ABSTRACT
Telehealth is a tool used to diagnose and treat patients at a distance. Telehealth quickly became essential during the COVID-19 pandemic as a result of stay-at-home orders. Regulatory waivers encouraged the use of telehealth as an alternative to the in-person encounter to limit the spread of disease. The pandemic incited a rapid growth in telehealth, and new legislation, new technologies, and providers new to virtual care changed the delivery of traditional telehealth. Postpandemic planning is necessary to support the safe integration of telehealth in the health care system. The purpose of this article is to discuss the current issues affecting telehealth and offer recommendations for safer virtual care. Critical considerations, beginning with an assessment of remote patient acuity, are needed to ensure the standard of care for telehealth is equivalent to the in-person setting. A triage protocol to screen patients seeking virtual services is required to prevent underestimation of severity of illness, sort patients to place of service, and determine if a need exists to escalate to an in-person evaluation or higher level of care. A standard approach to triage may minimize the risks to patient safety and support the appropriate use of telehealth technologies.
Keywords: Acuity, nurse practitioners, telehealth, telemedicine, triage
Introduction
The COVID-19 pandemic accelerated the rapid adoption of telehealth into the U.S. health care system in response to physical distancing and quarantine guidelines (Byrne, 2020). The Centers for Disease Control and Prevention (CDC) issued guidance to health care systems during the emergence of the pandemic and recommended the use of remote services, such as telehealth, to health care systems to reduce exposure to ill persons, preserve personal protective equipment, and prevent surges of COVID-19 cases in hospitals (CDC, 2020). A Morbidity and Mortality Weekly Report noted the potential of telehealth to increase access to care, reduce disease burden for patients and providers, and preserve the shortage of protective equipment and provider capacity (Koonin et al., 2020). To further support the use of telehealth during the pandemic, several regulations on the provisions of telehealth, reimbursement policies, and the Health Insurance Portability and Accountability Act (HIPAA) were relaxed to ensure health care access for Americans (Byrne, 2020; Centers for Medicare & Medicaid Services[CMS], 2021a; Koonin et al., 2020; Patel et al., 2021; Portnoy et al., 2020; United States Department of Health and Human Services [USDHHS], 2020). The purpose of this article was to inform practitioners of the current issues affecting telehealth and provide recommendations to shift toward safer telehealth practice.
Telehealth versus telemedicine
Universal definitions for telehealth terminology do not exist and are often used interchangeably (National Consortium of Telehealth Resource Centers [NCTRC], 2019). Telehealth, oftentimes mistakenly referred to as telemedicine, is the broad word used to describe telecommunication and remote health services delivered by a wide range of professionals, which includes nonclinical services, such as continuing education for providers (American Telemedicine Association [ATA], 2020; HealthIT.gov, 2020). Telemedicine, also referred to as video visits or virtual appointments, is a subset of telehealth and is specifically used to refer to the delivery of clinical services using technology to replace the in-person office appointment by way of real-time audio and video interaction (CDC, 2020; HealthIT.gov, 2020; Shaheen et al., 2020). Physicians, physician assistants, and nurse practitioners using telehealth are required to use telemedicine technology within existing regulatory frameworks to safely and effectively increase access to health care in settings to include the outpatient clinic, emergency department, acute care setting, urgent care, home, workplace setting, skilled nursing facility, and/or at the scene of an illness or injury (Shaheen et al., 2020).
Different telehealth modalities that connect providers and patients by way of technology are synchronous, asynchronous, and remote patient monitoring. Synchronous telehealth is real-time telephone or live audio and video interaction between a health provider and patient for the diagnosis and treatment of health conditions (ATA, 2020; NCTRC, 2021). Asynchronous telehealth is store-and-forward technology that records a history and is sent to a health provider or specialist to be reviewed at a different time. Remote patient monitoring is a type of asynchronous telehealth that allows for frequent monitoring of health data to assess for trends in chronic disease management (ATA, 2020; CDC, 2020).
Telemedicine standards
The American Academy of Family Physicians (AAFP, 2019) supports the use of telemedicine to improve health when practices are consistent with the standards of care. Telemedicine providers are expected to uphold the same standards of professional care as in-person interactions and adhere to telehealth regulations governing virtual practices (American Medical Association [AMA], 2021). Diagnosis and prescription writing solely based on an online form or phone-based consult is not considered an acceptable standard of care (Daniel & Sulmasy, 2015). AMA recommends providers ensure they have the necessary information to make well-grounded clinical decisions when a physical examination cannot be completed and take steps toward overcoming limitations when using telemedicine.
Rules and regulations
Telemedicine rules and regulations differ from state-to-state, and providers are responsible for ensuring their use of telemedicine is compliant with federal and state regulations (AAFP, 2019; AMA, 2018; Byrne, 2020; Daniel & Sulmasy, 2015). A wide variability of telehealth practices exists among providers (Bashshur et al., 2020; CDC, 2020). Practice variations include methods of establishing a new provider–patient relationship, types of virtual services delivered, and telehealth modality used to provide telemedicine services, such real-time audio and video technology versus audio-only encounters.
Pandemic telehealth
Telehealth has been the well-accepted pandemic safety net allowing health care providers to treat mildly ill patients without a physical presence (Koonin et al., 2020; Portnoy et al., 2020). The pandemic has highlighted a need for an evidence-based integrated telehealth framework to support the wide adoption of telemedicine with the expectation that technology will improve health care outcomes (Bashshur et al., 2020; Ohannessian et al., 2020). Large-scale telehealth adoption after the pandemic will depend on regulation and reimbursement; however, the continued utilization of virtual services after in-person primary care resumed suggests sustained interest in telehealth in the future (Byrne, 2020; Koonin et al., 2020; USDHHS, 2020).
Pandemic changes to telehealth practices
Emergency declarations and blanket waivers as a result of the pandemic permitted many practitioners using telehealth for the first time, the ability to deviate from standard practices, such as forgoing the telemedicine requirement for synchronous audio and video communication (CMS, 2021b). Federal legislation, such as the Audio-Only Telehealth Act (H.R. 9035, 2020), permitted audio-only interaction for certain services, which removed the video interaction of a patient–provider telemedicine encounter. In a prepandemic world, audio-only interaction was not considered telemedicine. Making a diagnosis and providing treatment solely based on audio-only communication was considered unprofessional conduct in some states (AMA, 2018). Modifying telehealth practices, such as removal of the video requirement for a telemedicine encounter, creates challenges for obtaining vital data for patient care decisions and interpreting behavioral clues necessary for a remote observational examination (Kichloo et al., 2020).
Provider telehealth competency
The rapid growth of telehealth has not accounted for the necessity of telehealth provider education (Rutledge et al., 2021). Provider telehealth education is widely variable, which is a risk for the delivery of substandard care. Many health care programs do not include telemedicine training within the curriculum (Porter, 2020). Telehealth practices vary among practitioners, and the essential elements to meet the standard of care, such as the required technology, history taking, and objective data collection, may not be similar (Bashshur et al., 2020).
Planning for a standardized telehealth approach
Telemedicine use across patient demographics and conditions varied during the pandemic (Patel et al., 2021). Deliberate planning for the larger and longer lasting uses of telehealth begins with a strategy to minimize risks to patient safety and a method to determine when in-patient care versus virtual care is more appropriate to develop systems in the future that can best support each medical specialty (CDC, 2020; Sikka et al., 2020). Opportunity exists for developing a safer telehealth infrastructure beginning with a standard procedure to screen patients who may be more suitable for an in-person evaluation due to urgency and/or necessity of an adequate physical examination (CDC, 2020; Ohannessian et al., 2020).
Acuity, triage, and patient resources
The term acuity has variation in meaning among practitioners and indicates the physical and psychological status of a patient (Brennan & Daly, 2009). Acuity is categorized differently based on triage system and can be color coded, ranked by number, or described as nonurgent to immediate priority (Napi et al., 2019). Triage scales are often used to sort and categorize patients by level of urgency and determine the resources needed for care (Brennan & Daly, 2009; Merriam-Webster, n.d.). Critical steps can be taken to minimize unintended risks to patient safety through triage protocols prescribed at a system level with consideration for a wide range of complaints. Triage algorithms can assist providers in identifying patients suitable for a telehealth encounter and screen potential vulnerable patients who require an in-person examination, diagnostic studies, and/or require referral for emergency care (Sikka et al., 2020).
Telehealth triage
The different types of triage systems that currently exist are primarily for mass casualty and emergency department sorting and not specific to the telehealth setting (Napi et al., 2019). A standardized telehealth triage tool is lacking, and little is known about the extent of a telehealth-specific triage algorithm for remote triage of patients seeking virtual health care services. No specific criteria exist that identify which types of patients are appropriate for a virtual encounter and which are best managed in-person. Criteria that specify the modality of telehealth based on acuity are also lacking, and practitioners are left to experience and individual decision-making regarding patient prioritization and setting of care. The variability of telehealth prepared practitioners, changing telehealth regulations, acuity concept, and the wide range of telehealth modalities that exist in a rapidly evolving telehealth environment warrants a telemedicine triage system.
Recommendations
Provider education
Current students
Opportunity exists for minimizing variability of telehealth practices to promote safer telehealth through education. The American Association of Colleges of Nursing (AACN) revised document, The Essentials: Core Competencies for Professional Nursing Education, includes a domain on informatics and health care technologies to enable quality and efficient care to achieve a consistent outcome in competency development. Domain 8, Information and Health care Technologies, is defined as information and communication technologies used to manage and improve the delivery of safe and high-quality health care services using best practices and regulatory standards (AACN, 2021).
Program directors are in the position to implement curricular changes for students to develop a unique set of skills and competencies required to use live interactive video and store-and-forward technologies for safe patient care (Porter, 2020). Rutledge et al. (2021) proposed a comprehensive telehealth framework for education to include four domains to guide content for telehealth competencies, which include planning, preparing, providing, and performance evaluation. Didactic education and simulation are methods for building competency in telehealth delivery and technologies along with incorporated clinical experiences (Rutledge et al., 2021).
The National Organization of Nurse Practitioner Faculties (NONPF, 2018) provides an online Telehealth Portal with faculty resources for NP education. NONPF recommends a set of telehealth competencies that students require to effectively deliver care using technology. Students need educational content to include telehealth definitions, rules and regulations, emergency waivers, reimbursement, telepresence, ethics, and hands-on practice with equipment and technologies.
Providers in practice
Telehealth education is available to providers in practice. NCTRC is funded by the USDHHS to provide the nation with telehealth education (NCTRC, 2021). Twelve regional and two national Telehealth Resource Centers (TRCs) are expertly staffed and tasked with helping practices implement successful and sustainable telehealth programs. The TRCs provide education, technical assistance, and a variety of resources to support providers using telehealth to include checklists, toolkits, and fact sheets. The TRCs offer a resource center with asynchronous provider education and hosts live webinars covering a wide range of telehealth topics to include practice and policy issues.
Telehealth triage process
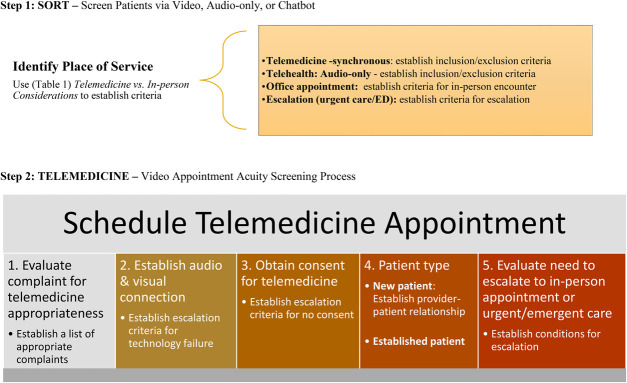
Several factors must be considered when determining the most appropriate place of service for patients and begins with triage. Triage is necessary for telemedicine effectiveness, maintaining standards of care, and safeguarding patient safety (Loeb et al., 2020). A standard telehealth triage decision support is needed for consistent telemedicine outcomes. A telehealth triage process should consider the factors affecting the appropriateness of care setting, in-person versus virtual (Table 1), and identify inclusion and exclusion criteria uniquely tailored to the organization. Patients who are considered appropriate for a telemedicine encounter must also meet criteria for the most appropriate telehealth modality in the context of safety, such a real-time audio and video encounter versus an audio-only evaluation. A telehealth triage protocol (Figure 1) should include decision support that considers escalation to in-person evaluations at different points of the telehealth intake. The triage protocol should provide a method for providers to identify vulnerable patients who require transition to an in-person evaluation and include escalation criteria to ensure the appropriate use of telehealth services in the most appropriate setting (Sikka et al., 2020). An escalation plan should be included in the triage process to address technology and/or connection failures required for a successful telehealth appointment (Shaheen et al., 2020).
Table 1.
Telemedicine versus in-person considerations
| Factors Influencing Appropriateness for Telehealth Encounter | |
| Telehealth specialty setting, place of service | • Outpatient—primary care, endocrine, cardiology, neurology, gastroenterology, orthopedic, urology, geriatrics, pediatrics, nephrology, pulmonology/sleep, pain management, rural care, urgent care, school, military • Emergency department (ED), prehospital emergency medical services • Nursing home/skilled nursing facility • Remote patient monitoring at home • Hospital, critical care unit • Behavioral health • Teaching/education (Shaheen et al., 2020; NCTRC, 2021) |
| Patient setting | Remote • Patient at home and provider at another location Originating • Patient at clinic/site with telepresenter (i.e., patient at a clinic or hospital with medical assistant or nurse and is assisting provider at another location with the appointment (Shaheen et al., 2020; NCTRC, 2021) |
| Provider factors | Regulations • License and certification • Confidentiality/HIPAA • Informed consent • Business associate agreement(s) • Understand telehealth legislation and reimbursement policies prepandemic, pandemic changes, and postpandemic • Telemedicine practices and documentation, dedicated telehealth space Education & experience • Telehealth didactic and/or hands-on training • Comfort level with technology • Telepresence competency • Triage ability • Ability to perform and interpret a virtual physical examination based on complaint type • Ability to select most appropriate telehealth modality based on presenting complaint • Ability to accommodate patients who are hard of hearing or have decreased vision Technology • Equipment, computer, software/applications • Electronic health record • Functioning camera, microphone • Internet, Wi-Fi, and/or cellular connection (Shaheen et al., 2020; Bashshur et al., 2020; Loeb et al., 2020) |
| Patient factors | • Acuity and severity of illness: nonurgent, low risk • Age • Gender/condition based • Preference for telemedicine • Level of comfort and familiarity with technology • Social/health disparities—“digital divide” o Access to internet or Wi-Fi o Access to functioning technology (smartphone or computer with camera and microphone) o Insurance type o Number of comorbidities o Ability to describe symptoms and severity • Complaint o Acute, common complaint (Shaheen et al., 2020; AMA, 2018; Bashshur et al., 2020; CDC, 2020; Kichloo et al., 2020; Loeb et al., 2020; Patel et al., 2021) |
| Category/encounter type | Provider–patient encounter • New patient—criteria for establishing a provider–patient relationship • Established patient • Specialist consult • Scheduled appointment • Unscheduled appointment • Follow-up Provider–provider encounter • Consultation (AMA, 2018) |
| Appointment type & modality for patients requesting telehealth | Acute appointment*—Triage required to assess patient acuity and appointment type should be matched with most appropriate telehealth modality or determine need for escalation • Audio and video encounter with digital medical kit (i.e., electronic stethoscope, electronic otoscope) • Audio and video encounter without digital medical kit • Audio only: no access to observational assessment Chronic care appointment or follow-up*—Triage required to match patient acuity with telehealth modality or determine need for escalation • Audio and video encounter with digital medical kit (i.e., electronic stethoscope, electronic otoscope) • Audio and video encounter without digital medical kit • Audio only: no access to observational assessment In-person • Triage tool and criteria needed to determine in-person vs. virtual encounter • Consider resources needed to address patient complaint Higher level of care criteria • Triage tool needed to assess need for escalation of care Consult (specialist, radiologist) • Synchronous audio and video • Asynchronous • Audio-only (Kichloo et al., 2020; NCTRC, 2021) |
| Patient acuity, severity, & resources | Triage method • Chatbot • Audio-only triage line • Synchronous audio and video consultation • Telehealth triage tool for safer telehealth • Electronic health record tool Severity of illness • Physical and psychological status of patient Resources • Number and type of resources necessary to address the patient complaint virtually versus in-person o Laboratory and diagnostic studies o Parenteral medication o Special procedure o Specialist consult (Brennan & Daly, 2009; Kichloo et al., 2020) |
| Telehealth utilization | • Telehealth as triage tool to determine appropriateness for telehealth, in-person, or escalation of care • Low-risk urgent care • Telemedicine to diagnose and treat a complaint/condition • Telemedicine as a follow-up—posthospital discharge, check-in • Telemedicine for specialty consultation (CDC, 2020; Kichloo et al., 2020; Portnoy et al., 2020; Sikka et al., 2020) |
| Physical examination | Audio and video • With digital medical kit • Observational assessment—no digital medical kit Audio only • No observational assessment or physical examination—requires a triage method for appropriateness of audio-only within scope of state and federal legislation (Kichloo et al., 2020) |
| Escalation or follow-up | Escalation • Improper functioning technology • High patient acuity • Number of resources required to treat patient Follow-up appointment • In-person, telehealth, or hospital discharge • Assessment of response to treatment plan and/or prescribed medication • Post-telemedicine virtual check-in (Sikka et al., 2020) |
Consider synchronous audio/video for an unscheduled telehealth appointment.
Figure 1.
Illustrates the two-step triage process for determining the appropriateness of care management via telemedicine. The process is intended to be adaptable across settings in the approach to the patient seeking telehealth services. Step 1 begins with the initial sorting (triage) of patients via video, audio-only, or chatbot and establishes place of services using (Table 1) considerations for telemedicine versus in-person care. The place of service requires individualized inclusion/exclusion criteria for synchronous telemedicine, audio-only telehealth, in-person office appointment, or escalation of care. Step 2 is the video appointment acuity screening process for patients deemed appropriate for synchronous telemedicine. The process for scheduling a telemedicine appointment requires establishing criteria for appropriateness of telemedicine and screening for need for escalation based on the requirements for a telemedicine appointment.
Research
ACEP noted the absence of best practices for telehealth for acute unscheduled appointments, with a specific need for guidance and standards for remote telehealth practices (Shaheen et al., 2020). With the exponential growth of telehealth and technology during the pandemic, opportunities exist to explore a method that health care providers can use to differentiate the most appropriate setting of care. A valid and reliable triage tool is needed for providers to identify urgent/emergent patients who require an escalation of care (Sikka et al., 2020). A telehealth triage tool can assist in screening complaints ineligible for telehealth to support safe care in a variety of settings.
Conclusion
Nurse practitioners are in the position to lead initiatives for safer telehealth through the standardization of triage. The goal of telehealth triage is to evaluate the appropriateness of complaints for telemedicine and redirect more acute patients to an in-person evaluation. A shift from reactional to deliberate telehealth is needed to ensure patients receive the standard of care, regardless of place of service. Critical next steps include provider education and development of a valid and reliable triage tool necessary for safer virtual care.
Footnotes
Competing interests: The authors report no conflicts of interest.
M. M. Kobeissi and S. D. Ruppert conceptualized the article idea and content. M. M. Kobeissi wrote the original draft. S. D. Ruppert contributed to content development, meaningful revision, and editing of the manuscript throughout the process.
References
- American Academy of Family Physicians (AAFP). (2019). Telemedicine. AAFP. https://www.aafp.org/dam/AAFP/documents/advocacy/health_it/telehealth/BKG-Telemedicine.pdf. [Google Scholar]
- American Association of Colleges of Nursing (AACN). (2021). The Essentials: Core competencies for professional nursing. AACN. https://www.aacnnursing.org/Portals/42/AcademicNursing/pdf/Essentials-2021.pdf. [Google Scholar]
- American Medical Association (AMA). (2018). Establishment of a patient-physician relationship via telemedicine. AMA. https://www.ama-assn.org/system/files/2018-10/ama-chart-telemedicine-patient-physician-relationship.pdf. [Google Scholar]
- American Medical Association (AMA). (2021). Ethical practice in telemedicine. AMA. https://www.ama-assn.org/delivering-care/ethics/ethical-practice-telemedicine. [Google Scholar]
- American Telemedicine Association (ATA). (2020). 2020 telehealth taxonomy. ATA. https://www.americantelemed.org/resource/why-telemedicine/. [Google Scholar]
- Bashshur R. L. Frenk J. M., & Shannon G. W. (2020). Perspective: Beyond the COVID pandemic, telemedicine, and healthcare. Telemedicine and e-Health, 26, 1–4. 10.1089/tmj.2020.0328. [DOI] [PubMed] [Google Scholar]
- Brennan C. W., & Daly B. J. (2009). Patient acuity: A concept analysis. Journal of Advanced Nursing, 65, 1114–1126. [DOI] [PubMed] [Google Scholar]
- Byrne M. D. (2020). Telehealth and the COVID-19 pandemic. Journal of PeriAnesthesia Nursing, 35, 548–551. 10.1016/j.jopan.2020.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicaid and Medicaid Services (CMS). (2021b). COVID-19 emergency declaration blanket waivers for health care providers. CMS. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf. [Google Scholar]
- Centers for Medicare and Medicaid Services (CMS) (2021a). Coronavirus waivers & flexibilities. CMS. https://www.cms.gov/about-cms/emergency-preparedness-response-operations/current-emergencies/coronavirus-waivers. [Google Scholar]
- Centers for Medicare and Medicaid Services. (2020). Using telehealth to expand access to essential health services during the COVID-19 pandemic. CMS. https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html. [Google Scholar]
- Daniel H., Sulmasy L. S. (2015). Policy recommendations to guide the use of telemedicine in primary care settings: An American College of Physicians position paper. Annals of Internal Medicine, 163, 787–789. https://www.acpjournals.org/doi/10.7326/M15-0498. [DOI] [PubMed] [Google Scholar]
- HealthIT.gov. (2020). Telemedicine and telehealth. https://www.healthit.gov/topic/health-it-health-care-settings/telemedicine-and-telehealth. [Google Scholar]
- Kichloo A. Albosta M. Detloff K. Wani F. El-Amir Z. Singh J. Aljadah M. Chakinala R. Kanugula A. Solanki S., & Chugh S. (2020). Telemedicine, the current COVID-19 pandemic and the future: A narrative review and perspectives moving forward in the USA. Journal of Family Medicine and Community Health, 8, e000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koonin L. M., Hoots B., Tsang C. A., Leroy Z., Farris K., Jolly B. T., Antall P., McCabe B., Zelis C. B., Tong I., & Harris A. M. (2020). Trends in the use of telehealth during the emergence of the COVID-19 pandemic—United States, January-March 2020. MMWR. Morbidity and Mortality Weekly Report, 69, 1595–1599. https://www.cdc.gov/mmwr/volumes/69/wr/mm6943a3.htm#:∼:text=During%20the%20early%20pandemic%20period%20in%202020%2C%20the%20percentage%20of,March%20(p%3C0.05). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb A. E. Rao S. S. Ficke J. R. Morris C. D. Riley L. H., & Levin A. S. (2020). Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. American Academy of Orthopedic Surgeons, 28, e469–e476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merriam-Webster and Triage (n.d.).. In Merriam-Webster.com dictionary. https://www.merriam-webster.com/dictionary/triage. Retrieved April 3, 2021. [Google Scholar]
- Napi N. M. Zaidan A. A. Zaidan B. B. Albahri O. S. Alsalem M. A., & Albahri A. S. (2019). Medical emergency triage and patient prioritization in a telemedicine environment: A systematic review. Health and Technology, 9, 679–700. 10.1007/s12553-019-00357-w. [DOI] [Google Scholar]
- National Consortium of Telehealth Resource Centers (NCTRC) (2021). Telehealth basics. NCTRC. https://telehealthresourcecenter.org/collections/telehealth-basics/. [Google Scholar]
- National Organization of Nurse Practitioner Faculties. (2018). NONPF supports telehealth in nurse practitioner education [white paper]. NONPF. https://cdn.ymaws.com/www.nonpf.org/resource/resmgr/2018_Slate/Telehealth_Paper_2018.pdf. [Google Scholar]
- Ohannessian R. Duong T. A., & Odone A. (2020). Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: A call to action. JMIR Public Health and Surveillance, 6, e18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel S. Mahrotra A. Huskamp H. A. Uscher-Pines L. Ganguli I., & Barnett M. L. (2021). Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Affairs, 2, 349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Permanency for Audio-Only Telehealth Act, H.R.9035, 116th Cong. (2020). https://www.congress.gov/bill/116th-congress/house-bill/9035/text?r=2&s=1. [Google Scholar]
- Porter S. (2020). Study: FM residents need more telehealth training. AAFP. https://www.aafp.org/news/education-professional-development/20200121residenttelehealth.html. [Google Scholar]
- Portnoy J. Waller M., & Elliot T. (2020). Telemedicine in the era of COVID-19. American Academy of Allergy, Asthma, & Immunology, 8, 1489–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutledge C. Mason A. M. Behnke L., & Downes L. (2021). Telehealth competencies for nursing education and practice. Nurse Educator. 46, 300–305. doi: 10.1097/NNE.0000000000000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaheen E. Davidson P. Mendoza P. Tannebaum R. Cichon P. Earnst D. Guyette F. Joshi A. Landry K., & Sikka N. (2020). Practice guidance for emergency telehealth and acute unscheduled care telehealth. American College of Emergency Physicians. https://www.acep.org/globalassets/sites/acep/media/sections/emergency-telehealth/acep-practice-guidance-for-emergency-telehealth-and-acute-unschedulel-care-telehealth-final.pdf. [Google Scholar]
- Sikka N. Willis J. Fitall E. Hall K. K., & Gale B. (2020). Telehealth and patient safety during the COVID-19 response. Agency for Healthcare Research and Quality. https://psnet.ahrq.gov/perspective/telehealth-and-patient-safety-during-covid-19-response. [Google Scholar]
- United States Department of Health & Human Services. (2020). Medicare beneficiary use of telehealth visits: Early data from the start of the COVID-19 pandemic. USDHHS. https://aspe.hhs.gov/system/files/pdf/263866/hp-issue-brief-medicare-telehealth.pdf. [Google Scholar]