Abstract
Although improvements in acute care for traumatic brain injury (TBI) have increased the patient survival rate, many survivors often suffer from neuropsychiatric sequelae such as depression. This study investigated the influence of TBI on the risk of depression using South Korean nationwide data. Data were extracted from the National Health Insurance Service database for patients who experienced TBI from 2010 to 2017 (n = 1,141,593) and for 1:1 matched controls without TBI (n = 1,141,593). Patients under 18 years old or with a history of depression were excluded. TBI was used as a time-varying exposure and a time-dependent Cox regression model was adopted. Age, sex, insurance premium and type, region of residence, past psychiatric diseases, and Charlson Comorbidity Index were adjusted. The incidence of depression in the patients with TBI and matched controls was 34.60 and 21.42 per 1000 person-years, respectively. The risk of depression was higher in the patients with TBI (hazard ratio [HR] 1.19, 95% confidence interval [CI] = 1.18-1.20) than in the matched control group. After stratification by sex and age, the risk was higher in men and the younger age group. In subgroup analyses, patients with skull fracture showed the highest risk of depression. Notably, during the first year after TBI, the depression risk was almost 11 times higher than that in the matched control group (HR 11.71, 95% CI = 11.54-11.87). Our findings highlight a significant association of TBI with an increased risk of subsequent depression. Therefore, continuous awareness with regard to patients' mental health is needed.
Keywords: depression, epidemiology, longitudinal cohort study, traumatic brain injury
Introduction
Globally, TBI is the primary reason for global mortality and morbidity in persons under 45 years of age.1 Although improvements in acute care for TBI have increased the patient survival rate, survivors often suffer from neuropsychiatric sequelae after TBI.2 Primarily, depression is the most common psychiatric disorder reported after TBI.3,4 This may be because TBI causes temporary or permanent dysfunction in the brain, which limits a patient's activities, affects participation in society, and lowers the quality of life.5-7
Depression that is not given adequate attention after TBI is likely to develop into more severe conditions that require acute treatment, thus increasing the range of efforts and resources devoted to patient rehabilitation.8 Therefore, an estimation of the prevalence of post-TBI depression, as well as its onset time after injury, is necessary to guide programs that can identify post-TBI depression within the population at large. These efforts may lead to timely treatment administration and better prognosis for the patients.
Although previous studies report a relationship between TBI and depression, this is the first study that includes a total of 2.2 million adult participants using data from a nationwide, mandatory, government-established health insurance system in South Korea. The National Health Insurance Service (NHIS) is a social insurance benefit scheme that covers the whole South Korean population and provides lifelong coverage for the prevention and treatment of diseases and injuries that result from daily life activities.9 The NHIS database gathers the socioeconomic information, details of any diagnosed illnesses, and sustained medical expenses for each of its beneficiaries.9 Using this nationwide health insurance database, we were able to conduct a population-level study with a relatively long follow-up period of 7 years. This study aimed to investigate the risk of post-TBI depression and to identify susceptible patients who might need preferential treatment.
Methods
Study population
This national retrospective cohort study used data from the National Health Insurance Service-National Health Information Database (NHIS-NHID) in South Korea.10 All South Korean citizens are required to enroll in the NHIS and are identified by a 13-digit resident registration number from birth10,11 that is used in all South Korean hospitals and clinics to claim their patient's treatment bills from the NHIS.10,12 Therefore, the probability of overlapping medical records is very small, even if a patient's residence changes.10,11 All medical treatments in South Korea are tracked without exception using the Korean Health Insurance Review and Assessment Service system.10-12 Additionally, an administrative entity must be notified of an individual's death before a funeral in South Korea, and medical doctors must record the causes and dates of death on death certificates.10,12 Therefore, the NHIS database contains the information of patients who have developed TBI as a result of daily life activities.9
The study population was selected from the NHIS database between 2008 and 2017, and the baseline of this study is 2010. The time between 2008 and 2009 was designated as the wash-out period for TBI. According to the TBI definition by the International Classification of Disease-10 (ICD-10) codes (Supplementary Table S1),13 2,134,610 patients, who were diagnosed with TBI between January 2008 and December 2017, were included (Supplementary Fig. S1). A total of 6,898,377 participants who have never been diagnosed with TBI between 2008 and 2017 were randomly selected from other hospital encounters from individuals without TBI. In this population, participants who had no demographic variables at the baseline were excluded (n = 546,506). The participants who died (n = 36,638) or had a previous TBI (n = 153,201) or depression diagnosis (n = 299,385) before the baseline were excluded. Adolescents under 18 years old also were excluded (n = 1,735,576). The participants who had missing variables with residence or income were excluded (n = 256,795). After these exclusions, 1,141,614 patients with TBI and 4,563,212 controls without TBI were demographically-matched 1:1 on age, sex, income, and region of residence. Finally, 1,141,593 patients with TBI and 1:1 matched controls (n = 1,141,593) were included in this study. Median follow-up time of the participants was 7 years. This study was exempted from ethics approval by the institutional review board of Seoul National University Hospital (IRB No. E-2003-104-1110), because the data in the NHIS were anonymized and de-identified. Accordingly, informed consent was also waived.
Variables
The incidence of depression with major depressive disorder (MDD), single episode (F32), recurrent MDD (F33), dysthymic disorder (F34.1), and mixed anxiety and depressive disorder (F41.2) was estimated following the ICD-10 codes.14-16
All sociodemographic factors were included at the baseline. The age groups were categorized into three classes (younger age group [18-39], middle age group [40-59], and older age group [60+ years]). The insurance premium, reflecting household income levels, was categorized into quartiles.11 The region of residence was classified into two groups according to administrative districts12: urban (Seoul, Busan, Daegu, Incheon, Gwangju, Daejeon, and Ulsan) and rural (Gyeonggi, Gangwon, Chungcheongbuk, Chungcheongnam, Jeollabuk, Jeollanam, Gyeongsangbuk, Gyeongsangnam, and Jeju). The psychiatric diseases that occurred within the last 2 years before the baseline were considered as a history of past psychiatric diseases. Dementia (F00‒F04, F06, F07), psychotic disorders (F20‒F25, F28‒F29), affective disorders (F30‒F34, F38‒39), anxiety-related and stress-related disorders (F40‒F48), alcohol or drug misuse (F10‒F16, F18‒F19), and mental retardation (F70‒F79) were included as past psychiatric diseases.17,18 To assess comorbidities, Charlson Comorbidity Index (CCI) scores were calculated according to ICD-10 codes and categorized into four classes (scores as 0, 1, 2‒3, ≥ 4).19
Statistical analysis
The end-point was defined as the incidence of depression, death, or the end of the study period (December 31, 2017), whichever came first. Participants who died before the onset of depression were defined as censored. Adjusted survival curve was adopted to observe overall depression-free survival curves according to TBI occurrence. Time-dependent Cox regression model was used to assess hazard ratios (HRs) with 95% confidence intervals (CIs). TBI was used as a time-varying exposure,20 since participants defined as patients with TBI did not have TBI at the baseline but have developed TBI over time. From the patients with TBI, the person-time prior to the occurrence of TBI was considered as unexposed person-time.21
Confounding factors including age, sex, insurance type and premium, region of residence, past psychiatric diseases, and CCI were adjusted in the fully adjusted model. All confounding variables were selected by step-wise selection method with statistical significance (p < 0.05).
Since the occurrence of depression can be affected by sociodemographic status, stratification was conducted according to several sociodemographic confounders. Stratification was performed according to several sociodemographic factors including age, sex, insurance premium, region of residence, and insurance types. Both patients with TBI and controls without TBI were separated by strata according to those factors. Interactions terms were created by introducing variable × variable to find out interactions across different sociodemographic characteristics.
To examine the groups of patients with TBI more vulnerable to the risk of depression, subgroup analyses were conducted. Subgroup analyses were conducted according to TBI severity and time since TBI diagnosis. Patients with TBI were divided into subgroups and then compared with controls. TBI severity was classified as mild TBI, moderate-to-severe TBI, and skull fracture. Only concussion (S06.0) was classified as mild TBI, and all other TBIs (S06.1-S06.9) were classified as moderate-to-severe TBI. Skull fracture (S02.0, S02.1, S02.7, S02.8, S02.9) were classified as skull fracture.13
Two sensitivity analyses were performed in this study. First, we modified the definition of depression by excluding recurrent depressive disorder (F33; n = 15,629). Second, we examined the risk of depression after TBI caused by motor vehicle accidents. Because the NHIS data does not cover patients injured in motor vehicle accidents, we separately obtained a motor vehicle insurance database between 2014 and 2019 from the Korea Health Insurance Review and Assessment (HIRA; Supplementary Fig. S2). Briefly, 1,397,385 individuals who were injured in motor vehicle accidents in 2014 were included and followed up until the date of their final treatment; those who died before the onset of depression were censored. After 1:1 demographical matching according to age and sex, 134,607 patients with TBI and a corresponding number of controls were analyzed. The median and maximum follow-up times were 12 days and 6 years, respectively.
All statistical analyses were performed using SAS statistical software, version 9.4 (SAS Institute, Cary, NC). Adjusted survival curve was created by “survminer” R packages, using R, version 4.0.3 (R Development Core Team, Vienna, Austria). All p values reported are two-sided; p values <0.05 were considered statistically significant.
Results
Data were analyzed from 1,141,593 patients with TBI and 1,141,593 controls. The demographic and clinical characteristics of participants with or without TBI are presented in Table 1. The general characteristics including age, sex, region of residence, and insurance premium were exactly same due to matching. During the follow-up time, 240,969 and 155,288 depression cases occurred in patients with TBI and controls, respectively. The incidence rate of depression per 1000 person-years was also higher in patients with TBI than controls (34.60 and 21.42, respectively). Adjusted survival curves also presented that the risk of depression is higher in patients with TBI (Supplementary Fig. S3). Among those patients with TBI, 79.65% had concussion, 18.02% had brain injury other than concussion, and the remaining 2.33% had skull fractures.
Table 1.
Sociodemographic Characteristics of Participants
| TBI (n = 1,141,593) | Without TBI controls (n = 1,141,593) | |
|---|---|---|
| Depression (n, %) | 240,969 (21.11) | 155,288 (13.60) |
| Person-years (years) | 6,964,765 | 7,249,614 |
| Incidence rate of depression, per 1000 person-years |
34.60 | 21.42 |
| Mean age (standard deviation) | 47.13 (16.71) | 47.13 (16.71) |
| Age group (n, %) | ||
| 18-29 years | 206,182 (18.06) | 206,182 (18.06) |
| 30-39 years | 186,204 (16.31) | 186,204 (16.31) |
| 40-49 years | 246,958 (21.63) | 246,958 (21.63) |
| 50-59 years | 232,443 (20.36) | 232,443 (20.36) |
| 60+ years | 269,806 (23.63) | 269,806 (23.63) |
| Sex (n, %) | ||
| Male | 613,758 (53.76) | 613,758 (53.76) |
| Female | 527,835 (46.24) | 527,835 (46.24) |
| Region of residence (n, %) | ||
| Urban | 513,029 (44.94) | 513,029 (44.94) |
| Rural | 628,564 (55.06) | 628,564 (55.06) |
| Insurance type (n, %) | ||
| Self-employed | 449,130 (39.34) | 403,845 (35.38) |
| Employee insured | 632,991 (55.45) | 678,276 (59.41) |
| Medical aid | 59,472 (5.21) | 59,472 (5.21) |
| Insurance premium (n, %) | ||
| 1st Quartile | 294,722 (25.82) | 294,722 (25.82) |
| 2nd Quartile | 243,094 (21.29) | 243,094 (21.29) |
| 3rd Quartile | 280,130 (24.54) | 280,130 (24.54) |
| 4th Quartile | 323,647 (28.35) | 323,647 (28.35) |
| History of psychiatric diseases (n, %) | ||
| Dementia | 10,882 (0.95) | 12,337 (1.08) |
| Psychotic disorders | 7,718 (0.68) | 7,395 (0.65) |
| Affective disorders | 104,50 (0.92) | 8,203 (0.72) |
| Anxiety-related or stress-related disorders | 127,039 (11.13) | 108,282 (9.49) |
| Alcohol or drug misuse | 10,534 (0.92) | 4,091 (0.36) |
| Mental retardation | 1,904 (0.17) | 1,190 (0.10) |
| CCI group (n, %) | ||
| 0 | 655,780 (57.44) | 692,302 (60.64) |
| 1 | 260,612 (22.83) | 240,568 (21.07) |
| 2-3 | 169,432 (14.84) | 154,987 (13.58) |
| 4+ | 55,769 (4.89) | 53,736 (4.71) |
| Types of brain injury | ||
| Concussion | - | 909,312 (79.65) |
| Brain injury other than concussion | - | 205,692 (18.02) |
| Skull fracture | - | 26,589 (2.33) |
TBI, traumatic brain injury; CCI, Charlson Comorbidity Index.
The associations between TBI and depression are shown in Table 2. TBI was significantly associated with the risk of depression after full adjustment (HR 1.19, 95% CI 1.18‒1.20). Covariates in the fully adjusted model are listed below (Table 2). To observe the effect of TBI on the new onset of depression, we performed a sensitivity analysis (Supplementary Table S2). The results were similar even after the participants, who were diagnosed with recurrent MDD (F33), were excluded.
Table 2.
Multi-Variable Time-Dependent Cox Regression for Occurrence of Depression after TBI (n = 2,283,186)
| Hazard ratios | p value | |
|---|---|---|
| TBI (model 1) | 1.23 (1.22–1.24) | < 0.0001 |
| TBI (model 2) | 1.22 (1.21–1.23) | < 0.0001 |
| TBI (model 3) | 1.20 (1.19–1.21) | < 0.0001 |
| TBI (model 4, fully adjusted) | 1.19 (1.18–1.20) | < 0.0001 |
| Age (year) | 1.01 (1.01–1.01) | < 0.0001 |
| Sex | ||
| Male | 1.0 | |
| Female | 1.44 (1.43–1.45) | < 0.0001 |
| Region of residence | ||
| Urban | 1.0 | |
| Rural | 1.04 (1.04–1.05) | < 0.0001 |
| Insurance type | ||
| Employee insured | 1.0 | |
| Self-employed | 1.10 (1.09–1.10) | < 0.0001 |
| Medical aid | 1.35 (1.33–1.37) | |
| Insurance premium | ||
| 1st Quartile (lowest income) | 1.0 | |
| 2nd Quartile | 0.96 (0.95–0.96) | < 0.0001 |
| 3rd Quartile | 0.94 (0.94–0.95) | < 0.0001 |
| 4th Quartile (highest income) | 0.94 (0.94–0.95) | < 0.0001 |
| History of psychiatric diseases (yes) | ||
| Dementia | 1.12 (1.10–1.15) | < 0.0001 |
| Psychotic disorders | 1.72 (1.67–1.76) | < 0.0001 |
| Affective disorders | 1.73 (1.69–1.77) | < 0.0001 |
| Anxiety-related or stress-related disorders | 1.74 (1.73–1.76) | < 0.0001 |
| Alcohol or drug misuse | 2.64 (2.58–2.71) | < 0.0001 |
| Mental retardation | 1.34 (1.26–1.44) | < 0.0001 |
| CCI group | ||
| 0 | 1.0 | |
| 1 | 1.34 (1.33–1.35) | < 0.0001 |
| 2-3 | 1.59 (1.58–1.61) | < 0.0001 |
| 4+ | 1.84 (1.81–1.86) | < 0.0001 |
Model 1: adjusted for age and sex.
Model 2: adjusted for age, sex, insurance premium, region of residence, and insurance type.
Model 3: adjusted for age, sex, insurance premium, region of residence, insurance type, and history of psychiatric diseases.
Model 4: adjusted for age, sex, insurance premium, region of residence, insurance type, history of psychiatric diseases, and Charlson comorbidity index group.
TBI, traumatic brain injury; CCI, Charlson Comorbidity Index; HR, hazard ratio; CI, confidence interval.
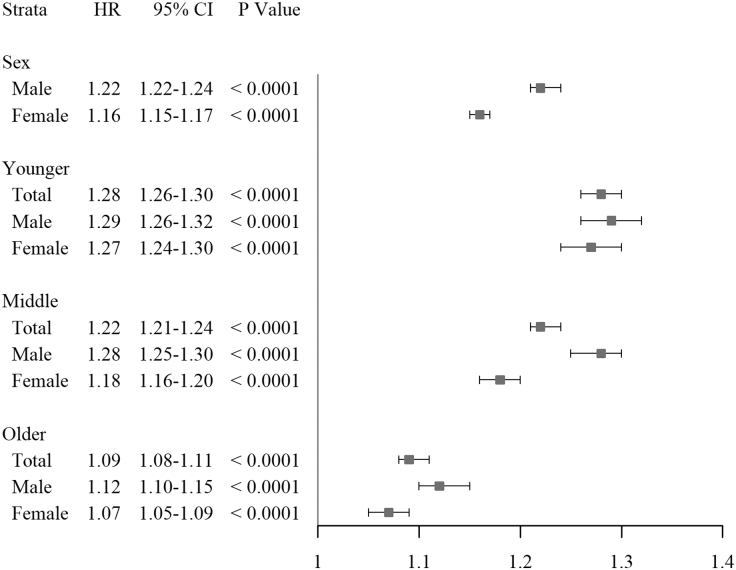
Stratification by sex or age groups (Fig. 1) revealed that males had a higher risk of depression than females (HR 1.22, 95% CI 1.22–1.24), and the younger age group had the highest risk of depression than middle or older age groups (HR 1.28, 95% CI 1.6‒1.30). After further stratification by both sex and age groups, males showed a higher risk of depression than females across all age groups.
FIG. 1.
Fully adjusted hazard ratios for depression after stratification by sex and age group. The model was adjusted for age, sex, insurance premium, region of residence, insurance type, history of psychiatric diseases, and Charlson Comorbidity Index group. Sex was excluded in this model when the strata was divided by sex. HR, hazard ratio; CI, confidence interval; Younger, younger age group (18-39 years); Middle, middle age group (40-59 years); Older, older age group (60+ years).
Supplementary Table S3 displays stratification by insurance premium, region of residence, and insurance types. After stratification by insurance premium, which reflects household income level, the highest quartile income group showed the lowest risk of depression (HR 1.15, 95% CI 1.13‒1.17). Region of residence was not an effect modifier of the association between TBI and depression. Stratification by insurance type revealed that self-employed insurance group showed a higher risk of depression than other types of insurance groups (HR 1.20, 95% CI 1.18‒1.21). These sociodemographic factors including insurance premiums, region of residence, and insurance types showed significant interactions with both age and sex (Supplementary Table S3).
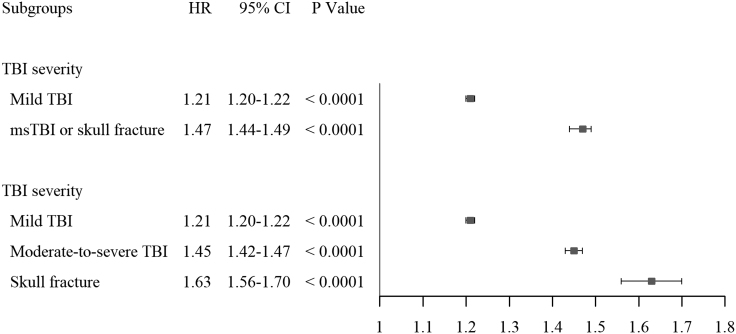
In the subgroup analysis by TBI severity, patients with moderate-to-severe TBI or skull fracture showed a higher risk of depression than patients with concussion (HR 1.47, 95% CI 1.44‒1.49; Fig. 2). When the subgroup was divided into three categories, patients with skull fracture showed the highest risk than other mild TBI or moderate-to-severe TBI (HR 1.63, 95% CI 1.56‒1.70), although the proportion of these patients is relatively small (2.33%; Table 1).
FIG. 2.
Fully adjusted hazard ratios for depression according to TBI severity. The model was adjusted for age, sex, insurance premium, region of residence, insurance type, history of psychiatric diseases, and Charlson Comorbidity Index group. TBI, traumatic brain injury; HR, hazard ratio; CI, confidence interval; msTBI, moderate-to-severe TBI.
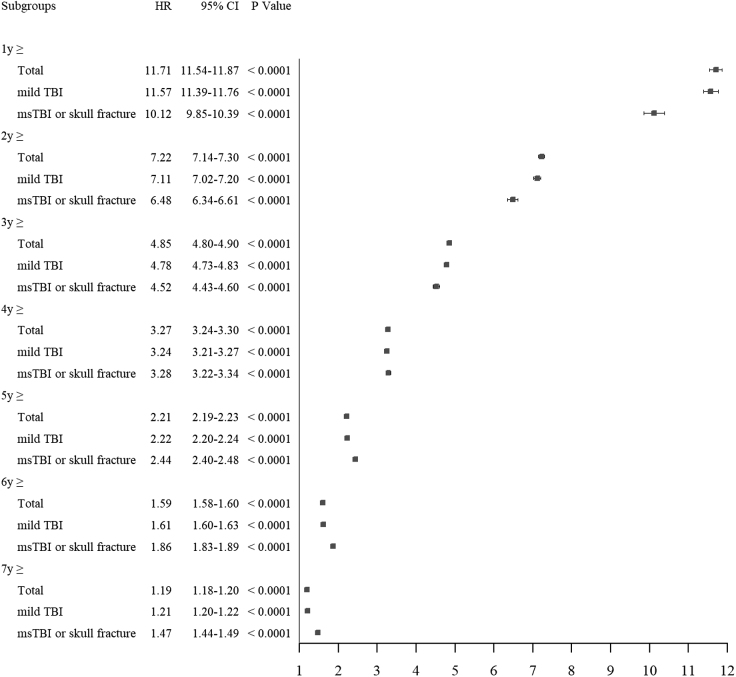
During the first year after TBI, the risk of depression was almost 11 times higher than controls without TBI (HR 11.71, 95% CI 11.54‒11.87; Fig. 3). The risk of depression during 5 years after TBI was still twice than that in the group without TBI (HR 2.21, 95% CI 2.19‒2.23). From the 1st to 3 years after TBI, patients with mild TBI showed a higher risk of depression than patients with moderate-to-severe TBI or skull fracture. However, from 5 years after TBI, the risk of depression was higher in patients with moderate-to-severe TBI or skull fracture.
FIG. 3.
Fully adjusted hazard ratios for depression according to subgroups of the time since diagnosis of TBI. The model was adjusted for age, sex, insurance premium, region of residence, insurance type, history of psychiatric diseases, and Charlson Comorbidity Index group. TBI, traumatic brain injury; HR, hazard ratio; CI, confidence interval; msTBI, moderate-to-severe TBI.
Finally, we examined the risk of post-TBI depression following motor vehicle accidents. Baseline characteristics of the age- and sex-matched patients with TBI and controls, collected from the automobile insurance database, are presented in Supplementary Table S4. After age and sex adjustment, the risk of depression was significantly higher in patients with TBI from motor vehicle accidents than in the controls (HR 2.44, 95% CI 2.14‒2.77) (Supplementary Table S5).
Discussion
This nationwide study revealed that TBI is significantly associated with an increased risk of depression in the South Korean population. After stratification, males, younger age group, self-employed group had a higher risk of depression, whereas the highest income group showed the lowest risk of depression. In subgroup analyses, patients with skull fracture showed the highest risk of depression than patients with mild TBI or moderate-to-severe TBI. Finally, the risk of depression increased by almost 11 times during the first year after TBI.
Several studies also support our findings. In a prospective longitudinal cohort study, the weight-adjusted prevalence of MDD 6 months after injuries was 9.0% (standard error [SE] = 1.0) in patients with mild TBI and 5.5% (SE = 2.4) in patients with non-head orthopedic trauma.22 Delmonico and colleagues23 revealed that mild TBI was positively associated with depression after a 4-year follow-up; for patients with TBI, the odds ratio (OR) of developing depressive disorders was almost twofold that for control individuals. The risk of depression was at its highest during the first year,23 a finding that is in agreement with our result that patients with TBI have a sharply increased risk of depression during the first year after injury. Although concussions are generally considered milder than other types of moderate-to-severe TBI or skull fractures, the risk of depression during the first year after a concussion was also dramatically higher.
In addition, a cross-sectional study found that participants with a lifetime history of TBI accompanied by loss of consciousness had a higher risk of developing lifetime depression (OR = 2.1; 95% CI = 1.6-2.8) and all risk behaviors.24 Osborn and colleagues also found that lifetime TBI, sustained at any time since birth, was significantly associated with the development of depression (OR = 1.19; 95% CI = 1.00‒1.40).25 In this study, we also found that the risk of depression remained substantially higher even 5 years after TBI, indicating that brain injuries can affect the patient's mental health for a considerable period of time. Therefore, continuous awareness with regard to patients' mental wellbeing is needed.
Our results on effect modification by sex and age (Fig. 1) can be compared with previous studies. First, our results showed that males are at higher risk of post-TBI depression than females, which is consistent with that of previous research.4 However, our findings concerning age showed different results compared to those of a previous study.4 Albrecht and colleagues26 reported that older patients were at higher risk of depression than younger patients. They suggested that older TBI patients are more likely to live in a nursing home, where they are screened for depression more often. However, community-residing elderly people experience more depression than those in nursing homes in South Korea. In our results, the younger age group had the highest risk of depression, more than the middle or older age groups. A possible explanation is that the more socially active younger age group might be more susceptible to depression because they are likely to experience considerable difficulties with social or physical changes after the trauma. Actually, the prevalence of post-TBI depression is highest in young adults.25 However, further research is needed to clarify the potential effects of age on the association between TBI and depression.
The present study has several strengths. First and foremost, this study is one of the largest nationwide population studies on TBI and the subsequent incidence of depression. Because South Korea provides mandatory NHIS for all citizens, we were able to include all patients with traumatic brain injury as the study population who were covered by NHIS in South Korea from 2010 to 2017. These millions of participants allowed this statistically well-powered association study. Second, only clinically diagnosed depression was included using the medical records within NHIS. Therefore, recall bias was prevented. Additionally, we included both major and minor depression diagnoses to avoid underestimating depression in South Korea. Finally, we adjusted for various confounding variables from sociodemographic variables to underlying diseases to diminish the influence of confounding. Especially, since depression can be affected by previous psychiatric diseases, a wide range of psychiatric disorders were adjusted as confounding variables.
This study has several limitations. First, although the NHIS generally covers ∼97% of the population,27 victims of motor vehicle or industrial accidents are not included in this database because they are covered by motor vehicle or industrial accident compensation insurance, respectively. However, our sensitivity analyses showed that patients with TBI from motor vehicle accidents also had a higher risk of depression than those without TBI. These results indicated that despite a different etiology, TBI resulting from motor vehicle accidents also increases the risk of depression. Second, participants with missing variables for income or residence (such as unemployed or homeless, respectively) were excluded from the study. This might have caused a selection bias. Third, data for treatment, medication, and cause of accident are limited in this study. Further studies are needed to include these.
Fourth, even though we adjusted various confounding variables, potential residual confounding might have occurred due to the observational design. Fifth, the diagnoses of depression reported in the source register (NHIS-NHID) relied on routine clinical assessments and were not validated through a standardized diagnostic process. However, this limitation can be offset against that register-based data might be more generalizable to the entire population even though they are less accurate than research-based data.28 Finally, separating symptoms of depression from those caused by brain injuries can be confusing. Sometimes, symptoms of a myriad of other emotional, cognitive, or behavioral consequences of TBI including diminished motivation, behavioral dyscontrol, post-traumatic stress disorder, pseudobulbar affect, or endocrinologic abnormalities, may inflate the prevalence of depression. Therefore, further studies based on a standardized depression diagnostic process is also needed.13
Conclusion
Using large-scale national health insurance data, this study demonstrated that TBI is significantly associated with an increased risk of depression in the South Korean population. Therefore, continuous awareness with regard to the mental wellbeing of patients diagnosed with TBI is needed.
Supplementary Material
Acknowledgments
The data of this study are available from the National Health Insurance Service (NHIS), but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the NHIS. The results do not necessarily represent the opinion of the National Health Insurance Corporation.
Authors' Contributions
Y.C. helped draft this article. E.Y.K. critically revised the manuscript for important intellectual content. J.S. contributed to the statistical analysis of data. H.K.K. contributed to the acquisition of data. Y.S.L., H.Y.P., and J.H.L. contributed to the interpretation of data. B.M.O., H.Y.P., and J.H.L. contributed to conception and design of this article. H.Y.P. and J.H.L. contributed to the final review of the version to be published.
Funding Information
This study was supported by a grant from the Ministry of Land, Infrastructure and Transport (MOLIT) Research Fund (J.H.L., 07-2021-5030), (H.Y.P., 07-2020-0541).
Author Disclosure Statement
No competing financial interests exist.
Supplementary Material
References
- 1. Kaur, P., and Sharma, S. (2018). Recent advances in pathophysiology of traumatic brain injury. Curr. Neuropharmacol. 16, 1224–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yeh, T.C., Chien, W.C., Chung, C.H., Liang, C.S., Chang, H.A., Kao, Y.C., Yeh, H.W., Yang, Y.J., and Tzeng, N.S. (2020). Psychiatric disorders after traumatic brain injury: a nationwide population-based cohort study and the effects of rehabilitation therapies. Arch. Phys. Med. Rehabil. 101, 822–831. [DOI] [PubMed] [Google Scholar]
- 3. Bryant, R.A., O'Donnell, M.L., Creamer, M., McFarlane, A.C., Clark, C.R., and Silove, D. (2010). The psychiatric sequelae of traumatic injury. Am. J. Psychiatry 167, 312–320. [DOI] [PubMed] [Google Scholar]
- 4. Albrecht, J.S., Barbour, L., Abariga, S.A., Rao, V., and Perfetto, E.M. (2019). Risk of depression after traumatic brain injury in a large national sample. J. Neurotrauma 36, 300–307. [DOI] [PubMed] [Google Scholar]
- 5. Lin, C.L., Dumont, A.S., Zhang, J.H., Zuccarello, M., and Chen, C.S. (2017). Improving and predicting outcomes of traumatic brain injury: neuroplasticity, imaging modalities, and perspective therapy. Neural Plast. 2017, 4752546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mausbach, B.T., Chattillion, E.A., Moore, R.C., Roepke, S.K., Depp, C.A., and Roesch, S. (2011). Activity restriction and depression in medical patients and their caregivers: a meta-analysis. Clin. Psychol. Rev. 31, 900–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cappa, K.A., Conger, J.C., and Conger, A.J. (2011). Injury severity and outcome: a meta-analysis of prospective studies on TBI outcome. Health Psychol. 30, 542–560. [DOI] [PubMed] [Google Scholar]
- 8. Hardeveld, F., Spijker, J., De Graaf, R., Nolen, W.A., and Beekman, A.T. (2010). Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr. Scand. 122, 184–191. [DOI] [PubMed] [Google Scholar]
- 9. Song, S.O., Jung, C.H., Song, Y.D., Park, C.Y., Kwon, H.S., Cha, B.S., Park, J.Y., Lee, K.U., Ko, K.S., and Lee, B.W. (2014). Background and data configuration process of a nationwide population-based study using the Korean national health insurance system. Diabetes Metab. J. 38, 395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cheol Seong, S., Kim, Y.Y., Khang, Y.H., Heon Park, J., Kang, H.J., Lee, H., Do, C.H., Song, J.S., Hyon Bang, J., Ha, S., Lee, E.J., and Ae Shin, S. (2017). Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int. J. Epidemiol. 46, 799–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim, S.Y., Kim, H.J., Park, E.K., Joe, J., Sim, S., and Choi, H.G. (2017). Severe hearing impairment and risk of depression: a national cohort study. PLoS One 12, e0179973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Choi, H.G., Jung, Y.J., and Lee, S.W. (2019). Increased risk of osteoporosis with hysterectomy: a longitudinal follow-up study using a national sample cohort. Am. J. Obstet. Gynecol. 220, 573 e571–573 e513. [DOI] [PubMed] [Google Scholar]
- 13. Madsen, T., Erlangsen, A., Orlovska, S., Mofaddy, R., Nordentoft, M., and Benros, M.E. (2018). Association between traumatic brain injury and risk of suicide. JAMA 320, 580–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Park, H., Park, C.M., Woo, J.M., Shin, J.Y., Lee, E.K., and Kwon, S.H. (2021). Real-world data analysis of the clinical and economic burden and risk factors in patients with major depressive disorder with an inadequate response to initial antidepressants. J. Med. Econ. 24, 589–597. [DOI] [PubMed] [Google Scholar]
- 15. Jang, S., Cho, H., Kang, C., and Jang, S. (2020). Antidepressant adherence and its predictors in immigrants with depression: a population-based study. Medicine (Baltimore) 99, e23308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Oh, T.K., Park, H.Y., and Song, I.A. (2021). Depression and long-term survival among South Korean sepsis survivors: a nationwide cohort study from 2011 to 2014. Crit. Care Med. 49, 1470–1480. [DOI] [PubMed] [Google Scholar]
- 17. Lee, S.W., Yang, J.M., Moon, S.Y., Yoo, I.K., Ha, E.K., Kim, S.Y., Park, U.M., Choi, S., Lee, S.H., Ahn, Y.M., Kim, J.M., Koh, H.Y., and Yon, D.K. (2020). Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry 7, 1025–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nevriana, A., Pierce, M., Dalman, C., Wicks, S., Hasselberg, M., Hope, H., Abel, K.M., and Kosidou, K. (2020). Association between maternal and paternal mental illness and risk of injuries in children and adolescents: nationwide register based cohort study in Sweden. BMJ 369, m853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Quan, H., Sundararajan, V., Halfon, P., Fong, A., Burnand, B., Luthi, J.C., Saunders, L.D., Beck, C.A., Feasby, T.E., and Ghali, W.A. (2005). Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 43, 1130–1139. [DOI] [PubMed] [Google Scholar]
- 20. Fisher, L.D., and Lin, D.Y. (1999). Time-dependent covariates in the Cox proportional-hazards regression model. Annu. Rev. Public Health 20, 145–157. [DOI] [PubMed] [Google Scholar]
- 21. Hwangbo, Y., Kang, D., Kang, M., Kim, S., Lee, E.K., Kim, Y.A., Chang, Y.J., Choi, K.S., Jung, S.Y., Woo, S.M., Ahn, J.S., Sim, S.H., Hong, Y.S., Pastor-Barriuso, R., Guallar, E., Lee, E.S., Kong, S.Y., and Cho, J. (2018). Incidence of diabetes After cancer development: a Korean national cohort study. JAMA Oncol. 4, 1099–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fuller-Thomson, E., Tulipano, M.J., and Song, M. (2012). The association between depression, suicidal ideation, and stroke in a population-based sample. Int. J. Stroke 7, 188-194. [DOI] [PubMed] [Google Scholar]
- 23. Delmonico, R.L., Theodore, B.R., Sandel, M.E., Armstrong, M.A., and Camicia, M. (2021). Prevalence of depression and anxiety disorders following mild traumatic brain injury. PMR. [DOI] [PubMed] [Google Scholar]
- 24. Waltzman, D., Daugherty, J., Sarmiento, K. and Proescholdbell, S. (2021). Lifetime history of traumatic brain injury with loss of consciousness and the likelihood for lifetime depression and risk behaviors: 2017 BRFSS North Carolina. J. Head Trauma Rehabil. 36, E40–E49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Osborn, A.J., Mathias, J.L., Fairweather-Schmidt, A.K. and Anstey, K.J. (2018). Traumatic brain injury and depression in a community-based sample: A cohort study across the adult life span. J. Head Trauma Rehabil. 33, 62–72. [DOI] [PubMed] [Google Scholar]
- 26. Chung, S. (2008). Residential status and depression among Korean elderly people: A comparison between residents of nursing home and those based in the community. Health Soc. Care Community 16, 370–377. [DOI] [PubMed] [Google Scholar]
- 27. Lee, Y.H., Han, K., Ko, S.H., Ko, K.S., Lee, K.U. and Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes, A. (2016). Data analytic process of a nationwide population-based study using national health information database established by National Health Insurance Service. Diabetes Metab. J. 40, 79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kessing, L.V., Willer, I., Andersen, P.K. and Bukh, J.D. (2017). Rate and predictors of conversion from unipolar to bipolar disorder: A systematic review and meta-analysis. Bipolar Disord. 19, 324–335. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.