Abstract
Vaccine hesitancy can hinder the successful roll-out of vaccines. This paper examines COVID-19 vaccine hesitancy in the European Union, drawing from a large-scale cross-national survey covering all 27 EU Member States, carried out between February and March 2021 (n = 29,755). We study the determinants of vaccine hesitancy, focusing on the role of social media use. In multivariate regression models, we find statistically significant (p < 0.05) impacts on vaccine hesitancy of heavy use of social media and using social media as a main source of news. However, the effect of social media and the drivers of vaccine hesitancy vary depending on the reason for hesitancy. Most notably, hesitancy due to health concerns is mainly driven by physical health status and less by social media use, while views that COVID-19 risks are exaggerated (or that COVID-19 does not exist) are more common among men, people in good health, and those using social media as their main source of news.
Keywords: COVID-19, Vaccine, Hesitancy, Hesitancy reasons, Social media, News sources
1. Introduction
Vaccines play a crucial role in the response to the COVID19-crisis. They can boost the immune response against the original SARS-CoV-2 virus, as well as provide protection against the emerging viral variants that could render existing vaccines ineffective.
The vaccine rollout in the European Union has been difficult, with Member States facing continuous challenges in relation to the limited supply of vaccines. Beyond issues related to the logistics of developing, testing, manufacturing and distributing vaccines, the public’s confidence in and acceptance of vaccines is far from universal. Effective and clear communication about the efficacy and safety of vaccines likely plays a crucial role in addressing vaccine hesitancy.
Vaccine hesitancy is defined by the World Health Organisation as a “delay in acceptance or refusal of vaccines despite availability of vaccination services” [1]. While vaccine hesitancy can be traced back to the 1800s [2], it has recently become a serious threat that can hinder the efforts that have led to the advancement of human health through science [3]. This has become even more relevant during the COVID-19 pandemic, with vaccine hesitancy potentially undermining communities' ability to reach thresholds of coverage necessary for herd immunity against COVID-19 – unnecessarily perpetuating the pandemic and resulting in untold suffering and deaths [4].
Vaccine hesitancy is a complex and dynamic social process that has only been studied in more depth in recent years [5]. An individual's attitude towards vaccines can range from complete refusal of all vaccines to complete vaccine acceptance. Existing literature has identified several drivers of vaccine hesitancy, both at the individual and the societal level [6], [7]. More recently, social media use, and information sources more generally, have been identified as potentially important drivers of vaccine hesitancy [8], [9], [10], [11], [12], [13], [14].
Social media can serve as a forum for the proliferation of vaccination misinformation and as a platform for the anti-vaccination movement [11]. Well before the COVID-19 pandemic, it has been demonstrated that exposure to vaccine-critical websites and blogs negatively impacts the intention to vaccinate [15]. Furthermore, it has been found that using social media as a source of health information has a significant negative association with influenza vaccine uptake [16]. Misinformation regarding COVID-19 and vaccination against SARS-CoV-2 emerged on social media platforms, threatening to erode public confidence [9].
Understanding vaccine hesitancy in times of COVID-19 and the role played by social media is of importance for the success of the efforts to end the pandemic. A great deal of research has been carried out on the socio-demographic determinants of vaccine hesitancy – ranging from qualitative single-country work to large scale surveys across dozens of countries [17], [18], [19], [20], [21]. However, to the best of our knowledge, this paper presents the first large-scale cross-national analysis in the European Union, covering all Member States, on how social media use influences vaccine hesitancy generally, and the reasons for vaccine hesitancy more specifically.
We examine the links between COVID-19 vaccine hesitancy and a comprehensive set of covariates: individual socio-demographic characteristics, health status, exposure to COVID-19 (close persons having been diagnosed with or died from COVID-19), as well as time spent on social media and the use of social media as a source of news. We explore the reasons for hesitancy, distinguishing between concerns for own health, lack of trust in vaccine safety, and perceived low risk of illness (views that the risk of COVID-19 is exaggerated, or COVID-19 does not exist). We test and affirm the hypothesis that the impact of social media on vaccine hesitancy operates not only via the time spent on social media, but also whether social media is used as main source of news.
The rest of the paper is organised as follows. Section 2 outlines the methodology including the study design and participants, survey questions and statistical analyses. Section 3 discusses the results and contextualises them in relation to existing research. Section 4 concludes.
2. Methods
2.1. Study design and participants
We conducted a cross-sectional, population-based online survey using a structured questionnaire from February 15th to March 30th 2021, covering adults aged 18 and over, living in the European Union. The recruitment of the participants was carried out through snowball sampling methods as well as via promotions on social media. The survey was the third round of the “Living, working and COVID-19” e-survey that was initiated in April 2020. The second round of the survey was carried out between June and July 2020. The third round of the survey collected 46,800 responses. The survey investigates the impacts of the pandemic on living and working conditions. It is the only large-scale survey providing EU-wide information on attitudes towards vaccination and social media use, in addition to the necessary socio-demographic control variables.
The majority of the e-survey questions were based on questions contained in the European Quality of Life Survey (EQLS) [22] and the European Working Conditions Survey (EWCS) [23], ensuring that questions were tested and passed cognitive quality controls before the e-survey was fielded. Being a non-probabilistic survey and therefore non-representative of the underlying population, an a posteriori weighting was performed.1 All analyses in this paper are weighted to population benchmarks to account for survey design and non-response, in order to reflect the socio-demographic composition of the European Union and its Member States. The socio-demographic characteristics of the analysis sample are presented in Appendix Table A1.
2.2. Dependent variables
The intention of the non-vaccinated respondents to get vaccinated was measured by the question “How likely or unlikely is it that you will take the COVID-19 vaccine when it becomes available to you?” and scored with a 5-point scale, ranging from “very likely” to “very unlikely”. The distribution of the answers is presented in Table 1 . Overall, 71% are (very or rather) likely to take the vaccine, while 8% are neutral (neither likely nor unlikely) and 21% are (very or rather) unlikely to take the vaccine. We define vaccine hesitancy using a binary indicator variable: an individual is defined as hesitant if they respond to the question about likelihood of vaccination with “rather unlikely” or “very unlikely”.
Table 1.
Likelihood to vaccinate.
| % | N | |
|---|---|---|
| Very likely | 58.3 | 17,573 |
| Rather likely | 13.0 | 4,179 |
| Neither likely nor unlikely | 8.0 | 2,314 |
| Rather unlikely | 6.5 | 2,042 |
| Very unlikely | 14.3 | 3,647 |
| Total | 100.0 | 29,755 |
Notes. Answers to question “How likely or unlikely is it that you will take the COVID-19 vaccine when it becomes available to you?” Weighted data.
Vaccine hesitant respondents were asked a follow-up question about the reason(s) why it is unlikely that they would take the COVID-19 vaccine. Options included 5 possible reasons, allowing multiple response options. Two of the reasons capture views that the associated risks are perceived to outweigh the benefits (i.e., possible implications of vaccination on respondent's own health; concern about vaccine safety) while two capture that the respondent perceives risk associated with COVID-19 to be low (i.e., exaggeration of COVID-19 risk; scepticism about the existence of COVID-19). A fifth answer option captured other reasons (not elaborated in the questionnaire).
Table 2 presents the percentages of vaccine-hesitant respondents who selected the various reasons for why it is unlikely that they will take the COVID-19 vaccine. Vaccine safety is the most common reason given (reported by 61% of the vaccine-hesitant respondents), followed by the risk of COVID-19 being exaggerated (41%), concern that vaccine will make health issues worse (28%), and the view that COVID-19 does not exist (6%). Other reasons were quoted by 12% of vaccine-hesitant respondents. As multiple response options were allowed, the percentages do not sum to 100. Following analyses of the characteristics of people giving different reasons, in the multivariate models we group reasons into the following three categories: i) health concerns, ii) vaccine safety, and iii) exaggeration.
Table 2.
Reasons for vaccine hesitancy.
| % | |
|---|---|
| I am worried that it will make my health issues worse | 27.8 |
| I do not trust the safety of the vaccine | 60.9 |
| I think the risk of COVID-19 is exaggerated | 41.2 |
| I think COVID-19 doesn't exist | 6.4 |
| Other reason | 12.0 |
| Observations | 5,689 |
Notes. Answers to question “Why is it unlikely that you will take the COVID-19 vaccine?” Weighted data.
2.3. Methodology
From the full sample (n = 46,800) of the third round of the survey, we restrict our analysis to individuals who have not received a COVID-19 vaccine and therefore were asked the question about vaccination likelihood. After removing these observations, the remaining sample size reduces to 42,210. Further, following Schwarzinger et al. (2021), individuals with history of SARS-CoV-2 infection are excluded, reducing the sample size to 38,192 [27]. The multivariate analysis requires non-missing values for all the included variables, bringing the final analysis sample size to 29,755. The characteristics of the analysed sample are described in Appendix Table A1.
Logistic regression models were estimated using maximum likelihood techniques with Stata statistical software (16.1) logit command.2 Marginal effects of variables were calculated at the mean values of the covariates. Multivariate models allow the investigation of the independent effect of social media use (and other explanatory variables) on the likelihood of a person being vaccine hesitant (and on the likelihood of a person reporting a specific reason for vaccine hesitancy). Accounting for the confounding effect of age, for example, is important in understanding the relationship of social media use and vaccine hesitancy. This is because age and social media use correlated, while also being correlated with vaccine hesitancy. In addition, as at the time of the survey, EU countries were experiencing different stages of the COVID-19 pandemic, country indicator variables were added in order to control for country heterogeneity. Independent variables were added step-wise in order to examine their correlations and joint impacts on vaccine hesitancy.
3. Results
3.1. Country variation in vaccine hesitancy
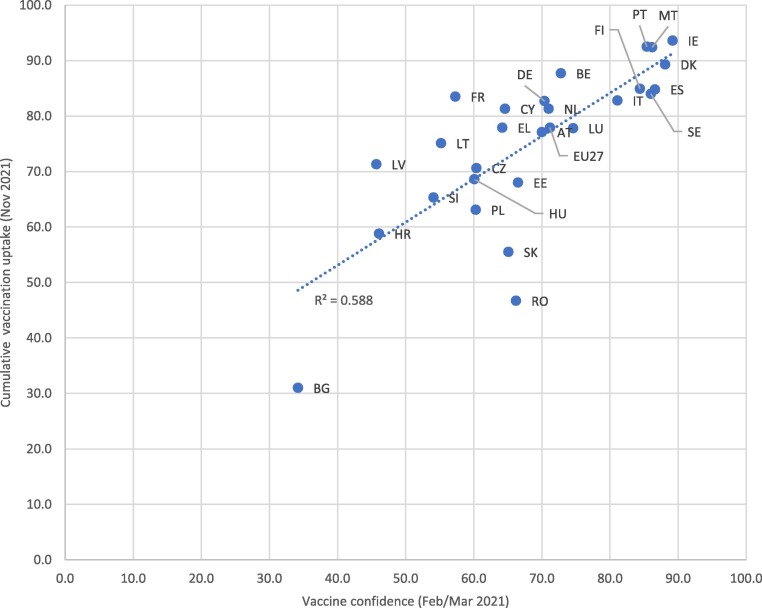
Table 3 presents vaccine hesitancy statistics by country. The overall rate of vaccine hesitancy is 20.8%, varying considerably among Member States, with an east–west divide discernible. Vaccine hesitancy is below 10% in most of the Nordic countries (Denmark, Finland and Sweden) and some South Mediterranean countries (Italy, Portugal and Spain) as well as Ireland. Hesitancy is above 30% in some eastern European countries: Bulgaria, Croatia, Latvia and Slovenia. The last column on Table 3 presents the realised cumulative uptake of full vaccination among adults (18+) in each EU Member State as of Week 48 (in November) of 2021.3 It is evident that the vaccination intentions recorded in the survey data correspond closely with the subsequent vaccine uptake, with the ranking of countries similar across both measures. Appendix Fig. A1 shows a graphical representation of this relationship, illustrating a relatively strong association, with a correlation coefficient of 0.77.
Table 3.
Vaccination likelihood by country.
| Likely | Neutral | Unlikely | Total | N | Realised uptake* | |
|---|---|---|---|---|---|---|
| % | % | % | % | % | ||
| Austria | 70.0 | 8.1 | 21.9 | 100.0 | 609 | 77.1 |
| Belgium | 72.8 | 8.2 | 19.0 | 100.0 | 1,123 | 87.7 |
| Bulgaria | 34.2 | 6.2 | 59.6 | 100.0 | 1,554 | 31.0 |
| Croatia | 46.1 | 12.8 | 41.2 | 100.0 | 911 | 58.8 |
| Cyprus | 64.6 | 11.7 | 23.7 | 100.0 | 470 | 81.3 |
| Czechia | 60.4 | 9.8 | 29.7 | 100.0 | 882 | 70.6 |
| Denmark | 88.1 | 6.2 | 5.7 | 100.0 | 944 | 89.3 |
| Estonia | 66.5 | 7.7 | 25.8 | 100.0 | 670 | 68.0 |
| Finland | 84.4 | 3.5 | 12.2 | 100.0 | 797 | 84.9 |
| France | 57.3 | 14.1 | 28.6 | 100.0 | 726 | 83.5 |
| Germany | 70.4 | 7.3 | 22.3 | 100.0 | 2,032 | 82.7 |
| Greece | 64.2 | 13.3 | 22.4 | 100.0 | 3,928 | 77.9 |
| Hungary | 60.1 | 12.8 | 27.1 | 100.0 | 2,047 | 68.6 |
| Ireland | 89.2 | 3.1 | 7.6 | 100.0 | 2,096 | 93.6 |
| Italy | 81.1 | 5.4 | 13.5 | 100.0 | 1,313 | 82.8 |
| Latvia | 45.7 | 8.6 | 45.7 | 100.0 | 704 | 71.3 |
| Lithuania | 55.2 | 13.8 | 31.0 | 100.0 | 1,180 | 75.1 |
| Luxembourg | 74.6 | 8.9 | 16.5 | 100.0 | 287 | 77.8 |
| Malta | 86.2 | 7.1 | 6.6 | 100.0 | 423 | 92.4 |
| Netherlands | 71.0 | 5.6 | 23.5 | 100.0 | 607 | 81.3 |
| Poland | 60.3 | 7.1 | 32.5 | 100.0 | 753 | 63.1 |
| Portugal | 85.4 | 4.5 | 10.1 | 100.0 | 1,588 | 92.5 |
| Romania | 66.2 | 10.6 | 23.3 | 100.0 | 959 | 46.7 |
| Slovakia | 65.1 | 8.3 | 26.6 | 100.0 | 772 | 55.5 |
| Slovenia | 54.1 | 6.9 | 39.0 | 100.0 | 659 | 65.3 |
| Spain | 86.6 | 6.4 | 7.1 | 100.0 | 1,083 | 84.8 |
| Sweden | 86.0 | 4.4 | 9.6 | 100.0 | 638 | 84.0 |
| Total | 71.2 | 8.0 | 20.8 | 100.0 | 29,755 | 77.9 |
Notes. Weighted data. *Cumulative uptake (%) of full vaccination as of week 48 of 2021 among adults (18+), obtained from the online database of COVID-19 Vaccine Tracker of the European Centre for Disease Prevention and Control.
Fig. A1.
Vaccine confidence (Feb/March 2021) and realised cumulative vaccination uptake (Week 48, November 2021), by EU Member State Notes. Vaccine confidence data are weighted. Vaccine uptake data have been obtained from the COVID-19 Vaccine Tracker of the European Centre for Disease Prevention and Control.
3.2. Bivariate determinants of vaccine hesitancy
Bivariate associations between vaccine hesitancy and individual-level predictors are presented in Table 4, Table 5 . Social media use is measured in two ways: intensity of use (the time spent using social media, e.g. Facebook, Twitter, Instagram) and type of use (the respondent's main source of news being social media or blogs, e.g. Facebook, Twitter, Instagram, Youtube). Individuals who use social media heavily (more than 3 h daily) have higher rates of vaccine hesitancy in comparison with people who use social media less than daily. A sizeable difference in hesitancy rates is observed between people who use social media or blogs as their main source of news, in comparison with people who use press as their main source of news.
Table 4.
Vaccination likelihood by individual characteristics (1/2).
| Likely | Neutral | Unlikely | Total | N | |
|---|---|---|---|---|---|
| % | % | % | % | ||
| Social media use | |||||
| Less than daily | 77.5 | 7.4 | 15.1 | 100.0 | 2,866 |
| Daily: under 3 h | 72.0 | 7.9 | 20.1 | 100.0 | 20,087 |
| Daily: 3 + hours | 65.7 | 8.5 | 25.8 | 100.0 | 6,802 |
| Main news source | |||||
| Press | 79.4 | 6.1 | 14.5 | 100.0 | 12,018 |
| Radio | 74.3 | 6.3 | 19.5 | 100.0 | 2,167 |
| TV | 72.3 | 9.4 | 18.3 | 100.0 | 9,388 |
| Social media or blogs | 51.2 | 10.0 | 38.8 | 100.0 | 6,182 |
| Gender | |||||
| Female | 71.6 | 8.6 | 19.8 | 100.0 | 18,978 |
| Male | 70.8 | 7.3 | 21.9 | 100.0 | 10,777 |
| Age group | |||||
| 18–29 years | 74.0 | 9.5 | 16.6 | 100.0 | 2,429 |
| 30–39 years | 68.9 | 8.0 | 23.1 | 100.0 | 3,756 |
| 40–49 years | 67.4 | 9.0 | 23.6 | 100.0 | 5,529 |
| 50–59 years | 67.9 | 7.4 | 24.6 | 100.0 | 8,022 |
| 60–69 years | 73.5 | 7.3 | 19.2 | 100.0 | 7,245 |
| 70 + years | 76.8 | 7.0 | 16.2 | 100.0 | 2,774 |
| Location type | |||||
| The open countryside | 63.0 | 7.0 | 29.9 | 100.0 | 2,329 |
| A village/small town | 69.0 | 8.4 | 22.6 | 100.0 | 7,939 |
| A medium to large town | 71.3 | 8.4 | 20.3 | 100.0 | 7,720 |
| A city or city suburb | 78.1 | 7.5 | 14.5 | 100.0 | 11,767 |
| Total | 71.2 | 8.0 | 20.8 | 100.0 | 29,755 |
Notes. Weighted data.
Table 5.
Vaccination likelihood by individual characteristics (2/2).
| Likely | Neutral | Unlikely | Total | N | |
|---|---|---|---|---|---|
| % |
% |
% |
% |
||
| Employment status | |||||
| Employed | 72.3 | 7.9 | 19.8 | 100.0 | 14,642 |
| Self-employed | 67.2 | 7.2 | 25.5 | 100.0 | 2,440 |
| Unemployed | 57.6 | 10.7 | 31.8 | 100.0 | 2,805 |
| Ill/disabled | 53.0 | 10.6 | 36.4 | 100.0 | 757 |
| Retired | 74.6 | 7.3 | 18.1 | 100.0 | 7,127 |
| Homemaker | 66.3 | 9.3 | 24.4 | 100.0 | 1,012 |
| Student | 82.8 | 6.6 | 10.6 | 100.0 | 972 |
| Education level | |||||
| Primary education | 67.1 | 11.1 | 21.8 | 100.0 | 541 |
| Secondary education | 68.1 | 8.2 | 23.7 | 100.0 | 9,494 |
| Tertiary education | 79.2 | 6.9 | 13.9 | 100.0 | 19,720 |
| Lives with spouse | |||||
| No | 69.7 | 8.7 | 21.6 | 100.0 | 11,367 |
| Yes | 72.4 | 7.4 | 20.1 | 100.0 | 18,388 |
| Children in household | |||||
| No | 72.3 | 7.7 | 20.0 | 100.0 | 19,407 |
| Yes | 69.1 | 8.6 | 22.3 | 100.0 | 10,348 |
| Self-rated health | |||||
| (Very) bad health | 62.4 | 9.0 | 28.6 | 100.0 | 2,481 |
| Fair health | 69.6 | 9.8 | 20.6 | 100.0 | 9,068 |
| Good health | 74.4 | 7.0 | 18.6 | 100.0 | 13,469 |
| Very good health | 70.0 | 6.3 | 23.7 | 100.0 | 4,737 |
| Chronic health problem / disability | |||||
| No | 71.4 | 6.8 | 21.8 | 100.0 | 16,063 |
| Yes | 71.0 | 9.3 | 19.7 | 100.0 | 13,692 |
| Close person had Covid | |||||
| No | 69.3 | 8.1 | 22.7 | 100.0 | 18,437 |
| Yes | 74.6 | 7.8 | 17.6 | 100.0 | 11,318 |
| Close person died of Covid | |||||
| No | 70.7 | 7.8 | 21.4 | 100.0 | 27,045 |
| Yes | 75.5 | 9.4 | 15.1 | 100.0 | 2,710 |
| Total | 71.2 | 8.0 | 20.8 | 100.0 | 29,755 |
Notes. Weighted data.
Vaccine hesitancy is higher among men than women, has an inverted U-shaped relationship with age, and is higher among people living in the countryside in comparison with people living in cities or city suburbs. When it comes to employment status, vaccine hesitancy is highest among working-age people outside of the labour market, although students are the least likely to be vaccine hesitant. Differences in terms of household composition are not marked. Perhaps surprisingly, people with secondary-level education are significantly more vaccine hesitant than people with third-level education and slightly more hesitant than people with primary-level education.
Vaccine hesitancy has a U-shaped relationship with self-assessed physical health: hesitancy is highest among people in (very) bad health, and second-highest among people in very good health. People with fair or good health report lowest hesitancy. This likely reflects that people in bad physical health are concerned about the health risks associated with vaccination (side effects), and people in good physical health perceive the risks associated with vaccination to outweigh the risks associated with COVID-19 infection. These hypotheses are tested and affirmed in analyses below of the various reasons that people report for their vaccine hesitancy. COVID-19 related variables (knowing a close person who was tested positive for COVID-19 or died from COVID-19) are associated with lower vaccine hesitancy.
3.3. Regression analysis of vaccine hesitancy
Table 6 presents marginal effects from an initial logistic regression model where only the country indicator variables are included, allowing for an evaluation of statistical significance of the country differences in vaccine hesitancy. In subsequent models, country indicators are included in the models but for brevity, their associated marginal effect estimates are not reported.
Table 6.
Logistic model, marginal effects.
| m.e. | s.e. | |
|---|---|---|
| Austria | 0.00 | (.) |
| Belgium | −0.03 | (0.03) |
| Bulgaria | 0.38*** | (0.03) |
| Croatia | 0.19*** | (0.03) |
| Cyprus | 0.02 | (0.04) |
| Czechia | 0.08** | (0.03) |
| Denmark | −0.16*** | (0.03) |
| Estonia | 0.04 | (0.03) |
| Finland | −0.10*** | (0.03) |
| France | 0.07* | (0.04) |
| Germany | 0.00 | (0.03) |
| Greece | 0.01 | (0.03) |
| Hungary | 0.05* | (0.03) |
| Ireland | −0.14*** | (0.03) |
| Italy | −0.08*** | (0.03) |
| Latvia | 0.24*** | (0.04) |
| Lithuania | 0.09*** | (0.03) |
| Luxembourg | −0.05 | (0.04) |
| Malta | −0.15*** | (0.03) |
| Netherlands | 0.02 | (0.04) |
| Poland | 0.11*** | (0.04) |
| Portugal | −0.12*** | (0.03) |
| Romania | 0.01 | (0.03) |
| Slovakia | 0.05 | (0.04) |
| Slovenia | 0.17*** | (0.04) |
| Spain | −0.15*** | (0.03) |
| Sweden | −0.12*** | (0.03) |
| Observations | 29,755 | |
| Pseudo R-squared | 0.057 |
Notes. Standard errors in parentheses. * p < 0.10, ** p < 0.05, *** p < 0.01. Dependent variable: 1 if vaccination is rather unlikely or very unlikely ; 0 otherwise. Weighted data.
Moving beyond bivariate relationships, Table 7 presents the marginal effects from the main multivariate models. Model 1 includes socio-demographic variables only, while in Model 2 also health variables are included. Model 3 adds variables indicating exposure to COVID-19 among close persons. Social media use indicators are added in Models 4 (intensity of social media use) and 5 (using social media as the main source of news).
Table 7.
Logistic model, marginal effects.
| (1) |
(2) |
(3) |
(4) |
(5) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| m.e. | s.e. | m.e. | s.e. | m.e. | s.e. | m.e. | s.e. | m.e. | s.e. | |
| Female | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Male | 0.02* | (0.01) | 0.02* | (0.01) | 0.02* | (0.01) | 0.02* | (0.01) | 0.01 | (0.01) |
| 18–29 years | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| 30–39 years | 0.04 | (0.03) | 0.04 | (0.03) | 0.03 | (0.03) | 0.04 | (0.03) | 0.04 | (0.03) |
| 40–49 years | 0.02 | (0.03) | 0.02 | (0.03) | 0.01 | (0.03) | 0.02 | (0.03) | 0.03 | (0.03) |
| 50–59 years | 0.02 | (0.03) | 0.02 | (0.03) | 0.02 | (0.03) | 0.03 | (0.03) | 0.04 | (0.03) |
| 60–69 years | −0.02 | (0.03) | −0.02 | (0.03) | −0.02 | (0.03) | −0.01 | (0.03) | 0.00 | (0.03) |
| 70 + years | −0.05* | (0.03) | −0.05 | (0.03) | −0.05 | (0.03) | −0.04 | (0.03) | −0.02 | (0.03) |
| The open countryside | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| A village/small town | −0.06** | (0.02) | −0.06** | (0.02) | −0.06** | (0.02) | −0.06*** | (0.02) | −0.06** | (0.02) |
| A medium to large town | −0.07*** | (0.02) | −0.07*** | (0.02) | −0.07*** | (0.02) | −0.07*** | (0.02) | −0.08*** | (0.03) |
| A city or city suburb | −0.13*** | (0.02) | −0.13*** | (0.02) | −0.12*** | (0.02) | −0.13*** | (0.02) | −0.13*** | (0.02) |
| Employed | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Self-employed | 0.06** | (0.03) | 0.06** | (0.03) | 0.06** | (0.03) | 0.06** | (0.03) | 0.05** | (0.03) |
| Unemployed | 0.10*** | (0.03) | 0.10*** | (0.03) | 0.09*** | (0.03) | 0.09*** | (0.03) | 0.08*** | (0.03) |
| Ill/disabled | 0.13*** | (0.04) | 0.13*** | (0.05) | 0.13*** | (0.05) | 0.12** | (0.05) | 0.10* | (0.05) |
| Retired | 0.03 | (0.02) | 0.03 | (0.02) | 0.02 | (0.02) | 0.02 | (0.02) | 0.01 | (0.02) |
| Homemaker | 0.04 | (0.04) | 0.04 | (0.04) | 0.03 | (0.03) | 0.02 | (0.03) | 0.01 | (0.03) |
| Student | −0.10*** | (0.02) | −0.10*** | (0.02) | −0.10*** | (0.02) | −0.10*** | (0.02) | −0.11*** | (0.02) |
| No spouse | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Lives with spouse | −0.03** | (0.01) | −0.03** | (0.01) | −0.03** | (0.01) | −0.03** | (0.01) | −0.03* | (0.01) |
| No children in household | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Children in household | 0.03** | (0.02) | 0.03* | (0.02) | 0.03** | (0.02) | 0.03** | (0.02) | 0.03** | (0.02) |
| Primary education | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Secondary education | 0.02 | (0.03) | 0.03 | (0.03) | 0.03 | (0.03) | 0.03 | (0.03) | 0.04 | (0.03) |
| Tertiary education | −0.06** | (0.03) | −0.06** | (0.03) | −0.06* | (0.03) | −0.05* | (0.03) | −0.04 | (0.03) |
| (Very) bad health | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | ||
| Fair health | −0.07** | (0.03) | −0.07** | (0.03) | −0.06** | (0.03) | −0.06** | (0.03) | ||
| Good health | −0.10*** | (0.03) | −0.09*** | (0.03) | −0.09*** | (0.03) | −0.08*** | (0.03) | ||
| Very good health | −0.05 | (0.03) | −0.05 | (0.03) | −0.05 | (0.03) | −0.04 | (0.03) | ||
| Chronic health problem / disability | −0.05*** | (0.01) | −0.05*** | (0.01) | −0.05*** | (0.01) | −0.05*** | (0.01) | ||
| Close person had Covid | −0.03** | (0.01) | −0.03** | (0.01) | −0.03** | (0.01) | ||||
| Close person died of Covid | −0.04 | (0.02) | −0.04* | (0.02) | −0.04* | (0.02) | ||||
| Social media: Less than daily | 0.00 | (.) | 0.00 | (.) | ||||||
| Social media: Daily: under 3 h | 0.05*** | (0.02) | 0.04* | (0.02) | ||||||
| Social media: Daily: 3 + hours | 0.10*** | (0.02) | 0.05** | (0.02) | ||||||
| Main news source: Traditional (press/radio/TV) | 0.00 | (.) | ||||||||
| Main news source: Social media/blogs | 0.20*** | (0.02) | ||||||||
| Country dummies | Yes | Yes | Yes | Yes | Yes | |||||
| Observations | 29,755 | 29,755 | 29,755 | 29,755 | 29,755 | |||||
| Pseudo R-squared | 0.055 | 0.061 | 0.064 | 0.069 | 0.102 | |||||
Notes. Standard errors in parentheses. * p < 0.10, ** p < 0.05, *** p < 0.01. Dependent variable: 1 if vaccination is rather unlikely or very unlikely ; 0 otherwise. Weighted data.
Focusing firstly on the main predictors of interest in Model 5, the marginal effects can be interpreted in the following way: while holding the other covariates constant (at their mean level), the likelihood of being vaccine hesitant is 5 percentage points higher among people who use social media for 3 or more hours daily, in comparison with the reference group (people who use social media less than daily). This difference is statistically significant at the 5% level of significance. There appears to be a dose–response relationship in terms of the intensity of social media use: the likelihood of being vaccine hesitant is 4 percentage points higher among people who use social media daily (but for<3 h) than the reference group, and this difference is only marginally statistically significant (p < 0.10). Vaccine hesitancy is strongly related to using social media as a source of news: the likelihood of vaccine hesitancy is 20 percentage points higher among people who report social media as their main source of news, in comparison with the reference group who use traditional news sources (press, radio or TV), while controlling for all covariates. This difference is statistically significant at the 1% level of significance.
In a robustness analysis, a linear probability model (LPM) estimate (including the same covariates as in Model 5 of Table 7) of the coefficient related to time spent on social media, as well as using social media as a main news source, are practically identical in magnitude and statistical significance to those obtained from the logistic regression – see Model 1 in Appendix Table A2. The coefficients related to other covariates are also closely aligned with those of the logistic model.
Interaction effects allow for an investigation of the heterogeneity in the relationships between social media use and vaccine hesitancy across population groups. From the estimation of models where associations are allowed to differ by gender, it is evident that both are stronger among men than among women – in fact, the effect of time spent on social media becomes insignificant even at the 10% level among women (see Model 1 in Appendix Table A3). When it comes to differences by education level, the difference in vaccine hesitancy varies significantly by time spent using social media only among people with tertiary education (see Model 2 in Appendix Table A3 – similarly to the findings of Chang (2018), who found that highly educated mothers in the US were more likely to reduce their children’s vaccinations as a result of the controversy linking the measles-mumps-rubella (MMR) vaccine with autism [14]. The suggested mechanism is that the time taken to digest and react to health information decreases with education. When it comes to the source of news however, the strength of the relationship between social media and vaccine hesitancy is of similar magnitude across all educational groups.
Next, we discuss other covariates whose associations remain statistically significant (p < 0.10) in all of the step-wise specifications. Physical location of residence is significant and linear: people living in cities or city suburbs are 13 percentage points less likely to be vaccine-hesitant than people living in the open countryside, as also found in existing literature [28]. In comparison with employed individuals, vaccine hesitancy is higher among people who are self-employed, unemployed, or unable to work due to a long-term illness or disability. Conversely, students are 11 percentage points less likely to be vaccine-hesitant than employed individuals. In terms of previous analyses that include indicators of labour market status, Edwards et al. (2021) did not find a difference between being in or outside employment [29].
Variables that characterise family composition have small but statistically significant impacts: people who live with a spouse or partner are 3 percentage points less likely to be vaccine hesitant than people without a spouse or partner, while presence of children in the household increases vaccine hesitancy by 3 percentage points. We are not aware of other research examining the relationship between vaccine hesitancy and household composition. Existing research has usually found a negative relationship between education and vaccine hesitancy [29], [30], [31]. In our analysis, the significance of having tertiary education in reducing the likelihood of vaccine hesitancy decreases as social media use indicators are added to the model, indicating the correlation between education and social media use, and adding to our understanding of the mechanisms behind this relationship.
The U-shaped relationship with self-reported health status persists in multivariate analysis. Similar evidence is found by Soares et al. (2021), while Edwards et al. (2021) do not find any significant correlation between self-perceived health status and vaccine hesitancy, while Soares et al. (2021) also find the U-shaped association [29], [32]. Exposure to COVID-19 among close persons is found to increase the intention to get a COVID-19 vaccine, as also found by Thunstrom et al. (2020) [33]. Conversely, Edwards et al. (2021) found no significant association between exposure to COVID-19 and vaccine hesitancy [29].
In Models 1–4, we find a very small difference in vaccine hesitancy between men and women, and this difference becomes statistically insignificant once both social media use indicators are included in the model. In recent literature, the relationship between gender and hesitancy is unclear. While some studies have found women to have higher vaccine hesitancy than men [12], [34], [35], some have found the opposite [36], [37], while other studies found the difference between men and women as non-significant [38].
3.4. Reasons for vaccine hesitancy
To establish a deeper understanding of the drivers of COVID-19 vaccine hesitancy, we fit separate multivariate logistic models of the likelihood of reporting specific reasons for vaccine hesitancy. We examine the differences across the models in order to characterise the groups driven by different reasons for hesitancy. Table 8 presents the estimates from these models.4 As expected, because vaccine safety is the most commonly reported reason for vaccine hesitancy, the marginal effects presented for Model 2 coincide relatively closely with those of Model 5 in Table 7 (of overall vaccine hesitancy), with the exception of vaccine safety concerns being heightened among individuals with secondary-level education. Of the three categories of vaccine hesitancy reasons, vaccine safety concerns are the most related to the intensity of social media use.
Table 8.
Logistic model, marginal effects.
| (1) |
(2) |
(3) |
||||
|---|---|---|---|---|---|---|
| Health worry |
Vaccine safety |
Exaggeration |
||||
| Female | m.e. | s.e. | m.e. | s.e. | m.e. | s.e. |
| Female | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Male | 0.00 | (0.01) | 0.01 | (0.01) | 0.04*** | (0.01) |
| 18–29 years | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| 30–39 years | −0.01 | (0.02) | 0.02 | (0.02) | 0.00 | (0.02) |
| 40–49 years | −0.02 | (0.02) | 0.01 | (0.02) | 0.00 | (0.02) |
| 50–59 years | −0.02 | (0.02) | −0.00 | (0.02) | −0.02 | (0.02) |
| 60–69 years | −0.02 | (0.02) | −0.02 | (0.02) | −0.03 | (0.02) |
| 70 + years | −0.03* | (0.02) | −0.00 | (0.03) | −0.05** | (0.02) |
| The open countryside | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| A village/small town | 0.00 | (0.01) | −0.05** | (0.02) | −0.01 | (0.01) |
| A medium to large town | −0.01 | (0.01) | −0.06*** | (0.02) | −0.03* | (0.01) |
| A city or city suburb | −0.02 | (0.01) | −0.09*** | (0.02) | −0.05*** | (0.01) |
| Employed | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Self-employed | 0.01 | (0.02) | 0.01 | (0.02) | 0.03* | (0.02) |
| Unemployed | 0.01 | (0.01) | 0.07*** | (0.02) | 0.03** | (0.02) |
| Ill/disabled | 0.01 | (0.02) | 0.04 | (0.03) | 0.03 | (0.04) |
| Retired | −0.01 | (0.01) | −0.00 | (0.02) | 0.03 | (0.02) |
| Homemaker | −0.00 | (0.01) | −0.00 | (0.03) | −0.01 | (0.02) |
| Student | −0.03*** | (0.01) | −0.07*** | (0.01) | −0.04*** | (0.01) |
| No spouse | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Lives with spouse | −0.00 | (0.01) | −0.00 | (0.01) | −0.01 | (0.01) |
| No children in household | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Children in household | −0.00 | (0.01) | 0.03** | (0.01) | 0.01 | (0.01) |
| Primary education | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Secondary education | 0.00 | (0.01) | 0.05*** | (0.02) | 0.02 | (0.01) |
| Tertiary education | −0.02 | (0.01) | 0.01 | (0.02) | −0.01 | (0.01) |
| (Very) bad health | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Fair health | −0.04** | (0.02) | −0.04* | (0.02) | 0.02 | (0.01) |
| Good health | −0.06*** | (0.02) | −0.04* | (0.02) | 0.01 | (0.01) |
| Very good health | −0.06*** | (0.02) | −0.02 | (0.03) | 0.05*** | (0.02) |
| Chronic health problem / disability | 0.02*** | (0.01) | −0.01 | (0.01) | −0.03*** | (0.01) |
| Close person had Covid | −0.01 | (0.01) | −0.02* | (0.01) | −0.01 | (0.01) |
| Close person died of Covid | −0.02 | (0.01) | −0.05*** | (0.02) | −0.03* | (0.02) |
| Social media: Less than daily | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Social media: Daily: under 3 h | 0.01 | (0.01) | 0.05*** | (0.01) | 0.01 | (0.01) |
| Social media: Daily: 3 + hours | 0.03** | (0.01) | 0.06*** | (0.02) | 0.01 | (0.01) |
| Main news source: Traditional (press/radio/TV) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Main news source: Social media/blogs | 0.04*** | (0.01) | 0.10*** | (0.01) | 0.12*** | (0.01) |
| Country dummies | Yes | Yes | Yes | |||
| Observations | 29,755 | 29,755 | 29,755 | |||
| Pseudo R-squared | 0.090 | 0.082 | 0.138 | |||
Notes. Standard errors in parentheses. * p < 0.10, ** p < 0.05, *** p < 0.01.
Dependent variable:
Model 1: 1 if vaccine hesitant with reason “I am worried that it will make my health issues worse”; 0 otherwise.
Model 2: 1 if vaccine hesitant with reason “I do not trust the safety of the vaccine”; 0 otherwise.
Model 3: 1 if vaccine hesitant with reason “I think the risk of COVID-19 is exaggerated” or “I think COVID-19 doesn’t exist”; 0 otherwise.
Weighted data.
The nuances emerge when examining the estimates of Model 1: hesitancy due to a health worry is strongly (and in this case, linearly) related to health: individuals in better health are least likely to report being concerned about COVID-19 vaccines making their health issues worse. Of the modelled categories of vaccine hesitancy reasons, health concerns are the least related to the use of social media as a source of news.
The drivers for reporting exaggeration of COVID-19 risk as the reason for vaccine hesitancy are, in parts, different to those of other reasons for vaccine hesitancy. People who are vaccine-hesitant because they view COVID-19 risks as exaggerated – or believe that COVID-19 doesn't exist – are more likely to be male and in very good health. For the group reporting these reasons for vaccine hesitancy, the intensity of social media use plays no significant role, but the use of social media as a source of news is a strong determinant: the likelihood of reporting reasons of COVID-19 exaggeration is 12 percentage points higher among people who report social media as their main news source. The results confirm the findings in past research regarding social media use and vaccine hesitancy.
4. Conclusion
Vaccine hesitancy is a serious threat to the effective roll-out of vaccination programmes against COVID-19. Hence, vaccine hesitancy may undermine the chances of achieving herd immunity and overcoming the pandemic. This paper examines the determinants of COVID-19 vaccine hesitancy in the European Union. We study the determinants of different kinds of vaccine hesitancy. In particular, we focus on the roles of i) the use of social media as a news source, and ii) the intensity of social media use, as drivers of vaccine hesitancy. While most previous studies analyse this relationship using data from single (or a small number of) countries, this study is unique as it provides a cross-national analysis, covering all EU countries, of the effect of social media use on vaccine hesitancy.
Our analysis shows a significant relationship between the use of social media and vaccination likelihood. In particular it documents the strong effect of using social media as the main source of information on vaccine hesitancy. The findings show that groups with higher vaccine hesitancy are more reliant on social media as a source of news. This type of information can be useful in engaging with these groups, both for providing valid information and for responding to their potential concerns – as shown, concerns about the vaccine safety in particular are the most related to the intensity of social media use. The lessons to be learnt in using various communication channels effectively are likely to have relevance not only in facilitating current vaccination programmes, but also in terms of developing general health literacy in the future.
These findings suggest that combating misinformation regarding COVID-19 vaccines on social media is critical in limiting the effect disinformation on public perceptions of vaccines and preventing the surge of vaccine hesitancy. Public outreach is the cornerstone of the COVID-19 vaccine deployment. In order to gain public trust and confidence, clear and unbiased information and transparent messages about vaccines need to be conveyed by policymakers and scientists. Given these findings, national governments and supranational organisations need to urgently implement reliable strategies in order to address the detrimental effect of misinformation that can escalate vaccine hesitancy.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We are grateful to the Editor and two anonymous referees for their helpful comments and insights. We thank Daphne Ahrendt, Eszter Sandor, Tadas Leončikas and the wider team at Eurofound for the design and implementation of the survey, the preparation of the dataset, and for their helpful comments on the draft manuscript.
Data statement
Applications to access the data used in this study can be made to Eurofound.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Eurofound is the EU agency for the improvement of living and working conditions. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the ones of Eurofound.
All authors approved this version of the manuscript.
All authors attest they meet the ICMJE criteria for authorship.
Footnotes
Data were weighted by the following weighting variables: age crossed with gender in 12 age-gender combinations: 18–24, 25–34, 35–44, 45–54, 55–64, 65+, male and female. People who answered “In another way” to the question on gender were randomly allocated to male and female groups for weighting purposes using the sample function in base R (but not for analytical purposes). Targets for age and gender were 2020 Eurostat estimates by country for population aged 18+. Urbanisation: two categories: urban and rural, based on respondent’s own assessment collected in four urbanisation categories. For weighting, respondents with missing values were randomised into the categories. Targets for urbanisation were (weighted) estimates for self-defined urbanisation from the 2016 European Quality of Life Survey by country, using the same question, by age, gender and country. Education: two categories: tertiary and non-tertiary. For weighting, respondents with missing values for these variables were randomised into the two categories. Targets for education levels were results from the 2020 Labour Force Survey by age, gender and country. Weighting was completed with the anesrake R-package by country using the wpct function [24]. The limit for discrepancy for selecting variables (pctlim) was set at 0.05 (5%). The cap (maximum weight) started at 4 and was increased for each country in the function until convergence, minimum weight was set at 0.05. Extreme weights were trimmed using the trimWeights function of the survey R-package [25]. The resulting weights were grossed up to adult population size by country, then rescaled to have a mean of 1, both using the mutate function in the dplyr R-package [26].
As robustness checks, linear probability models (LPM) were also estimated, by fitting ordinary least regression (OLS) models using the regress command in Stata. The results are discussed in the Results section.
The data have been obtained from the COVID-19 Vaccine Tracker of the European Centre for Disease Prevention and Control.
Appendix.
Table A1.
Descriptive statistics of the analysis sample.
| % | N | |
|---|---|---|
| Gender | ||
| Female | 53.2 | 18,978 |
| Male | 46.8 | 10,777 |
| Age group | ||
| 18–29 years | 14.5 | 2,429 |
| 30–39 years | 14.8 | 3,756 |
| 40–49 years | 16.4 | 5,529 |
| 50–59 years | 19.6 | 8,022 |
| 60–69 years | 21.7 | 7,245 |
| 70 + years | 13.0 | 2,774 |
| Location type | ||
| The open countryside | 11.7 | 2,329 |
| A village/small town | 40.6 | 7,939 |
| A medium to large town | 20.5 | 7,720 |
| A city or city suburb | 27.3 | 11,767 |
| Employment status | ||
| Employed | 43.1 | 14,642 |
| Self-employed | 6.2 | 2,440 |
| Unemployed | 9.4 | 2,805 |
| Ill/disabled | 2.9 | 757 |
| Retired | 28.3 | 7,127 |
| Homemaker | 3.1 | 1,012 |
| Student | 7.1 | 972 |
| Lives with spouse | ||
| No | 43.9 | 11,367 |
| Yes | 56.1 | 18,388 |
| Children in household | ||
| No | 67.2 | 19,407 |
| Yes | 32.8 | 10,348 |
| Education level | ||
| Primary education | 4.9 | 541 |
| Secondary education | 66.4 | 9,494 |
| Tertiary education | 28.6 | 19,720 |
| Self-rated health | ||
| (Very) bad health | 8.6 | 2,481 |
| Fair health | 31.7 | 9,068 |
| Good health | 46.2 | 13,469 |
| Very good health | 13.5 | 4,737 |
| Chronic health problem / disability | ||
| No | 52.2 | 16,063 |
| Yes | 47.8 | 13,692 |
| Close person had Covid | ||
| No | 62.7 | 18,437 |
| Yes | 37.3 | 11,318 |
| Close person died of Covid | ||
| No | 89.6 | 27,045 |
| Yes | 10.4 | 2,710 |
| Social media use | ||
| Less than daily | 10.3 | 2,866 |
| Daily: under 3 h | 68.6 | 20,087 |
| Daily: 3 + hours | 21.1 | 6,802 |
| Main news source | ||
| Traditional (press, radio, TV) | 81.0 | 23,573 |
| Social media/blogs | 19.0 | 6,182 |
| Total | 29,755 | |
Notes: Weighted data.
Table A2.
Estimates of Linear Probability Models (LPM).
|
(1) |
(2) |
(3) |
(4) |
|||||
|---|---|---|---|---|---|---|---|---|
| Coeff. | s.e. | Coeff. | s.e. | Coeff. | s.e. | Coeff. | s.e. | |
| Female | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Male | 0.02 | (0.01) | 0.01 | (0.01) | 0.01 | (0.01) | 0.05*** | (0.01) |
| 18–29 years | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| 30–39 years | 0.04 | (0.03) | −0.01 | (0.02) | 0.02 | (0.03) | 0.00 | (0.03) |
| 40–49 years | 0.03 | (0.03) | −0.02 | (0.02) | 0.01 | (0.03) | 0.00 | (0.02) |
| 50–59 years | 0.04 | (0.03) | −0.03 | (0.02) | −0.00 | (0.02) | −0.02 | (0.02) |
| 60–69 years | 0.00 | (0.03) | −0.03 | (0.02) | −0.02 | (0.03) | −0.03 | (0.03) |
| 70 + years | −0.02 | (0.04) | −0.04* | (0.02) | −0.01 | (0.03) | −0.07** | (0.03) |
| The open countryside | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| A village/small town | −0.06*** | (0.02) | 0.00 | (0.02) | −0.06** | (0.02) | −0.02 | (0.02) |
| A medium to large town | −0.08*** | (0.02) | −0.01 | (0.02) | −0.06*** | (0.02) | −0.03* | (0.02) |
| A city or city suburb | −0.13*** | (0.02) | −0.02 | (0.02) | −0.10*** | (0.02) | −0.06*** | (0.02) |
| Employed | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Self-employed | 0.06** | (0.02) | 0.01 | (0.02) | 0.01 | (0.02) | 0.05** | (0.02) |
| Unemployed | 0.08*** | (0.03) | 0.01 | (0.02) | 0.08*** | (0.03) | 0.05** | (0.02) |
| Ill/disabled | 0.11** | (0.05) | 0.05 | (0.04) | 0.06 | (0.04) | 0.03 | (0.04) |
| Retired | 0.01 | (0.02) | −0.01 | (0.01) | −0.00 | (0.02) | 0.02 | (0.02) |
| Homemaker | 0.01 | (0.03) | −0.00 | (0.02) | −0.00 | (0.03) | −0.01 | (0.03) |
| Student | −0.13*** | (0.03) | −0.05** | (0.02) | −0.09*** | (0.02) | −0.09*** | (0.02) |
| No spouse | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Lives with spouse | −0.02* | (0.01) | −0.00 | (0.01) | −0.00 | (0.01) | −0.01 | (0.01) |
| No children in household | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Children in household | 0.03* | (0.02) | −0.00 | (0.01) | 0.03** | (0.01) | 0.01 | (0.01) |
| Primary education | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Secondary education | 0.04 | (0.03) | 0.00 | (0.02) | 0.06*** | (0.02) | 0.02 | (0.02) |
| Tertiary education | −0.03 | (0.03) | −0.02 | (0.01) | 0.02 | (0.02) | −0.02 | (0.02) |
| (Very) bad health | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Fair health | −0.06** | (0.03) | −0.05** | (0.02) | −0.05** | (0.02) | 0.02 | (0.02) |
| Good health | −0.08*** | (0.03) | −0.08*** | (0.02) | −0.05** | (0.03) | 0.02 | (0.02) |
| Very good health | −0.04 | (0.03) | −0.08*** | (0.02) | −0.03 | (0.03) | 0.06*** | (0.02) |
| Chronic health problem / disability | −0.04*** | (0.01) | 0.02*** | (0.01) | −0.01 | (0.01) | −0.04*** | (0.01) |
| Close person had Covid | −0.03** | (0.01) | −0.01 | (0.01) | −0.02* | (0.01) | −0.01 | (0.01) |
| Close person died of Covid | −0.04* | (0.02) | −0.02* | (0.01) | −0.05*** | (0.01) | −0.03** | (0.01) |
| Social media: Less than daily | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Social media: Daily: under 3 h | 0.03* | (0.02) | 0.01 | (0.01) | 0.05*** | (0.01) | 0.01 | (0.01) |
| Social media: Daily: 3 + hours | 0.05** | (0.02) | 0.03** | (0.01) | 0.06*** | (0.02) | 0.01 | (0.02) |
| Main news source: Traditional (press/radio/TV) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) | 0.00 | (.) |
| Main news source: Social media/blogs | 0.20*** | (0.02) | 0.05*** | (0.01) | 0.11*** | (0.02) | 0.14*** | (0.01) |
| Constant | 0.36*** | (0.06) | 0.14*** | (0.03) | 0.19*** | (0.04) | 0.11*** | (0.04) |
| Country dummies | Yes | Yes | Yes | Yes | ||||
| Observations | 29,755 | 29,755 | 29,755 | 29,755 | ||||
| R-squared | 0.105 | 0.044 | 0.063 | 0.089 | ||||
Notes. Standard errors in parentheses. * p < 0.10, ** p < 0.05, *** p < 0.01.
Dependent variable:
Model 1: 1 if vaccination is rather unlikely or very unlikely ; 0 otherwise.
Model 2: 1 if vaccine hesitant with reason “I am worried that it will make my health issues worse”; 0 otherwise.
Model 3: 1 if vaccine hesitant with reason “I do not trust the safety of the vaccine”; 0 otherwise.
Model 4: 1 if vaccine hesitant with reason “I think the risk of COVID-19 is exaggerated” or “I think COVID-19 doesn’t exist”; 0 otherwise.
Weighted data.
Table A3.
Marginal effects from logistic models with the inclusion of interaction terms (extensions of Model 5 in Table 7).
| (1) | (2) | |||||
|---|---|---|---|---|---|---|
| m.e. | s.e. | m.e. | s.e. | |||
| Social media: Less than daily | (ref.) | Social media: Less than daily | (ref.) | |||
| Social media: Daily: under 3 h | Social media: Daily: under 3 h | |||||
| Female | 0.03 | (0.03) | Primary education | −0.14 | (0.13) | |
| Male | 0.04 | (0.03) | Secondary education | 0.04 | (0.03) | |
| Social media: Daily: 3 + hours | Tertiary education | 0.06*** | (0.01) | |||
| Female | 0.04 | (0.03) | Social media: Daily: 3 + hours | |||
| Male | 0.06* | (0.04) | Primary education | 0.02 | (0.14) | |
| Secondary education | 0.04 | (0.03) | ||||
| Main news source: Traditional (press, radio, TV) | (ref.) | Tertiary education | 0.07*** | (0.02) | ||
| Main news source: Social media/blogs | ||||||
| Female | 0.19*** | (0.02) | Main news source: Traditional (press, radio, TV) | (ref.) | ||
| Male | 0.21*** | (0.03) | Main news source: Social media/blogs | |||
| Primary education | 0.20*** | (0.06) | ||||
| Observations | 29,755 | Secondary education | 0.21*** | (0.02) | ||
| Tertiary education | 0.18*** | (0.02) | ||||
| Observations | 29,755 | |||||
Notes: Standard errors in parentheses. * p < 0.10, ** p < 0.05, *** p < 0.01. Weighted data. The models include all the covariates included in Model 5 in Table 7, in addition to the reported interactions.
References
- 1.World Health Organisation, Report of the SAGE working group on vaccine hesitancy (2014).
- 2.Stern A.M., Markel H. The history of vaccines and immunization: familiar patterns, new challenges. Health Aff. 2005;24(3):611–621. doi: 10.1377/hlthaff.24.3.611. [DOI] [PubMed] [Google Scholar]
- 3.Petrelli F., Contratti C., Tanzi E., Grappasonni I. Vaccine hesitancy, a public health problem. Ann Ig. 2018;30(2):86–103. doi: 10.7416/ai.2018.2200. [DOI] [PubMed] [Google Scholar]
- 4.Wiysonge C.S., Ndwandwe D., Ryan J., Jaca A., Batouré O., Anya B.-P.-M., et al. Vaccine hesitancy in the era of COVID-19: could lessons from the past help in divining the future? Human Vaccines & Immunotherapeutics. 2021:1–3. doi: 10.1080/21645515.2021.1893062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dubé E., Gagnon D., Ouakki M., Bettinger J.A., Guay M., Halperin S., et al. Understanding vaccine hesitancy in Canada: results of a consultation study by the Canadian Immunization Research Network. PLoS ONE. 2016;11(6) doi: 10.1371/journal.pone.0156118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lantos J.D., Jackson M.A., Opel D.J., Marcuse E.K., Myers A.L., Connelly B.L. Controversies in vaccine mandates. Current Problems in Pediatric and Adolescent Health Care. 2010;40(3):38–58. doi: 10.1016/j.cppeds.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Benin A.L., Wisler-Scher D.J., Colson E., Shapiro E.D., Holmboe E.S. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117(5):1532–1541. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- 8.Murphy J., Vallières F., Bentall R.P., Shevlin M., McBride O., Hartman T.K., et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12(1) doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Puri N., Coomes E.A., Haghbayan H., Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Human Vaccines & Immunotherapeutics. 2020:1–8. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Romer D., Jamieson K.H. Conspiracy theories as barriers to controlling the spread of COVID19 in the US. Soc Sci Med. 2020;263 doi: 10.1016/j.socscimed.2020.113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.S. L. Wilson, C. Wiysonge, Social media and vaccine hesitancy, BMJ Global Health 5 (10) (2020) e004206. 305 [DOI] [PMC free article] [PubMed]
- 12.Earnshaw V.A., Eaton L.A., Kalichman S.C., Brousseau N.M., Hill E.C., Fox A.B. COVID-19 conspiracy beliefs, health behaviors, and policy support. Translational Behavioral Medicine. 2020;10(4):850–856. doi: 10.1093/tbm/ibaa090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carrieri V., Madio L., Principe F. Vaccine hesitancy and (fake) news: Quasi-experimental evidence from Italy. Health Econ. 2019;28(11):1377–1382. doi: 10.1002/hec.3937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang L.V. Information, education, and health behaviors: Evidence from the MMR vaccine autism controversy. Health Econ. 2018;27(7):1043–1062. doi: 10.1002/hec.3645. [DOI] [PubMed] [Google Scholar]
- 15.Betsch C., Renkewitz F., Betsch T., Ulshöfer C. The influence of vaccine-critical websites on perceiving vaccination risks. Journal of Health Psychology. 2010;15(3):446–455. doi: 10.1177/1359105309353647. [DOI] [PubMed] [Google Scholar]
- 16.Ahmed N., Quinn S.C., Hancock G.R., Freimuth V.S., Jamison A. Social media use and influenza vaccine uptake among white and African American adults. Vaccine. 2018;36(49):7556–7561. doi: 10.1016/j.vaccine.2018.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dubé E., Laberge C., Guay M., Bramadat P., Roy R., Bettinger J.A. Vaccine hesitancy: an overview. Human Vaccines & Immunotherapeutics. 2013;9(8):1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dubé E., Gagnon D., MacDonald N., Bocquier A., Peretti-Watel P., Verger P. Underlying factors impacting vaccine hesitancy in high income countries: a review of qualitative studies. Expert Review of Vaccines. 2018;17(11):989–1004. doi: 10.1080/14760584.2018.1541406. [DOI] [PubMed] [Google Scholar]
- 19.MacDonald N.E., et al. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 20.Larson H.J., De Figueiredo A., Xiahong Z., Schulz W.S., Verger P., Johnston I.G., et al. global insights through a 67-country survey. EBioMedicine. 2016;12(2016):295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessels R., Luyten J., Tubeuf S. Willingness to get vaccinated against Covid-19 and attitudes towards vaccination in general. Vaccine. 2021;39(33):4716–4722. doi: 10.1016/j.vaccine.2021.05.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eurofound . Publications Office of the European Union; Luxembourg: 2017. European Quality of Life Survey 2016: Quality of life, quality of public services, and quality of society: Overview report. [Google Scholar]
- 23.Eurofound . Publications Office of the European Union; Luxembourg: 2017. Sixth European Working Conditions Survey—overview report (2017 update) [Google Scholar]
- 24.Pasek J., Pasek M.J. Package ‘anesrake’, The Comprehensive R Archive. Network. 2018 [Google Scholar]
- 25.T. Lumley, Package ‘survey’, Available at the following link: https://cran.r-project.org/ (2020)
- 26.Wickham H., Averick M., Bryan J., Chang W., McGowan L., François R., et al. Welcome to the tidyverse. Journal of Open Source Software. 2019;4(43):1686. doi: 10.21105/joss10.21105/joss.01686. [DOI] [Google Scholar]
- 27.Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. The Lancet Public Health. 2021;6(4):e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of US adults. Ann Intern Med. 2020;173(12):964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Edwards B., Biddle N., Gray M., Sollis K., Di Gennaro F. COVID-19 vaccine hesitancy and resistance: Correlates in a nationally representative longitudinal survey of the Australian population. PLoS ONE. 2021;16(3) doi: 10.1371/journal.pone.0248892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hawkins R.B., Charles E.J., Mehaffey J.H. Socio-economic status and COVID-19-related cases and fatalities. Public Health. 2020;189:129–134. doi: 10.1016/j.puhe.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bibbins-Domingo K. This Time Must Be Different: Disparities During the COVID-19 Pandemic. Ann Intern Med. 2020;173(3):233–234. doi: 10.7326/M20-2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Soares P., Rocha J.V., Moniz M., Gama A., Laires P.A., Pedro A.R., et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines. 2021;9(3):300. doi: 10.3390/vaccines9030300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thunstrom L., Ashworth M., Finnoff D., Newbold S. Hesitancy towards a COVID-19 vaccine and prospects for herd immunity. Available at SSRN. 2020;3593098 doi: 10.1007/s10393-021-01524-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ward J.K., Alleaume C., Peretti-Watel P., Seror V., Cortaredona S., Launay O., et al. The French public’s attitudes to a future COVID-19 vaccine: The politicization of a public health issue. Soc Sci Med. 2020;265 doi: 10.1016/j.socscimed.2020.113414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel J., et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21(7):977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Detoc M., Bruel S., Frappe P., Tardy B., Botelho-Nevers E., Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38(45):7002–7006. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Graffigna G., Palamenghi L., Boccia S., Barello S. Relationship between citizens’ health engagement and intention to take the COVID-19 vaccine in Italy: A mediation analysis. Vaccines. 2020;8(4):576. doi: 10.3390/vaccines8040576. [DOI] [PMC free article] [PubMed] [Google Scholar]