Abstract
Introduction
Patient positioning is an essential consideration for the optimisation of radiation dose during CT examinations. The study objectives seek to explore the effects of vertical off‐centring, localiser direction (0° and 180°), and phantom positioning (supine and prone) on radiation dose, using three different tube voltages in multidetector computed tomography (MDCT) imaging.
Methods
The trunk of a PBU‐60 anthropomorphic phantom was imaged using a Discovery CT750 HD – 128 slice (GE Healthcare). Images employing 0° and 180° localisers were acquired in supine and prone orientation for each combination of vertical off‐centring (±100, ±60 and ±30 mm) and different tube voltages (80, 120 and 140 kVp), using the system’s automatic tube current modulation (ATCM) function. The displayed volume CT dose index (CTDIvol) and dose length product (DLP) were recorded.
Results
With incremental table off‐centring of ±100 mm, the dose at 120 kVp in the supine position ranged from 63% to 196% (0° localiser) and from 66% to 191% (180° localiser) as compared to iso‐centre. While in the prone position, the dose ranged from 62% to 195% (0° localiser); and 62% to 193% (180° localiser), with a notable dose increase at higher tube voltages. Dose variation and vertical off‐centring showed a significant relationship for both 0° and 180° localisers (r = 0.94 and 0.96, respectively, P < 0.001). The CTDIvol variation between supine and prone phantom positions at ±100 mm off‐centring was 0.22 mGy (2.9%), and 0.19 mGy (2.3%) when the 0° and 180 ° localisers were utilised, respectively.
Conclusions
Phantom off‐centring and localiser direction evidenced large dose variation. It is recommended that the 0° localiser is employed during CT examinations, in order to minimise the potential additional radiation dose which may result from off‐centring and the use of lower tube voltages where clinically appropriate.
Phantom off‐centring and localiser direction evidenced large dose variation. The authors recommend the acquisition of a 0° localiser, to reduce the increase in the total organ doses resultant from patient off‐centring or the dedicated use of automated positioning tools such as a 3D camera.
Introduction
Since the introduction of computed tomography (CT) in 1971, there has been continuous technological advancement which has allowed for increased image quality and diagnostic capabilities. Subsequently, CT has evolved to become a vital diagnostic tool in medical imaging, replacing a number of conventional radiography procedures. 1 However, the contribution of CT to the burden of population dose has continued to increase, this increase being proportional to the rapidly growing number of CT examinations performed worldwide. 2 In response, CT manufacturers continue to develop and implement technological tools, such as iterative reconstruction techniques, automated tube voltage selection (ATVS) and adaptive beam collimation in conjunction with the use of a bowtie filter to optimise radiation dose. 3 , 4 , 5 Another fundamental dose management technique is automatic tube current modulation (ATCM), which has enabled dose reduction of up to 60% without compromising diagnostic image quality. 6
Bowtie filters are prepatient attenuators which are commonly applied in CT scanners, with different dimensions being utilised according to scanner manufacturers (or different models of the same manufacturer) based on acquisition geometry and exposure settings. 7 The specialised shape of the bowtie filter compensates for variation in patient attenuation across the scan field of view (SFOV), by allowing for the maximum intensity to be directed to thicker parts of the patient while reducing X‐ray intensity in peripheral areas where patient attenuation decreases. 8 , 9 It is used to reduce patient dose by modulating radiation output as a function of the angle of the X‐ray beam. 10 The optimal use of the bowtie filter and operation of the ATCM ultimately require the patient to be optimally centred in the CT scanner, at the gantry iso‐centre. 8 Although ATCM systems have different approaches depending on the individual model of scanner, or the manufacturer, the information from localiser radiographs still has a significant role in determining the degree to which tube current is modulated. 11
Frontal localiser radiographs can be taken in 0° (anteroposterior (AP)) or 180° (posteroanterior (PA)) source angles, while 90° or 270° (the ‘3 or 9o’clock’) are the projections for lateral localiser radiographs. Previous studies have recommended the 180° localiser radiograph in preference to the 0° source angle in CT examinations for different body regions, namely, head, thorax and abdomen‐pelvis as a way of reducing radiation dose to anteriorly located radiosensitive organs (breast, and thyroid). 12 , 13 Another study demonstrated minimisation of dose variation resulting from positioning errors by acquiring 90° localiser as a final acquisition angle. 14 However, it is generally accepted that the dose during localiser radiographs is lower than the subsequent CT scan. 15
It is widely recognised that patient off‐centring results in undesirable effects on patient dose and image noise. 8 , 14 , 16 , 17 , 18 Namasivayam et al. 19 and Li et al. 17 reported that 95% of patients undergoing chest and abdominal CT examination in their respective studies were vertically off‐centred in the y plane. There is a general acceptance that radiographers tend to off‐centre patients below the centre of rotation of the scanner, with thinner and smaller patients likely to be centred lower than obese patients. 16 , 18 Further, X‐ray attenuation and dose distribution are directly impacted by localiser radiograph size which is evidenced by the varied attenuation recorded when dose modulation systems (ATCM and ATVS) are being applied. 20 Therefore, it is expected that patient off‐centring will cause a change in relative dose as a result of magnification or minification of the projected localiser radiograph, especially when high attenuation structures such as the spine are present. 21
The aim of this study, then, is to investigate the effects of vertical off‐centring on dose associated with ATCM using different localiser directions, phantom positioning (supine or prone) and tube voltage.
Materials and Methods
Phantom and CT protocol
The torso of a PBU‐60 anthropomorphic phantom (Kyoto Kagaku Co., Ltd., Kyoto, Japan) was scanned using a Discovery CT750 HD ‐ 128 slice (GE Healthcare) multidetector CT (MDCT) scanner (Fig. 1). All scans were planned and performed with identical scan coverage from above the lung apices to the level of the anterior superior iliac spine (ASIS).
Figure 1.
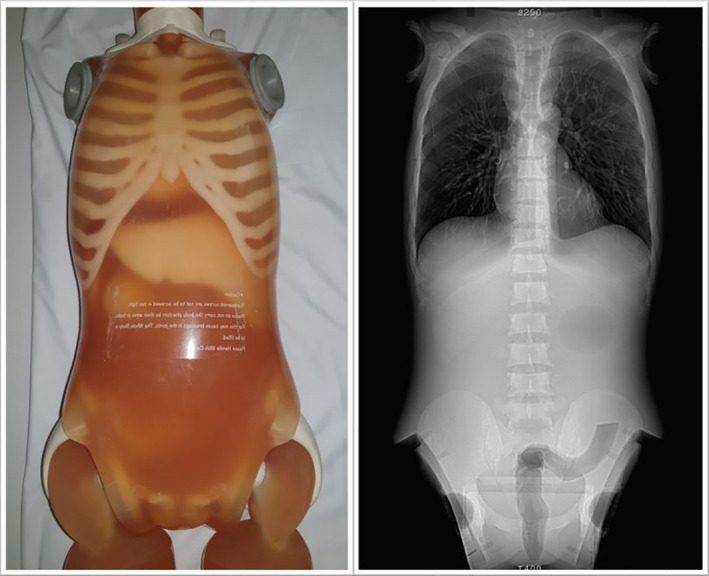
PBU‐60 anthropomorphic phantom (left) and CT localiser image (right). The phantom is of average human body size with two‐dimensional internal structures simulating lung, bone and soft tissue densities.
The phantom was initially scanned at the gantry iso‐centre, using the manufacturer’s recommended clinical settings for an adult of similar size. The localiser radiograph X‐ray tube voltage (kVp) and X‐ray tube current (mA) were 120 and 10, respectively. Scans were started with the lateral (LAT) localiser (90⁰). The phantom’s geometric centre (the anterior posterior midpoint) was aligned with the scanner’s iso‐centre using the in‐built laser. The phantom was scanned at six vertical levels: 30, 60 and 100 mm above and below the iso‐centre (the positive and negative values of off‐centring were recorded as the CT table shifted above and below the axis of rotation of the scanner, respectively). Localiser radiographs were performed before the scan at each table position to enable proper ATCM function. A noise index (NI) was used as a reference parameter for image quality. The index reported the measured standard deviation (SD) at the centre of an image using a phantom simulating human attenuation. The ATCM employed the information of the estimated attenuation and shape from the localiser radiograph to achieve constant image noise through the scan. The scanner then varied the tube current for all projections at each rotation to meet the target value. 11
A helical scan was performed utilising the factors of 120 kVp, 5 mm slice thickness, 0.5‐s, rotation time, pitch 1.375 and the standard reconstruction kernel. The large bowtie filter was selected automatically using the large body option for the 50 cm reconstruction diameter field of view (FOV). The tube current varied between 15 and 625 mA as a function of attenuation using the inbuilt ATCM system. Scanning was repeated at 80 and 140 kVp for each table height while maintaining other scanning parameters.
Radiation dose and phantom width measurements
To explore the effects of the localiser direction and phantom positioning with each vertical off‐centring increment, the phantom was first placed supine. At each table increment off‐centring, localisers were obtained in both 90⁰ and 0° and 90⁰and 180° orientations. This was then repeated with the phantom in the prone position. The terminology 0° vs. 180° has been used instead of AP and PA localisers to best differentiate orientation as the localiser descriptor will invariably keep changing with respect to the phantom position (supine and prone). Using 0° vs. 180° describes the localiser location regardless of the phantom position. For each scanning protocol, the volume CT dose index (CTDIvol) and dose length product (DLP) were recorded. The apparent phantom size (projected localiser size) was determined for each vertical height position as the projected width from the localiser radiograph. Results were then normalised by dividing the width measurement on the actual transverse diameter (293 mm) of the measured corresponding axial image. These normalised widths were plotted as a function of vertical shifting.
Statistical analysis
Data were analysed using SPSS, Version 26 (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp). A dependent paired t‐test was conducted to explore the dose as a function of vertical off‐centring between phantom positions (supine and prone), using SPSS. Pearson’s correlation coefficient was used to assess the relationship between apparent phantom size (projected localiser size) and vertical‐ off‐centring, with P < 0.05 considered statistically significant.
Results
Variation in CTDIvol and DLP showed a significant and strong positive relationship with vertical off‐centring for both 0° and 180° localisers (r = 0.94 and 0.96 respectively, P < 0.001). Variation of the radiation output was a function of the average mAs variation based on the apparent phantom size in the acquired localiser.
Incremental table off‐centring was seen to cause variation of the scanner CTDIvol and DLP. Compared to the dose at the iso‐centre, when the phantom was in the supine position at 120 kVp, the percentage dose variation ranged from 71% to +196% with the 0° localiser and 66% to 191% with the 180° localiser. Dose variations with the phantom in the prone position were 69% to 195% with the 0° localiser and 65% to 193% with the 180° localiser. As expected, the values of CTDIvol were greatest when the phantom was positioned 100 mm below the iso‐centre with the 180° localiser, and the lowest with the 0° localiser at the same table height, and conversely for phantom positioning 100 mm above the iso‐centre. In summary, the closer the proximity of the phantom to the X‐ray tube, the more magnified the localiser image, leading to higher radiation output resulting from higher photon flux concerning the inverse square law.
A dependent paired t‐test showed a statistically significant difference in dose between both phantom positions (supine and prone) as a function of vertical off‐centring. The results showed dose in the supine position (M = 4.23, SD = 1.34) were lower than on prone position (M = 4.28, SD = 1.37), t(20) = −2.63, P < 0.05, when 0° localiser was acquired. Furthermore, using a 180° localiser, the dose in the supine position (M = 4.83, SD = 1.58) was higher than the prone position (M = 4.7, SD = 1.55), t(20) = 6.468, P < 0.001. However, the dose varied from 2.3% to 2.9% between both positions when the 0° and 180° localisers were acquired, respectively, (Fig. 2).
Figure 2.
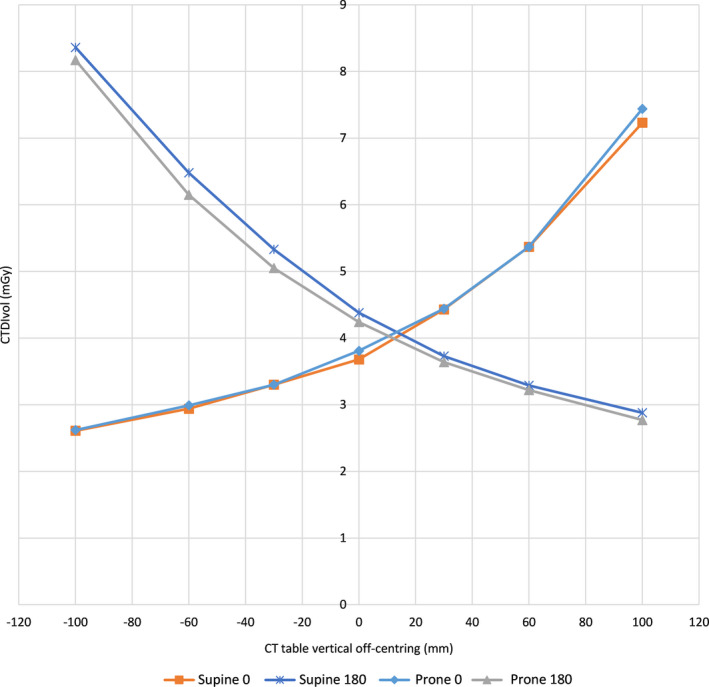
The CTDIvol variation as a function of vertical off‐centring with different localiser direction and phantom position at 120 kVp. This figure is consistent with the results from seven scanners from Paolicchi et al. 22
The transverse diameter (width) of the projected localiser at the level of the thoracic spine (T9) varied from 253 to 383 mm, depending on the localiser orientation and vertical off‐centring. The resultant value was compared to the transverse diameter of the measured corresponding axial image (293 mm). The percentage magnification and minification, at the minimum and maximum table heights (±100 mm), were 25.9%, 9.6% for the 0° localiser, and 30.7%, 9.6% for the 180° localiser, respectively, correlated with the degree of vertical off‐centring.
Figure 3 shows the effect of vertical off‐centring, phantom position and localiser direction on measurements of phantom size. There was a positive relationship between the vertical off‐centring and the apparent phantom size when utilising different localiser directions and phantom positions, this being r = 0.99. The linear model was found to fit the data well with r 2 ≥ 0.98 in all cases.
Figure 3.
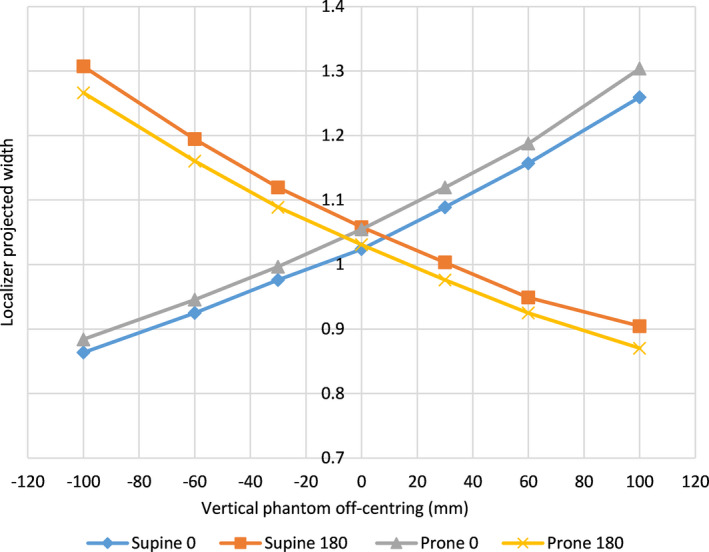
The projected phantom width as a function of vertical off‐centring was acquired at 0° and 180° in both the supine and prone positions. The values were normalised to the actual phantom size.
At different phantom positions, vertical off‐centring and localiser directions, the doses at 120 kVp were 91% to 97% and at 80 kVp 18% to 33% greater than iso‐centre dose, (Fig. 4).
Figure 4.
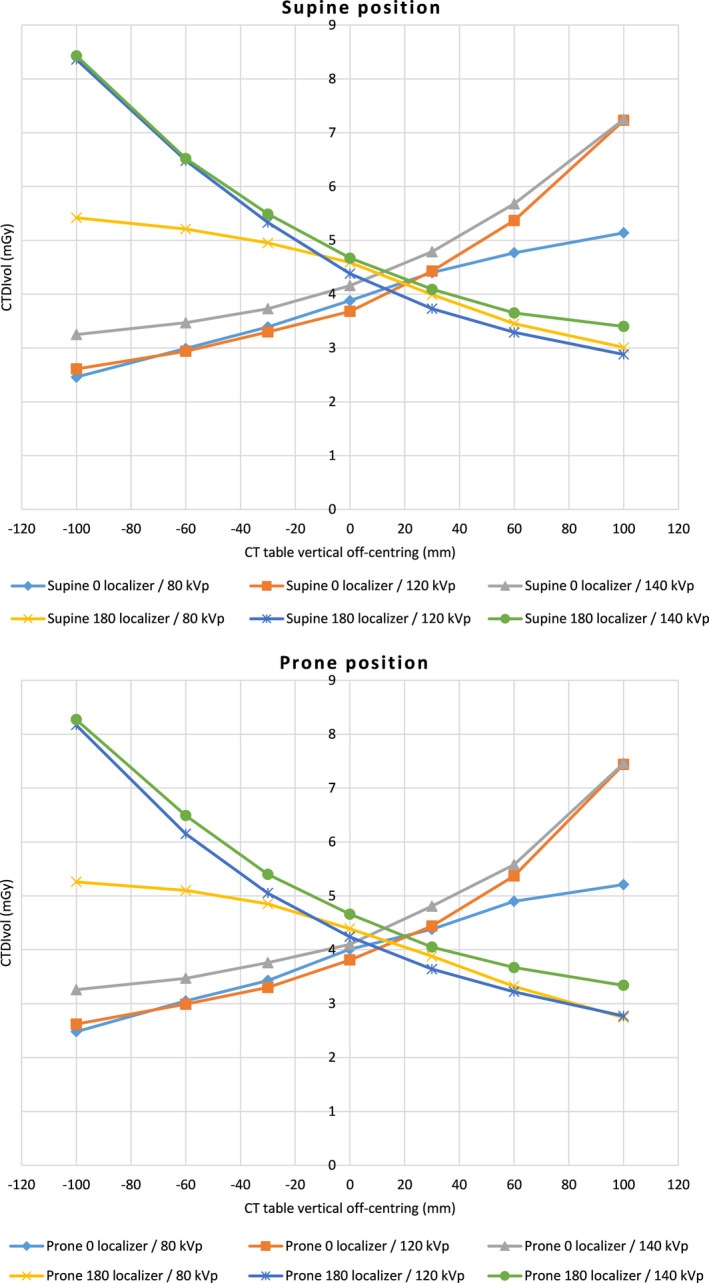
The CTDIvol variation as a function of vertical off‐centring with 0° and 180° localiser direction, different phantom positions and tube voltage.
Discussion
The findings of this experimental study demonstrate that the closer the proximity of the phantom to the X‐ray tube, the greater the magnification of the localiser radiograph, which is expected. At 100 mm above and below the gantry iso‐centre, however, the magnification effect was more pronounced for localisers acquired in the 180° projection (30.7%) compared to the 0° localiser (25.9%) when the phantom was at supine position. Similarly, the magnification for the 0° localiser projection was larger (30.4%) compared to the 180° localiser (26.6%) when the phantom was in the prone position. Firstly, this can be explained due to differences in anatomical geometry between the anterior and posterior thoracic surface area of the phantom, and with respect to the divergence of the X‐ray beam, thus magnification is larger when the posterior surface of the phantom is closer to the localiser. Secondly, the phantom was visually centred ~15 mm below the gantry iso‐centre in the supine position, and since the similar iso‐centre marker on the phantom was used, the phantom was positioned above the gantry iso‐centre in the prone position. This relationship is reported in Figure 3. This was consistent with the findings for six scanners from three different manufacturers in a study published in 2020. 22
The relative dose over a range of body sizes can be estimated from AP and LAT dimensions with correlation to doses measured using the known dimensions of cylindrical phantoms using a scaling factor. It is worth noting that the displayed CTDIvol on the CT images reflects doses delivered to cylindrical CT dose phantoms under the same imaging parameters such as kVp and mAs. The actual doses delivered to a patient (or any other scanned object such as anthropomorphic phantoms) should utilise size based corrections as recommended by the American Association of Physicists in Medicine (AAMP) report 204. 23
In the current study, the CTDIvol and DLP measurements varied as a function of phantom off‐centring. The highest values were recorded at −100 mm when a 180° localiser was used in both the supine (CTDIvol 8.36 mGy and DLP 459.4 mGy*cm) and prone positions (CTDIvol 8.27 mGy and DLP 454.4 mGy*cm) (Fig. 2). Dose variation can be explained by the basic physical principle that the projection of the phantom is minimised or magnified on the detector surface, the increase or decrease depending on the degree of phantom off‐centring relative to the gantry iso‐centre. The size of the localiser affects the tube current selection of the ATCM.
Seven scanners produced by four different manufacturers were previously used to assess the influence of CT localiser direction and vertical off‐centring on the dose. 22 It was found that the highest CTDIvol values were recorded on all scanners utilised in the study when examinations were planned on the 180° localiser compared to the 0° localiser. In the same study, Paolicchi et al. showed a marked change in CTDIvol as a result of ±60 mm vertical off‐centring. 22 Using a Discovery HD scanner, they recorded a dose variation from −26% to +32% with a 0° localiser, and from +39% to −44% with a 180° localiser. This study used a similar scanner type and the same degrees of off‐centring, but importantly used a different phantom, which reported dose variation from −20% to +46% with the 0° localiser, and from +25% to −48% with the 180° localiser.
Several studies have investigated the effect of off‐centring on dose and image quality. 8 , 14 , 16 , 18 , 21 , 22 , 24 The importance of these studies aligns with the fact that off‐centring in clinical practice is alarmingly commonplace with one study reporting 95% of patients undergoing thoracic or abdominal CT examinations were vertically off‐centred. 17 A retrospective study of 549 patients by Toth and Ge reported a mean lateral positioning error of 0.0 mm, and from −66 to 34 mm in the vertical direction. 16 Another study showed a mean value of off‐centring (−43 mm) with the minimum and maximum off‐centring from −88 mm to 16 mm. 24 Studies based on visual estimate centring have shown that patients were off‐centred by a mean of 22, 16 23, 8 25.6 17 and 25‐35 mm 18 below gantry iso‐centre. It is clear from the literature that the centre of mass of the patient tends to be positioned below the scanner centre of rotation, rather than above. For example, the study by Habibzadeh et al. 8 reported 85% of patients were positioned below the iso‐centre.
To combat this issue, radiographer knowledge and professional practice should ideally be updated with regard to the importance of patient centring and the consequences of miscentring on radiation dose. Improved positioning accuracy could also be achieved through the installation of automated patient positioning tools, such as 3D cameras. 25 However, in the absence of these key interventions, the authors recommend acquisition using a 0° localiser to reduce any increase in the total organ doses resultant from patient off‐centring. This recommendation is based on previous retrospective studies, reporting a trend to misposition patients below the gantry iso‐centre and the current experimental findings. However, in some situations, it is acknowledge that the table height may be required to be off‐centred to meet the clinical need. In this case, the authors recommend acquisition using the localiser farthest from patient body.
A central aim of this study was to examine the effect of phantom position on radiation dose as a function of phantom off‐centring. The influence of phantom position (spines’ location) was more pronounced at the largest off‐centring increment (± 100 mm), and when the spine was shifted closer to the X‐ray tube, which is known to result in higher beam attenuation. The CTDIvol variation between positions (supine and prone) was reported at +100 mm off‐centring to be 0.22 mGy (2.9%), when a 0° localiser was acquired and 0.19 mGy (2.3%) with a 180° localise at −100 mm off‐centring. This can be explained by the spines location for each scan acquisition. Kaasalainen et al. examined the effect of vertical off‐centring and localiser direction on the function of ATVS and ATCM. 21 They explained the extensive change in the relative dose being due to the larger magnification of the spine.
The effect of tube voltage selection on the dose with vertical off‐centring was also examined. The current findings reported in Figure 4 suggest a benefit of applying lower tube voltage settings when it is applicable with the results evidencing, a maximum percentage dose change of 33% at 80 kVp, increasing to 97% at 120 kVp at 100 mm off‐centring.
Limitations
A limitation of this study is that only one model scanner from one manufacturer was evaluated, and only one bowtie filter size was used. However, a similar trend would be expected. Further research should be undertaken to further investigate the association between dose variation and image quality.
Conclusion
Dose optimisation in MDCT has been demonstrated to be impacted by the misalignment of the phantom to the bowtie filter and localiser direction. The closer the off‐centred phantom was to the X‐ray tube, the more magnified the localiser image, leading to higher radiation output with ATCM due to higher photon flux.
Given the known trend for patients to be vertically off‐centred and taking into consideration the results of this study and the current literature, the authors recommend a 0° localiser to be acquired during CT examinations, in order to minimise the potential for additional radiation dose which may result from patient off‐centring. The technique parameters that assure minimum CTDIvol must be linked to accurate centring to maintain optimal imaging conditions. Increased education for radiographers on methods to optimise patient centring to reduce patient dose is strongly suggested.
Further research is needed to validate this study and to additionally examine the impact of phantom size on radiation dose as a function of vertical off‐centring and examining CT scanners from other vendors.
Acknowledgement
I would like to acknowledge all the staff working in I‐MED Radiology Network / Wagga Wagga for their timely support, and I would like to give my special thanks to The Hashemite University for their generosity with my PhD scholarship.
J Med Radiat Sci. 69(2022) 5–12
References
- 1. Cropp RJ, Seslija P, Tso D, Thakur Y. Scanner and kVp dependence of measured CT numbers in the ACR CT phantom. J Appl Clin Med Phys 2013; 14: 4417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cool DA, Kase KR, Boice JD. NCRP Report no.180‐management of exposure to ionizing radiation: NCRP radiation protection guidance for the United States. J Radiol Prot 2019; 39: 966–77. [DOI] [PubMed] [Google Scholar]
- 3. Lurz M, Lell MM, Wuest W, et al. Automated tube voltage selection in thoracoabdominal computed tomography at high pitch using a third‐generation dual‐source scanner: image quality and radiation dose performance. Invest Radiol 2015; 50: 352–60. [DOI] [PubMed] [Google Scholar]
- 4. Booij R, Dijkshoorn ML, van Straten M. Efficacy of a dynamic collimator for overranging dose reduction in a second‐ and third‐generation dual source CT scanner. Eur Radiol 2017; 27: 3618–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Abdullah KA, McEntee MF, Reed W, Kench PL. Development of an organ‐specific insert phantom generated using a 3D printer for investigations of cardiac computed tomography protocols. J Med Radiat Sci 2018; 65: 175–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kalender WA, Buchenau S, Deak P, et al. Technical approaches to the optimisation of CT. Phys Med 2008; 24: 71–9. [DOI] [PubMed] [Google Scholar]
- 7. Zhang G, Marshall N, Jacobs R, Liu Q, Bosmans H. Bowtie filtration for dedicated cone beam CT of the head and neck: a simulation study. Br J Radiol 2013; 86: 20130002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Habibzadeh MA, Ay MR, Asl AR, Ghadiri H, Zaidi H. Impact of miscentering on patient dose and image noise in x‐ray CT imaging: phantom and clinical studies. Phys Med 2012; 28: 191–9. [DOI] [PubMed] [Google Scholar]
- 9. Toth TL. Dose reduction opportunities for CT scanners. Pediatr Radiol 2002; 32: 261–7. [DOI] [PubMed] [Google Scholar]
- 10. Hsieh SS, Pelc NJ. The feasibility of a piecewise‐linear dynamic bowtie filter. Med Phys 2013; 40: 31910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Merzan D, Nowik P, Poludniowski G, Bujila R. Evaluating the impact of scan settings on automatic tube current modulation in CT using a novel phantom. Br J Radiol 2017; 90: 20160308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schmidt B, Saltybaeva N, Kolditz D, Kalender WA. Assessment of patient dose from CT localizer radiographs. Med Phys 2013; 40: 84301. [DOI] [PubMed] [Google Scholar]
- 13. Saltybaeva N, Krauss A, Alkadhi H. Effect of localizer radiography projection on organ dose at chest CT with automatic tube current modulation. Radiology 2017; 282: 842–9. [DOI] [PubMed] [Google Scholar]
- 14. Lambert JW, Kumar S, Chen JS, Wang ZJ, Gould RG, Yeh BM. Investigating the CT localizer radiograph: acquisition parameters, patient centring and their combined influence on radiation dose. Br J Radiol 2015; 88: 20140730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Singh S, Petrovic D, Jamnik E, et al. Effect of localizer radiograph on radiation dose associated with automatic exposure control: human cadaver and patient study. J Comput Assist Tomogr 2014; 38: 293–8. [DOI] [PubMed] [Google Scholar]
- 16. Toth T, Ge Z, Daly MP. The influence of patient centering on CT dose and image noise. Med Phys 2007; 34: 3093–101. [DOI] [PubMed] [Google Scholar]
- 17. Li J, Udayasankar UK, Toth TL, Seamans J, Small WC, Kalra MK. Automatic patient centering for MDCT: effect on radiation dose. AJR Am J Roentgenol 2007; 188: 547–52. [DOI] [PubMed] [Google Scholar]
- 18. Kaasalainen T, Palmu K, Reijonen V, Kortesniemi M. Effect of patient centering on patient dose and image noise in chest CT. AJR Am J Roentgenol 2014; 203: 123–30. [DOI] [PubMed] [Google Scholar]
- 19. Namasivayam S, Kalra M, Mittal P, Small W. Can Radiation Exposure Associated with Abdominal and/or Pelvic CT be Minimized with Better Practice. ARRS, Vancouver, Canada, 2006. [Google Scholar]
- 20. Kalra MK, Maher MM, Toth TL, et al. Strategies for CT radiation dose optimization. Radiology 2004; 230: 619–28. [DOI] [PubMed] [Google Scholar]
- 21. Kaasalainen T, Mäkelä T, Kortesniemi M. The effect of vertical centering and scout direction on automatic tube voltage selection in chest CT: a preliminary phantom study on two different CT equipments. Eur J Radiol Open 2019; 6: 24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Paolicchi F, Bastiani L, Negri J, Caramella D. Effect of CT localizer radiographs on radiation dose associated with automatic tube current modulation: a multivendor study. Curr Probl Diagn Radiol 2020; 49: 34–41. [DOI] [PubMed] [Google Scholar]
- 23. Brady SL, Kaufman RA. Investigation of American Association of Physicists in Medicine Report 204 size‐specific dose estimates for pediatric CT implementation. Radiology 2012; 265: 832–40. [DOI] [PubMed] [Google Scholar]
- 24. Sukupova L, Vedlich D, Jiru F. Consequences of the patient's mis‐centering on the radiation dose and image quality in CT imaging – phantom and clinical study. Univers J Med Sci 2016; 4: 102–7. [Google Scholar]
- 25. Dane B, O’Donnell T, Liu S, et al. Radiation dose reduction, improved isocenter accuracy and CT scan time savings with automatic patient positioning by a 3D camera. Eur J Radiol 2021; 136: 109537. [DOI] [PubMed] [Google Scholar]


