P.138
Systemic Sclerosis–Rheumatoid Arthritis Overlap Syndrome. Description of 10 Incidents
N. Zotos1, M. Gianniki2, M. Gerasimou1, E. Tatsina1, D. Bougias2, L. Papageorgiou1, C. Mitsis1, A. Zotou1, A. Pournou1, N. Tsifetaki2
1 Immunology Department, Ioannina, Greece, 2 Rheumatology Department, Ioannina, GREECE
Introduction: During the last six years among the patients, diagnosed with Diffuse Systemic Scleroderma, that had follow up care in our department, 10 of them were identified with coexisting Rheumatoid Arthritis, ACR criteria. Patients with Mixed Connective Tissue Disease and Systemic Lupus Erythematosus/Systemic Sclerosis overlap syndrome were excluded.
Material and Methods: These are 8 women and 2 men aged 33 to 71 and disease duration was 8-24 years. The first symptom of all patients was arthritis of the small joints of the hand, followed by the Raynaud Phenomenon. All of them had esophageal and pulmonary involvement with affected lung function tests (type of restrictive lung disease) and CT findings. All patients exhibited wrist osteoarthritis, proximal interphalangeal joints arthritis, metacarpophalangeal joint arthritis and one of them exhibited temporomandibular joint osteopenia, narrowing of medial joint space, and radiographic erosions.
Results: All of them had increased CRP and Gamma globulins levels, positive ANA test (>1/640 speckled/nucleolar), 4 patients had positive RF test, 4 patients had positive anti-CCP antibodies test, 2 patients had positive anti-CCP antibodies and RF test and 9 patients had positive anti-Scl-70 antibodies test.
Patients showed progressive progression of arthritis despite treatment with D-Penicillamine n=10, prednisolone n=10, hydroxychloroquine n=8, methotrexate n=7, azathioprine n=2, cyclophosphamide n=8,anti TNF n=2.
Conclusions: A percentage of erosive RA overlap syndrome was observed in patients with Diffuse Systemic Scleroderma. These patients are a subgroup with pulmonary affection, positive SCL70 antibodies test, increased CRP levels, and positive RF and/or anti-CCP antibodies test. Our results are consistent with the international literature regarding the clinical-laboratory profile of these patients.
P.139
Interleukin-17 and Interleukine-23 Profile and Clinical Association in Patients with Systemic Sclerosis
A. Zekovic, N. Damjanov
Institute of Rheumatology, Belgrade, SERBIA
Introduction: Growing evidence suggests that T-cell proliferation and cytokine secretion play role in the pathogenesis of systemic sclerosis (SSc). In this study we evaluated Interleukin-17A(IL17A), Interleukin-17F(IL17F) and interleukine-23 (IL23) profile in patients with systemic sclerosis and assessed its association with organ involvement in SSc.
Material and Methods: Study included 63 patients with SSc and 13 healthy controls. We measured IL-17 and IL-23 production in peripheral blood mononuclear cells (PBMCs) by reverse transcriptase-polymerase chain reaction (qRT-PCR) and enzyme-linked immunosorbent assay (ELISA). Patients were assessed for organ involvement associated with SSc.
Results: IL-17A mRNA levels were increased in all patients with SSc and significantly increased in patients with disease duration of 5 to 10 years and > 15 years (4.7 vs 1.2 and 6.1 vs. 1.2, p< 0.05, respectively) compared to controls. In patients with disease duration < 5 years, IL-17F mRNA and IL-23 mRNA were decreased, compared to controls (0.63 vs. 1.2 and 0.73 vs. 1.1, p<0.01). IL-17 and IL-23 serum concentration was higher in patients with interstitial lung involvement (ILD), compared to controls (p< 0.05). IL-23 serum levels were positively associated with total GIT score (r 0.35, p<0.05). Kidney impairment was associated with higher levels of IL-17 in SSc patients, compared to controls (p< 0.05).
Conclusions: There is a correlation between disease duration and changes in IL-17 and IL-23 levels in SSc. IL-17 overproduction in SSc patients may be associated with ILD and kidney involvement, while IL-23 levels correlate with GIT impairment.
P.140
The Association of Sociodemographic and Disease Variables with Hand Function in Systemic Sclerosis: a Scleroderma Patient-Centered Intervention (Spin) Cohort Study
K. Turner1, L. Kwakkenbos1,2, T. Sanchez1, M. Carrier1, L. Mouthon3, M. Hudson 1, 4, E. Van Den Ende5, A. Schouffoer6, J. Welling7, M. Sauvé8, B. Thombs1, 2
1 Lady Davis Institute for Medical Research, Jewish General Hospital, Montreal, CANADA, 2 Department of Psychiatry, McGill University, Montreal, CANADA, 3 Université Paris Descartes, Paris, FRANCE, 4 Department of Medicine, McGill University, Montreal, CANADA, 5 Sint Maartenskliniek, Nijmegen, THE NETHERLANDS, 6 Leiden University Medical Center, Leiden, THE NETHERLANDS, 7 Dutch patient organization for systemic autoimmune diseases (NVLE), Nijmegen, THE NETHERLANDS, 8 Scleroderma Society of Ontario and Scleroderma Canada, Hamilton, CANADA
Introduction: Impaired hand function in systemic sclerosis (SSc) is a primary cause of disability and contributes to lower health-related quality of life. Many disease manifestations, including digital ulcers (DU), skin involvement, Raynaud’s syndrome, synovitis, joint contractures, and tendon friction rubs may influence hand function. Only two relatively small studies have used multivariable analyses to examine factors associated with hand function, and both found that DU influences hand functioning. However, no large multivariable studies have examined the range of factors that may be associated with hand function in SSc. The objective of this study was to evaluate the independent associations of sociodemographic, lifestyle, and disease-related factors with hand functioning in SSc.
Material and Methods: The sample consisted of patients enrolled in the Scleroderma Patient-centered Intervention Network Cohort. Hand function was measured using the Cochin Hand Function Scale. Multiple linear regression analysis was used to identify independent correlates of impaired hand function. Variables entered into the model were selected a priori and included demographic characteristics; disease subtype; disease duration; modified Rodnan Skin Score; severity of Raynaud’s phenomenon; presence of puffy fingers, sclerodactyly, fingertip pitting scars, digital tip ulcers, tendon friction rubs, small joint contractures, skin thickening proximal to the metacorpophalangeal joints; presence of systemic lupus erythematosus, Sjogren’s syndrome, rheumatoid arthritis, and idiopathic inflammatory myositis; body mass index; alcohol consumption; and smoking.
Results: In total, 952 participants (88% female) had complete data for all variables and were included in the analysis. Participants had a mean age of 55.3 years (SD = 12.2). Average disease duration was 11.2 years (SD = 8.7). Variables significantly associated with more impaired hand function in the multivariate model included having diffuse SSc (standardized regression coefficient, beta (β)= 0.16, p < 0.001), Raynaud’s phenomenon severity (β = 0.22 p < 0.001), finger ulcer severity (β = 0.25, p < 0.001,) having moderate (β = 0.17, p < 0.001) or severe small joint contractures (β = 0.21, p < 0.001), having rheumatoid arthritis (β = 0.06, p = 0.030), and having idiopathic inflammatory myositis (β = 0.07, p = 0.009), a higher body mass index (β = 0.08, p = 0.003), and currently smoking (β = 0.08, p = 0.004).
Conclusions: The findings of this study will help inform therapeutic and self-care interventions that target impaired hand function.
P.141
Causes and Predictors of Mortality in Systemic Sclerosis in South Africans
M. Tikly, C. Ickinger, Z. Dire
Chris Hani Baragwanath Hospital, University of the Witwatersrand, Johannesburg, SOUTH AFRICA
Introduction: Systemic sclerosis (SSc) is known associated with significant morbidity and mortality but to date no studies have been published on causes of death and predictors of mortality in South Africa. The objective of the present study was to determine the spectrum of causes of death and to determine predictors of death in patients with SSc attending a tertiary centre in urban South Africa.
Material and Methods: A retrospective record review of 174 patients who attended the Connective Tissue disease clinic at Chris Hani Baragwanath Academic Hospital from 1990-2015 was undertaken
Results: 92.5% of the patient were of African descent .The female to male ratio was 7:1. The mean age at diagnosis was 42. The mean follow up duration was 65.8 months. The estimated survival rates were at 5 years and 10 years. The major cause of death was cardiopulmonary. Univariate analysis for predictors of mortality shows that digital ulcers, telangiectasia, cor pulmonale, proteinuria, renal dysfunction and high CRP are associated with a high mortality
Conclusions: The cause of death in our study was predominantly disease related which is in accordance which that reported in other studies. With cardiopulmonary being the leading cause of death matching that reported in recent data. SSc still carries a high mortality rate.
P.142
The Validation of Cochin Hand Functional Scale Questionnaire in Turkish Speaking Patients with Systemic Sclerosis
D. Temiz Karadag, S. Tekeoglu, O. Ozdemir Isik, A. Yazicioglu, A. Cefle
Kocaeli University Medicine School- Department of Rheumatology, Kocaeli, TURKEY
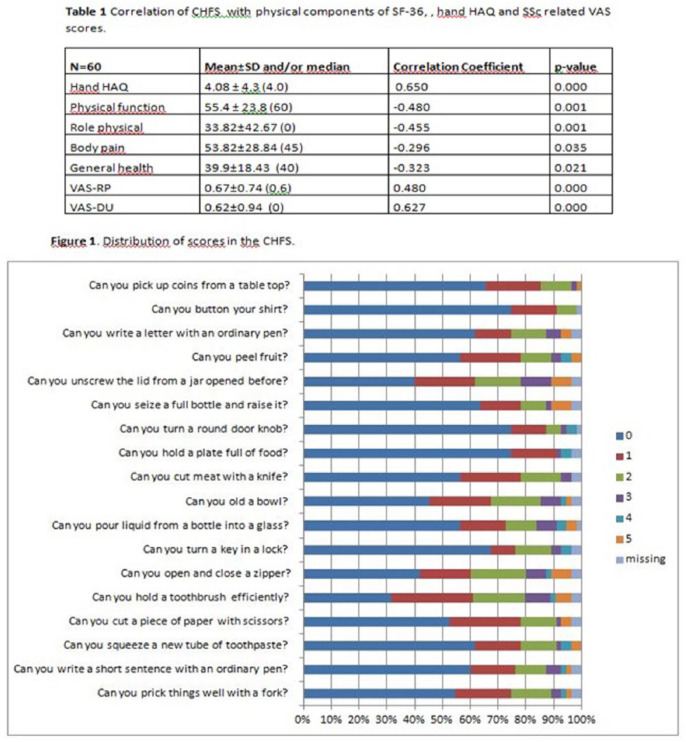
Introduction: The Duruöz Hand Index, also called the Cochin Hand Function Scale (CHFS), is a self-reported disability questionnaire that includes 18 items about daily activities related to hand function in rheumathoid arthritis patients. The objective of this study is to perform cross-cultural adaptation and validation of the CHFS in patients with SSc.
Material and Methods: Fifty five patients who fulfilled the 2013 ACR/EULAR Classification Criteria for Systemic Sclerosis ACR criteria for SSc were recruited. Fithy five percent of the patients fulfilled the criteria for limited systemic sclerosis (lcSSc). We evaluated intraobserver reproducibility using the intraclass correlation coefficient (ICC). The known-groups construct validity was obtained by stratifying patients according to involvements related to hand functions. We evaluated the convergent validity using Spearman’s correlation with hand related items of Health Assessment Questionnaire (hand-HAQ), visual analogue scale (VAS) related to Raynaud phenomenon (RP), VAS related to digital ulcers (DU) and physical components of Short Form 36 version 2(SF36v2).
Results: Results: Eighty percent of the patients were female and the median age was 56 years old. Finger tip digital ulcers were observed in 15 patients (27.3%), pitting scars in 27 (49%), calcinosis in 5 (9%) and contractures in 4 (7.3%). CHFS demonstrated high retest reliability (ICCs= 0.784–0.946) and showed negative correlation with physical function, role physical, bodily pain and general health components of physical-related scores in the SF-36 (r=-0.480 ;– 0.455;-0.296; -0.323, respectively). The reproducibility in the CHFS was good (intra-class correlation coefficients greater than 0.75). CHFS correlated well with hand-HAQ, VAS-RP and VAS-DU in S-HAQ (r= 0.650; 0.480; 0.627, respectively); with total MRSS and MRSS of the hands (r=0.396; 0.717, respectively). Although the instruments could not discriminate between the subsets of SSc, patients with digital ulcers and contractures had significantly higher scores (p=0,004 and 0,003 respectively).
Conclusions: The Turkish version of the Cochin hand functional scale questionnaire meet the requirements of reproducibility and validity. This study forms the basis for future studies to evaluate the properties of Cochin hand functional scale questionnaire in Turkish speaking SSc patients more extensively.
P.143
Withdrawn
P.144
Cytokine/Growth Factors Multiplex Assay Reflects/Identifies Phenotypic Variations among Scleroderma Patients
Y. Suliman1, S. Kafaja2, M.F. Alemam3, I. Valera2, J. Grotts4, D.E. Furst2
1 Rheumatology and Rehabilitation Dept., Faculty of Medicine. Assiut University, Assiut, EGYPT, 2 Rheumatology Division, Department of Medicine. David Geffen School of Medicine. University of California Los Angeles, Los Angeles, USA, 3 Clinical Pathology and Laboratory Medicine. Qena Faculty of Medicine. South Valley University, Qena, EGYPT, 4 biostatistics core, university of California Los Angeles, Los Angeles, USA
Introduction: Systemic sclerosis (SSc)is a complex disease characterized by diverse clinical presentations, which reflects heterogeneous pathogenic mechanisms. Circulating proteins in SSc serum offer the potential to identify different driving pathogenic pathways, as well as surrogate markers for clinical outcomes. We used multiplex analysis to profile well-characterized SSc patients and identify potential surrogate markers for varied phenotypic presentations.
Material and Methods: Serum samples from 70 SSc patients meeting the ACR/EULAR 2013 SSc criteria and 8 healthy controls were recruited. A custom 15-plex magnetic kit included selected markers: innate immune function ( IL-1b, IL-1RA, TNF-a, IL-6, IP-10 and IFN-a ), adaptive immune function (IL-10, IFN-g and IL-17A a), Chemokines (MIP-1a) and Growth factors with vascular functions (EGF, FGF-2, VEGF-A, PDG-AA, and PDG-AB/BB). Marker levels in SSc versus ctr were compared by Wilcoxon Rank Sum test. Linear regression model was used to evaluate the relation between clinical parameters and measured immune markers.
Results: In 70 pts, mean age 56 (± 13.9) yrs; 58 (84%) females, PAH: 23(32%); skin ulcers: 19(28%) interstitial lung disease (ILD): 40 (55%) (table1).
Multiplex profiling of serum of SSc patients showed lower levels of tested markers in SSc pts vs controls in the following: PDGF-AB/BB, EGF, IFNa2, IL-17A and IP-10(p= 0.025, 0.011, 0.012, 0.038 and 0.062 respectively). Multiple correlations were seen between the markers and clinical variables as well as patient reported outcomes (PROs).
ILD associated significantly with innate (TNF-a),Adaptive(IL-10, IL-17) and growth factor vascular markers (VEGF). Echocardiographic findings: Ejection fraction related significantly to growth factors and chemokines (VEGF, MIP-1a),Right ventricular systolic pressure [RVSP] and related to innate and adaptive immunity (TNf-a, IL-6, IL-17, IP-10, IL-10).
For each of the below, p<0.05. Patient global correlated with all pathogenetic aspects: innate (TNF-a, IL-1b, IL-6, IP-10), adaptive ( IL-10), growth factors (FGF)and chemokines(MIP-1a), as expected. Breathing VAS, Raynaud’s VAS, Skin ulcer VAS and gastrointesinal VASs all related reasonably and logically to aspects of immune function, vascular abnormality, growth factors and chemokines. HAQ-DI related only to IL-1RA.
Conclusions: We examined a selected number of immune biomarkers which seem to correlate with clinical and pt reported outcome measures. Further longitudinal studies are warranted, which may aid in developing predictors of disease severity and organ involvement.
P.145
Humanistic and Cost Burden of Systemic Sclerosis: a Review of the Literature
A. Fischer1, E. Zimovetz2, C. Ling2, D. Esser3, N. Schoof3
1 University of Colorado School of Medicine, Denver, USA, 2 RTI Health Solutions, Manchester, UNITED KINGDOM, 3 Boehringer Ingelheim GmbH, Ingelheim, GERMANY
Introduction: Systemic sclerosis (SSc), or systemic scleroderma, is a chronic multisystem autoimmune disease characterised by widespread vascular injury and progressive fibrosis of the skin and internal organs. Patients with SSc have decreased survival, with pulmonary involvement as the main cause of death. Current treatments for SSc manage a range of symptoms but not the cause of the disease. Our review describes the humanistic and cost burden of SSc.
Material and Methods: A structured review of the literature was conducted, using predefined search strategies to search PubMed, Embase, and the Cochrane Library. Grey literature searches also were conducted.
Results: In total, 2,226 articles were identified in the databases and 52 were included; an additional 10 sources were included from the grey literature. The review identified six studies reporting relevant cost estimates conducted in five different countries and four studies that assessed the humanistic burden of SSc. Total direct annual medical costs per patient for Europe varied from €3,544 to €8,452. For Canada, these costs were reported to be from Can$5,038 to Can$10,673. In the United States, the total direct health care costs were reported to be US$17,365 to US$18,396. Different key drivers of direct costs were reported, including hospitalizations, outpatients, and medication. The total annual costs per patient were reported at Can$18,453 in Canada and varied from €11,074 to €22,459 in Europe. Indirect costs represented the largest component of the total costs. EQ-5D utility scores were lower for patients with SSc than those observed in the general population, with reported mean values of 0.49 and 0.68, respectively. The average value of the Health Assessment Questionnaire for patients with SSc was significantly higher than the control population (0.94), and the average value of the SF-36 was significantly lower than the control population: 49.99 for the physical dimension and 58.42 for the mental dimension.
Conclusions: Overall, there is a paucity of information on the burden of SSc. Nonetheless, our review indicates that the quality of life of patients with SSc is considerably lower than that of the general population. In, addition, SSc places a considerable economic burden on health care systems and society as a whole.
P.146
Clinical Characterisation of 133 Adults with Linear Morphoea; Comparing Paediatric and Adult Onset Disease
A. Saracino, C. George, V. Ong, C. Fonseca, C. Orteu, C. Denton
Royal Free Hospital, London, UNITED KINGDOM
Introduction: Linear morphoea (LM) is an uncommon and severe subtype of morphoea affecting the trunk, limbs and/or craniofacial sites. It can be potentially debilitating, with extracutaneous manifestations (ECM) and permanent disfiguring scarring. LM is more prevalent in paediatric populations, and our knowledge of disease in adults is limited.
Material and Methods: Utilizing the unique patient cohort at our tertiary-referral scleroderma service, we conducted a clinico-epidemiological study of patients presenting with LM from January 2014 to April 2017. We aimed to characterize our large adult cohort, and compare adult and paediatric onset disease.
Results: Of 298 patients presenting with a diagnosis of morphoea, 133 (44.6%) had LM; 77.8% were female. Fifty-eight (43.6%) had adult onset LM. Mean age of disease onset was 10.4 years in paediatric onset vs. 35.5 years in adult onset. There was a 2-year mean delay to diagnosis (95% CI: 1.5-2.5). Those with paediatric onset LM had significantly more cumulative disease related damage, as reflected by a mean peak mLoSDI score of 19.5 (95% CI: 17.0-22.0) compared to 8.1 (95% CI: 4.4-11.8) in the adult onset group (p<0.001). Significantly more patients with adult onset LM had quiescent disease (controlled on therapy or in remission) than those with paediatric onset LM (22 (55.0%) vs 9 (29.0%), p=0.0332). There were no other significant differences in clinical features, investigation parameters or prescribed treatments in adult and paediatric onset groups. Cutaneous symptoms were present in 89 patients (66.9%); more prevalent amongst those with LM of the trunk/limbs (p=0.001, OR 3.4 [95%CI: 1.4-7.5]). ECM were recorded in 76 (57.1%) patients overall, including Raynaud’s in 26 (19.5%). Fatigue, joint involvement and raised eosinophil counts were more prevalent in those with >1 affected body site (p<0.05). ANA was positive in 40.4%, raised ESR present in 25.0% and raised immunoglobulins in 27.3%. The most commonly prescribed treatments were methotrexate (n=98, 73.7%), 0.5% tacrolimus ointment (n=64, 48.1%) and intravenous pulsed methylprednisolone (n=61, 45.9%). Of those with active paediatric onset disease on treatment, the mean time since disease onset was 15.9 years.
Conclusions: To our knowledge, we have described the largest cohort of adults with LM. The prevalence of ECM, joint involvement and raised serological markers, some particularly prevalent in those with more widespread disease, highlight the systemic nature of LM. Notably, disease was more likely to be active amongst those with paediatric onset disease, with higher cumulative disease related damage. Thus, management guidelines for subgroups of adults with LM may have clinical utility.
P.147
Significant Impact of Skin Disease in Systemic Sclerosis and Patient Perceived Benefits of Specialist Dermatology Input
A. Saracino, A. Mizara, V. Ong, C. Denton
Royal Free Hospital, London, UNITED KINGDOM
Introduction: The complex and life-threatening nature of systemic sclerosis (SSc) is challenging and necessitates multi-speciality management. Potentially life-threatening internal organ involvement has historically been the main clinical and research focus in SSc and other connective tissue diseases. However, dermatological manifestations can result in significant symptoms, functional impairment, disfiguring scarring and negative body image. Despite this skin related disease burden, dermatological manifestations often remain under-prioritised and under-treated. The objectives of this study were to establish the QoL and psychosocial impact of skin manifestations in patients with SSc, and determine the patient perceived benefits of dermatological input.
Material and Methods: This was a prospective questionnaire-based study of randomly selected patients seen at our tertiary referral scleroderma service from April to August 2016. All patients had cutaneous manifestations and were seen by a consultant dermatologist on the day of their appointment. A study questionnaire was completed by all participants’ pre and post dermatological consultation.
Results: Fifty-patients were included (68% female). The majority of patients had an underlying diagnosis of SSc (n=38, 76%) or SSc-overlap (n=9, 18%). Musculoskeletal involvement was recorded in 78%, gastrointestinal involvement in 46%, lung disease in 32% and renal involvement in 12%. Skin complications were most frequently selected as the disease manifestations patients “worried about the most” (n=18, 36%). When asked which organ(s) “affect your daily life the most”, skin was also most frequently selected (n=34, 68%). Average pre-dermatology consultation Visual Analogue Scale (VAS) score for skin related “concern” was 7.8 ([SD=2.0], range 4 to 10), falling to 4.3 immediately post-dermatology consultation ([SD=2.0], range 0 to 9; p<0.05). All patients ‘strongly agreed’ that seeing a dermatologist was helpful, added value to the rheumatology led scleroderma service and hoped it would be available at future appointments.
Conclusions: This study highlights the significant skin burden and related psychosocial and QoL impact in SSc. Cutaneous manifestations resulted in more “worry” and “effect on daily life” than other organ systems. Such impact was present despite the concurrent existence of often significant internal organ disease. To date, potentially life-threatening complications have been the main focus in SSc. However, as long-term outcomes improve, it is important to focus also on the psychosocial effects of skin and appearance. We have demonstrated the importance of formally measuring this, and the potential benefits of routine shared multispecialty management.
P.148
Systemic Sclerosis - a 12 Years Retrospective Study of an Internal Medicine (Autoimmune Diseases) and Rheumatology Appointments in a Small Hospital Centre
A. Sanches, R. Assis, S. Martins, J. Madruga, J. Garcia, M. Carvalho
CHMT- Centro Hospital do Médio Tejo, Unidade de Torres Novas, Torres Novas, PORTUGAL
Introduction: Systemic sclerosis (SSc) is an autoimmune disease characterized by excessive deposition of collagen fibers. The prevalence rates range from 4-489 per million individuals. The clinical manifestations are diverse (from localized skin involvement to multi-systemic affection) as are the severity and outcome of the disease. The authors aimed to characterize the patients with SSc followed in Internal Medicine and Rheumatology appointments of a small hospital centre.
Material and Methods: The authors developed a retrospective study based on the consult of the clinical process and statistical analysis of the data of the patients with the diagnosis of SSc, followed in Internal Medicine (Autoimmune Diseases) and Rheumatology appointments from 2005-2017.
Results: A total of 30 patients were included. Of these only four were men, the mean actual age was 64,1 years old and the age at diagnosis varied from 21- 83 years old. Six patients died during follow up. The first manifestation of the disease was the Raynaud’s phenomenon in 12 patients. Regarding SSc subtype, it was found that most of these patients had limited cutaneous SSc. Regarding the comorbidities, the most prevalent were: gastrointestinal involvement (10 patients), arterial hypertension (9 patients), pulmonary disease (7 patients), dyslipidemia (6 patients), pulmonary arterial hypertension (5 patients), thyroid disease (5 patients), cancer (4 patients), type 2 diabetes mellitus (4 patients), venous insufficiency (4 patients), Sjögren syndrome (3 patients), osteoporosis (2 patients), scleroderma renal crisis (2 patients) and depression (2 patients).
Conclusions: Although this is a study with a small sample, it was an important tool to be aware of the pathologies that affect this population of patients. The multidisciplinary approach, the education of the patients specially regarding warning signs, the close follow up and the availability of the team are points to achieve better outcomes and to improve the quality of life of the patients with systemic sclerosis.
P.149
High Frequency of Cancer in a Large Brazilian Cohort of Patients with Systemic Sclerosis
P. Sampaio-Barros, A. P. Luppino-Assad, H. Silva, D. Andrade
Division of Rheumatology, University of São Paulo, São Paulo, BRAZIL
Introduction: A higher prevalence of cancer has been described in patients with systemic sclerosis (SSc). The objective of this study is to analyze the frequency of cancer in a large Brazilian cohort of patients with SSc.
Material and Methods: 626 patients classified as SSc according to the ACR/EULAR criteria, attended in a single referral scleroderma outpatient clinic in Brazil between 2010 and 2016 were studied. Patients with a confirmed diagnosis of cancer were evaluated regarding demographic, clinical and laboratory features. Statistical significance was considered when p < 0.05.
Results: 67 SSc patients (10.7%) had a diagnosis of cancer during the follow-up, showing distinct neoplasias: breast-12; skin-12, including basal cell-5, epidermoid-3, melanoma-3 and squamous cell-1; colon, esophagus, lung and thyroid-6 each; uterus-4; lymphoma-3; bladder, stomach and prostate-2 each; adrenal, appendix, liver, ovary, parotid and kidney-1 each. SSc patients with cancer were older (63,75 + 13.40 years vs. 54,33 + 13.91 years; p < 0.001), also presenting higher age at disease onset (47,73 + 14.39 years vs. 41,19 + 13.89 years; p = 0.001), age at diagnosis (50,42 + 14.01 years vs. 43,64 + 14.05 years; p = < 0.001) and disease duration (16,12 + 9.90 years vs. 13,05 + 9.06 years; p = 0.018). They also presented statistical association with limited SSc (p = 0.002), telangiectasias (p = 0.062), Barrett esophagus (p = 0.001), peripheral neuropathy (p = 0.007) and anti-Scl70 antibody (p = 0.065; trend). It was also observed an association with Sjogren syndrome (p = 0.032) and death (p = 0.004). Multivariate logistic regression analysis showed that limited SSc, Barrett esophagus and age at onset were significantly associated with cancer.
Conclusions: Cancer was frequent in this large Brazilian series of SSc patients, specially breast and skin cancer, significantly associated to limited SSc and death.
P.150
The Role of Inflammatory Markers in Assessment of Disease Activity in Systemic Sclerosis
L.J. Ross1,2, W. Stevens2, C. Rabusa2, M. Wilson2, N. Ferdowsi1, J. Walker3, J. Sahhar4,5, G.S. Ngian4,5, J. Zochling6, J. Roddy7, K. Tymms8, G. Major9, G. Strickland2, S. Proudman10,11, M. Nikpour1,2
1 Department of Medicine, The University of Melbourne at St Vincent’s Hospital, Melbourne, AUSTRALIA, 2 Department of Rheumatology, St Vincent’s Hospital, Melbourne, AUSTRALIA, 3 Rheumatology Unit, Flinders Medical Centre, Adelaide, AUSTRALIA, 4 Department of Rheumatology, Monash Health & Monash University, Melbourne, AUSTRALIA, 5 Department of Medicine, Monash Health & Monash University, Melbourne, AUSTRALIA, 6 Department of Rheumatology, Menzies Institute for Medical Research, Hobart, AUSTRALIA, 7 Department of Rheumatology, Fiona Stanley Hospital, Perth, AUSTRALIA, 8 Department of Rheumatology, Canberra Hospital, Canberra, AUSTRALIA, 9 Department of Rheumatology, John Hunter Hospital, Newcastle, AUSTRALIA, 10 Rheumatology Unit, Royal Adelaide Hospital, Adelaide, AUSTRALIA, 11 Discipline of Medicine, University of Adelaide, Adelaide, AUSTRALIA
Introduction: Although the pathogenesis of systemic sclerosis (SSc) is a triad of fibrosis, vasculopathy and inflammation, the role of the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) in measurement of disease activity remains controversial. We evaluated the relationship between clinical features of SSc and raised inflammatory markers to determine if increased ESR and CRP levels correlate with features of disease activity over time.
Material and Methods: Patients enrolled in the Australian Scleroderma Cohort Study (ASCS) who fulfilled 2013 ACR/EULAR criteria for the diagnosis of SSc were included in this study. Generalized estimating equations (GEEs) were used to determine the relationship between ESR 20mm/hr and CRP 5mg/L and features of disease over the duration of the study. The associations between increasing inflammatory markers and change in modified Rodnan Skin Score and respiratory function tests were analysed.
Results: There were 1,545 patients included in this study who were followed for a mean (SD) 3.52±2.91 years and a total of 6,119 study visits. Approximately half of the patients recorded elevated inflammatory markers on at least one occasion.
Overall, there was an association between raised ESR and CRP and fibrotic and vasculopathic manifestations of disease as well as inflammatory disease manifestations. In multivariable analysis, raised ESR was associated with fibrotic lung disease and pulmonary arterial hypertension, indicated by reduced forced vital capacity (FVC) <80% (OR 1.28 p=0.018) and diffusing capacity of the lung (DLCO) <80% (OR 1.47 p<0.001). Proximal muscle strength was inversely correlated with raised ESR (OR 0.68 p=0.001). Respiratory manifestations of disease were also associated with raised CRP; FVC <80% (OR 1.39 p=0.002) and DLCO <80% (OR 1.26 p=0.024), as well as cutaneous and articular manifestations of disease (mRSS >20 OR 2.08 p<0.001 and tendon friction rub OR 2.19 p<0.001).
Of note, there was an inverse correlation between raised ESR and CRP and hypocomplementaemia (ESR OR 0.77 p=0.012; CRP OR 0.77 p=0.019).
Rising inflammatory markers were associated with deteriorating respiratory function tests; a 10% decrease in FVC was associated with a 2-fold increase in both ESR and CRP values (OR 1.60 p=0.032). No association between worsening mRSS and increasing inflammatory markers was found (OR 0.83 p=0.393).
Conclusions: Elevated ESR and CRP are associated with fibrotic and vasculopathic as well as inflammatory manifestations of disease, namely cutaneous, respiratory and musculoskeletal features. This indicates that inflammatory markers have a role in the assessment of SSc disease activity.
P.151
Challenges and Service Preferences of Informal Caregivers of People with Systemic Sclerosis
D.B. Rice1, M. Cañedo-Ayala1, M.E. Carrier1, J. Cumin1, V. Malcarne2, 3, M. Hagedoorn4, B.D. Thombs1,5, 6, S.S.C. Caregiver Committee1
1 Lady Davis Institute for Medical Research, Jewish General Hospital, Department of Psychiatry, Montreal, CANADA, 2 San Diego State University, Department of Psychology, San Diego, USA, 3 Joint Doctoral Program in Clinical Psychology, San Diego, USA, 4 University of Groningen, Department of Psychology, Groningen, THE NETHERLANDS, 5 McGill University, Departments of Psychiatry; Epidemiology, Biostatistics, and Occupational Health; Medicine; Psychology, Montreal, CANADA, 6 McGill University, Department of Educational and Counselling Psychology, Montreal, CANADA
Introduction: Many people living with Systemic Sclerosis (SSc) receive support and care from an informal caregiver. Informal caregivers are family members or friends who provide care and support to a loved one because of a health condition, such as SSc. Caregiving can result in negative consequences such as having to manage additional tasks, work-related stressors, and physical and mental health decline. The most common challenges among caregivers to a loved one with SSc are unknown. The purpose of our study was to determine the (1) challenges most frequently experienced by informal caregivers of people with SSc, and (2) the preferred support services that could be provided to caregivers.
Material and Methods: Current or previous caregivers of people with SSc were eligible to participate in this study. Participants recruited in North America, Europe, and Australia, completed an online questionnaire that was developed from focus group data. The importance of challenges was rated on a scale from 1-4 (1 = not important to 4 = very important). Likelihood of using support services was also rated on a scale from 1-4 (1 = not likely to 4 = very likely).
Results: A total of 202 informal caregivers (79 women (39%)) to people with SSc completed the questionnaire. The average age of respondents was 57.2 (standard deviation [SD] = 14.4), and caregivers were providing support to a partner (72%), parent (12%), child (7%), friend (5%), or sibling (4%). The highest rated challenges that participants rated as being important fell under the categories of emotional difficulties of the care recipient (mean = 3.2, SD = 0.7); changes in relationship dynamics (mean = 3.1; SD = 0.9); and role strain (mean = 3.1; SD = 0.8). Support services that caregivers rated as being most likely to use were (1) a caregiver newsletter (mean = 2.7; SD = 1.0); (2) an online website for caregivers of newly diagnosed patients (mean = 2.7; SD = 1.1); and (3) an information package about SSc for caregivers of newly diagnosed patients (mean = 2.5; SD = 1.1).
Conclusions: Findings suggest that coping with the care-recipient’s emotional difficulties, changes in the relationship dynamics, and role strain are challenges that are important to caregivers to persons with SSc. Further, interventions that are accessible online and provide caregivers with education soon after the SSc diagnosis would be most likely to be used caregivers.
P.152
Nominal Technique Focus Groups to Explore the Challenges and Support Preferences of Informal Caregivers of People with Scleroderma
D.B. Rice1, M. Cañedo-Ayala1, S.T. Gumuchian2, M. Hagedoorn3, V. Malcarne 4, 5, B.D. Thombs 1,2, 6, S.S.C. Caregiver Committee1
1 Lady Davis Institute for Medical Research, Jewish General Hospital, Department of Psychiatry, Montreal, CANADA, 2 McGill University, Department of Education and Counselling, Montreal, CANADA, 3 University Medical Center Groningen, Department of Psychology, Groningen, THE NETHERLANDS, 4 San Diego State University, Department of Psychology, San Diego, USA, 5 Joint Doctoral Program in Clinical Psychology, San Diego, USA, 6 McGill University, Departments of Psychology, Psychiatry, and Medicine, Montreal, CANADA
Introduction: Many people with Systemic Sclerosis (SSc) depend on informal caregivers. Informal caregivers are people who provide unpaid support for a family member or friend with a health condition. Little is known about the experience of informal caregivers of people with SSc. This study explored (1) the challenges experienced by informal caregivers of people with SSc, and (2) their preferences for potential support services.
Material and Methods: Participants were 18 years or older and had provided unpaid support or care for a friend or family member with SSc within the last 12 months. A nominal group technique was used to structure three focus groups that were conducted during SSc patient conferences held in the United States and Canada. Each focus group was conducted by trained moderators and lasted approximately 60-90 minutes. Participants were asked to independently identify a list of key challenges in caregiving and desired support services. Next, each participant stated and explained their list one at a time in a round-robin format. Moderators typed a master list containing all items stated by the participants. This list was then reviewed by the group to remove or merge overlapping items. Once a final list of items was generated, participants independently rated the importance of each challenge from 1 (not at all important) to 10 (very important) and the likelihood of using the generated support services from 1 (not at all likely) to 10 (very likely).
Results: A total of 6 males and 7 females participated in the focus groups. Participants’ mean age was 59.8 years (standard deviation = 12.6). Participants were providing care for a partner (62%), parent (8%), child (15%), or friend (15%). A list of 61 unique challenges was generated. The challenges identified most frequently were related to a lack of information, resources, and support needs. A list of 18 unique support services were also generated by caregivers. The most common support services generated by participants were internet-based and included education about SSc and emotional support.
Conclusions: A variety of challenges were identified by informal caregivers for persons with SSc. Some of the most important challenges identified were related to information, resources, and support needs. Internet-based support services were identified as one of the support services that caregivers would be most likely to use.
P.153
Survival and Prognosis Factors in Systemic Sclerosis : Data of a French Multicenter Cohort of Incident Patients, Systematic Review and Meta-Analysis of the Literature
M.R. Pokeerbux 1,2,3,4, J. Giovannelli 1,2, L. Dauchet5, L. Mouthon6, C. Agard7, J.C. Lega8, Y. Allanore9, P. Jego10, B. Bienvenu11, S. Berthier12, O. Fain13, E. Hachulla1,2,3,4, D. Launay 1,2,3,4
1 Univ. Lille, U995 - LIRIC - Lille Inflammation Research International Center, Lille, FRANCE, 2 INSERM, U995, Lille, FRANCE, 3 CHU Lille, Département de Médecine Interne et Immunologie Clinique, Lille, FRANCE, 4 Centre de Référence des Maladies Autoimmunes et Systémiques Rares du Nord et Nord-Ouest de France (CeRAINO), Lille, FRANCE, 5 CHU Lille, Département Epidémiologie, Lille, FRANCE, 6 Hôpital Cochin-APHP-Service de Médecine Interne, Paris, FRANCE, 7 CHU Nantes, Service de Médecine Interne, Nantes, FRANCE, 8 CHU Lyon Sud, Service de Médecine Interne, Lyon, FRANCE, 9 Hôpital Cochin-APHP-Service de Rhumatologie, Paris, FRANCE, 10 Service de Médecine Interne, CHU Rennes, Rennes, FRANCE, 11 Service de Médecine Interne, CHU Caen, Caen, FRANCE, 12 Service de médecine interne et immunologie clinique, Dijon, FRANCE, 13 Hôpital Saint-Antoine-APHP-Service de Médecine Interne, Paris, FRANCE
Introduction: Several studies have assessed prognosis factors in systemic sclerosis (SSc), but only few have investigated extensive clinical and laboratory factors in a large, incident and well phenotyped population. The aim of the present study was to describe survival, standardized mortality ratio (SMR) and prognostic factors in a well-phenotyped and multicenter French cohort of incident SSc patients. A systematic review and meta-analysis of cohort studies to assess SMR and prognostic factors in SSc was then performed.
Material and Methods: Survival, SMR and prognosis factors were assessed in a cohort of SSc patients followed in five referral centers in France. A systematic review of the literature was carried out in Pubmed up to July 2017. Cohort studies of unselected SSc patients reporting SMR and prognostic factors were included in the analysis. We calculated the pooled summary estimates of SMR and hazard ratios (HR) of prognosis factors.
Results: Out of the 42 referral centers included in the French SSc registry, the present analysis was restricted to 5 centers to ensure the lowest rate of missing data. 625 SSc patients (28.6% of diffuse SSc (dcSSc)) with recent diagnosis were followed from January 2000 to December 2013. Mean age at disease onset was 50.6± 14.5 years and mean follow-up was 5.2±3.6 years. 104 deaths were recorded. Overall survival rates at 1, 3, 5 and 10 years from diagnosis were 98.0%, 92.5%, 85.9% and 71.7% respectively. Overall SMR was 5.73 [95% confidence interval (CI) 4.68-6.94]. Age at diagnosis>60 years, dcSSc, scleroderma renal crisis, severe dyspnoea, FVC<70%, DLCO<70%, pulmonary hypertension (PH), telangiectases, valvular disease, malignancy, anemia, CRP>8mg/l were associated with a poorer survival.
Eighteen articles were included in the SMR meta-analysis, representing a total population of 11,329 patients and 33 studies were included in the prognosis factors meta-analysis, representing a total of 23,520 patients. Pooled SMR was 3.45 [95% CI 3.03 – 3.94]. Age at disease onset, age at diagnosis, male sex, black race, dcSSc subtype, anti-Scl70 autoantibodies, cardiac and renal involvements, interstitial lung disease, PH and malignancy were significantly associated with a worse prognosis. Presence of ACA autoantibodies was associated with a better survival.
Conclusions: Our study confirms a high mortality rate in SSc and previously described prognosis factors related to skin extension, autoantibody status and organ involvement while reporting new association such as telangiectases and valvular disease.
P.154
Reasons for Attending Support Groups and Organizational Preferences: the North American Support Group Survey
M. Pepin1, L. Kwakkenbos1,2,3, S. Pelaez2,4, M.-E. Carrier1, V.L. Malcarne5, S.T. Gumuchian1,2, V.C. Delisle1,2, G. El-Baalbaki6, B.D. Thombs1,2
1 Lady Davis Institute for Medical Research, Jewish General Hospital, Montreal, CANADA, 2 Department of Psychiatry, McGill University, Montreal, CANADA, 3 Behavioural Science Institute, Clinical Psychology, Radboud University, Nijmegen, THE NETHERLANDS, 4 Department of Educational and Counselling Psychology, McGill University, Montreal, CANADA, 5 Department of Psychology, San Diego State University, San Diego, California, USA., San Diego, USA, 6 Department of Psychology, Université du Québec à Montréal, Montreal, CANADA
Introduction: Many people with systemic sclerosis (SSc, or scleroderma) have organized peer-facilitated support groups to share and receive SSc-specific information and support. A recent survey explored reasons people join and continue to attend SSc support groups in Europe and Australia, and three main reasons were identified: (1) interpersonal and social support (e.g., openly talking about my fears and feelings regarding living with scleroderma) (2) disease treatment and symptom management (e.g., learning strategies that may help to reduce or control medication side effects) and (3) other aspects of living with SSc (e.g., learning how to talk with family and friends about my scleroderma). The purpose of the present study was to replicate these previous results in a sample of patients with SSc from North America. If the reasons for attending support groups can be generalized to different SSc samples, we can use this information to build programs to improve support groups for SSc internationally and provide greater access by creating additional support groups.
Material and Methods: A 30-item survey was used to assess reasons for attendance among SSc patients in Canada and the United States. Confirmatory Factor Analysis was performed with Mplus 7 to confirm the three-factors that grouped reasons for SSc support group attendance into themes in the previous European support group members survey: (1) interpersonal and social support (2) disease treatment and symptom management strategies (3) and other aspects of living with SSc.
Results: In total, 171 members (86.6% women) completed the online support group survey. The mean age was 56.3 years, and the mean time since diagnosis was 10.1 years. The 3-factor model showed good fit to the data (χ² [399] = 646.0, P < 0.001, TLI = 0.97, CFI = 0.97, RMSEA = 0.06). On average, respondents rated 21.8 of 30 items (73%) as Important or Very Important reasons for joining or continue to attend. The two items most commonly rated as Important or Very Important were (1) Learning how other group members deal with issues related to scleroderma and (2) Learning about current scleroderma research.
Conclusions: Findings of our study suggest that reasons for attending support groups are similar for patients from Europe, Australia and North America. The result will be used to build programs and to improve SSc support groups, which will be disseminated by the Scleroderma Society of Canada and Scleroderma Foundation in the US, as well as other SSc patient organizations across the globe.
P.155
Impact of Standardized Training on Accuracy of the Modified Rodnan Skin Scoring (MRSS) in Systemic Sclerosis (SSc)
J.W. Park1, G.Y. Ahn2, J.W. Kim3, E.S. Park4, J.H. Kang5, S.H. Chang6, I.A. Choi7, S.J. Yoo8, J.K. Park1, K.C. Shin9, Y.B. Park4, J.B. Jun2, L. Czirják10, Y. Allanore11, M. Matucci-Cerinic12, E.B. Lee1
1 Division of Rheumatology, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, SOUTH KOREA, 2 Department of Rheumatology, Hanyang University Hospital for Rheumatic Diseases, Seoul, SOUTH KOREA, 3 Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, SOUTH KOREA, 4 Division of Rheumatology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, SOUTH KOREA, 5 Division of Rheumatology, Department of Internal Medicine, Chonnam National University Medical School & Hospital, Gwangju, SOUTH KOREA, 6 Division of Rheumatology, Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, SOUTH KOREA, 7 Division of Rheumatology, Department of Internal Medicine, Chungbuk National University Hospital, Chungbuk National Univ, Cheongju, SOUTH KOREA, 8 Division of Rheumatology, Department of Internal Medicine, School of Medicine, Chungnam National University, Chungnam Na, Daejeon, SOUTH KOREA, 9 Division of Rheumatology, Department of Internal Medicine, SNU Boramae Medical Center, Seoul, SOUTH KOREA, 10 Department of Rheumatology and Immunology of Medical Centre, University of Pécs, Pécs, HUNGARY, 11 Paris Descartes University and Cochin Hospital, AP-HP, Paris, FRANCE, 12 Department of Experimental and Clinical Medicine, University of Florence, Florence, Italy; Department of Geriatric Medic, Florence, ITALY
Introduction: In SSc, standardization of mRSS is essential for the success of clinical trials. Only few studies have investigated the effect of standardized education on the accuracy of mRSS in practice.
Material and Methods: 10 rheumatologists (6 professors, 4 fellows) participated to the study. They all received standardized mRSS training program composed of two steps; 1) lecture regarding how to perform a mRSS, 2) live demonstration using one representative patient by master instructor (MMC). Physicians were asked to perform mRSS on 8 patients for three times, one day before the training, after the lecture, and after the live demonstration. Baseline mRSS (Gold standard skin score) was determined by the master instructor before the first skin scoring was performed by physicians. The accuracy of mRSS was estimated by the difference between skin scores measured by each physician during the training course and gold standard skin score. Mixed effect model with random effect for both patients and physicians was used for statistical analysis.
Results: Median (IQR) gold standard skin score of patients was 11.0 (10.0). Before the training course, mean (SD) difference between skin scores measured by each physician and gold standard skin score was estimated at 7.7 (9.5). The difference was numerically decreased after the lecture (β= -1.96 95% CI -3.95 to 0.03) and after the demonstration (β= -1.11 95% CI -3.11 to 0.88) in unadjusted model. Effect of training program on accuracy of skin scoring was more prominent in the clinical fellows than the professors (p < 0.001). In addition, accuracy of mRSS was associated with disease duration (β= 0.85 95% CI 0.43 to 1.28) and baseline skin thickness score (β= -0.72 95% CI -0.93 to -0.51). After adjusting these covariates, difference from gold standard was significantly reduced after the lecture (adjusted β= -5.62 95% CI -10.98 to -1.15). However, live demonstration did not lead to additional enhancement (adjusted β= 1.44 95% CI -1.52 to 4.41). Inter-observer reliabilities of mRSS estimated by intra-class correlation (95% CI) before the training, after the lecture, and after the live demonstration were 0.88 (0.70 to 0.97), 0.63 (0.07 to 0.91) and 0.66 (0.15 to 0.92), respectively, which were not significantly different.
Conclusions: The standardized training program significantly enhanced the accuracy of mRSS. However, the data show that in case of live demonstration, more intense program is still required.
P.156
Prevalence, Severity and Clinical Significance of Pain in Patients with Systemic Sclerosis
P. Ostojic1, N. Djurovic1, B. Stojic1, S. Knezevic-Apostolski2, D. Bartolovic3
1 Institute of Rheumatology, School of Medicine, University of Belgrade, Belgrade, SERBIA, 2 Outpatient neurological clinic - Apostolski, Belgrade, SERBIA, 3 Department of Medical Biochemistry, Clinical Center of Serbia, Belgrade, SERBIA
Introduction: This study aims to assess prevalence, severity and type of pain in patients with systemic sclerosis (SSc), and impact of pain on disease status, depression and quality of life
Material and Methods: 42 consecutive patients with SSc were included in this study. We assessed prevalence and severity of different types of pain (during attacks of Raynaud’s phenomenon, pain caused by ischemic ulcers, odynophagia, arthralgia, headache, back pain, chest pain and neuropathic pain) in our patients. Relationship among different types of pain with disease status, symptoms of depression and quality of life was estimated. Disease status was assessed using the Scleroderma Assessment Questionnaire (SAQ), occurrence of depressive symptoms by the Beck’s Depression Inventory (BDI), whilst quality of life was evaluated using the EQ-5D index. All patients with neuropathic underwent detailed neurological and electroneurography (ENG) examination, as well as HgbA1C and vitamin B12 level testing.
Results: 92.9% of patients reported different types of pain. Arthralgia was the most common type of pain, present in 78.6% of patients, followed by pain during attacks of Raynaud’s phenomenon (69%), back pain (47.6%), headache (31%), chest pain (23.8%), odynophagia (21.4%) and painful ischemic ulcers (19%). Pain caused by ischemic ulcers was reported as most severe (median 8.5 on a 0-10 scale). All types of pain were equally frequent in patients with lSSc and dSSc, but joint pain was more intense (p=0.02) in dSSc (7.6 vs. 5.5). Severity of depression positively correlated with severity of joint pain (p<0.001). Moreover, a significant correlation was noticed only between joint pain and the EQ-5D index (p=0.009). Compared to patients with intermittent pain, patients suffering from chronic pain have a significantly lower mean value of EQ-PD index (0.52 vs 0.79, z=-4.12, p<0,001). Presence of neuropathic pain is associated with more severe SSc, symptoms of depression and worse quality of life. Almost all SSc patients with neuropatic pain (90.9%) have typical symptoms and signs for polyneuropathy. However, in only few of them polyneuropathy could be detected by ENG.
Conclusions: Arthralgia is the most common type of pain in SSc, but pain caused by ischemic ulcers was reported as most severe. Intense joint pain, chronic pain and neuopathic pain are associated with more severe form of the disease, depression and poorer quality of life. Patients with neuropathic pain had typical symptoms and signs for polyneuropathy, but in few of them it was confirmed by ENG, suggesting small-fiber polyneuropathy as cause of neuropathic pain in most of patients.
P.157
Performance of the 2016 Revised Eustar Activity Index for Systemic Sclerosis in a Single-Center Cohort
R. Oneata1, Am. Gheorghiu1, A. Briceag1, A. Radu1, S. Magda2, T. Constantinescu3, R. Jurcut4, A. Soare1, R. Dobrota1, O. Olteanu1, M. Speriatu1, L. Macovei1, M. Milicescu1, M. Sasu1, M. Bojinca1, V. Stoica1, C. Mihai1
1 Spitalul Clinic Dr Cantacuzino, Clinica de Medicina Interna si Reumatologie, UMF Carol Davila, Bucharest, ROMANIA, 2 Spitalul Universitar de Urgenta Bucuresti, Clinica de Cardiologie, UMF Carol Davila, Bucharest, ROMANIA, 3 Institutul de Pneumologie Marius Nasta, UMF Carol Davila, Bucharest, ROMANIA, 4 Institutul de Urgenta pentru Boli Cardiovasculare C.C.Iliescu, UMF Carol Davila, Bucharest, ROMANIA
Introduction: In 2016, the European Scleroderma Trials and Research (EUSTAR) group developed a revised activity index for Systemic Sclerosis (SSc) in order to improve the European Scleroderma Study Group’s (EScSG) 2001 activity index.
Objective: This study aimed to evaluate the performance of the revised EUSTAR 2016 activity index (RAI) in a single-center cohort of patients with SSc.
Material and Methods: The study included all patients with complete data for the RAI, the EScSG 2001 activity score, the Scleroderma Health Assessment Questionnaire (SHAQ) score and physician’s global assessment of the disease on the visual analogue scale (VAS), both at enrolment and at follow-up (at 6-12 months). The associations between scores were assessed using Spearman’s rank correlation coefficient.
Results: Fourty-seven patients were included (males/females 3/44, median age±IQR 53.22±19.48 years, 29/18 with diffuse/limited cutaneous SSc). The median activity score was 1.42±1.84 at enrolment and 1.4±2.83 at follow-up. 14 patients had active disease at both visits. Both RAI and EScSG had stronger correlations with HAQ, SHAQ and VAS at enrolment than at the follow-up visit (see Table 1). RAI index >=2.5 and EScSG >=3 identified active disease as defined by VAS with a moderate sensitivity and a high specificity (see Table 1).
Conclusions: Both the RAI and the EScSG scores correlated moderately with the physician’s global assessment of disease activity and with the functional scores. Sensitivity and specificity were good, with similar performance of the activity scores.
This study is part of QUANTICAP project (PN-II-PT-PCCA-2013-4-1589, contract - UEFISCDI 188/2014).
P.158
Determinants of Health-Related Quality of Life in a Multinational Systemic Sclerosis Inception Cohort
K. Morrisroe1, M. Hudson2, M. Baron2, J.K. De Vries-Bouwstra3, P.E. Carreira4, D.M. Wuttge5, M. Wang2, T. Frech6, W. Stevens7, S. Proudman8, M. Nikpour1, Insync9
1 University of Melbourne at St Vincent’s Hospital Melbourne - Department of Medicine, Melbourne, AUSTRALIA, 2 Jewish General Hospital - Lady David Research Institute - Division of Rheumatology, Montreal, CANADA, 3 Leiden University Medical Centre - Department of Rheumatology, Leiden, THE NETHERLANDS, 4 Hospital Universitario 12 de Octubre - Department of Rheumatology, Madrid, SPAIN, 5 Lund University and Skåne University Hospital - Department of Clinical Sciences - Section of Rheumatology, Lund, SWEDEN, 6 University of Utah - Department of Internal Medicine - Division of Rheumatology, Salt Lake City, USA, 7 St Vincent’s Hospital Melbourne - Department of Rheumatology, Melbourne, AUSTRALIA, 8 Royal Adelaide Hospital - Department of Rheumatology, Adelaide, AUSTRALIA, 9 The International Systemic Sclerosis Inception Cohort (INSYNC) collaboration
Introduction: Health related quality of life (HRQoL) is known to be severely affected by systemic sclerosis (SSc) but it is not known how early in the disease this occurs. Our aim was to evaluate health related quality of life (HRQoL) and its determinants in a multinational inception cohort. We also wished to determine if we could study this issue with pooled individual data from multiple countries rather than a meta-analysis of data.
Material and Methods: SSc patients within 2 years of disease onset were recruited from 5 countries participating in the International Systemic Sclerosis Inception Cohort (INSYNC). Data from each country’s database were exported for analysis using a harmonized platform. HRQoL was assessed using the Medical Outcomes Short Form-36 (SF-36). Multivariable linear regression assessed associations between HRQoL and determinants in cohorts separately and meta-analysis generated pooled estimates. The analyses were repeated using individual patient data.
Results: Of the 637 SSc patients recruited, the majority were female (80.2%-83.3%), aged between 52.4-56.7 years with limited cutaneous disease subtype (48.6%-66.7%). HRQoL scores were lower for SSc patients than the general population (SF-36 physical component summary (PCS) score (36.4-39.6), mental component summary (MCS) score (41.0-46.4)). Determinants of SF-36 PCS by meta-analysis included increasing age (β=-0.1, 95%CI -0.2, -0.01), diffuse cutaneous disease subtype (β=-8.4, 95%CI -10.6, -6.3), and pulmonary arterial hypertension (β=-10.9, 95%CI -16.6, -5.3). Increasing age (β=0.09, 95%CI 0.0, 0.18) was the only variable associated with SF-36 MCS. Analyses using individual patient data revealed similar results to those of the meta-analysis of cohort data.
Conclusions: Our study shows that HRQoL is markedly decreased in early SSc and also shows that pooled individual patient data analysis is valid in the INSYNC dataset.
P.159
Quantifying the Burden of Systemic Sclerosis: a Data Linkage Study
K. Morrisroe1, W. Stevens2, J. Sahhar3, G-S. Ngian3, C. Rabusa2, N. Ferdowsi2, S. Proudman4, M. Nikpour1
1 University of Melbourne at St Vincent’s Hospital Melbourne - Department of Medicine, Melbourne, AUSTRALIA, 2 St Vincent’s Hospital Melbourne - Department of Rheumatology, Melbourne, AUSTRALIA, 3 Monash Medical Centre - Department of Rheumatology, Melbourne, AUSTRALIA, 4 Royal Adelaide Hospital - Department of Rheumatology, Adelaide, AUSTRALIA
Introduction: Systemic sclerosis (SSc) is an incurable multi-organ autoimmune disease with substantial morbidity and mortality. Due to varied clinical manifestations, patients with SSc are usually on multiple medications and require frequent hospitalization and consultation with specialists and allied health from a broad range of disciplines. We hypothesize that the cost of healthcare in SSc is substantial, and sought to quantify this health service utilization and associated cost among Australian SSc patients.
Material and Methods: Health service use was captured by means of data linkage. Data for all Victorian SSc patients enrolled in the Australian Scleroderma Cohort Study (ASCS) (n=531) between 2011-2015 were linked with the Victorian hospital admissions and emergency presentations data sets and the Medicare Benefits Schedule (MBS), which contains all government subsidized ambulatory care services. Hospitalization cost was calculated based on the financial year of admission, admission diagnosis, length of stay and the corresponding value of each admission unit for that financial year. Ambulatory care cost was based on the MBS fee payable by the Australian government for each service, and medication cost was estimated from the Pharmaceutical Benefits Scheme (PBS). Cost was extrapolated to all Australian SSc patients based on SSc prevalence (21.1 per 100,000) and population data (Australian population 24,304,682 in 2015).
Results: Total health service utilization cost to the Australian government extrapolated to all Australian SSc patients between 2011-2015 amounted to AUD$298,065,737.15 (USD$219,376,382.55), which is an average annual cost of AUD$59,613,147.43 (USD$43,875,276.51) and annual cost per patient of AUD$11,622.76 (USD$8,554.35). Hospital costs, including inpatient hospitalization and emergency department presentations, accounted for the majority (44.5%) of these costs, followed by medication cost (31.1%) and ambulatory care cost (24.4%). Determinants of hospitalization included older age at SSc onset (OR 1.02, p=0.05), pulmonary arterial hypertension (PAH) (OR 2.1, p=0.02), digital ulcers (OR 1.6, p=0.04), gastrointestinal involvement (OR 1.7, p=0.01), hand dysfunction (OR 1.7, p=0.01) and stroke (OR 2.7, p=0.03).
Conclusions: Our study provides the most comprehensive assessment of healthcare utilization and its determinants in SSc to date, and highlights the substantial direct cost of this disease despite its low prevalence. Linkage of clinical and administrative data sets allows the collection of information regarding direct costs of healthcare use in SSc without recall bias. These findings can be used to guide resource allocation and the development of tailored policies to improve patient outcomes.
P.160
Characteristic Clinical Features of Patients from Korean Cohort of Systemic Sclerosis
K.W. Moon1, S.S. Lee2, Y.J. Lee3, J.B. Jun4, S.W. Kang5, J.H. Ju6, S.H. Chang7, I.A. Choi8, Ty. Kang9, Y.B. Park10, E.B. Lee11, S.G. Lee12
1 Division of Rheumatology, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, SOUTH KOREA, 2 Department of Rheumatology, Chonnam National University Medical School, Gwanagju, SOUTH KOREA, 3 Division of Rheumatology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, SOUTH KOREA, 4 Department of Rheumatology, Hanyang University Hospital for Rheumatic Diseases, Seoul, SOUTH KOREA, 5 Rheumatology, Department of Internal Medicine, School of Medicine, Chungnam National University, Chungnam National Unive, Daejeon, SOUTH KOREA, 6 Division of Rheumatology, Department of Internal Medicine, Seoul St. Mary’s Hospital, Institute of Medical Science, Coll, Seoul, SOUTH KOREA, 7 Division of Rheumatology, Department of Internal Medicine, Soonchunhyang University College of Medicine Hospital, Cheonan, SOUTH KOREA, 8 Division of Rheumatology, Department of Internal Medicine, Chungbuk National University Hospital, Chungbuk National Univ, Cheongju, SOUTH KOREA, 9 Department of Rheumatology, Yonsei Univeristy Wonju College of Medicine, Wonju, SOUTH KOREA, 10 Division of Rheumatology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, SOUTH KOREA, 11 Division of Rheumatology, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, SOUTH KOREA, 12 Division of Rheumatology, Department of Internal Medicine, Pusan National University, Pusan, SOUTH KOREA
Introduction: Systemic sclerosis (SSc) is a connective tissue disease of unknown etiology and characterized by fibrosis of the skin and internal organ. Clinical characteristics of the SSc patients are different depending on the ethnic groups. Recently, Korean SSc cohort was initiated. The aim of this study was to investigate demographic, clinical and laboratory characteristics of Korean patients with SSc depending on the extent of skin involvement.
Material and Methods: A total of 751 Korean patients with SSc from 12 representative centers from South Korea were enrolled to evaluate demographic and clinical features, laboratory data, and internal organ involvement. The data were obtained from medical record review based on the predefined criteria. Clinical and laboratory characteristics were compared between diffuse (dcSSc) and limited cutaneous subsets (lcSSc).
Results: Clinical and laboratory characteristics of patients with SSc were summarized in table 1. Six hundred fifty one patietns (86.7%)s were women, mean age was 48.9 ± 13.3 years. Two hundreds sixty four patients (35.2%) were belonged to dcSSc, and 487 (64.8%) patients belonged to lcSSc. The most commonly involved organ was lung (Interstitial Lung Disease, ILD). In compared to patients with lcSSc, patients with dcSSc had younger age, lower BMI, earlier symptom onset, higher modified Rodnan skin score, longer follow-up duration, lower FVC, FEV1, and DLCO level. The prevalence of pulmonary arterial hypertension was similar between dcSSc and lcSSc groups. Gastroesophageal reflux disease, ILD, cardiovascular involvement, renal crisis, and death rate were significantly more observed in dcSSc than lcSSc. There were 46 (6.1%) cases of cancers and lung cancer was most prevalent.
Conclusions: In Korean SSc patients, the most commonly observed internal organ manifestation is interstitial lung disease. Unlike Caucasian population, the prevalence of pulmonary arterial hypertension is similar between dcSSc and lcSSc population.
P.161
Modified Rodnan Skin Score (MRSS) Teaching in a High Number of Students: Results from the Eustar Course
M. Radic1, T. Minier2, I. Bozic1, M. Petric1, P. Airo3, N. Damjanov4, O. Kowal-Bielecka5, O. Distler6, E.J. Kucharz7, S. Novak8, A. Vacca9, Y. Allanore10, M. Matucci-Cerinic11, L. Czirják2, D. Martinovic Kaliterna1
1 University of Split School of Medicine, Division of Rheumatology and Clinical Immunology, Split, CROATIA, 2 University of Pecs, Department of Rheumatology and Immunology, Pecs, HUNGARY, 3 Spedali Civili of Brescia, Rheumatology and Clinical Immunology, Brescia, ITALY, 4 Institute of Rheumatology, Belgrade, SERBIA, 5 Medical University of Bialystok, Department of Rheumatology and Internal Medicine, Bialystok, POLAND, 6 University Hospital Zürich, Department of Rheumatology, Zürich, SWITZERLAND, 7 Medical University of Silesia, Department of Internal Medicine and Rheumatology, Katowice, POLAND, 8 KBC Rijeka, Dep. of Rheumatology and Clinical Immunology, Internal medicine, Rijeka, CROATIA, 9 II Chair of Rheumatology, University of Cagliari-Policlinico Universitario, Monserrato, ITALY, 10 Paris Descartes University, Rheumatology A department, Paris, FRANCE, 11 University of Florence, Department of Medicine, Section of Rheumatology, Florence, ITALY
Introduction: Teaching of mRSS is very important in randomised clinical trials (RCTs) to assure a correct evaluation of SSc patients. During the EUSTAR Educational Course in Split, Croatia in 2017, students from all over Europe participated in a mRSS teaching course. Aim: to teach young rheumatologists to measure mRSS in everyday clinical practice and for RCTs.
Material and Methods: A lecture on mRSS scoring technique was given by one of the master teachers (LC) for all students, followed by a video presentation on mRSS scoring (YA). Each patient was also assessed by one master teacher and this score was considered as ‘gold standard’. Students were randomly split into 12 groups. Seven groups were considered as ’intensive’ training groups and were assigned to 7 master teachers; five groups were considered as ’minimal’ training groups and were assigned to five rheumatologists experienced in mRSS scoring. Students in the ’intensive’ groups participated in a bed-side demonstration of mRSS scoring lead by an expert teacher lasting approximately 20-30 minutes. Afterwards, each student assessed 3-4 patients. Some students assessed mainly patients with limited skin involvement (lSSc) (n=5).
Results: Altogether 42-49 students assessed the 6 diffuse cutaneous SSc (dSSc) patients. The within patient standard deviation (SD) was 6.2 points, the coefficient of variation (CV) was 33% for the whole group. For the ‘intensive” training group CV was 35%, within patient SD was 6.6 points, and for the ‘minimal’ training group CV was 32%, the within patient SD was 5.9 points. In average, 43% of students assessing the dSSc patients have measured in the same range, as did the master teacher (difference of equal to or less than 5 points in the mRSS compared to the ‘gold standard’ value). There was no significant difference between the ‘intensive’ and ‘minimal’ training group in this aspect either (~50% vs. ~41%). Five patients with lSSc were also assessed by 8-17 students. ~20% of the students scored at least once a mRSS of 14 or higher indicating that 1/5 of the lSSc cases might be misclassified into the dcSSc subset in the daily practice.
Conclusions: Moreover, the problem of a correct performance of the mRSS needs to be addressed in order to avoid misclassifying patients with limited skin involvement in particular in RCTs.
P.162
Prevalence, Risk Factors and Assessment of Depressive Symptoms in Patients with Systemic Sclerosis
C. March1, D. Huscher2, E. Preis1, A. Makowka1, F. Buttgereit1, G. Riemekasten3, K. Norman4, E. Siegert1
1 Department of Rheumatology and clinical Immunology, Charité-Universitätsmedizin, Berlin, GERMANY, 2 Deutsches Rheuma-Forschungszentrum, Berlin, GERMANY, 3 Department of Rheumatology, Universitaetsklinium, Luebeck, GERMANY, 4 Research Group on Geriatrics, Charité-Universitaetsmedizin, Berlin, GERMANY
Introduction: This study evaluates the prevalence of depressive symptoms among Systemic Sclerosis (SSc) patients using the Major Depression Inventory (MDI). In a second step it identifies possible risk factors and analyses the current standard of care in order to raise awareness and improve clinical care for SSc patients.
Material and Methods: 94 SSc patients, 82 (87%) women and 12 (13%) men, were recruited for this study. They completed the MDI, Short Form 36 Health Survey (SF-36®), Scleroderma Health Assessment Questionnaire (SHAQ), Brief Fatigue Inventory (BFI) and Physical Activity Questionnaire (IPAQ). Clinical parameters were assessed according to standardised procedures. Discharge letters and a questionnaire for physicians were analysed for evaluation of depressive symptoms.
Results: Our cohort is representative for SSc patients as it reflects the skewed proportion between women and men, as well as the proportions of patients with limited or diffuse cutaneous SSc and age profile. The prevalence of depressive symptoms was 22.3%. It correlated with female sex (p = 0.047), underweight (p = 0.002), fatigue (p < 0.001), decreased quality of life (p < 0.001) and less physical activity (p = 0.048). The latter three were confirmed as independent risk factors in a multivariable regression analysis. The analysis of the current standard of care revealed no assessment of depressive symptoms in the majority of patients (89.4%), including 19 patients presenting with depressive symptoms according to the MDI score. The questionnaire for physicians revealed a lack of clinical routine in evaluating mental health issues, as well as re-evaluation.
Conclusions: This study confirms the high prevalence of depressive symptoms in SSc. There is an unmet need of a regular assessment of mental health during SSc consultations. Fatigue, decreased quality of life and reduced physical activity were ascertained as independent risk factors, but special attention should also be paid to weight loss and underweight.
P.163
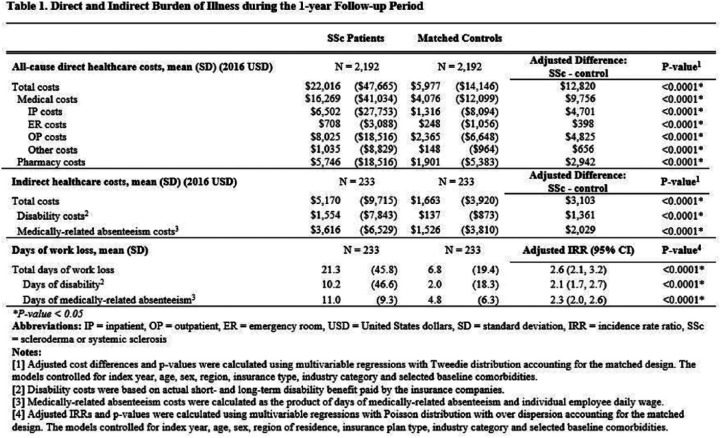
Burden of Illness of Systemic Sclerosis Among Commercially Insured Patients
Z. Zhou1, Y. Yu2, W. Tang1, X. Liu1, Z. Zhou1, D. Macaulay1, A. Fischer3
1 Analysis Group, Inc., Boston, MA, USA, 2 Boehringer Ingelheim Pharmaceuticals, Inc, Ridgefield, CT, USA, 3 University of Colorado School of Medicine, Denver, CO, USA
Introduction: Systemic sclerosis (SSc) is a rare autoimmune disease characterized by varying degrees of organ fibrosis and vasculopathy. There are limited data on burden of SSc in the United States (US). The present study aimed to quantify the economic burdens among patients diagnosed with SSc in the US.
Material and Methods: Data from a large de-identified, privately insured US claims database, including work loss from a subset of companies, were used. Adult patients were selected if they had >=1 inpatient (IP) or emergency room (ER) visit with an SSc diagnosis or >=2 SSc diagnoses in other settings between 1/1/2005 and 3/31/2015. The first SSc diagnosis date was defined as the index date. SSc patients were continuously enrolled for >=6 months before (baseline) and >=12 months after the index date (follow-up). SSc patients were matched 1:1 to controls who had no diagnosis of SSc in their claims history on index date, age, sex, region, insurance plan type, and work loss data availability. All-cause healthcare resource use (HRU), direct costs, work loss days, and indirect costs during the follow-up were estimated and compared between SSc patients and matched controls. Multivariable regressions were used to adjust for baseline covariates including index year, age, sex, region, insurance plan type, industry and selected baseline comorbidities.
Results: The study included 2,192 pairs of SSc patients and matched controls; 233 pairs had available work loss data. The mean age was 57.6 years old (SD = 13.8); the majority were female (84.3%). After adjusting for baseline covariates, SSc patients had more annual IP admissions (adjusted [adj.] incidence rate ratio [IRR] = 2.4), outpatient visits (adj. IRR = 2.3), and ER visits (adj. IRR = 2.0) (all p<0.0001), compared to controls. SSc patients also incurred higher annual total direct costs (adj. difference = $12,820), compared to controls, driven by medical costs (adj. difference = $9,756) and pharmacy costs (adj. difference = $2,942) (all p<0.0001). For the work loss analysis, SSc patients had longer annual total work loss days (21.3 vs. 6.8 days, adj. IRR = 2.6) and higher annual total indirect costs (adj. difference = $3,103) than controls (both p<0.0001).
Conclusions: This study demonstrated the substantial economic burden of SSc including increased HRU, work loss days, and direct and indirect costs, compared to those without SSc. This significant burden underscores the need for more effective treatments for SSc to improve disease management and reduce burden of illness.
P.164
Important Topics Not Discussed During Systemic Sclerosis Consultations: Impact on Patients and Caregivers
C.P. Denton1, B. Laird2, L. Moros3, J.L. Luna Flores3
1 UCL; Centre for Rheumatology, Royal Free Hospital, London, UNITED KINGDOM, 2 Reframe Ltd, Hove, UNITED KINGDOM, 3 Boehringer Ingelheim, Ingelheim, GERMANY
Introduction: For patients with systemic sclerosis (SSc), the course of disease can be unpredictable and the treatment choices can be complex. This can be challenging to understand and explain. As a result, it is often difficult for patients and caregivers to get a clear understanding of the condition, treatment options and likely outcomes. Physicians and nurses may be unsure about how much a patient wants to know, what their particular issues or concerns may be, and how best to explain concepts without using complex medical terms. This is especially an issue with SSc-associated organ involvement, such as SSc-associated interstitial lung disease (SSc-ILD). This study explored the information and communication needs of patients with SSc-ILD and their caregivers, and how these needs could be addressed.
Material and Methods: Qualitative research was conducted across 5 countries with 42 physicians who treated patients with SSc (rheumatologists, pulmonologists, internal medicine specialists, dermatologists), 21 patients diagnosed with SSc-ILD, 16 specialist nurses, and 5 caregivers. Individual in-depth interviews and observed conversations between pairs of patients, doctors, and nurses discussing their experiences of SSc-ILD were audio recorded, transcribed and analysed using linguistic techniques.
Results: Healthcare professionals, patients, and their caregivers were most likely to refrain from talking about the patient’s prognosis, especially with regard to whether and when the patient might die. Patients and caregivers were often afraid or unsure how to ask, while physicians did not mention it for fear of causing distress. In addition, particularly early on in the condition, physicians usually do not have enough information to answer this question. Other key questions from patients were about relationships, family, and work, but they often felt that their physician was not the right person to ask. Nurses were available and willing to talk about these topics, but often said they did not feel informed or knowledgeable enough to answer the questions fully. As a result, topics of key importance to patients and their caregivers are rarely openly discussed, creating an uncertainty about their future and leaving patients less equipped to manage their disease.
Conclusions: By proactively raising these difficult but important topics, physicians and nurses could help patients and caregivers better manage and plan their lives with SSc. This study shows that a multi-professional, team based approach, is likely to give better communication outcomes and address patient’s needs and priorities.
P.165
Challenges in Physician-Patient Communication Limit Patient Understanding and Support in Systemic Sclerosis with Interstitial Lung Disease (SSc-ILD)
C.P. Denton1, B. Laird2, L. Moros3, J.L. Luna Flores3
1 University College London, Centre for Rheumatology, Royal Free Hospital, London, UNITED KINGDOM, 2 Reframe Ltd, Hove, UNITED KINGDOM, 3 Boehringer Ingelheim, Ingelheim, GERMANY
Introduction: Systemic sclerosis (SSc) is a complex and rare condition. This can make it difficult for physicians to explain to patients about their prognosis and treatment options without using complicated medical terms. As a result, patients may not understand what is happening to their bodies, and can feel uncertain about their future or the best choice of treatment options for them. This study observed how physicians and patients with SSc-associated interstitial lung disease (SSc-ILD) communicate with each other. We assessed the language they use, how well they understand one another, and whether both parties give and receive the information they need from the consultation.
Material and Methods: Twenty-three consultations between physicians (rheumatologists, pulmonologists) and patients (19 real, 4 actors) across 5 countries were directly observed and recorded (audio or video). The patients had diagnosed SSc-ILD, either limited or diffuse, of varying severity. In some patients, their SSc was affecting other internal organs in addition to their lungs. None of the study participants were known to one another. Consultations were analysed using linguistic techniques.
Results: There were three key issues that prevented physicians and patients from communicating well with one another.
The language used (plain language or medical terms) was important. Physicians typically tried to use plain language to describe complex concepts, but often started using medical terms when the description became more complicated. In many cases, patients used medical terms without fully understanding them, so the physician incorrectly assumed the patient knew more than they actually did.
The amount of information shared, and the rapport built up between patient and physician, depended on what information the physician focused on during the consultation and whether the patient had enough opportunity to tell their story. Communication was better when the patient was able to tell their story but was guided by the physician, who collected the required information along the way.
The different ways in which patients and physicians were thinking about SSc-ILD affected what information patients shared, and how they interpreted what the physician was saying.
Conclusions: During consultations with patients with SSc-ILD, these three key issues limit bidirectional understanding of the condition and the patient experience. They could mean that both parties miss important information that would help them identify issues and manage the condition more effectively, including self-help management approaches. Strategies should be developed with physicians to facilitate effective communication and increase patient understanding and support.
P.166
The Assessment of Exposure to Inorganic Particles: Implementing the Same Questionnaire in a Nation-Wide Survey (N=2739) and on a Specific Sample of Ssc Patients from a Regional Referral Center
C. Cavalin 1,2,3, A. Lescoat 4,5, A. Ballerie4, O. Macchi6, M. Catinon7, C. Chemarin7, M. Vincent7, PA. Rosental 1,8, P. Jégo 4,5
1 Centre d’ Etudes Européennes de Sciences Po, Paris, FRANCE, 2 Laboratoire Interdisciplinaire d’ Evaluation des Politiques Publiques, Paris, FRANCE, 3 Centre Etudes d’ Emploi et du Travail, Noisy-le-Grand, FRANCE, 4 Department of Internal Medicine, CHU Rennes, University of Rennes 1, Rennes, FRANCE, 5 INSERM, U1085, Research Institute in Health, Environment and Occupation / IRSET, Rennes, FRANCE, 6 Centre de Recherches Historiques; EHESS, Paris, FRANCE, 7 Laboratoire MINAPATH, Lyon, FRANCE, 8 Institut National d’ Etudes Démographiques, Paris, FRANCE
Introduction: In 1957, Erasmus suggested that the inhalation of crystalline silica particles might constitute a risk factor for developing SSc. Since then, many case-control and cohort studies have confirmed the association of silica exposure with SSc and the relevance of the Erasmus’ syndrome. However, occupational exposures to crystalline silica keep being under-estimated in SSc patients, not to mention the invisibility of non-occupational exposures (e.g. do-it-yourself, scouring powder use).
Material and Methods: The SILICOSIS project has developed a specific questionnaire through a multidisciplinary approach (social sciences, statistics and medicine). The objective is to correlate occupational and non-occupational exposures to inorganic particles, and the onset and symptomatology of diverse pathologies, on the whole life course.
1/ This questionnaire was tested twice in the general population in France (n=825; n=2739; respondents sampled in the French rolling census), in the ELIPSSilice 1 and 2 surveys, aiming to produce an unprecedented statistical framing for the prevalence of exposure to inorganic particles. Respondents were asked about several systemic and autoimmune diseases (e.g. SSc, systemic lupus, rheumatoid arthritis).
2/ This questionnaire was tested on a specific population of diagnosed SSc patients (n=68) in a referral center. The association of silica exposure with the main clinical manifestations of the disease was evaluated. The ELIPSSilice samples were used to sample up to 4 controls for each SSc patient (matched on sex, age and tobacco use), in order to build a case-control study.
Results: 1/ In ELIPSSilice1, exposure scores were significantly higher for self-reported ill people (n=187) than for self-declared healthy people (n=638) (Wilcoxon’s test= 67672.5, p-value = 0.005099). The part played by occupational (rather than non-occupational) exposures was also heavier in self-declared ill people. Analogous results will be presented on the ELIPSSilice2 respondents (n=2739), matched with the SSc patients.
2/Considering SSc patients, only occupational exposures were associated with clinical characteristics: farm working, stone carving or building operations were specially associated with diffuse SSc and interstitial lung disease (univariate analysis : respectively OR=4.43 (1.41-13.93) and OR=3.14 (1.08-9.15)). After adjustment on sex, age and tobacco use, diffuse SSc was still significantly associated with occupational exposure to silica dust (p=0.01).
Conclusions: The SILICOSIS questionnaire addresses the lack of occupational and environmental data that prevents medical staff from assessing the etiology of several diseases such as SSc. The SILICOSIS questionnaire may be relevant in assisting clinical practice to screen all exposures to inorganic particles, and a useful epidemiological tool to explore environmental factors of diseases of unknown etiology.
P.167
Health Status and Quality of Life of Patients with Systemic Sclerosis in 2017
M. Lacoste, S. Palat, K. Ly, G. Gondran, E. Liozon, E. Le Coustumier, H. Bezanahary, A. Fauchais
University Hospital, Limoges, FRANCE
Introduction: Systemic sclerosis (Ssc) is a rare and incurable disease with life-threatening and disabling complications. The organ involvement exists very early in the evolution of the Ssc, even without skin involvement. The aim of this study was to describe the physical and psychological health status of patients with Ssc in a French Internal Medicine department.
Material and Methods: We performed a retrospective study of patients diagnosed between 2000 and 2016. The social, clinical, para-clinical characteristics and the health-related quality of life (HRQoL) scales were analyzed according to the level of skin involvement and the presence of a severe organ involvement.
Results: One hundred and four patients were included. The 2013 ACR/EULAR criteria were met for 87 patients. Four very early forms known as Red Flag have been identified. The criterion puffy fingers was missing for 13 false negatives. More than three-quarters of the patients were workers or employees (77%). An occupational exposure was found in 34% of our sample, especially silica (12%). These occupational exposures were more frequently found in diffuse cutaneous Ssc (dcSsc) (p=0.012). Twenty-four patients had dcSsc and 33 patients had severe organ involvement (cardiac, pulmonary and/or renal involvement). There was a higher proportion of severe organ involvement in the dcSsc (16/24 vs 17/80, p < 0.0001). Twenty-one percent of the patients had a TLCO < or = 55% and the TLCO/VA ratio was correlated with severe organ involvement (p=0.004). There was a significant alteration in the six-minute walk distance (6MWD) when patients had severe organ involvement (498 m +/- 72 vs 407 m +/- 171, p=0.012). Anti-Scl-70 antibodies were more frequent in patients with severe organ involvement (p < 0.0001). The presence of avascular areas at nailfold capillaroscopy was correlated with digital ulcers (active or past) (p=0.016) and the two main fatal complications of Ssc: Pulmonary Arterial Hypertension (PAH) (p=0.014) and interstitial lung disease (p=0.035). In our study, the association between the presence of digital ulcers and pathological manometry was present (p=0.0217). The overall disability (sHAQ) was correlated with the severity of the disease (p=0.003). Anxiety (assessed by the HAD anxiety/depression scale) and lower resilience (CD-RISC) were more pronounced in the dcSsc, respectively (p=0.005) and (p=0.028). Alexithymia (TAS-20) was also more impaired in this group (p=0.04).
Conclusions: Early detection of complications by non-invasive examinations (such as nailfold capillaroscopy, plethysmography coupled with 6MWD) as well as socio-occupational care, assessment of overall disability and HRQoL are part of the overall management of scleroderma patients.
P.168
The Course of Mouth Opening and Its Relationship with Disease Characteristics, Global Functioning, Quality of Life and Mouth Handicap in Systemic Sclerosis
S.J.H. Khidir, M. Boonstra, G.W.M. Boerrigter, E.M. Voogt-van der Harst, S.A. Bergstra, N. Ajmone Marsan, M.K. Ninaber, T.W.J. Huizinga, J.K. de Vries-Bouwstra
Leiden University Medical Center, Leiden, THE NETHERLANDS
Introduction: Cross-sectional research showed that reduced maximal mouth opening (MMO) in Systemic Sclerosis (SSc) correlated with higher disease severity and lower oral quality of life. However, the natural history of MMO in SSc is not well described. Our objectives were to evaluate in SSc patients 1) the course of MMO, 2) disease characteristics predictive for decreasing MMO and 3) the relationship between the course of MMO and global functioning, quality of life and mouth handicap.
Material and Methods: SSc patients were included from the Leiden Combined Care In Systemic Sclerosis (CCISS) cohort. Annual follow-up includes measurement of MMO, assessment of global functioning (Health Assessment Questionnaire; HAQ), quality of life (Short Form-36; SF-36) and mouth handicap (Mouth Handicap in Systemic Sclerosis scale; MHISS). We assessed mean MMO, prevalence of microstomia (MMO<30.00 mm) and decreasing MMO (decline >5.00 mm/year) over time. Predictors for decreasing MMO over time were determined by a linear mixed model, including gender, body mass index, age and baseline clinical parameters reflecting organ involvement. Additionally, the relation between HAQ, SF-36, MHISS and longitudinal MMO was analysed.
Results: We included 382 patients, mean age 54±14 years, 83% female, 25% diffuse cutaneous SSc (dcSSc). The median follow-up was 2.0 years (IQR 0.0-3.0). Mean MMO during six years follow-up ranged from 40.18-42.45 mm. Over time the mean percentage of patients with microstomia was stable (mean 9%, range 6-12%). Decreasing MMO between two consecutive annual measurements was observed in 5-17% (mean 10%) of patients at each time point. Baseline disease characteristics predictive for decreasing MMO over time were: more extended cutaneous involvement (dcSSc [B= -4.08, 95%CI= -6.83 to -1.32)], limited cutaneous SSc [B= -2.15, 95%CI= -4.17 to -0.12]), presence of peripheral vasculopathy (B= -2.29, 95%CI= -3.78 to -0.80), pulmonary involvement (B= -1.77, 95%CI= -3.39 to -0.15) and gastrointestinal involvement (B= -2.65, 95%CI= -4.14 to -1.15). Baseline HAQ (B= -1.64, 95%CI= -2.68 to -0.59), SF-36 physical component (B= 0.08, 95%CI= 0.01 to 0.14) and MHISS (B= -0.15, 95%CI= -0.24 to -0.06) correlated significantly with longitudinal MMO.
Conclusions: Over time, mouth opening is relatively stable in the majority of SSc patients. Microstomia is seen in 9% and decreasing MMO in 10% of patients, and is associated with more severe disease including pulmonary and gastrointestinal involvement. As decreasing mouth opening correlates with lower global functioning and quality of life, there is need for treatment strategies specifically targeting mouth opening in SSc.
P.169
Scleroderma Cohort in Abu Dhabi
M. Al Maini, A. Las Alas, R. Aneja, T. Khan, N. Ibrahim, H. Al Mashari, S. Gonuguntla, K. Khawaja
Al-Mafraq Hospital, Abu Dhabi, UNITED ARAB EMIRATES
Introduction: Systemic sclerosis (scleroderma, SSC) is a complex and life threatening autoimmune disease associated with multiple co-morbidities. No data available on the SSC patients living in Abu Dhabi in the United Arab Emirates. Our objective is to describe the cohort of SSC in Abu Dhabi which is the capital city of the United Arab Emirates (UAE).
Material and Methods: Scleroderma identified according to ACR EULAR criteria and identified through the hospital electronic medical records system, which was implemented from January 2011 for medical documentation in all public hospitals in Abu- Dhabi and districts. Patients identified from 1st of January 2011 to 31 of June 2017. Retrospective review of electronic medical records and paper case notes was performed on all patients with the diagnosis of scleroderma who presented during this period.
Results: Total of 49 patients (range 3-75 years). Out of these ten were below 16 years of age. Male 30.6% (n-15) female 69.4% (n-34).
The native patients from the United Arab were 36.5% (n-18). Other Arab countries 49% (n-24) and 14.4 % (n-7) of other nationalities. Diffuse scleroderma 32.7% (n-16), Limited 49% (n-24), 12.2% (n-6) mixed or overlap syndrome and 6% (n-3) unspecified Scleroderma. Skin thickening of the fingers of both hands extending proximal to MCP joints in 77.55% (n-38) and Sclerodactyly/Puffy fingers in 51% (n-25). Digital ulceration 30.6% (n-21). Telangectasia and abnormal nail folds capillaroscopy in 4% (n-4). Reynaud’s phenomenon in 65.3% (n-32). Interstitial lung disease 34.7% (n-17). Pulmonary hypertension in 3 patients of the mixed and unspecified scleroderma patients. Joint synovitis in 18.4 % (n-9). Restrictions of joint function 59 % (n-29). Arthralgia 59% (n-29). Muscle weakness 30.6% (n-15). Dysphagia 38.7 % (n-19). Gastro esophageal reflux 47% (n-23) and significant weight loss 14.3% (n-7). Family history of autoimmune conditions 22% (n-11). Two patients deceased.
Conclusions: Our patients are of multiethnic background and of generally younger age group compared to western data. Raynaud’s phenomenon present in 65.3% of our patients despite warm climate.
P.170
Can Novel Autoantibody Profiling Predict Disease Manifestations in an Inception Cohort of Systemic Sclerosis Patients?
B. Kersten, R.L. Smeets, F.H.J. Van Den Hoogen, C.H.M. Van Den Ende, M.C. Vonk
Radboudumc, Nijmegen, THE NETHERLANDS
Introduction: Autoantibody profiling plays a prominent role in the classification of systemic sclerosis (SSc); it also can be used for disease prognosis. Previously used determinations of autoantibody evaluation did not include RNA polymerase III (anti-RNAP3). Recent studies have shown the importance of this autoantibody with respect to complications and prognosis. The aim of this study is to evaluate the occurrence of the different autoantibodies in a well characterized cohort of SSc.
Material and Methods: A total of 350 consecutive patients from the Nijmegen Systemic Sclerosis Cohort were included in this study. All patients fulfilled the ACR/EULAR 2013 classification criteria for SSc. Patients were sub classified as limited cutaneous SSc (LcSSc), diffuse cutaneous SSc (DcSSc) or SSc overlap syndrome according to Leroy and Medsger. Blood samples were collected at regular outpatient clinic visits and analyzed using LIA. (SSc and ENA immunoblot, Euroimmun, Lubeck, Germany). Clinical data was collected prospectively as described before.
Results: Thirty-three percent of patients were male. Sixty-six percent of the patients were classified as LcSSc, 31% as DcSSc and 2% as overlap syndrome. ANA was positive in 94% of all patients. Anticentromere antibodies (ACA) were present in 29% of the patients, 29% had antitopoisomerase antibodies (ATA) and 6.1% were anti-RNAP3 positive. Severe organ complications occurred in 58%, namely 12% PAH, 40% ILD, 5% cardiac and 0,9% renal crisis. When compared to the recently described Australian cohort our cohort contains more male patients and patients with the diffuse subtype, both associated with worse prognosis. The Nijmegen cohort comprises mainly Caucasians and contains more patients with ATA antibodies and less ACA and anti-RNAP3. Due to the fact that the prevalence of anti-RNAP3 is relatively low in our cohort, the value of this antibody for prognosis is limited in our population. Regarding serious organ complications, we noticed that the prevalence in our cohort of PAH was the same compared to the Australian cohort. However, ILD was slightly more common and renal crisis was much less prevalent.
Conclusions: Anti-RNAP3 antibodies are less prevalent in the Nijmegen cohort of SSc patients. Prevalence of autoantibodies and clinical characteristics differ to some extent with a recently published Australian Cohort, probably due to ethnical differences.
P.171
A Psychosocial Model of Quality of Life in Iranian Patients with Systemic Sclerosis; a 12-Month Longitudinal Study
H. Kavosi1, A. Javinani1, Sh. Mostafaei1,2, Ar. Jamshidi1, R. Atef Yekta3, M. Mahmoudi1, A. Kazemnejad2, F. Gharibdoost4
1 Rheumatology Research Center, Tehran University of Medical Sciences, Tehran, IRAN, 2 Department of Biostatistics, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, IRAN, 3 Anesthesiology Department, Shariati Hospital, Tehran University of Medical Sciences, Tehran, IRAN,4, Rheumatology Research Center, Tehran University of Medical Scie, Tehran, IRAN
Introduction: Systemic sclerosis (SSc) is an autoimmune disease with multi-organ involvements due to obliterative vasculopathy and connective tissue fibrosis. The chronicity, disabilities, systemic nature of SSc and its female predominance can lead to psychological disorders and impaired quality of life (QoL). In contrast to major other disorders which in the end stages have the evident signs of illness, SSc patients encountered most of the disabilities and deformities in the early hood of their disease. The aim of current study was to find a psychosocial model of QoL in Iranian patients with SSc.
Material and Methods: This is a longitudinal study with 12-month follow-up performed on 111 patients selected by simple random approach. Patients were collected from the SSc outpatient clinic of Rheumatology Research Center, Tehran University of Medical Sciences. Individuals with known psychological diseases, neurologic disorders and individuals taking anti-psychotic agents excluded from the study. Clinical manifestations were collected in the baseline and defined according to the Medsger’s severity score. The psychological disturbances were evaluated by Depression Anxiety Stress Scale-21 (DASS-21) and the patients’ QoL assessed by WHOQoL-BREF. Both of these questionnaires were used because they were previously validated in Persian. Questionnaires were completed at the baseline and after 12-month of follow-up. In order to analyze the impact of psychological disturbances, clinical manifestations, demographic features and QoL on each other; the principal component analysis (PCA) was applied.
Results: This study consist of 111 patients with the mean age of 41.68±11.75 years and the mean disease duration of 7.16±5.29 years. The female to male ratio was approximately 5:1 with nearly equal distribution of SSc subtype (54.1% of diffuse cutaneous SSc vs. 45.9% of limited cutaneous SSc). At the baseline, according to path analyses the psychological disturbances have the major effect on QoL with the total standardized effect of -1.12. Demographic features and clinical manifestations have influence on QoL by the total standardized effect of -0.480 and -0.486, respectively. At the end of the follow up, the total standardized effect of psychological disturbances, clinical manifestations and demographic feature on QoL was -0.3276, -0.2654 and -0.0061, respectively.
Conclusions: This longitudinal study showed that the psychological disturbances have the significant effect on patients’ QoL at the baseline but its influence diminish over the time. Nevertheless, the clinical manifestations have the most steady and constant effect on QoL over the time in comparison with demographic features and psychological disturbances.
P.172
Epidemiology and Survival of Systemic Sclerosis-Systemic Lupus Erythematosus Overlap Syndrome
S. Alharbi1,2,3,4, Z. Ahmad 2,3, A. Bookman1, Z. Touma 1,5, J. Sanchez-Guerrero 1,2,3, N. Mitsakakis 5,6, S. Johnson1,2,3,5
1 University Health Network - Toronto Scleroderma Program, Toronto, CANADA, 2 Mount Sinai Hospital - Division of Rheumatology, Toronto, CANADA, 3 University of Toronto - Division of Rheumatology, Toronto, CANADA, 4 Taibah University, Medina, SAUDI ARABIA, 5 University of Toronto - Institute of Health Policy, Management and Evaluation, Toronto, CANADA, 6 University of Toronto - Toronto Health Economics and Technology Assessment Collaborative, Toronto, CANADA
Introduction: Systemic sclerosis (SSc) is an immune disorder characterized by vasculopathy and fibrosis that may overlap with another disease such as systemic lupus erythematous (SLE). Little is known about the epidemiology, clinical characteristics, and survival of SSc-SLE overlap (also called lupoderma). We evaluated the prevalence of SSc-SLE overlap syndrome, differences in SSc clinical characteristics and survival compared with SSc without SLE.
Material and Methods: A cohort study was conducted including subjects who fulfilled the ACR-EULAR classification criteria for SSc and/or the ACR criteria for SLE. The primary outcome was the time from diagnosis to death from all causes. Survival was evaluated using Kaplan Meier curves and Cox Proportional Hazard models.
Results: We identified 1252 subjects (SSc n=1166, SSc-SLE n=86) with a SSc-SLE prevalence of 6.8%. SSc-SLE were younger at diagnosis (37.9 years versus 47.9 years, p<0.001), more frequently had lupus anticoagulant (6% versus 0.3%, p<0.001), anticardiolipin antibody (6% versus 0.9%, p<0.001), and pulmonary arterial hypertension (PAH) (52% versus 31%, p<0.001). SSc-SLE less frequently had calcinosis (13% versus 27%, p=0.007), telangiectasia (49% versus 75%, p<0.001) and diffuse subtype (12% versus 35%, p<0.001). There were no significant differences in the occurrence of renal crisis (7% versus 7%), interstitial lung disease (40% versus 34%), and digital ulcers (38% versus 32%). SSc-SLE had better survival (median 26.1 versus 22.4 years), but this was not statistically significant (log rank p=0.06). Female sex and diffuse subtype attenuated survival differences between groups (Hazard Ratio 0.70, 95%CI 0.45, 1.11).
Conclusions: SSc-SLE are younger at diagnosis, more frequently have PAH, and less frequently have cutaneous manifestations of SSc. SSc-SLE patients should be monitored for pulmonary hypertension, interstitial lung disease, renal crisis and digital ulcers.
P.173
Ethnic Variation in Systemic Sclerosis Morbidity and Mortality
H. Al-Sheikh1,2,3, Z. Ahmad 1,2,3, S. Johnson1,2,3
1 Sinai Health Systems - Department of Medicine, Toronto, CANADA, 2 University Health Network - Department of Medicine, Toronto, CANADA, 3 University of Toronto - Department of Medicine, Toronto, CANADA
Introduction: Systemic sclerosis (SSc) is an uncommon connective tissue disease characterized by pathological skin thickening and can involve multiple internal organs. Ethnic variations in SSc have been reported in clinical manifestations, severity of the disease as well as survival. Our aim was to compare the survival and disease manifestations across ethnicity among SSc patients.
Material and Methods: The Toronto Scleroderma Program is the largest single-center, multiethnic, longitudinal SSc cohort in Canada. Patients are followed every 6 to 12 months using a standardized protocol. Patients who fulfilled the American College of Rheumatology-European League Against Rheumatism classification criteria for SSc and are 16 years of age or older were included in our retrospective cohort study. The study period was 1970–2017. Ethnicity was self-reported and was categorized as: Caucasian, African-American, Hispanic, Arab, East-Asian, First Nations or Persian. The primary outcome was the time from diagnosis to death from all causes. Secondary outcomes were differences in disease duration, SSc subtype, clinical manifestations, and serology. Survival probabilities and median survival times were determined using Kaplan-Meier survival curves. Cox proportional hazard models were used to estimate adjusted survival.
Results: 1005 subjects were evaluated, the majority of whom were Caucasian (n=745 (74%), African-American n=58 (6%)), South Asian (n=69 (7%)), and East Asian (n=80 (8%)). Compared to Caucasians, East Asians less frequently had calcinosis (29% versus 9%, p=0.002), and esophageal dysmotility (88% versus 69%, p=0.002); African-Americans more frequently had interstitial lung disease (31% versus 53%, p=0.007); and First Nation subjects more frequently had diffuse cutaneous disease (35% versus 56%, p=0.02) and diabetes (5% versus 33%, p=0.03). There were no differences across ethnicities in the prevalence of pulmonary hypertension, renal crisis, or digital ulcers.
We found no difference in the short-term survival across ethnicities. However, in the long-term, there was trend for Hispanic subject to have better survival (81.3% (95%CI 63, 100), while First Nations (58.3% (95%CI 25, 100) and South Asian subjects (52.6% (95%CI 32, 87) had worst survival at 15 years and 20 years, respectively. East Asians appear to have the longest median survival time 43.3 years.
Conclusions: Ethnic variations in disease SSc disease manifestations are observed. However, in the setting of a universal health care system, this does not result in significant differences in survival.
P.174
Clinical and Prognostic Profile of Systemic Sclerosis: Analysis in a Single Centre Clinical Cohort in China
S. Hu, D. Xu, Y. Hou, Y. Wang, M. Li, X. Zeng
Peking Union Medical College Hospital, Beijing, CHINA
Introduction: Systemic sclerosis (SSc) is an autoimmune disease of unknown etiology. SSc clinical cohort studies have been carried out in many countries worldwide, but there is no clinical and prognostic analysis based on large-scale clinical cohort of SSc patients in china. The aim of the study is to accomplish the clinical and prognostic analysis of Chinese SSc PUMCH single-centered cohort.
Material and Methods: This research is based on Chinese Rheumatism Data Center (CRDC). Patients diagnosed with SSc and eligible for this research were followed up. Demographic, clinical and outcome date were gathered for statistical analysis. Mann-Whitney and χ2 tests were used to identify differences among groups; Kaplan-Meier analysis was used to estimate survival, and Cox proportional hazards regression analysis was used to identify factors associated with mortality.
Results: A total of 448 patients were included, of whom 56.7% were lcSSc. Women predominated in the entire cohort. Mean age at diagnosis was 40 years. The prevalence of ILD and pulmonary arterial hypertension (PAH) was 85.5% and 21.6% respectively. Valvular disease, left ventricular diastolic dysfunction and pericardial effusion were common in cardiac involvement. LVEF decrease and scleroderma renal crisis (SRC) were rare. Over 2167 patient-years, 23 of 40 deaths were attributable to SSc. Median survival time was 53 months. Survival rates from disease onset were 97.3%, 94.3%, 90.8% and 87.5% at 1, 3, 5 and 10 years, respectively, with poorer survival in patients with PAH. Independent prognostic factors for mortality were PAH (HR 7.7, 95%CI 3.2,19.1) and pericardial effusion (HR 7.0, 95%CI 2.4,20.2).
Conclusions: Ten-year survival is 87.5% in Chinese SSc patients. PAH at baseline and pericardial effusion are the main risk factors for mortality. PAH is the major cause of death.
P.175
Expert Consensus on the Annual Systemic Investigation of Organ Involvement in Systemic Sclerosis
A. Hoffmann-Vold1, O. Distler2, O. Kowal-Bielecka3, D. Khanna4, Y. Allanore5, Eustar Network, Sctc
1 Oslo University Hospital, Dept. of Rheumatology, Oslo, NORWAY, 2 University Hospital Zürich, Dept. of Rheumatology, Zürich, SWITZERLAND, 3 Medical University of Bialystok, Dept. of Rheumatology, Bialystok, POLAND, 4 University of Michigan, Dept. of Rheumatology, Ann Arbor, USA, 5 Cochin Hospital, Dept. of Rheumatology, Paris, FRANCE
Introduction: Systemic sclerosis (SSc) is a progressive, severe multi-organ disease but to date, there are no standardized international guidelines for follow-up of SSc patients. The goal of this project was to improve the standard-of-care for patients with SSc through developing and implementing evidence-based guidelines for annual systematic investigation.
Material and Methods: The Delphi method was applied. All experts in SSc from the EUSTAR network and the scleroderma clinical trial consortium (SCTC) were invited to participate and answer questionnaires in five rounds. In the first round, domains of interest for an annual systematic investigation were determined and in the second round confirmed. In the third round, tools for each domain were determined and confirmed in the fourth round. The preliminary results were discussed with an expert panel at the EUSTAR reloaded meeting. In the fifth round, consensus on the final tools for each domain from the fourth round was emerged by all experts. Parameters rated >80% by more than 80% of the experts were rated as acceptable in all steps.
Results: In total, 132 international centers participated with 71.3% of the experts seeing >50 SSc patients annually. Initially, 23 domains and 204 tools were suggested. After 5 Delphi rounds, 80% of experts agreed on 10 domains and the following tools: (1) Lung (Dyspnea, Functional class (NYHA), Auscultation, Lung function test); (2) Heart (Dyspnea, Heart rate, Blood pressure, Leg edema, Functional class (NYHA), ECG, ECHO, Concurrent heart disease); (3) Laboratory (Acute phase reactants, CK, Hematology, Renal and Liver function test; (4) Musculoskeletal (Hand and finger edema (puffy fingers), Joint contracture, Tender/swollen joints, Calcification, Arthritis, Tendon friction rub count, Muscle weakness and stiffness); (5) Raynaud’s phenomenon (Frequency and severity); (6) Digital ulcers (Presence or absence of distal finger ulcers and proximal ulcers, Number of ulcers, Development of new ulcers during the last year, Gangrene, Amputation, Co-existing conditions (i.e. diabetes), Smoking Status and Pitting scars); (7) Renal (Blood pressure, Serum creatinine, eGFR, Urine analysis, Proteinuria; (8) Skin and mucosa (Puffy hand, Skin thickening, Extent of Skin thickening, Skin worsening or improving (patients reported), Telangiectasia, Calcinosis and modified Rodnan Skin Score (mRSS)); (9) Treatment (Type of treatment and Date of initiation and finalization of every drug); (10) GI (Night and day time heart burn/reflux, Dysphagia, diarrhea, weighting, weight loss since last visit).
Conclusions: Through five Delphi rounds with world leading experts in SSc evidence-based guidelines including strongly suggested tools for minimum annual systemic investigation of organ involvement in SSc were established.
P.176
Immunogenicity and Safety of Pneumococcal Vaccination in Patients with Systemic Sclerosis
R. Hesselstrand1, J. Nagel1, T. Saxne1, P. Geborek1, L. Skattum2, Mc. Kapetanovic1
1 Department of Clinical Sciences, Section for Rheumatology, Lund University, Lund, SWEDEN, 2 Department of Laboratory Medicine, Section of Microbiology, Immunology and Glycobiology, Lund University, Lund, SWEDEN
Introduction: The objective was to study the impact of disease and treatment with disease modifying antirheumatic drugs (DMARDs) on antibody response elicited by either 13-valent pneumococcal conjugate vaccine (PCV13) or 23-valent pneumococcal polysaccharide vaccine (PPV23) in patients with systemic sclerosis (SSc) compared to controls.
Material and Methods: 44 SSc patients and 49 controls were immunized with a single dose of either PCV13 or PPV23. Twelve patients were treated with DMARDs (mycophenolate mofetil=7; azathioprine=4 and azathioprine+hydroxychloroquine=1). Antibody levels to pneumococcal capsular polysaccharides 6B and 23F were measured in sera collected before and 4-6 weeks after vaccination using standard ELISA. The functionality of antibodies was studied using opsonophagocytic assay (OPA) performed on serotype 23F.
Results: Number of patients, percentage female (%), mean age and mean disease duration (years) at vaccination were: 32, 94%, 57.5 and 11.4 years in SSc without DMARDs; 12, 100%, 55.5 and 6.2 years in SSc patients on DMARDs and 49, 63% and 50.6 years in controls. Postvaccination antibody levels for both serotypes increased significantly in SSc without DMARDs and controls (p<0.001) but in SSc patients on DMARDs only for 6B (p=0.04). Compared to controls and SSc without DMARDs, patients with SSc receiving DMARDs had lower postvaccination antibody levels for both serotypes. The functionality of antibodies for 23F did not differ between the 3 groups. No significant difference in immunogenicity between PCV13 and PPV23 was seen.
Conclusions: Pneumococcal vaccination using either PCV13 or PPV23 yielded satisfactory antibody response in SSc patients without DMARD treatment, but a lower response in patients treated with synthetic DMARDs. This suggests a need of vaccination before start of treatment. Type of pneumococcal vaccine (conjugate vs polysaccharide) did not have a significant impact on the antibody response.
P.177
Management of Pulmonary Hypertension in Scleroderma: Are We in Compliance with the Recommendations? Our Experience in Internal Medecine
D. Hakem, N. Slimani, A. Berrah
Internal Medicine, Dr Mohammad-Lamine’s Debaghine, Universitary Center of Bab-El-Oued, Algiers, ALGERIA
Introduction: The current recommendations for the management of pulmonary hypertension ‘PH’ in systemic scleroderma ‘SSc’ are based on simplified and validated algorithms. From screening to diagnosis and therapeutic evaluation, practitioners today have simple, effective tools for appropriate care.
Purpose: Review through our practices the quality of our management of PH during SSc in conforming to the international recommendations.
Material and Methods: Through a questionnaire given to general practitioners, specialists - in internal medicine - we have evaluated the different stages of this management. The questionnaire is based on several items of difficulty ranging from classification, physiopathology, genetics, and assessment tools to therapeutic management of PH occurring in SSc.
Results: The preliminary results are indicators of a management that remains to be perfectly perfaired by the awareness of the general practitioners and public health far from a university pool. Internists who receive this condition on the front line have well developed cardiovascular explorations for screening and follow-up of these disabling and cumbersome conditions in terms of overall joint and visceral management (heart, lung, kidney, liver…).
Conclusions: It is imperative to homogenize our practices in the management of PH during SSc and to adapt as best as possible the recommendations to our environment. The skills and means - even if they remain scattered - exist they will have to be used to the best. Explorations having a cost so must be practiced and repeated according to a reflective algorithm. Finally, only a national register will allow us to evaluate the quality of our care.
P.178
Patient Education Augmented Self Efficacy in Patients with Systemic Sclerosis
K. Gunnarsson, A. Nordin
Karolinska Institute - Department of Rheumatology, Stockholm, SWEDEN
Introduction: Systemic sclerosis (SSc) is an unusual inflammatory systemic disease with a complex and diverse presentation. When a patient is diagnosed with SSc there is often a big need for information and education of the patients that can be challenging to achieve during a usual doctor visit. This can cause anxiety and it can be difficult for the patients to handle information about the disease found on the internet etc.
Our aim of our project was to measure whether patient education augments the self-efficacy and understanding of the disease for patients with SSc and also to evaluate the quality of the patient education meetings.
Material and Methods: 10 patients participated in our project. 2 of the patients couldn’t participate in all meetings and weren’t included in the written evaluation. The education consisted of 3 meetings, each during 2 hours. The subjects discussed were physical activity, medical aids, fatigue, ulcers, Raynauds phenomenon and gastrointestinal disturbances. Invited speakers were doctors, nurses, nutritionists and physical therapists. Patients were asked to evaluate their self-efficacy in a written questionnaire before and after the patient education meetings. We used self-efficacy/self-management instruments developed by Kate Lorig at Stanford University. Patients also made written and oral evaluation of the patient education.
Results: Self-efficacy augmented in 12 of 13 questions that were evaluated. All participants could recommend the education program to other patients with SSc. All participants thought that they had got a better understanding for the disease (6 patients agreed fully and 2 patients partially) by the patient education. All patients thought that the organization of the course and the number of participants worked out well. The patient education was perceived as informative and educative by both patients and invited speakers and there was a mutual learning and a lot of discussion.
Conclusions: Patient education can help patients with SSc to augment their self-efficacy and get a better understanding of their disease. Patient education could in the long run be helpful for the patients to relieve their anxiety. It can also be helpful to teach the patients in which situations it is necessary to contact their doctor urgently and in which situations it can be enough with self-care etc. This could contribute to a more effective use of the resources in the health care system and better satisfaction for the patients. Video classrooms could also be an alternative and reduces the need to invite the same speakers in repeated situations.
P.179
Late-Onset Systemic Sclerosis- Experience of a Eustar Center
L. Groseanu1, T. Gudu1,2, A. Balanescu1,2, V. Bojinca1,2, I. Saulescu1,2, A. Borangiu1,2, D. Opris_Belinski1,2, C. Constantinescu1,2, D. Mazilu1,2, M. Negru1,2, F. Berghea1,2, M. Abobului1,2, S. Daia_Iliescu1,2, R. Ionescu1,2
1 Sf Maria Clinical Hospital-Department of Internal Medicine and Rheumatology, Bucharest, ROMANIA, 2 Carol Davila University of Medicine and Pharmacy, Bucharest, ROMANIA
Introduction: Whether the systemic sclerosis (SSc) disease phenotype varies with older age of onset is unclear. Few and discrepant data are reported on patients suffering from late-onset SSc.
Material and Methods: A retrospective cohort study was conducted to evaluate age-based differences of disease manifestations and survival of SSc patients in EUSTAR center 096. A complete baseline evaluation of all patients was done according to MEDS evaluation sheets. A complete follow-up was done every year. 139 patients were followed between january 2005- ianuary 2017 with a mean follow-up of 8.23(3.56) years. Late-onset SSc was defined as onset of non-Raynaud disease features at or beyond 60 years of age.
Results: There were 22 patients (15.82%) beyond 60 years of age.There were no significant differencies between the two groups regarding the sex distribution, disease subset, disease duration, Rodnan skin score, incidence of digital ulcers, gastrointestinal, musculoarticular, renal, lung or heart involvement, specific scleroderma antibodies. The elderly patients have a longer interval between Raynaud and nonRaynaud symptoms onset (44.73 vs 26.8 months, p=0.002). The incidence of pulmonary arterial hypertension is higher in the elderly group (45,45% vs 38.46, p=0.015). Although there was no significant difference for major organ involvement between groups, there was a slight tendency to use more immunosupressants in older patients (p=0.06). Elderly patients mostly come from rural environment (63.63% vs 17.94%, p=0.02) and have a higher incidence of essential hypertension (59.09% vs 17.94%, p=0.001). Older age did not seem to be a risk factor for higher mortality either (p=0.13). There were only 9 patients beyond 65 years of age, so validity of statistical data would have been doubtful.
Conclusions: No major phenotypic variations were identified in the late onset SSc group, except the higher prevalence of pulmonary hypertension. These features may in part be determined by the underlying cardiovascular disease in elder
P.180
Diagnosis of Systemic Sclerosis – “A Tangled Story”
L. Groseanu1, T. Gudu2, A. Balanescu1,2, V. Bojinca1,2, D. Opris-Belinski1,2, D. Mazilu1,2, I. Saulescu1,2, S. Daia-Iiescu1,2, A. Borangiu1,2, C. Constantinescu1,2, R. Ionescu1,2
1 Carol Davila University of Medicine and Pharmacy, Bucharest, ROMANIA, 2 Sf Maria Clinical Hospital, Bucharest, ROMANIA
Introduction: Proper diagnosis of systemic sclerosis (SSc) is often long and difficult, since it is such a rare disease and one which few doctors or patients are familiar with.
Material and Methods: We conducted a cross-sectional study to establish the interval between the symptoms’ onset of SSc and what type of investigations are performed until the patients reach the final diagnosis
Results: The group included 47 patients, of which only 5 were males and 17 from rural areas.The medium age was 53 (14.4) years. Medium disease duration was 8.5 (9.3) years.
First symptom of onset was Raynaud phenomena 91.3% of the cases, followed by skin changes (56.5%), puffy fingers (52,2%), gastrointestinal and musculoarticular symptoms (23.9% each).
The medium duration between the first symptom and a medical consult was 6(63.5)months. The first medical consult was done by a internal medicine specialist - 38.29%, a rheumatologist- 29.78% a gastroenterologist -12.76%, a dermatologist-8.51%, a nephrologist and a pneumologist (4.25%)
The first suspected diagnosis was SSc in 14 cases, Raynaud syndrome in 8, connective tissue disease in 5, rheumatoid arthritis in 4, cancer, autoimmune hepatitis, idiopathic pulmonary fibrosis each in 2 cases and none in 10 cases.
The medium number of consults until diagnosis was 3.4(1.7). The medium duration from the first symptom until the diagnosis was 39.25(74.03)months.
The first investigations recommended were blood tests in almost all of the patients (95.74%), but only a third of them included specific autoantibodies. Capillaroscopy was performed as an initial diagnostic test in only 6 patients (12.76%). The mean interval from disease onset until the first capillaroscopy was 13.5(28.85)months, to specific autoantibodies was 40.17(61.28) month, to echocardiography was 36.38(53.9) months, to lung function tests and lung CT – 41.76(65.8) months.
There were no significant differences between patients coming from rural environment and those from urban environment. The only significant statistical difference between diffuse and limited subset was the time the patient was referred to echocardiography (p=0.045). The only difference between males and females was related to the interval until capillaroscopy (13.98(20.49)months in females, 4.8(5.02)months in males, p=0.028).
Conclusions: Scleroderma is a less well-known disease. This lack of awareness contributes to delayed diagnosis and delayed onset of therapy. Often such diagnostic uncertainty and frustration takes a huge toll on the psychological well-being of these patients, who describe their journey to diagnosis as being one of the most difficult part of their illness. One of our missions as rheumatologist is to increase recognition of this disorder.
P.181
Determinants of Life Quality in Systemic Sclerosis and Patient Perception of the Disease
L. Groseanu1, A. Dima1, A. Balanescu 1,2, V. Bojinca 1,2, A. Borangiu 1,2, I. Saulescu 1,2, C. Constantinescu 1,2, D. Mazilu 1,2, D. Opris-Belinski 1,2, S. Daia 1,2, R. Ionescu 1,2
1 Sf Maria Clinical Hospital, Department of Internal Medicine and Rheumatology, Bucharest, ROMANIA, 2 Carol Davila University of Medicine and Pharmacy, Bucharest, ROMANIA
Introduction: Systemic sclerosis (SSc) is a chronic multi-system autoimmune disease associated with disability and reduced quality of life.
Material and Methods: We performed a prospective case-control study on EUSTAR cohort 096. 50 SSc patients were evaluated between august 2015-june 2016. Socio-demographic information, disease characteristics and self-assessment questionnaires: Health assessment questionnaire (HAQ), EuroQol-5D (EQ5D) and the Brief Illness Perception Questionnaire (IPQ)-were collected.
Results: The group included 41 females, 9 males, 31 limited and 19 diffuse SSc subsets.
Medium HAQ value was 0.93(0.6). Patients with higher Rodnan skin score (p=0.002), synovitis (p=0.028), late capillaroscopic pattern (p=0.028), muscle weakness(p=0.001), gastrointestinal involvement (p=0.013) and those on immunosupresants (p=0.024) have a poor life quality.
According to EQ-5D, the quality of life was related to organ involvement. 46% had no mobility problems, 48% had some and 6% were confined to bed; mobility was influenced by lung involvement (p=0.008), digital ulcers (p=0.034) and Medsger scores (p=0.017). 44% of the patients did not have self-care problems, 48% had some and 8% were not able to wash dry themselves; self-care was influenced by the Rodnan score (p=0.02), diffuse subset (p=0.023), disease activity score (p=0.019), muscle weakness (p=0.03) and gastrointestinal involvement (p=0.021). 20% of the patients had no problems in performing usual activities, 64% had some and 16% were not able to perform them; the performance was influenced by disease subset (p=0.015), Medsger score (p=0.02), cardiac involvement (p=0.026) and the use of immunosuppresants (p=0.014). 16% of the patients had none pain/discomfort, 52% had some and 38% had extreme pain/discomfort; 14% were not anxious/depressed, 66% were moderately and 20% were extremely anxious/depressed.
The illness had a great impact on patients life 7.3(2.5). The main determinant was pulmonary fibrosis (p=0.04). The patients consider that their disease will continue for a long time 8.73(2.63). Most of the patients do not feel to have a good control on their disease 6.36(3.3) and do not think that the treatment is very helpful 7.92(2.76). The intensity of the symptoms is quite severe 7.52(2.76), related to digital ulcers (p=0.039) and gastrointestinal involvement (p=0.019) Almost all patients are very concerned about their disease 9.12(2.36) are emotionally affected by their disease 7.68(2.67) .
Conclusions: This study confirms the magnitude of impaired life quality in patients with SSc with impact on mobility, self-care, usual activities. The major determinants are the extend of skin, musculoarticular, gastrointestinal involvement and digital ulcers. Often patients are anxious/depressed, had a high pain intensity and the perception of this illness is pessimistic.
P.182
Mean Number of Capillaries Predicts Disease Activity At 6 Months Follow-Up
A.M. Gheorghiu1, R. Oneata1, A. Radu1, A. Briceag1, C. Draganescu1, C. Vrancianu1, S. Magda2, T. Constantinescu3, A. Soare1, R. Dobrota1, I. Ancuta1, C. Ciofu1, L. Macovei1, M. Milicescu1, M. Sasu1, O. Olteanu1, A. Enuica4, T. Necsoiu4, O. Linte4, G. Stan4, B. Comanescu4, M. Bojinca1, V. Stoica1, C. Mihai1
1 Cantacuzino Clinical Hospital, Internal Medicine and Rheumatology Department, Carol Davila UMF, Bucharest, ROMANIA, 2 Cardiology Department, University Emergency Hospital, Carol Davila UMF, Bucharest, ROMANIA, 3 Marius Nasta National Pneumology Institute, Carol Davila UMF, Bucharest, ROMANIA, 4 Optoelectronica, Bucharest, ROMANIA
Introduction: Nailfold capillaroscopy (NFC) is essential in the evaluation and classification of systemic sclerosis (SSc). In recent years, the mean number of capillaries was considered a promising tool for assessing vascular involvement in SSc, however there is no consensus yet over how many digits should be analyzed and how.
Objective: Investigation of the associations of the mean number of capillaries, measured by NFC, with disease activity (measured by the EScSG activity score) and vascular involvement (digital ulcers (DUs) or history of DUs) in a single-center cohort of patients with SSc.
Material and Methods: Sixty eight patients with SSc (mean(SD) age 52.9(11.0) years, disease duration 9.2(7.1)years, male gender 7(10.3%) and diffuse cutaneous involvement 22(34.2%)) fulfilling the ACR/EULAR 2013 classification criteria, were included in the study. NFC and extensive assessment per the recommendations of EUSTAR were performed in all patients. Fifty-four patients had a follow-up at 6 months. Eight digits were examined (II to V of both hands) by NFC; four images for each finger were saved. The NFC images were assessed by two experienced raters independently, scoring the mean number of capillaries in all fingers (m_nr/pat), in the 3rd finger of the dominant hand (m_nr/3rd dom) and in the 4th finger of the non-dominant hand (m_nr/4th non-dom) for each patient. Moreover, ‘early’, ‘active’, ‘late’ Cutolo patterns and unclassifiable in any pattern were also recorded.
Results: 2176 images were scored at baseline and 1728 at follow-up. The m_nr/pat at baseline ranged between 3.4-9.1, with a mean(SD) of 5.6(1.7) for rater 1, respectively 3.3-8.9, 5.2(1.4) for rater 2.
There was good to excellent correlation (Spearman’s rho) at baseline and follow-up of the m_nr/pat with m_nr/3rd dom, m_nr/4th non-dom and Cutolo patterns, and fair correlation of m_nr/3rd dom with m_nr/4th non-dom and Cutolo patterns.
We found significant differences of all mean scores of capillaries between patients with and without DUs (m_nr/pat 5.04(1.4) vs. 6.4(1.8), p=0.016 for reader 1, by Mann Whitney U test). Using linear regression adjusted for age, gender and history of DUs, mean number of capillaries was associated with disease activity at follow-up (table 1).
Conclusions: The mean number of capillaries had a good association with the history of DUs and predicted disease activity at 6 months follow-up. The m_nr/pat performed better in our analysis than the m_nr/3rd dom and m_nr/4th non-dom, however these could be used alternatively in clinical practice as they are less time consuming.
Acknowledgements: Part of the QUANTICAP project, financed by the UEFISCDI-PN-II-PT-PCCA-2013-4-1589 grant.
P.183
Assessing Survival, Causes of Deaths and Predictors of Mortality in Systemic Sclerosis; Results from a Complete, Nationwide Cohort
H. Fretheim1, M. Seip2, A.K. Halse3, H. Bitter4, M. Wallenius5, T. Garen1, Ø. Molberg1, A.M. Hoffmann-Vold1
1 Department of Rheumatology - Oslo University Hospital, Oslo, NORWAY, 2 Department of Rheumatology - University Hospital of North Norway, Tromsø, NORWAY, 3 Department of Rheumatology - Haukeland University Hospital, Bergen, NORWAY, 4 Department of Rheumatology - Hospital of Southern Norway, Kristiansand, NORWAY, 5 Department of Rheumatology, St. Olav’s University Hospital, Trondheim, NORWAY
Introduction: Mortality in systemic sclerosis (SSc) has predominantly been assessed in tertiary referral cohorts where referral bias is unavoidable. We aimed to assess survival, causes of deaths and predictors of mortality, using the unique nationwide Norwegian SSc (Nor-SSc) cohort.
Material and Methods: Nor-SSc included all adult patients resident in Norway; (A) registered with ICD-10 code M34 (SSc) in a public hospital database between January 2000 and March 2017 (B) had a clinical SSc diagnosis verified by a rheumatologist and (C) met the 1980 ACR and/or 2013 ACR/EULAR classification criteria for SSc. Baseline clinical data and vital status were available in all patients, and clinical follow-up data in 70% of patients. We obtained causes of death from death certificates and validated this information by chart review. Factors predicting fatal outcome were assessed by Cox regression analyses with two models; one that included baseline characteristics, and one that included disease progression parameters.
Results: Nor-SSc included 969 patients. Mean age at disease onset was 49 years, 84% of patients were female and 78% had limited cutaneous SSc. 248(25.6%) died during the observation period.
The overall 5-and 10-year survival estimates in the total Nor-SSc cohort were 90% and 79%; with reduced survival in patients with pulmonary arterial hypertension(PAH) (74% and 51%), and severe interstitial lung disease (ILD) marked by lung fibrosis extent >10% on CT (85% and 58%). Cause of death was related to SSc in 37%. The major causes of death related to SSc were ILD(44%), PAH(20%), and gastrointestinal complications(16%).
The following baseline characteristics predicted mortality in univariable Cox analyses; age at diagnosis, male gender, diffuse cutaneous SSc(dcSSc), anti-topoisomerase antibody (ATA), NT-proBNP, systolic pulmonary arterial pressure (sPAP) on echocardiogram, FVC%, DLCO%, NYHA class, lung fibrosis%, modified Rodnan skin score (mRSS), GAVE, 6-minutes’ walk test (6MWT) and obstipation. The final multivariable model included age at diagnosis(HR 1.11,CI95%1.08-1.14,p<0.000), males(HR 2.03,CI95%1.07-3.84,p=0.030), sPAP(HR 1.02,95%CI1.01-1.03,p<0.001), lung fibrosis%(HR 1.02,95%CI1.01-1.04p=0.012), mRSS(HR 1.05,95%CI1.03-1.08,p<0.001) and 6MWT(HR 0.99,95%CI0.99-0.99,p<0.001) at baseline (C-index 0.86).
Disease progression parameters predicting mortality in univariable analyses included the following new onset variables: lung fibrosis>10%, FVC<70%, DLCO<60%, sPAP>40mmHg and NT-proBNP>60 pmol/L. In the multivariable cox model, we found that age at diagnosis(HR 1.1,P=0.000,95%CI1.06-1.15.), new onset fibrosis>10%(HR 3.2, 95%CI1.03-10.06,p=0.045) and FVC<70%(HR 3.6,95%CI1.03-12.88,p=0.045) predicted mortality (C-index 0.82).
Conclusions: Results from the nationwide Nor-SSc cohort confirm that survival is reduced in SSc, with PAH and ILD as major causes. Prediction models suggest that mortality risk is mainly determined by baseline characteristics, but also influenced by disease progression parameters.
P.184
Outcomes of Limited Cutaneous Systemic Sclerosis Patients: a Eustar Database Study
C. Frantz1, D. Huscher2, E. Hachulla3, A. Balbir-Gurman4, G. Riemekasten5, E. Siegert6, P. Airò7, B. Joven8, S. Vettori9, F. Cozzi10, S. Ullman11, L. Czirjàk12, Y. Allanore1
1 Rheumatology A Department, Cochin Hospital, Paris Descartes University, Paris, FRANCE, 2 Epidemiology unit, German Rheumatism Research Centre, Berlin, GERMANY, 3 Department of Internal Medicine, Hôpital Claude Huriez, Lille University, Lille, FRANCE, 4 B Shine Rheumatology Unit, Rambam Health Care Campus, Haifa, ISRAEL, 5 Department of Rheumatology, University of Lübeck, Lübeck, GERMANY, 6 Department of Rheumatology and Clinical Immunology, Charité University Hospital, Berlin, GERMANY, 7 Rheumatology and Clinical Immunology, Spedali Civili of Brescia, Brescia, ITALY, 8 Servicio de Reumatologia, Hospital Universitario 12 de Octubre, Madrid, SPAIN, 9 Department of Clinical and Experimental Medicine, ‘F-Magrassi’ II, Napoli, ITALY, 10 Rheumatology Unit, Department of Medicine, University of Padova, Padova, ITALY, 11 Department of Dermatology, University Hospital of Copenhagen, Hospital Bispebjerg, Copenhagen, DENMARK, 12 Department of Immunology and Rheumatology, University of Pécs, Pécs, HUNGARY
Introduction: Several studies have consistently showed that the extent of skin involvement has a major impact on disease prognosis in the diffuse cutaneous subtype of systemic sclerosis. The large majority of the ongoing clinical trials aim at identifying efficient drug in this subset. By contrast, little is known about the limited cutaneous subset (LcSSc) and the translation of the data coming for DcSSc to LcSSc is uncertain. Therefore, our aim was to investigate skin and lung involvement trajectories of LcSSc patients using the large EUSTAR registry.
Material and Methods: We analyzed the longitudinal data extracted from the EUSTAR cohort collected before February 2017. Worsening of skin fibrosis was defined by an increase in modified Rodnan skin score (mRSS) > 3.5 points from baseline to 2nd visit. Interstitial lung disease (ILD) was defined by any fibrosis on imaging (X-ray/computed tomography). Worsening of ILD was defined by a decrease of FVC > 10% from baseline to 2nd visit. For predicting models, predictors with p<0.2 in the univariate analysis were included in the logistic regression analysis.
Results: 8013 LcSSc were included with a mean follow-up of about 3.33.7 years. At baseline, meanSD mRSS was 65 and ILD was present in 28.4% of all patients.
Worsening of skin fibrosis was observed in 6.4% (19/298), 7.8% (97/1248) and 9.8% (289/2957) of LcSSc patients at 6, 12 and 24 months follow-up respectively. In multivariate analysis, variables predicting skin fibrosis progression were elevated European Scleroderma Study Group activity index (EScSG-AI) (OR 95 IC: 1.22 1.05-1.4, p=0.007) for 12 months progression and EScSG-AI (1.24 1.13-1.38, p<0.001 ) and mRSS (0.95 0.93-0.98, p=0.001) for 24 months progression.
Worsening of ILD was observed in 11.7% (23/196) and 19.9% (65/326) of LcSSc patients with ILD at baseline, at 12 and 24 months follow-up respectively. In multivariate analysis, variables predicting ILD progression at 24 months were EScSG-AI>3 (OR 95 IC: 3.8 1.51-9.56, p=0.005), FVC (1.03 1.01-1.04, p<0.001) and LVEF (0.91 0.85-0.97, p=0.005).
Conclusions: It appears that only few LcSSc patients progress for skin fibrosis ; this limits the use of mRSS in this subset and the potential of anti-fibrotic drugs of skin disease. However, a substantial rate of ILD progression was identified as well as relevant predictors. These results support the inclusion of LcSSc patients in SSc-ILD trials evaluating anti-fibrotic drugs. Our predictive models will be helpful to define enriched population in future clinical trials.
P.185
Clinical Characteristics and Mortality Rate for Thai Elderly Onset Systemic Sclerosis
C. Foocharoen, R. Apipattarakul, S. Netwijitpan, A. Mahakkanukrauh, S. Suwannaroj, P. Limpawattana, R. Nanagara
Department of Medicine, Faculty of Medicine, Khon Kaen University, Khon Kaen, THAILAND
Introduction: Elderly, over against adult, Caucasian systemic sclerosis (SSc) patients are at greater risk of pulmonary arterial hypertension (PAH), renal impairment, cardiac disease, and muscle weakness, but a lower risk for digital ischemia. There is, however, no report of a clinical comparison between Thai adult vs. elderly onset diffuse cutaneous SSc (dcSSc). Objectives of our study were to identify the clinical differences and mortality rate between adult and elderly onset SSc.
Material and Methods: We conducted a historical cohort study of SSc patients followed up at Srinagarind Hospital, Khon Kaen University, Thailand, between January 2007 and December 2011. SSc patients 60 years of age and above were defined as elderly onset SSc. Clinical differences between adult and elderly onset were identified. Cox regression analysis was used to estimate the probability of survival and for assessing the factors associated with mortality.
Results: The medical records of 350 SSc patients were reviewed; 53 patients (15.1%) had elderly onset SSc. According to the multivariate analysis, elderly onset SSc had a higher WHO functional class, more frequent weakness, hyperCKaemia, and less pulmonary fibrosis than adult onset SSc (p=0.004, 0.02, 0.02, 0.02, respectively. For the total 2,399 person-years, the incidence of mortality was 3.8 per 100 person-years with a median survival rate of 15.9 years (95%CI 12.4-17.3). The mortality rate of elderly onset SSc was 12.7 per 100 person-years whereas adult onset was 2.9 per 100 person-years with a median survival of 4.9 years (95%CI 3.8-7.4) and 16.1 years (95%CI 14.8-23.4), respectively. The mortality rate of elderly SSc onset was significantly higher than that of adult SSc onset (HR 5.71 (95%CI 3.54-9.20). The Cox regression analysis indicated that digital ulcer and tendon friction rub had a respective HR of 7.39 (95%CI 1.28-42.60) and 37.23 (95%CI 2.10-659.09) for predicting mortality of elderly onset SSc. Neither severity of skin tightness nor SSc subset was associated with mortality.
Conclusions: Myopathy and limitation of physical activity were frequently found among elderly onset SSc over against pulmonary involvement than in adult onset SSc. Median survival of elderly onset SSc was 11 years shorter than adult onset SSc. Digital ulcer and tendon friction rub were associated with a high mortality rate in elderly onset SSc.
P.186
Proposal for a Juvenile Systemic Sclerosis Response Index(JSSCRI): Result of the Consensus Meeting in Hamburg. Germany 11Th of December 2016
I. Foeldvari1, D. Furst2, J. Anton3, E. Baildem4, M. Blakley5, T. Constantin6, P. Costa Reis7, M. Curran8, M. Cutolo9, C. Denton10, K. Fligelstone11, B. Hinrichs12, F. Ingegnoli13, A. Höger1, D. Nemcova14, C. Pain4, C. Pilkington15, V. Smith16, D. Khanna17
1 Hamburger Zentrum fuer Kinder- und Jugendrheumatologie, Hamburg, GERMANY, 2 UCLA, Los Angeles, USA, 3 Sant Joan de Déu Hospital, Barcelona, SPAIN, 4 Alder Hey Childrens Foundation NHS Trust, Liverpool, UNITED KINGDOM, 5 Indiana University, Indianapolis, USA, 6 Semmelweis University, Budapest, HUNGARY, 7 Hospital de Santa Maria, Lisbon, PORTUGAL, 8 Northwestern University, Chicago, USA, 9 University of Genova, Genova, ITALY, 10 Royal Free Hospital, London, UNITED KINGDOM, 11 FESCA, London, UNITED KINGDOM, 12 Practice Buchholz, AMS, Hamburg, GERMANY, 13 University of Milan, Milano, ITALY, 14 Department of Pediatrics and Adolescent Medicine, Prague, CZECH REPUBLIC, 15 Great Ormond Street Hospital (GOSH), London, UNITED KINGDOM, 16 GU(H), Ghent, BELGIUM, 17 University Michigan, Michigan, USA
Introduction: Juvenile Systemic Sclerosis (jSSc) is an orphan disease. There is increaseing interest to test novel therapies in management of fibrotic diseases. Therefore, is very important to develop a Response Index for jSSc (JSScRI) to separate effective therapies from placebo. In 2014 at the First Consensus Meeting in Hamburg, following two rounds of Delphi, a proposal for domains and items for a JSScRI were made. In 2016, the 2nd JSScRI Consensus Meeting was held in Hamburg, Germany.
Material and Methods: Before the 2nD JSScRI Consensus Meeting, the items from the first JSScRI Consensus Meeting (2014) were scored in a Delphi by the participants to the current meeting. Participants included 14 experts in adult and juvenile SSc and a patient partner. During the subsequent face to face NGT meeting, moderated by DEF, the items were scored anonymously by the participants after a nominal group discussion moderated by DEF. The domains and items were scored regarding their importance for 1 year clinical trial. The items were scored 1(not relevant at all) to 9(most relevant). A Priori, it was agreed by the participants that the goal of the NGT was to exclude items that are 1. Not feasible and 2. Don’t represent an outcome measure but may represent the impact of disease on quality of life and vocational and avocational activity. Items that scored a median score of <4 or where greater than 1/3 of participants scored 1-3 [despite the item have a median score > 3] were excluded.
Results: 71 items in 13 domains were scored. 6 Items were not scored as they were felt not to represent an outcome measure or non-feasible and and 6 items received a median score less then 4.
Table 1 provides an example of musculoskeletal involvement with Median score for different outcome measures. ll).
Conclusions: In a rigorous, NGT consensus meeting, some item reduction for the JSScRI was achieved. These will be tested in a prospective, inception cohort of juvenile SSc patients. clerosis inception cohort (www.juvenile-scleroderma.com)
P.187
Assessing the Prevalence of Juvenile Systemic Sclerosis in Childhood Using Administrative Claims Data from the United States
I. Foeldvari1, T. Beukelman2, F. Xie2
1 Hamburger Zentrum fuer Kinder- und Jugendrheumatologie, Hamburg, GERMANY, 2 University of Alabama at Birmingham, Birmingham, USA
Introduction: Juvenile systemic Sclerosis (jSSc) is an orphan disease. There are some data regarding the incidence, but nearly no data exist regarding the prevalence of jSSc. To plan prospective trials, it is very important to gain data regarding the prevalence of jSSc.
Material and Methods: We used Truven MarketScan® commercial insurance claims data from the United States for the years 2010 through 2014, inclusive. In each individual calendar year, we identified all persons in the claims data who were less than 16 years old. Among these persons, we identified all persons with at least 1 physician diagnosis code for systemic sclerosis (ICD-9 710.1) and then removed any person with a diagnosis code for localized scleroderma (ICD-9 701.0). From this remaining group of patients, we identified patients with at least one filled prescription or infusion claim for immunosuppressant medications often used to treat systemic sclerosis, namely methotrexate, mycophenolate mofetil, or cyclophosphamide. We assumed these children had jSSc and calculated the estimated prevalence and 95% confidence interval using a Poisson distribution.
Results: The results for each calendar year are shown in the Table. Very few children received diagnosis codes for systemic sclerosis. Approximately 70% of these patients did not have concurrent diagnoses of localized scleroderma, but only approximately 14% of those had treatment with immunosuppressant medications often used to treat systemic sclerosis. The prevalence estimates were approximately 3 per 1 million children and were relatively stable from year to year.
Conclusions: Using diagnosis codes and medication usage from administrative claims, we estimated the prevalence of jSSc to be approximately 3 per 1 million children.
P.188
Is There a Difference in the Clinical Presentation of Juvenile Systemic Scleroderma Patients According the Age of Onset: Results from the Juvenile Scleroderma Inception Cohort. www.juvenile-scleroderm
I. Foeldvari1, J. Klotsche2, O. Kasapcopur3, A. Adrovic3, V. Stanevicha3, M.T. Terreri3, E. Alexeeva3, M. Katsicas3, V. Smith3, R. Cimaz3, M. Kostik3, T. Lehman3, J. Anton3, W.A. Sifuentes-Giraldo3, F. Sztajnbok3, T. Avcin3, M. Janarthanan3, M.J. Santos3, M. Moll3, D. Nemcova3, N. Helmus1
1 Hamburger Zentrum fuer Kinder- und Jugendrheumatologie, Hamburg, GERMANY, 2 German Rheumatism Research Center, Berlin, GERMANY, 3 jSSc Collaborative Group, Hamburg, GERMANY
Introduction: Juvenile systemic sclerosis (jSSc) is an orphan autoimmune disease. It was rarely looked at the differences between the clinical presentations of patients at different paediatric age groups. The juvenile scleroderma inception cohort (www.juvenile-scleroderma.com) is a prospective standardized register for patients with jSSc.
Material and Methods: Patients with jSSc were included worldwide to the juvenile scleroderma inception cohort. We compared the demographics and clinical characteristics of the patients at different age ranges. We created 3 cohorts with different age ranges at onset of disease. Patents aged less than 5 years (Group1), 5-10 years (Group2) and over 10 years (Group3) at the time of diagnosis of the first non-Raynaud involvement of jSSc.
Results: Up till now 88 patients were enrolled,14 patients (15%) in Group1, 22 (25%) in Group2 and 52 (59%) in Group3. Diffuse subtype occurred in 71% in Group1, in 82% in Group2 and in 65% in Group3. Most patients were Caucasian. Disease duration at time of inclusion into the cohort was 3.9 years in Group1, 4.9 years in Group2 and 2.2 years in Group3. ANA positivity was 57% in Group1, 77% in Group2 and 86% in Group3. Anti-scl 70 was around 30% in all groups. Anti-Centromere positivity was 7 to 10%. Mean modified skin score was 12.4 in Group1, 16.5 in Group2 and 15.9 in Group3. Raynaud Phenomenon occurred in 85 to 95% of the patients. History of active or inactive ulceration occurred in 57% in Group1, 62% in Group2 and 43% in Group3. Decreased FVC under 80% occurred in 43% in Group1, 32% in Group2 and 30% in Group3. Pulmonary hypertension occurred in 7% in Group1 and in 10% in Group3. No renal hypertension was observed. Urinary sedimentary changes occurred in 7% in Group1 and in 10% in Group3. Gastrointestinal involvement occurred in 21% in Group1, 45% in Group2 and 27% in Group3. Musculoskeletal involvement occurred in 58 to 64 %. Patient global disease activity (VAS 0-100) was 42.8 to 47.9. Patient global disease damage (VAS 0-100) was 39.6- to 45.0. Physician global disease activity (VAS 0-100) was 35.4-40.0. Physician global disease damage (VAS 0-100) was 37.1 in Group1, 41.3 in Group2 and 27.7 in Group3.
Conclusions: It seems to be that patients, with onset of the disease in younger age have more severe disease as patients with disease onset after the age of 10 years. We need more patients in our cohort to gain more sufficient data to prove our preliminary observation.
P.189
Are Patients with Overlap Features Different from Patients Without? Results from the Juvenile Systemic Scleroderma Cohort (www.juvenile-scleroderma.com)
I. Foeldvari1, J. Klotsche2, O. Kasapcopur3, A. Adrovic3, V. Stanevicha3, K. Torok3, M.T. Terreri3, E. Alexeeva3, M. Katsikas3, V. Smith3, F. Sztajnbok3, T. Avcin3, R. Cimaz3, A. Jordi3, M. Kostik3, T. Lehman3, W.A. Sifuentes-Giraldo3, S. Appenzeller3, M. Janarthanan3, M. Moll3, D. Nemcova3, M.J. Santos3, N. Helmus1
1 Hamburger Zentrum fuer Kinder- und Jugendrheumatologie, Hamburg, GERMANY, 2 German Rheumatism Research Center, Berlin, GERMANY, 3 jSSc Collaborative Group, Hamburg, GERMANY
Introduction: Juvenile systemic sclerosis (jSSc) patients with overlap features seems to have a better long term outcome (1). There is currently no data, where the clinical characteristics of patients with and without overlap features were compared.
Material and Methods: Patients, fulfilling the PRES jSSc-classification criteria were included. Organ involvement was assessed using the standardized assessment. Patients were classified to diffuse (dcjSSc) and limited (lcjSSc) subtype and grouped as patients with and without overlap features.
Results: Till April 2016 eighty patients were enrolled. We present data at time point of the enrollment. 11 of the patients had overlap features (oJSSc). 6 of 58 (10%) in the dcjSSc and 5 of 22 (23%) in the lcjSSc. Most patients were Caucasian. Female/male ratio differed in the groups, in the nojSSc 3.9:1 and in the ojSSc 11:1 (p=0.1). Mean disease duration was 3.6 years in the non-overlap features group (nojSSc) and 3.2 years in the ojSSc group. Patients with nojSSc were 35% Scl-70 positive and ojSSc group none (p=0.032). Decreased DLCO occurred in 48% in the nojSSc and in 100% in the ojSSc group (p=0.088). Renal involvement was more frequent in the ojSSc group with 18% compared to 4% the nojSSc (p=0.078). Swollen joints occurred in 63% in the ojSSc and in 29% in the nojSSc group (p<0.001). Muscle weakness combined with joint contractures occurred in 43% in the ojSSc and in 8% in the nojSSc group (p=0.011).
Conclusions: Patients with overlap features have distinct characteristics compared with patients with nojSSc. This characteristics were no Scl-70 positivity, higher portion of interstitial lung disease, renal involvement, arthritis and muscle involvement accompanied by joint contractures. The future larger patient data collection in our cohort will help to make the differences more accentuated.
Literature
1.Foeldvari I, Nihtyanova SI, Wierk A, Denton CP. Characteristics of Patients with Juvenile Onset Systemic Sclerosis in an Adult Single-center Cohort. J Rheumatol 2010;37:2422- 6.
P.190
Male Patients Have a More Severe Course As Female Patients with Diffuse Juvenile Systemic Scleroderma? Results from the Juvenile Scleroderma Inception Cohort www.juvenile-scleroderma.com
I. Foeldvari1, J. Klotsche2, O. Kasapcopur3, A. Adrovic3, V. Stanevicha3, K. Torok3, M.T. Terreri3, E. Alexeeva3, M. Katsikas3, V. Smith3, F. Sztajnbok3, T. Avcin3, R. Cimaz3, A. Jordi3, M. Kostik3, T. Lehman,3, W.A. Sifuentes-Giraldo3, S. Appenzeller3, M. Janarthanan3, M. Moll3, D. Nemcova3, M.J. Santos3, N. Helmus1
1 Hamburger Zentrum fuer Kinder- und Jugendrheumatologie, Hamburg, GERMANY, 2 German Rheumatism Research Center, Berlin, GERMANY, 3 jSSc Collaborative Group, Hamburg, GERMANY
Introduction: In adult systemic scleroderma patients male have a more sever course. This issue was never evaluated in a larger juvenile scleroderma cohort.
Material and Methods: Patients with jSSc were included worldwide to the jSScI cohort. We compared the demographics and clinical characteristics of male and female dcjSSc patients at the time of the enrollment into the jSSci.
Results: Sixty-two dcjSSc patients were enrolled Up till April 2016. 11/62 (18%) of the patients were male (M) and 51/62 female (F) (82%). The mean age of the onset of Raynaud symptoms was 8.0 in M and 9.4 years in the F patients and the non-Raynaud symptoms was 8.2 in M and 10.0 in F patients. At the time of the enrollment the mean MRSS was 24.3 in M and 17.3 in F patients. Anti-Scl 70 positivity was found in 4/11 (36.4%) in M and 14/49 (28.6%) in F patients. Anticentromere positivity occurred in 2/11 (18.2%) in M and 0/23 (0%) in F patients (p=0.035). Capillary changes were present in 8/11(73%) of the M and 30/51 (59%) of F patients, but 36% of M and F had already history of ulcerations. 7/11 (64%) of the M and 21/51 (41%) of the F patients had cardiopulmonary involvement. pulmonary hypertension occurred in F patients (n=6). 7/11 (64%) of M and 11/51 (22%) of F patients had signs of interstitial lung disease (p=0.005). No renal crisis was observed till enrollment. 37% in both sexes had gastrointestinal involvement. Patient global disease damage was on a VAS (0- 100) 56.9 in M and in 38.4 in F (p=0.014) and patient global disease activity was 58.8 in M and 41.9 in M (p=0.024). Physician global of disease activity on a VAS was 58.9 in M and 36.9 in F (p=0.004) and physician global disease damage was 60.2 in M and 31.2 in F (p=0.001).
Conclusions: Male patients had a significantly more severe disease course at time point of enrollment. This finding overlaps to the observation in adult cohorts.
P.191
Update on the Juvenile Systemic Sclerosis Inception Cohort Project. Characteristics of the First 97 Patients At First Assessment. www.juvenile-scleroderma.com
I. Foeldvari1, J. Klotsche2, O. Kasapcopur3, A. Adrovic3, V. Stanevicha3, K. Torok,3, M.T. Terreri3, E. Alexeeva3, M. Katsikas3, V. Smith3, F. Sztajnbok3, T. Avcin3, R. Cimaz3, A. Jordi3, M. Kostik3, T. Lehman3, W.A. Sifuentes-Giraldo3, S. Appenzeller3, M. Janarthanan3, M. Moll3, D. Nemcova3, M.J. Santos3, N. Helmus1
1 Hamburger Zentrum fuer Kinder- und Jugendrheumatologie, Hamburg, GERMANY, 2 German Rheumatism Research Center, Berlin, GERMANY, 3 jSSc Collaborative Group, Hamburg, GERMANY
Introduction: Juvenile systemic sclerosis (jSSc) is an orphan autoimmune disease. Currently just smaller retrospective data exist regarding presentation of organ involvement. In the previous studies assessment of the organ involvement was not standardized. Our project is the first one, where data of jSSc patients were collected prospectively and with a standardized assessment. We present the data at the time of inclusion.
Material and Methods: Patients with jSSc were recruited worldwide and were prospectively assessed, using the proposed standardized patient assessment
Results: 30 centers from 19 countries agreed to participate on the project. The assent and consent forms were translated into the local native languages. Until now 97 patients have been enrolled with a mean disease duration of 3.1 years. Seventy-seven (79%) of the 97 patients were females. The mean age of the onset of Raynaud’s phenomenon was 9.6 years (+4.1 years), the youngest 1,5 years old. The mean age at the onset of the non-Raynaud presentation of jSSc was 10.3 years (+4.1 years). 68 (70%) of the 50 have diffuse subtype. 7/68 in the diffuse (10%) and 3/29 in the limited subtype (10%) had an overlap feature. Seventy-nine % of the patients received a disease modifying drug.
At the time of the inclusion the mean modified Rodnan Skin Score was 15.7, in the diffuse 18.6 and in the limited 7.7. 61/97 (63%) had already capillary changes and 44/95 (46%) already had history of ulcerations, 18/95 (19%) had active ulcerations at the time of the inclusion. 20/63 (32%) had decreased FVC under 80% and 18/39(46%) had decreased DLCO less than 80%. 28/58 (36%) had signs of interstitial lung disease on HRCT. 7/97 (7%) patients had pulmonary hypertension assessed by echo. 6/97 (6%) had urine sedimentary changes, 3 of them significant proteinuria, but no hypertension or renal crisis was observed. 28/97 (29%) of them esophageal involvement. 58/97 (59.8%) had musculoskeletal involvement. ANA positivity occurred in 77/97 (81%) and 32/92 (34%) of them were anti-Scl 70 positive. 4/62 (6%) had anticentromere positivity.
Conclusions: We present the data on the first 97 patients with jSSc included in our cohort. The current recruitment data confirms that pediatric patients are different from the adult patients, with a higher proportion of diffuse subset patients with 70% and 15% of patients with overlap features. Anti-centromere antibodies occurring only in 6% of patients.
P.192
Changes in Causes of Death in Systemic Sclerosis: 1995-2015: Data from Eustar Network
M. Elhai1, E. Hachulla2, A. Balbir-Gurman3, G. Riemekasten4, P. Airò5, B. Joven6, S. Vettori7, F. Cozzi8, S. Ullman9, L. Czirják10, M. Tikly11, U. Müller-Ladner12, P. Caramaschi13, O. Distler14, F. Iannone15, L.P. Ananieva16, R. Hesselstrand17, R. Becvar18, A. Gabrielli19, M. Matucci-Cerinic20, Y. Allanore1
1 Paris Descartes University, INSERM U1016, Sorbonne Paris Cité, Rheumatology A department, Cochin Hospital, Paris, FRANCE, 2 Department of Internal Medicine, Hôpital Claude Huriez, University Lille Nord-de-France, Lille, FRANCE, 3 B. Shine Rheumatology Unit, Rambam Health Care Campus, Rappaport Faculty of Medicine, Technion Institute of Technology, Haifa, ISRAEL, 4 Department of Rheumatology, University of Lübeck, Lübeck, GERMANY, 5 UO Reumatologia ed Immunologia Clinica Spedali Civili Brescia, Brescia, ITALY, 6 Servicio de Reumatologia, Hospital Universitario 12 de Octubre, Madrid, SPAIN, 7 Department of Clinical and Experimental Medicine F Magrassi II, Naples, ITALY, 8 Rheumatology Unit, Department of Medicine, University of Padova, Padova, ITALY, 9 University Hospital of Copenhagen, Department of Dermatology, Hospital Bispebjerg, Copenhagen, DENMARK, 10 Department of Immunology and Rheumatology, University of Pécs, Pécs, HUNGARY, 11 Chris Hani Baragwanath Academic Hospital University of the Witwatersrand, Johannesburg, SOUTH AFRICA, 12 Department of Rheumatology and Clinical Immunology, Justus-Liebig University Giessen, Kerckhoff Clinic, Bad Nauheim, GERMANY, 13 Rheumatology Unit, Department of Medicine, University of Verona, Verona, ITALY, 14 Department of Rheumatology, University Hospital Zurich, Zurich, SWITZERLAND, 15 Interdisciplinary Department of Medicine-Rheumatology Unit, Policlinico, University of Bari, Bari, ITALY, 16 VA Nasonova Institute of Rheumatology, Moscow, RUSSIA, 17 Department of Clinical Sciences Lund, Section of Rheumatology, Lund University, Skåne University Hospital, Lund, SWEDEN, 18 Institute of Rheumatology, 1st Medical School, Charles University, Praha, CZECH REPUBLIC, 19 Clinica Medica, Dipartimento di Scienze Cliniche e Molecolari, Università Politecnica delle Marche, Ancona, ITALY, 20 Section of Internal Medicine and Division of Rheumatology, Azienda Ospedaliero-Universitaria Careggi (AOUC), Florence, ITALY
Introduction: Systemic Sclerosis (SSc) is a severe auto-immune disease associated with a high mortality. In a recent study (Elhai M et al. ARD 2017), we highlighted the major contribution of the cardiopulmonary system to SSc-mortality. However, the evolution in causes of death in SSc over the past 20 years remains unknown. The aim of this complementary study was to document the changes in organ system causes of mortality in SSc over the past 20 years in the international EUSTAR cohort.
Material and Methods: In our previous study, the latest 2014 data extract from the EUSTAR cohort was analysed and investigators from each center, with at-least one death recorded, were asked to indicate the single primary cause of death according to standardized definitions. For the present study, causes of death were analyzed in four time periods between 1995 and 2015. Comparison in causes of death according to time periods was performed using Anova.
Results: A total of 1072 deaths were recorded in EUSTAR. Causes of death and year of the death were available for 764 (71.3%) deaths: 80 deaths were recorded between 1995 and 2005, 262 between 2006 and 2008, 250 between 2009 and 2011 and 172 between 2012 and 2015. In the four time periods, lung fibrosis was the leading cause of deaths responsible for 18 to 22% of deaths. The frequency of deaths due to renal crisis significantly decreased over the 20 years from 5/80 (6.3%) in 1995-2005 to 1/172 (0.6%) in 2012-2015 (p=0.03), whereas the proportion of patients who died from cancer had a trend to increase over time (9/80 (11.3%) in 1995-2005 to 33/172 (19.2%) in 2012-2015) (p=0.06). There was no significant change over time regarding deaths secondary to lung fibrosis, pulmonary arterial hypertension (15% of deaths), heart involvement (12%), atherosclerosis (5%), infection (9%) or gastrointestinal involvement (4%).
Conclusions: In this study, we observed a change in the pattern of SSc-deaths over the past 20 years with a gradual increase in cancer-related deaths, whereas deaths secondary to renal crisis have become extremely rare.
P.193
The Eular Systemic Sclerosis Impact of Disease (Scleroid) Score – a New Patient-Reported Outcome Measure for Patients with Systemic Sclerosis – Preliminary Results from the Ongoing Validation Study
R. Dobrota1, M. Becker1, K. Fligelstone2, J. Fransen3, A. Kennedy4, Y. Allanore5, P. Carreira6, L. Czirjak7, C. Denton8, R. Hesselstrand9, G. Sandqvist9, O. Kowal-Bielecka10, M. Matucci Cerinic11, C. Mihai12, A. Gheorghiu12, U. Mueller-Ladner13, M. Vonk3, T. Heiberg14, O. Distler1
1 Department of Rheumatology, University Hospital Zurich, Zurich, SWITZERLAND, 2 FESCA, London, UNITED KINGDOM, 3 Department of Rheumatology, Radboud University Medical Center, Nijmegen, THE NETHERLANDS, 4 FESCA, Dublin, IRELAND, 5 Department of Rheumatology, University Paris Descartes and Cochin Hospital, Paris, FRANCE, 6 Division of Rheumatology, Hospital 12 de Octubre, Madrid, SPAIN, 7 Department of Immunology and Rheumatology, Faculty of Medicine, University of Pecs, Pecs, HUNGARY, 8 Centre for Rheumatology, Royal Free and University College London Medical School, Royal Free Campus, London, UNITED KINGDOM, 9 Department of Rheumatology, Lund University, Lund, SWEDEN, 10 Department of Rheumatology and Internal Medicine, Medical University of Bialystok, Bialystok, POLAND, 11 Department of Rheumatology, University of Florence, Florence, ITALY, 12 Department of Internal Medicine and Rheumatology, Cantacuzino Hospital, Carol Davila University of Medicine and Pharmacy, Bucharest, ROMANIA, 13 Department of Rheumatology and Clinical Immunology, Justus-Liebig University Giessen, Kerckhoff-Klinik, Bad Nauheim, GERMANY, 14 Department of Health and Social Sciences, Oestfold University College, Oslo, NORWAY
Introduction: Patient reported outcome measures (PROM) are acknowledged to have a key role for future clinical trials with new therapeutic approaches. Given the unmet need of a validated, comprehensive PROM in systemic sclerosis (SSc), the ScleroID questionnaire was developed by a team of patients with SSc and medical experts in the field. This is intended as a brief, disease-specific, patient-derived, disease impact score for research and clinical use in SSc. Here, we present the preliminary analysis from the ongoing ScleroID validation study.
Material and Methods: This EULAR-endorsed project involves 11 European expert SSc centers. Patients fullfilling the ACR/EULAR 2013 criteria were prospectively included since 05/16 in the ongoing observational cohort study. Patients filled in the novel ScleroID questionnaire, as well as selected comparators SHAQ, EQ5D, SF36. Additionally, they weighted the 10 dimensions of the ScleroID by distributing 100 points according to the perceived impact on their health. The final score calculation will be based on the ranking of the weights. The study includes a reliability arm (follow-up questionnaire 7-10 days from baseline), as well as a longitudinal arm, looking at sensitivity to change at follow-up visits after 6 and 12 months from baseline.
Results: As of 01/2017 the study cohort included 224 patients with valid baseline data, 44 also had a reliability visit and 6 a 6-months follow-up visit. 84.4% of patients were female, 54.4% had limited SSc, median age 58, and median disease duration 8 years. The highest preliminary median weights for ScleroID dimensions were for Raynaud, impaired hand function, fatigue and pain. Except for pain, these dimensions were also scored most highly in the ScleroID questionnaire at baseline.
As of 09/2017, 380 patients (76% of target) were enrolled into the study. A comprehensive pre-final analysis will be performed end of 2017.
Conclusions: The EULAR ScleroID score is a novel tool designed for use for scientific and clinical purposes to display the disease impact of SSc. In this preliminary analysis, Raynaud syndrome, impaired hand function, and fatigue were the main patient reported drivers of disease impact. Further recruitment and validation of this new instrument is ongoing.
P.194
Normalization of Acr Criss Numerator for Baseline Data Offers a Measure of Magnitude of Response: Results from a Real-Life Observational Study
G. Abignano, J. Blagojevic, G. Bagnato, S. Eng, M. Buch, P. Emery, F. Del Galdo
Leeds Institute of Rheumatic and Musculoskeletal Medicine, Leeds, UNITED KINGDOM
Introduction: The Composite Response Index in Systemic Sclerosis (CRISS) is a 2-step process for the probability of improvement of patients with dcSSC ranging from 0.0 (no improvement) to 1.0. Patients with decline in cardio-pulmonary-renal involvement are assigned score 0.0 in step 1. All remaining subjects are assessed for the differences (delta) in 5 domains (mRSS, FVC, patient (PT GA) and physician globals (MD GA), and HAQ-DI (CRISS numerator) and scored 0 to 1 according to the value of the ratio: numerator/1+ numerator.
Objective: Here we aimed to determine the value of CRISS numerator in assessing magnitude of response in dcSSC in an observational cohort (quantitative CRISS – qCRISS).
Material and Methods: Consecutive dcSSc patients were included in the study at a single centre. Clinical data were collected at baseline and 12 months and CRISS calculated using the published formula. To explore the quantitative value of the numerator, each of the 5 domains was corrected for their baseline value (e.g (12 months-baseline)/baseline = Delta % or δ%) while keeping their original relative weight in the formula. The weighted sum was then divided by the number of domains. The resulting quantitate CRISS formula resulted in (-0.81*δ%mRSS+ 0.21*δ%FVC-0.4*δ%PTGA-0.44*δ%MDGA-3.41*δ%HAQ-DI)/5. The quantitative CRISS was then compared with CRISS score.
Results: Thirty-one dcSSc patients were enrolled (12 M; mean age=50.3 ±11.5). 16 patients had CRISS = 0%. 15 patients had a positive CRISS ranging from 1% to 99%. qCRISS had a significant correlation with CRISS (Pearson R -0.378, p =0.0429) despite the low number of patients enrolled. 12/16 patients with CRISS =0% showed a negative qCRISS (negative response = worsening) ranging from -4% to -214%. 13/16 with positive CRISS showed a corresponding positive qCRISS ranging from 1% to 59%.
Conclusions: Normalization by baseline data within CRISS numerator offers a quantitative score to assess magnitude of response, considering the 5 domains and their relative weight within the original CRISS. The qCRISS measures magnitude of response rather than probability of response and includes the possibility of measuring worsening of disease. Application of this simple formula to the results of RCTs adopting CRISS as explorative efficacy objective will determine the validity of qCRISS in offering quantitative assessment of response in SSc .
P.195
Factors Influencing Patient Interest in Participating in an Online Self - Care Intervention: a Scleroderma Patient - Centered Intervention Network (Spin) Cohort Study
L. Kwakkenbos 1,2, J. Cumin2, M-E. Carrier2, I. Boutron3, S. Bartlett4, 5, V. Malcarne6, 7, L. Mouthon3, 8, W. Nielson9, 10, J. Welling11, B. Thombs1, 2
1 Department of Psychiatry, McGill University, Montreal, CANADA, 2 Lady Davis Institute for Medical Research, Jewish General Hospital, Montreal, CANADA, 3 Université Paris Descartes, Assistance Publique-Hôpitaux de Paris, Paris, FRANCE, 4 Department of Medicine, McGill University, Montreal, CANADA, 5 McGill University Health Center, Montreal, CANADA, 6 Department of Psychology, San Diego State University, San Diego, USA, 7 Joint Doctoral Program in Clinical Psychology, San Diego State/ University of California, San Diego, USA, 8 Service de Médecine Interne, Hôpital Cochin, Paris, FRANCE, 9 Department of Psychology, Western University, London, CANADA, 10 Lawson Health Research Institute, London, CANADA, 11 NVLE Dutch patient organisation for systemic autoimmune diseases, Utrecht, THE NETHERLANDS
Introduction: The SPIN Cohort was created to develop and test online self-care interventions for people living with scleroderma (systemic sclerosis, SSc). Patients in the observational Cohort complete assessments every 3 months, consent to be automatically assessed for eligibility when trials are conducted, and, if eligible, to be randomized to be offered one of SPIN’s interventions. In order to offer interventions to patients interested in using online self-help tools, a ‘signaling questionnaire’ was designed to identify patients who would be likely to accept an intervention offer. The signaling questionnaire inquiries about interest in 9 different interventions, each designed to address a different problem associated with SSc. It is not known, however, what factors influence patient interest in participating in a particular online intervention, and if intervention- specific signaling questions provide unique information or replicate broader characteristics, such as overall willingness to participate in any intervention or patient- reported self-efficacy. The objective of this study was to determine factors that explain responses to intervention-specific signaling items.
Material and Methods: Participants consisted of SPIN Cohort participants from Canada, the US, the UK and France who completed baseline questionnaires from March 2014 through June 2017. Signaling questions queried about interventions to address fatigue, hand function, sleep, emotions and stress, body image concerns, pain, self-efficacy for managing SSc, nutrition, and exercise, on a 0 (not likely at all) to 10 (very likely) scale. Linear regression analyses were conducted for each of the 9 signaling questions, separately. Predictor variables included demographic variables, general interest in online interventions (mean of the remaining signaling questions), patient-reported self-efficacy, and severity of symptom associated with the individual signaling question.
Results: A total of 964 participants completed all baseline measures and were included in analyses (116 men; 12%). Mean signaling question scores per item ranged from 5.1 to 7.0. General interest in online interventions was the strongest predictor for all individual signaling questions (standardized regression coefficient Beta from 0.61 (sleep) to 0.80 (self- management)). Smaller, but statistically significant, associations were found with the symptom associated with the respective signaling question for 7 of 9 signalling questions and with general patient self-efficacy for 6 of 9 signaling questions.
Conclusions: Findings suggest that the main factor influencing patients’ interest in participating in a disease specific online self-care intervention is their general interest in participating in interventions.
P.196
High-Throughput Quantitative Histology in Systemic Sclerosis Skin Disease Using Computer Vision
C. Correia1, R. Saber1, A. Hoffmann1, T. Wood2, M. Whitfield2, M. Hinchcliff1, J. Mahoney3
1 Northwestern University Feinberg School of Medicine, Chicago, USA, 2 Geisel School of Medicine at Dartmouth, Department of Molecular and Systems Biology, Hanover, USA, 3 University of Vermont, Department of Neurological Sciences, Burlington, USA
Introduction: Dermal punch biopsies are frequently obtained for clinical and research indications in patients with systemic sclerosis (SSc) yet there are no validated, automated systems to quantify inflammatory cell infiltrates, thickened collagen bundles, or abnormal adnexal structures using imaging of stained immunohistochemical sections of skin biopsies. Significant advances in computer vision called deep neural networks (DNNs) have demonstrated human-level pattern recognition abilities using mathematical transformations of input images that quantify hundreds of thousands of image features. Therefore, publicly available DNNs algorithms have the potential to radically augment current histological analyses using robust, reproducible, and high-throughput image feature quantification. We hypothesized that DNNs applied to sections of stained dermal biopsies from patients with SSc would be highly correlated with modified Rodnan skin score (mRSS) and skin gene expression.
Material and Methods: One rheumatologist performed local modified Rodnan skin score (mRSS) assessments of the non-dominant forearm (0-3) followed by two side-by-side 4mm dermal punch biopsy for six patients with SSc. Photomicrographs of 4µm sections of one biopsy stained with Masson trichrome were obtained using a Leico SCN400 slide scanner (Wetzlar, Germany). Slide images were analyzed using the AlexNet deep neural network using the Matlab Deep Learning toolbox. The other biopsy was used to measure gene expression by DNA microarray. Correlations between DNNs quantitative features, mRSS, and gene expression were determined. Functional gene networks were analyzed using the STRING database.
Results: We identified 90 DNNs quantitative image features that correlated significantly with mRSS (p < 0.05, Bonferroni-Holm correction). Using these features, biopsies clustered into three clusters corresponding to low (mean = 0.13), intermediate (mean = 0.91), and high (mean = 1.7) mRSS. Gene expression levels for 488 genes in the biopsies were significantly correlated with quantitative features (p < 0.05, Bonferroni-Holm correction). Among these 488 genes, 194 genes formed a large functional network in the STRING database. This network included genes associated with STAT3 signaling, ubiquitin mediated proteolysis, and spliceosome components, indicating that DNNs identify histological features associated with inflammation and cell metabolism.
Conclusions: This proof-of-principal study demonstrates that DNNs are sensitive to clinically relevant features of SSc skin and to the complex relationship between pathological gene expression and histopathology of affected skin. These results suggest that DNNs dramatically expand the quantifiable SSc phenome and that histological samples can now be incorporated into system-level models of SSc.
P.197
Clinical Characteristics and Outcome of Patients Presenting Anti Pm-Scl Antibodies in an Internal Medicine Unit
G. Chalhoub
Central regional Hospital of Mercy, Ars Laquenexy, FRANCE
Introduction: We were interested in sharing our experience regarding clinical characteristics and outcome of patients presenting anti PM-Scl antibodies in our internal medicine unit.
These antibodies are described in systemic sclerosis, myositis or overlap syndromes.
Material and Methods: This is a retrospective analysis of patients’ files presenting either Scleroderma and or polymyositis performed over a 10 years follow up period (2007-2017).
This analysis includes 47 patients with Scleroderma and 15 autoimmune polymyositis (50 women and 12 men). The age average was 56.5 years.
All patients presented antinuclear antibodies. An anti ENA activity was observed in 60 cases and anti PM-Scl antibodies was noted in 4 female patients.
All the 4 patients with anti PM-Scl antibodies presented a Raynaud’s syndrome, arthritis and or arthralgia, a sclerodactily and 2 of them presented diffuse facial talengectasic lesions.
Elevated Creatinine phosphokinase was noted in 3 cases. Anticentromere antibodies was positive in 1 patient, 2 patients with DNA antibodies, 2 patients with monoclonal gammopathy of unknown significance (MGUS) and one patient presented multiple autoimmunity syndrome(systemic lupus erythematosis, scleroderma, hemolytic anemia and the all revealing an underlying Hodgkin lymphoma).
One patient presented an interstitial pulmonary disease (IPD).
Results: The 4 patients received calcium channel blockers, 2 patients received an immuno-suppressive treatment (Mycophenolate Mofetil) and one patient treated with corticoides and intensive chemotherapy for her Hodgkin lymphoma.
Clinical improvement was noted in all patients especially the rheumatic and cutaneous signs. The patient with Hodgkin lymphoma is still in remission.
The patient with the MGUS and IPD developed recently a low grade Waldenström disease, leading to a progressive withdrawal of her immunosuppressive treatment.
Conclusions: Our small series with anti-PM-Scl antibodies is concordant with that of the literature since anti-PM-Scl antibodies have been found to be of low prevalence and most often associated with non evolutive prognosis.
Our study reveals that the anti-PM-Scl antibodies predispose to sclerodermal manifestations rather than myositic signs.
The relation between PM-Scl antibodies and MGUS is not yet elucidated. This association may predispose to rapid evolution towards malignant lymphoproliferation. More studies must be performed to understand the relationship between both of them.
P.198
Caregiver, Care Recipient, and Caregiving Factors Associated with Symptoms of Depression Among Informal Caregivers of People Living with Systemic Sclerosis
M. Cañedo Ayala1, D.B. Rice 1,2, B. Levis 1,3, M-E. Carrier1, J. Cumin1, V. Malcarne 4,5, M. Hagedoorn6, S.S.C. Caregiver Committee1, B.D. Thombs 1,2,3,7
1 Lady Davis Institute for Medical Research, Jewish General Hospital, Department of Psychiatry, Montreal, CANADA, 2 McGill University, Department of Psychology, Montreal, CANADA, 3 McGill University, Department of Epidemiology, Biostatistics, and Occupational Health, Montreal, CANADA, 4 San Diego State University, Department of Psychology, San Diego, USA, 5 San Diego State University and the University of California, San Diego Joint Doctoral Program in Clinical Psychology, San Diego, USA, 6 University of Groningen, Department of Psychology, Groningen, THE NETHERLANDS, 7 McGill University, Departments of Psychiatry; Medicine; and Educational and Counselling Psychology, Montreal, CANADA
Introduction: Very little research has examined the experiences of informal caregivers of people living with systemic sclerosis (SSc). Informal caregivers are family members or friends who provide unpaid care for people with a health condition. Caregiving has been associated with a high level of burden and reduced mental health in common chronic diseases. Our study aimed to identify factors that are associated with depressive symptoms among informal caregivers of people with SSc, including caregiver characteristics, care recipient characteristics, and caregiving-related factors.
Material and Methods: An online survey was developed based on input from focus groups and collaborators. The survey was advertised to caregivers through patients enrolled in the Scleroderma Patient-centered Intervention Network Cohort and through SSc patient organizations. The survey was available to complete from December 2016 to June 2017 via Qualtrics, an online survey software. Eligible respondents were informal caregivers of people with SSc who were 18 years or older and fluent in English or French. The online survey gathered demographic information, caregiver burden through the 12-item Zarit Burden Interview, and depressive symptoms with the Patient Health Questionnaire-8. Multiple linear regression was used to assess the independent associations of caregiver (age, gender, years of education, current occupation, relation to care-recipient), care recipient (age, SSc subtype) and caregiving-related variables (hours of care per week, caregiver burden) with depressive symptoms.
Results: A total of 202 caregivers (79 women, 123 men) completed the survey and were included in analyses. The mean age was 57.2 years (standard deviation = 14.4). Most caregivers were partners (72.3%) or children (11.9%) of the person with SSc for whom they provided care. The majority of caregivers were either employed (47.0%) or retired (39.6%). The mean PHQ-8 score was 4.6 (standard deviation = 5.4). Controlling for other variables in the model, self-reported caregiver burden (standardized regression coefficient, beta (β = 0.54, p = 0.001) and hours of care per week (β = 0.17, p = 0.005) were significantly associated with more severe depressive symptoms. No other variables were significantly associated with depressive symptoms in the multivariate regression model.
Conclusions: Greater caregiver burden and more hours spent providing care per week were independently associated with symptoms of depression among a sample of caregivers of persons diagnosed with SSc. Programs designed to reduce caregiver burden in SSc should be developed and tested to address caregiver burden.
P.199
Acute Hospital Admissions in Patients with Systemic Sclerosis
J. Caetano1, L. Boavida1, M. Amaral1,2, S. Oliveira1, J.D. Alves 1, 2
1 Systemic Autoimmune Diseases Unit, Department of Medicine IV, Fernando Fonseca Hospital, Amadora, PORTUGAL, 2 CEDOC / NOVA Medical School, Lisbon, PORTUGAL
Introduction: Systemic sclerosis (SSc) is associated with significant high morbidity and mortality rates. Multiple studies have analysed predictors of morbidity and death in SSc, with interstitial lung disease (ILD) and pulmonary hypertension (PH) being the worst prognostic factors. There are very few reports evaluating acute hospital admission patterns in SSc, other than in Intensive Care Units. The purpose of this study is to analyse the causes of acute hospitalizations and predictors of in-hospital mortality in SSc.
Material and Methods: Retrospective review of all acute hospital admissions of SSc patients fulfilling the 2013 EULAR/ACR Classification Criteria, from a single referral center cohort, between 2010-2016; data were obtained by medical records review. T-test and Chi-square test were used to compare binary variables. Logistic regression analyses were performed to identify factors associated with hospital admissions and mortality.
Results: From a cohort of 64 patients, 38 (59%) were acutely hospitalized, comprising a total of 104 admissions. 82% were female, 34% with diffuse cutaneous SSc, mean age at the first admission of 54±16years, and mean disease duration of 5±6years. 58% (n=22) had ILD, 16% (n=6) had severe bowel involvement, 13% (n=5) had PH, 10.5% (n=4) had cardiac SSc and 3% (n=1) had SSc renal crisis; 74% (n=28) of the patients were under immunosuppressive therapy.
The principal reason for hospitalization was infection (27%, n=28) particularly pneumonia (n=15) and septic arthritis/soft tissue infections (n=7). 26 of these patients (93%) were under immunosuppression. The other main reasons for admission were cardiac complications (24%, n=25), including PH (n=6), worsening Raynaud’s phenomenon with digital ulcers (15%, n=16) and progression of ILD (11.5%, n=12). Surgical admissions were less frequent (7%, n=7). ILD was the only baseline clinical characteristic associated with acute hospitalization (OR 8.67, 95%CI 7.7-29.7, p=0.003).
There were 4 deaths (in-hospital mortality rate of 10.5%), 1 due to pneumonia, 1 due to malignancy and 2 due to heart failure. The presence of PH associated with a 10 times increased odds of in-hospital mortality (OR 10.2, 95% 2.3-34.0, p=0.017). Gender, age, time since disease onset, cutaneous disease subtype, autoantibodies, immunosuppression, presence of infection and other baseline organ involvement did not associate with mortality.
Conclusions: Although a frequent reason for acute admission, infection did not compromise the prognosis of SSc during acute hospitalizations. Supporting previous studies in non-hospitalized SSc patients, ILD and PH are the major predictors of poor outcomes, enhancing the importance of finding new therapeutic targets for these disease-related complications.
P.200
Mental Health Care in Systemic Sclerosis: Rates of Utilization and Associated Factors in the Scleroderma Patient-Centered Intervention Network Cohort
K. Becetti1, L. Kwakkenbos 2,3, M. Carrier2, J.K. Gordon1, J. Nguyen1, C. Mancuso1, B.D. Thombs 2,3, R.F. Spiera1, SPIN Investigators
1 Hospital for Special Surgery, New York, USA, 2 Lady Davis Institute for Medical Research, Jewish General Hospital, Montreal, Quebec, CANADA, 3 McGill University, Montreal, Quebec, CANADA
Introduction: Systemic sclerosis (SSc) is associated with high rates of depression, anxiety, and body image distress. Interventions to address the disease’s psychosocial impact are recommended as an essential aspect of care. However, mental health care practices are understudied in SSc. In this study, we aimed to explore the rate of mental health services (MHS) use among patients with SSc and evaluate demographic, psychological, and disease-specific factors associated with MHS utilization.
Material and Methods: We included patients with SSc enrolled in the Scleroderma Patient-centered Intervention Network (SPIN) Cohort. Medical variables were provided by enrolling physicians. Patients completed demographic variables and indicated whether they had seen a health professional to address a mental health concern in the preceding 3 months. They also completed questionnaires evaluating symptoms of disability and psychosocial distress. The rate of MHS use and type of MHS provider were determined for the entire cohort and by strata of depression symptom scores (Patient Health Questionnaire [PHQ-8]). Patients who used MHS were compared to those who did not and multivariable logistic regression was used to identify variables independently associated with MHS utilization.
Results: The analysis included 1000 patients with a mean (± standard deviation) age of 55.2 ± 12.1 years and disease duration of 11.6 ± 8.9 years. 87% were females and 41% had diffuse SSc. 20% had moderate depression symptoms (PHQ-8 10-15) and 2% had severe depression symptoms (PHQ-8 greater than 20). Only 20% of the entire cohort, 33% of the patients with moderate depression, and 45% of those with severe depression used MHS in the preceding 3 months. General practitioners were the most common providers of MHS (59%), followed by psychologists (21%), psychiatrists (13%), and rheumatologists (16%). MHS use was independently associated with being on disability (odds ratio [OR] 2.50, 95% confidence interval [CI] 1.33-4.69), having earlier disease (OR 0.97, 95% CI 0.95-0.99), esophageal symptoms (OR 2.40, 95% CI 1.14-5.06), and higher depression (OR 1.05, 95% CI 1.00-1.10) and anxiety (OR 1.05, 95% CI 1.02-1.08) symptom scores.
Conclusions: In this large international SSc cohort, 20% of all patients (and less than 1/3 of patients with moderate-severe depression symptoms) received any mental health care in the preceding 3 months. Of these, only 34% received care from a mental health specialist. MHS use was associated with factors previously shown to correlate with psychological distress in SSc. Additional studies are needed to evaluate the mental health care needs of SSc patients and determine barriers to MHS utilization.
P.201
Skin Biopsies in Patients with Systemic Sclerosis: a Retrospective Cohort Study
I. Atzeni1, A. Eman Abdulle1, J. Westra2, A.J. Stel2, D.J. Mulder1
1 University Medical Center Groningen & Internal Medicine, Groningen, THE NETHERLANDS, 2 University Medical Center Groningen & Rheumatology and Clinical Immunology, Groningen, THE NETHERLANDS
Introduction: In 2013, new classification criteria for systemic sclerosis (SSc) have been published, which include criteria for skin involvement as well as several other factors. Therefore, the presence of overt skin involvement is not mandatory anymore for the diagnosis of SSc. Although this is not common practice anymore, the clinician may choose to perform a skin biopsy when diagnostic uncertainty exists. We assessed for which indications skin biopsies were performed in our center, their outcomes and final diagnosis.
Material and Methods: In our tertiary referral center, all consecutive patients classified as SSc, MCTD or the suspicion of secondary Raynaud’s were retrospectively assessed for the presence of skin biopsy results from 1997 to 2017. A positive skin biopsy was defined as a definite diagnosis from the pathologist. Possible scleroderma was defined as the suspicion of scleroderma like changes without all characteristic histopathological changes such as hyalinised collagen, myofibroblast predominance or an increased epidermal thickness.
Results: In total, 535 patients were assessed, in whom 134 (25%; mean age 48 (±17), SSc: 87 (66%), MCTD: 25 (18%), unclassified: 22 (16%)) a skin biopsy had been taken at least once. Of all skin biopsies, in 64 (47%) the indication was confirming the clinical suspicion of scleroderma. Other CTD-related indications included: graft vs host disease (GVHD, 2%), calcinosis (2%), vasculopathy (6%), (dermato)myositis (4%), and lupus (4%). In 47 patients (35%), the indication was not SSc related. In 30 (47%) of the patients in whom the indication for skin biopsy was confirmation of SSc, clear histopathological changes were seen matching scleroderma and in 9 (14%) scleroderma was suspected. In 5 (8%) patients, histopathology was compatible with morphea and in 4 (6%) with other autoimmune diseases. In the remaining 16 (23%) patients, histopathology showed a different diagnosis in 11 (17%) and in 5 (8%) the results were normal.
Conclusions: Although the diagnosis of SSc can be made on a clinical basis, skin biopsies have been performed relatively regularly in our hospital in the past 20 years. Importantly, the diagnosis scleroderma was confirmed in the majority of the cases and the yield of an alternative diagnosis was low. Although these are only preliminary results and additional patient characteristics need to be assessed, they underline that diagnosis of SSc should be primarily made on a clinical basis and that skin biopsies should only be taken when diagnostic uncertainty is present.
P.202
Managing Systemic Sclerosis: Assessing the Educational Needs of Rheumatologists
Z. Ahmad 1,2, 3, S. Johnson 1,2, 3
1 Sinai Health System - Department of Medicine, Toronto, CANADA, 2 University Health Network - Department of Medicine, Toronto, CANADA, 3 University of Toronto - Department of Medicine, Toronto, CANADA
Introduction: Systemic sclerosis (SSc) is an uncommon, complex and heterogeneous condition, making it challenging to manage. Individual rheumatologists see relatively few cases and patient surveys identify numerous gaps in clinical care. There are no published data on the educational needs of rheumatologists caring for patients with SSc. We aimed to determine rheumatologists’ self-rated knowledge and learning needs.
Material and Methods: Survey questions were adapted from the EULAR Recommendations for the Treatment of SSc with reference to patient-identified care gaps. The survey was conducted on paper and on SurveyMonkey (a cloud-based online survey development software program). The target audience was Ontario rheumatologists, serving a population of 13.6 million. We sought to explore self-reported knowledge, experience, attitudes and perceived barriers in caring for SSc patients. Physician demographics and preferred educational methods were also collected. Gaps between perceived and desired knowledge were calculated to identify the greatest unmet learning needs.
Results: One hundred and eighteen responses were received with a response rate of 54%. The greatest unmet learning needs were seen in the management of sexual dysfunction (average gap of 1.4 on a 5-point scale), pulmonary hypertension (1.1), interstitial lung disease (1.0) and gastrointestinal manifestations of the disease (1.0). The smallest learning gap concerned screening recommendations (0.7). 19% of rheumatologists agreed with the statement “Scleroderma is an untreatable disease.” Agreement with this statement was highest (33%) among rheumatologists who treat relatively small numbers (1-10) of scleroderma patients.
Conclusions: We have identified several unmet learning needs regarding the management of SSc among rheumatologists. These can be used to inform future educational resources and programs for rheumatologists regarding SSc and to direct further research into their needs.
P.203
Correlation of the American College of Rheumatology Provisional Composite Response Index in Systemic Sclerosis with Serum Biomarkers of Fibrogenesis in an Observational Cohort
G. Abignano 1-3, J. Blagojevic 1,2,4, S. Eng 1,2, M. Buch 1,2, P. Emery 1,2, D. Khanna5, F. Del Galdo 1,2
1 Leeds Institute of Rheumatic and Musculoskeletal Medicine, University of Leeds, Leeds, UNITED KINGDOM, 2 Leeds Biomedical Research Centre, Leeds Teaching Hospitals NHS Trust, Leeds, UNITED KINGDOM, 3 Rheumatology Institute of Lucania (IReL), Rheumatology Department of Lucania, Potenza, ITALY, 4 Department of Experimental and Clinical Medicine, University of Florence, Florence, ITALY, 5 University of Michigan Scleroderma Program, Ann Arbor, USA
Introduction: The CRISS is a composite index of response in diffuse cutaneous systemic sclerosis (dcSSc).It is a 2-step process for the probability of improvement ranging from 0.0 (no improvement) to 1.0. Two independent studies including in total 464 patients from 6 different centres have shown that skin, lung and overall fibrosis correlate with three serum biomarkers PIIINP, TIMP-1 and HA, either singularly or combined in the ELF Test algorithm. Here we aimed to determine whether CRISS correlated with the serum concentration of one or more of the ELF biomarkers and explore the scope to build a combined score with better performance in measuring the probability of clinical response in dcSSc.
Material and Methods: Consecutive dcSSc patients were included in the study at a single centre. Clinical data and serum were collected at baseline,12 and 24 months. CRISS, ELF score and correlation between them were calculated at the same time points. Comparison between two groups and correlation were performed using Mann-Whitney and Spearman’s tests, respectively.
Results: Thirty-one dcSSc patients were enrolled (12 M; mean age=50.3 ±11.5 years). CRISS at 12 months was 0% in 19 patients, whereas in the remaining 12 patients it ranged from 0.1 to 1.0 (median=0.35). Five out of the 12 CRISS “responders” had a CRISS 24-12>0.0, the remaining 7 had no further response (CRISS=0). Overall CRISS 24-0 was>0.0 in 16 patients (median=0.065,range=0.01-0.93). No clinical features at baseline were significantly different in responders vs non-responders at 12 or 24 months, including mRSS, FVC%,DLCO%, autoantibody profile, age, disease duration, Medsger Severity Score,CRP (p>0.05 for all). TIMP-1 concentration at baseline was significantly lower in patients with CRISS>0 vs.CRISS=0 (218.5 vs 265.9 respectively, p=0.03), similar trend was observed for TIMP-1 at 12 months and CRISS 24 months. Accordingly, TIMP-1 at baseline or 12 months showed a statistically significant correlation with CRISS 24 months (R=-0.389 and -0.374, respectively; p<0.05 for both).
Conclusions: This is the first evaluation of CRISS in an observational setting. Despite single centre setting and low number, we show that in any 12 months interval a proportion between 38 and 51% of patients show a CRISS>0. Whereas only 6 to 22.5% of patients showed a CRISS>0.10. None of the routinely used clinical parameters can predict CRISS at 12 months whereas TIMP-1 concentration at baseline is significantly lower in the responders. This needs to be explored in additional cohorts and opens the possibility to include serum biomarkers of fibrogenesis within a combined response index for SSc.