Abstract
Background:
Comorbid substance use disorder and mental health conditions are common in women of reproductive age. We sought to understand the prevalence of substance use and substance use disorder by depression and anxiety disorder status and the independent association between depression and anxiety disorder status with receiving substance use treatment.
Methods:
A sample of 106,142 women ages 18–44 years was drawn from the 2008 to 2014 National Survey on Drug Use and Health. Differences in demographics, substance use, substance use disorders, and treatment by major depressive episode (MDE), and anxiety disorder status, were assessed with chi-squared tests. The independent association between MDE and anxiety disorder with substance use treatment was assessed with adjusted prevalence ratios.
Results:
Women with MDE and/or anxiety disorder had higher prevalence of substance use and substance use disorder than women with no MDE or anxiety disorder (p < 0.001). Less than a quarter of women with substance use disorders and both MDE and anxiety disorder received mental health and substance use treatment. After adjustment, women with substance use disorder and MDE and anxiety disorder, MDE only, or anxiety disorder only were more likely to receive substance use treatment (respectively, 2.4, 1.6, and 2.2 times) than women with no MDE or anxiety disorder (p < 0.001).
Conclusions:
Women with MDE and/or anxiety disorder are significantly more likely to suffer from substance use and substance use disorders than their counterparts. Integrating substance use treatment services and mental health services in settings frequently visited by reproductive-aged women may increase receipt of combined treatment.
Keywords: substance use disorder, depression, anxiety, women, treatment
Introduction
Approximately 7%–14% of reproductive-aged women suffer from depression and 12%–15% suffer from anxiety.1–5 Although depression and anxiety are distinct disorders,6 they often co-occur; an estimated 43%–45% of women affected by depression are also affected by anxiety.3 Depression and anxiety during pregnancy are associated with poor pregnancy outcomes, including preterm delivery and low birthweight infants.7,8
Reproductive-aged, pregnant, and postpartum women with depression or anxiety are more likely to use substances compared with those without depression or anxiety.3,9 Approximately 82% of pregnant and postpartum women with major depressive disorder use substances, and 36% meet the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for substance use disorders.3 In an outpatient clinic sample, 21% of women with opioid use disorder had lifetime anxiety.10 However, the prevalence of substance use disorders among women of reproductive age with depression or anxiety in a nationally representative, population-based sample is unknown.
The co-occurrence of substance use disorders with mental health conditions increases the complexity of diagnosis and treatment.11,12 A previous study found that among depressed adults, comorbid substance use disorder decreases the likelihood of receiving depression care.13 Less than 33% of adults with co-occurring substance use and mental health disorders received any treatment in the past year,14,15 and among those in treatment, 72%–77% are seen in the mental health system rather than in substance use disorder-specific services.16 For women specifically, less than half with depression or anxiety symptoms receive any treatment2,3,5,17,18 and less than 10% with substance use disorders receive any treatment.5,19 Few studies have examined treatment receipt for co-occurring conditions in reproductive-aged women.3 Receiving combined treatment (both mental health and substance use treatment) can improve overall wellness of patients with co-occurring conditions. It is important to estimate the prevalence and correlates of substance use disorder and treatment among women with depression and/or anxiety because substance use during pregnancy is associated with adverse infant outcomes such as low birthweight and neonatal abstinence syndrome,20–22 and the comorbidity may yield greater impairment to mother and infant health.11
We aimed to describe the prevalence of sociodemographic characteristics, substance use, substance use disorder, and substance use treatment in women of reproductive age (18–44 years) by depression and anxiety disorder status. We examined the independent association of receiving any substance use treatment by depression and anxiety disorder status and other correlates among reproductive-aged women.
Materials and Methods
Data source and sample
Data were drawn from the 2008 to 2014 National Surveys on Drug Use and Health (NSDUH), a nationally representative, cross-sectional survey sponsored by the U.S. Substance Abuse and Mental Health Services Administration (SAMHSA).23 The NSDUH collects information on substance use, mental health, and treatment in the civilian, noninstitutionalized, U.S. population aged 12 years and older. Sampling is state based with an independent, multistage area probability sample within each state and District of Columbia. Introductory letters are sent to sampled addresses, followed by a visit by an interviewer. Interviews are conducted with randomly sampled individuals from each household, using both computer-assisted personal interviewing by the interviewer and audio computer-assisted self-interviewing (ACASI) for sensitive topics. Further details about the survey design and methods can be found elsewhere.24–30 Analyses used deidentified public use data, and thus, the study was exempt from institutional review board review. To increase statistical power to detect nonfrequent events, 7 years of data were combined, and the 2015 data were not used because of changes in methodology regarding substance use questions.31
Weighted interview response rates for 2008–2014 ranged from 72.8% in 2014 to 77.1% in 2009 for women. Among respondents who completed the survey from 2008 to 2014, the sample was restricted to 102,142 (27.1%) adult women of reproductive age (18–44), as reported in previous studies,21,32–34 with data on pregnancy status, substance use, major depressive episodes (MDEs), anxiety disorders, and treatment for mental health and substance use disorders.
Measures
Depression and/or anxiety disorder status.
In the NSDUH, respondents were classified as having MDE in the last year if they reported more than five of the nine DSM-IV MDE symptoms for the majority of days in a 2-week period in the last year, with at least one symptom being depressed mood, loss of interest, or pleasure in doing things. No exclusions were made for MDE caused by substance use disorder. In the NSDUH, respondents were classified as having anxiety disorder if they indicated that a medical professional diagnosed them with anxiety disorder in the past year. Using these variables, we created a four-category outcome variable: MDE and anxiety disorder, MDE only, anxiety disorder only, and no MDE or anxiety disorder.
Substance use.
The NSDUH asked questions regarding tobacco (cigarettes, chewing tobacco, snuff, cigars, and pipe tobacco), alcohol, illicit drug (cocaine, hallucinogens, heroin, inhalants, and marijuana), and nonmedical prescription medicine (pain relievers, tranquilizers, sedatives, and stimulants) use to ascertain past-month and past-year use for each substance. Using these values, we created three-category variables for tobacco, illicit drug, and nonmedical prescription drug use: past month (use in the past month), past 2–12 months (use in the past year, but not the past month), and no use (no use in the past 12 months). We created four-category variables for alcohol use: heavy use (drinking ≥5 drinks on the same occasion 5 or more days in the past 30 days), binge but not heavy use (drinking ≥5 drinks on the same occasion 1 day or more in the past 30 days), past-month use but not binge or heavy use, and no use. While SAMHSA currently defines binge drinking for females as ≥4 drinks on the same occasion,35 the NSDUH did not distinguish binge drinking by gender before 2015.36
Substance use disorders.
The NSDUH asked questions regarding substance use dependence (time spent getting and using, increased tolerance, continued use after emotional or physical problems, and withdrawal symptoms) and abuse (problems at work, school, with family or friends, or with the law) for each substance. The NSDUH combined responses to create variables reflecting substance use disorder present in the past year, as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).6 We created an illicit drug use disorder variable (at least one disorder of cocaine, hallucinogen, heroin, inhalant, or marijuana) and a nonmedical prescription drug use disorder variable (at least one disorder of pain relievers, sedatives, stimulants, or tranquilizers) and utilized the existing NSDUH alcohol use disorder variable. We combined alcohol, illicit, and nonmedical prescription drug use disorder variables to denote any substance use disorder.
Mental health and substance use treatment.
The NSDUH indicated whether mental health treatment was received in the last year by combining responses regarding mental health treatment, inpatient care, outpatient care, and prescription medication for problems with emotions, nerves, and mental health. The NSDUH indicated whether substance use treatment was received in the last year by combining responses regarding substance use treatment, detoxification, and counseling for problems associated with alcohol or drug use; it should be noted that treatment for nicotine use disorder was not ascertained in the survey. Using these variables, we created a four-level treatment in the past-year variable: combined treatment (mental health and substance use treatment), mental health treatment only, substance use treatment only, and no treatment.
Pregnancy status and sociodemographic characteristics.
NSDUH self-report variables included pregnancy status at the time of the interview, age in years, race/ethnicity, education, marital status, employment, annual household income, and health insurance.
Data analysis
Among reproductive-aged women, Pearson’s chi-squared tests were conducted to assess whether sociodemographic characteristics, substance use, and the prevalence of each type of substance use disorder differed by mental health status (MDE and anxiety disorder, MDE only, anxiety disorder only, and no MDE or anxiety disorder). Among women with substance use disorder, Pearson’s chi-squared tests were conducted to assess whether treatment receipt (combined treatment, any mental health treatment, any substance use treatment, and no treatment) differed by MDE and anxiety disorder status for each type of substance use disorder.
We explored the bivariate associations between treatment receipt and sociodemographic characteristics to inform our adjusted model. To examine the independent association between MDE and anxiety disorder status and substance use treatment, unadjusted and adjusted prevalence ratios of receiving any substance use treatment in the past year were estimated for women with any substance use disorders using multivariate general linear models with Poisson distribution, adjusted for pregnancy status, age, race/ethnicity, education, marital status, employment, income, health insurance, and past-year tobacco use. All analyses were conducted using Stata 14.0 with weighting to account for the complex survey design and probability of sampling.
Results
Sample characteristics
Overall, 3.3%, 7.1%, and 5.8% of women of reproductive age in our sample had past-year MDE and anxiety disorder, MDE only, and anxiety disorder only, respectively (Table 1). Compared with women with no MDE or anxiety disorder, women experiencing MDE and/or an anxiety disorder were more likely to be white (p < 0.001), have incomes <$20,000 (<0.0001), and have public insurance (p < 0.001). They were also less likely to have college or higher education (p < 0.0001), less likely to be married (p < 0.001), and less likely to work full-time (p < 0.001; Table 1).
Table 1.
Characteristics of Women of Reproductive Age by Major Depressive Episode and Anxiety Disorder Status, National Surveys on Drug Use and Health, 2008–2014 (N = 106,142)
| Mental health status | |||||
|---|---|---|---|---|---|
| MDE and anxiety disorder (n = 3,495) | MDE only (n = 8,158) | Anxiety disorder only (n = 6,107) | No MDE or anxiety disorder (n = 88,382) | ||
| Characteristic | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | p-Valuea |
| Totalb | 3.3 (3.1–3.4) | 7.1 (6.9–7.3) | 5.8 (5.5–6.0) | 83.9 (83.6–84.2) | |
| Pregnant | 1.8 (1.3–2.4) | 2.4 (2.0–2.9) | 2.9 (2.5–3.5) | 4.4 (4.1–4.6) | <0.0001 |
| Age in years | <0.0001 | ||||
| 18–25 | 29.4 (27.7–31.1) | 35.9 (34.6–37.3) | 27.5 (26.4–28.8) | 29.9 (29.3–30.4) | |
| 26–34 | 32.0 (29.7–34.4) | 31.1 (29.5–32.7) | 36.4 (34.5–38.3) | 32.9 (32.4–33.5) | |
| 35–44 | 38.6 (36.1–41.2) | 33.0 (31.5–34.6) | 36.1 (34.0–38.2) | 37.2 (36.6–37.8) | |
| Race/ethnicity | <0.0001 | ||||
| Non-Hispanic white | 78.7 (76.5–80.8) | 63.2 (61.4–65.0 | 80.1 (78.2–81.9) | 56.7 (56.1–57.3) | |
| Non-Hispanic black | 7.9 (6.5–9.5) | 14.3 (13.1–15.6) | 5.7 (4.9–6.7) | 14.6 (14.2–15.1) | |
| Hispanic | 9.1 (7.6–10.8) | 15.8 (14.7–16.9) | 9.9 (8.6–11.3) | 19.5 (18.9–20.1) | |
| Non-Hispanic other | 4.4 (3.4–5.5) | 6.7 (5.9–7.7) | 4.3 (3.3–5.5) | 9.2 (8.8–9.5) | |
| Education | <0.0001 | ||||
| Less than high school | 12.4 (10.8–14.2) | 11.9 (10.9–12.9) | 11.1 (10.2–12.2) | 12.0 (11.7–12.4) | |
| High school graduate | 25.4 (23.3–27.6) | 27.5 (26.1–29.0) | 26.1 (24.6–27.6) | 26.2 (25.7–26.6) | |
| Some college | 37.1 (34.0–40.2) | 33.7 (32.2–35.4) | 33.1 (31.3–34.9) | 30.6 (30.2–31.1) | |
| College or more | 25.2 (22.9–27.6) | 26.9 (25.4–28.5) | 29.7 (28.1–31.5) | 31.8 (31.1–32.5) | |
| Marital status | <0.0001 | ||||
| Married | 30.9 (28.7–33.2) | 33.2 (31.1–35.3) | 41.6 (39.6–43.7) | 46.8 (46.2–47.4) | |
| Divorced, separated, or widowed | 22.3 (20.1–24.7) | 15.5 (14.2–16.8) | 14.8 (13.5–16.2) | 10.4 (10.1–10.8) | |
| Never married | 46.8 (43.8–49.8) | 51.3 (49.4–53.3) | 43.6 (41.4–45.8) | 42.8 (42.2–43.4) | |
| Employment | <0.0001 | ||||
| Full-time | 36.9 (34.3–39.6) | 45.4 (43.4–47.4) | 46.1 (44.1–48.1) | 50.7 (50.1–51.2) | |
| Part-time | 20.8 (18.7–23.1) | 22.5 (21.1–24.0) | 20.3 (18.8–21.9) | 20.7 (20.3–21.1) | |
| Other | 9.1 (7.6–10.9) | 9.3 (8.4–10.1) | 7.2 (6.2–8.4) | 6.6 (6.3–6.8) | |
| Unemployed | 33.2 (31.0–35.5) | 22.9 (21.2–24.7) | 26.4 (24.6–28.2 | 22.1 (21.6–22.6) | |
| Income | <0.0001 | ||||
| <$20,000 | 30.7 (28.8–32.8) | 26.0 (24.5–27.6) | 23.6 (21.8–25.6) | 21.3 (20.8–21.9) | |
| $20,000-$49,999 | 33.1 (30.7–35.7) | 34.5 (32.9–36.1) | 30.8 (28.9–32.7) | 32.0 (31.4–32.6) | |
| $50,000-$74,999 | 15.4 (13.6–17.4) | 15.7 (14.3–17.2) | 16.1 (14.7–17.7) | 17.1 (16.7–17.5) | |
| ≥$75,000 | 20.7 (18.4–23.2) | 23.8 (22.0–25.8) | 29.5 (27.6–31.5) | 29.6 (28.9–30.4) | |
| Insurance | <0.0001 | ||||
| Any private | 51.2 (48.5–53.8) | 56.0 (54.2–57.7) | 61.9 (60.0–63.9) | 62.3 (61.6–63.0) | |
| Public only | 27.8 (25.6–30.2) | 19.3 (18.1–20.6 | 21.3 (19.8–22.7) | 15.6 (15.2–16.0) | |
| Otherc | 2.8 (2.2–3.5) | 2.8 (2.3–3.3) | 2.4 (1.9–3.0) | 2.5 (2.4–2.7) | |
| Uninsured | 18.2 (16.4–20.2) | 21.9 (20.5–23.4) | 14.5 (13.3–15.7) | 19.6 (19.1–20.1) | |
| Tobaccoc | <0.0001 | ||||
| Past-month use | 49.6 (47.1–52.1) | 38.1 (36.0–40.1) | 44.5 (42.2–46.7) | 25.0 (24.6–25.5) | |
| Past 2–12-month use | 7.6 (6.4–9.0) | 8.6 (7.8–9.5) | 8.1 (7.0–9.2) | 5.9 (5.7–6.1) | |
| No use | 42.8 (40.5–45.2) | 53.3 (51.4–55.3) | 47.5 (45.3–49.6) | 69.1 (68.6–69.5) | |
| Alcohol, past month | <0.0001 | ||||
| Heavy use | 9.1 (7.3–11.3) | 7.4 (6.5–8.3) | 8.7 (7.7–9.9) | 4.9 (4.6–5.1) | |
| Binge but not heavy | 21.3 (19.6–23.2) | 24.2 (22.9–25.7) | 23.6 (22.1–25.1) | 19.1 (18.8–19.5) | |
| Use but not binge or heavy | 31.4 (28.8–34.0) | 31.3 (29.5–33.1) | 32.0 (30.2–33.9) | 32.0 (31.5–32.6) | |
| No use | 38.2 (35.4–41.0) | 37.1 (35.5–38.8) | 35.7 (33.8–37.6) | 43.9 (43.4–44.5) | |
| Illicit drugd | <0.0001 | ||||
| Past-month use | 18.6 (16.5–20.9) | 13.6 (12.5–14.8 | 14.4 (13.2–15.7) | 7.4 (7.2–7.7) | |
| Past 2–12-month use | 13.1 (11.6–14.8) | 11.7 (10.7–12.7) | 10.3 (9.3–11.4) | 6.2 (6.0–6.3) | |
| No use | 68.3 (65.6–70.9) | 74.7 (73.1–76.3) | 75.3 (73.6–77.0) | 86.4 (86.1–86.7) | |
| Nonmedical prescription druge | <0.0001 | ||||
| Past-month use | 10.9 (9.6–12.5) | 6.8 (6.1–7.6) | 7.7 (6.7–8.7) | 2.6 (2.5–2.8) | |
| Past 2–12-month use | 11.4 (9.9–13.0) | 9.5 (8.5–10.5) | 9.3 (8.2–10.6) | 4.1 (4.0–4.3) | |
| No use | 77.7 (75.7–79.6) | 83.7 (82.4–85.0) | 83.0 (81.4–84.5) | 93.3 (93.1–93.5) | |
Column differences based on Pearson’s chi-squared tests.
Row percentages provided.
Tobacco includes cigarettes, chewing tobacco, snuff, cigars, and/or pipe tobacco.
Illicit drug includes cocaine, hallucinogens, heroin, inhalants, and marijuana.
Nonmedical prescription drug includes pain relievers, tranquilizers, sedatives, and stimulants.
MDE, major depressive episode.
Substance use
Women of reproductive age with both MDE and anxiety disorder, MDE only, or anxiety disorder only had higher prevalence of past-month substance use than women with no MDE or anxiety disorder (p < 0.001; Table 1). The prevalence of tobacco, illicit drug, and nonmedical prescription drug use in the past 2–12 months was also higher in women with MDE and/or anxiety disorder (Table 1), and the prevalence of substance use disorders was significantly higher among women with MDE and/or anxiety disorder than among women with neither (p < 0.001; Fig. 1). Overall, 27.3% of women with both MDE and anxiety disorder, 20.9% of women with MDE only, and 16.4% of women with anxiety disorder only met the criteria for any substance use disorders, compared with 9.4% of women with no MDE or anxiety disorder; prevalence varied by type of substance use disorder (Fig. 1).
FIG. 1.
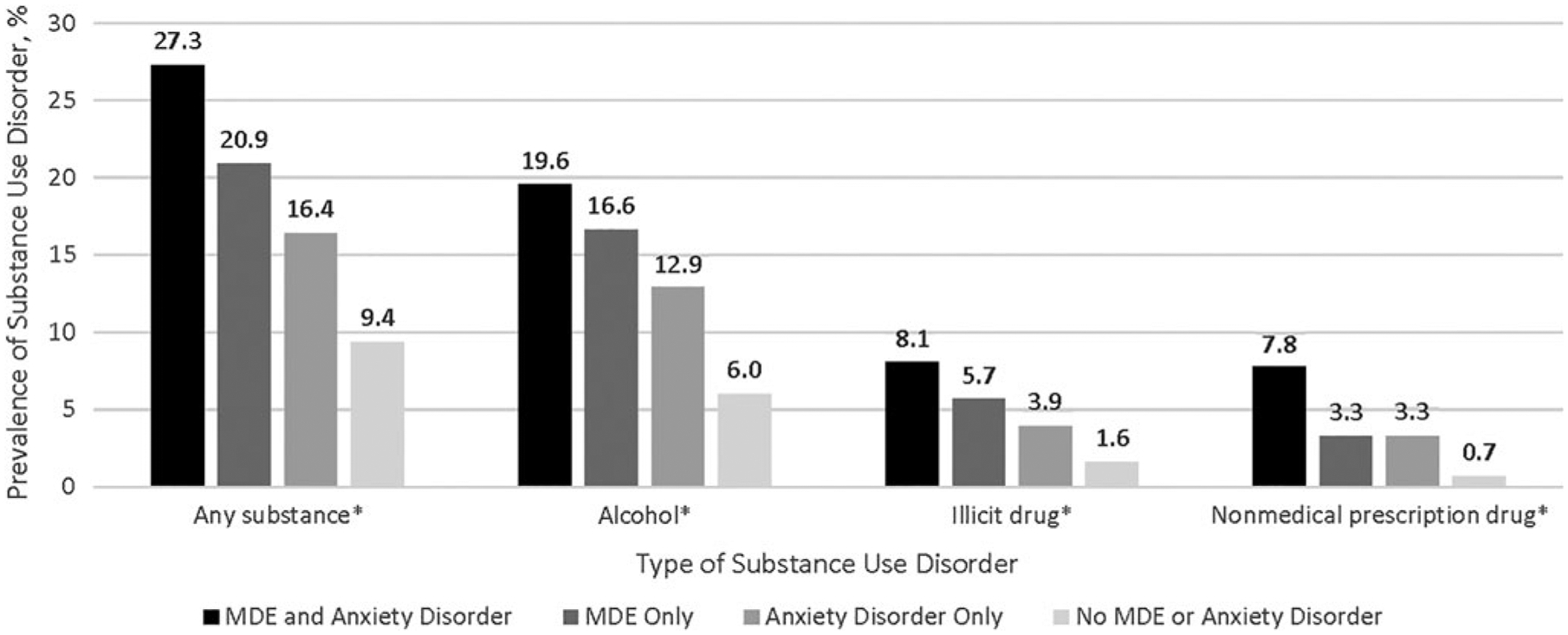
The prevalence of varying types of substance use disordera among reproductive-aged women by MDE and anxiety disorder statusb (n = 106,142). aSubstance use disorder is defined as abuse and/or dependence of any substance use (n = 12,625); alcohol (n = 10,033); illicit drugs (cocaine, hallucinogens, heroin, inhalants, and marijuana) (n = 3,345); and nonmedical prescription drugs (n = 1,655). bDifferences assessed with Pearson’s chi-squared tests. *p < 0.0001. MDE, major depressive episode.
Mental health and substance use treatment
Among women with substance use disorder, the prevalence of combined treatment was 19.1% among women with both MDE and anxiety disorder, 14.0% among women with anxiety disorder only, and 7.2% among women with MDE only; and this pattern was similar for women with alcohol and illicit drug use disorders (Table 2). Among women with nonmedical prescription drug use disorder, the pattern differed and the prevalence of combined treatment was 29.1% among women with only anxiety disorder, followed by 28.4% among women with both MDE and anxiety disorder, and 16.9% among women with MDE only (Table 2).
Table 2.
Utilization of Mental Health Treatment and Substance Treatment Among Reproductive-Aged Women with a Substance Use Disorder by Major Depressive Episode and Anxiety Disorder Status
| Mental health status | |||||
|---|---|---|---|---|---|
| MDE and anxiety disorder | MDE only | Anxiety disorder only | No MDE or anxiety disorder | ||
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | p-Valuea | |
| Any substance use disordersb (n = 12,625) | |||||
| Combined treatmentc | 19.1 (15.5–23.4) | 7.2 (5.6–9.3) | 14.0 (10.7–18.1) | 2.2 (1.7–2.9) | <0.0001 |
| Mental health treatment only | 72.8 (68.3–76.8) | 32.5 (29.4–35.7) | 64.6 (60.6–68.5) | 16.0 (14.7–17.4) | |
| Substance use treatment only | 1.5 (0.7–3.1) | 4.0 (2.7–5.8) | 2.6 (1.8–3.8) | 3.6 (3.1—4.3) | |
| No treatment | 6.7 (5.1–8.6) | 56.4 (52.8–59.8) | 18.8 (16.3–21.5) | 78.1 (76.5–79.6) | |
| Alcohol use disorder (n = 10,033) | |||||
| Combined treatmentc | 14.7 (11.4–18.8) | 6.1 (4.5–8.3) | 12.5 (8.9–17.4) | 1.7 (1.3–2.3) | <0.0001 |
| Mental health treatment only | 77.5 (72.5–81.7) | 31.6 (28.0–35.5) | 67.1 (62.0–71.8) | 15.8 (14.3–17.4) | |
| Substance use treatment only | 1.4 (0.5–4.0) | 3.5 (2.3–5.4) | 1.9 (1.1–3.2) | 3.1 (2.5–3.7) | |
| No treatment | 6.5 (5.0–8.4) | 58.7 (54.6–62.7) | 18.6 (15.6–21.9) | 79.5 (77.8–81.1) | |
| Illicit drug use disorder (n = 3,345)d | |||||
| Combined treatmentc | 33.6 (26.0–42.1) | 12.1 (8.6–16.8) | 22.9 (16.6–30.8) | 4.0 (3.0–5.2) | <0.0001 |
| Mental health treatment only | 56.6 (48.7–64.1) | 27.8 (22.1–34.2) | 53.5 (44.6–62.1) | 16.2 (13.3–19.6) | |
| Substance use treatment only | 2.9 (1.1–6.9) | 7.5 (4.3–12.9) | 5.8 (3.5–9.5) | 6.5 (5.0–8.4) | |
| No treatment | 7.0 (4.6–10.4) | 52.6 (46.3–58.9) | 17.8 (13.0–23.8) | 73.3 (69.7–76.7) | |
| Nonmedical prescription drug use disorder (n = 1,655)e | |||||
| Combined treatmentc | 28.4 (21.0–37.2) | 16.9 (11.9–23.3) | 29.1 (19.3–41.2) | 8.6 (5.8–12.6) | <0.0001 |
| Mental health treatment only | 62.7 (53.4–71.2) | 37.4 (29.2–46.4) | 45.5 (35.3–56.2) | 20.5 (16.2–25.7) | |
| Substance use treatment only | 1.4 (0.4–5.5) | 9.0 (4.3–18.0) | 7.3 (4.4–11.9) | 8.0 (6.1–10.4) | |
| No treatment | 7.5 (4.0–13.6) | 36.6 (28.9–45.2) | 18.1 (11.8–26.9) | 62.9 (57.1–68.3) | |
Column differences based on Pearson’s chi-squared test.
Any substance use disorder is defined as abusing and/or being dependent on any one of the following substances: alcohol, cocaine, hallucinogens, heroin, inhalants, marijuana, pain relievers, sedatives, stimulants, and tranquilizers.
Combined treatment includes receipt of both mental health treatment and substance use treatment in the past year.
Illicit drug use disorder is defined as abusing and/or being dependent on any one of the following illicit drugs: cocaine, hallucinogens, heroin, inhalants, and marijuana.
Nonmedical prescription drug use disorder is defined as abusing and/or being dependent on any one of the following prescription drugs: pain relievers, tranquilizers, sedatives, and stimulants.
Regarding substance use treatment, about half of women with co-occurring MDE only and specific substance use disorders (56.4% of any, 58.7% alcohol, and 52.6% of illicit drug use disorder) reported receiving no treatment for either condition (Table 2). Notably, a majority of women with only substance use disorders do not receive any treatment (78.1% of women with any substance use disorder, 79.5% of women with alcohol use disorder, 73.3% of illicit drug use disorder, and 62.9% of women with nonmedical prescription drug use disorder). Women identified as 35–44 years old, non-Hispanic white, having less than a college education, unmarried, unemployed, and having nonprivate insurance were more likely to have received substance use treatment than their counterparts (p < 0.05; data not shown).
After adjustment for sociodemographic characteristics and tobacco use, the prevalence of receiving any substance use treatment was 2.4 times, 1.6 times, and 2.2 times higher for women with both MDE and anxiety disorder, MDE only, and anxiety disorder only, respectively, compared with women with no MDE or anxiety disorder (p < 0.001; Table 3). Women with a substance use disorder who were younger (p < 0.01), non-Hispanic black (p < 0.001), and Hispanic (p = 0.013) were less likely to receive any substance use treatment. High school (p = 0.004) or less than high school education (p = 0.016), other types of employment (nonfull or part-time) (p < 0.0001), unemployed (p = 0.003), public insurance (p = 0.001), other types of insurance (p = 0.002), and past-year tobacco use (p < 0.001) were associated with increased prevalence of receiving any substance use treatment (Table 3).
Table 3.
Correlates of Receiving Any Substance Treatment Among Women with Substance Use Disorder, n = 12,625
| Any substance treatment PR (95% CI) | ||
|---|---|---|
| Characteristic | Model 1 | Model 2a |
| MDE and anxiety disorder status | ||
| Both MDE and anxiety disorder | 3.5 (2.7–4.5)*** | 2.4 (1.8–3.0)*** |
| MDE only | 1.9 (1.5–2.4)*** | 1.6 (1.3–2.0)*** |
| Anxiety disorder only | 2.8 (2.1–3.8)*** | 2.2 (1.7–2.9)*** |
| No MDE or anxiety disorder | 1.0 | 1.0 |
| Pregnant | 1.3 (0.9–1.8) | |
| Age, years | ||
| 18–25 | 0.6 (0.5–0.8)** | |
| 26–34 | 1.0 (0.8–1.2) | |
| 35–44 | 1.0 | |
| Race/ethnicity | ||
| Non-Hispanic white | 1.0 | |
| Non-Hispanic black | 0.6 (0.4–0.7)*** | |
| Hispanic | 0.7 (0.5–0.9)* | |
| Non-Hispanic other | 0.8 (0.5–1.1) | |
| Education | ||
| Less than high school | 1.8 (1.2–2.6)** | |
| High school graduate | 1.5 (1.1–2.1)* | |
| Some college | 1.4 (1.0–1.9) | |
| College or more | 1.0 | |
| Marital status | ||
| Married | 1.0 | |
| Divorced, separated, or widowed | 1.2 (0.9–1.6) | |
| Never married | 1.1 (0.9–1.5) | |
| Employment | ||
| Full-time | 1.0 | |
| Part-time | 1.1 (0.8–1.4) | |
| Other | 1.7 (1.3–2.4)*** | |
| Unemployed | 1.6 (1.2–2.1)** | |
| Income | ||
| <$20,000 | 1.1 (0.8–1.5) | |
| $20,000-$49,999 | 1.1 (0.7–1.6) | |
| $50,000-$74,999 | 1.0 (0.7–1.5) | |
| ≥$75,000 | 1.0 | |
| Insurance | ||
| Any private | 1.0 | |
| Public only | 1.6 (1.2–2.1)** | |
| Other | 1.9 (1.3–2.7)** | |
| Uninsured | 1.2 (0.9–1.6) | |
| Tobacco user, past year | 2.6 (2.1–3.4)*** | |
Any substance use disorder is defined as abusing or being dependent on any one of the following substances: alcohol, cocaine, hallucinogens, heroin, inhalants, marijuana, pain relievers, sedatives, stimulants, and tranquilizers, regardless of tobacco status.
p < 0.05;
p < 0.01;
p < 0.001.
Adjusted for pregnancy status, age, race/ethnicity, education, marital status, employment, income, health insurance, and past-year tobacco use.
Discussion
In this nationally representative, population-based study, less than a quarter of women with co-occurring substance use disorder and MDE or anxiety disorder received both mental health and substance use treatment. More specifically, the prevalence of combined treatment varied by type of substance use disorder, ranging from less than 15% in women with co-occurring alcohol disorder to less than 34% in women with co-occurring illicit drug disorder. Low rates of combination treatment may be due to stigma, underdiagnoses of both conditions, a shortage of behavioral health providers, and financial barriers.14 While treating one condition may improve the other, mental health or substance use treatment alone may not address the needs of co-occurring conditions.37 Combined treatment is associated with better outcomes, including decreased substance use, improved psychiatric symptoms, and reduced hospitalizations.38
Overall, our estimates of mental health treatment for those with MDE or anxiety disorder (40%–92%) are substantially higher than previous studies reporting that less than half of nonpregnant and pregnant women with mental health conditions receive treatment.2,3,5,17,18 The increased levels of treatment may be due to several reasons. Substance use accompanied by a comorbid mental health condition has been shown to increase the likelihood of seeking treatment.16 In addition, in our study, anxiety disorder status was based on self-reported diagnosis, which may improve ascertainment of treatment or referral treatment. In contrast, use of DSM-IV criteria to identify women with depressive symptoms allows us to capture individuals with symptoms regardless of diagnosis status. An estimated 40% of reproductive-aged women with depressive symptoms are not diagnosed with depression and thus may not be identified for treatment.2
Two groups of women with substance use disorders were found to have the lowest prevalence of any treatment: women with co-occurring MDE and alcohol or illicit drug use disorders and women with substance use disorders and no MDE or anxiety disorder, with more than half not receiving treatment. In addition, among women with co-occurring mental health disorders and substance use disorders, the prevalence of mental health treatment was higher than substance use treatment. Low rates of substance use treatment in women with substance use disorder alone and women with co-occurring conditions may be because mental health treatment is more available or easily reimbursed than substance use treatment. Public and private health insurance usually provide more benefits for mental health treatment than substance use treatment.39,40 In addition, the enactment of several federal and state policy initiatives has expanded access to mental health care41; receipt of mental health treatment has increased in recent years.42,43 Similar increases in substance use treatment have not been observed, potentially due to strong stigma and financial barriers.39
In addition to these access barriers, it is possible that individuals with mental health disorders may be more likely to have help-seeking behavior, be engaged in services, or feel less stigma toward substance use treatment than those with substance use disorder alone.14,44 Younger, non-Hispanic black, Hispanic, and privately insured women were less likely to receive substance use treatment, consistent with other studies.45 Our study showed that women who had lower levels of education, were unemployed, and had public insurance were more likely to receive substance use treatment. These characteristics, indicative of a lower socioeconomic status, have been found to be associated with an increased likelihood of treatment,19,46,47 potentially explained by the increased severity of substance use and substance use disorders in these groups,48 or reflective of the preference for cash payments, instead of insurance, at treatment centers.49 However, gaps in treatment were identified in the study. By addressing barriers related to financial burden and stigma, increasing provider efforts to engage subgroups of women with lower utilization of treatment, and integrating mental health treatment with substance use treatment, it may be possible to improve screening and treatment of substance use disorder.
Overall, we found the prevalence of substance use and substance use disorders to be higher among women with MDE and/or anxiety disorder than among women with neither condition. The prevalence of substance use disorders was highest among women with both MDE and anxiety disorder, followed by women with only one of the two mental health conditions examined. Individuals with mental health conditions may use substances as a coping mechanism,50,51 and substance use may worsen mental health conditions.52 Co-occurring conditions impair women’s psychiatric, family, and social functioning and affect women’s willingness to be screened and affect treatment adherence.53 The U.S. Preventive Services Task Force recommends universal depression screening for all adults, including pregnant and postpartum women,54 and has created a research plan to assess substance use screening in adolescents and adults, including pregnant women.55 The American College of Obstetricians and Gynecologists recommends depression screening for all women, both as part of the well-women visit and during the perinatal period56 and routine screening for substance use disorder for women.57
Limitations
This study has some limitations. First, all measures were self-reported, which may introduce social desirability bias in responses for education, income, and substance use, therefore misclassifying true prevalence. However, the use of ACASI in the NSDUH may increase reporting of sensitive behaviors.58 Second, anxiety disorders in our study were based on receipt of a doctor’s diagnosis and may misclassify women with symptoms but no diagnosis. Thus, estimates of treatment may be higher in our study and may not be generalizable to those women with anxiety symptoms and no diagnosis. Third, the available data were not able to ascertain other mental health conditions such as bipolar disorder or substance-induced mental health conditions; it is possible that reported depressive symptoms are related to substance use, rather than independent symptoms. Fourth, the assessment of nonmedical prescription drug use disorder differed from the assessment of other substances, potentially resulting in ascertainment bias. Fifth, the NSDUH is representative only of the civilian, noninstitutionalized population, and cannot be generalized to other groups (e.g., homeless persons) where substance use disorder and mental health disorders are more common.59 Last, it is not known if the associations reported here are changing over time, but if so, by combining 7 years of data, we present a time-averaged association, not the association at any particular time.
Conclusions
In conclusion, the prevalence of substance use and substance use disorder is higher among women with MDE and/or anxiety disorder. Women with a substance use disorder that co-occurs with MDE and/or anxiety disorder were more likely to receive any treatment than women with a substance use disorder, but no MDE or anxiety disorder. Noteworthy are low rates of combined treatment among women with co-occurring MDE and/or anxiety disorder and substance use disorders. By addressing the stigma and financial barriers to screening and treating for substance use and mental health conditions, and integrating substance use treatment services with mental health services in settings frequently used by reproductive-aged women, it may be possible to increase combined treatment.
Footnotes
Publisher's Disclaimer: Disclaimer
Publisher's Disclaimer: The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the U.S. Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
Author Disclosure Statement
All authors declare that they have no conflict of interest.
References
- 1.Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: Systematic review. Obstet Gynecol 2004;103:698–709. [DOI] [PubMed] [Google Scholar]
- 2.Ko JY, Farr SL, Dietz PM, Robbins CL. Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005–2009. J Womens Health (Larchmt) 2012;21:830–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Le Strat Y, Dubertret C, Le Foll B. Prevalence and correlates of major depressive episode in pregnant and postpartum women in the United States. J Affect Disord 2011; 135:128–138. [DOI] [PubMed] [Google Scholar]
- 4.Melville JL, Gavin A, Guo Y, Fan MY, Katon WJ. Depressive disorders during pregnancy: Prevalence and risk factors in a large urban sample. Obstet Gynecol 2010;116: 1064–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vesga-Lopez O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry 2008;65: 805–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th ed. Arlington, VA: American Psychiatric Association, 2013. [Google Scholar]
- 7.Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry 2010;67: 1012–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review. Women Birth 2015;28:179–193. [DOI] [PubMed] [Google Scholar]
- 9.Tong VT, Farr SL, Bombard J, D’Angelo D, Ko JY, England LJ. Smoking Before and During Pregnancy Among Women Reporting Depression or Anxiety. Obstet Gynecol 2016;128:562–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kidorf M, Disney ER, King VL, Neufeld K, Beilenson PL, Brooner RK. Prevalence of psychiatric and substance use disorders in opioid abusers in a community syringe exchange program. Drug Alcohol Depend 2004;74:115–122. [DOI] [PubMed] [Google Scholar]
- 11.Quello SB, Brady KT, Sonne SC. Mood disorders and substance use disorder: A complex comorbidity. Sci Pract Perspect 2005;3:13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wisner KL, Zarin DA, Holmboe ES, et al. Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry 2000;157:1933–1940. [DOI] [PubMed] [Google Scholar]
- 13.Han B, Olfson M, Mojtabai R. Depression care among depressed adults with and without comorbid substance use disorders in the United States. Depress Anxiety 2017;34:291–300. [DOI] [PubMed] [Google Scholar]
- 14.Harris KM, Edlund MJ. Use of mental health care and substance abuse treatment among adults with co-occurring disorders. Psychiatr Serv 2005;56:954–959. [DOI] [PubMed] [Google Scholar]
- 15.Watkins KE, Burnam A, Kung FY, Paddock S. A national survey of care for persons with co-occurring mental and substance use disorders. Psychiatr Serv 2001; 52:1062–1068. [DOI] [PubMed] [Google Scholar]
- 16.Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. Am J Orthopsychiatry 1996; 66:17–31. [DOI] [PubMed] [Google Scholar]
- 17.Byatt N, Xiao RS, Dinh KH, Waring ME. Mental health care use in relation to depressive symptoms among pregnant women in the USA. Arch Womens Ment Health 2016; 19:187–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geier ML, Hills N, Gonzales M, Tum K, Finley PR. Detection and treatment rates for perinatal depression in a state Medicaid population. CNS Spectr 2015;20:11–19. [DOI] [PubMed] [Google Scholar]
- 19.Terplan M, McNamara EJ, Chisolm MS. Pregnant and non-pregnant women with substance use disorders: The gap between treatment need and receipt. J Addict Dis 2012;31: 342–349. [DOI] [PubMed] [Google Scholar]
- 20.Behnke M, Smith VC, Committee on Substance Abuse, Committee on Fetus and Newborn. Prenatal substance abuse: Short- and long-term effects on the exposed fetus. Pediatrics 2013;131:e1009–e1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McHugh RK, Wigderson S, Greenfield SF. Epidemiology of substance use in reproductive-age women. Obstet Gynecol Clin North Am 2014;41:177–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Merritt T, Mazela J, Merritt A. Tobacco smoking and its consequences on reproductive health: The impact of a lifestyle choices including cigarette smoke exposure on fertility and birth defects. Przegl Lek 2013;70:779–783. [PubMed] [Google Scholar]
- 23.United States Department of Health and Human Services. National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration (SAMHSA), Center for Behavioral Health Statistics and Quality. Research Triangle Park, NC: RTI International, 2008–2014. [Google Scholar]
- 24.Center for Behavioral Health Statistics and Quality. 2009 National Survey on Drug Use and Health: Methodological summary and definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2010. [Google Scholar]
- 25.Center for Behavioral Health Statistics and Quality. 2014 National Survey on Drug Use and Health: Methodological summary and definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2015. [Google Scholar]
- 26.Center for Behavioral Health Statistics and Quality. 2013 National Survey on Drug Use and Health: Methodological summary and definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014. [Google Scholar]
- 27.Center for Behavioral Health Statistics and Quality. 2012 National Survey on Drug Use and Health: Methodological summary and definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2013. [Google Scholar]
- 28.Center for Behavioral Health Statistics and Quality. 2008 National Survey on Drug Use and Health: Methodological summary and definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2009. [Google Scholar]
- 29.Center for Behavioral Health Statistics and Quality. 2011 National Survey on Drug Use and Health: Methodological summary and definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2012. [Google Scholar]
- 30.Center for Behavioral Health Statistics and Quality. 2010 National Survey on Drug Use and Health: Methodological summary and definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2011. [Google Scholar]
- 31.Centers for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services, 2016. [Google Scholar]
- 32.Brown QL, Hasin DS, Keyes KM, Fink DS, Ravenell O, Martins SS. Health insurance, alcohol and tobacco use among pregnant and non-pregnant women of reproductive age. Drug Alcohol Depend 2016;166:116–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jarlenski M, Barry CL, Gollust S, Graves AJ, Kennedy-Hendricks A, Kozhimannil K. Polysubstance use among US women of reproductive age who use opioids for nonmedical reasons. Am J Public Health 2017;107:1308–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ko JY, Farr SL, Tong VT, Creanga AA, Callaghan WM. Prevalence and patterns of marijuana use among pregnant and nonpregnant women of reproductive age. Am J Obstet Gynecol 2015;213:201.e201–201.e210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Institute on Alcohol Abuse and Alcoholism. Alcohol facts and statistics. 2018; Available at: https://pubs.niaaa.nih.gov/publications/AlcoholFacts&Stats/AlcoholFacts&Stats.htm. Accessed January 30, 2019.
- 36.Center for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health: Methodological summary and definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2016. [Google Scholar]
- 37.Substance Abuse and Mental Health Services Administration. Substance abuse treatment for persons with co-occurring disorders. Treatment Improvment Protocol (TIP) Series, No. 42. HHS Publication No. (SMA) 13-3992. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2005. [Google Scholar]
- 38.Drake RE, O’Neal EL, Wallach MA. A systematic review of psychosocial research on psychosocial interventions for people with co-occurring severe mental and substance use disorders. J Subst Abuse Treat 2008;34:123–138. [DOI] [PubMed] [Google Scholar]
- 39.Ali MM, Teich JL, Mutter R. Reasons for not seeking substance use disorder treatment: variations by health insurance coverage. J Behav Health Serv Res 2017;44:63–74. [DOI] [PubMed] [Google Scholar]
- 40.Robert Wood Johnson Foundation. Health policy brief: Mental health parity. Health Aff, April 3, 2014. [Google Scholar]
- 41.Beronio K, Glied S, Frank R. How the affordable care act and mental health parity and addiction equity act greatly expand coverage of behavioral health care. J Behav Health Serv Res 2014;41:410–428. [DOI] [PubMed] [Google Scholar]
- 42.Mojtabai R National trends in mental health disability, 1997–2009. Am J Public Health 2011;101:2156–2163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mojtabai R, Jorm AF. Trends in psychological distress, depressive episodes and mental health treatment-seeking in the United States: 2001–2012. J Affect Disord 2015;174: 556–561. [DOI] [PubMed] [Google Scholar]
- 44.Wu LT, Ringwalt CL, Williams CE. Use of substance abuse treatment services by persons with mental health and substance use problems. Psychiatr Serv 2003;54:363–369. [DOI] [PubMed] [Google Scholar]
- 45.Green-Hennessy S Factors associated with receipt of behavioral health services among persons with substance dependence. Psychiatr Serv 2002;53:1592–1598. [DOI] [PubMed] [Google Scholar]
- 46.Weisner C Toward an alcohol treatment entry model: A comparison of problem drinkers in the general population and in treatment. Alcohol Clin Exp Res 1993;17:746–752. [DOI] [PubMed] [Google Scholar]
- 47.Ross HE, Lin E, Cunningham J. Mental health service use: A comparison of treated and untreated individuals with substance use disorders in Ontario. Can J Psychiatry 1999; 44:570–577. [DOI] [PubMed] [Google Scholar]
- 48.Henkel D Unemployment and substance use: A review of the literature (1990–2010). Curr Drug Abuse Rev 2011;4: 4–27. [DOI] [PubMed] [Google Scholar]
- 49.Patrick SW, Buntin MB, Martin PR, et al. Barriers to accessing treatment for pregnant women with opioid use disorder in Appalachian states. Subst Abus 2018. [Epub ahead of print]; DOI: 10.1080/08897077.2018.1488336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Steinberg ML, Williams JM, Li Y. Poor mental health and reduced decline in smoking prevalence. Am J Prev Med 2015;49:362–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: A systematic review of the qualitative and quantitative literature. BMJ Open 2014;4:e006414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bruins J, Pijnenborg MG, Bartels-Velthuis AA, et al. Cannabis use in people with severe mental illness: The association with physical and mental health—A cohort study. A Pharmacotherapy Monitoring and Outcome Survey study. J Psychopharmacol 2016;30:354–362. [DOI] [PubMed] [Google Scholar]
- 53.Davis L, Uezato A, Newell JM, Frazier E. Major depression and comorbid substance use disorders. Curr Opin Psychiatry 2008;21:14–18. [DOI] [PubMed] [Google Scholar]
- 54.Siu AL, Bibbins-Domingo K, Grossman DC, et al. Screening for depression in adults: US Preventive Services Task Force Recommendation statement. JAMA 2016;315: 380–387. [DOI] [PubMed] [Google Scholar]
- 55.U.S. Preventive Services Task Force. Final research plan for drug use in adolescents and adults, including pregnant women: Screening. 2016. www.uspreventiveservicestaskforce.org/Page/Document/final-research-plan/drug-use-in-adolescents-and-adults-including-pregnant-women-screening. Accessed March 30, 2018.
- 56.American College of Obstetricians Gynecologists. Screening for perinatal depression. Committee Opinion No. 630. Obstet Gynecol 2015;125:1268–1271. [DOI] [PubMed] [Google Scholar]
- 57.American College of Obstetricians Gynecologists. Alcohol abuse and other substance use disorders: Ethical issues in obstetric and gynecologic practice. Committee Opinion No. 633. Obstet Gynecol 2015;125:1529–1537. [DOI] [PubMed] [Google Scholar]
- 58.Brown JL, Swartzendruber A, DiClemente RJ. Application of audio computer-assisted self-interviews to collect self-reported health data: An overview. Caries Res 2013;47 Suppl 1:40–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bassuk E, Buckner J, Perloff J, Bassuk S. Prevalence of mental health and substance use disorders among homeless and low-income housed mothers. Am J Psychiatry 1998; 155:1561–1564. [DOI] [PubMed] [Google Scholar]


