 2 [1–3]d | 0.309 |
| Sex (male/female) | 35/39 | 15/9 | 0.243 |
| Marital status (living not alone/living alone) | 51/23 | 18/6 | 0.619 |
| Level of education (basic/high) | 37/34e | 12/8d | 0.616 |
| Ethnicity (Caucasian/other) | 59/15 | 17/7 | 0.404 |
| Functional ambulation level without orthosisb | 29/13/0c | 11/8/1d | 0.001* |
| Functional ambulation level with orthosisb | 46/21/7 | N/A | N/A |
| SF-36 physical component summary score (0–100) | 33 [27–40] | 32 [23–43]f | 0.768 |
| SF-36 mental component summary score (0–100) | 55 [45–61] | 52 [39–60]f | 0.435 |
| First orthosis (yes/no)a, (%) | 11 (15)/63 (85) | 14 (58)/10 (42) | 0.001* |
| Orthosis type (locked KAFO/SC-KAFO)a | 52 (70)/22 (30) | 10 (42)/14 (58) | 0.015* |
Data reported as median [interquartile range] or number.
Reported as number of participants (percentage).
Inside and around house only/rarely more than 1 km/often more than 1 km,
31 individuals could not walk without orthosis.
4 missing,
3 missing,
5 missing,
13 missing.
KAFO: knee-ankle-foot orthosis; SC: stance-control; N/A: not applicable; SF-36: 36-item Short Form Survey.
Significantly different between users and discontinued users; p < 0.05.
The reported predefined reasons for discontinued were “hinders activities” (n = 9), “not reducing the problem” (n = 6), “uncomfortable fitting” (n = 6), “could not get used to it” (n = 4), “able to walk again without KAFO” (n = 3) and “too heavy” (n = 2). Sixteen individuals mentioned additional reasons, including pain related to KAFO use (n = 3), pain unrelated to KAFO use (n = 2), fitting problems due to leg oedema or weight gain (n = 2), problems with knee joint securing (n = 1), and a defective knee joint (n = 1).
Goals of use
The most frequently mentioned goals of use for which the KAFO was prescribed were improving stability when walking (67%) or standing (56%) and improving walking performance in terms of distance, speed or duration (45%) (Table II). The median number of reported goals of use was 3 [IQR 1–5], with users reporting significantly more goals of use compared with discontinued users (users 4 [2–6] vs discontinued users 2 [1–3], p = 0.004).
Table II.
Goals of use
| Total (n = 98) | Users (n = 74) | Discontinued users (n = 24) | p- value | |
|---|---|---|---|---|
| Improving stability walking, n (%) | 66 (67) | 54 (73) | 12 (50) | 0.047* |
| Improving stability standing, n (%) | 55 (56) | 47 (64) | 8 (33) | 0.017* |
| Improving walking distance/speed/duration, n (%) | 44 (45) | 35 (47) | 9 (38) | 0.482 |
| Less effort walking, n (%) | 36 (37) | 33 (45) | 3 (13) | 0.006* |
| Less falling, n (%) | 33 (34) | 28 (38) | 5 (21) | 0.144 |
| Less fatigue walking, n (%) | 31 (32) | 26 (35) | 5 (21) | 0.218 |
| Less effort standing, n (%) | 28 (29) | 26 (35) | 5 (21) | 0.017* |
| Less fatigue standing, n (%) | 25 (26) | 23 (31) | 7 (21) | 0.031* |
| Less back pain, n (%) | 19 (19) | 17 (23) | 2 (8) | 0.145 |
| Less pain in orthosis leg, n (%) | 9 (9) | 7 (10) | 2 (8) | 1.000 |
| Less pain in non-orthosis leg, n (%) | 7 (7) | 5 (7) | 2 (8) | 1.000 |
| Other purpose, n (%) | 21 (21) | 16 (22) | 4 (11) | 1.000 |
| Number of goals per subjecta | 3 [1.0–5.3] | 4 [2.0–6.0] | 2 [1.0–3.0] | 0.004* |
Data are expressed as number (percentage) of participants.
Reported as median [interquartile range; IQR].
Significant difference between users and discontinued users; p < 0.05.
Differences between users and discontinued users regarding usability
Context of use
Users reported a lower functional ambulation level without orthosis (p < 0.001, Table I) and had a significantly lower median [IQR] overall score for standing- and walking-related goals of use compared with discontinued users (score users 2.1 [0.4–2.8] vs discontinued users 3.6 [1.9–4.1], p = 0.001 (Table III).
Table III.
Experience when walking with and without knee-ankle-foot orthosis (KAFO) and perceived effectiveness for users vs discontinued users
| Users (n = 74) |
Discontinued users (n = 24) |
Users vs discontinued users |
||||||
|---|---|---|---|---|---|---|---|---|
| Without KAFO | With KAFO | Delta | Withou KAFO | With KAFO | Delta | p-value without KAFO** | p-value with KAFO** | |
| Distance of walking | 1.0 [0.0–1.0] n = 70 |
3.0 [2.0–5.0] n = 67 |
2.0 [1.0–3.0] *p < 0.001 |
3.0 [1.3–4.0] n = 16 |
2.0 [1.0–4.0] n = 15 |
0.0 [–1.0–0.0] | 0.000** | 0.082 |
| Speed of walking | 1.0 [0.0–1.0] n = 70 |
3.0 [1.0–4.0] n = 67 |
1.0 [1.0–3.0] *p < 0.001 |
3.0 [1.0–4.0] n = 16 |
2.0 [1.0–3.0] n = 15 |
0.0 [–2.0–0.0] | 0.002** | 0.133 |
| Duration of walking | 1.0 [0.0–1.0] n = 70 |
3.0 [2.0–4.0] n = 67 |
2.0 [1.0–3.0] *p < 0.001 |
2.5 [1.0–4.0] n = 16 |
3.0 [1.0–4.0] n = 15 |
0.0 [–1.5–1.8] | 0.000** | 0.740 |
| Stability during walking | 1.0 [0.0–1.0] n = 70 |
5.0 [3.0–6.0] n = 67 |
4.0 [2.0–5.0] *p < 0.001 |
2.5 [1.0–4.0] n = 16 |
3.5 [2.3–5.0] n = 16 |
0.5 [–0.8–2.8] | 0.000** | 0.054 |
| Stability during standing |
1.0 [0.0–1.0] n = 68 |
4.5 [4.0–6.0] n = 68 |
3.0 [2.0–5.0] *p < 0.001 |
3.0 [1.0–3.8] n = 16 |
4.0 [2.3–5.0] n = 16 |
1.0 [0.0–2.8] *p = 0.023 |
0.000** | 0.160 |
| Amount of falls | 3.0 [1.0–5.0] n = 49 |
6.0 [4.0–7.0] n = 70 |
2.0 [0.5–4.0] *p < 0.001 |
4.5 [3.0–6.0] n = 14 |
5.5 [2.3–6.0] n = 16 |
0.0 [–1.0–0.3] | 0.128 | 0.296 |
| Pain on orthosis leg | 7.0 [2.0–7.0] n = 50 |
6.0 [4.0–7.0] n = 70 |
0.0 [–1.0–1.0] | 4.5 [3.8–6.0] n = 14 |
4.0 [3.0–6.0] n = 15 |
0.0 [–1.0–0.0] *p = 0.038 |
0.318 | 0.005** |
| Pain on non-orthosis leg |
6.0 [2.8–7.0] n = 50 |
6.0 [4.0–7.0] n = 68 |
0.0 [0.0–0.3] | 6.0 [4.5–7.0] n = 13 |
5.5 [3.5–7.0] n = 14 |
0.0 [0.0–0.0] | 0.837 | 0.413 |
| Pain on back | 4.0 [2.0–7.0] n = 50 |
6.0 [4.0–7.0] n = 70 |
0.0 [0.0–2.0] *p = 0.004 |
5.0 [3.0–7.0] n = 14 |
5.0 [3.0–7.0] n = 15 |
0.0 [–0.5–0.0] | 0.480 | 0.397 |
| Fatigue during walking | 1.0 [1.0–2.0] n = 49 |
4.0 [3.0–5.0] n = 69 |
2.0 [0.5–3.0] *p < 0.001 |
3.0 [2.0–4.3] n = 14 |
2.0 [1.0–4.0] n = 15 |
–1.0 [–2.0–0.0] *p = 0.023 |
0.000** | 0.004** |
| Fatigue during standing | 1.0 [1.0–2.3] n = 50 |
4.0 [3.0–6.0] n = 69 |
2.0 [1.0–3.5] *p < 0.001 |
3.0 [2.0–3.3] n = 14 |
3.0 [2.0–6.0] n = 15 |
1.0 [0.0–2.0] *p = 0.023 |
0.009** | 0.504 |
| Effort of walking | 1.0 [0.0–2.0] n = 69 |
4.0 [3.0–5.0] n = 70 |
3.0 [1.0–4.0] *p < 0.001 |
3.0 [1.0–3.0] n = 16 |
2.0 [1.0–4.0] n = 15 |
0.0 [–1.0–1.0] | 0.001** | 0.018** |
| Effort of standing | 1.0 [0.0–2.0] n = 70 |
4.0 [4.0–6.0] n = 69 |
3.0 [2.0–4.0] *p < 0.001 |
3.0 [1.0–3.0] n = 15 |
3.5 [2.0–6.0] n = 14 |
0.5 [0.0–3.0] *p = 0.028 |
0.002** | 0.541 |
| Mean ”overall” score | 2.1 [0.4–2.8] n = 72 |
4.3 [3.8–5.2] n = 68 |
2.2 [1.3–3.2] *p < 0.001 |
3.6 [1.9–4.1] n = 16 |
3.9 [2.6–4.7] n = 16 |
0.1 [–0.6–1.3] | 0.001** | 0.124 |
| Locked KAFO | 1.5 [0.0–2.6] n = 50 |
4.3 [3.7–5.4] n = 48 |
2.4 [1.5–3.4] *p < 0.001 |
2.6 [0.0–4.6] n = 5 |
3.8 [2.7–4.6] n = 5 |
0.2 [–0.7–3.5] | 0.449 | 0.157 |
| SC-KAFO | 2.2 [1.8–3.0] n = 22 |
4.1 [3.7–5.1] n = 22 |
1.9 [1.0–2.3] *p < 0.001 |
3.6 [2.8–4.2] n = 11 |
4.2 [2.5–4.7] n = 11 |
0.0 [–0.7–1.1] | 0.004** | 0.359 |
Data are expressed as median [interquartile range]. Scores range from 1 to 7 with 7 as most positive score. KAFO: knee-ankle-foot orthosis; SC: stance control.
Significant different with KAFO from without KAFO p < 0.05.
Significant different users from discontinued-users p < 0.05.
Among users, the percentage of individuals with a first orthosis was significantly lower (15%) than for discontinued users (58%, p < 0.001). Users were also more likely to have a locked KAFO than a SC-KAFO (70% users with locked KAFO, vs 42% discontinued users with locked KAFO, p = 0.015).
Perceived effectiveness
Users experienced significant improvements in nearly all standing- and walking-related goals of use while wearing their KAFO, whereas discontinued users experienced significant improvements in standing-related goals, but not in walking-related goals. Moreover, those who discontinued use reported worsening of fatigue during walking and pain in the affected leg when wearing the KAFO (Table III). Continued users perceived greater overall effectiveness of their KAFO, as indicated by a significantly larger median [IQR] difference score between walking with and without KAFO compared with discontinued users (users 2.2 [1.3–3.2] vs discontinued users 0.1 [–0.6–1.3], p < 0.001).
Satisfaction
Based on the D-QUEST, users were significantly more satisfied with orthosis-related aspects than discontinued users (median [IQR] score users 4.0 [3.4–4.3] vs discontinued users 2.9 [2.4–3.5], p < 0.001). There was no difference in service-related aspects (score users 4.3 [3.8–4.8] vs discontinued-users 4.0 [3.5–4.4], p = 0.395). Regarding KAFO-related aspects, users were most satisfied with “effectiveness” (82%), and the least with “adjustability” (63%). Discontinued users were most satisfied with “durability” (53%) and least satisfied with “ease of use” and “comfort” (both 18%).
Satisfaction with goals of use (Table IV) revealed that the proportion of users who were (very) satisfied was higher for all standing- and walking-related items compared with discontinued users, with stability during standing (74%) and walking (69%) receiving the highest scores and back pain (40%) and fatigue during walking (41%) scoring the lowest. Discontinued users were not satisfied with fatigue (75%) during walking and the effect on back pain (58%).
Table IV.
Satisfaction on goals of use for users vs discontinued users
| Users (n = 74) |
Discontinued users (n = 24) |
|||||
|---|---|---|---|---|---|---|
| (Very) satisfied, n (%) | Moderately satisfied, n (%) | (Totally) not satisfied, n (%) | (Very) satisfied, n (%) | Moderately satisfied, n (%) | (Totally) not satisfied, n (%) | |
| Distance of walking | 39 (53) | 24 (32) | 11 (15) | 3 (19) | 6 (38) | 7 (44) |
| Speed of walking | 34 (47) | 27 (37) | 12 (16) | 3 (19) | 5 (31) | 8 (50) |
| Duration of walking | 33 (45) | 27 (37) | 14 (19) | 2 (8) | 4 (17) | 10 (42) |
| Stability during walking | 50 (69) | 17 (23) | 6 (8) | 5 (21) | 8 (33) | 5 (21) |
| Stability during standing | 54 (74) | 17 (23) | 2 (3) | 8 (33) | 5 (21) | 5 (21) |
| Pain on orthosis leg | 23 (48) | 23 (48) | 2 (4) | 3 (25) | 4 (33) | 5 (42) |
| Pain on back | 19 (40) | 21 (45) | 7 (15) | 4 (33) | 1 (8) | 7 (58) |
| Fatigue during walking | 30 (41) | 30 (41) | 13 (18) | 0 (0) | 4 (25) | 12 (75) |
| Fatigue during standing | 39 (53) | 28 (38) | 6 (8) | 5 (31) | 6 (38) | 5 (31) |
| Effort of walking | 36 (49) | 28 (38) | 9 (12) | 1 (6) | 7 (41) | 9 (53) |
| Effort of standing | 47 (64) | 24 (32) | 3 (4) | 5 (29) | 8 (47) | 4 (24) |
| Looks | 51 (70) | 17 (23) | 5 (7) | 11 (61) | 3 (17) | 4 (22) |
| Fit | 6 (76) | 12 (16) | 6 (8) | 6 (33) | 4 (22) | 8 (44) |
Data are expressed as number (percentage) of participants. That some numbers do not add up to 74 for the users and 24 for the discontinued users is due to missing values.
DISCUSSION
This study survey included 98 polio survivors with a prescribed custom-made KAFO, and found that 76% continued to use their KAFO, often all day. Users and discontinued users differed regarding several important usability factors. For example, individuals who used their KAFO had a poorer walking ability status compared with discontinued users and were more likely to have experience with wearing an orthosis. Moreover, users reported more goals of use, experienced greater effectiveness in terms of goals of use when wearing the KAFO, and were more satisfied regarding goals of use and KAFO-related aspects, such as effectiveness and durability.
Since this is the first study to focus solely on the daily use of KAFOs by polio survivors, a comparison of the current results with previous data was not possible. However, the figure of 76% use in our survey is comparable to the 73% use of custom-made dorsiflexion-restricting AFOs (DR-AFOs) reported in a recent survey among 35 polio survivors (12), and considerably higher than the 59% daily use of both KAFOs and AFOs in polio survivors 2 months after clinical evaluation at a post-polio clinic (13). However, participants in the latter study were less experienced with wearing an orthosis, as individuals receiving a repeat prescription were not included in the analysis. In view of our finding that first-time orthosis users are more likely to discontinue use, a poorer experience may have contributed to lower daily use. The median daily wearing time in the current study was 13 h per day, considerably higher than the 9 h reported in the aforementioned survey on custom-made DR-AFOs (12). This difference may be due to the difference in study population characteristics. The current study population consisted of, predominantly experienced, KAFO users who were relatively severely affected by lower extremity muscle weakness compared with AFO users (12) and may therefore need to use their KAFO for longer periods during the day.
The main explanations for discontinued use reported in the current study were hindrance during activities, not reducing mobility problems and an uncomfortable fitting, all of which are familiar from earlier findings on lower extremity orthosis use in polio survivors (12, 13) and individuals with other neurological diseases (22). Furthermore, a recent qualitative study that included polio survivors with a KAFO prescribed for knee instability concluded that these issues were the most negative aspects of an orthosis (15). Although hindrance during activities was not further explored in our survey, in clinical practice patients commonly report hindrance from their KAFO when sitting down, climbing stairs or when cycling.
To identify further reasons for KAFO use or disuse, this study compared several usability factors between users and discontinued users. First, we found that individuals who used their KAFO exhibited poorer walking ability compared with discontinued users, as shown by a lower self-reported functional ambulation level and lower overall score on standing- and walking-related goals of use without orthosis. This corroborates a previous finding in polio survivors (12, 13) and individuals with neurological conditions (23) that lower limb orthotics are more likely to be used when mobility problems are very pronounced.
Secondly, our finding that KAFOs are used more frequently when participants had previous experience with wearing an orthosis has not been reported previously. However, our survey could not determine the finer nuances, such as whether this was related to experience immediately prior to the last received KAFO, past experience (e.g. during childhood), or experience wearing a KAFO (locked or SC-KAFO) or with an AFO. The topic “orthosis experience” therefore warrants further investigation in a prospective study. Nevertheless, our finding substantiates the results of a qualitative study that indicated a clear need for intensive support when first receiving an orthotic device, as people need time to adjust to an altered self-image (15), in addition to the practicalities of their KAFO in daily life, such as learning to operate the KAFO and adopting an efficient and functional gait pattern (24).
Thirdly, the current study found that users were more frequently supplied with a locked KAFO rather than a SC-KAFO compared with discontinued users. This was possibly related to the specific selection criteria for a SC-KAFO, including sufficient hip flexor and extensor strength and no major contractures or deformations (17), making individuals who received a SC-KAFO more likely to have a relatively good walking ability status without orthosis (Table III). Therefore, the consequent walking gains with the SC-KAFO may have been relatively limited. This probably explains some of the increased discontinued use. Another factor may have been the increased complexity of successfully delivering a SC-KAFO compared with a locked-KAFO in terms of alignment and (ankle and) knee joint settings, which are necessary to allow the knee joint to work reliably (25, 26). Learning to walk with a SC-KAFO is more difficult (27). Together, these factors probably contributed to the relatively high discontinued use of SC-KAFOs.
Among users, the perceived effectiveness of the KAFO was significantly higher on nearly all standing- and walking-related goals compared with discontinued users, similar to our findings in a sample of polio survivors using custom-made DR-AFOs (12). As discontinued users show a better walking ability without an orthosis, walking gains with a KAFO are most likely lower in this group and may have led individuals to discard their orthosis. This is also reflected by the lower number of reported goals of use for the KAFO in this group compared with the group of KAFO users. A similar trend has been reported previously in polio survivors and people with neurological disorders wearing (custom-made) AFOs and KAFOs (12, 13, 22). Thus, the perceived benefit from wearing a lower limb orthosis seems to be an important factor dictating use.
KAFO users were generally very satisfied, specifically regarding effectiveness, durability and fitting, which are main factors for determining satisfactory use (15, 28), in addition to satisfaction with goals of use. Amongst discontinued users, satisfaction was lowest for ease of use and comfort. Low satisfaction in terms of ease of use can imply problems with donning and doffing of the KAFO, which has been reported previously as a negative aspect of KAFO use in polio survivors (15) and individuals with inclusion body myositis (29). Performing activities such as going up and down stairs, cycling or operating the KAFO may also result in low satisfaction with ease of use (28, 30). It is important that these aspects receive specific attention when delivering a KAFO (11) in order to enhance compliance in using the KAFO (24).
Implications for practice
This study raises several important issues that should form part of shared decision-making when prescribing a custom-made KAFO in rehabilitation care. First, it is important to assess the individual’s self-perceived walking ability when walking without orthosis and to discuss the expected benefits when walking with a KAFO, as well as possible disadvantages, such as hindrance during certain activities of daily living. These issues are particularly important when prescribing a SC-KAFO, as this orthosis is usually prescribed in individuals with a better walking ability status. Furthermore, extra attention throughout the care process is required in the case of individuals with no prior experience of an orthosis. This includes setting goals and discussing expectations, extensive gait training and providing guidance on adjusting to a new self-image. In addition, as a KAFO is not necessarily prescribed for continuous wearing, intermittent use of the KAFO in specific situations (e.g. long walks outside the house) should be discussed in order to achieve more tailored use and enhance compliance. Finally, follow-up visits after delivery of the KAFO are advised to evaluate customization of use in daily life and to alleviate possible bottlenecks in this process (e.g. fitting problems or practical problems).
Strengths and limitations
This is the first study to date to assess the use and usability of custom-made KAFOs in a large group of polio survivors. The response rate to the study questionnaire was good, indicating that the results provide a reliable representation of our population. Nonetheless, the expert setting in which this study took place may limit generalizability to other orthotic care settings. Furthermore, the questionnaire included some self-designed questions that have not yet been validated, and answers may have been coloured by recall bias, especially among discontinued users, since the median time between completing the questionnaire and delivery of the last KAFO was 3.3 years (vs 2.6 years for users). Finally, the number of first-time orthosis users in the user group was probably lower compared with the discontinued user group, as satisfied first-time orthosis users will commonly receive a repeat prescription in the Netherlands after 2 years and accordingly become experienced users. Nevertheless, the proportion of first-time orthosis users in the discontinued-user group is still relatively high, indicating that our aforementioned advice concerning extra attention for this group remains important.
Conclusion
A majority of 76% of the polio survivors provided with a custom-made KAFO used their orthosis in daily life. Important usability factors were low perceived walking ability status without orthosis, previous orthosis experience, prescribed KAFO type, high perceived effectiveness and satisfaction when standing and walking with a KAFO. When prescribing a KAFO, it is important to consider these factors and discuss goals of use and expected benefits of the KAFO with the individuals concerned, especially in relation to perceived walking limitations and activities in daily life. Providing proper guidance and training upon delivery of the KAFO may especially be important in the case of first-time orthosis users.
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Nollet F, Beelen A, Prins MH, de Visser M, Sargeant AJ, Lankhorst GJ, et al. Disability and functional assessment in former polio patients with and without postpolio syndrome. Arch Phys Med Rehabil 1999; 80: 136–143. [DOI] [PubMed] [Google Scholar]
- 2.Bickerstaffe A, Beelen A, Nollet F. Circumstances and consequences of falls in polio survivors. J Rehabil Med 2010; 42: 908–915. [DOI] [PubMed] [Google Scholar]
- 3.Perry J, Clark D. Biomechanical abnormalities of post-polio patients and the implications for orthotic management. NeuroRehabilitation 1997; 8: 119–138. [DOI] [PubMed] [Google Scholar]
- 4.Brehm MA, Nollet F, Harlaar J. Energy demands of walking in persons with postpoliomyelitis syndrome: relationship with muscle strength and reproducibility. Arch Phys Med Rehabil 2006; 87: 136–140. [DOI] [PubMed] [Google Scholar]
- 5.Lygren H, Jones K, Grenstad T, Dreyer V, Farbu E, Rekand T. Perceived disability, fatigue, pain and measured isometric muscle strength in patients with post-polio symptoms. Physiother Res Int 2007; 12: 39–49. [DOI] [PubMed] [Google Scholar]
- 6.Ivanyi B, Nollet F, Redekop WK, de Haan R, Wohlgemuht M, van Wijngaarden JK, et al. Late onset polio sequelae: disabilities and handicaps in a population-based cohort of the 1956 poliomyelitis outbreak in The Netherlands. Arch Phys Med Rehabil 1999; 80: 687–690. [DOI] [PubMed] [Google Scholar]
- 7.Bickerstaffe A, Beelen A, Nollet F. Change in physical mobility over 10 years in post-polio syndrome. Neuromuscul Disord 2015; 25: 225–230. [DOI] [PubMed] [Google Scholar]
- 8.Jensen MP, Alschuler KN, Smith AE, Verrall AM, Goetz MC, Molton IR. Pain and fatigue in persons with postpolio syndrome: independent effects on functioning. Arch Phys Med Rehabil 2011; 92: 1796–1801. [DOI] [PubMed] [Google Scholar]
- 9.Hachisuka K, Makino K, Wada F, Saeki S, Yoshimoto N. Oxygen consumption, oxygen cost and physiological cost index in polio survivors: a comparison of walking without orthosis, with an ordinary or a carbon-fibre reinforced plastic knee-ankle-foot orthosis. J Rehabil Med 2007; 39: 646–650. [DOI] [PubMed] [Google Scholar]
- 10.Hsu JD, Michael JW, Fisk JR. AAOS atlas of orthoses and assistive devices. 4th edn. Nollet F. CTN, editor. Philadelphia: Mosby; 2008. [Google Scholar]
- 11.Brehm M, Nollet F. Beenorthesen bij neuromusculaire aandoeningen. [Leg orthoses in neuromuscular disorders]. Amsterdam: Reed Business; 2014. (in Dutch). [Google Scholar]
- 12.Ploeger HE, Bus SA, Brehm MA, Nollet F. Use and usability of custom-made dorsiflexion-restricting ankle-foot orthoses for calf muscle weakness in polio survivors: a cross-sectional survey. Eur J Phys Rehabil Med 2020; 56: 575–584. [DOI] [PubMed] [Google Scholar]
- 13.Waring WP, Maynard F, Grady W, Grady R, Boyles C. Influence of appropriate lower extremity orthotic management on ambulation, pain, and fatigue in a postpolio population. Arch Phys Med Rehabil 1989; 70: 371–375. [PubMed] [Google Scholar]
- 14.International Organization for Standardization (ISO).. Guidance on usability, 9241-11:1998(E). Geneva: ISO. [Google Scholar]
- 15.McCaughan D, Booth A, Jackson C, Lalor S, Ramdharry G, O’Connor RJ, et al. Orthotic management of instability of the knee related to neuromuscular and central nervous system disorders: qualitative interview study of patient perspectives. BMJ Open 2019; 9: e029313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008; 61: 344–349. [DOI] [PubMed] [Google Scholar]
- 17.Otto Bock HealthCare GmbH.. E-MAG Active – Information for Practitioners. [Date accessed Apr 1, 2021] Available from: https://media.ottobock.com/_web-site/orthotics/e-mag/files/e_mag_active_information_for_specialist_dea-lers.pdf.
- 18.Basko Healthcare - Swing Phase Lock 2 [Available from: https://basko.com/en-en/Products/Orthotic-components/Lower-extremity/Details/Swing-Phase-Lock-2-Orthotic-Knee-Joint?s=spl.
- 19.Brehm MA, Ploeger HE, Nollet F. Self-reported functional ambulation is related to physical mobility status in polio survivors; a cross-sectional observational study. Ann Phys Rehabil Med 2020: 101428. [DOI] [PubMed] [Google Scholar]
- 20.Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol 1998; 51: 1055–1068. [DOI] [PubMed] [Google Scholar]
- 21.Wessels RD, De Witte LP. Reliability and validity of the Dutch version of QUEST 2.0 with users of various types of assistive devices. Disabil Rehabil 2003; 25: 267–272. [DOI] [PubMed] [Google Scholar]
- 22.Swinnen E, Lafosse C, Van Nieuwenhoven J, Ilsbroukx S, Beckwee D, Kerckhofs E. Neurological patients and their lower limb orthotics: an observational pilot study about acceptance and satisfaction. Prosthet Orthot Int 2017; 41: 41–50. [DOI] [PubMed] [Google Scholar]
- 23.Ramdharry GM, Pollard AJ, Marsden JF, Reilly MM. Comparing gait performance of people with Charcot-Marie-Tooth disease who do and do not wear ankle foot orthoses. Physiother Res Internat 2012; 17: 191–199. [DOI] [PubMed] [Google Scholar]
- 24.Hebert JS. Ambulatory KAFOs: a physiatry perspective. JPO J Prosthet Orthot 2006; 18: P169–P174. [Google Scholar]
- 25.Andrysek J, Klejman S, Kooy J. Examination of knee joint moments on the function of knee-ankle-foot orthoses during walking. J Appl Biomech 2013; 29: 474–480. [DOI] [PubMed] [Google Scholar]
- 26.Bernhardt KA, Kaufman KR. Loads on the uprights of a knee-ankle-foot orthosis. Prosthet Orthot Int 2011; 35: 106–112. [DOI] [PubMed] [Google Scholar]
- 27.Yakimovich T, Lemaire ED, Kofman J. Preliminary kinematic evaluation of a new stance-control knee-ankle-foot orthosis. Clin Biomech (Bristol, Avon) 2006; 21: 1081–1089. [DOI] [PubMed] [Google Scholar]
- 28.Brehm MA, Beelen A, Doorenbosch CA, Harlaar J, Nollet F. Effect of carbon-composite knee-ankle-foot orthoses on walking efficiency and gait in former polio patients. J Rehabil Med 2007; 39: 651–657. [DOI] [PubMed] [Google Scholar]
- 29.Bernhardt KA, Irby SE, Kaufman KR. Consumer opinions of a stance control knee orthosis. Prosthet Orthot Int 2006. ; 30: 246–256. [DOI] [PubMed] [Google Scholar]
- 30.Edelstein JE. Ambulatory KAFOs: a physical therapist’s perspective. J Prosthet Orthot 2006; 18: 183–186. [Google Scholar]