Abstract
Background
Secondhand smoke (SHS) likely provides additional exposure to nicotine and toxins for smokers, but has been understudied. Our objective was to determine whether SHS exposure among smokers yields detectable differences in cotinine levels compared with unexposed smokers at the population level.
Methods
Using the US National Health and Nutrition Examination Survey (NHANES) for the years 1999–2012, we compared serum cotinine levels of 4547 current adult cigarette smokers stratified by self-reported SHS exposure sources (home and/or work) and smoking intensity. A weighted multivariable linear regression model determined the association between SHS exposure and cotinine levels among smokers.
Results
Smokers with SHS exposure at home (43.8%) had higher cotinine levels (β=0.483, p≤0.001) compared with those with no SHS exposure at home after controlling for the number of cigarettes smoked per day and number of days smoked in the previous 5 days, survey year, age, gender and education. Smokers with SHS exposure at work (20.0%) did not have significantly higher cotinine levels after adjustment. The adjusted geometric mean cotinine levels of light smokers (1–9 cigarettes per day) with no SHS exposure, exposure at work only, home only, and both home and work were 52.0, 62.7, 67.2, 74.4 ng/mL, respectively, compared with 219.4, 220.9, 255.2, 250.5 ng/mL among moderate/heavy smokers (≥10 cigarettes per day).
Conclusions
Smokers living in residences where others smoke inside the home had significantly higher cotinine levels than smokers reporting no SHS exposure, regardless of individual smoking intensity. Future research should target the role that SHS exposure may have in nicotine dependence, cessation outcomes and other health impacts among smokers.
INTRODUCTION
Efforts to reduce exposure to secondhand smoke (SHS) at home and in the workplace in the USA have benefitted non-smokers as well as smokers.1 Though declining in the USA, SHS exposure remains an important cause of preventable disability and early death responsible for approximately 41 000 deaths among US non-smoking adults each year.2 There is no safe level of exposure to SHS, which causes immediate deleterious effects on cardiovascular function and is a cause of coronary heart disease among non-smokers.3 SHS contains more than 50 carcinogens, is a cause of lung cancer, and is suggestive of being on the causal pathway of various other types of cancer.3 The estimation of disease burdens from SHS conventionally only accounts for the health effects on non-smokers but rarely considers its impacts on smokers. Since smokers already experience higher doses of nicotine and other toxins from active smoking than non-smokers exposed to SHS, the potential effect of additional exposure due to SHS among smokers is often overlooked and may even be assumed by many to be trivial. While the deleterious health effects of SHS exposure among smokers remain understudied, there has been evidence showing that SHS exposure at home is associated with higher rates of poor respiratory symptoms, medical consultations and hospitalisation among current smokers.1 4 5 Given the established evidence of dose–response relationships, both in amount smoked and lifetime duration, between active smoking and various diseases and poor health outcomes,6 it is plausible that the increased dose of exposure due to SHS among smokers could add to such disease burdens.2
The SHS in a smoker’s environment may directly or indirectly maintain nicotine dependence, encourage active smoking and impede cessation. SHS exposure at home has been shown to be independently associated with increased nicotine dependence among smokers.7–9 Nicotine inhaled from SHS travels to the brain where it occupies nicotinic acetylcholine receptors,10 which suggests that SHS exposure may facilitate the development and maintenance of nicotine dependence among smokers through a similar biological pathway as active smoking. Moreover, SHS provides visual and olfactory cues that prompt active smoking which sustains nicotine dependence.11 In terms of cessation, there is growing evidence that exposure to SHS among smokers is associated with lower intention to quit, fewer quit attempts and lower odds of achieving cessation compared with smokers unexposed to SHS.7 12 Therefore, determining if SHS increases nicotine uptake among smokers warrants further study.
The amount of SHS present in the environment in which smokers live and work may vary widely and its effect on cotinine levels is not fully understood. Cotinine, a metabolite of absorbed nicotine, serves as a biomarker of tobacco smoke exposure regardless of whether the source of smoke is mainstream (the smoke inhaled and then exhaled) or sidestream (the smoke produced by the ignited end of a combustible cigarette). Cotinine is a strong indicator of nicotine dependence.13 A tobacco industry study in the 1990s estimated that smokers were 21.2 times more exposed to SHS (which included the smoker’s own sidestream smoke), as measured by airborne nicotine, compared with non-smokers.14 Another study reported that among US daily smokers, living with one or more smokers who smoke inside the home was associated with increased serum cotinine levels but exposure to SHS in the workplace was not associated with an increase in cotinine levels.15 In contrast, a recent study of bar and nightclub employees who smoke reported that workplace air nicotine concentration was associated with hair nicotine levels, while living with another smoker was not.16 Similarly, living with a smoker who smokes inside the home was not associated with serum cotinine levels after adjusting for recency of smoking, time to first cigarette of the day, cigarettes per day and demographic characteristics among US adolescent current smokers.17 While one previous study assessed the effect of SHS exposure at home and workplaces on cotinine levels among daily smokers,15 no previous studies have examined that effect specifically among all smokers (including light/non-daily smokers), nor determined whether SHS exposure at home and workplaces results in higher cotinine levels among adult current smokers after controlling for smoking intensity and other covariates. In light of these contradictory findings, more studies are needed to determine if SHS exposure results in measurable and meaningful differences in nicotine uptake and exposure to toxins among smokers.
The objective of this study was to determine whether SHS exposure at home or/and workplaces results in detectable differences in serum cotinine levels among adult current smokers after controlling for smoking intensity, smoking frequency and other confounders.
METHODS
Data source
The National Health and Nutrition Examination Survey (NHANES) is a nationally representative sample of the US civilian non-institutionalised population administered by the National Center for Health Statistics (NCHS). The Continuous NHANES has been ongoing since 1999 with sampling occurring in 2-year survey cycles. The survey consists of interviews at home followed by a physical examination and a second interview that occur 2–4 weeks after the home interview either at a doctor’s office or mobile clinic. Laboratory work, including a blood draw used to determine serum cotinine levels, occurs at the time of physical examination. We merged seven cross-sectional survey cycles, or 14 years of NHANES data (1999–2012) for this analysis. Sampling weights are provided with the publicly available de-identified data sets since certain subgroups are oversampled (≥60 years and minority racial/ethnic groups). The Institutional Review Board of the NCHS approved all NHANES study protocols.
Inclusion and exclusion criteria
Included in this analysis were current cigarette smokers aged 20 years and older, defined as the survey participants who had smoked at least 100 cigarettes in their lifetime that captured established smoking behaviour as used by the centres for Disease Control and Prevention (CDC)18 and had smoked cigarettes at least one time in the 5 days prior to the examination interview when blood was drawn for cotinine measurement (see figure 1). The exclusion criteria included concurrent use of cigars, pipes, smokeless tobacco or other products containing nicotine (ie, nicotine gum, nicotine patch or other nicotine product) in the previous 5 days as these would have influenced cotinine levels, and missing cotinine measurements. We excluded households reporting only one household member who smokes inside the home from the analyses as they may not have had any additional sources of SHS since there was no way to distinguish the survey respondent who smokes from the smoker who smokes inside the home.
Figure 1.
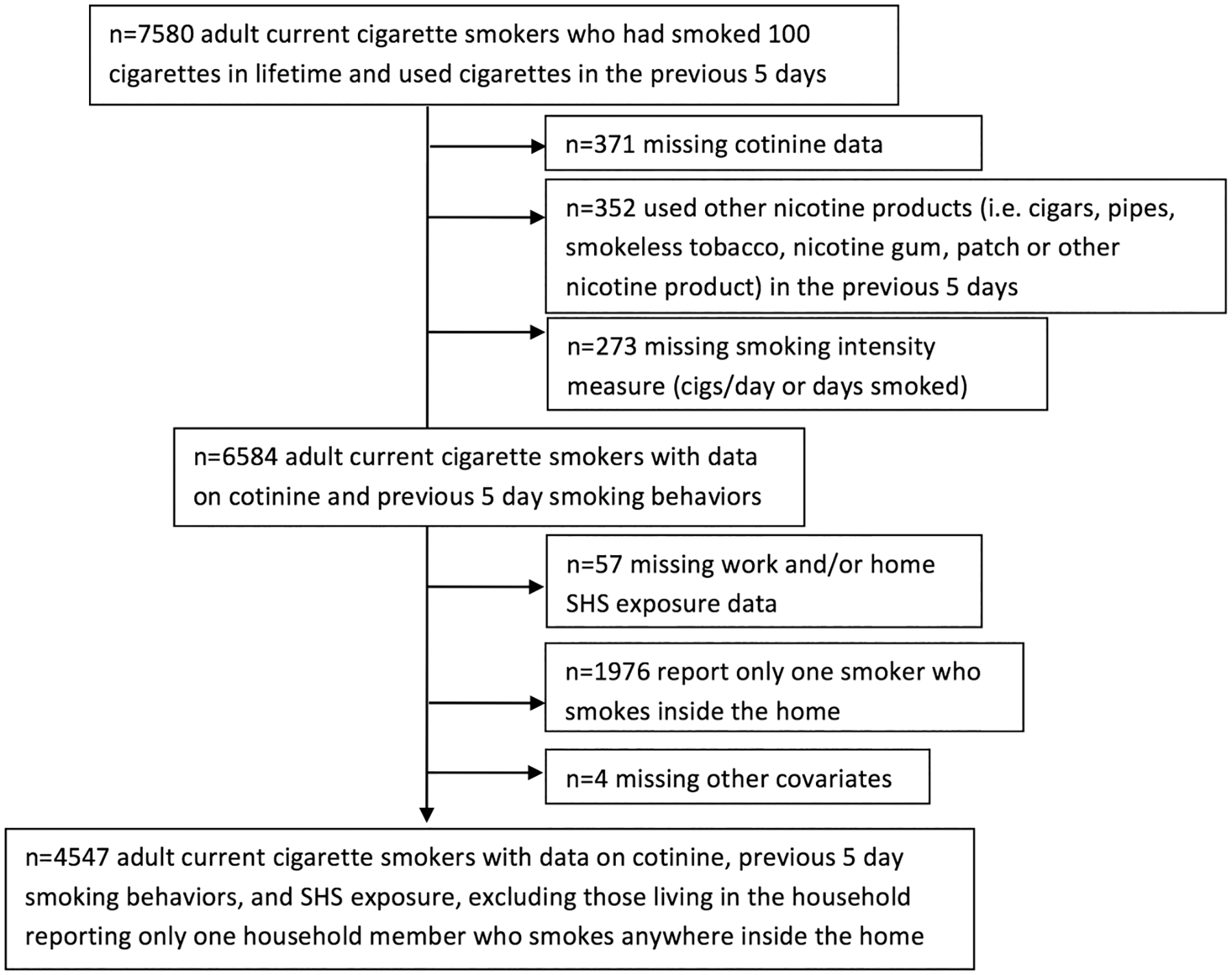
Sample selection criteria for selecting cigarette smokers with SHS exposure data, NHANES 1999–2012 (NHANES, National Health and Nutrition Examination Survey; SHS, secondhand smoke).
Smoker and smoke exposure classification
Serum cotinine was used as our outcome variable to measure total tobacco smoke exposure from both active smoking and SHS exposure. Laboratory methods for gathering, storing and processing of blood samples from participants were developed by the CDC and are described on the NHANES website (http://www.cdc.gov/nchs/nhanes.htm).
SHS exposure at home and work were our independent variables of interest. Since cotinine does not differentiate between active and SHS exposure, NHANES questionnaire items allowed us to determine SHS exposure at home or workplaces among smokers. With regard to home exposure, participants were asked “Does anyone who lives here smoke cigarettes, cigars, or pipes anywhere inside this home?” If the answer was “YES”, a subsequent question asked the number of smokers who smoke inside the home. Respondents who live in a household with at least two household members smoking inside the home were classified as being exposed to SHS in the home. Workplace exposure to SHS at the participant’s primary place of employment was measured by the question “How many hours per day can you smell the smoke from other people’s cigarettes, cigars, and/or pipes?” In the 2011–2012 survey cycle, the previous question was discontinued and replaced with “During the past 2 weeks, has anyone smoked cigarettes, cigars or pipes in the area in which you work?” Respondents from the 1999–2010 surveys who reported smelling the smoke for 1 h or more per day from other people’s cigarettes, cigars and/or pipes at work, and respondents from the 2011–2012 survey who reported someone smoking in their area of work in the past 2 weeks, were categorised as being exposed to SHS at work. Since only participants with current jobs were asked about workplace exposure, unemployed participants were categorised as having no workplace exposure.
Covariates
As predictors or potential confounders of cotinine levels, time since last cigarette (ie, day of the examination vs 1–5 days prior to the examination), smoking intensity (ie, light smokers using 1–9 cigarettes per day on average over the previous 5 days vs moderate/heavy smokers using 10+ cigarettes per day on average over the previous 5 days), smoking frequency (ie, the number of days smoked in previous 5 days), race (ie, non-Hispanic Caucasian, non-Hispanic African-American, Mexican American, other Hispanic, other race/ethnicity), educational attainment (ie, less than high school, high school graduate or equivalent, some college or above), age(continuous), gender and survey year (range 1–7 with 1=1999–2000 survey cycle and 7=2011–2012 survey cycle) were controlled for in the multivariable analysis. Poverty Income Ratio and marital status both had missing data (7.6% and 1.0% of the total sample size, respectively) and were added separately in multivariable analyses but neither was individually associated with cotinine levels and did not alter the associations between SHS and cotinine; therefore, they were not included in final multivariable models to optimise the sample size available. Employment status was not associated with cotinine levels in multivariable analysis and was excluded.
Statistical analysis
All the analyses were weighted using sampling weights from the NHANES to account for the survey design and oversampling of subgroups and were performed using SAS V.9.3 (SAS Institute Inc, Cary, North Carolina, USA). A multivariable linear regression model was used to determine the association between SHS exposure and cotinine levels among current smokers. Both SHS exposure variables, home and work, were included along with covariates in multivariable models. A significant interaction between home SHS exposure and the number of cigarettes smoked per day led us to stratify models by light and moderate/heavy smokers. Collinearity among covariates was assessed using tolerance values (defined as 1/variance inflation factor); no relationship between pairs of covariates was below our cut-off of 0.1. Using the results from our regression models, we used the LSMEANS statement to calculate the adjusted geometric means of the serum cotinine levels by SHS exposure source. These means were then compared using the Tukey-Kramer adjustment method to assess the pairwise relationships between SHS exposure source and non-exposure. Geometric means were used as a better estimate of central tendency due to the positively skewed distribution of cotinine levels in our sample.
RESULTS
During the years 1999–2012, the prevalence of US smokers who were exposed to SHS at home and/or work was 54.2% with 10.5% being exposed at workplace only, 34.2% at home only and 9.6% at both home and workplace. Compared with smokers unexposed to SHS, smokers exposed to SHS were more likely to be male (58.7% vs 54.8%; p=0.030), have lower educational attainment (30.3% vs 20.3% with less than a high school education; p<0.001; 35.6% vs 27.6% with high school degree or equivalent; p<0.001), and be non-Hispanic Caucasians (76.3% vs 68.9%; p≤0.001) or non-Hispanic African-Americans (10.7% vs 8.1%; p≤0.001; see table 1). There were no significant differences in age or household size between smokers with and without SHS exposure. In terms of smoking behaviour, smokers exposed to SHS smoked more cigarettes per day on average (16 vs 9; p≤0.001), smoked on more days in the previous 5 days (4.6 vs 4.1; p≤0.001), and were more likely to have smoked a cigarette on the same day as the medical examination interview when laboratory cotinine samples were obtained (78.9% vs 61.9%; p≤0.001). Smokers exposed to SHS at home were older and more likely to be female, while smokers exposed to SHS at work were younger and more likely to be male. Smokers exposed to SHS at work were more likely to report SHS exposure at home, and vice versa. SHS exposure at both home and work was more likely to be reported in earlier survey years.
Table 1.
Characteristics of cigarette smokers exposed and unexposed to SHS at home and workplace, USA, 1999–2012
| Characteristic | Overall (n=4547) M (SE) or per cent | No home or work exposure (n=2174) M (SE) or per cent | SHS exposure at home and/or work (n=2373) M (SE) or per cent | No home exposure (n=2602 M (SE) or per cent | SHS exposure at home (n=1945) M (SE) or per cent | No work exposure (n=3764) M (SE) or per cent | SHS exposure at work (n=783) M (SE) or per cent |
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Mean age | 40.5 (0.25) | 40.6 (0.36) | 40.4 (0.37) | 39.8 (0.34) | 41.4* (0.44) | 41.3 (0.29) | 37.5† (0.48) |
| Male | 56.9 | 54.8 | 58.7‡ | 59.0 | 54.3* | 52.9 | 72.8† |
| Education | |||||||
| Less than high school | 25.7 | 20.3 | 30.3‡ | 21.2 | 31.5* | 25.5 | 26.6 |
| High school graduate or equivalent | 31.9 | 27.6 | 35.6‡ | 28.0 | 37.1* | 31.7 | 33.1 |
| Some college | 42.4 | 52.1 | 34.1‡ | 50.8 | 31.5* | 42.9 | 40.3 |
| Race/ethnicity | |||||||
| Non-Hispanic white | 72.9 | 68.9 | 76.3‡ | 68.9 | 78.1* | 72.2 | 75.7 |
| Non-Hispanic black | 9.5 | 8.1 | 10.7‡ | 7.8 | 11.6* | 10.0 | 7.6 |
| Mexican American | 7.1 | 10.3 | 4.4‡ | 10.5 | 2.7* | 7.0 | 7.5 |
| Other Hispanic | 5.4 | 6.7 | 4.3‡ | 7.0 | 3.3* | 5.5 | 5.0 |
| Other/multiracial | 5.1 | 6.1 | 4.3‡ | 5.8 | 4.2* | 5.3 | 4.2 |
| Mean household size§ | 3.4 (0.04) | 3.3 (0.05) | 3.4 (0.05) | 3.4 (0.05) | 3.4 (0.06) | 3.4 (0.04) | 3.5 (0.07) |
| Mean survey year¶ | 4.0 | 4.3 (0.06) | 3.7‡ (0.10) | 4.2 (0.07) | 3.7* (0.12) | 4.1 (0.07) | 3.6† (0.13) |
| Smoking behaviours | |||||||
| Mean cigarettes per day in previous 5 days | 12.8 (0.29) | 9.0 (0.25) | 16.0‡(0.36) | 9.4 (0.25) | 17.2* (0.38) | 12.4 (0.29) | 14.3† (0.55) |
| Mean days smoked cigarettes in previous 5 days | 4.4 (0.03) | 4.1 (0.04) | 4.6‡ (0.02) | 4.1 (0.04) | 4.7* (0.02) | 4.4 (0.03) | 4.5 (0.04) |
| Most recent cigarette smoked on the day of examination | 71.1 | 61.9 | 78.9‡ | 62.8 | 81.8* | 71.1 | 71.0 |
| SHS exposure | |||||||
| SHS exposure at work | 20.0 | – | – | 18.6 | 22.0* | – | – |
| SHS exposure at home | 43.8 | – | – | – | – | 42.8 | 47.8† |
All percentages are weighted.
p<0.05 in pairwise comparison with no home exposure.
p<0.05 in pairwise comparison with no work exposure.
p<0.05 in pairwise comparison with no home or work exposure.
Household size only calculated on n=3958 since this variable was not collected in the 2011–2012 NHANES cycle.
Range 1–7 with 1=1999–2000 survey cycle and 7=2011–2012 survey cycle.
M, mean; NHANES, National Health and Nutrition Examination Survey; SHS, secondhand smoke.
Table 2 shows the adjusted and unadjusted associations between SHS exposure and cotinine levels. SHS exposure among smokers at work and home were both associated with higher cotinine levels compared with smokers without SHS exposure in unadjusted regression models (β=0.132, 95% CI 0.011 to 0.253; β=0.806, 95% CI 0.699 to 0.913, respectively). After controlling for all covariates, and including an interaction term between cigarettes per day and home SHS exposure, smokers who were exposed to SHS at home had higher cotinine levels compared with those without SHS exposure (β=0.483, 95% CI 0.353 to 0.614). The results from the separate multivariable regression models stratified by smoking intensity show that compared with those without home SHS exposure, the cotinine levels for those with SHS exposure at home were statistically significant among light smokers (β=0.239) and among moderate/heavy smokers (β=0.146); however, SHS exposure at work was not independently associated with an increase in cotinine levels among the light smoker group or the moderate/heavy smoker group.
Table 2.
Associations between secondhand smoke (SHS) exposure and serum cotinine level (ng/mL) among US adult smokers (ages ≥20), with stratification by smoking intensities, USA, 1999–2012
| All adult smokers (n=4547) | Light smokers* (n=2130) | Moderate/heavy smokers*(n=2417) | ||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted β (95% Cl) | p Value | Adjusted† β (95% Cl) | p Value | Adjusted† β (95% Cl) | p Value | Adjusted† β (95% Cl) | p Value | |
| SHS exposure | ||||||||
| SHS exposure at work (reference=none) | 0.132 (0.011 to 0.253) | 0.032 | 0.065 (−0.025 to 0.154) | 0.154 | 0.165 (−0.022 to 0.353) | 0.084 | −0.009 (−0.081 to 0.064) | 0.814 |
| SHS exposure at home (reference=none) | 0.806 (0.699 to 0.913) | <0.001 | 0.483 (0.353 to 0.614) | <0.001 | 0.239 (0.098 to 0.380) | 0.001 | 0.146 (0.083 to 0.208) | <0.001 |
| Smoking behaviours | ||||||||
| Mean cigarettes per day in previous 5 days (unit=1 cigarette per day) | 0.066 (0.060 to 0.072) | <0.001 | 0.038 (0.032 to 0.446) | <0.001 | – | – | – | – |
| Number of days smoked cigarettes in previous 5 days (unit=1 day smoked) | 0.810 (0.753 to 0.866) | <0.001 | 0.578 (0.507 to 0.649) | <0.001 | 0.582 (0.510 to 0.654) | <0.001 | 0.291 (0.045 to 0.538) | 0.021 |
| Most recent cigarette smoked on the same day of examination (reference=most recent cigarette smoked 1–4 days before the examination) | 1.508 (1.358 to 1.658) | <0.001 | 0.090 (0.021 to 0.201) | 0.112 | 0.254 (0.096 to 0.412) | 0.002 | 0.082 (−0.084 to 0.249) | 0.329 |
| Demographics | ||||||||
| Age (10 years interval) | 0.168 (0.130 to 0.206) | <0.001 | 0.059 (0.032 to 0.087) | <0.001 | 0.109 (0.061 to 0.158) | <0.001 | 0.038(0.017 to 0.059) | <0.001 |
| Gender (reference=male) | −0.005 (−0.095 to 0.084) | 0.906 | −0.055 (−0.128 to −0.018) | 0.137 | −0.086 (−0.239 to 0.068 | 0.273 | −0.084 (−0.133 to −0.029) | 0.003 |
| Education (reference=less than high school) | ||||||||
| High school graduate or equivalent | 0.028 to 0.063–0.119 | 0.545 | −0.009 (−0.081 to 0.062) | 0.793 | −0.001 (−0.177 to 0.177) | 0.997 | −0.011 (−0.067 to 0.046) | 0.713 |
| Some college | −0.369 (−0.482 to −0.257) | <0.001 | −0.103 (−0.169 to 0.037) | 0.002 | −0.108 (−0.250 to 0.034) | 0.136 | −0.084 (−0.160 to −0.008) | 0.032 |
| Race/ethnicity (reference=non-Hispanic white) | ||||||||
| Non-Hispanic black | 0.271 (−0.167 to 0.375) | <0.001 | 0.382 (0.307 to 0.456) | <0.001 | 0.471 (0.335 to 0.607) | <0.001 | 0.214 (0.141 to 0.287) | <0.001 |
| Mexican American | −1.418 (−1.621 to −1.215) | <0.001 | −0.574 (−0.731 to −0.416) | <0.001 | −0.685 (−0.894 to −0.476) | <0.001 | −0.184 (−0.297 to −0.071) | 0.002 |
| Other Hispanic | −0.733 (−0.951 to −0.516) | <0.001 | −0.246 (−0.405 to −0.087) | 0.003 | −0.331 (−0.567 to −0.094) | 0.007 | −0.015 (−0.099 to 0.068) | 0.715 |
| Mixed race/other | −0.384–0.639 to −0.129) | 0.004 | −0.128 (−0.284 to 0.028) | 0.106 | −0.273 (−0.561 to 0.014) | 0.062 | −0.007 (−0.073 to 0.087) | 0.870 |
| Interaction | ||||||||
| Cigarettes per day × home SHS exposure | – | – | −0.025 | <0.001 | – | – | – | – |
Bolded values represent significance of the p Value <0.05.
Light smokers smoked 1–9 cigarettes per day on average over the previous 5 days, moderate/heavy smokers smoked 10+ cigarettes per day on average over the previous 5 days.
Models adjusted for all covariates listed in the table as well as survey year (not shown).
The adjusted geometric means of cotinine levels among current smokers by SHS sources and smoking intensity are shown in table 3. Compared with the geometric mean of cotinine level for those with no home or work exposure (93.3 ng/mL), the geometric mean of cotinine level was significantly higher for those with SHS exposure at home only (123.2 ng/mL; p≤0.001) and SHS exposure at home and work (130.2 ng/mL; p≤0.001). When stratified by smoking intensity, the geometric means of cotinine levels were higher in smokers exposed to SHS at home only (67.2 ng/mL; p=0.015), and exposed to SHS at home and work (74.4 ng/mL; p=0.029), compared with those with no SHS exposure at home or work among both light smokers (52.0 ng/mL). The same pattern was true among moderate/heavy smokers with SHS exposure at home only (255.2 ng/mL; p≤0.001), and exposed to SHS at home and work (250.5 ng/mL; p=0.049), compared with those with no SHS exposure at home or work. The difference in the geometric means between those without SHS exposure at home and work and those exposed to SHS at work only were not statistically significant overall, or among light or moderate/heavy smokers.
Table 3.
Adjusted and weighted geometric mean of serum cotinine levels (ng/mL) by secondhand smoke (SHS) exposure source and smoking intensity among adult current smokers in the USA, 1999–2012
| No SHS exposure at home or work (n=2174) | SHS exposure at work only (n=428) | SHS exposure at home only (n=1590) | SHS exposure at home and work (n=355) | |
|---|---|---|---|---|
| Overall (all smoking intensity levels combined) Smoking intensity | 93.3 (87.1–100.0) | 106.0 (92.5–121.5) | 123.2*(114.1–133.1) | 130.2* (116.8–145.2) |
| Light smokers† | 52.0 (47.2–57.4) | 62.7 (51.3–76.5) | 67.2* (57.9–78.0) | 74.4* (58.2–95.2) |
| Moderate/heavy smokers† | 219.4 (204.9–235.1) | 220.9 (193.1–252.6) | 255.2*(236.1–275.8) | 250.5* (223.0–281.3) |
Adjusted for covariates used in multivariable linear regression models, stratified by smoking intensity, from table 2.
Pairwise t test yields significant difference in adjusted and weighted geometric mean cotinine level compared with those with no SHS exposure at home or work (p<0.05) for the same smoking intensity level.
Light smokers smoked 1–9 cigarettes per day on average over the previous 5 days, moderate/heavy smokers smoked 10+ cigarettes per day on average over the previous 5 days.
DISCUSSION
In our study, smokers who reported exposure to SHS smoke at home had higher overall nicotine uptake, measured by cotinine, than smokers reporting no exposure to SHS at home after controlling for other factors. That there are quantifiable differences in cotinine between those exposed and unexposed to SHS, even among smokers, adds biological evidence of added potential for harm among smokers with important health implications. To the best of our knowledge, our study is the first to reveal the effect of SHS on smoker’s cotinine levels at the population level after accounting for smoking intensity, other smoking behaviours and other factors.
SHS at home was independently associated with increased cotinine levels among both light smokers and moderate/heavy smokers. Although a saturation or plateau effect of cotinine with increasing nicotine uptake among adults has been described among adults who smoke approximately 15 cigarettes per day,19 SHS at home still accounted for an increase in cotinine levels among those who smoke 10 cigarettes per day or more.
SHS exposure among smokers in the home
Our study showed that more US smokers report exposure to SHS at the place of residence than in the workplace and that SHS exposure from inside the home had a greater effect on cotinine levels than SHS exposure at work. Smoke-free multiunit housing policies and voluntary smoke-free homes have been associated with less in-home SHS exposure among non-smokers.20 21 Restrictions on home smoking remain outside the purview of most current smoke-free legislation in the USA; thus for many, voluntary smoke-free homes are a primary mode of reducing SHS exposure in the home. Among smokers, voluntary smoke-free homes have resulted in higher quit rates and quit attempts among smokers, less likelihood of relapse among smokers who have quit, and less cigarette consumption among smokers.22–24 Our study may add biological mechanistic evidence that lower cotinine levels experienced by smokers living in smoke-free homes could influence or reinforce at least in part cigarette smoking reduction and cessation success among smokers with voluntary smoke-free homes, though more research warranted. Furthermore, smoking cessation programmes that are household/family based for multiple smokers may function not only through social support, but also through the removal of additional SHS exposures that lead to increased nicotine intake and behavioural cues. Therefore, non-smokers and smokers alike would benefit from voluntary smoke-free homes and multiunit housing policies to reduce SHS exposure.
SHS exposure among smokers in the workplace
Our study showed that while approximately one in five smokers reported SHS exposure at work, SHS exposure in the workplace was not independently associated with elevated cotinine levels among smokers after controlling for confounding factors. Therefore, currently, SHS exposure at home appears to be more salient to smokers’ cotinine levels. Our findings regarding work exposure on cotinine levels are consistent with results found elsewhere.15 SHS exposure at work was more likely to be reported in earlier NHANES survey years by participants in our study. Though unaccounted for in our analysis, occupation type and a variety of worksite policies and smoke-free laws for worksites by city and state in the USA have influenced exposure level.25 26 Such policies reflect a degree of public health success in that 28 states have implemented comprehensive smoke-free policies during the period of this study reducing worksite SHS exposure that have benefitted both smokers and non-smokers.27
Assessing SHS exposure among smokers
The challenge in assessing exposure to SHS may be greater among smokers than non-smokers. Non-smokers under-report exposure when comparing self-report with cotinine-measured exposure,28 and under-reporting SHS exposure could be even more common among smokers who are more accustomed to the sight and smell of cigarette smoke. The question used in NHANES to assess workplace SHS exposure between 1999 and 2010 asked if participants “smell the smoke from other people’s cigarettes, cigars, and/or pipes” while at work; assessing exposure based on smell only may explain why SHS exposure in the workplace was not independently associated with an increase in cotinine levels. With regard to measurement of SHS exposure in the home, the number of household smokers who smoke inside the home has been shown to be a strong measure of SHS previously29 and continued to differentiate cotinine levels among smokers even after accounting for smoking intensity in our study. Also, by excluding those with only one smoker who smokes inside the home (which may have been the self-same smoker) and defining SHS exposure as living in a home with at least two smokers who smoke inside the home, we increased our confidence that the elevated cotinine levels were at least in part from others’ SHS. At the same time, excluding smokers with only one smoker who smokes inside the home may have also resulted in an underestimation of SHS exposure in the home. Regardless, the overall amount of SHS exposure experienced by smokers in our study was likely underestimated as questions regarding SHS exposure experienced at locations other than home and work were not asked.
Limitations
Given the changes in SHS exposure among smokers, smoking intensity and the landscape of nicotine-containing products over the survey years, we controlled for survey year in the analyses but acknowledge that this may have resulted in an over adjustment for SHS at work compared with SHS at home since reductions in SHS were more pronounced in the workplace than at home. In addition, the different definitions of SHS exposure at work used in surveys from 1999 to 2010 and the 2011–2012 survey might have obscured the findings related to SHS exposure at work as the analyses combined different exposure scenarios, such as participants whose worksites permitted smoking in the earlier years versus those work in smoke-free worksites but expose to SHS at smoking breaks, which could not be accounted by the adjustment of the survey year in the analyses.
The magnitude of increase in adjusted geometric mean cotinine levels between smokers exposed to SHS at home and work compared with smokers unexposed was as high as 35 ng/mL (moderate/heavy smokers exposed at home only vs unexposed), an amount unlikely to be solely attributable to SHS exposure alone since non-smokers heavily exposed to SHS do not typically have cotinine levels greater than 10 ng/mL.30 Though we statistically controlled for cigarettes per day, smokers who report SHS exposures may unintentionally under-report their own smoking when triggered or reinforced by others’ smoking or being exposed to SHS. Other variation in individual smoking behaviour unmeasured in this analysis, such as depth of inhalation, may also account for some of this increase. In addition, alternative nicotine-containing products such as hookah and electronic cigarettes were not directly assessed and may have been an unmeasured source of nicotine. However, smokers who considered these products as ‘other nicotine products’ would have been excluded from our sample. Furthermore, we were unable to determine the degree to which a smoker’s own exhaled mainstream or sidestream smoke versus others’ SHS was responsible for the increases in cotinine. Smoker’s own sidestream or SHS may account for between 14% and 34% of their inhaled dose of benzo(a)pyrene (a constituent of cigarette smoke),31 though this may vary by individual depending on the environment that one smokes in and individual smoking behaviours.
Health policy and education recommendations
Given our findings of increased cotinine levels among smokers exposed to SHS, we suggest the following three policy considerations: (1) comprehensive smoke-free policies are still needed in 22 US states and would further protect non-smokers as well as smokers by eliminating smoking in all public indoor venues. Smoke-free policies have resulted in the adoption of voluntary smoke-free homes and would further protect non-smokers and smokers from additional exposure both at home and work; (2) our study underscores the importance of cessation for smokers and their cohabitants and peers that smoke, as only cessation can completely eliminate SHS. To this end, for cessation providers, more research on the clinical utility of SHS assessment among smokers to improve cessation outcomes could improve cessation rates; and (3) similarly, qualitative research has indicated that health education on the harm of SHS exposure should be directed at both non-smokers and smokers.32
CONCLUSION
The majority of US adult smokers live and/or work in locales where others smoke, which contributes a measurable and significant additional source of nicotine and toxin exposures. SHS exposure in the home environment was independently associated with higher cotinine levels for exposed smokers compared with smokers reporting no SHS exposure, irrespective of smoking intensity. As SHS can be a significant source of nicotine and toxins, even among smokers, public health efforts must continue to promote smoke-free homes and comprehensive worksite smoke-free policy. More research is needed on the role SHS may have in nicotine dependence, cessation outcomes and other health impacts among smokers.
What this paper adds.
While there is no safe level of cigarette smoke exposure, little attention has been given to the additional exposure that smokers receive from secondhand smoke. In a nationally representative US sample of over 4500 adult smokers, we detected higher cotinine levels among those exposed to secondhand smoke at home compared with smokers not exposed at home, independent of smoking intensity and other factors. Our findings add biological evidence that secondhand smoke exposure increases tobacco smoke exposure and nicotine uptake, as measured by cotinine levels, even among moderate/heavy smokers. Implications for tobacco control policy (eg, smoke-free homes among smokers and health education on secondhand smoke among smokers), nicotine dependence and smoking cessation treatment are further discussed in the paper.
Acknowledgements
The authors gratefully acknowledge the NHANES study participants for their participation.
Funding This work was supported by the National Cancer Institute grant number R25-CA113710, and the National Institute on Drug Abuse grant number P50-DA009253.
Footnotes
Competing interests None.
Ethics approval The Institutional Review Board of the National Center for Health Statistics.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement All data used for this analysis are publically available through the National Center for Health Statistics on the NHANES website (http://www.cdc.gov/nchs/nhanes.htm).
REFERENCES
- 1.Lam TH, Ho LM, Hedley AJ, et al. Secondhand smoke and respiratory ill health in current smokers. Tob Control 2005;14:307–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Max W, Sung HY, Shi Y. Deaths from secondhand smoke exposure in the United States: economic implications. Am J Public Health 2012;102:2173–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Office on Smoking and Health (US). The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and prevention (US), 2006. [PubMed] [Google Scholar]
- 4.Lai HK, Ho SY, Wang MP, et al. Secondhand smoke and respiratory symptoms among adolescent current smokers. Pediatrics 2009;124:1306–10. [DOI] [PubMed] [Google Scholar]
- 5.Wang MP, Ho SY, Lo WS, et al. Secondhand smoke exposure and health services use among adolescent current smokers. PLoS ONE 2013;8:e64322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.US Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014. [Google Scholar]
- 7.Okoli CT, Browning S, Rayens MK, et al. Secondhand tobacco smoke exposure, nicotine dependence, and smoking cessation. Public Health Nurs 2008;25:46–56. [DOI] [PubMed] [Google Scholar]
- 8.Wilson-Frederick SM, Williams CD, Garza MA, et al. Association of secondhand smoke exposure with nicotine dependence among Black smokers. Addict Behav 2011;36:412–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang MP, Ho SY, Lo WS, et al. Smoking family, secondhand smoke exposure at home, and nicotine addiction among adolescent smokers. Addict Behav 2012;37:743–6. [DOI] [PubMed] [Google Scholar]
- 10.Brody AL, Mandelkern MA, London ED, et al. Effect of secondhand smoke on occupancy of nicotinic acetylcholine receptors in brain. Arch Gen Psychiatry 2011;68:953–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sayette MA, Hufford MR. Effects of cue exposure and deprivation on cognitive resources in smokers. J Abnorm Psychol 1994;103:812–8. [DOI] [PubMed] [Google Scholar]
- 12.Wang MP, Ho SY, Lo WS, et al. Smoking family, secondhand smoke exposure at home, and quitting in adolescent smokers. Nicotine Tob Res 2013;15:185–91. [DOI] [PubMed] [Google Scholar]
- 13.Muscat JE, Stellman SD, Caraballo RS, et al. Time to first cigarette after waking predicts cotinine levels. Cancer Epidemiol Biomarkers Prev 2009;18:3415–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ogden MW. Environmental tobacco smoke exposure of smokers relative to non-smokers. Anal Commun 1996;33:197–8. [Google Scholar]
- 15.Jain RB. Trends in serum cotinine concentrations among daily cigarette smokers: data from NHANES 1999–2010. Sci Total Environ 2013;472C:72–7. [DOI] [PubMed] [Google Scholar]
- 16.Jones MR, Wipfli H, Shahrir S, et al. Secondhand tobacco smoke: an occupational hazard for smoking and non-smoking bar and nightclub employees. Tob Control 2013;22:308–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Branstetter SA, Muscat JE. Time to first cigarette and serum cotinine levels in adolescent smokers: National Health and Nutrition Examination Survey, 2007–2010. Nicotine Tob Res 2013;15:701–7. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease C, Prevention. State-specific secondhand smoke exposure and current cigarette smoking among adults—United States, 2008. MMWR Morb Mortal Wkly Rep 2009;58:1232–5. [PubMed] [Google Scholar]
- 19.Caraballo RS, Giovino GA, Pechacek TF, et al. Racial and ethnic differences in serum cotinine levels of cigarette smokers: Third National Health and Nutrition Examination Survey, 1988–1991. JAMA 1998;280:135–9. [DOI] [PubMed] [Google Scholar]
- 20.Mills AL, Messer K, Gilpin EA, et al. The effect of smoke-free homes on adult smoking behavior: a review. Nicotine Tob Res 2009;11:1131–41. [DOI] [PubMed] [Google Scholar]
- 21.Spencer N, Blackburn C, Bonas S, et al. Parent reported home smoking bans and toddler (18–30 month) smoke exposure: a cross-sectional survey. Arch Dis Child 2005;90:670–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Borland R, Yong HH, Cummings KM, et al. Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control 2006;15(Suppl 3):iii42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gilpin EA, White MM, Farkas AJ, et al. Home smoking restrictions: which smokers have them and how they are associated with smoking behavior. Nicotine Tob Res 1999;1:153–62. [DOI] [PubMed] [Google Scholar]
- 24.Hyland A, Higbee C, Travers MJ, et al. Smoke-free homes and smoking cessation and relapse in a longitudinal population of adults. Nicotine Tob Res 2009;11:614–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arheart KL, Lee DJ, Dietz NA, et al. Declining trends in serum cotinine levels in US worker groups: the power of policy. J Occup Environ Med 2008;50:57–63. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC). State smoke-free laws for worksites, restaurants, and bars–United States, 2000–2010. MMWR Morb Mortal Wkly Rep 2011;60:472–5. [PubMed] [Google Scholar]
- 27.Association AL. State Smokefree Workplace Laws. Secondary State Smokefree Workplace Laws September 1, 2014 2014. http://www.lungusa2.org/slati/reports/secondhand-smoke-laws-factsheet-092014.pdf [Google Scholar]
- 28.Max W, Sung HY, Shi Y. Who is exposed to secondhand smoke? Self-reported and serum cotinine measured exposure in the U.S., 1999–2006. Int J Environ Res Public Health 2009;6:1633–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coultas DB, Howard CA, Peake GT, et al. Salivary cotinine levels and involuntary tobacco smoke exposure in children and adults in New Mexico. Am Rev Respir Dis 1987;136:305–9. [DOI] [PubMed] [Google Scholar]
- 30.Benowitz NL, Bernert JT, Caraballo RS, et al. Optimal serum cotinine levels for distinguishing cigarette smokers and nonsmokers within different racial/ethnic groups in the United States between 1999 and 2004. Am J Epidemiol 2009;169:236–48. [DOI] [PubMed] [Google Scholar]
- 31.Piccardo MT, Stella A, Valerio F. Is the smokers exposure to environmental tobacco smoke negligible? Environ Health 2010;9:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kostygina G, Hahn EJ, Rayens MK. ‘It’s about the smoke, not the smoker’: messages that motivate rural communities to support smoke-free policies. Health Educ Res 2014;29:58–71. [DOI] [PMC free article] [PubMed] [Google Scholar]


