Abstract
Introduction:
Outcomes related to Covid-19 in systemic sclerosis patients could be influenced by internal organ involvement and/or immunosuppressive treatment, leading to efforts to shield patients from Covid-19 transmission. We examined the impact of Covid-19 on the lived experience of systemic sclerosis with regards to other aspects of daily living including occupation and emotional well-being.
Method:
Individuals with systemic sclerosis or relatives/carers participated in an online survey, disseminated through international patient associations and social media pages, designed to examine the impact of Covid-19 on living with a rare disease.
Results:
Responses from 121 individuals (98% were patients with systemic sclerosis) from 14 countries were evaluable. Covid-19 was considered a probable/definite personal threat (93%) or threat for the individual they care for (100%). Approximately two-thirds of responders reported either cancellation or postponement/delay to appointments, diagnostic tests, medical therapies at home (e.g. infusions), surgery or transplant, psychiatry follow-up or rehabilitation services. Twenty-six percent reported at least one systemic sclerosis medicine/treatment had been unavailable, and 6% had to either stop taking usual medications or use an alternative. Most reported online consultations/telemedicine via phone (88%) and online (96%) as being ‘fairly’ or ‘very’ useful. Respondents reported tensions among family members (45%) and difficulty overcoming problems (48%). Restrictions on movement left around two-thirds feeling isolated (61%), unhappy and/or depressed (64%), although the majority (85%) reported a strengthening of the family unit.
Conclusion:
Covid-19 has resulted in significant impact on the clinical-care and emotional well-being of systemic sclerosis patients. Changes to clinical care delivery have been well-received by patients including telemedicine consultations.
Keywords: Systemic sclerosis, scleroderma, Covid-19, clinical-care, emotional well-being, telemedicine
Introduction
Systemic sclerosis (SSc) carries a significant burden of disease-associated morbidity including reduced quality of life and high-associated mortality.1–4 Therefore, patients require regular clinical follow-up including screening for cardiorespiratory complications which can significantly improve survival (e.g. through the early detection of pulmonary hypertension).5,6 SSc is associated with significant emotional and social consequences including (but not limited to) anxiety, depression, fatigue, sleep disorders, body image dissatisfaction, and sexual dysfunction. Patients experience fear and uncertainty about the future and make many adaptations to self-manage their condition. For example, patients describe the need for constant vigilance and cold avoidance to prevent attacks of Raynaud’s phenomenon and/or the development of new digital ulcers.7,8 Patients with SSc also potentially require hospitalisation (both electively and urgently) throughout the course of their disease, including for the administration of intravenous-based vascular and immunosuppressive therapies. Furthermore, there still remains significant debate about the optimal timing for the safe reintroduction of immunosuppressive therapies in the context of confirmed Covid-19 infection. 9
Patients with SSc are potentially extremely vulnerable to poor outcomes including high mortality from Covid-19 (SARS-Cov-2) as a consequence of underlying major internal organ involvement and/or immunosuppressive treatment. A particular concern is the high prevalence of interstitial lung disease in SSc and potential lung injury related to Covid-19 infection.10,11 There are also significant diagnostic challenges because Covid-19 pneumonia can share many similar radiological abnormalities with SSc-interstitial lung disease (e.g. ground glass opacities).10,11 In addition to the direct threats relating to Covid-19, patients with SSc have also faced disruption to their previous standards of care relating to ‘in-person’ clinic appointments, therapeutic drug infusions, commencement of new immunomodulatory therapy and hospital-based investigations such as cardiopulmonary screening and cross-sectional imaging. However, international adjustments to the delivery of clinical care and new ways of working are likely to improve future care in SSc. 12
Against this background, our aims were to examine the impact of the Covid-19 pandemic on patients’ with SSc (1) clinical-care and (2) other aspects of daily life including occupation and emotional well-being, and to identify where patients can be better supported.
Method
Study design
An international survey was designed by EURORDIS-Rare Diseases Europe, a non-profit and non-governmental alliance of more than 900 patient organisations to understand how patients with rare disease experience the Covid-19 pandemic. The link to the survey was widely distributed including via the EURORDIS website, 13 patient organisations and on social media pages. The survey was translated into 23 languages in order to ensure broad geographical patient representation. The survey took place between April and May 2020; either the patient themself or a patient representative (relative/carer) could complete the survey. The survey (see Supplementary Data) was comprised of 30 questions which included patients’ demographic information, current measures in place against the Covid-19 pandemic and the perceived threat, interruption and the perceived impacts in usual aspects of their clinical-care, changes to their occupation, and their emotional well-being. All responses were fully anonymised, and there was no opportunity to verify diagnoses or responses. Respondents provided implied consent through completion of the voluntary survey. In view of the nature and distribution of the survey, the work was exempt from UK National Research Ethics Service and Health Research Authority regulations.
Results
Responders’ demographics
A total of 121 individuals, the majority of which were patients with SSc, responded to the survey from 14 countries worldwide. Most (>80%) individuals (‘responders’) reported living in Europe, with the majority in Italy (26%), Denmark (25%), Spain (18%), France (9%) or England (6%). When reported (n = 118), the survey was completed by patients themselves (98%) or by their spouse or a patient representative (2%). The majority of responders were female (93%). Most (95%) responders were older than 35 years; in particular, either between 35 and 49 years (37%) or 50 and 64 years (45%). Less than one-fifth of responders were either 65 years or older (13%) or between 25 and 34 years (5%). Almost all (99%) responders identified that social distancing was in place including avoiding mass gatherings and maintaining distances from others when possible.
Perceived impact and threat of Covid-19
Over half of respondents indicated that the interruptions related to the Covid-19 pandemic were either ‘probably’ or ‘definitively’ affecting patients’ health (59%) or well-being (69%). The majority of respondents (n = 121) felt that Covid-19 posed either a ‘high’ (54%) or ‘very high’ (39%) personal threat or threat for the individual they care for (100%). Around three-quarters felt that they had access to all the information they needed either ‘some’ (28%) or ‘most’ (44%) of the time.
Impact of Covid-19 on clinical-care
Two-thirds of patients (63%) were receiving at least part of their clinical care for SSc through a hospital. Of these, half (52%) did not attend the hospital themselves because they were fearful of contracting Covid-19. Respondents also indicated that they had been told not to attend the hospital if they became unwell for reasons other than Covid-19 (41%) or that the hospital/unit which provides care for SSc was closed (21%).
Figure 1 depicts the reported interruption in different aspects of care for patients with SSc provided by healthcare professionals since the beginning of the Covid-19 pandemic. Around two-thirds of responders reported either complete cancellation or postponement/delay to appointments with clinicians who manage their SSc, diagnostic tests (including blood tests, medical imaging and cardiorespiratory investigations), medical therapies at home (e.g. infusions), surgery or transplant, psychiatry follow-up or rehabilitation services. One quarter (26%) of responders identified that at least one of their medicines/treatments needed for SSc had been unavailable temporarily when they visited their pharmacy or hospital, and 6% had to either stop taking it or take an alternative. Of those currently unaffected by disruptions to their medicines or treatment (n = 82), the majority were either afraid ‘a little’ (55%) or ‘a lot’ (13%) about future possible problems if the pandemic continues.
Figure 1.
Reported interruption in aspects of usual clinical care provided by healthcare professionals for patients with SSc since the beginning of the Covid-19 pandemic.
Experience of changes to clinical-care
The majority of responders (where applicable) indicated that their experience to changes in clinical-care was either ‘fairly’ or ‘very’ useful with prescription by email (94%), online consultations or other forms of telemedicine including via telephone (88%), and online education and training to help them manage their SSc (96%).
Impact of Covid-19 on occupation and emotional well-being
Impact on occupation
The majority (90%) of respondents (where applicable, n = 41) indicated that they had made changes to their working situation since the Covid-19 pandemic. Almost two-thirds were working from home (59%), 17% had to stop working and 15% significantly reduced their number of working hours.
Impact on emotional well-being
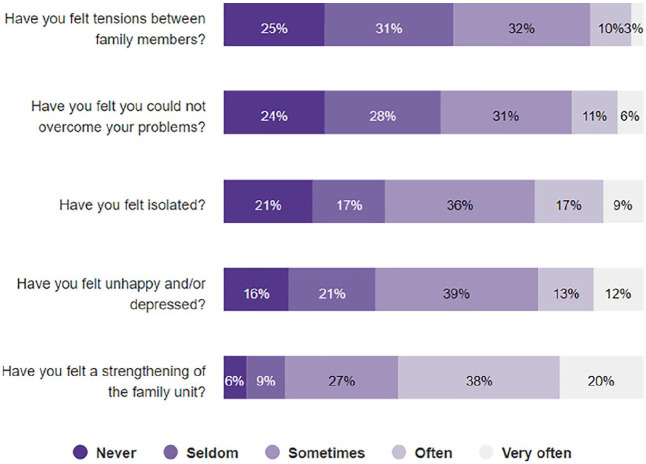
Figure 2 depicts the reported impact on patients with SSc emotional well-being since the Covid-19 pandemic. Respondents indicated that they felt tensions between their family members (45%), ‘sometimes’, ‘often’ or ‘very often’, they felt that they could not overcome their problems (48%), and two-thirds felt isolated (61%) or unhappy and/or depressed (64%). However, over three-quarters (85%) felt a strengthening of the family unit resulting from the Covid-19 pandemic.
Figure 2.
Impact on patients with SSc emotional well-being since the beginning of the Covid-19 pandemic.
Conclusion
The key findings from our study are that the Covid-19 pandemic has significantly impacted usual clinical-care, occupation and emotional well-being of patients with SSc. Patients experienced interruptions in all aspects of their clinical care including consultations, access to investigations including cardiorespiratory imaging and access to drug therapies. Patients and their caregivers feel that these interruptions are likely to have a significant detrimental impact on the health of patients with SSc. The Covid-19 pandemic is having a major impact on the working life and emotional well-being of patients with SSc. However, in response, there is evidence that the family unit is strengthening in order to face this unique challenge. Adding to an already unpredictable disease, the Covid-19 pandemic has been associated with significant fear and uncertainty about the future for patients with SSc and their caregivers. Clinicians are faced with the challenge of maintaining a crucial continuity of care for patients with SSc, including psychological support and medicines management.
Patients with SSc require close clinical review and timely access to potentially tissue saving therapies. As the Covid-19 pandemic continues, clinicians are rapidly adopting existing and new technologies to provide clinical care including consultations and renewal of prescribed therapies. The vast majority (~90%) of responders felt that such alternative methods were either ‘fairly’ or ‘very’ useful. Ciurea and colleagues 14 recently reported their experience from the Swiss Clinical Quality Management cohort of the impact of the Covid-19 pandemic on the disease activity of patients with inflammatory rheumatological conditions (axial spondlyloarthritis, rheumatoid arthritis and psoriatic arthritis). Despite a reduction in the number of consultations by half (52%), the number of remote assessments more than doubled. Reassuringly, the proportion of patients with disease flares remained stable and there was no detrimental impact on disease activity as assessed by patient-reported outcome measures. Accurate identification of patients with SSc and major internal organ-based complications (e.g. pulmonary hypertension and/or interstitial lung disease) 15 is required, with appropriate advice to shield.
Patients with SSc and their caregivers require high-quality accessible information of appropriate readability throughout the course of their disease and are increasingly using Internet/online sources of information and support (including patient-led organisations) to inform shared decision-making.16,17 However, of concern, the overall quality and readability of Internet-based SSc (and Raynaud’s phenomenon) information (prior to the Covid-19 pandemic) has been reported to be poor. 18 In response to the Covid-19 pandemic, the World Scleroderma Foundation (WSF) has developed preliminary practical advice based on patient management which were developed virtually by experts in rheumatology and associated specialities. 10 This includes the need to limit visits to the hospital/clinic and that this must be balanced against the risk of disease flare on the individual level. 10 Also, telemedicine consultations have been strongly endorsed. 10 Furthermore, it has been acknowledged that temporary drug interruption of immunosuppressive treatment may be considered in Covid-19 infection, again highlighting the need to balance the risk of disease flare, and also the need for future research in this area. 10 At the present time, no change in vascular/vasoactive therapy has been proposed for vascular and renal involvement in patients with SSc at risk of developing or experiencing Covid-19. 10
As expected, in the earlier stages of the rapidly developing Covid-19 pandemic, there were significant interruptions to existing treatment for patients with SSc. For example, Crisafulli et al. 19 reported their single-centre (Brescia, Italy) early experience (since 23 January) of an adapted, centralised outpatients for patients with rheumatic diseases. Of 64 patients with SSc who were receiving periodic intravenous iloprost infusions, the majority (73%) briefly discontinued their iloprost therapy. Despite interruption in treatment, there was no significant increase in new digital ulcers, but a slight increase in ulcer severity. A key aspect is that throughout this period, there was regular communication with patients with SSc to optimise the timely reintroduction of treatment. There are also potential opportunities to learn from innovative models of care that have been developed in response to the Covid-19 pandemic in other chronic health conditions (e.g. diabetes mellitus). 20
The EURORDIS survey has a number of important points for consideration. Although the sample size was fairly small (n = 121), it has benefitted from widespread geographical participation from patients with SSc, including translation of the survey into 23 languages. The survey was conducted towards the beginning of the Covid-19 pandemic and therefore responders’ attitudes and beliefs, and their experience of managing SSc, may have changed during the evolving crisis, including through adaptations and changing governmental guidance. Also, specific disease-related information (e.g. disease subtype and severity) was not collected as these factors may have important implications for the impact of the Covid-19 pandemic in patients with SSc. Further research is required to examine the impact on the lived experience of patients with SSc between the first and subsequent ‘waves’ of the pandemic including once vaccination is available.
In conclusion, the Covid-19 pandemic has resulted in significant impact on patients with SSc routine clinical-care and emotional well-being. Changes to the delivery of different aspects of clinical care have been well-received by patients with SSc, including telemedicine consultations and further research is now required to understand the utility potential, effectiveness and sustainability of these interventions. The potential for future pandemics also underlines the importance of rising to the challenge of maintaining a continuity of care for patients who require regular clinical follow-up. Patients with SSc require careful individual assessment to determine their risk of disease flare from interruptions in treatment. There are still many practical uncertainties about patient management in Covid-19 and future research is urgently needed to understand the interventions that can ensure continuity of care for a global challenge that may ‘never go away’.
Supplemental Material
Supplemental material, sj-doc-1-jso-10.1177_2397198321999927 for Impact of Covid-19 on clinical care and lived experience of systemic sclerosis: An international survey from EURORDIS-Rare Diseases Europe by Michael Hughes, John D Pauling, Andrew Moore and Jennifer Jones in Journal of Scleroderma and Related Disorders
Acknowledgments
The authors would like to thank the Rare Barometer team at EURORDIS-Rare Diseases Europe for access to the aggregated survey data. The Editor/Editorial Board Member of JSRD is an author of this paper, therefore, the peer review process was managed by alternative members of the Board and the submitting Editor/Board member had no involvement in the decision-making process.
Footnotes
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship and/or publication of this article: M.H. has received speaker honoraria (<$10,000) from Actelion pharmaceuticals. J.J.’s work at Genetic Alliance UK is supported through a partnership agreement with Alexion. J.P. has received speaker’s honoraria and research grant support (>$10,000) from Actelion pharmaceuticals. He has undertaken consultancy work for Actelion pharmaceuticals, Sojournix Pharma and Boehringer Ingelheim. The remaining author has no conflicts to declare.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iDs: Michael Hughes  https://orcid.org/0000-0003-3361-4909
https://orcid.org/0000-0003-3361-4909
John D Pauling  https://orcid.org/0000-0002-2793-2364
https://orcid.org/0000-0002-2793-2364
Supplemental material: Supplemental material for this article is available online.
References
- 1. Bassel M, Hudson M, Taillefer SS, et al. Frequency and impact of symptoms experienced by patients with systemic sclerosis: results from a Canadian National Survey. Rheumatology 2011; 50(4): 762–767. [DOI] [PubMed] [Google Scholar]
- 2. Denton CP, Khanna DK. Systemic sclerosis. Lancet 2017; 390(10103): 1685–1699. [DOI] [PubMed] [Google Scholar]
- 3. Park EH, Strand V, Oh YJ, et al. Health-related quality of life in systemic sclerosis compared with other rheumatic diseases: a cross-sectional study. Arthritis Res Ther 2019; 21(1): 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Moore DF, Steen VD. Overall mortality. J Scleroderma Relat Disord. Epub ahead of print 8 June 2020. DOI: 10.1177/2397198320924873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Humbert M, Yaici A, de Groote P, et al. Screening for pulmonary arterial hypertension in patients with systemic sclerosis: clinical characteristics at diagnosis and long-term survival. Arthritis Rheum 2011; 63(11): 3522–3530. [DOI] [PubMed] [Google Scholar]
- 6. Denton C, Hughes M, Gak N, et al. BSR and BHPR guideline for the treatment of systemic sclerosis. Rheumatology 2016; 55(10): 1906–1910. [DOI] [PubMed] [Google Scholar]
- 7. Bruni C, Matucci-Cerinic M. Response to: ‘Correspondence on “Systemic sclerosis and the COVID-19 pandemic: World Scleroderma Foundation preliminary advice for patient management”’ by Snarskaya and Vasileva. Ann Rheum Dis. Epub ahead of print 6 January 2021. DOI: 10.1136/annrheumdis-2020-219533. [DOI] [PubMed] [Google Scholar]
- 8. Pauling JD, Domsic RT, Saketkoo LA, et al. Multinational qualitative research study exploring the patient experience of Raynaud’s phenomenon in systemic sclerosis. Arthritis Care Res 2018; 70(9): 1373–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hughes M, Pauling JD, Jones J, et al. A multi-centre qualitative study exploring the patient experience of digital ulcers in systemic sclerosis. Arthritis Care Res 2020; 72(5): 723–733. [DOI] [PubMed] [Google Scholar]
- 10. Matucci-Cerinic M, Bruni C, Allanore Y, et al. Systemic sclerosis and the COVID-19 pandemic: World Scleroderma Foundation preliminary advice for patient management. Ann Rheum Dis 2020; 79(6): 724–726. [DOI] [PubMed] [Google Scholar]
- 11. Orlandi M, Lepri G, Bruni C, et al. The systemic sclerosis patient in the COVID-19 era: the challenging crossroad between immunosuppression, differential diagnosis and long-term psychological distress. Clin Rheumatol 2020; 39(7): 2043–2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Denton CP, Campochiaro C, Bruni C, et al. COVID-19 and systemic sclerosis: Rising to the challenge of a pandemic. J Scleroderma Relat Disord. Epub ahead of print 18 October 2020. DOI: 10.1177/2397198320963393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. EURODIS, https://www.eurordis.org/rare-barometer-programme
- 14. Ciurea A, Papagiannoulis E, Bürki K, et al. Impact of the COVID-19 pandemic on the disease course of patients with inflammatory rheumatic diseases: results from the Swiss Clinical Quality Management cohort. Ann Rheum Dis 2021; 80: 238–241. [DOI] [PubMed] [Google Scholar]
- 15. Reilly E, Skeoch S, Hardcastle S, et al. Evaluation of a patient self-stratification methodology to identify those in need of shielding during COVID-19. Clin Med 2020; 20(6): e212–e214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hughes M. Effect of season on internet searches for information on Raynaud phenomenon. J Rheumatol 2019; 46(11): 1543–1544. [DOI] [PubMed] [Google Scholar]
- 17. Hughes M, Baker A, Farrington S, et al. Patient organisation-led initiatives can play an important role in raising awareness about Raynaud’s phenomenon and encourage earlier healthcare utilisation for high-risk groups. Ann Rheum Dis 2019; 78(3): 439–441. [DOI] [PubMed] [Google Scholar]
- 18. Devgire V, Martin AF, McKenzie L, et al. A systematic review of internet-based information for individuals with Raynaud’s phenomenon and patients with systemic sclerosis. Clin Rheumatol 2020; 39(8): 2363–2367. [DOI] [PubMed] [Google Scholar]
- 19. Crisafulli F, Lazzaroni M-G, Zingarelli S, et al. Impact of COVID-19 on outpatient therapy with iloprost for systemic sclerosis digital ulcers. J Scleroderma Relat Disord. Epub ahead of print 10 September 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Agarwal S, Griffith ML, Murphy EJ, et al. Innovations in diabetes care for a better ‘new normal’ beyond COVID-19. J Clin Endocrinol Metab 2021; 106(1): e377–e181. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-doc-1-jso-10.1177_2397198321999927 for Impact of Covid-19 on clinical care and lived experience of systemic sclerosis: An international survey from EURORDIS-Rare Diseases Europe by Michael Hughes, John D Pauling, Andrew Moore and Jennifer Jones in Journal of Scleroderma and Related Disorders