Abstract
Introduction
Aimed to develop a simple and robust volumetric modulated arc radiotherapy (VMAT) solution for comprehensive lymph node (CLN) breast cancer without increase in low‐dose wash.
Methods
Forty CLN‐breast patient data sets were utilised to develop a knowledge‐based planning (KBP) VMAT model, which limits low‐dose wash using iterative learning and base‐tangential methods as benchmark. Another twenty data sets were employed to validate the model comparing KBP‐generated ipsilateral VMAT (ipsi‐VMAT) plans against the benchmarked hybrid (h)‐VMAT (departmental standard) and bowtie‐VMAT (published best practice) methods. Planning target volume (PTV), conformity/homogeneity index (CI/HI), organ‐at‐risk (OAR), remaining‐volume‐at‐risk (RVR) and blinded radiation oncologist (RO) plan preference were evaluated.
Results
Ipsi‐ and bowtie‐VMAT plans were dosimetrically equivalent, achieving greater nodal target coverage (P < 0.05) compared to h‐VMAT with minor reduction in breast coverage. CI was enhanced for a small reduction in breast HI with improved dose sparing to ipsilateral‐lung and humeral head (P < 0.05) at immaterial expense to spinal cord. Significantly, low‐dose wash to OARs and RVR were comparable between all plan types demonstrating a simple VMAT class solution robust to patient‐specific anatomic variation can be applied to CLN breast without need for complex beam modification (hybrid plans, avoidance sectors or other). This result was supported by blinded RO review.
Conclusions
A simple and robust ipsilateral VMAT class solution for CLN breast generated using iterative KBP modelling can achieve clinically acceptable target coverage and OAR sparing without unwanted increase in low‐dose wash associated with increased second malignancy risk.
Keywords: Breast, cancer, knowledge‐based planning, lymph nodes, radiotherapy, simultaneous integrated boost (SIB), VMAT
Comprehensive lymph nodal (CLN) radiotherapy can improve the outcomes for advanced breast cancer patients, but it can be particularly challenging to balance target coverage and organ‐at‐risk sparing without complex beam modification (VMAT avoidance sectors, hybrid IMRT/VMAT fields, other) to limit the low‐dose wash and potential second malignancy risk. By presenting the first application of iterative learning to a knowledge‐based planning model in CLN‐breast radiotherapy, this study demonstrates that a simple and robust ipsilateral VMAT class solution can be applied without increase in low‐dose wash compared to benchmark base‐tangential IMRT/VMAT methods.

Introduction
Breast cancer is one of the most commonly diagnosed cancers, estimated to account for up to 30% of all new cancer cases in women and contributes significantly to the workload of most radiotherapy departments. 1 Radiotherapy treatment is an integral component in local and regional management of breast cancer reducing local recurrence and, in higher risk patients, improving survival in the adjuvant setting. 2 , 3
The difficulty of modern breast radiotherapy with inclusion of comprehensive lymph nodes (CLN) including supraclavicular, axillary and internal mammary nodes for at‐risk patients has created challenges for planning based on three‐dimensional conformal radiotherapy (3DCRT). 4 This difficulty is exacerbated for patients which have an implant/expander or require simultaneous integrated boost (SIB) to the tumour bed. 5 Intensity modulated radiotherapy (IMRT) and volumetric arc therapy (VMAT) improve the balance between target coverage and organ‐at‐risk (OAR) sparing, but their traditional application tends to be limited to the most demanding CLN‐breast cases due to concerns of increased low‐dose wash and potential secondary malignancy risk. 6 As such, recent CLN‐breast planning studies have focussed on modified IMRT or VMAT applications, which deliver a base portion of the dose tangentially using opposed fields or partial arcs (portals) to limit the secondary cancer risk profile similar to that of 3DCRT. 7 But whilst VMAT plans have the added advantage of fewer monitor units (MU) and shorter delivery times compared to their IMRT counterparts, 8 these contemporary base‐tangential VMAT techniques are disadvantaged by their increased planning complexity. 5 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 Indeed, such modified VMAT approaches require at least one of either base‐hybrid plans (3DCRT or IMRT), pre‐defined avoidance sectors, junctions, split arcs or non‐coplanar beams in order to limit low‐dose wash and improve plan quality.
To reduce complexity and improve planning consistency, standardised beam arrangements and application of machine learning via knowledge‐based planning (KBP) is appropriate. In particular, KBP software such as RapidPlan™ (Varian Medical Systems, Palo Alto, CA, USA), which leverages curated patient anatomy and high quality plans has been shown to improve quality, consistency and efficiency of breast radiotherapy treatment. 17 By applying KBP modelling using iterative learning and complex modified base‐tangential techniques as benchmark, 18 we hypothesise that a simple ipsilateral VMAT solution for CLN‐breast cancer can achieve clinically acceptable target coverage and OAR sparing without an otherwise increase in low‐dose wash and potential secondary malignancy risk. This works presents the first clinical implementation of an iterative KBP model in CLN‐breast radiotherapy.
Methods
Ethics approval for this retrospective study of low and negligible risk was granted by the Northern Sydney Local Health District Human Research Ethics Committee (LNR/2020/ETH01286).
Preparation
Planning data sets from 60 (30 left‐sided and 30 right‐sided) de‐identified conserved breast cancer patients who previously received CLN radiotherapy treatment were selected at random in this study. Non‐contrast CT helical acquisition was with 2 mm slice thickness and 600 mm field of view (512 2 pixel matrix) at 120 kVp on a Brilliance Big Bore scanner (Philips Medical Systems, Cleveland, OH, USA). All patients were immobilised in the supine position at 5–10° incline with arms raised above their head on the AccessTM Supine Breast board (Qfix, Avondale, PA, USA). Scans for left‐sided patients were acquired in deep inspiration breath‐hold (DIBH) using the Real‐Time Position Management (RPM) System (Varian Medical Systems).
Two subspecialised breast radiation oncologists (RO) delineated clinical target volumes (CTV) and OARs on each of the 60 patient data sets according to ESTRO consensus guidelines. 19 This included conserved breast, tumour bed, axillary nodes, supraclavicular nodes and internal mammary nodes. Planning target volumes (PTV) with a uniform 0.5 cm CTV expansion (cropped 0.5 cm from skin) were added, with heart and left anterior descending coronary artery (LADCA) contoured per Feng et al. 20 A remaining volume at risk (RVR), defined as the Body minus all target and OAR structures, 21 was included to supplement the assessment of low‐dose wash.
A dose of 50 Gy in 25 fractions was prescribed to the breast, supraclavicular fossa and axilla, 45 Gy to the internal mammary nodes and 57 Gy SIB to the tumour bed. Three coplanar planning techniques with isocentre placed in lung behind the chest‐wall interface were investigated as detailed below. All plans were optimised in Eclipse™ treatment planning system v15.6 (Varian Medical Systems) and calculated using the Halcyon 6MV flattening filter free (FFF) beam model with Acuros XB dose‐to‐medium (2mm grid size).
Hybrid (h)‐VMAT (in‐house low‐dose wash benchmark): Extending on work originally published by Jöst et al, 22 plan consists of two tangentially opposed IMRT fields to deliver a 30 Gy base to the conserved breast and inferior IMC/Axilla, junctioned with an angled anterior IMRT field (15 or 345 degrees depending on laterality) to deliver a 20 Gy base to the SCF and superior IMC/Axilla. Two ipsilateral VMAT fields spanning an extra 20° beyond the tangential gantry angles are then used to deliver the remaining dose to the target volumes (Figure 1a), with an additional arc in cases where dose coverage was suboptimal due to difficult anatomic configuration.
Bowtie‐VMAT (published benchmark): Includes three ipsilateral VMAT fields spanning 220° but with two of the fields including an appositional avoidance sector (dose‐rate drops to zero) to largely limit fluence delivery to tangential sub arcs of approximately 70° range without compromising coverage of the supraclavicular fossa (Figure 1b).
Ipsi‐VMAT (proposed class solution): Three ipsilateral VMAT fields spanning 220° (Figure 1c). For a right‐sided treatment the arcs move between 200° and 60° gantry angles. For left‐sided treatments the treatment arcs move between 160° and 300°. The start and stop gantry angles were chosen to shape the dose distribution to the patient’s chest‐wall off the heart and lung, independent of patient size and geometry.
Figure 1.
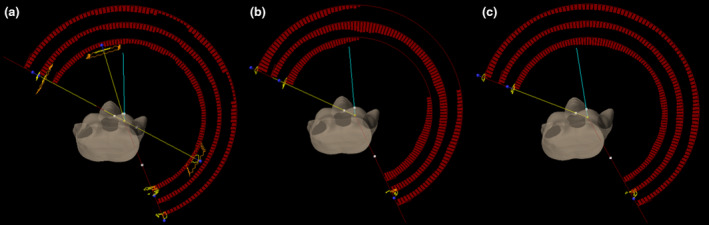
Planning techniques used for dosimetric plan comparison. Field arrangements for (a) h‐VMAT, (b) bowtie‐VMAT and (c) ipsi‐VMAT plans. The h‐VMAT technique includes 2 base‐tangential IMRT fields, 1 base anterior oblique IMRT field and 2–3 ipsilateral VMAT arcs. The bowtie‐VMAT technique consists of 3 ipsilateral VMAT arcs, 2 of which restrict fluence delivery to tangential portals (via 70° appositional avoidance sectors). The ipsi‐VMAT technique consists of 3 ipsilateral VMAT arcs.
Development of the iterative breast nodal knowledge‐based plan model
Benchmarked h‐VMAT plans were manually generated by the department’s expert breast planners and repeatedly optimised in order to achieve the clinical objectives detailed in Tables 1 and 2 per the SKAGEN order of priority. 23 Planning data sets from 40 of the 60 CLN‐breast cancer patients (20 left‐ and 20 right‐sided) were then included in development of the iterative VMAT breast nodal KBP model, using low‐dose wash of the h‐VMAT plans as benchmark. The model was re‐trained initially using outputted bowtie‐VMAT plans as input for the next iteration of the model. 18 When low‐dose wash of the bowtie‐VMAT plans met the h‐VMAT benchmark through refinement of the models optimisation parameters, ipsi‐VMAT plans were then used as input for the final iterations of the model. 18 In total five iterations were performed to produce the final refined model, beyond that negligible improvements (change in V5 Gy < 1%) were seen.
Table 1.
Departmental target goals and dosimetric parameters achieved for each planning type.
| Target name |
Volume (cc) Median (IQR) |
DVH Goal |
h‐VMAT Median (IQR) |
Bowtie‐VMAT Median (IQR) |
Ipsi‐VMAT Median (IQR) |
P‐Value (Welch’s t‐test) Ipsi‐VMAT vs h‐VMAT |
P‐Value (Welch’s t‐test) Ipsi‐VMAT vs Bowtie‐VMAT |
Reported range from published literature 5, 9, 14, 15, 16, 30 |
|---|---|---|---|---|---|---|---|---|
| PTVp_TB |
32.1 cc (29.7–56.4 cc) |
D95% ≥ 95% (54.15 Gy) |
56.1 Gy (55.8–56.3 Gy) |
56.2 Gy (55.9–56.4 Gy) |
56.3 Gy (56.1–56.6 Gy) |
0.14 | 0.16 | |
| D98% |
55.7 Gy (55.4–55.9 Gy) |
55.8 Gy (55.5–55.9 Gy) |
55.9 Gy (55.7–56.2 Gy) |
0.38 | 0.20 | |||
| D50% |
57.8 Gy (57.6–58.0 Gy) |
57.8 Gy (57.6–58.1 Gy) |
57.9 Gy (57.6–58.4 Gy) |
0.13 | 0.38 | |||
| D2% (max) |
59.2 Gy (59.0–59.7 Gy) |
59.6 Gy (59.2–60.1 Gy) |
59.6 Gy (59.2–60.2 Gy) |
0.03* | 0.68 | |||
| HI |
0.057 (0.053–0.064) |
0.059 (0.056–0.065) |
0.057 (0.052–0.061) |
0.89 | 0.06 | |||
| PTVp_Br |
639.4 cc (487.5–961.0 cc) |
D95% ≥ 95% (47.50 Gy) |
48.7 (48.6–49.0) |
47.5 (47.5–47.7) |
47.5 (47.5–47.5) |
<0.01* | 0.12 | 45.6–49.5 Gy |
| D98% |
48.1 Gy (47.7–48.3 Gy) |
46.4 Gy (46.3–46.6 Gy) |
46.3 Gy (46.0–46.5 Gy) |
<0.01* | 0.06 | |||
| D50% |
50.6 Gy (50.2–50.9 Gy) |
50.6 Gy (50.4–51.3 Gy) |
50.7 Gy (50.4–51.3 Gy) |
0.08 | 0.70 | |||
| D2% (max) |
58.1 Gy (57.8–58.5 Gy) |
58.1 Gy (57.9–58.5 Gy) |
58.3 Gy (57.8–58.8 Gy) |
0.25 | 0.68 | |||
| HI |
0.183 (0.175–0.196) |
0.208 (0.204–0.214) |
0.212 (0.204–0.218) |
<0.01* | 0.39 | |||
| PTVn_SCF |
91.6 cc (77.3–110.9 cc) |
D95% ≥ 95% (47.50 Gy) |
47.9 Gy (47.8–48.1 Gy) |
48.4 Gy (48.0–48.6 Gy) |
48.6 Gy (48.3–48.8 Gy) |
<0.01* | 0.18 | 42.5–48.7 Gy |
| D98% |
47.3 Gy (47.1–47.6) Gy |
47.4 Gy (46.8–47.7 Gy) |
47.7 Gy (47.1–48.0 Gy) |
0.23 | 0.29 | |||
| D50% |
49.6 Gy (49.5–49.8 Gy) |
50.5 Gy (50.3–50.9 Gy) |
50.6 Gy (50.3–51.0 Gy) |
<0.01* | 0.55 | |||
| D2% (max) |
51.1 Gy (50.9–51.2 Gy) |
52.2 Gy (51.9–52.8 Gy) |
52.2 Gy (51.8 ‐ 52.6 Gy) |
<0.01* | 0.84 | 51.5–55.0 Gy | ||
| HI |
0.063 (0.062–0.069) |
0.076 (0.071–0.084) |
0.072 (0.066–0.086) |
<0.01* | 0.22 | |||
| PTVn_Ax |
158.8 cc (123.2–204.9 cc) |
D95% ≥ 95% (47.50 Gy) |
48.0 Gy (47.9–48.2 Gy) |
48.6 Gy (48.5–48.9 Gy) |
48.7 Gy (48.5–48.8 Gy) |
<0.01* | 0.80 | 48.9–49.2 Gy |
| D98% |
47.6 Gy (47.3–47.7 Gy) |
47.8 Gy (47.6–48.1 Gy) |
48.0 Gy (47.6–48.2 Gy) |
<0.01* | 0.86 | |||
| D50% |
49.5 Gy (49.5–49.7 Gy) |
50.5 Gy (50.3–50.8 Gy) |
50.6 Gy (50.2–50.9 Gy) |
<0.01* | 0.51 | |||
| D2% (max) |
51.2 Gy (50.9–51.6 Gy) |
52.3 Gy (51.8–52.9 Gy) |
52.4 Gy (51.9–53.3 Gy) |
<0.01* | 0.97 | 55.0 Gy | ||
| HI |
0.065 (0.057–0.074) |
0.069 (0.064–0.085) |
0.072 (0.064–0.085) |
0.33 | 0.95 | |||
| PTVn_IMN |
30.1 cc (26.3–36.7 cc) |
D95% ≥ 95% (42.75 Gy) |
43.6 Gy (43.2–44.3 Gy) |
44.1 Gy (42.8–44.8 Gy) |
44.5 Gy (43.5–45.0 Gy) |
0.05* | 0.37 | 44.6–51.1 Gy |
| D98% |
42.8 Gy (42.3–43.6 Gy) |
43.0 Gy (41.5–43.8 Gy) |
43.4 Gy (42.1–44.1 Gy) |
0.37 | 0.20 | |||
| D50% |
47.4 Gy (46.8–48.0 Gy) |
48.8 Gy (48.2–49.0 Gy) |
48.8 Gy (48.5–49.2 Gy) |
<0.01* | 0.18 | |||
| D2% (max) |
50.8 Gy (50.6–50.97 Gy) |
51.9 Gy (51.5–52.3 Gy) |
51.8 Gy (51.4–52.7 Gy) |
<0.01* | 0.92 | 55.0 Gy | ||
| HI |
0.126 (0.113–0.137) |
0.126 (0.113–0.142) |
0.125 (0.109–0.154) |
0.46 | 0.72 | |||
| Conformity Index | CI (Combined PTV, 45 Gy isodose) |
0.673 (0.663–0.694) |
0.694 (0.686–0.711) |
0.712 (0.693–0.736) |
<0.01* | 0.09 | ||
|
CI (PTVp_TB, 54.15 Gy isodose) |
0.597 (0.536–0.675) |
0.586 (0.523–0.608) |
0.593 (0.531–0.640) |
0.17 | 0.74 | |||
| Monitor Units | Total MU |
839 MU (785–880 MU) |
595 MU (568–628 MU) |
652 MU (616–69 MU) |
<0.01* | <0.01* | 973–1568 MU |
PTV, planning target volume; TB, tumour bed; Br, conserved breast; SCF, supraclavicular fossa; Ax, axilla; IMN, internal mammary nodes; D, dose; V, volume; Max, maximum; cc, cubic centimetres; HI, homogeneity index; CI, conformity index; DVH, dose‐volume histogram; MU, monitor unit; IQR, interquartile range; DNE, does not exist.
*Statistically significant with P < 0.05.
Table 2.
Departmental OAR goals and dosimetric parameters achieved for each planning type.
| Organ Name | DVH Goal | h‐VMAT | Bowtie‐VMAT | Ipsi‐VMAT | P‐Value (Welch’s t‐test) | P‐Value (Welch’s t‐test) | Reported range from published literature 5, 9, 14, 15, 16, 30 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) | Number (percentage) of patients who met goal | Median (IQR) | Number (percentage) of patients who met goal | Median (IQR) | Number (percentage) of patients who met goal | Ipsi‐VMAT vs h‐VMAT | Ipsi‐VMAT vs bowtie‐VMAT | |||
| Heart Left Lesion | Mean ≤ 3 Gy |
2.0 Gy (1.5–2.5 Gy) |
10 (100%) |
2.0 Gy (1.4–2.4 Gy) |
10 (100%) |
2.0 Gy (1.4–2.5 Gy) |
10 (100%) | 0.87 | 0.98 | 3.0–11.7 Gy |
| V5 Gy ≤ 10% |
2.0% (1.0–4.6%) |
10 (100%) |
2.4% (1.4–4.9%) |
9 (90%) |
1.8% (0.5–5.2%) |
10 (100%) | 0.96 | 0.76 | 11.4–75.7% | |
| V10 Gy ≤ 5% |
0.2% (0.0–1.1%) |
9 (90%) |
0.2% (0.0–1.1%) |
10 (100%) |
0.2% (0.0–1.3%) |
10 (100%) | 0.76 | 0.97 | 4.2–41.7% | |
| D2cc ≤ 20 Gy |
8.1 Gy (5.8–12.5 Gy) |
8 (80%) |
8.8 Gy (7.0–13.9 Gy) |
9 (90%) |
8.0 Gy (5.1–14.4 Gy) |
9 (90%) | 0.89 | 0.93 | 22.5–42.8 Gy | |
| Heart Right Lesion | Mean ≤ 2 Gy |
1.6 Gy (1.4–2.2 Gy) |
7 (70%) |
1.5 Gy (1.4–1.9 Gy) |
9 (90%) |
1.6 Gy (1.4–2.2 Gy) |
7 (70%) | 0.91 | 0.57 | 3.0–11.7 Gy |
| V5 Gy v 6% |
1.6% (0.3–2.4%) |
10 (100%) |
0.8% (0.4–1.8%) |
10 (100%) |
1.7% (0.7–3.1%) |
9 (90%) | 0.65 | 0.35 | 11.4–75.7% | |
| LADCA | D0.04cc ≤ 20 Gy |
10.9 Gy (6.1–20.3 Gy) |
8 (80%) |
13.8 Gy (8.9–18.2 Gy) |
9 (90%) |
14.7 Gy (8.6–19.1 Gy) |
9 (90%) | 0.68 | 0.97 | 31.4 Gy |
| Lung Ipsilateral | Mean ≤ 12 Gy |
12.3 Gy (11.8–13.1 Gy) |
8 (40%) |
11.5 Gy (10.9–12.5 Gy) |
13 (65%) |
11.7 Gy (10.8–12.3 Gy) |
13 (65%) | 0.05* | 0.99 | 13.6–16.4 Gy |
| V5 Gy ≤ 50% |
48.2% (45.3–49.8%) |
16 (80%) |
46.8% (42.9–49.4%) |
16 (80%) |
48.0% (43.7–50.1%) |
15 (75%) | 0.70 | 0.53 | 59.8–84.9% | |
| V10 Gy ≤ 35% |
36.1% (33.5–38.8%) |
8 (40%) |
33.3% (30.8–34.5%) |
16 (80%) |
33.6% (31.4–350%) |
16 (80%) | 0.04* | 0.51 | 45.7–53.5% | |
| V20 Gy ≤ 20% |
25.4% (23.8–28.2%) |
2 (10%) |
22.8% (21.1–23.8%) |
3 (15%) |
23.1% (21.1–23.9%) |
3 (15%) | < 0.01* | 0.71 | 20.8–27.8% | |
| Lung Contralateral | Mean ≤ 2 Gy |
1.9 Gy (1.8–2.2 Gy) |
12 (60%) |
1.9 Gy (1.7–2.0 Gy) |
15 (75%) |
2.0 Gy (1.8–2.1 Gy) |
10 (50%) | 0.71 | 0.06 | 2.0–3.6 Gy |
| V5 Gy (%) |
4.4% (2.5–5.9%) |
4.9% (4.3–5.7%) |
4.7% (3.1–6.3%) |
0.79 | 0.87 | 9.1–23.9% | ||||
| Contralateral Breast | Mean ≤ 3 Gy |
2.2 Gy (1.8–2.5 Gy) |
17 (85%) |
2.0 Gy (1.7–2.4 Gy) |
19 (95%) |
2.1 Gy (1.8–2.5 Gy) |
17 (85%) | 0.57 | 0.62 | 3.4–4.5 Gy |
| V5 Gy (%) |
2.7% (0.4–5.2%) |
6.6% (3.6–9.1%) |
6.6% (4.1–10.8%) |
0.20 | 0.87 | 21.8–30.2% | ||||
| D2cc ≤ 12 Gy |
6.7 Gy (5.2–21.2 Gy) |
13 (65%) |
9.0 Gy (7.5–12.6 Gy) |
15 (75%) |
8.6 Gy (6.9–10.6 Gy) |
17 (85%) | 0.16 | 0.33 | 12.9–22.4 Gy | |
| Oesophagus | D0.1cc ≤ 30 Gy |
16.1 Gy (13.8–22.9 Gy) |
19 (95%) |
15.9 Gy (13.9–20.8 Gy) |
18 (90%) |
16.6 (12.9–19.2 Gy) |
19 (95%) | 0.53 | 0.88 | 27.2–30.7 Gy |
| Spinal Cord | D0.1cc ≤ 20 Gy |
7.3 Gy (6.5–7.9 Gy) |
20 (100%) |
10.9 Gy (8.9–12.2 Gy) |
20 (100%) |
13.3 Gy (11.7–14.6 Gy) |
20 (100%) | < 0.01* | < 0.01* | 12.5–17.2 Gy |
| Humeral Head | D0.1cc ≤ 30 Gy |
29.4 Gy (25.8–31.9 Gy) |
12 (60%) |
26.7 Gy (20.3–32.1 Gy) |
12 (60%) |
24.1 Gy (14.8–28.4 Gy) |
18 (90%) | < 0.01* | 0.24 | 26.0 Gy |
| Thyroid | V30 Gy ≤ 62.5% |
20.8% (2.1–35.9%) |
20 (100%) |
17.7% (0.8–34.3%) |
20 (100%) |
15.6% (0.5–29.4%) |
20 (100%) | 0.32 | 0.55 | DNE |
| Trachea | D0.04cc ≤ 47.5 Gy |
30.3 Gy (25.5–37.3 Gy) |
20 (100%) |
34.2 Gy (27.8–37.9 Gy) |
20 (100%) |
31.6 Gy (25.9–36.3 Gy) |
20 (100%) | 0.96 | 0.34 | DNE |
| Liver | D2cc ≤ 45 Gy |
37.1 Gy (16.9–44.5 Gy) |
8 (80%) |
27.2 Gy (17.8–34.3 Gy) |
10 (100%) |
28.3 Gy (19.0–35.0 Gy) |
10 (100%) | 0.35 | 0.80 | DNE |
LADCA, left anterior descending left coronary artery; D, dose; V, volume; Max, maximum; cc, cubic centimetres; DVH, dose‐volume histogram; MU, monitor unit; IQR, interquartile range; DNE, does not exist.
*Statistically significant with P < 0.05.
The breast nodal KBP model was used to validate bowtie‐ and ipsi‐VMAT plans on each of the 20 remaining CLN‐breast patient data sets (10 left‐ and 10 right‐sided). These plans were generated with a single pass of the KBP model and normalised up to ± 5% to achieve target coverage. The manually generated h‐VMAT calculated on the same 20 data sets were used for comparison. For the purpose of this work, a minimum target coverage of D95% > 95% was mandated per departmental protocol for all three plan types to allow direct comparison of OAR dose‐volume histograms (DVHs).
Quantitative analysis of the dose to each structure was performed by calculating the population DVH median and interquartile range (IQR) for each plan type. Clinical objectives along with ICRU 83 target dose reporting values (D98%, D50%, and D2%), 21 the number of patients meeting each objective and statistical significance of the difference between the ipsi‐VMAT and benchmarked plans determined using Welch’s t test for unequal variances were also assessed. In addition, total MUs were assessed to evaluate treatment efficiency and the homogeneity index, HI (= (D2%–D95%)/D50%) calculated to determine the level of dose variation across the PTVs for each plan type. D95% was chosen in the numerator for HI (instead of D98% per ICRU 83) since it defines the minimum target dose coverage goal, with a HI value of zero indicating that the dose distribution is almost homogeneous. Dose conformity was evaluated per the conformity index, CI defined by van’t Riet et al. 24 Conformity indexes were calculated for the 54.15 Gy (95% of 57 Gy) isodose coverage of the tumour bed volume and the 45 Gy (90% of 50 Gy) isodose coverage of the remaining target volumes combined, noting a CI value of one indicates the dose distribution is perfectly conformal to the target volume.
Blinded clinician plan comparison
The dose distribution and DVH curves of the three plan types generated on the 20‐patient validation cohort were assessed by three subspecialist breast ROs to determine that plan type was preferred. The ROs were blinded to plan type to help prevent any subjective bias based on pre‐conceived notions of increased second malignancy risk founded on current published consensus for breast VMAT. 8 The ROs completed this review together and came to a consensus of their order of preference for the plan types for each patient. A tally of their preferences was taken with 1 point being given to the preferred plan and no points to the other plans. If two plans were considered equal best, then 0.5 points were given to each of those two plan types; and if all three plans were assessed to be equivalent 0.3 points were given to each.
Results
Validation of the iterative breast nodal knowledge‐based plan model
Figure 2 shows target coverage for all plan types was similar due to the optimisation and normalisation process used, with no statistically significant difference between bowtie‐ and ipsi‐VMAT methods. However, as detailed in Table 1, h‐VMAT plans did generate improved minimum D95% isodose coverage in the conserved breast (P < 0.01) at the expense of reduced coverage to all nodal target volumes (P < 0.05). When using either of the bowtie or ipsi‐VMAT techniques, dose homogeneity was slightly reduced but conformity improved when compared to the hybrid approach. An example of the dose distribution generated by each plan type for the same patient is displayed in Figure 3.
Figure 2.
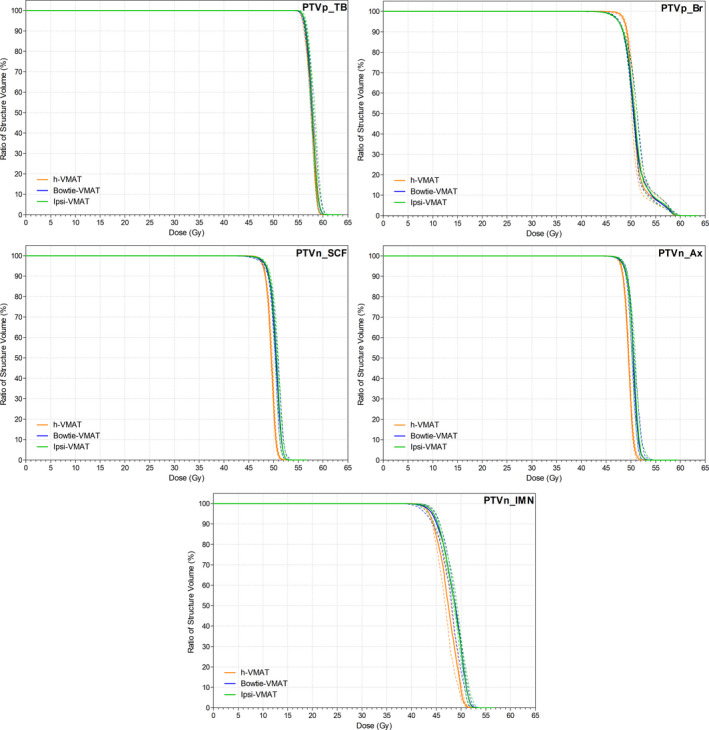
Target Structure DVH comparison. Median and IQR values of percentage dose received to planning target volumes (PTV) for the tumour bed (PTVp_TB), breast (PTVp_Br), supraclavicular nodes (PTVn_SCF), axillary nodes (PTVn_Ax) and internal mammary nodes (PTVn_IMN) for each plan type: h‐VMAT, bowtie‐VMAT and ipsi‐VMAT.
Figure 3.
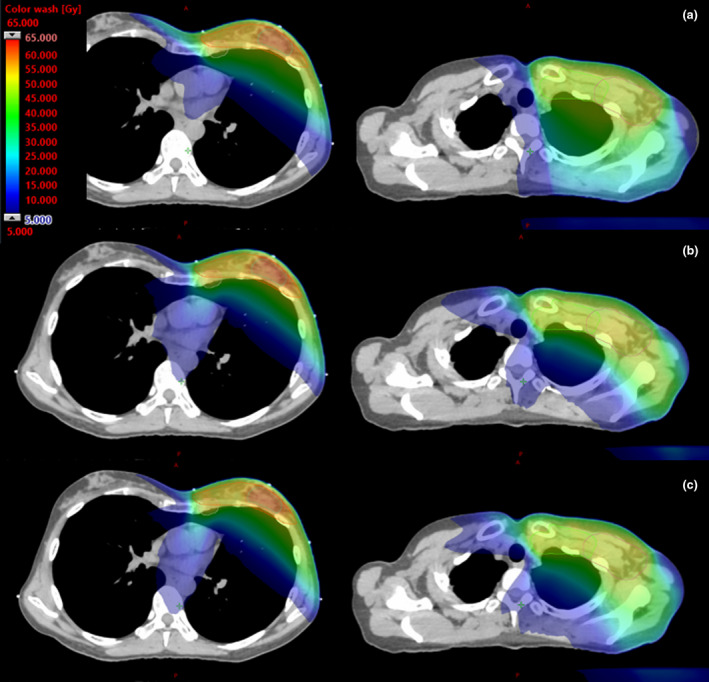
Dose distribution comparison. An example dose distribution achieved by each planning technique on the same left breast DIBH patient for (a) h‐VMAT, (b) bowtie‐VMAT and (c) ipsi‐VMAT techniques. The PTV breast (red), tumour bed (blue), supraclavicular fossa (green), axilla (maroon) and internal mammary chain (pink) are displayed and dose wash on CT slices through the inferior (left) and superior (right) target volumes presented.
With respect to OAR sparing, Figure 4 shows negligible difference in dose between bowtie‐ and ipsi‐VMAT methods except in spinal cord D0.1cc maximum (P < 0.01). Even so, Table 2 details that the maximum spinal cord dose values remained below the 20 Gy goal for all patient plans. In comparison, the h‐VMAT technique generated a statistically significant higher dose to the ipsilateral lung and humeral head in terms of reported mean, V10 Gy, V20 Gy and D0.1cc DVH metrics compared to ipsi‐VMAT with reduced planning goal compliance (P = 0.05, P = 0.04, P < 0.01 and P < 0.01, respectively). However, h‐VMAT did best reduce spinal cord D0.1cc dose maximum when compared to the alternate VMAT options (P < 0.01) with no statistically significant difference in dose to heart, LADCA, contralateral lung or contralateral breast.
Figure 4.
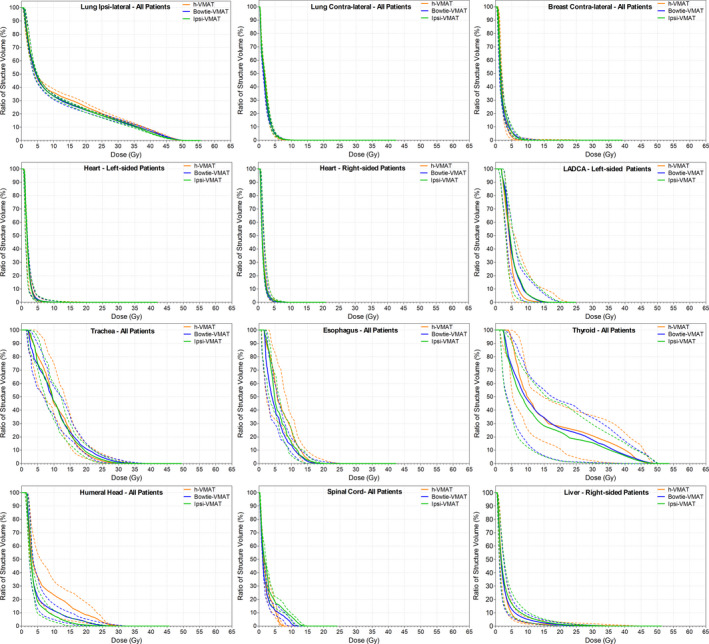
Organs at Risk DVH comparison. Median and IQR values of percentage dose received to the OAR structures for each plan type: h‐VMAT, bowtie‐VMAT and ipsi‐VMAT.
Figure 5 displays the variation in spill dose to the RVR, with no statistically significant difference in low‐dose wash between h‐VMAT (V5 Gy = 19.6%), bowtie‐VMAT (V5 Gy = 20.9%) and ipsi‐VMAT (V5 Gy = 22.8%) techniques. However, as detailed in Table 1, h‐VMAT generated upwards of 30–40% more MU than both bowtie‐VMAT and ipsi‐VMAT methods (839 MU, 595 MU and 652 MU, respectively).
Figure 5.
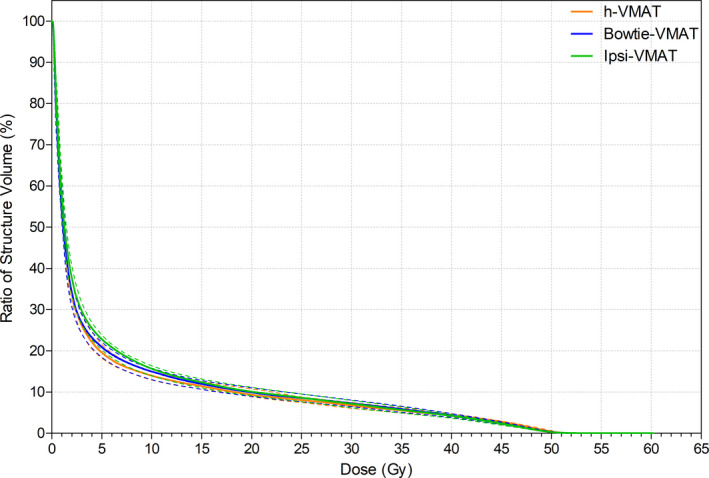
Remaining volume at risk DVH comparison. Median and IQR values of percentage dose received to the remaining volume at risk (Body minus PTVs and OARs) for each plan type: h‐VMAT, bowtie‐VMAT and ipsi‐VMAT.
Blinded clinician plan comparison
Both ipsi‐VMAT and bowtie‐VMAT techniques performed well during the blinded RO‐planning consensus review. When preferencing all patient plans bowtie‐VMAT tallied the highest at 9.8 points, followed by the ipsi‐VMAT technique (8.8 points) and lastly the h‐VMAT technique (1.3 points). Ratio of scores were similar when filtered for laterality.
Discussion
CLN irradiation can improve outcomes for advanced breast cancer patients, but it can be challenging to achieve target coverage and OAR sparing. 8 Recent literature suggests that the balance is changing between the clinical importance of increased low‐dose wash of IMRT or VMAT compared to improvements in local cancer control and reduced OAR toxicity. 25 , 26 Even so, further clinical outcome data are needed to allay concerns of increased potential second malignancy risk. 27 , 28 Indeed, recent breast nodal planning studies show increasingly complex beam modification methods (hybrid plans, avoidance sectors, other) in order to improve plan quality and limit low‐dose wash. 5 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 29 , 30 However, by applying iterative KBP modelling, this study demonstrates a simple ipsi‐VMAT solution for CLN‐breast patients can limit low‐dose wash to the heart, lungs, contralateral breast and RVR without compromise in plan quality when compared to tangentially constrained h‐VMAT (departmental standard) and bowtie‐VMAT (published best practice) benchmark methods. As such, use of a simple VMAT technique should not be discounted in the nodal breast clinical setting so long as optimisation is sufficiently refined to limit low‐dose wash and produce the plans intended.
Both ipsi‐VMAT and bowtie‐VMAT plans in this study were practically equivalent in terms of target coverage, OAR sparing and MU. Compared to the h‐VMAT plans, the ipsi‐VMAT plans gave improved nodal target coverage, conformity and dose to ipsilateral lung and humeral head. The trade‐off was a marginal reduction in breast target coverage, homogeneity and increased dose to spinal cord. This dose distribution was preferred by our subspecialist breast ROs in the blinded plan review in‐line with the SKAGEN order of priority (noting the lower dose coverage in conserved breast was in regions of low risk away from the tumour bed), 23 with the quality of the ipsi‐VMAT plans adjudged to be equivalent to bowtie‐VMAT and superior to h‐VMAT. In many Institutions, there may be embedded belief that ipsi‐VMAT contributes increased risk of second malignancy with its clinical application. Our quantitative and qualitative analysis of this cohort should support an evolution in such beliefs that simple ipsi‐VMAT performs equivocally with much more complex techniques in dosimetry. There are clear advantages to workflow, with the highly refined ipsi‐VMAT KBP model with preset beam geometry providing an automated class solution that significantly simplifies the CLN‐breast planning process by being robust to patient‐specific anatomical variation in addition to removing need for any complex beam modification. This has anecdotally helped our department improve planning quality, consistency and efficiency (reduced planning time) compared to our previous in‐house h‐VMAT solution; whilst the reduced MU load is also expected to improve patient compliance in DIBH to better spare the heart. 8 , 17
Compared to the majority of DVH objectives commonly reported by published literature in the CLN‐breast setting (with standard 50 Gy in 25 fraction prescription), we have demonstrated that an iterative KBP ipsi‐VMAT solution achieves superior OAR doses (Table 2) even with addition of a SIB of 57 Gy to the tumour bed. It should be noted, however, that the overlapping SIB volume in the breast target prevents direct comparison of HI to plans with single‐dose levels, and that the comparative review is limited . Results could also be influenced by planning left‐sided patients in DIBH, using an Acuros XB dose‐to‐medium calculation algorithm, 31 or that the Varian Halcyon treatment unit is installed with a dual layer MLC (reducing MLC leakage). But given the inherent limitations of planning comparison studies, we are prospectively collecting outcome and toxicity data on all patients to compliment this work for future reporting purposes.
Since clinically implementing the ipsi‐VMAT technique on our Varian Halcyon treatment unit in mid‐2020, we have found need to produce separate KBP models in both breast alone and breast/SCF settings to better spare heart, lungs and contralateral breast. Meanwhile we have found no issue in adapting the models to chest‐wall (including expander) and bilateral patients, although all models have had to be reconfigured for hypo‐fractionated regimes where prescribed. Similarly, we have found no issue in applying the models for treatment on Varian TrueBeam treatment units (Millennium MLC) so long as jaw tracking is applied to reduce MLC leakage; that is, maintain low‐dose wash equivalence between plans. To ensure plan robustness to inter‐ and intra‐fraction motion, skin flash is added per the recommendations of Rossi et al. 32 Specifically, an 8mm virtual bolus (−350HU) and 5mm planning PTV extension outside the Body was introduced for optimisation with the breast KBP model before virtual bolus was removed for dose calculation and re‐normalisation. 33 For any systematic deformations in body structure greater than 1.0cm observed on daily cone beam computed tomography (CBCT), re‐planning is requested by treatment staff. 32
Conclusions
A simple ipsilateral VMAT solution for CLN‐breast cancer generated using iterative KBP modelling can achieve clinically acceptable target coverage and OAR sparing without increase in low‐dose wash compared to benchmark base‐tangential techniques. This automated class solution significantly simplifies the CLN‐breast planning process by being robust to patient‐specific anatomical variation in addition to removing need for any complex beam modification.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not‐for‐profit sectors.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgement
The authors gratefully acknowledge all the staff at Northern Sydney Cancer Centre for making this work possible.
J Med Radiat Sci. 69(2022) 85–97
Data Availability Statement
Available from the corresponding author on reasonable request.
References
- 1. Australian Institute of Health Welfare , Cancer data in Australia. AIHW, 2020. [Cited 16 July, 2016]. Available from: https://www.aihw.gov.au/reports/cancer/cancer‐data‐in‐australia
- 2.Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effect of radiotherapy after mastectomy and axillary surgery on 10‐year recurrence and 20‐year breast cancer mortality: meta‐analysis of individual patient data for 8135 women in 22 randomised trials. The Lancet 2014; 383: 2127–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Poortmans PM, Collette S, Kirkove C, et al. Internal mammary and medial supraclavicular irradiation in breast cancer. N Engl J Med 2015; 373: 317–27. [DOI] [PubMed] [Google Scholar]
- 4. Wang X, Yu TK, Salehpour M, Zhang SX, Sun TL, Buchholz TA. Breast cancer regional radiation fields for supraclavicular and axillary lymph node treatment: Is a posterior axillary boost field technique optimal? Int J Radiat Oncol Biol Phys 2009; 74: 86–91. [DOI] [PubMed] [Google Scholar]
- 5. Kuo L, Ballangrud ÅM, Ho AY, Mechalakos JG, Li G, Hong L. A VMAT planning technique for locally advanced breast cancer patients with expander or implant reconstructions requiring comprehensive postmastectomy radiation therapy. Med Dosim 2019; 44: 150–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang Q, Liu J, Ao N, et al. Secondary cancer risk after radiation therapy for breast cancer with different radiotherapy techniques. Sci Rep 2020; 10: 1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fogliata A, De Rose F, Franceschini D, et al. Critical appraisal of the risk of secondary cancer induction from breast radiation therapy with volumetric modulated arc therapy relative to 3D conformal therapy. Int J Radiat Oncol Biol Phys 2018; 100: 785–93. [DOI] [PubMed] [Google Scholar]
- 8. Cozzi L, Lohr F, Fogliata A, et al. Critical appraisal of the role of volumetric modulated arc therapy in the radiation therapy management of breast cancer. Radiat Oncol 2017; 12: 200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dumane VA, Bakst R, Green S. Dose to organs in the supraclavicular region when covering the Internal Mammary Nodes (IMNs) in breast cancer patients: a comparison of Volumetric Modulated Arc Therapy (VMAT) versus 3D and VMAT. PLoS One 2018; 13: e0205770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van Duren‐Koopman MJ, Tol JP, Dahele M, et al. Personalized automated treatment planning for breast plus locoregional lymph nodes using Hybrid RapidArc. Pract Radiat Oncol. 2018; 8: 332–41. [DOI] [PubMed] [Google Scholar]
- 11. Pasler M, Lutterbach J, Björnsgard M, Reichmann U, Bartelt S, Georg D. VMAT techniques for lymph node‐positive left sided breast cancer. Med Phys 2015; 25: 104–11. [DOI] [PubMed] [Google Scholar]
- 12. Ranger A, Dunlop A, Hutchinson K, et al. A dosimetric comparison of breast radiotherapy techniques to treat locoregional lymph nodes including the internal mammary chain. Clin Oncol (R Coll Radiol) 2018; 30: 346–53. [DOI] [PubMed] [Google Scholar]
- 13. Iorio GC, Franco P, Gallio E, et al. Volumetric modulated arc therapy (VMAT) to deliver nodal irradiation in breast cancer patients. Med Oncol 2017; 35: 1. [DOI] [PubMed] [Google Scholar]
- 14. Yu P‐C, Wu C‐J, Nien H‐H, Lui LT, Shaw S, Tsai Y‐L. Tangent‐based volumetric modulated arc therapy for advanced left breast cancer. Radiation Oncology 2018; 13: 236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rossi M, Boman E, Kapanen M. Contralateral tissue sparing in lymph node‐positive breast cancer radiotherapy with VMAT technique. Med Dosim 2019; 44: 117–21. [DOI] [PubMed] [Google Scholar]
- 16. Xie Y, Bourgeois D, Guo B, Zhang R. Postmastectomy radiotherapy for left‐sided breast cancer patients: comparison of advanced techniques. Med Dosim 2020; 45: 34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fogliata A, Nicolini G, Bourgier C, et al. Performance of a Knowledge‐Based Model for Optimization of Volumetric Modulated Arc Therapy Plans for Single and Bilateral Breast Irradiation. PLoS One 2015; 10: e0145137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fogliata A, Cozzi L, Reggiori G, et al. RapidPlan knowledge based planning: iterative learning process and model ability to steer planning strategies. Radiation Oncology 2019; 14: 187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Offersen BV, Boersma LJ, Kirkove C, et al. ESTRO consensus guideline on target volume delineation for elective radiation therapy of early stage breast cancer. Radiother Oncol 2015; 114: 3–10. [DOI] [PubMed] [Google Scholar]
- 20. Feng M, Moran JM, Koelling T, et al. Development and validation of a heart atlas to study cardiac exposure to radiation following treatment for breast cancer. Int J Radiat Oncol Biol Phys 2011; 79: 10–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. ICRU . Prescribing, recording, and reporting photon‐beam intensity‐modulated radiation therapy (IMRT). ICRU Report 83. J. ICRU. 2016; 10. 10.1093/jicru/ndq002 [DOI] [Google Scholar]
- 22. Jöst V, Kretschmer M, Sabatino M, et al. Heart dose reduction in breast cancer treatment with simultaneous integrated boost. Strahlenther Onkol 2015; 191: 734–41. [DOI] [PubMed] [Google Scholar]
- 23. Danish Breast Cancer Cooperative Group . The SKAGEN Trial 1. Moderately hypofractionated loco‐regional adjuvant radiation therapy of early breast cancer combined with a simultaneous integrated boost in patients with an indication for boost: DBCG HYPO II, a randomised clinically controlled trial. [Cited 25 June, 2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT02384733. Published 2015.
- 24. Avt R, Mak ACA, Moerland MA, Elders LH, van der Zee W. A conformation number to quantify the degree of conformality in brachytherapy and external beam irradiation: application to the prostate. Int J Radiat Oncol Biol Phys 1997; 37: 731–6. [DOI] [PubMed] [Google Scholar]
- 25. Donovan EM, James H, Bonora M, Yarnold JR, Evans PM. Second cancer incidence risk estimates using BEIR VII models for standard and complex external beam radiotherapy for early breast cancer. Med Phys 2012; 39: 5814–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Filippi AR, Vanoni V, Meduri B, et al. Intensity modulated radiation therapy and second cancer risk in adults. Int J Radiat Oncol Biol Phys 2018; 100: 17–20. [DOI] [PubMed] [Google Scholar]
- 27. Stovall M, Smith SA, Langholz BM, et al. Dose to the contralateral breast from radiotherapy and risk of second primary breast cancer in the WECARE study. Int J Radiat Oncol Biol Phys 2008; 72: 1021–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Xie L, Lin C, Zhang H, Bao X. Second malignancy in young early‐stage breast cancer patients with modern radiotherapy: A long‐term population‐based study (A STROBE‐compliant study). Medicine 2018; 97: e0593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lai Y, Chen Y, Wu S, et al. Modified volumetric modulated arc therapy in left sided breast cancer after radical mastectomy with flattening filter free versus flattened beams. Medicine 2016; 95: e3295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Coffey A, Renucci L, Hunzeker A, Lenards N. Whole breast nodal irradiation using supine VMAT and prone 3D planning: a case study. Med Dosim 2017; 42: 185–9. [DOI] [PubMed] [Google Scholar]
- 31. Zifodya JM, Challens CHC, Hsieh W‐L. From AAA to Acuros XB‐clinical implications of selecting either Acuros XB dose‐to‐water or dose‐to‐medium. Australas Phys Eng S 2016; 39: 431–9. [DOI] [PubMed] [Google Scholar]
- 32. Rossi M, Boman E, Kapanen M. Optimal selection of optimization bolus thickness in planning of VMAT breast radiotherapy treatments. Med Dosim 2019; 44: 266–73. [DOI] [PubMed] [Google Scholar]
- 33. Lizondo M, Latorre‐Musoll A, Ribas M, et al. Pseudo skin flash on VMAT in breast radiotherapy: Optimization of virtual bolus thickness and HU values. Physica Med 2019; 63: 56–62. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available from the corresponding author on reasonable request.


