Abstract
In the past three decades since the inception of human organ transplantation, cytomegalovirus (CMV) has gained increasing clinical import because it is a common pathogen in the immunocompromised transplant recipient. Patients may suffer from severe manifestations of this infection along with the threat of potential fatality. Additionally, the dynamic evolution of immunosuppressive and antiviral agents has brought forth changes in the natural history of CMV infection and disease. Transplant physicians now face the daunting task of recognizing and managing the changing spectrum of CMV infection and its consequences in the organ recipient. For the microbiology laboratory, the emphasis has been geared toward the development of more sophisticated detection assays, including methods to detect emerging antiviral resistance. The discovery of novel antiviral chemotherapy is an important theme of clinical research. Investigations have also focused on preventative measures for CMV disease in the solid-organ transplant population. In all, while much has been achieved in the overall management of CMV infection, the current understanding of CMV pathogenesis and therapy still leaves much to be learned before success can be claimed.
Despite advances in surgical techniques and immunosuppressive therapy to prevent allograft rejection, cytomegalovirus (CMV) remains a major health threat after solid-organ transplantation. Indeed, the clinical importance of this virus has grown in parallel with the increasing number of solid-organ transplant recipients. In transplant recipients, the clinical symptoms related to CMV disease and the prevention of CMV infection show variation among different patient populations, depending on the type of transplant and the intensity of immunosuppression. The prevalence of life-threatening CMV complications has, fortunately, been reduced by pharmacologic intervention, resulting in improved patient survival. Treatment and prevention of CMV infection have assumed increasing importance in the care of transplant recipients relative to the availability of effective antiviral agents as well as new diagnostic techniques. This article reviews the epidemiology of CMV infection in solid-organ transplant recipients and describes the varied clinical manifestations of CMV disease. Techniques for CMV detection currently in use are outlined. Pharmacologic interventions, both for the treatment and the prevention of CMV disease in solid-organ transplant recipients, are reviewed.
EPIDEMIOLOGY
Infection caused by CMV is common, affecting most of the population, but associated disease is an exceptional event in normal individuals. However, among immunosuppressed patients, such as recipients of organ allografts, CMV provokes a number of disparate outcomes.
CMV shares with other herpesviruses the ability to remain latent in tissues after it has occasioned acute infection. Unlike other herpesviruses such as herpes simplex virus and varicella-zoster virus, which remain latent in highly restricted areas of the body, latent CMV can be found in multiple body sites, although it causes disease in only some of these and then only in certain patient groups (181). CMV infects humans of all ages, although the peak period of viral acquisition in the general population occurs early in life (57, 202). In the population at large, primary infection occurs by direct close personal contact via exposure to bodily fluids such as saliva, tears, urine, stool, semen, and breast milk. Infants may acquire CMV transplacentally as a result of maternal viremia or perinatally via breast milk. In later childhood, close physical contact facilitates transmission. Notably, infection in children is usually asymptomatic. Young children in day care centers transmit the virus to other children as well as to susceptible adults, including transplant recipients (3, 4, 188, 331, 442). In large day care centers, approximately half of all children experience active CMV infections and 10% to 15% of uninfected children become infected each year (138, 210, 310). The highest prevalence rates of active viral transmission and excretion are found in children 13 to 24 months of age (97). Depending on the population surveyed, the prevalence of CMV antibody seropositivity in various regions ranges from 40 to 100% (25, 202, 283, 389, 468). In populations from high socioeconomic environments, up to 62% of adolescents are CMV seropositive (178, 283). It is estimated that the annual incidence of CMV infection for female day care workers of childbearing age may be as high as 20% (3, 4, 331). CMV can be heterosexually and homosexually transmitted; seroprevalence is high among patients examined at sexually transmitted disease clinics (60, 69, 100, 191, 216, 303, 435, 439, 495).
Approximately 50% of transplant patients excrete CMV in body secretions (e.g., saliva and urine) at some stage after organ transplantation (9, 177, 388); this usually begins in the first month following transplant surgery. Viral shedding reaches peak levels during the second and third months following transplantation, at which time it may be associated with disease (177, 248). The incidence of symptoms related to CMV infection varies among different types of allograft recipients (Table 1). In general, liver, pancreas, lung, intestinal, and heart transplant recipients have a greater incidence of CMV disease than do kidney transplant recipients. Symptomatic infections occur in approximately 39 to 41% of heart-lung, 9 to 35% of heart, 22 to 29% of liver and pancreas, and 8 to 32% of renal transplant recipients not receiving antiviral prophylaxis (179, 201, 334). Recipients of living-related kidney allografts experience less morbidity associated with CMV infection than do those receiving cadaveric renal allografts (450).
TABLE 1.
CMV disease in solid-organ transplant recipients
| Organ transplanted | Frequency of CMV disease (%)a | Organ predisposed to infection |
|---|---|---|
| Kidney | 8–32 | |
| Liver | 22–29 | Liver |
| Heart | 9–35 | |
| Kidney-pancreas | 50 | Pancreas |
| Small bowel | 22 | Intestine |
| Heart-lung | 39–41 | Lung |
In the transplant population, three patterns of CMV infection are observed, each with a different propensity for causing clinical disease. Primary infection develops in a CMV-seronegative individual who receives blood products and/or an organ from a CMV-seropositive donor. Most primary CMV infections in organ transplant recipients are due to transplantation of an organ carrying latent virus from a seropositive donor. Secondary or reactivation infection occurs when latent CMV reactivates posttransplantation in a CMV-seropositive recipient. CMV superinfection or reinfection occurs in a CMV-seropositive host who receives cells and/or an organ from a seropositive donor, with reactivation of latent virus present in the allograft or reinfection by a new strain of CMV. It is not possible to distinguish superinfection from reactivation infection unless sophisticated genetic studies are used (63, 64, 67). Nonetheless, there is some indication that reinfection is more frequent than reactivation of endogenous CMV (67). The frequency of primary infection depends on the number of susceptible or CMV-seronegative organ recipients and the availability of a source of transmission. Symptomatic disease occurs most frequently in patients experiencing primary infection, where it occurs in 40 to 60% of patients (26, 101, 198, 299, 420, 433).
PATHOGENESIS
Following primary CMV infection in the normal host, the virus remains in a latent state (or persists as a low-grade chronic infection), a feature it shares with other herpesviruses. CMV genomic material has been found in monocytes/macrophages (405, 434), neutrophils (158, 405), lymphocytes (412), and endothelial cells (173); however, the exact site(s) of latency remains to be elucidated. Three virus-associated factors have been found to be important in the pathogenesis of CMV disease: the cell-bound nature of CMV, its tendency to disseminate throughout the body via the bloodstream, and its monocytotropic character. The presence of latent virus in monocytes forms a circulating reservoir that may sustain full viral replication when differentiation into macrophages occurs (462).
Whatever the site(s) of latency, reactivation of latent virus is the critical step in the pathogenesis of CMV infection following solid-organ transplantation. The replication of CMV occurs in a temporally regulated fashion, with the immediate-early (IE) genes regulating the subsequent transcription and translation of the early and late gene products (251). A number of factors can affect the interaction between the host immune system and the virus, most important of which is a shift in favor of the virus when the host immune system is compromised, such that infection can be associated with disease. There is no evidence that the varied clinical manifestations are due to strains of CMV with different virulence or tissue tropism; the major determinant of disease appears to be in host factors.
Following primary CMV infection in the normal host, long-term immunity develops, controlling viral persistence—a situation that is lacking following solid-organ transplantation. While humoral immunity provides the best evidence of prior infection and the ability to transmit the virus, cytotoxic T lymphocytes are the key host defense against CMV (47, 135). Failure to reconstitute CMV-specific cellular immunity after transplantation leads to progressive CMV disease (45, 365, 374, 506). The spectrum and severity of clinical CMV disease are dependent on the type of organ transplant, the pretransplant serologic status of the donor and recipient, the immunosuppressive regimen used, and the intensity of graft rejection.
The single most important risk factor for the development of CMV disease in any solid-organ transplant is primary CMV exposure (35, 63, 64, 137, 166, 183, 351, 420, 427). Secondary infections occurring in CMV-seropositive hosts often remain asymptomatic because immunologic memory can be rapidly mobilized, limiting the extent of viral replication. In contrast, primary infections occurring in seronegative individuals who have no preexisting immunity may be associated with severe morbidity (and even mortality), because extensive viral replication may occur before antiviral immune responses are mounted (462). Modification of immunity by the use of antilymphocyte antibodies or other agents that influence cell-mediated immunity, increases the risk of CMV disease (260, 393). There is some suggestion that allograft recipients with human leukocyte antigen (HLA)-B7-positive donors are at an increased risk for developing active CMV infection and disease (45).
CMV is an active inducer of some members of the herpesvirus family (1). Rises in Epstein-Barr virus (EBV) antibody titers are seen in transplant recipients with symptomatic CMV infection (12, 206). Evidence of human herpesvirus 6 (HHV-6) seroconversion following liver transplantation may be a marker for CMV disease (98), and HHV-6 may infect the liver allograft in association with CMV infection (257). HHV-6 infection itself is not usually associated with severe clinical manifestations in liver transplant recipients unless accompanied by concomitant CMV infection (194). After renal transplantation, HHV-6 reactivation and the simultaneous detection of both HHV-6 and CMV DNA in either urine or serum is a strong predictor of CMV disease (93, 369).
The critical exogenous factor influencing CMV reactivation following transplantation is the type and intensity of immunosuppressive therapy (389). The level of immunosuppression in any given patient is determined by the dose, duration, and temporal sequence in which immunosuppressive medications are administered, which in turn influences the course of CMV infection posttransplantation. Most antirejection agents used in solid-organ transplantation depress cell-mediated immunity; however, blunted antibody responses and leukopenia may also result from the use of these agents. Azathioprine inhibits cell proliferation and may result in leukopenia. Cyclosporine has minimal effect on reactivation of latent virus but interferes significantly with the ability of the host to control such infection (389). High cyclosporine levels in blood have been associated with an increased risk of developing CMV disease (34). It has been proposed that immunosuppression with tacrolimus (FK506) may be associated with a lower incidence of CMV disease than cyclosporine (422), but this remains to be proved. Steroids by themselves appear to have a minimal effect on reactivation of latent CMV. However, the addition of high doses of corticosteroid to antilymphocyte therapy has been associated with a higher incidence and increased severity of CMV disease (260). Mycophenolate mofetil (MMF) selectively suppresses the proliferation of T and B lymphocytes. While its use has dramatically reduced the incidence of rejection in renal transplant patients, a slight increase in CMV invasive disease has been noted in MMF-treated patients (especially those given high doses) compared to those receiving conventional azathioprine-containing immunosuppressive regimens (164, 204, 287, 306, 481); this effect has not been seen when MMF is given at lower doses (401). A similar effect has not been noted in liver transplant recipients receiving MMF-tacrolimus-corticosteroid immunosuppression compared with those receiving the tacrolimus-corticosteroid combination (108). Nor was a difference in the incidence of CMV infection observed in lung transplant patients given either an azathioprine-containing regimen or MMF-based immunosuppression (387). Interestingly, MMF potentiates the anti-CMV activities of acyclovir as well as of ganciclovir (321).
The use of such compounds as antithymocyte or antilymphocyte globulin and muromonab-anti-CD3 (OKT3) monoclonal antibodies, either as induction therapy or for allograft rejection treatment, enhances the rate of symptomatic CMV infection, especially in CMV-seropositive individuals (9, 17, 45, 61, 197, 221, 242, 332, 344, 351, 359, 389, 420, 453, 505). These compounds not only diminish the capability of the host to mount immune surveillance but also increase reactivation of latent CMV from infected cells (45, 197, 242, 332, 359, 453). The risk is maximal when antilymphocyte therapy is used for the treatment of organ rejection, with CMV disease being diagnosed three to four times more frequently than in patients not receiving antilymphocyte therapy (197, 301, 394).
As new immunosuppressive agents are developed and introduced as part of the treatment arsenal for transplant patients, the incidence, severity, and relapse rates of CMV infection may be modified. This will have implications for viral surveillance and prophylaxis or preemptive therapy.
In addition to pharmacologic agents, pre- and posttransplantation circumstances that contribute to further enhance immunosuppression and/or the reactivation of latent CMV infection in the transplant recipient have been identified. A number of variables are associated with the development of CMV disease in liver transplant recipients. These are retransplantation for acute rejection (344, 451); fulminant hepatitis and preoperative liver dysfunction (17, 317); and infections with bacteria, hepatitis C virus (recurrence), and HHV-6 and HHV-7 (327, 421, 424). Other parameters that represent markers for CMV disease in liver transplant recipients include a prolonged prothrombin time and the occurrence of hepatic artery thrombosis (344).
Factors known to predispose kidney transplant patients to CMV infection include receipt of CMV-contaminated blood products, cadaveric allograft transplantation, and donor-recipient HLA mismatch (39, 162, 351, 402).
The amount of virus present in the transplanted graft may influence the frequency and severity of CMV disease posttransplantation. While this theory remains to be proven, it could explain the high rate of symptomatic CMV infection observed in lung and intestinal transplant recipients, reflecting the transmission of a higher latent CMV burden contained in larger amounts of tissue with more endothelial and lymphoid compartments. The clinical severity of CMV infection would then be commensurate with the presence or absence of specific immunity to CMV in the recipient. Consequently, prophylactic measures found to be effective for renal transplant recipients may not apply to lung or intestinal allograft recipients.
The way in which CMV induces organ dysfunction remains a matter of debate. Direct viral cytopathogenicity may be a factor, as in cases of CMV retinitis and gastrointestinal ulceration (462). The number of CMV-infected cells is however, not always a reflection of clinical disease severity: large numbers of CMV-infected cells may be present in tissues of asymptomatic patients, whereas small numbers of CMV-infected cells may be present in those with severe or fatal disease (462). CMV-triggered immune reactivity has been proposed, but sound evidence to support this is lacking (184, 427). Once CMV is activated and even before clinical manifestations occur, infection of circulating leukocytes, particularly granulocytes, can be demonstrated (398, 408, 479). Infected leukocytes presumably serve as means of transporting this highly cell-associated virus to other body sites. A phenomenon of particular interest is the interaction of CMV with the host response. One aspect of this interplay is the immunomodulating effect of the virus. CMV causes a metabolic abnormality in lymphocytes and monocytes that impairs their ability to produce and respond to cytokines (219). The virus itself appears to suppress the function of antigen-specific cytotoxic T lymphocytes and causes a change in the proportions of T-cell subsets, with an inversion of the CD4+ to CD8+ cell ratio (58, 103, 411, 413). CMV infection increases susceptibility to infection with other opportunistic agents, including Pneumocystis carinii, Aspergillus fumigatus, and Candida albicans (389). Furthermore, a higher rate of severe bacterial infections occurs in association with CMV infection in liver transplant recipients (316, 344, 477).
Regardless of the pattern and type of CMV transmission, the majority of patients who develop symptomatic disease do so 1 to 4 months after transplantation. CMV disease occurring later in the posttransplantation period may be noted in association with community-acquired primary infection, relapsing disease, the use of antilymphocyte antibody therapy to reverse rejection or, in liver transplant recipients, recurrent hepatitis C virus infection (196, 424).
CLINICAL MANIFESTATIONS
The consequences of CMV infection in solid-organ transplant recipients can be grouped into four categories. First, CMV causes a variety of infectious diseases syndromes produced by the virus itself. Second, CMV is associated with an augmented immunosuppressed state beyond that caused by administering immunosuppressive drugs, which may explain the frequent association of CMV with other infectious disease processes. Third, infection with CMV has been associated with allograft dysfunction. Fourth, CMV infection has been associated with decreased survival among transplant recipients.
Infectious Disease Syndromes
Depending on pretransplantation immunity and the degree of immunosuppression posttransplantation, CMV infection in solid-organ transplant recipients causes a wide range of clinical manifestations, from asymptomatic infection to severe, potentially lethal CMV disease. The term “symptomatic CMV infection” is used interchangeably with “CMV disease” herein. Most cases of symptomatic CMV infection are of mild to moderate severity and are rarely fatal in the current era of organ transplantation.
Mildly symptomatic CMV infection, or the so-called “CMV syndrome,” usually presents insidiously with fever, anorexia, and malaise without additional signs or symptoms. Prolonged fever lasting as long as 3 to 4 weeks may be the only manifestation of symptomatic CMV infection. Myalgias, arthralgias, and arthritis may occur, but the mononucleosis syndrome accompanied by lymphadenopathy or splenomegaly typically seen in immunocompetent hosts is rarely seen in transplant recipients. Hematologic abnormalities such as leukopenia, typically without the presence of atypical lymphocytes, and thrombocytopenia, are common. This viral syndrome may be self-limited or may progress to clinically evident organ involvement.
The clinical manifestations of CMV disease may be relatively nonspecific and can be difficult to differentiate from illnesses caused by a variety of other opportunistic microbes, acute graft rejection, and drug toxicity—all of which can cause fever and even organ dysfunction in transplant patients. Furthermore, several of these conditions may be present simultaneously. The clinical diagnosis of CMV is therefore unreliable; rapid and sensitive laboratory tests are essential diagnostic tools. Although viremic episodes usually accompany clinical symptoms, viremia as documented by surveillance cultures can be the sole indication of CMV infection in the absence of symptoms. Such asymptomatic viremia may herald CMV disease (231, 351, 352). Furthermore, asymptomatic infection may alter the posttransplantation course indirectly by its association with other infectious complications, such as bacterial and fungal infections (342, 344).
The consequences of CMV disease are similar in all transplant patients, although specific organ involvement by CMV frequently corresponds to the organ transplanted. CMV hepatitis occurs most frequently in liver transplant recipients; CMV pancreatitis occurs most often in pancreas transplant recipients; and CMV pneumonitis afflicts lung and heart-lung transplant recipients most regularly, especially among CMV-seronegative recipients of corresponding organs from CMV-seropositive donors (Table 1). A form of necrotizing and crescentic glomerulonephritis with intraglomerular CMV inclusions has been reported in a renal transplant patient (94). In addition, CMV myocarditis, although rare, typically presents in heart transplant recipients (180) and can cause cardiac dysfunction. Several possible explanations for the aforementioned phenomenon exist: an interaction between the effects of the virus itself and the effects of rejection on the allograft, a greater initial viral burden in the allograft (where reactivation first occurs), and/or the representation of a sequestered site for viral replication by the allograft. In addition, increased surveillance of the transplanted organ by tissue biopsy and culture may result in the more frequent recognition of its involvement with CMV.
Seronegative transplant recipients who acquire primary infection via transfusion of blood products generally have less severe CMV disease than do those who acquire the infection from transplanted organs (350). Patients with symptomatic CMV infection may develop pneumonitis, which characteristically presents as a dry, nonproductive cough within the first week of onset of constitutional symptoms (132, 389). A subset of these patients will have progressive dyspnea resulting in respiratory distress. Although physical examination may be unrevealing, arterial blood gas analysis may show hypoxemia. Chest X-ray appearances of CMV pneumonia include bilateral interstitial, unilateral lobar and nodular infiltrates (215). While a handful of transplant recipients with CMV pneumonia develop total opacification of the lung, this finding is distinctly unusual and should suggest the presence of other possible pathologies. The differential diagnoses would include allograft rejection and pneumonia caused by bacterial and fungal microorganisms, including P. carinii. In lung and heart-lung transplant recipients, however, CMV pneumonitis may present acutely, progressing over a short period to respiratory failure.
An important presentation of CMV infection is gastrointestinal disease. CMV can affect any segment of the gastrointestinal tract from the esophagus and stomach to the small and large intestines. Symptoms include dysphagia, odynophagia, nausea, vomiting, delayed gastric emptying, abdominal pain, gastrointestinal hemorrhage, and diarrhea (159, 441, 484). Intestinal perforation may ensue. A high index of suspicion for CMV colitis should be maintained in any organ recipient who presents with lower gastrointestinal tract bleeding in the first 4 months following transplantation. CMV enteritis may be lethal, and so early detection and intervention is required (329). Findings on endoscopy include erythema, diffuse shallow erosions, and localized ulcerations. These changes are not, however, specific for CMV disease, and tissue biopsy is essential for diagnostic confirmation (159, 456). CMV inclusion bodies or positive CMV cultures may be found from tissue(s) obtained at endoscopy even in the absence of gross intestinal mucosal abnormality; the significance and relevance of this finding is nonetheless unclear (425, 441). CMV has also been associated with biliary disease (241) and mesenteric/intestinal vasculitis, resulting in ischemic colitis (309).
Abnormal liver function tests occur in 30 to 55% of all solid-organ transplant recipients with systemic CMV infection (338). Among liver transplant recipients who develop symptomatic CMV disease, infection of the liver allograft is the most common manifestation. CMV hepatitis typically manifests as a elevation in the concentrations of gamma-glutamyltransferase and alkaline phosphatase, which peak 2 to 4 days following the rise in aminotransferase levels, with only minimal increases in bilirubin values (340). Differentiation of viral infection from rejection as a cause of hepatocellular dysfunction in liver transplant recipients can be a major problem; the only way this distinction can be made is by liver biopsy.
Chorioretinitis is generally considered to be an uncommon manifestation of CMV disease in transplant recipients, in contrast to patients with AIDS. Recently, however, evidence of healed scars consistent with CMV retinitis or active CMV retinitis has been found in a surprisingly high percentage (7.3%) of heart transplant recipients (134); this finding awaits more confirmation. CMV retinitis in solid-organ transplant recipients is distinctive in that it usually presents late (typically after more than 6 months) in the posttransplantation period. Patients may be asymptomatic at the time of diagnosis or may experience scotomata and/or decreased visual acuity. Although symptoms may be restricted to one eye initially, progression to bilateral involvement may occur (389). The diagnosis is made funduscopically; retinal lesions consist of fluffy white perivascular infiltrates, hemorrhage, and irregular sheathing of retinal vessels.
Less common presentations of CMV disease in organ transplant recipients include CMV involvement of the ureter, epididymis, skin, endometrium, and central nervous system (encephalitis, transverse myelitis) (233, 258, 291, 307, 330, 337, 346, 362, 403, 444, 452). There are anecdotal reports of CMV causing laryngitis (269), glomerulonephritis (167), and cutaneous infection (337) in solid-organ transplant recipients. Disseminated CMV disease is an ominous finding and may be fatal. Congenital CMV infection has been found in the offspring of female liver transplant recipients (247).
Opportunistic Superinfections
An important effect of CMV infection on the transplant patient is its potentiation of the individual's net state of immunosuppression, resulting in an increased susceptibility to opportunistic superinfection with a variety of pathogens. The clinical markers that delineate the patient with the most risk are viremia and CMV-induced leukopenia (394). Pulmonary superinfection may occur with P. carinii, A. fumigatus, and bacteria (389). CMV infection is a risk factor for the development of bacterial infection in liver transplant recipients (127, 316, 344, 475). There are also data to support the notion that bacterial sepsis in this group of patients predisposes to CMV infection (316). In the same fashion, having CMV disease or being a CMV-seronegative recipient of a CMV-seropositive donor liver appears to be associated with invasive fungal disease (146, 487). CMV pneumonia or viremia is highly predictive of the development of invasive aspergillosis following lung transplantation (209). These findings raise the question of the need for antiviral prophylaxis not only for the prevention of CMV infection itself but also for the prevention of its sequelae.
Allograft Dysfunction and Rejection
The association of CMV with allograft dysfunction is controversial. Infection with CMV has been associated with early-onset allograft rejection in renal transplant recipients (139). CMV-induced tubulointerstitial disease has been described following kidney transplantation (286). This is associated with a glomerulopathy characterized by hypertrophy and necrosis of endothelial cells, narrowing or obliteration of capillary lumens, and accumulation of mononuclear cells and fibrillary material in glomerular capillaries (375). Likewise, the incidence of chronic allograft nephropathy 2 years after transplantation is higher in patients who developed CMV infection (438). The role of CMV infection in renal allograft rejection has been investigated in a cohort of 242 renal transplant patients, 65% of who developed CMV infection (361). The incidence of rejection was significantly higher in those with antecedent CMV infection: 45% among infected patients versus 11% among noninfected patients. In another study, CMV-seropositive donor status was associated with lower graft survival rates than CMV-seronegative donor status (199). A recent report alluded to an association of CMV with renal artery stenosis in the transplanted kidney (360). This would imply that prevention of CMV infection might diminish the incidence of acute rejection episodes and possibly even chronic rejection and might improve the function and long-term survival of the renal graft. In one study, 80% of renal allograft recipients with biopsy-proven rejection responded to antiviral therapy with ganciclovir without modification of the immunosuppression regimen (373). CMV has an adverse effect on allograft survival. Graft survival is significantly reduced in CMV-seronegative recipients of CMV-seropositive living-related donor kidneys compared to CMV-seropositive recipients of the same allografts (410). In a separate cohort involving kidney and kidney-pancreas transplant recipients, the 3-year graft survival was 49 to 63% in those with one or more episodes of CMV disease and 78 to 81% in those without CMV infection or with asymptomatic CMV infection (402). Finally, in a retrospective analysis, the preemptive treatment of CMV viremia with ganciclovir in renal transplant recipients prevented CMV-induced renal injury and graft loss; patient survival was not different between patients with and without CMV infection (9).
Further evidence supporting the association of CMV infection with allograft injury comes from the experience with cardiac transplant recipients. CMV has been linked to the development of left ventricular dysfunction (293) and an increased incidence of graft atherosclerosis that is believed to be a manifestation of chronic rejection (144, 171, 229, 292, 415). However, a study of serial blood and endomyocardial tissue specimens from heart transplant recipients showed no association between acute rejection and the detection of CMV by using culture and a semi-quantitative PCR assay (46). While different patterns in the peak levels of CMV DNA in the blood and the heart were seen between those who experienced rejection and those who did not, none of the findings was associated with the development of rejection itself, supporting the view that CMV infection and rejection are independent events. By using angiographic criteria and autopsy findings for coronary artery evaluation, it was found that the risk of acquiring allograft coronary artery disease was not increased in association with active CMV infection (99). Further studies in which in situ DNA hybridization was used to detect the presence of CMV DNA in coronary arteries of cardiac allografts do not support a direct role for CMV in the development of accelerated coronary artery disease (187). While there may be no difference in the incidence of rejection, an increase in the repeated rejection rate in transplant recipients with heart allografts from CMV-seropositive donors suggests the possible impact of CMV in the enhancement but not in the induction of rejection (87). An interesting association has been made between CMV and hepatitis C virus coinfection and an increased risk for allograft vascular disease in a heart transplant population (82). It is also suggested that CMV plays a role in the development of bronchiolitis obliterans in lung transplant patients (27, 28, 227, 243, 414); CMV seropositivity and infection were both identified as risk factors (193).
As suggested above, the direct effects of CMV infection on the liver can mimic hepatic allograft rejection. In addition, the contributing effects of recurrent viral hepatitides on the graft are difficult to ascertain. In the setting of CMV viremia, histopathologic findings of focal necrosis and clustering of neutrophils within the liver lobules distinct from that of typical allograft rejection have been described (340). After liver transplantation for chronic hepatitis C, patients who develop CMV viremia incur a significantly greater risk of allograft cirrhosis and graft failure from recurrence of hepatitis C infection (384). Contrary to previous studies describing CMV infection as a risk factor for the development of the vanishing bile duct syndrome (a form of ductopenic rejection frequently leading to graft loss and the need for retransplantation) (326), no association was found between these two events when patients were monitored with the antigenemia assay (476). Nevertheless, the persistence of CMV DNA within hepatocytes of patients with the vanishing bile duct syndrome, determined by in situ hybridization, lends credence to this association (13). In patients monitored for up to 3 years, CMV disease was strongly associated with chronic rejection: 29% among the infected versus 8% among the noninfected subjects (89). Additionally, the receipt of CMV-seropositive allografts by CMV-seronegative liver transplant candidates may predispose these individuals to the development of hepatic artery thrombosis (274).
In patients undergoing intestinal transplantation, a positive donor CMV serology is associated with increased graft loss (467).
The causative link between CMV and allograft injury remains speculative, and more studies are needed to corroborate this association.
Patient Outcome
The indirect effects of CMV infection on graft and patient survival have been increasingly recognized in recent years. CMV disease resulted in decreased patient survival in a group of kidney transplant patients with 4 years of follow-up (117).
The long-term outcome of individuals with CMV infection following liver transplantation has generated intense interest among transplant physicians. Among those monitored for a long period, CMV disease has proved to be an independent risk factor for reduced rates of patient (and graft) survival after liver transplantation. CMV disease in individuals who have received liver transplants has been independently associated with higher mortality rates at 1 year (123, 124) and with increased costs and longer hospital lengths of stay in the first posttransplant year (123). In other studies, previous CMV infection and/or disease led to poorer patient outcomes at 1 year and up to a twofold-increased risk of death or graft loss during 3 (92) and 5 (385) years of follow-up. Untreated symptomatic CMV viremia is an identified risk factor for death or retransplantation in liver transplant recipients (17). The mechanism underlying such poor outcome for CMV-infected graft recipients is postulated to be a consequence of the indirect effects of CMV infection, although the specifics of this interaction remain to be determined.
The impact of CMV disease on patient survival has also been studied among heart transplant recipients. In one study, the 5-year survival was 32% in the group that developed CMV compared to 68% in the no-CMV group (171). The predominant causes of death were infection and graft atherosclerosis, both of which were more prevalent in the group with CMV disease (171). A CMV-seropositive donor has been identified as a risk factor for mortality following heart transplantation (290). CMV-seronegative lung transplant patients who received allografts from seropositive donors developed early bronchiolitis obliterans syndrome at a greater frequency and tended to have worse survivals compared to those who were not CMV mismatched (427).
Although controversial, results of epidemiologic studies suggested an enhanced risk of EBV-related posttransplantation lymphoproliferative disease (PTLD) in CMV-infected transplant patients (17). A history of preceding symptomatic CMV disease is a risk factor for the development of PTLD after organ transplantation (31, 276). A CMV seromismatch amplifies the risk of PTLD four- to sixfold in EBV-seronegative recipients of EBV-seropositive organs (488).
An implication of the above findings is that CMV prophylaxis may affect graft and/or patient survival. In this regard, a recent study has shown an improved 3-year kidney allograft survival in patients receiving CMV prophylaxis (39).
Recurrent Infection
Like other members of the herpesvirus group, CMV is associated with persistent latent infection. While treatment of CMV disease with currently available antiviral agents frequently controls the acute manifestations of the illness, it does not eradicate CMV infection. In solid-organ transplant recipients, CMV disease may recur after successful treatment of the initial episode. Recurrent disease is a substantial cause of posttransplantation morbidity; the reported rates of reoccurrence vary with the organ transplanted. Studies of kidney and kidney-pancreas transplant recipients indicate that disease relapses occur in 6 to 31% of patients (208, 217, 402). Recurrent CMV disease occurs at an incidence of 26 to 31% after liver transplantation (125, 126, 478). Although intestinal transplantation is done much less frequently than transplantation of other solid organs, recurrent CMV disease may occur in over half of those who have received prior treatment for CMV (277). The bowel allograft is the most common site of involvement for recurrent CMV episodes in intestinal transplantation recipients. CMV disease recurred in up to 12% of cardiac transplant patients monitored for up to 1 year after the initial episode (234). The broad range of relapse rates may be reflective of differences in the definitions of CMV infection and disease, variations in treatment regimens, dissimilarity in immunosuppressive regimens, and/or variability in the number of patients at risk amongst different studies, or true differences in disease recurrence among the diverse types of solid organ transplant recipients. For study purposes, the adoption of the criteria for the definition of CMV infection and disease established during two International CMV Workshops is encouraged (264, 265).
Most cases of recurrent CMV disease occur within 3 months after treatment for the first episode and tend to involve multiple organs. Recurrent disease has been associated with increased death rates (126). Despite the relatively high rates of CMV recurrence, epidemiologic data on the factors that predict relapse are scant. A cadaver organ source for renal transplantation is a significant risk factor for recurrent disease (208). Among recipients of liver allografts, primary infection is associated with a higher incidence of disease relapse (125, 126), suggesting that a deficient immunologic response in the host incites viral reactivation. These observations carry the implication that CMV viral burden may be partly responsible for relapsing infection. A large number of activated CD8+ cytotoxic T lymphocytes and a low quantitative level of CMV antigenemia at the end of antiviral therapy were both associated with a low risk of relapse (478). Conversely, the loss or persistent lack of CMV-specific T-helper response following infection has been associated with chronic and recurrent CMV disease (506). Antirejection therapy is postulated to be a predictor of disease recurrence (208, 277, 402). Investigations are in progress to determine the role of the CMV burden in modifying the course of CMV disease and the frequency of disease relapse. Clearly, there is a need for more specific markers that can identify patients at risk. This will enable the identification of the subgroup of solid-organ transplant recipients at a higher risk for recurrent illness, in whom more intensive therapeutic, prophylactic, or surveillance approaches may be warranted to curtail the adverse patient and/or graft outcomes that result from recurrent CMV infection.
DIAGNOSIS
Because of the considerable impact of CMV infection in transplantation, rapid and accurate methods of diagnosis are of utmost importance. The array of diagnostic tools now available allows not only precise serologic determination of past exposure to CMV infection but also the identification of CMV components (e.g., viral DNA and infected leukocytes) in blood during viremia and in infected organs. Broadly categorized, diagnostic studies for CMV include serologic and virologic tests (Tables 2 and 3). The methodological aspects of a number of molecular procedures applicable to the investigation of CMV have been recently reviewed (40, 205).
TABLE 2.
Diagnostic testing for CMV
| Method | Specimen(s)a | Comments |
|---|---|---|
| Serology | Blood | Not helpful in diagnosing CMV infection or disease in transplant recipients because of delayed seroconversion; good for pretransplantation evaluation to assess the likelihood of reactivation infection (if positive) or susceptibility to primary infection (if negative) |
| Conventional tube cell culture | Blood, tissue, urine, BAL, CSFb | Long (1–3 wk) turnaround time; cytotoxicity occasionally precludes viral isolation; used for viral isolation for antiviral susceptibility testing |
| Shell vial assay | Blood, tissue, urine, BAL, CSFb | Rapid (1–2 days); positive result from blood implies active CMV infection |
| Antigenemia assay | Blood | Rapid (same day); requires little laboratory support; more sensitive than shell vial assay, less sensitive than PCR; quantitative results |
| Histopathology | Tissue | Detects viral inclusion bodies; insensitive marker of CMV disease; sensitivity enhanced with immunostaining; requires use of invasive procedures to obtain sample |
| In situ DNA hybridization | Tissueb | Confirmation of tissue involvement with CMV |
| PCR amplification | Blood, tissue, urine, BAL, CSFb | Detects viral DNA and/or RNA; extremely sensitive, but not specific for symptomatic infection; allows quantitation of viral load; not standardized |
| Hybrid capture assay | Blood, tissueb | Rapid; detects viral DNA; less sensitive than PCR |
| bDNA assay | Blood, CSFb | Less sensitive than PCR; highly reproducible |
| NASBA | Blood, tissueb | Detects viral RNA; highly sensitive; investigational |
Abbreviations: BAL, bronchoalveolar lavage fluid; CSF, cerebrospinal fluid.
Other bodily fluids and clinical specimens may also be amenable for testing.
TABLE 3.
Prognostic values of methods for CMV detection in blood
| Method and sample (reference) | Sensitivity (%)a | Specificity (%)a | Lead time (days)b |
|---|---|---|---|
| Shell vial assay | |||
| Blood (163, 351) | 8–63 | 86–88 | 2–16 |
| PCR amplification | |||
| Serum/plasma (297, 336) | 50–100 | 45–63 | 12–16 |
| Peripheral blood mononuclear cells (92, 297) | 20–100 | 35–91 | 14–21 |
| Reverse transcriptase PCR (335) | 17 | 97 | 0 |
| Antigenemia assay (107, 117, 239, 458, 464, 469, 474) | 50–83 | 71–80 | 4–14 |
Sensitivity and specificity as a marker of future CMV disease.
Number of days preceding clinical symptoms that assay is positive.
Serology
The main utility of serologic studies in organ transplantation is as an accurate and sensitive means of determining a past history of CMV infection in potential organ donors and allograft recipients. CMV serology is also useful for screening potential blood donors. Serology is an insensitive marker of active CMV infection in the organ transplant population and is therefore of limited diagnostic usefulness (282, 409, 482). Many patients with positive CMV cultures do not show concomitant evidence of seroconversion (343).
Serology requires a short execution time, is safe, and can be completely automated. Numerous test methods are available for the determination of the anti-CMV antibody titer in serum with different degrees of sensitivity; these include complement fixation, enzyme-linked immunosorbent assay (ELISA) and latex agglutination (111, 250). The most widely used procedure is the ELISA, for which there are various commercial products. Compared to complement fixation, ELISA gives higher antibody titers, is easier to perform, and eliminates the problem of anticomplementary sera (65).
Histopathology
The diagnosis of CMV infection has traditionally been based on the histologic recognition of cytomegalic inclusion bodies that have the characteristic intranuclear owl-eye appearance in haematoxylin and eosin-stained tissue specimens. Tissue biopsy is an important tool for diagnosing the causes of allograft dysfunction and can often differentiate inflammatory response provoked by CMV from cellular rejection (29, 73, 472). The presence of viral inclusion bodies in liver tissue, for instance, correlates with active disease in most cases (73). Conversely, CMV may be detected in cultures of biopsy specimens that are negative on histopathology (340).
Immunostaining
The use of immunohistochemistry has increased the sensitivity for the histologic diagnosis of CMV disease compared to standard hematoxylin and eosin staining (29, 73, 119, 341). Immunostaining techniques use either a monoclonal or a polyclonal antibody against an early CMV antigen. When this procedure was used on liver allograft biopsy specimens, its sensitivity and specificity approached 84 and 97% in one study (341). False-negative results may occur, however, because of the focal distribution of CMV-positive cells (73). Moreover, while the histologic criteria for acute liver graft rejection are well accepted, the criteria for the histomorphologic changes associated with CMV hepatitis vary considerably (29). While important for the identification of localized CMV disease, tissue diagnosis is limited in many instances by the need to use invasive procedures to obtain samples.
In Situ Hybridization
In situ hybridization (ISH) with CMV-specific complementary DNA probes applied to cellular material has facilitated the histopathological identification of infected cells in tissue (288, 341). Hybridization has conventionally been performed with probes labeled with radioactive isotopes, which then allows the detection of sequence specific nucleic acid following autoradiographic analysis (140). The routine use of radioactive isotopes has largely been replaced by biotinylated DNA and electrochemiluminescent labels (113, 312). Biotinylated probes may be used for the direct detection of CMV inclusions in formaldehyde-fixed, paraffin-embedded tissue sections in cases where active infection is present (Fig. 1). Estimation and quantification of nucleic acid present in tissue samples or cellular smears may also be possible with ISH. The comparative sensitivity of ISH for diagnosing CMV disease varies in different studies. Most reports do not favor the use of ISH over conventional histopathologic examination for the diagnosis of CMV organ disease (29, 73, 119, 341, 364). Nonetheless, this method allows the rapid detection of CMV in tissues (286, 472).
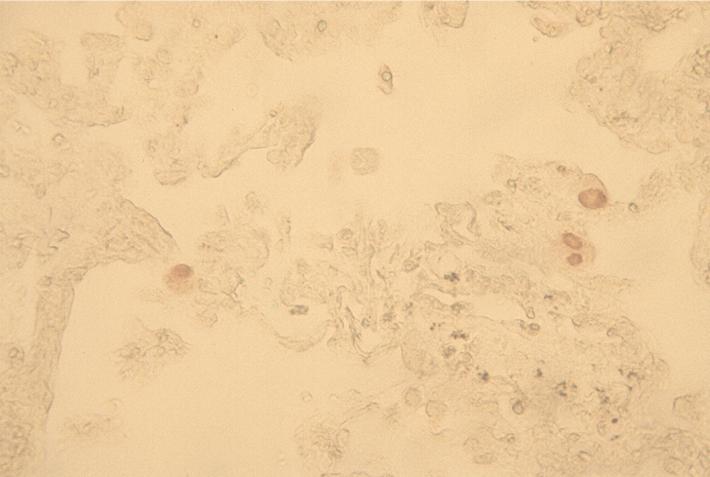
FIG. 1.
CMV is visualized by the in situ hybridization technique on a sample of lung tissue.
ISH studies may be of greatest use when the results of conventional histopathology are equivocal (492, 503). Furthermore, the test specificity for allograft biopsy specimens is as high as 100% (286, 341, 492). Applications for this test include the diagnosis of CMV pneumonitis (113, 160, 436, 493), hepatitis (286, 341) and gastroenteritis (65, 308, 503). However, the techniques involved are cumbersome. Specimen preparation consists of securing the sample to a glass slide and denaturing the DNA without detaching or destroying the morphologic identity of the cells.
Cytomegalic Endothelial Cells
Within the last decade, circulating cytomegalic endothelial cells (CEC) have been found in the blood of immunocompromised patients with disseminated CMV (173, 348). The presence of these cells is considered to indicate extensive endothelial damage. They are derived from infected endothelial cells of small blood vessels; these cells progressively enlarge, become detached, and enter the bloodstream. These cells can be identified by cytocentrifugation of the mononuclear fraction of leukocytes onto glass slides followed by endothelial cell-specific staining. A method for quantification of CEC in peripheral blood has also been described (220). In patients with AIDS, the detection of CEC is associated with lack of anti-CMV treatment, emergence of drug-resistant CMV, insufficient treatment, or transient response to antiviral therapy (152). In the transplant recipient population, CEC are not observed in patients taking prophylactic or preemptive therapy. More data pertaining to the applicability of this test in organ transplantation should be forthcoming.
Viral Isolation
Conventional detection of CMV in clinical specimens is achieved by direct viral culture. The detection of CMV in tissue cultures from peripheral sites such as urine or saliva is often uninformative because the virus may be present in these sites for prolonged periods after the acute phase of infection and during viral reactivation. Nevertheless, viral isolation from these sites indicates a relative risk of about twofold for future CMV disease (231, 351, 352). Furthermore, viral isolation from any site in a CMV-seronegative transplant recipient is indicative of primary CMV infection.
For conventional cell culture, clinical specimens are inoculated onto human fibroblast cells, e.g., cells obtained from the foreskin or embryonic lung, and incubated at 37°C. In the standard tube cell culture technique, CMV exhibits a typical cytopathic effect (CPE) characterized by foci of flat, swollen cells (Fig. 2). The time required for the development of CPE is directly related to the titer of the virus in the sample. Typically, the mean time for CPE to be visible is 8 days, but it can range from 2 to 21 days. The long time required for diagnostic confirmation by this method limits its clinical usefulness. Cytotoxic effects of leukocytes on the fibroblasts and overgrowth of more rapidly growing microorganisms (such as herpes simplex virus or bacteria) may preclude viral isolation. Many modern clinical microbiology laboratories no longer routinely offer tube cell culture for CMV. Viral isolation may, however, be useful for some antiviral susceptibility testing methods (see below).
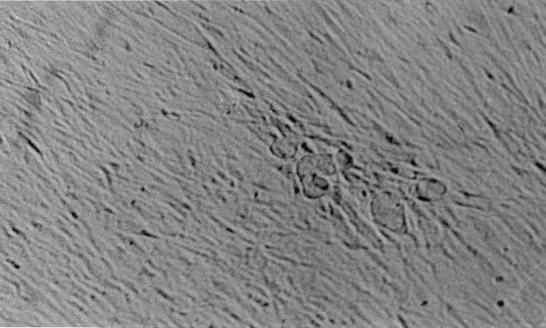
FIG. 2.
On a standard cell culture inoculated onto a human fibroblast monolayer at 37°C, CMV characteristically exhibits cytopathic effects, appearing as foci of flat, swollen cells.
Several rapid tests for the identification of CMV have been developed. Modifications of the traditional method for viral culture have allowed the early detection of CMV in cell culture. Detection of CMV-specific early-antigen fluorescent foci by using the shell vial assay permits the detection of CMV prior to the development of CPE in conventional tube cell culture (Fig. 3). Shell vial assays are performed in vials containing 12-mm round coverslips containing a fibroblast monolayer (161). Centrifugation of specimen onto the cell monolayers greatly assists absorption of virus, increasing apparent infectivity of the viral inoculum (65, 68). The shell vial assay utilizes a monoclonal antibody directed at the immediate-early (IE) viral antigen to detect CMV by indirect immunofluorescence after 16 h of incubation (345, 371). Due to a high rate of false-negative results, viremia is useful only in the setting of a positive result and should be considered a parameter of risk for the development of CMV disease (305). Akin to bacterial blood cultures, multiple viral blood cultures may be necessary to detect CMV by the shell vial assay (333). Nevertheless, the number of positives identified by the shell vial assay is greater than that detected by conventional culture (318). Development of viremia detected by shell vial culture more than 2 months after liver transplantation is a strong predictor of CMV disease (278).
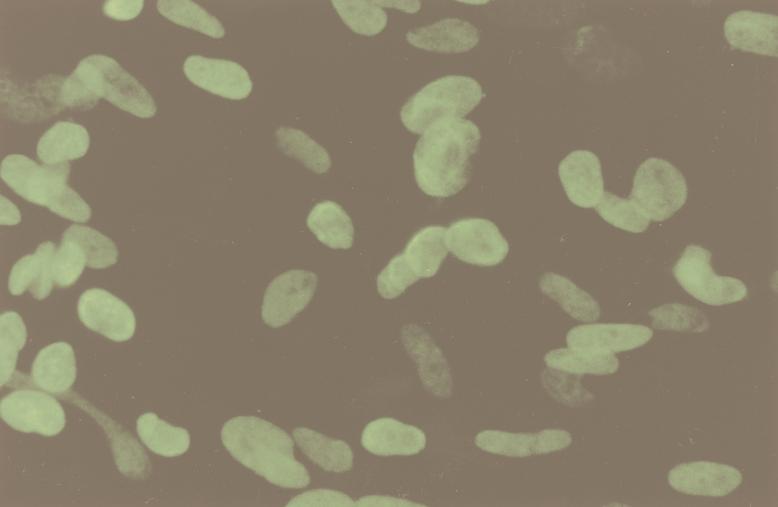
FIG. 3.
Detection of CMV-specific early-antigen fluorescent foci in the shell vial assay indicates the presence of the virus.
A delay in specimen processing of longer than 24 h severely compromises the sensitivity of the shell vial assay, limiting its usefulness for testing samples that are mailed in from patients in the outpatient setting. As the interval to sample processing increases, the sensitivity of the shell vial culture progressively declines, with only 44 to 55% positivity at 24 h and 10% positivity at 48 h (50, 252, 380). Storage at either room temperature or 4°C has no significant effect on shell vial culture results (380). Additionally, the test sensitivity increases with increasing quantities of polymorphonuclear leukocytes inoculated in shell vials (372). Quantitative culture methods involving the shell vial assay has been described (20, 68, 154, 449, 460), but the practical value of this approach is not apparent.
Overall, the culture-based assays do not require highly specialized equipment. Problems often encountered include poor plaque formation by some CMV strains, rapid loss of viability, and nonspecific monolayer toxicity.
Antigenemia Assay
The antigenemia assay has been a major advance in the diagnosis of CMV infection in organ transplantation. The presence of CMV antigenemia in blood leukocytes provides an early marker of active CMV infection and is a rapid test for the detection of CMV viremia (474). This assay depends on the use of monoclonal antibodies that detect the viral pp65 antigen, a structural late protein expressed in blood leukocytes during the early phase of the CMV replication cycle (Fig. 4). This test is limited to detection of the virus in leukocytes; the demonstration of positive-staining signals in the nuclei of leukocytes indicates a positive result. The test not only gives a qualitative result but is also quantitative, correlating closely with viremia and clinical disease severity (266, 323, 466).
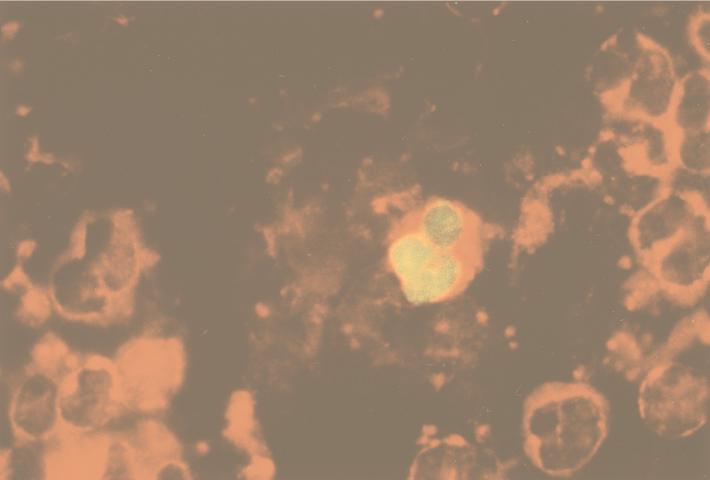
FIG. 4.
Expression of CMV pp65 antigen in polymorphonuclear leukocytes on a cytospin slide detected by immunoperoxidase staining. Courtesy of K. St. George and C. Rinaldo, University of Pittsburgh Medical Center.
CMV antigenemia testing consists of a number of steps, including isolation of blood leukocytes by dextran sedimentation or direct leukocyte lysis, preparation of microscopic slides, immunostaining with the use of monoclonal antibody to CMV, microscopic evaluation, and quantitative scoring (115, 203, 463, 465). Cytospin slides containing a given cell number are prepared by centrifugation of leukocyte-rich supernatant. Slide fixation is performed with either formaldehyde or acetone; superior results are obtained with formalin fixation (41, 158, 466). Slides are stained with monoclonal antibody directed against the CMV lower matrix phosphoprotein pp65 antigen. Immunodetection of CMV antigen is possible with either indirect immunoperoxidase or indirect immunofluorescence methods (463). Immunoperoxidase staining enables the enumeration of negative cells in conjunction with positive cells, resulting in a more accurate assessment of positivity; in contrast, immunofluorescence gives clearer signals from positive cells (463). Another technique involves the use of alkaline phosphatase/anti-alkaline phosphatase (APAAP) staining in an effort to improve test sensitivity and specificity (158). The results may be reported as the number of positively stained cells relative to the number of cells used to prepare the slide. Another method is to quantify the result per 50,000 cells, estimated by the number of cells on each slide (227, 479). Interlaboratory variability is nonetheless substantial (36).
The presence of a small number of antigen-positive cells following solid-organ transplantation generally indicates asymptomatic infection, whereas a large number implies an increased likelihood of CMV disease; the exact cutoffs for this assay, however, remain to be defined and may vary among different types of transplant recipients and among individual assays (142, 266, 311, 323, 466, 505). While antigenemia is highly sensitive and specific for the diagnosis of CMV infection, both the specificity and positive predictive value of the test for the diagnosis of CMV disease are less impressive; that is, patients with asymptomatic infection are frequently antigenemia positive (313, 505). Within a group of kidney transplant patients, an inverse correlation between the host humoral and cellular immunocompetence and antigenemia test positivity has been demonstrated (465). Larger numbers of positive cells may be seen in association with primary CMV infection than in association with either reactivation infection or reinfection (211). Overall, the sensitivity of antigenemia testing is close to 100% for CMV disease and 60 to 70% for asymptomatic infection (36, 169). Antigen detection may also be used for the direct identification of CMV-infected cells in bronchoalveolar lavage fluid (436, 437).
Antigenemia has several inherent advantages. It is a normalized assay, giving a measurement of the number of CMV-positive cells relative to a fixed number of leukocytes. It is fast, with a typical hands-on time of 4 to 5 h. Additionally, certain modifications to the test can allow a shorter processing time (203). The assay is easy to perform, does not depend on cell culture technology, does not require the use of sophisticated laboratory equipment, and has a greater sensitivity than viral isolation (151, 253, 479). Its ability to quantify the viral burden is its best feature. The major drawback of this test is the need for immediate (within 6 h) processing of blood samples to achieve optimal sensitivity (406). Delays in sample processing for longer than 24 h result in significant decreases in the number of detectable pp65-positive cells in blood specimens (41, 406); with some modifications and the use of stabilization reagents, this obstacle may be overcome (55). False-negative results may occur in neutropenic patients, since the antigenemia test depends on the presence of a sufficient number of polymorphonuclear leukocytes (261). It also has the disadvantage of being labor intensive; it demands the skill of an experienced technician for accurate test interpretation. Moreover, variations exist with regard to the exact method, and therefore results from different laboratories may be difficult to compare. In sum, a qualitative antigenemia test result is a sensitive marker for the presence of CMV in the blood but does not necessarily mean CMV disease. On the other hand, its quantitative version is a useful tool for predicting CMV disease and for monitoring antiviral therapy.
PCR Amplification
Nucleic acid amplification by PCR has become a widely available diagnostic tool for CMV; it is increasingly being used in solid-organ transplantation. PCR techniques can detect CMV DNA in peripheral blood leukocytes (91, 278) and whole blood (231), as well as CMV RNA in leukocytes (169, 170, 335, 368). Although CMV is a cell-associated virus, CMV DNA can also be detected in cell-free body fluids such as serum (81, 107, 122, 315, 336) and plasma (117, 151, 440).
PCR is a target amplification method that uses DNA polymerase to produce elaboration of target DNA. The assay involves several basic steps, namely, specimen preparation, DNA extraction, amplification by thermal cycling, and amplicon detection. Depending on the clinical specimen being used, extraction of nucleic acid is done by one of a number of ways. Alkali lysis with proteinase K digestion followed by heat inactivation of the enzyme is in common use. An additive extraction step involving phenol-chloroform has also been described. However, some authors have reported that alkali lysis and proteinase K digestion alone is superior for detecting CMV DNA in blood leukocytes compared with additive phenol-chloroform extraction (117, 118).
Performing PCR on DNA extracted from infected leukocytes allows the rapid diagnosis of CMV infection. Although PCR is extremely sensitive and specific in detecting the presence of CMV DNA, there is the concern that a positive signal resulting from the presence of very few DNA copies may not differentiate between replicating and latent viruses (91, 142, 157, 507). On the other hand, negative CMV detection by PCR strongly advocates against CMV infection (33, 278, 347, 448). Additionally, a positive PCR signal for CMV in a seronegative recipient is significant because it indicates primary infection (278). The detection of latent CMV DNA in seropositive patients in the absence of clinical disease limits the clinical utility of CMV PCR. This shortcoming, together with the hypothesis that active viral replication may lead to the release of virus from cells into serum, has led to studies comparing leukocyte and serum PCR for CMV. Among solid-organ transplant recipients, the detection of viral DNA in serum by using CMV PCR is a sensitive and specific indicator of early infection (81, 107, 122). While further studies are needed to determine its prognostic value in the various groups of organ transplant patients, serum or plasma has a number of advantages over separated leukocytes for the detection of virus: it is readily available as it is one of the commonest specimens sent to the laboratory, and it requires very little preparation before DNA extraction. Comparative studies with peripheral blood leukocytes and plasma samples have been done for organ transplant recipients (117, 151, 190). While plasma PCR may be of clinical utility, further evaluation is needed before firm recommendations can be made on its applicability. PCR can also be of clinical value when analyzing urine (78, 121), bronchoalveolar lavage fluid (240, 448), cerebrospinal fluid (70, 170, 491, 499), aqueous and vitreous humor samples (133, 149, 304), tissue biopsy samples (48, 54, 112, 268, 501), and other miscellaneous body fluids (259).
Several protocols for the PCR detection of CMV have been described. However, these tests vary in the technical aspects of the amplification procedure, such as choice of target sequence, characteristics of primers, amplification rounds, and use of nested PCR assays or hybridization steps targeting internal sequences of the amplicon. The lack of standardization of the test methodology complicates the identification of the optimal assay with the highest sensitivity and specificity for CMV disease. Standardization of qualitative PCR methods has not yet been achieved. These assays should also be standardized for the number of cells from which DNA is extracted (379). An advantage of amplification methods over culture and antigen detection assays is that samples can be stored at room temperature for up to 72 h with no significant alteration in the level of detectable DNA (50, 380, 406). As well, PCR can detect CMV DNA from the blood of patients with localized disease. However, PCR techniques are technically challenging, especially when used for the detection of viral RNA (see below), and are subject to possible false-positive results secondary to contamination. Accordingly, strict quality control is necessary when performing PCR in clinical laboratories (182).
Although PCR for CMV DNA detection in peripheral blood leukocytes is currently the most sensitive procedure for detecting viral infection, when PCR is carried out in a nonquantitative way, it is of little clinical value since the results obtained do not correlate with clinical symptoms (305). In CMV-seropositive recipients, CMV DNA detection by PCR often fails to correlate with disease; therefore, specific test modifications are needed (157). The measurement of viral load by quantitative PCR appears to be a promising development that may be important for the diagnosis and prediction of CMV disease, for differentiation of latent from active infection, and for monitoring of therapy (91, 122, 141, 315, 358, 379). Methods developed for DNA quantitation by PCR may be classified into three categories: semiquantitative, competitive, and noncompetitive quantitative assays.
Semiquantitative PCR methods provide only relative data. These procedures are designed to perform titer determinations of the target template or of an external control by end-point sample dilution prior to PCR (102, 245) or by coamplification of target and an endogenous cellular (e.g., β-globin) DNA sequence (228). The amount of DNA is extrapolated from a standard curve derived from the amplification of known amounts of the external standard. By using this method, significantly higher levels of CMV DNA were seen in liver transplant recipients with CMV disease than in asymptomatic CMV-infected allograft recipients (101, 122, 255, 347). After treatment, clearance of CMV DNA with undetectable PCR signal has been associated with the disappearance of symptoms (101).
Competitive quantitative PCR methods are based on the coamplification of an exogenous template as an internal standard that competes with the target DNA sequence using the same set of primers (148). The two amplification products are differentiated by the presence or absence of a restriction site or by differences in electrophoretic mobility in a temperature gradient gel electrophoresis system. The amplified target is measured by densitometric evaluation of ethidium bromide-stained gels or after hybridization procedures.
In a noncompetitive quantitative PCR approach, an internal standard is used that has the same primer binding sites as the target nucleic acid but differs in the intervening sequences used for detection of the amplified product (151, 200). The internal standard is added at a known copy number; the target and internal standard are coamplified and detected with probes that have different binding sites.
Quantitation of CMV DNA in blood leukocytes may have practical implications for the diagnosis of visceral organ disease during viremia. The median quantity of DNA in the leukocytes of patients with visceral organ disease is significantly greater than that in patients with viremia alone (399). Compared with serum samples, peripheral blood leukocyte specimens from patients with CMV disease have generally higher CMV DNA titers (347). By using a quantitative PCR method on paired buffy coats and sera from liver transplant patients with symptomatic CMV infection, serum titers were found to be concordant with buffy coat titers (315). The CMV titer in serum falls as symptoms resolve with specific antiviral therapy. Similarly, viral DNA detection in plasma is consistently associated with leukocyte DNA titers, although leukocyte titers are consistently higher than those from plasma (151). Quantitative PCR on tissue samples, e.g., transbronchial biopsy specimens, also has potential applications for the diagnosis of CMV disease (240). Prospective studies will allow the confirmation of the predictive value of determining the viral load in body tissues.
High CMV DNA titers in blood are associated with clinical symptoms in transplant patients. CMV infections occurring early in the posttransplantation period, that is, within 2 months of transplantation, appear to have higher viral loads, most probably because immunosuppression is more intense, and are usually associated with disease (278). Viral titers rise presymptomatically in some cases (314). In addition, the maximum CMV DNA level during infection is significantly higher in patients who are experiencing primary infection compared to those who have asymptomatic and/or reactivation CMV infection (148, 278, 314, 378, 399, 470). After the initiation of antiviral therapy, CMV DNA levels in blood fall rapidly, correlating with the disappearance of clinical symptoms. In contrast, patients unresponsive to therapy have persistent high levels of virus DNA (347, 470).
Quantitative PCR is being touted as possibly one of the best diagnostic methods for CMV diagnosis (135). However, each of the techniques suffers from one or more of several pitfalls. Namely, they provide relative rather than absolute figures, may need two different primer pairs for amplification, lack standardization, are labor-intensive, and engender long turnaround times. In general, most quantitative PCR protocols have not been universally applicable because of their expense, laborious detection procedures, and a limited potential for batch testing. Notwithstanding, PCR has the potential to rapidly and accurately quantify small amounts of target nucleic acids in clinical specimens. With more sophisticated technical developments, these problems may be rectified, especially with the evolution of automated methods that are standardized to provide results that are reproducible and reliable within a short period.
As an example, a commercially available PCR-based test, the AMPLICOR CMV Test (Roche Molecular Systems, Branchburg, N.J.) has been developed for the detection of viral nucleic acid. It is a microwell plate assay designed to detect CMV DNA in an ELISA-like colorimetric format following nucleic acid amplification. Preliminary evaluation shows concordance of the results of the AMPLICOR CMV Test with the antigenemia assay (200). The COBAS AMPLICOR CMV Monitor (Roche Molecular Systems) is a fully automated system intended for PCR amplification, detection, and quantitation of CMV in clinical samples (96, 218). This system amplifies target CMV DNA, captures the biotinylated amplification product with a specific oligonucleotide probe, and detects the bound products colorimetrically. In addition to accuracy of automated results, the COBAS AMPLICOR system provides labor savings, simplifies laboratory setup, consolidates steps, and reduces hands-on time; results are produced in less than 6 h.
To identify active viral replication, some workers have developed amplification assays for viral mRNA in leukocytes (169, 170, 368). The presence of CMV IE mRNA has been demonstrated in monocytes and polymorphonuclear leukocytes during active CMV infection (249, 463). Reverse transcriptase PCR can be used to selectively detect viral mRNA transcripts coding for structural and nonstructural proteins in peripheral blood leukocytes. The absence of circulating mRNA is associated with a lack of CMV-associated symptoms, irrespective of the presence or absence of CMV DNA, while its presence is detected only in the setting of disease (368). It appears to be less sensitive, however, than the pp65 antigen test (302) and shell vial culture and PCR (335) in diagnosing CMV disease. RNA degradation in vitro can give rise to false-negative results (169, 368). Nevertheless, its excellent specificity makes it a potentially useful tool for distinguishing asymptomatic infection from clinical disease and in the follow-up of patients treated for CMV infection.
Other Amplification Methods
Non-PCR procedures including those that amplify the signal generated rather than the DNA or RNA themselves are also available as quantitative tests to detect CMV DNA. These tests, which use whole-blood and leukocyte samples, utilize chemiluminescence for signal detection and can provide quantitative results.
The hybrid capture assay (HCA; Digene Diagnostics Inc., Silver Spring, Md.), is a solution hybridization antibody capture assay that uses an RNA probe to hybridize with viral DNA (289). The resultant hybrid is captured by a monoclonal antibody specific for the DNA-RNA hybrids, and the resulting signal is measured on a luminometer. Unlike PCR, this assay detects CMV DNA directly and does not require an amplification step. Qualitative and quantitative assessment of CMV DNA are obtained. A handful of studies evaluating the HCA for solid-organ transplants show that high leukocytic viral loads strongly correlate with the onset of CMV disease, indicating more intense viral replication (244, 272, 381, 399). After ganciclovir treatment, significant reductions in the viral loads are observed; a positive result is associated with recurrence of active CMV infection (213). The HCA provides a rapid (less than 6 h) quantitative measure of CMV activity in leukocytes and is well suited for large-volume testing. However, data is lacking to support its superiority over other test methods such as antigenemia and PCR assays and to advocate its routine clinical application at present.
The branched DNA (bDNA) assay (Chiron Corp., Emeryville, Calif.) uses bDNA amplifiers to effect signal amplification during hybridization (62). It measures viral nucleic acids directly from clinical specimens by boosting the reporter signal rather than amplifying target sequences as the means of detection. The bDNA molecule contains multiple binding sites for an enzyme-labeled probe. The target nucleic acid is bound to the bDNA molecule, and the complex is detected with a chemiluminescent substrate. The test allows the direct quantification of CMV DNA in blood. The lack of amplification makes the test less susceptible to contamination. Although this test is less sensitive than most antigenemia and PCR assays, it may be amenable to routine use in the clinical setting (111). Data supporting the value of this test in solid-organ transplant recipients is needed.
Nucleic acid sequence-based amplification (NASBA) is a specific isothermal technique of amplification. Unlike PCR, NASBA is most suitable for the amplification of large quantities of RNA. Nucleic acid is extracted from whole blood. The amplification process involves the coordinated isothermal activities of three different enzymes (74, 205). The test has the ability to synthesize large numbers of a specific single-stranded viral RNA sequence from a double-stranded DNA molecule generated from the original RNA target; RNA is specifically expressed during active viral replication. The diagnostic value of monitoring CMV late pp67 mRNA expression by NASBA (NucliSens CMV pp67; Organon Teknika) has been evaluated in patients who have undergone kidney transplantation (38). These data suggest that NASBA may be more sensitive than the antigenemia assay for the detection of CMV infection. This assay offers some advantages over other tests. Whole-blood samples used for NASBA can be stored prior to testing, and the test can be completed in a day. The method is standardized; however, the extraction procedure is cumbersome. Additional clinical testing will better elucidate the role of CMV pp67 mRNA detection by NASBA in CMV diagnosis of solid-organ transplants.
Until recently, the primary application for diagnostic tests for CMV infection in transplant recipients has been either to confirm or to exclude CMV as the cause of clinical symptoms. The availability of antiviral drugs has introduced new applications for virologic monitoring. The increasing use of surveillance and preemptive therapy for CMV indicates the need for sensitive tests that become positive well before the onset of symptoms. While the shell vial culture method has previously been a widely used test, the antigenemia assay offers more rapid results, enhanced sensitivity, and earlier diagnosis of CMV infection. The development of molecular techniques has also provided a sensitive tool for early CMV detection. The ability to quantify viral load exists with these last two methods. Comparative analysis of CMV diagnostic assays shows that the antigenemia and PCR assays both turn positive before the onset of clinical symptoms; in general, PCR tends to turn positive earlier than does the antigenemia assay. The shell vial assay is markedly less sensitive for the early detection of CMV infection (458).
Novel applications of preexisting laboratory tests are being explored as potential adjunctive tools in CMV diagnosis. For instance, measurement of the CD8+ CD38+ T-cell subset is proposed to be a useful immunologic parameter in the follow-up of patients following organ transplantation (32). In a study of kidney transplant individuals, CD38+ antigen expression on cytotoxic CD8+ T cells was shown to drastically increase during the active phase of CMV disease, appearing before or at the time of the initial manifestations of infection (32).
Laboratory tests are increasingly being used to direct the duration of antiviral therapy (211, 476). It is apparent that further studies evaluating qualitative and quantitative PCRs as well as antigenemia techniques are needed to determine their role in the therapeutic monitoring of CMV infection in organ transplant recipients.
Viral Susceptibility Testing
A potential risk associated with the use of antiviral chemotherapy is the emergence of resistant viruses. Additionally, the increasing usage of drug therapy for both the prevention and treatment of CMV infection has accentuated the need for rapid methods of antiviral sensitivity testing and for identification of the emergence of resistant virus strains.
The two most commonly used methods to detect and measure antiviral drug susceptibility are the plaque reduction assay and the DNA hybridization assay. Both assays detect phenotypic resistance to the drug being tested. Each requires CMV isolation and passage in cell culture, which requires 4 to 6 weeks; only then does chemosensitivity testing begin (150, 363, 443). The plaque reduction assay measures viral efficiency in forming plaques in the presence of drug (443). Human fibroblast cell monolayers are infected with viral isolates containing a specified titer of PFU. Cultures are incubated with medium containing serial concentrations of an antiviral agent (150, 153, 154, 262). The results are obtained by counting the number of plaques formed after 96 h of incubation and are expressed as the drug concentration producing 50% inhibition of the virus. Alternatively, the presence of a resistant CMV strain may be detected by a <50% reduction in the plaque count detected by using an immunoperoxidase staining technique (155). The DNA hybridization assay measures the reduction of viral DNA synthesis by using a CMV DNA probe in the presence of a drug (84). Viral DNA is quantified following incubation on monolayers infected with a known concentration of the CMV isolate in the presence of the drug. The ability to swiftly detect resistant CMV strains directly in clinical specimens is desirable; such rapid assays include modifications of currently used tests.
The limitation of these assays is that they can be performed only on specimens from patients with high levels of viremia. Also, because of the complexities and variables involved in antiviral susceptibility testing of CMV isolates, the results of these assays should be interpreted with caution. Efforts to establish cutoff values defining drug susceptible and resistant CMV isolates are being refined. The capability of a flow cytometric assay based on the determination of the effect of a drug on viral antigen synthesis to measure susceptibilities of CMV to ganciclovir is being studied (294, 295). The test has the potential advantages of a shorter processing time and is amenable to automation.
Mutations in two specific CMV genes, the phosphotransferase gene UL97 and the DNA polymerase gene UL54, confer ganciclovir resistance of CMV (24, 42, 114, 131, 426). The protein kinase encoded by the CMV UL97 gene plays a crucial role in the initial phosphorylation of ganciclovir to its active form. Alterations in the CMV UL54 gene have also been responsible for conferring foscarnet resistance (23). Mutations in the polymerase gene occurring in addition to mutations in the phosphotransferase gene may increase the level of resistance to ganciclovir or confer cross-resistance to other anti-CMV drugs (66, 238, 426, 454, 459). By PCR detection of specific codon mutations, using selective restriction enzyme analysis or product sequencing, rapid screening for resistant strains is possible while avoiding viral propagation as needed for conventional susceptibility testing (10). Such an approach could be potentially useful in the clinical setting. The limitations of molecular methods for the rapid assessment of antiviral resistance include the presence of small numbers of leukocytes infected with CMV mutant strains, the presence of novel resistance-associated mutations, and the existence of multiple viral genotypes in the same person. Finally, measurement of the viral load may be used as a surrogate marker of drug resistance (40).
Overall, with ongoing developments in laboratory tests for CMV diagnosis, it may eventually be possible to choose between a wide range of clinical tests for different clinical situations, standardized according to clinical criteria.
TREATMENT
In the last decade, considerable progress has been made in the use of antiviral chemotherapy to prevent and treat CMV disease following organ transplantation. A range of regimens for CMV disease management have evolved, encompassing the identification of risk factors, the early detection of CMV infection followed by the initiation of specific antiviral therapy, prophylactic antiviral strategies, reduction in immunosuppression, prophylaxis and treatment of superinfection, selective use of intravenous immunoglobulin, and surveillance viral detection to monitor the response to therapy (248, 450, 485). Surveillance viral monitoring may include serial CMV cultures (blood, urine) and biopsy with viral culture of tissue specimens whenever clinically indicated. There is data to indicate that routine cultures of urine and blood performed during the first 2 months after transplantation are useful in predicting CMV disease in liver transplant recipients (129).
Prior to the availability of ganciclovir, treatment modalities necessitated a reduction in immunosuppressive therapy, which in turn caused an increased incidence of graft rejection. Currently, the use of ganciclovir for CMV disease allows baseline immunosuppression to be maintained and allograft rejection to be treated with high-dose steroids and even with potent antilymphocyte antibody (494).
The optimal duration of antiviral therapy in an individual patient is unknown but is commonly determined by the clinical response and elimination of CMV from surveillance viral cultures. On occasion, repeat evaluation of tissue specimens is necessary. In studies of bone marrow transplant recipients, a negative result of a PCR assay in either blood or urine at the conclusion of antiviral therapy seemed to be a better marker for effective antiviral treatment than did clinical improvement or negative blood cultures (112). In solid-organ transplant recipients, a similar approach might indicate the appropriate time when ganciclovir therapy may be safely discontinued (470, 480).
Quantitative antigenemia and CD8+ T lymphocytes in peripheral blood are other potential markers indicating adequacy of antiviral therapy (478). Antigenemia assays correlate well with the clinical course of illness in kidney transplant recipients treated for CMV disease (266, 458). The levels of antigenemia decrease within 3 to 4 days after initiation of effective antiviral therapy (477). It should be noted, however, that early initiation of treatment in patients with primary CMV infection may also be followed by a significant rise in antigenemia during the first week of therapy and delayed antigenemia clearance (156). Thus, shifting to an alternative antiviral drug based solely on early increasing antigenemia levels may not be justified.
Analysis and virologic follow-up of antiviral therapy show that qualitative monitoring of leukocyte CMV DNA is a sensitive virologic parameter to evaluate treatment efficacy (151). Significant decreases in viral loads are observed during ganciclovir administration (213, 314, 470). The discontinuation of treatment when CMV PCR is positive in bronchoalveolar lavage specimens of lung transplant recipients (448) and in blood specimens of kidney/kidney-pancreas transplant recipients (213) has been associated with recurrence of CMV infection. Disappearance of the PCR signal in leukocytes might represent a primary end point to be achieved during antiviral therapy to delay or prevent a relapse of CMV disease (151). On the other hand, a positive PCR assay might persist for months following organ transplantation despite effective antiviral therapy. In this regard, the quantitation of CMV by PCR may be of value for monitoring the efficacy of chemotherapy; the subject has generated research interest. Prospective studies will determine the utility of measuring the circulating CMV DNA load (both at the beginning of and after treatment) for predicting clinical outcome in immunocompromised hosts. Overall, the value of PCR in this setting remains to be determined.
Quantitative PCR appears to be a promising method for comparing the antiviral effects of different drugs and determining the length of therapy (44). CMV DNA titers that remain essentially unchanged after initiation of therapy suggest inadequate dosing or resistance to the antiviral drug in use; increases in titer after therapy may herald a relapse of CMV disease (347). Quantitative assays of viral load and the clinical response to treatment will probably play an increasing role in guiding CMV treatment. Assays that are better standardized and have defined cutoff levels are desired. Nonetheless, antigenemia assays and PCR-based tests are becoming routine procedures in the surveillance as well as therapeutic monitoring of organ transplant recipients with CMV infection.
Before the introduction of ganciclovir, therapeutic options for symptomatic or invasive CMV disease in the immunocompromised transplant host were limited. Currently available antiviral agents with proven efficacy against CMV include ganciclovir, foscarnet, and cidofovir; these agents inhibit the synthesis of metabolically active virus and are not active against non-replicating or latent virus.
Ganciclovir
Ganciclovir, 9-[2-hydroxy-1-(hydroxymethyl)-ethoxymethyl]guanine, has excellent activity against members of the herpes family of viruses (7, 80). It is a prodrug which is phosphorylated to ganciclovir 5′-monophosphate by a protein encoded by the UL97 open reading frame of human CMV and then to the di- and triphosphate forms by host cellular kinases (263, 455). The active drug inhibits viral replication by competing with deoxyguanosine triphosphate as a substrate for the enzyme DNA polymerase (224, 324). The incorporation of ganciclovir triphosphate into the growing chain of viral DNA slows extension, thus inhibiting viral replication.
Intravenous ganciclovir has been successfully used in uncontrolled, nonrandomized therapeutic trials to treat solid-organ transplant recipients with CMV disease (52, 59, 77, 83, 88, 90, 106, 116, 185, 186, 192, 207, 212, 217, 226, 254, 275, 281, 296, 322, 324, 325, 339, 386, 397, 428, 430, 446, 451, 490, 496). To date, intravenous ganciclovir remains the drug of choice for the treatment of CMV disease. One caveat is that treatment of CMV may not reduce disease severity if the pathogenesis of the disease is immune system mediated (184, 370). The usual dose of intravenous ganciclovir is 5 mg/kg every 12 h. Because of its predominant renal excretion, the dosage should be decreased in patients with renal impairment. The concentrations of ganciclovir in blood are decreased by 50% after 4 h of hemodialysis; thus, ganciclovir must be readministered shortly after dialysis (457). CMV disease is typically treated with 2 weeks of intravenous ganciclovir, although it has been suggested that a longer duration of therapy may be required for gastrointestinal CMV disease (419). Retinitis responds well to antiviral therapy, suggesting that active viral replication and direct viral CPE are the major factors responsible for CMV disease at this location (328). In contrast, CMV interstitial pneumonitis responds poorly to antiviral therapy alone, even though ganciclovir dramatically reduces viral replication in the lungs (418), suggesting that mechanisms other than viral replication and direct CPE contribute to CMV-related pathology (175). Unlike treatment of CMV disease in patients with AIDS, long-term maintenance is seldom required in recipients of organ allografts.
Recurrent CMV disease appears to respond to ganciclovir as well as does initial CMV disease (402). In the event of recurrent disease despite therapy, determination of the susceptibility of the isolated CMV strain to currently available antiviral drugs may be considered; the occurrence of resistant strains has been documented among organ transplant recipients (10, 271, 383).
Oral ganciclovir has recently been approved for use in solid-organ transplant recipients for the prevention of CMV disease. The absorption of ganciclovir following oral administration is poor; still, levels within the 50% inhibitory concentration for most CMV strains could be achieved (349). Its utility in the treatment of CMV infection and disease following solid-organ transplantation has yet to be determined. Oral ganciclovir may be useful for maintenance therapy in patients treated with intravenous ganciclovir who are identified to be at increased risk for recurrent CMV (320); this also needs to be studied further.
Adverse effects of ganciclovir when administered to solid-organ transplant patients are less frequent than in bone marrow transplant recipients and AIDS patients. They include leukopenia, thrombocytopenia, anemia, eosinophilia, bone marrow hypoplasia, hemolysis, nausea, infusion site reactions, diarrhea, renal toxicity, seizures, mental status changes, fever, rash, and hepatocellular dysfunction (52, 80, 85, 131, 403, 416). The occurrence of hypercalcemia has also complicated ganciclovir therapy (147). Hematologic parameters and renal function should be monitored in patients receiving ganciclovir. Renal toxicity may occur when the drug is used in conjunction with other nephrotoxic agents such as amphotericin B, azathioprine, and cyclosporin A and when used in children. The long-term safety of ganciclovir in both adult and pediatric transplant recipients has yet to be established (86).
Valganciclovir
Valganciclovir is a valine ester of the active drug ganciclovir that is formulated as an oral agent. It has the distinct advantage over ganciclovir of having markedly increased oral bioavailability, attaining levels in serum that approach those of intravenously administered ganciclovir. Clinical studies on the pharmacokinetics of this drug in liver transplant recipients are under way. The accessibility of this agent could potentially simplify the treatment of CMV infection in immunosuppressed hosts.
Foscarnet
There is far less experience with the use of foscarnet, trisodium phosphonoformate hexahydrate, for treatment of CMV disease in organ transplantation (30, 237, 267, 377). Until more data are available, foscarnet should be reserved for patients who are intolerant of ganciclovir or who have failed ganciclovir therapy. Foscarnet is an inorganic pyrophosphate analog that does not need to be phosphorylated into an active form by viral or host cell enzymes. It selectively inhibits viral DNA polymerase and is virustatic. Its main side effects are nephrotoxicity, anemia, electrolyte imbalance, nausea, vomiting, and seizures. Foscarnet is administered intravenously at a dose of 60 mg/kg three times daily, with dose adjustments in patients with renal failure. Combination therapy with ganciclovir and foscarnet exhibits synergistic antiviral activity in vitro (279). Studies with bone marrow transplant recipients suggest that the combination of ganciclovir and foscarnet may prove efficacious in the treatment of CMV infection (15, 16). These findings merit further investigation. Foscarnet should be useful to treat CMV disease caused by ganciclovir-resistant CMV strains.
Cidofovir
Cidofovir, (S)-1-[3-hydroxy-2-(phosphonylmethoxy)propyl]cytosine, a nucleotide analog of dCMP, is a novel agent that has been introduced to the antiviral pharmacopoeia. Unlike ganciclovir, cidofovir does not require viral enzymes for activation (230). In addition to being active against CMV, cidofovir is active against various other viruses including adenovirus, herpes simplex virus, EBV, hepatitis B virus, polyomavirus, and human papillomavirus. It is used almost exclusively for the treatment of CMV infection in patients with AIDS. Current intravenous dose recommendations are 5 mg/kg once weekly for two doses and then 5 mg/kg once every other week; dosage adjustments are made in patients with impaired renal function. A major drawback of cidofovir is its associated nephrotoxicity; this can be partially averted by the concurrent administration of probenecid. Neutropenia and constitutional reactions to probenecid may be encountered. Cidofovir is, however, an attractive alternative to the other compounds because its long half-life allows infrequent intravenous dosing intervals, thus avoiding the need for long-term intravenous access. The applicability of cidofovir use in solid-organ transplants remains investigational; it may have a niche in the treatment of certain strains of virus resistant to other currently available therapies. A prodrug of cidofovir is being developed; it appears to be less nephrotoxic than the parent compound.
Acyclovir
Although high concentrations of acyclovir, 9-[(2-hydroxyethoxy)methyl]-9H-guanine, inhibit CMV in vitro, clinical trials have demonstrated no benefit from acyclovir in the treatment of CMV infection (486).
Immunoglobulin Therapy
CMV hyperimmune globulin has been found by some investigators to be ineffective in the treatment of CMV disease in solid-organ transplant recipients (53); others allude to a possible benefit to be gained from passive immunotherapy (256, 367). The role of combining CMV-specific immune globulin with ganciclovir for invasive CMV disease is controversial (390). The cost of immune globulin administration also should be considered. Nevertheless, combination therapy may be warranted in specific subsets of patients, e.g., those with severe CMV pneumonia.
Antiviral Resistance
Clinical CMV isolates resistant to antiviral agents have been identified in solid-organ transplant recipients. Certain mutations in the viral UL97 and UL54 genes confer ganciclovir resistance to CMV (24, 42, 114, 131, 426). Codon changes in the DNA polymerase gene UL54 are responsible for foscarnet resistance (23). Cross-resistance to other antiviral agents has been demonstrated in certain isolates. High-level ganciclovir-resistant isolates are often cross-resistant to cidofovir and may have reduced sensitivity to foscarnet (66, 238, 426, 454, 459). So far, in vitro ganciclovir resistance has not been common in solid-organ transplant recipients. Nevertheless, reports that ganciclovir resistance can be a clinically significant problem in this population are increasing (10, 22, 384). It is possible that the incidence of resistance will increase further with changes in the ways that primary prophylaxis and treatment for CMV are administered. This indicates a need for increased vigilance for antiviral resistance, especially as new oral antiviral preparations are used for prolonged periods, either for prophylaxis or as treatment.
New Anti-CMV Drugs
Novel antiviral compounds such as benzimidazole (508), adefovir (504), and lobucavir (461) are currently under investigation and might further improve the management of CMV infection. Moreover, antisense oligonucleotides complementary to RNA transcripts of IE genes provide a novel mechanism of inhibition for viral replication (11). Such agents, including fomivirsen (285), are being studied. Effective and less toxic CMV inhibitors that can stop viral replication and prevent CMV reactivation are needed. As more patients receive organ transplants, the search to identify and develop such drugs will intensify.
PREVENTION
The ability of CMV to predispose solid-organ transplant recipients to superinfection with other organisms and to decreased graft and patient survival, coupled with its properties as an immunomodulating agent, has hastened the pursuit to find effective prophylactic strategies to prevent infection (176). To date, a number of measures for preventing CMV infection have been evaluated: (i) selection of allografts from CMV-seronegative donors for CMV-seronegative recipients; (ii) use of CMV-seronegative, filtered, or leukocyte-poor blood products; (iii) active immunization with a vaccine; (iv) passive immunization with immune globulin; (v) prophylaxis with antiviral agents; (vi) preemptive therapy; and (vii) adoptive immunotherapy.
Avoidance of Infection
Since primary CMV infections are more likely to produce morbidity than are reactivation infections and since the donor organ is a demonstrated source of virus, matching of donor and recipient by serologic status is an ideal way of decreasing the overall frequency of illness due to CMV. Knowledge of the CMV serostatus of the donor and recipient pretransplantation identifies individuals who might develop CMV disease following organ transplantation. Protective matching of seronegative donors with seronegative recipients decreases both the incidence and severity of CMV disease. However, because of the scarcity of donor organs, constraints on organ transplantability, and the ever-increasing waiting time for organ transplantation, allocation of allografts on the basis of CMV serologic compatibility has not been widely implemented (400).
The risk of transfusion-acquired CMV infection is proportional to the volume of blood products transfused. One of the simplest and most direct ways to reduce the risk of CMV infection is to ensure the use of CMV-seronegative blood products in CMV-seronegative transplant recipients. Viral transmission by blood products is decreased with the use of CMV antibody-negative blood products or high-efficiency leukocyte filters to remove viable leukocytes that harbor CMV (366, 404).
Active Immunization
Administration of a CMV vaccine to seronegative transplant candidates is theoretically a simple and effective way of reducing the risk of CMV infection and disease. Vaccination of renal transplant recipients with live attenuated vaccines prepared from the Towne and Toledo strains of CMV has been evaluated (355). The Towne live-virus vaccine was shown to reduce disease severity among those who were CMV seronegative at the time of vaccination and who subsequently received a kidney from a seropositive donor (354, 355). Although the vaccine did not completely prevent CMV disease, it appeared to reduce the severity of primary infection. Compared to normal volunteers, the immunogenic response to vaccination was muted by immune suppression. The failure of vaccinated seronegative recipients to seroconvert occurred at a relatively high rate (24%) (280, 353). The Towne vaccine fell short of its expected efficacy by its inability to prevent superinfection with other strains of human CMV (356). The use of an effective subunit vaccine may be a more promising alternative. Work on the development of such a subunit vaccine has focused on the viral envelope glycoprotein, designated gB (356). It seems likely that as more is learned about the immune system mechanisms involved in the control of the virus, it will become possible to induce immunologic protection with inactivated, recombinant DNA-produced vaccines (91, 214). Although complete protection against CMV may not be achieved by vaccination, partial immunity may obviate the development of serious manifestations of CMV infection and disease. Moreover, a suboptimal vaccine may suffice when used in combination with other therapies, such as antiviral drugs and/or immunoglobulin administration.
Immunoglobulin Prophylaxis
Human immunoglobulin preparations have been studied as prophylactic agents against CMV infection after organ transplantation (21, 75, 130, 174, 222, 395, 431–433) (Table 4). Standard immunoglobulin preparations contain antibodies from blood and plasma of donors with natural antibodies against CMV, and they vary in their content of neutralizing antibody titers against CMV. By contrast, when blood from donors with high antibody titers against CMV is used, CMV hyperimmune globulin has five to eight times the neutralizing antibody titer of unselected immunoglobulin (95). Passive immune prophylaxis may reduce the severity of CMV disease in some solid-organ transplant settings.
TABLE 4.
Summary of randomized passive immunoprophylaxis trials in solid-organ transplant recipientsd
| Type of transplant | Reference | Type of study | No. of patients studied (no. of D+/R− patients)a | Prophylactic regimen |
|---|---|---|---|---|
| Kidney | 174 | Primary and secondary prophylaxis, non-placebo controlled | 24 | Hyperimmune serum 0.1 g/kg days 0, 1, and every 3 wk for 6 mo |
| vs. | ||||
| 24 | no treatment | |||
| 130 | Primary and secondary prophylaxis | 42 | Hyperimmune globulin (Cytotect; Biotest-Pharma, Dreieich, Germany) 10 g on days 0, 18, 38, 58, and 78 | |
| vs. | ||||
| 34 | immunoglobulin (Intraglobin; Biotest-Pharma, Dreieich, Germany) 10 g (same schedule) | |||
| 433 | Primary prophylaxis, non-placebo controlled | 24 (24) | CMV immune globulin (Mass. Public Health Biological Laboratories) 150 mg/kg for 72 h; 100 mg/kg at wk 2 and 4; 50 mg/kg at wk 6, 8, 12, 16 | |
| vs. | ||||
| 35 (35) | no treatment | |||
| 75 | Primary prophylaxis, non-placebo controlled | 27 (27) | Unselected immunoglobulin 500 mg/kg within 48 h and at wk 1; 250 mg/kg per wk for 5 wk | |
| vs. | ||||
| 24 (24) | ganciclovir 2.5 mg/kg/day i.v. for 21 days | |||
| 222 | Primary and secondary prophylaxis, non-placebo controlled | 15 (1) | Polyvalent immunoglobulin (GamImune N; Bayer Corp., West Haven, Conn.) 500 mg/kg within 48 h posttransplant, then weekly for 23 wk | |
| vs. | ||||
| 13 (1) | no treatment | |||
| Liver | 71 | Primary and secondary prophylaxis, prospective, placebo controlled | 25 (0) | Immunoglobulin (Sandoglobulin; Novartis Pharmaceuticals, East Hanover, N.J.) 500 mg/kg on days 1, 7, 14, 21, 28, 42, 56, 70, and 84 |
| vs. | ||||
| 25 (4) | albumin at a similar concentration on same days | |||
| 395 | Primary prophylaxis of recipient, controlled, prospective | 22 (15) | CMV immunoglobulin 250 mg/kg on day 0; then 125 mg/kg every 10 days for 3 mo | |
| vs. | ||||
| 12 (7) | no prophylaxis | |||
| 432 | Primary and secondary prophylaxis, double-blinded | 69 (19) | CMV immunoglobulin (Mass. Public Health Biological Laboratories) 150 mg/kg within 72 h of transplant and at wk 2, 4, 6, and 8; 100 mg/kg at wk 12 and 16 | |
| vs. | ||||
| 72 (19) | placebo (1% serum albumin) | |||
| 431 | Primary prophylaxis (R−); compared with seronegative receiving placebo in above random-assignment trial | 21 (9) | CMV immunoglobulin (Mass. Public Health Biological Laboratories) 150 mg/kg within 72 h of transplant and at wk 2, 4, 6, and 8; 100 mg/kg at wk 12 and 16 | |
| 44 (19) | placebo |
| Outcome(s)b | CMV diseaseb | Mortalityc |
|---|---|---|
| Beneficial effect on CMV illness but not infection in patients on cyclosporine and not in those on azathioprine/ATG | 0% vs. 17% (cyclosporin); 58% vs. 37% (azathioprine/ATG) | Not reported |
| No change in CMV infection; decreased severity of symptoms of primary infection in the hyperimmune globulin group | Not reported | 0% vs. 0% |
| Reduced CMV-associated syndromes, fungal and parasitic superinfections | 21% vs. 60% | 4% vs. 14% |
| Both regimens reduced CMV syndromes and invasive CMV infection (compared to historical controls); ganciclovir was much cheaper | 22% vs. 21% | 0% vs. 0% |
| No benefit | 53% vs. 77% | Not reported |
| No benefit | 32% vs. 20% | None reported |
| Decreased rate of CMV disease in D+/R− | 27% vs. 86% (D+/R−), 14% vs. 0% (D−/R−) | Not reported |
| Reduction in severe CMV disease; no effect in D+/R− group | 19% vs. 31% | 17% vs. 25% |
| Reduction in severe CMV disease in D+/R− group | 14% vs. 32% | Not reported |
If known, the number of CMV-negative patients given donor-positive organs (D+/R−) is shown in parentheses.
ATG, antithymocyte globulin; i.v., intravenous; p.o., peroral.
Among patients given the drug, the percentage refers to the first versus the second regimen.
Studies of kidney transplant recipients receiving hyperimmune CMV immunoglobulin preparations have shown significant reductions in symptomatic illness due to CMV (39, 433) and in the incidence of opportunistic infections in globulin recipients (433). Although the preventative efficacy is attenuated when antilymphocyte antibodies are administered, CMV hyperimmune globulin prevents primary disease (429) and may completely prevent CMV-related deaths (300). In randomized controlled trials, CMV immunoglobulin preparations have been effective in preventing CMV disease in liver transplant recipients as well (395, 431, 432). In addition, disease severity was reduced in all those who received passive immunotherapy, even those treated with antilymphocyte therapy (433). Nevertheless, the protective effect of immunoglobulin in CMV-seronegative liver transplant recipients of organs from CMV-seropositive donors appears to be borderline (473). Studies of CMV prophylaxis with CMV immunoglobulin in other solid organ transplant recipients suggest that globulin prophylaxis may be effective (395, 407). A meta-analysis of studies of cardiac transplants indicates that CMV immunoglobulin reduces the rate of disease without affecting the rate of asymptomatic infection (473). A randomized trial with heart, lung, and kidney transplant recipients showed no difference when acyclovir was used with or without unselected immunoglobulin (21). In a small group of lung transplant patients, the use of CMV immunoglobulin in high-risk individuals had a positive clinical impact by reducing CMV-associated morbidity (223). Finally, a meta-analysis of CMV immunoglobulin studies of transplant patients indicated the effectiveness of CMV immunoglobulin in the prevention and treatment of CMV infection among patients undergoing organ transplants (498). Most of these studies support the concept that prophylactic immunoglobulin therapy can attenuate the severity of CMV disease after transplantation. In part, the reason for the apparent limited efficacy of immunoglobulin prophylaxis may be secondary to insufficient antibody titers (14). Additionally, CMV immunoglobulin, beyond its proven efficacy in decreasing the incidence of severe CMV-associated disease, reduces the frequency of invasive fungal disease (432) and is associated with increased survival when used prophylactically in liver transplant recipients (128).
The incidence of adverse effects related to immunoglobulin administration is usually less than 5%, and the manifestations are typically mild and self-limited. Headaches, back or abdominal pain, nausea, vomiting, shortness of breath, fever, chills, and myalgias are the most commonly reported. Anaphylactic reactions have been described in patients with immunoglobulin A deficiency given preparations that contain immunoglobulin A. Contamination of some immunoglobulin preparations with hepatitis C virus has occurred (37). All currently manufactured preparations require both screening of plasma pools for anti-hepatitis C virus antibody and the removal of hepatitis C virus-positive products, as well as additional viral inactivation steps. Whether there is the potential for transmission of other yet unidentified pathogens is unknown.
While immunoglobulin therapy appears to have low toxicity, the cost of prophylaxis (typically several thousand dollars per patient) is high and protection against CMV is only partial. Additionally, this therapy is logistically difficult to administer. A formal comparison between antiviral and immunoglobulin prophylaxis has suggested that immunoglobulin and ganciclovir both reduce symptomatic CMV infection but that the latter is a much cheaper option (75). Together, the results of randomized trials with solid-organ transplant indicate that (i) immunoglobulin preparations confer some degree of efficacy in preventing CMV disease, this being more consistent with CMV hyperimmune globulin preparations; (ii) these benefits are attenuated when antilymphocyte therapy is used; (iii) renal transplant recipients are more likely to benefit from CMV hyperimmune globulin than are nonrenal (e.g., liver) transplant recipients, especially within the high-risk (CMV donor positive-recipient negative) group; and (iv) the advantages include the relatively infrequent administration (weekly intervals) and the lack of need for continuous intravenous access. The main disadvantage of immunoglobulin therapy is cost. Pharmacoeconomic studies comparing the administration of effective antiviral agents and CMV hyperimmune globulin will have to be performed to address cost and benefit issues (75). In liver, lung, and perhaps heart and pancreas transplants, high-risk individuals may require enhanced prophylaxis; this may be achieved by combining CMV hyperimmune globulin with antiviral agents. Thus, the role of prophylactic CMV immunoglobulin or gamma globulin preparations for the prevention of CMV disease remains to be better defined.
Specific Antiviral Prophylaxis
Universal prophylaxis against CMV implies that all transplant patients receive antiviral therapy. The ideal CMV prophylactic regimen should possess a number of features. The foremost criteria for such an agent is that it be effective in an oral formulation, if frequent administration is required, or in an intravenous formulation that can be given at infrequent intervals (e.g., weekly), and that it be efficacious without the need for virologic monitoring. It should be safe, requiring minimal laboratory evaluations and drug monitoring, and having few adverse interactions with other medications used in organ transplantation. Lastly, the drug should possess pan-virustatic/cidal activity against CMV as well as other herpes viruses, with minimal potential for inducing antiviral resistance. The present-day knowledge of CMV pathogenesis as well as CMV prophylaxis leaves much to be learned; significant advances are necessary to achieve the goals set forth for the effective prevention of CMV disease.
Current prophylactic approaches vary widely among different transplant programs (5, 8, 18, 26, 72, 104, 105, 143, 145, 172, 232, 236, 273, 284, 299, 319, 382, 396, 423, 497) (Table 5). Reasons for the discrepancies reflect the absence of large, multicenter, randomized trials evaluating the efficacy of countless preventive strategies. In addition, the results of small single-center studies are frequently difficult to reproduce, since differences in end points, definitions, viral surveillance, type of immunosuppressive regimen, patient population, and frequency of antilymphocyte antibody treatment are common. More importantly, inherent differences among the types of solid-organ transplants must be considered.
TABLE 5.
Summary of randomized antiviral drug prophylaxis trials in solid-organ transplant recipientsd
| Drug and type of transplant | Reference | Type of study | Number of patients studied (# of D+/R− patients)a | Prophylactic regimenb | Outcome(s) | CMV diseasec | Mortalityc |
|---|---|---|---|---|---|---|---|
| Acyclovir | |||||||
| Kidney | 26 | Primary and secondary prophylaxis, prospective, double-blind, placebo controlled | 53 (6) | Acyclovir 800 mg p.o. 4 times a day for 12 wk beginning before transplant | Decreased CMV infection and disease, especially in the D+/R− subgroup | 8% vs. 29% | 4% vs. 6% |
| vs. | |||||||
| 51 (7) | placebo | ||||||
| 236 | Primary prophylaxis, prospective | 22 (22) | Acyclovir 800–3,200 mg/day p.o. for 12 wk | No difference | 40% vs. 40% | Not reported | |
| vs. | |||||||
| 10 (10) | no prophylaxis | ||||||
| 136 | Primary and secondary prophylaxis (excluding D−/R−) | 39 (13) | Acyclovir 800 mg p.o. 4 times a day for 12 wk plus CMV immunoglobulin every 2 wk for 16 wk | Decreased CMV infection with oral acyclovir only for donor-negative group; decreased CMV infection with oral ganciclovir in all | 38% vs. 2.5% | 5% vs. 2.5% | |
| vs. | |||||||
| 40 (14) | ganciclovir 1 g p.o. 3 times a day for 12 wk plus CMV immune globulin every 2 wk for 16 wk | ||||||
| Kidney, kidney-pancreas, kidney-islet cell, pancreas, liver | 105 | Primary and secondary prophylaxis, prospective, non-placebo controlled | 133 (32) | Acyclovir 800 mg p.o. or 400 mg i.v. 4 times a day for 12 wk or for 6 wk after any antirejection therapy | Decreased CMV disease in the acyclovir group | 21% vs. 32% | 10% vs. 14% |
| vs. | |||||||
| 133 (31) | ganciclovir 5 mg/kg i.v. twice a day for 7 days plus immunoglobulin (Sandoglobulin; Novartis Pharmaceuticals Corp., East Hanover, N.J.) or Minnesota CMV immunoglobulin 100 mg/kg on i.v. days 1, 4, and 7 | ||||||
| Liver | 396 | Secondary prophylaxis, controlled, prospective | 60 (0) | Acyclovir 500 mg/m2 i.v. 3 times a day for 10 days, then acyclovir 3,200 mg/day p.o. through 3 mo | Decreased CMV infection and disease | 7% vs. 23% | “No effect on survival” |
| vs. | |||||||
| 60 (0) | no prophylaxis | ||||||
| 423 | Primary prophylaxis and preemptive therapy, controlled, prospective | 24 (2) | Acyclovir 800 mg p.o. 4 times a day for 24 wk | Oral acyclovir ineffective | 29% vs. 4% | 13% vs. 13% | |
| vs. | |||||||
| 23 (2) | ganciclovir 5 mg/kg i.v. for 7 days when CMV culture positive | ||||||
| 145 | Secondary prophylaxis (R+), prospective | 37 (0) | Acyclovir 400 mg p.o. 5 times a day for 16 wk | Decreased CMV disease | 5% vs. 27% | 19% vs. 22% | |
| vs. | |||||||
| 36 (0) | no prophylaxis | ||||||
| emsHeart, lung, and kidney | 21 | Primary prophylaxis, prospective, stratified (type of transplant and prophylactic immunosuppression) | 11 (11) | Acyclovir 800 mg p.o. 4 times a day for 12 wk | Acyclovir with or without immunoglobulin did not prevent primary CMV infection or disease | 64% vs. 80% | 9% vs. 0% |
| vs. | |||||||
| 10 (10) | acyclovir 800 mg p.o. 4 times a day for 12 wk with immune globulin 300 mg/kg i.v. every 2 wk for 6 doses | ||||||
| Ganciclovir | |||||||
| Kidney (cadaver) | 382 | Primary prophylaxis | 17 (17) | Ganciclovir 5 mg/kg i.v. twice a day for 14 days (days 14–28) | Delayed onset of CMV infection; reduced severity of CMV disease; no change in incidence of CMV infection or disease | 47% vs. 73% | 0% vs. 0% |
| vs. | |||||||
| 17 (17) | No ganciclovir | ||||||
| 8 | Primary prophylaxis, prospective, open-label, controlled | 21 (4) | Ganciclovir 750 mg p.o. twice a day for 12 wk | Decreased CMV infection | 5% vs. 27% | 0% vs. 5% | |
| vs. | |||||||
| 22 (4) | no ganciclovir | ||||||
| Heart | 273 | Primary and secondary prophylaxis, stratified (R+ vs. D+/R−), prospective, double-blind | 28 (9) | Ganciclovir 5 mg/kg i.v. 3 times a wk for 6 wk; then for another 2 wk for each treated rejection episode through 12 wk | Reduced CMV disease in D+/R− patients, reduced CMV disease morbidity in the R+ subgroup | 11% vs. 71% | None |
| vs. | |||||||
| 28 (7) | placebo | ||||||
| 299 | Primary and secondary prophylaxis, stratified (R+ vs. D+/R−), prospective, double-blind, placebo controlled | 76 (19) | Ganciclovir 5 mg/kg i.v. twice a day for 14 days, then 6 mg/kg 5 times a wk for 14 days | Reduced incidence of CMV illness in the R+ subgroup, delayed incidence of CMV shedding | 16% vs. 43% | 4% vs. 1% | |
| vs. | |||||||
| 73 (16) | placebo | ||||||
| 5 | Secondary prophylaxis, prospective, non-placebo controlled | 16 (0) | Ganciclovir 5 mg/kg i.v. twice a day for 14 days | Higher incidence of CMV disease in the immunoglobulin group | 6% vs. 40% | 6% vs. 13% | |
| vs. | |||||||
| 15 (0) | CMV immunoglobulin (Cytogam; Medimmune, Inc., Gaithersburg, Md.) 100 mg/kg within 24 h of transplant and at wk 2, 4, 6, 8, 10 | ||||||
| Lung | 104 | Primary and secondary prophylaxis (excluding D−/R−) | 13 (3) | Ganciclovir 5 mg/kg i.v. 4 times a day for 2 wk, starting day 7, then 5 mg/kg/day for 1 wk, then 5 mg/kg/day 5 days a wk till day 90 | Decreased CMV infection and disease, increased median infection-free duration | 0% vs. 25% | 15% vs. 25% |
| vs. | |||||||
| 12 (3) | ganciclovir 5 mg/kg i.v. 4 times a day for 2 weeks, starting day 7, then 5 mg/kg/day for 1 wk, then acyclovir 800 mg p.o. 4 times a day til day 90 | ||||||
| Lung, heart-lung | 195 | Primary and secondary prophylaxis | 35 (5) | Ganciclovir 5 mg/kg i.v. twice a day on days 8–21, then 5 mg/kg i.v. till day 90 | no difference in CMV infection nor disease | 51% vs. 30% | 14% vs. 35% |
| vs. | |||||||
| 37 (5) | ganciclovir 5 mg/kg i.v. twice a day on days 8–21, then 5 mg/kg/day i.v. 3 times a wk till day 90 | ||||||
| Liver | 232 | Primary prophylaxis, prospective, placebo controlled | 29 | Ganciclovir 5 mg/kg/day for 30 days with i.v. immunoglobulin 1 g/kg once, then 500 mg/kg/wk at wk 1–8, then 2×/week at wk 10–16 | No difference in CMV disease | 17% vs. 26% | 21% vs. 15% |
| vs. | |||||||
| 27 | placebo plus immunoglobulin | ||||||
| 172 | Primary and secondary prophylaxis, pediatric | 24 (7) | Ganciclovir 5 mg/kg i.v. twice a day for 2 wk, then acyclovir 800 mg/m2 p.o. 4 times a day for 50 wk | No difference | 29% vs. 84% | ||
| vs. | |||||||
| 24 (5) | ganciclovir 5 mg/kg i.v. twice a day for 2 wk | ||||||
| 143 | Primary prophylaxis, prospective, double-blind, placebo controlled | 150 (21) | Ganciclovir 1,000 mg p.o. 3 times a day for 98 days | Effective in decreasing CMV disease | 5% vs. 19% | 7% vs. 10% | |
| vs. | |||||||
| 154 (25) | placebo | ||||||
| 18 | Primary and secondary prophylaxis, prospective, non-placebo controlled | 83 (12) | Ganciclovir 5mg/kg i.v. twice a day for 14 days, then acyclovir 800 mg p.o. 4 times a day for 106 days | Decreased CMV disease in ganciclovir group, even for patients in the D+/R− group | 11% vs. 23% | 7% vs. 8% | |
| vs. | |||||||
| 84 (13) | acyclovir 800 mg p.o. 4 times a day for 120 days | ||||||
| 319 | Primary and secondary prophylaxis, prospective | 52 (9) | Acyclovir 5 mg/kg/day i.v. till discharge, then 5 mg/kg/day p.o. with immunoglobulin (Sandoglobulin; Novartis Pharmaceuticals Corp., East Hanover, N.J.) 200 mg/kg i.v. twice a wk | Decreased CMV disease in ganciclovir group | 15% vs. 4% | 14% vs. 13% | |
| vs. | |||||||
| 52 (7) | ganciclovir 5 mg/kg/day i.v. till discharge, then acyclovir 5 mg/kg/day p.o. with immunoglobulin 200 mg/kg i.v. twice a wk | ||||||
| 284 | Primary and secondary prophylaxis, prospective | 71 (11) | Acyclovir 800 mg p.o. 4 times a day for 3 mo | Decreased CMV infection and disease; delayed onset of CMV infection in ganciclovir group; no decrease in primary CMV infection | 28% vs. 9% | 7% vs. 12% | |
| vs. | |||||||
| 68 (7) | ganciclovir 5 mg/kg/day i.v. for 2 wk, then acyclovir 800 mg p.o. 4 times a day for 2.5 mo | ||||||
| 72 | Primary and secondary prophylaxis (excluding D−/R−), prospective | 33 (3) | Ganciclovir 5 mg/kg i.v. twice a day for 14 days during wk 3 and 4 posttransplantation | No difference in clinical infection; lower incidence of serologically diagnosed infection in ganciclovir group | 27% vs. 34% | 3% vs. 19% | |
| vs. | |||||||
| 32 (7) | no prophylaxis | ||||||
| 497 | Primary and secondary prophylaxis, prospective, non-placebo controlled | 124 (10) | Ganciclovir 6 mg/kg/day i.v. on days 1–30; then Monday–Friday through day 100 | Decreased CMV infection and disease in ganciclovir group | 0.8% vs. 10% | 15% vs. 14% | |
| vs. | |||||||
| 126 (11) | acyclovir 10 mg/kg i.v. 3 times a day till discharge; then 800 mg p.o. 4 times a day till day 100 |
If known, the number of CMV-negative patients given donor-positive organs (D+/R−) is shown in parentheses.
p.o., peroral; i.v., intravenous.
Among patients given the drug, the percentage refers to the first versus the second listed regimen.
Some retrospective studies on the efficacy of acyclovir prophylaxis in high-risk renal transplant patients document a high breakthrough and mortality from primary CMV disease in patients who received oral acyclovir (165, 502). However, a randomized, placebo-controlled trial using high-dose oral acyclovir has shown acyclovir to have a moderately beneficial effect in preventing CMV disease following kidney transplantation (26). Similarly, high-dose acyclovir with targeted intravenous ganciclovir administration during antilymphocyte antibody therapy appears to be an effective strategy against CMV reactivation in those receiving either a kidney or kidney-pancreas allograft (35, 417). Results of similar studies done on liver transplant recipients have been disappointing (284, 423, 497), although one study suggested a beneficial effect with 2 g of oral acyclovir a day taken by CMV-seropositive liver transplant recipients for 16 weeks (145). While acyclovir is not particularly active against CMV in vitro, it is possible that the achievable cellular levels will inhibit the small amounts of replicating virus that are present as it emerges from latency. Recently published data shows valacyclovir, the prodrug of acyclovir, to be effective in preventing CMV disease in kidney transplant recipients (269a).
Adverse effects of acyclovir administration include phlebitis after intravenous infusion, renal toxicity, confusion, delirium, lethargy, lightheadedness, tremors, seizures, nausea, vomiting, and rash. Although acyclovir meets many of the criteria for an ideal prophylactic drug, its efficacy as an anti-CMV compound is suboptimal. Based on current data, it can be indicated as a primary agent only for non-high-risk renal transplant recipients.
Intravenous ganciclovir administered to heart (299), liver (18, 72, 284, 319, 497), kidney (382), and lung (104) transplant recipients has been successful in preventing CMV disease. Decreased and delayed CMV disease was observed in liver transplant recipients receiving 2 weeks of ganciclovir followed by high-dose acyclovir compared to the effect in those receiving only high-dose acyclovir (18, 284). However, a study of pediatric liver transplant recipients demonstrated no benefit with 2 weeks of intravenous ganciclovir followed by high-dose oral acyclovir for CMV prophylaxis (172). Yet another study showed that ganciclovir administered for 100 days after liver transplantation significantly decreased the incidence of CMV disease (497).
The rate of CMV infection and disease is higher in lung transplant recipients than in other solid-organ transplant recipients. Therefore, prolonging the administration of ganciclovir could theoretically reduce CMV-associated morbidity. Within this context, ganciclovir administration beginning 1 week after lung transplantation and continued until day 90 was slightly more effective than a 3-week course of ganciclovir followed by high-dose oral acyclovir (104). A reduction in the frequency of CMV infection occurred, although this effect was not maintained as the follow-up period increased.
An alternative approach is to combine intravenous ganciclovir with intravenous immunoglobulin. In a randomized placebo-controlled trial, intravenous ganciclovir given for 30 days versus placebo given concurrently with intravenous immunoglobulin for 30 days to pediatric liver transplant recipients at risk for primary CMV disease did not show any benefit of ganciclovir in the prevention of CMV disease above that achieved by intravenous immunoglobulin alone (232). The prophylactic administration of ganciclovir in combination with hyperimmune globulin to lung transplant recipients averted the development of serious CMV disease in those at risk, i.e., those with either donor or recipient CMV seropositivity (189). It is possible that lung and gastrointestinal transplant recipients and high-risk recipients of other organ allografts will require protracted courses of antiviral prophylaxis to successfully avert the development of CMV disease.
The administration of intravenous ganciclovir for 100 days is not generally acceptable because of the need for continuous intravenous access and the costs this entails. Recently, an oral formulation of ganciclovir has become available. Data on the efficacy of oral ganciclovir in the prevention of CMV disease following liver transplantation has been published (143). In this study, both CMV-seropositive recipients and CMV-seronegative recipients of seropositive allografts were randomized to receive either placebo or oral ganciclovir, 1 g three times a day until day 98 after transplantation. Those who received oral ganciclovir had a significantly lower incidence and delayed onset of both CMV infection and disease. This beneficial effect was not attenuated by the use of antilymphocyte therapy. In a similar fashion, a 12-week course of oral ganciclovir (1 g three times a day) given to recipients of kidneys from CMV-seropositive donors, begun at the time of transplantation, prevented CMV infection and disease during the period of prophylaxis (51). Although achievable ganciclovir levels in serum following oral administration are significantly lower than those achieved following parenteral administration, they may be sufficient to inhibit viral replication following transplantation.
Data from prospective randomized trials of antiviral prophylaxis in solid-organ transplant recipients have established a clinically significant beneficial effect of antiviral agents in reducing the incidence of both CMV infection and disease (79). Although not standard practice in all transplantation programs, oral ganciclovir should be considered for CMV prophylaxis for CMV-seropositive recipient or donor CMV-seropositive/recipient CMV-seronegative liver and heart transplant patients, and for donor CMV-seropositive/recipient CMV-seronegative kidney transplant recipients. For donor CMV-seropositive/recipient CMV-seronegative lung transplant recipients, intravenous followed by oral ganciclovir may be used in combination with immunoglobulin, and for CMV-seropositive lung transplant recipients, intravenous followed by oral ganciclovir may be used, although standard regimens have not been established. In general, prophylactic antiviral agents should not be used in seronegative transplant recipients receiving organs from seronegative donors.
Prophylaxis against CMV may have the added benefit of preventing other superinfection, especially those for which CMV infection is itself a risk factor. For instance, prophylactic ganciclovir administration reduces fungal as well as CMV infections in cardiac transplant recipients (487). Despite ganciclovir prophylaxis, however, there is evidence that cardiac transplant recipients who develop CMV disease have inferior long-term survival and graft function and a higher incidence of coronary atherosclerosis compared to those who do not have the disease (473).
The effect of prolonged ganciclovir prophylaxis on the emergence of resistant viral strains has not been extensively studied. While an early study showed that antiviral prophylaxis in solid-organ transplant recipients did not select for ganciclovir-resistant isolates of CMV (43), reports that the use of ganciclovir may select for drug-resistant CMV have been increasing (22, 271, 383). As with any pharmacologic agent, the costs of prophylactic ganciclovir administration must be taken into account (Table 6). As well, use of the intravenous formulation necessitates the placement of vascular catheters for extended venous access, and this carries an increased risk for line infections.
TABLE 6.
Cost of antiviral prophylaxis for CMV infection in solid-organ transplant recipientsa
| Prophylactic regimenb | Charge |
|---|---|
| Acyclovir 800 mg orally qid for 14 days (inpatient) | $125.68 |
| Acyclovir 800 mg orally qid for 120 days (14 days inpatient and 106 days outpatient) | $1,683.98c |
| Acyclovir 5 mg/kg intravenously tid for 14 days (inpatient) | $2,158.80d |
| Valacyclovir 2 g orally qid for 90 days (14 days inpatient and 76 days outpatient) | $4,328.79e |
| Ganciclovir 5 mg/kg intravenously bid for 14 days (inpatient) | $1,646.75d |
| Ganciclovir 5 mg/kg intravenously 5 days a week for 3 months (outpatient) | $3,399.60d |
| Ganciclovir 3 g/day orally for 16 weeks (outpatient) | $5,613.05f |
| CMV immunoglobulin (Cytogam; Medimmune Inc., Gaithersburg, Md.) 150 mg/kg within 72 h; 200 mg/kg at wk 2, 4, 6, and 8; 50 mg/kg at wk 12 and 16 | $16,892.33d |
Outpatient costs reflect Mayo Clinic Pharmacy charges as of 15 January 1998. Mark-up, preparation, and in-hospital administration charges are included. Outpatient administration of intravenous preparations not included. The cost of intravenous ganciclovir therapy for 5 days per week is based on home administration using the Intermate system.
qid, four times a day; tid, three times a day; bid, twice a day.
Cost based on generic brand of acyclovir (Schein Pharmaceutical, Inc., Florham Park, N.J.).
Cost based on the dose for a 70-kg kidney transplant patient. The dose for other types of solid-organ transplant recipients (e.g., liver transplant recipients) may be higher and thus the cost will increase.
Cost based on a 500-mg caplet (Valtrex; Glaxo Wellcome, Inc., Research Triangle Park, N.C.).
Cost based on a 250-mg capsule (Cytovene; Roche Laboratories, Inc., Nutley, N.J.).
Studies of foscarnet prophylaxis in solid-organ transplant recipients have not been done. The drug requires intravenous administration and is not a suitable prophylactic agent because of its significant nephrotoxicity. CMV monoclonal antibody is being developed, but its use will be costly; unless it proves to be highly efficacious, it will probably not be cost-effective. Cidofovir exerts potent antiviral activity against CMV, including some ganciclovir-resistant strains. Its long half-life allows a less frequent dosing interval by the parenteral route, making it an attractive candidate agent for CMV prophylaxis. A major drawback is the resulting nephrotoxicity; coadministration of probenecid could potentially reduce the incidence of this undesirable complication (19). Lobucavir is another active oral anti-CMV agent (49); its clinical efficacy for CMV prophylaxis is as yet not clear. The prodrug of ganciclovir, valganciclovir, is similarly very active against CMV; the ease of oral administration combined with its high bioavailability certainly makes this drug a very attractive choice among all the antiviral agents.
The ideal anti-CMV prophylactic regimen(s) has yet to be established. A number of protocols have been adopted by various transplant institutions. Regimens are based on the type of organ transplant, the assessment of an individual's risk for acquiring CMV infection, laboratory detection of CMV, and the intensity of immunosuppression.
Preemptive Prophylaxis
The introduction of rapid diagnostic tests has enabled clinicians to detect viral replication and therefore to diagnose active CMV infection prior to the onset of overt disease. This provides an opportunity for the initiation of early antiviral treatment. This so-called preemptive therapy is defined as highly effective treatment administered for a brief period to individuals who are at the highest risk for the development of serious CMV disease (391). This approach has the advantage of avoiding unnecessary prophylaxis in patients who are at no increased risk for CMV-associated morbidity and death. Early therapy given in this manner is dependent on a laboratory marker or patient characteristic which identifies the subgroup of individuals at an increased risk for disease at a time when antimicrobial intervention would be maximally effective in aborting the impending disease process (392).
The detection of markers for early CMV infection is an essential aspect of the success of preemptive treatment. Candidate laboratory tests include molecular assays that detect CMV DNA or RNA, antigenemia tests, and rapid viral cultures (2, 33, 91, 163, 239, 297, 335, 336, 351, 464, 474). It becomes imperative that the test chosen not only detect the presence of CMV sufficiently in advance of onset of symptoms, but also predict subsequent CMV disease and the need for antiviral therapy. The sensitivity and specificity of a laboratory assay as a marker of future CMV disease in the different solid-organ transplant populations is a matter of debate. The utility of any of these assays can be effectively established only when evaluated in the context of an effective antiviral agent. The ideal scenario consists of the performance of a relatively inexpensive surveillance test to detect the presence of an early marker for CMV disease, with a quick turnaround time, at the period when the risk of viral acquisition after organ transplantation is at the highest (i.e., 2 to 6 weeks). This is followed by the initiation of treatment with a highly effective anti-CMV agent that is taken orally by those identified with a positive disease marker (76, 110, 143, 197, 300, 423, 447, 453) (Table 7).
TABLE 7.
Randomized trials of preemptive therapy in solid-organ transplant recipientsd
| Type of transplant | Reference | Type of study | No. of patients studied (no. of D+/R− patients)a | Prophylactic regimenb | Outcome(s) | CMV diseasec | Mortalityc |
|---|---|---|---|---|---|---|---|
| Kidney | 447 | Secondary prophylaxis, >6 days of prophylactic treatment posttransplant with ALG or OKT3 or treatment within first 2 weeks for acute rejection | 16 (0) | Immunoglobulin (Sandoglobulin; Novartis Pharmaceuticals Corp., East Hanover, N.J.) 500 mg/kg i.v. on day 0 and wk 2 and 4; 250 mg/kg at wk 6 and 8 | Reduction in severity of symptomatic CMV illness and incidence of CMV complications | 13% vs. 39% | Not reported |
| vs. | |||||||
| 18 (0) | untreated controls | ||||||
| 300 | Primary and secondary prophylaxis of patients receiving ATG for rejection, double-blind, placebo controlled | 19 (5) | CMV immunoglobulin (Cytogam; Medimmune Inc., Gaithersburg, Md.) 100 mg/kg/day on day of ATG therapy and days 7, 14, 35, 56, and 77 thereafter | Prevented fatal CMV disease; should be targeted to D+/R− group | 37% vs. 30% | 0% vs. 20% | |
| vs. | |||||||
| 20 (4) | placebo (albumin) | ||||||
| 197 | Secondary prophylaxis of patients receiving OKT3 or ALG, non-placebo controlled, prospective | 64 (0) | Ganciclovir 2.5 mg/kg i.v. twice a day till termination of antilymphocyte therapy | Ganciclovir reduced excessive occurrence of CMV disease | 14% vs. 33% | 2% vs. 4% | |
| vs. | |||||||
| 49 (0) | untreated controls | ||||||
| 76 | Primary and secondary prophylaxis of patients on OKT3, prospective, non-placebo controlled | 22 (0) | Ganciclovir 2.5 mg/kg i.v. on day that antilymphocyte antibody therapy was given | Reduction in CMV disease | 0% vs. 17% | 100% vs. 100% | |
| vs. | |||||||
| 18 (0) | no prophylaxis | ||||||
| Liver | 453 | Secondary prophylaxis of patients on antilymphocyte antibody preparations, prospective, non-placebo controlled | 50 (14) | Immunoglobulin (Gammagard; Baxter Healthcare Corp., Glendale, Calif.) 0.5 g/kg i.v. on days 1, 3, 5, then each wk for 3 wk with acyclovir 400 mg p.o. 5 times a day for 3 months | No benefit | Not shown | 10% vs. 22% |
| vs. | |||||||
| 50 (3) | no prophylaxis | ||||||
| 423 | Primary and secondary prophylaxis; stratified by donor and recipient CMV serostatus | 24 (2) | Acyclovir 800 mg p.o. 4 times a day for 24 wk | Ganciclovir provided effective prophylaxis against CMV disease | 29% vs. 4% | 13% vs. 13% | |
| vs. | |||||||
| 23 (2) | ganciclovir 5 mg/kg i.v. twice a day for 7 days if surveillance cultures (buffy coat, urine) yield CMV |
If known, the number of CMV-negative patients given donor-positive organs (D+/R−) is shown in parentheses.
ALG, antilymphocyte globulin; ATG, antithymocyte globulin; i.v., intravenous; p.o., peroral.
Among patients given the drug, the percentage refers to the first versus the second listed regimen.
Among liver transplant recipients, a 7-day course of intravenous ganciclovir started when CMV was cultured from surveillance blood or urine cultures provided effective prophylaxis against symptomatic illness (423). However, CMV disease developed in 63% of those without prior positive surveillance cultures. Since the sensitivity of the shell vial assay as an early marker of CMV disease is poor (8 to 63%) (347), it is not a reliable test on which to base preemptive therapy.
Antigenemia testing shows promise as a marker for preemptive therapy (109, 211). By using CMV antigenemia as the diagnostic assay, intravenous ganciclovir given to those with positive tests was highly effective in preventing CMV disease (168). Test positivity may precede CMV disease onset by up to 14 days (107, 117, 458, 466, 469), allowing for timely intervention. In cardiac transplant recipients, antigenemia is 83% sensitive as an early marker for the future development of symptomatic CMV infection but precedes the onset of overt disease by only 5 days (239). In one study, preemptive treatment with ganciclovir based on antigenemia reduced the incidence of disease in lung and heart transplant patients while omitting unnecessary antiviral prophylaxis in those who were CMV antigen negative (110).
In a study involving nine renal transplant patients monitored twice weekly, antigenemia-positive subjects were randomized to receive intravenous ganciclovir, 5 mg/kg/day for 10 days, versus observation alone (464). Each of four patients who received preemptive therapy remained asymptomatic; when the treatment was stopped, antigen levels increased in three of the four and these three subsequently manifested symptomatic CMV infection. CMV disease developed rapidly in the five control patients. These outcomes suggest that ganciclovir therapy was not started early enough (i.e., positive antigenemia tests occurred too late for preemptive therapy to be of significant benefit) or that either higher doses and/or longer courses of ganciclovir therapy are required to successfully prevent CMV disease. This vignette illustrates the complexities involved in the institution of preemptive therapy.
Standard methods for the detection of viral nucleic acids, including PCR-based tests, have been used to diagnose CMV infection presymptomatically. With advancements in molecular biotechnology, PCR can be performed quickly and can give quantitative information. PCR performed on peripheral blood leukocytes gives the earliest positive signal of CMV replication, followed by PCR performed on plasma or serum (500). In one study, peripheral blood leukocyte PCR positivity preceded CMV disease by 17 days while serum PCR positivity preceded CMV disease by 12 days (298). Importantly, different PCR assay conditions, including primer set selections, may influence the sensitivity of such assays. This could potentially be used to guide preemptive therapy. Studies performed on liver transplant recipients have shown that among the donor-seropositive/recipient-seronegative group, PCR positivity in peripheral blood lymphocytes strongly predicts the subsequent development of CMV disease, suggesting that in this patient group, qualitative PCR remains a reliable indicator on which to base preemptive treatment (2, 297). A study performed with kidney transplant recipients has shown that quantitative PCR detection of CMV in peripheral blood leukocytes may provide an indicator of impending symptomatic disease (378). Although quantitative PCR assays are attractive tests for the diagnosis of established CMV disease, qualitative assays may be sufficient for the early diagnosis of CMV infection before the development of disease (33, 255, 358).
Among renal allograft recipients who receive antithymocyte induction therapy, PCR of buffy coat specimen is superior to conventional culture monitoring for the detection of CMV viremia (51, 120). Based on a positive CMV PCR, preemptive therapy with ganciclovir decreased symptomatic CMV episodes, although the overall cost was equivalent between those who received preemptive therapy and those in whom treatment was deferred (51).
PCR detection of CMV DNA in transbronchial lung biopsy specimens from lung transplant recipients within the first month after transplantation indicates a greatly increased risk for developing CMV disease (235). Quantitation of PCR-amplified CMV particles in bronchoalveolar lavage specimens has been successfully used to predict the development of CMV pneumonitis in lung and heart-lung transplant patients, and its use as a marker for preemptive therapy has been suggested (56). PCR quantitation of CMV DNA in blood and urine appears to be another potential assay for predicting clinical disease (101, 141, 378). PCR is a sensitive method for the early detection of CMV in allograft intestinal biopsy specimens and may be a valuable marker for preemptive therapy after intestinal transplantation (246). For early diagnosis, detection of CMV mRNA by PCR is inferior to the antigenemia assay (302). At present, PCR is the most sensitive assay and provides the earliest marker of CMV disease in solid-organ transplant recipients.
In addition to laboratory diagnosis of CMV, individuals at risk for CMV infection may be identified by certain patient profiles. Antirejection treatment and the use of antilymphocyte antibodies following transplantation pose significant threats for the development of CMV disease (242, 359). For viral prophylaxis to be efficacious, the potency of antiviral strategies needs to be proportionate to the intensity of the anti-rejection regimen. As demonstrated in renal transplant recipients in whom antithymocyte globulin therapy is a risk factor for CMV disease, the concomitant administration of intravenous ganciclovir decreased the incidence of CMV disease (76, 197). This may potentially provide a cost-effective strategy of significantly improving the outcome of organ transplantation in CMV-seropositive patients. Preemptive intravenous ganciclovir therapy in seropositive liver transplant recipients treated with OKT3 for steroid-resistant rejection resulted in a delay in the time of onset of CMV infection and a decrease in the frequency and severity of CMV disease (270). Intravenous ganciclovir given to CMV-seropositive kidney and liver transplant patients receiving antilymphocyte antibody therapy virtually prevented CMV disease in allograft recipients (471). The efficacy of immunoglobulin for preemptive therapy is less clear. Among liver transplant recipients, immunoglobulin alone reduced the severity of CMV disease associated with antilymphocyte therapy (351, 447); used in combination with acyclovir during antilymphocyte therapy, immunoglobulin infusion did not reduce the rate of CMV disease (453).
Overall, preemptive therapy is a promising concept in the management of CMV infection following solid-organ transplantation. Routine monitoring for CMV infection may be warranted after organ transplantation. While several categories of patients might benefit from preemptive therapy, transplant recipients with early primary CMV infection will gain the most benefit. This mode of therapy has made possible the safe administration of antilymphocyte antirejection therapy in patients with steroid-resistant disease (483). Early detection of infection may have important consequences for patient management. At present, there is no consensus on whether PCR or antigenemia testing is to be preferred in directing preemptive treatment. Besides, new developments are rapidly occurring in CMV diagnostics, necessitating the need for continued study and clinical validation of test methods. In addition, the development of effective, safe, inexpensive oral antiviral agents may preclude the need for preemptive therapy.
Adoptive Immunotherapy
Since immunity to CMV prior to transplantation decreases the incidence of CMV disease following transplantation, boosting the immune system after transplantation should have a beneficial effect in decreasing CMV disease. A fascinating new development in CMV immunotherapy is the concept of adoptive transfer of CMV-specific cytotoxic T cells (248). Class I major histocompatibility complex-restricted CMV-specific cytotoxic lymphocytes are important in the control of CMV infections in healthy and immunosuppressed individuals (365, 374). Expanding the number and function of virus-specific cytotoxic T lymphocytes to reduce the incidence of CMV disease following bone marrow transplantation is now a reality (376, 489). Tentative experience of using T-cell immunotherapy of CMV infection in bone marrow transplant recipients reveals that therapy with CD8+ T cells prevents CMV disease and accelerates the resolution of active infection (357, 445). This approach has not been evaluated in the solid-organ transplant recipient population.
CONCLUSIONS
While CMV disease continues to be a formidable issue in clinical transplantation, substantial progress has been made during the last decade with respect to the diagnosis and monitoring of CMV infection. Sensitive detection systems for CMV-specific proteins and nucleic acid sequences have been developed. In addition, although CMV infection (like most other infections in the transplant recipient) is better prevented than treated, much progress in the treatment of active infection has been made. A strong motivation for continued pharmaceutical development is making available nontoxic, orally active antiviral drugs that will further improve the clinical management of this infection. The impetus for research in the present era not only is toward the treatment of active CMV disease but also has focused on the prevention of the far-reaching consequences of CMV infection and disease in the overall long-term outcome of this vulnerable patient population. It is likely that emerging technologic advances and specific antiviral agents will play increasing roles in the investigations of CMV infection in the next few years. Thus, a combined prevention-treatment plan for the management of CMV disease is now a reality.
ACKNOWLEDGMENTS
We thank K. St. George and C. Rinaldo, University of Pittsburgh Medical Center, for supplying Fig. 4.
REFERENCES
- 1.Aalto S M, Linnavuori K, Peltola H, Vuori E, Weissbrich B, Schubert J, Hedman L, Hedman K. Immunoreactivation of Epstein-Barr virus due to cytomegalovirus primary infection. J Med Virol. 1998;56:186–191. [PubMed] [Google Scholar]
- 2.Abecassis M M, Koffron A J, Kaplan B, Buckingham M, Muldoon J P, Cribbins A J, Kaufman D B, Fryer J P, Stuart J, Stuart F P. The role of PCR in the diagnosis and management of CMV in solid organ recipients: what is the predictive value for the development of disease and should PCR be used to guide antiviral therapy? Transplantation. 1997;63:275–279. doi: 10.1097/00007890-199701270-00017. [DOI] [PubMed] [Google Scholar]
- 3.Adler S P. Cytomegalovirus and child day care. Evidence for an increased infection rate among day-care workers. N Engl J Med. 1989;321:1290–1296. doi: 10.1056/NEJM198911093211903. [DOI] [PubMed] [Google Scholar]
- 4.Adler S P. Cytomegalovirus and child day care: risk factors for maternal infection. Pediatr Infect Dis J. 1991;10:590–594. doi: 10.1097/00006454-199108000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Aguado J M, Gomez-Sanchez M A, Lumbreras C, Delgado J, Lizasoain M, Otero J R, Rufilanchas J J, Noriega A R. Prospective randomized trial of efficacy of ganciclovir versus that of anti-cytomegalovirus (CMV) immunoglobulin to prevent CMV disease in CMV-seropolitive heart transplant recipients treated with OKT3. Antimicrob Agents Chemother. 1995;39:1643–1645. doi: 10.1128/aac.39.7.1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reference deleted.
- 7.Agut H, Huraux J M, Collandre H, Montagnier L. Susceptibility of human herpesvirus 6 to acyclovir and ganciclovir. Lancet. 1989;ii:626. doi: 10.1016/s0140-6736(89)90754-x. [DOI] [PubMed] [Google Scholar]
- 8.Ahsan N, Holman M J, Yang H C. Efficacy of oral ganciclovir in prevention of cytomegalovirus infection in post-kidney transplant patients. Clin Transplant. 1997;11:633–639. [PubMed] [Google Scholar]
- 9.Akposso K, Rondeau E, Haymann J P, Peraldi M N, Marlin C, Sraer J D. Long-term prognosis of renal transplantation after preemptive treatment of cytomegalovirus infection. Transplantation. 1997;63:974–976. doi: 10.1097/00007890-199704150-00012. [DOI] [PubMed] [Google Scholar]
- 10.Alain S, Honderlick P, Grenet D, Stern M, Vadam C, Sanson-Le Pors M J, Mazeron M C. Failure of ganciclovir treatment associated with selection of a ganciclovir-resistant cytomegalovirus strain in a lung transplant recipient. Transplantation. 1997;63:1533–1536. doi: 10.1097/00007890-199705270-00031. [DOI] [PubMed] [Google Scholar]
- 11.Anderson K P, Fox M C, Brown-Driver V, Martin M J, Azad R F. Inhibition of human cytomegalovirus immediate-early gene expression by an antisense oligonucleotide complementary to immediate-early RNA. Antimicrob Agents Chemother. 1996;40:2004–2011. doi: 10.1128/aac.40.9.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Armstrong J A, Evans A S, Rao N, Ho M. Viral infections in renal transplant recipients. Infect Immun. 1976;14:970–975. doi: 10.1128/iai.14.4.970-975.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arnold J C, Portmann B C, O'Grady J G, Naoumov N V, Alexander G J M, Williams R. Cytomegalovirus infection persists in the liver graft in the vanishing bile duct syndrome. Hepatology. 1992;16:285–292. doi: 10.1002/hep.1840160202. [DOI] [PubMed] [Google Scholar]
- 14.Bachmann M F, Kalinke U, Althage A, Freer G, Burkhart C, Roost H, Aguet M, Hengartner H, Zinkernagel R M. The role of antibody concentration and avidity in antiviral protection. Science. 1997;276:2024–2027. doi: 10.1126/science.276.5321.2024. [DOI] [PubMed] [Google Scholar]
- 15.Bacigalupo A, Bregante S, Tedone E, Isaza A, Van Lint M T, Moro F, Trespi G, Occhini D, Gualandi F, Lamparelli T, Marmont A M. Combined foscarnet-ganciclovir treatment for cytomegalovirus infections after allogeneic hemopoietic stem cell transplantation (HSCT) Bone Marrow Transplant. 1996;2:110–114. [PubMed] [Google Scholar]
- 16.Bacigalupo A, Bregante S, Tedone E, Isaza A, Van Lint M T, Trespi G, Occhini D, Gualandi F, Lamparelli T, Marmont A M. Combined foscarnet-ganciclovir treatment for cytomegalovirus infections after allogeneic hemopoietic stem cell transplantation. Transplantation. 1996;62:376–380. doi: 10.1097/00007890-199608150-00013. [DOI] [PubMed] [Google Scholar]
- 17.Badley A D, Patel R, Portela D F, Harmsen W S, Smith T F, Ilstrup D M, Steers J L, Wiesner R H, Paya C V. Prognostic significance and risk factors of untreated cytomegalovirus viremia In liver transplant recipients. J Infect Dis. 1996;173:446–449. doi: 10.1093/infdis/173.2.446. [DOI] [PubMed] [Google Scholar]
- 18.Badley A D, Seaberg E C, Porayko M K, Wiesner R H, Keating M R, Wilhelm M P, Walker R C, Patel R, Marshall W F, DeBernardi M, Zetterman R, Steers J L, Paya C V. Prophylaxis of cytomegalovirus infection in liver transplantation: a randomized trial comparing a combination of ganciclovir and acyclovir to acyclovir. NIDDK Liver Transplantation Database. Transplantation. 1997;64:66–73. doi: 10.1097/00007890-199707150-00013. [DOI] [PubMed] [Google Scholar]
- 19.Bailey T C. Prevention of cytomegalovirus disease. Semin Respir Infect. 1993;8:225–232. [PubMed] [Google Scholar]
- 20.Bailey T C, Buller R S, Ettinger N A, Trulock E P, Gaudreault-Keener M, Langlois T M, Fornoff J E, Cooper J D, Storch G A. Quantitative analysis of cytomegalovirus viremia in lung transplant recipients. J Infect Dis. 1995;171:1006–1010. doi: 10.1093/infdis/171.4.1006. [DOI] [PubMed] [Google Scholar]
- 21.Bailey T C, Ettinger N A, Trulock E P, Storch G A, Cooper J D, Powderly W G. Failure of high-dose oral acyclovir with or without globulin to prevent primary cytomegalovirus disease in recipients of solid organ transplants. Am J Med. 1993;95:273–278. doi: 10.1016/0002-9343(93)90279-x. [DOI] [PubMed] [Google Scholar]
- 22.Baldanti F, Simoncini L, Sarasini A, Zavattoni M, Grossi P, Revello M G, Gerna G. Ganciclovir resistance as a result of oral ganciclovir in a heart transplant recipient with multiple human cytomegalovirus strains in the blood. Transplantation. 1998;66:324–329. doi: 10.1097/00007890-199808150-00008. [DOI] [PubMed] [Google Scholar]
- 23.Baldanti F, Underwood M R, Stanat S C, Biron K K, Chou S, Sarasini A, Silini E, Gerna G. Single amino acid changes in the DNA polymerase confer foscarnet resistance and slow-growth phenotype, while mutations in the UL97-encoded phosphotransferase confer ganciclovir resistance in three double-resistant human cytomegalovirus strains recovered from patients with AIDS. J Virol. 1996;70:1390–1395. doi: 10.1128/jvi.70.3.1390-1395.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baldanti F, Underwood M R, Talarico C L, Simoncini L, Sarasini A, Biron K K, Gerna G. The Cys607→Tyr change in the UL97 phosphotransferase confers ganciclovir resistance to two human cytomegalovirus strains recovered from two immunocompromised patients. Antimicrob Agents Chemother. 1998;42:444–446. doi: 10.1128/aac.42.2.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bale J F, Zimmerman B, Dawson J D, Souza I E, Petheram S J, Murph J R. Cytomegalovirus transmission in child care homes. Arch Pediatr Adolesc Med. 1999;153:75–79. doi: 10.1001/archpedi.153.1.75. [DOI] [PubMed] [Google Scholar]
- 26.Balfour H H, Chace B A, Stapleton J T, Simmons R L, Fryd D S. A randomized placebo-controlled trial of oral acyclovir for the prevention of cytomegalovirus disease in recipients of renal allografts. N Engl J Med. 1989;320:1381–1387. doi: 10.1056/NEJM198905253202105. [DOI] [PubMed] [Google Scholar]
- 27.Bando K, Paradis I L, Komatsu K, Konishi H, Matsushima M, Keena R J, Hardesty R L, Armitage J M, Griffith B P. Analysis of time-dependent risks for infection, rejection, and death after pulmonary transplantation. J Thorac Cardiovasc Surg. 1995;109:49–59. doi: 10.1016/s0022-5223(95)70419-1. [DOI] [PubMed] [Google Scholar]
- 28.Bando K, Paradis I L, Similo S, Konishi H, Komatsu K, Zullo T G, Yousem S A, Close J M, Zeevi A, Duquesnoy R J, et al. Obliterative bronchiolitis after lung and heart-lung transplantation. An analysis of risk factors and management. J Thorac Cardiovasc Surg. 1995;110:4–14. doi: 10.1016/S0022-5223(05)80003-0. [DOI] [PubMed] [Google Scholar]
- 29.Barkholt L M, Ehrnst A, Veress B. Clinical use of immunohistopathologic methods for the diagnosis of cytomegalovirus hepatitis in human liver allograft biopsy specimens. Scand J Gastroenterol. 1994;29:553–560. doi: 10.3109/00365529409092472. [DOI] [PubMed] [Google Scholar]
- 30.Barkholt L M, Ericzon B G, Ehrnst A, Forsgren M, Andersson J P. Cytomegalovirus infections in liver transplant patients: incidence and outcome. Transplant Proc. 1990;22:235–237. [PubMed] [Google Scholar]
- 31.Basgoz N, Preiksaitis J K. Post-transplant lymphoproliferative disorder. Infect Dis Clin North Am. 1995;9:901–923. [PubMed] [Google Scholar]
- 32.Belles-Isles M, Houde I, Lachance J G, Noel R, Kingma I, Roy R. Monitoring of cytomegalovirus infections by the CD8+CD38+ T-cell subset in kidney transplant recipients. Transplantation. 1998;65:279–282. doi: 10.1097/00007890-199801270-00026. [DOI] [PubMed] [Google Scholar]
- 33.Benedetti E, Mihalov M, Asolati M, Kirby J, Dunn T, Raofi V, Fontaine M, Pollak R. A prospective study of the predictive value of polymerase chain reaction assay for cytomegalovirus in asymptomatic kidney transplant recipients. Clin Transplant. 1998;12:391–395. [PubMed] [Google Scholar]
- 34.Best N G, Trull A K, Tan K K, Spiegelhalter D J, Wreghitt T G, Wallwork J. Blood cyclosporine concentrations and cytomegalovirus infection following heart transplantation. Transplantation. 1995;60:689–694. doi: 10.1097/00007890-199510150-00013. [DOI] [PubMed] [Google Scholar]
- 35.Birkeland S A, Andersen H K, Gahrnhansen B. Prophylaxis against herpes infections in kidney transplant patients with special emphasis on CMV. Scand J Infect Dis. 1998;30:221–226. doi: 10.1080/00365549850160837. [DOI] [PubMed] [Google Scholar]
- 36.Bitsch A, Kirchner H, Dupke R, Bein G. Cytomegalovirus transcripts in peripheral blood leukocytes of actively infected transplant patients detected by reverse transcription-polymerase chain reaction. J Infect Dis. 1993;167:740–743. doi: 10.1093/infdis/167.3.740. [DOI] [PubMed] [Google Scholar]
- 37.Bjøro K, Frøland S, Yun Z, et al. Hepatitis C infection in patients with hypogammaglobulinemia after treatment with contaminated immune globulin. N Engl J Med. 1994;331:1607–1611. doi: 10.1056/NEJM199412153312402. [DOI] [PubMed] [Google Scholar]
- 38.Blok M J, Goossens V J, Vanherle S J, Top B, Tacken N, Middeldorp J M, Christiaans M H, van Hooff J P, Bruggeman C A. Diagnostic value of monitoring human cytomegalovirus late pp67 mRNA expression in renal-allograft recipients by nucleic acid sequence-based amplification. J Clin Microbiol. 1998;36:1341–1346. doi: 10.1128/jcm.36.5.1341-1346.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bock G H, Sullivan E K, Miller D, Gimon D, Alexander S, Ellis E, Elshihabi I. Cytomegalovirus infections following renal transplantation—effects on antiviral prophylaxis: a report of the North American Pediatric Renal Transplant Cooperative Study. Pediatr Nephrol. 1997;11:665–671. doi: 10.1007/s004670050361. [DOI] [PubMed] [Google Scholar]
- 40.Boeckh M, Boivin G. Quantitation of cytomegalovirus: methodologic aspects and clinical applications. Clin Microbiol Rev. 1998;11:533–554. doi: 10.1128/cmr.11.3.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boeckh M, Woogerd P M, Stevens-Ayers T, Ray C G, Bowden R A. Factors influencing detection of quantitative cytomegalovirus antigenemia. J Clin Microbiol. 1994;32:832–834. doi: 10.1128/jcm.32.3.832-834.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boivin G, Chou S, Quirk M R, Erice A, Jordan M C. Detection of ganciclovir resistance mutations quantitation of cytomegalovirus (CMV) DNA in leukocytes of patients with fatal disseminated CMV disease. J Infect Dis. 1996;173:523–528. doi: 10.1093/infdis/173.3.523. [DOI] [PubMed] [Google Scholar]
- 43.Boivin G, Erice A, Crane D D, Dunn D L, Balfour H H. Ganciclovir susceptibilities of cytomegalovirus (CMV) isolates from solid organ transplant recipients with CMV viremia after antiviral prophylaxis. J Infect Dis. 1993;168:322–325. doi: 10.1093/infdis/168.2.332. [DOI] [PubMed] [Google Scholar]
- 44.Boivin G, Quirk M R, Kringstad B A, Germain M, Jordan M C. Early effects of ganciclovir therapy on the quantity of cytomegalovirus DNA in leukocytes of immunocompromised patients. Antimicrob Agents Chemother. 1997;41:860–862. doi: 10.1128/aac.41.4.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Boland G J, Hene R J, Ververs C, de Haan M A, de Gast G C. Factors influencing the occurrence of active cytomegalovirus (CMV) infections after organ transplantation. Clin Exp Immunol. 1993;94:306–312. doi: 10.1111/j.1365-2249.1993.tb03448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boriskin Y S, Booth J C, Corbishley C M, Madden B P, McKenna W J, Murday A J, Steel H M. Human cytomegalovirus and acute rejection after heart transplantation are not directly associated. J Med Virol. 1996;50:59–70. doi: 10.1002/(SICI)1096-9071(199609)50:1<59::AID-JMV11>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 47.Borysiewicz L K, Graham S, Hickling J K, Mason P D, Sissons J G. Human cytomegalovirus-specific cytotoxic T cells: their precursor frequency and stage specificity. Eur J Immunol. 1988;18:269–275. doi: 10.1002/eji.1830180214. [DOI] [PubMed] [Google Scholar]
- 48.Brainard J A, Greenson J K, Vesy C J, Tesi R J, Papp A C, Snyder P J, Western L, Prior T W. Detection of cytomegalovirus in liver transplant biopsies. A comparison of light microscopy, immunohistochemistry, duplex PCR and nested PCR. Transplantation. 1994;57:1753–1757. [PubMed] [Google Scholar]
- 49.Braitman A, Suerdel M R, Olsen S J, Tuamori A V, Lynch J S, Blue B, Michalik T, Filed A K, Bonner D P, Clark J M. Evaluation of SQ 34,514L pharmacokinetics and efficacy in experimental herpesvirus infections in mice. Antimicrob Agents Chemother. 1991;35:1464–1468. doi: 10.1128/aac.35.7.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brennan D C, Garlock K A, Lippmann B A, Buller R S, Gaudreault-Keener M, Lowell J A, Miller S B, Shenoy S, Howard T K, Storch G A. Control of cytomegalovirus-associated morbidity in renal transplant patients using intensive monitoring and either preemptive or deferred therapy. J Am Soc Nephrol. 1997;8:118–125. doi: 10.1681/ASN.V81118. [DOI] [PubMed] [Google Scholar]
- 51.Brennan D C, Garlock K A, Singer G G, Schnitzler M A, Lippmann B J, Buller R S, Gaudreault-Keener M, Lowell J A, Shenoy S, Howard T K, Storch G A. Prophylactic oral ganciclovir compared with deferred therapy for control of cytomegalovirus in renal transplant recipients. Transplantation. 1997;64:1843–1846. doi: 10.1097/00007890-199712270-00036. [DOI] [PubMed] [Google Scholar]
- 52.Buhles W C, Mastre B J, Tinker A J, Strand V, Koretz S H. Ganciclovir treatment of life- or sight-threatening cytomegalovirus infection: experience in 314 immunocompromised patients. Rev Infect Dis. 1988;106:S495–S506. doi: 10.1093/clinids/10.supplement_3.s495. [DOI] [PubMed] [Google Scholar]
- 53.Burdelski M, Schmidt K, Hoyer P F, Bernsau U, Galaske R, Brodehl J, Ringe B, Lauchart W, Wonigeit K, Pichlmayr R. Liver transplantation in children: the Hanover experience. Transplant Proc. 1987;19:3277–3281. [PubMed] [Google Scholar]
- 54.Burgart L J, Heller M J, Reznicek M J, Greiner T C, Teneyck C J, Robinson R A. Cytomegalovirus detection in bone marrow transplant patients with idiopathic pneumonitis. A clinicopathologic study of the clinical utility of the polymerase chain reaction on open lung biopsy specimen tissue. Am J Clin Pathol. 1991;96:572–576. doi: 10.1093/ajcp/96.5.572. [DOI] [PubMed] [Google Scholar]
- 55.Bush C E, Sluchakcarlsen J A. Evaluation of a leukocyte stabilization reagent for use in the cytomegalovirus pp65 antigenemia assay. J Clin Microbiol. 1998;36:3410–3411. doi: 10.1128/jcm.36.11.3410-3411.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cagle P T, Buttone G, Holland V A, Samo T, Demmler G J, Noon G P, Lawrence E C. Semiquantitative measurement of cytomegalovirus DNA in lung and heart-lung transplant patients by in vitro DNA amplification. Chest. 1992;101:93–96. doi: 10.1378/chest.101.1.93. [DOI] [PubMed] [Google Scholar]
- 57.Carlstrom G, Jalling B. Cytomegalovirus infections in different groups of paediatric patients. Acta Paediatr Scand. 1970;59:303–309. doi: 10.1111/j.1651-2227.1970.tb09008.x. [DOI] [PubMed] [Google Scholar]
- 58.Carney W P, Rubin R H, Hoffman R A, Hansen W P, Healey K, Hirsch M S. Analysis of T lymphocyte subsets in cytomegalovirus mononucleosis. J Immunol. 1981;126:2114–2116. [PubMed] [Google Scholar]
- 59.Cerrina J, Bavoux E, Le Roy Ladurie F, Herve P, Lafont D, Simonneau G, Dartevelle P. Ganciclovir treatment of cytomegalovirus infection in heart-lung and double-lung transplant recipients. Transplant Proc. 1991;23:1174–1175. [PubMed] [Google Scholar]
- 60.Chandler S H, Holmes K K, Wentworth B B, Gutman L T, Wiesner P J, Alexander E R, Handsfield H H. The epidemiology of cytomegaloviral infection in women attending a sexually transmitted disease clinic. J Infect Dis. 1985;152:597–605. doi: 10.1093/infdis/152.3.597. [DOI] [PubMed] [Google Scholar]
- 61.Cheeseman S H, Rubin R H, Stewart J A, Tolkoff-Rubin N E, Cosimi A B, Cantell K, Gilbert J, Winkle S, Herrin J T, Black P H, Russell P S, Hirsch M S. Controlled clinical trial of prophylactic human-leukocyte interferon in renal transplantation. N Engl J Med. 1979;300:1345–1349. doi: 10.1056/NEJM197906143002401. [DOI] [PubMed] [Google Scholar]
- 62.Chernoff D N, Miner R C, Hoo B S, Shen L P, Kelso R J, Jekic-McMullen D, Lalezari J P, Chou S, Drew W L, Kolberg J A. Quantification of cytomegalovirus DNA in peripheral blood leukocytes by a branched-DNA signal amplification assay. J Clin Microbiol. 1997;35:2740–2744. doi: 10.1128/jcm.35.11.2740-2744.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chou S. Acquisition of donor strains of cytomegalovirus by renal-transplant recipients. N Engl J Med. 1986;314:1418–1423. doi: 10.1056/NEJM198605293142205. [DOI] [PubMed] [Google Scholar]
- 64.Chou S. Cytomegalovirus infection and reinfection transmitted by heart transplantation. J Infect Dis. 1987;155:1054–1056. doi: 10.1093/infdis/155.5.1054. [DOI] [PubMed] [Google Scholar]
- 65.Chou S. Newer methods for diagnosis of cytomegalovirus infection. Rev Infect Dis. 1990;12(Suppl. 7):S727–S736. doi: 10.1093/clinids/12.supplement_7.s727. [DOI] [PubMed] [Google Scholar]
- 66.Chou S, Marousek G, Guentzel S, Follansbee S E, Poscher M E, Lalezari J P, Miner R C, Drew W L. Evolution of mutations conferring multidrug resistance during prophylaxis and therapy for cytomegalovirus disease. J Infect Dis. 1997;176:786–789. doi: 10.1086/517302. [DOI] [PubMed] [Google Scholar]
- 67.Chou S W. Reactivation and recombination of multiple cytomegalovirus strains from individual organ donors. J Infect Dis. 1989;160:11–15. doi: 10.1093/infdis/160.1.11. [DOI] [PubMed] [Google Scholar]
- 68.Chou S W, Scott K M. Rapid quantitation of cytomegalovirus and assay of neutralizing antibody by using monoclonal antibody to the major immediate-early viral protein. J Clin Microbiol. 1988;26:504–507. doi: 10.1128/jcm.26.3.504-507.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chretien J H, McGinniss C G, Muller A. Venereal causes of cytomegalovirus mononucleosis. JAMA. 1977;238:1644–1645. [PubMed] [Google Scholar]
- 70.Cinque P, Vago L, Brytting M, Castagna A, Accordini A, Sundqvist V A, Zanchetta N, Monforte A D, Wahren B, Lazzarin A, et al. Cytomegalovirus infection of the central nervous system in patients with AIDS: diagnosis by DNA amplification from cerebrospinal fluid. J Infect Dis. 1992;166:1408–1411. doi: 10.1093/infdis/166.6.1408. [DOI] [PubMed] [Google Scholar]
- 71.Cofer J B, Morris C A, Sutker W L, Husberg B S, Goldstein R M, Gonwa T A, Klintmalm G B. A randomized double-blind study of the effect of prophylactic immune globulin on the incidence and severity of CMV infection in the liver transplant recipient. Transplant Proc. 1991;23:1525–1527. [PubMed] [Google Scholar]
- 72.Cohen A T, O'Grady J G, Sutherland S, Sallie R, Tan K-C, Williams R. Controlled trial of prophylactic versus therapeutic use of ganciclovir in liver transplantation in adults. J Med Virol. 1993;40:5–9. doi: 10.1002/jmv.1890400103. [DOI] [PubMed] [Google Scholar]
- 73.Colina F, Juca N T, Moreno E, Ballestin C, Farina J, Nevado M, Lumbreras C, Gomez-Sanz R. Histological diagnosis of cytomegalovirus hepatitis in liver allografts. J Clin Pathol. 1995;48:351–357. doi: 10.1136/jcp.48.4.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Compton J. Nucleic acid sequence-based amplification. Nature. 1991;350:91–92. doi: 10.1038/350091a0. [DOI] [PubMed] [Google Scholar]
- 75.Conti D J, Freed B M, Gruber S A, Lempert N. Prophylaxis of primary cytomegalovirus disease in renal transplant patients. A trial of ganciclovir vs. immunoglobulin. Arch Surg. 1994;129:443–447. doi: 10.1001/archsurg.1994.01420280121016. [DOI] [PubMed] [Google Scholar]
- 76.Conti D J, Freed B M, Singh T P, Gallichio M, Gruber S A, Lempert N. Preemptive ganciclovir therapy in cytomegalovirus-seropositive renal transplants recipients. Arch Surg. 1995;130:1217–1221. doi: 10.1001/archsurg.1995.01430110075014. [DOI] [PubMed] [Google Scholar]
- 77.Cooper D K C, Novitzky D, Schlegel V, Muchmore J S, Cucchiara A, Zudhi N. Successful management of symptomatic cytomegalovirus disease with ganciclovir after heart transplantation. J Heart Lung Transplant. 1991;10:656–663. [PubMed] [Google Scholar]
- 78.Cope A V, Sweny P, Sabin C, Rees L, Griffiths P D, Emery V C. Quantity of cytomegalovirus viruria is a major risk factor for cytomegalovirus disease after renal transplantation. J Med Virol. 1997;52(2):200–205. [PubMed] [Google Scholar]
- 79.Couchoud C, Cucherat M, Haugh M, Pouteil-Noble C. Cytomegalovirus prophylaxis with antiviral agents in solid organ transplantation: a meta-analysis. Transplantation. 1998;65:641–647. doi: 10.1097/00007890-199803150-00007. [DOI] [PubMed] [Google Scholar]
- 80.Crumpacker C S. Ganciclovir. N Engl J Med. 1996;335:721–729. doi: 10.1056/NEJM199609053351007. [DOI] [PubMed] [Google Scholar]
- 81.Cunningham R, Harris A, Frankton A, Irving W. Detection of cytomegalovirus using PCR in serum from renal transplant recipients. J Clin Pathol. 1995;48:575–577. doi: 10.1136/jcp.48.6.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dalbello B, Klersy C, Grossi P, Gavazzi A, Ippoliti G, Rinaldi M, Vigano M, Arbustini E. Combined human cytomegalovirus and hepatitis C virus infections increase the risk of allograft vascular disease in heart transplant recipients. Transplant Proc. 1998;30:2086–2090. doi: 10.1016/s0041-1345(98)00583-1. [DOI] [PubMed] [Google Scholar]
- 83.D'Allesandro A M, Pirsch J D, Stratta R J, Sollinger H W, Kalayoglu M, Belzer F O. Successful treatment of severe cytomegalovirus infections with ganciclovir and CMV hyperimmune globulin in liver transplant recipients. Transplant Proc. 1989;21:3560–3561. [PubMed] [Google Scholar]
- 84.Dankner W M, McCutchan J A, Richman D D, Hirata K, Spector S A. Localization of human cytomegalovirus in peripheral blood leukocytes by in situ hybridization. J Infect Dis. 1990;161:31–36. doi: 10.1093/infdis/161.1.31. [DOI] [PubMed] [Google Scholar]
- 85.Davis C, Springmeyer S, Gmerek B. Central nervous system side effects of ganciclovir. N Engl J Med. 1990;322:933–934. doi: 10.1056/NEJM199003293221315. [DOI] [PubMed] [Google Scholar]
- 86.De Armond B. Safety considerations in the use of ganciclovir in immunocompromised patients. Transplant Proc. 1991;23(Suppl. 1):26–29. [PubMed] [Google Scholar]
- 87.Decoene C, Pol A, Dewilde A, Wattre P, Coppin M C, Gosselin B, Stankowiak C, Warembourg H. Relationship between CMV and graft rejection after heart transplantation. Transplant Int. 1996;9(Suppl. 1):S241–S242. doi: 10.1007/978-3-662-00818-8_62. [DOI] [PubMed] [Google Scholar]
- 88.de Hemptinne B, Lamy M E, Salizzoni M, Cornu C, Mostin J, Fevery J, De Groote V, Otte J B. Successful treatment of cytomegalovirus disease with 9-(1,3-dihydroxy-2-propoxymethyl guanine) Transplant Proc. 1988;20:652–655. [PubMed] [Google Scholar]
- 89.Dejong M D, Galasso G J, Gazzard B, Griffiths P D, Jabs D A, Kern E R, Spector S A. Summary of the II International Symposium on Cytomegalovirus. Antiviral Res. 1998;39:141–162. doi: 10.1016/s0166-3542(98)00044-8. [DOI] [PubMed] [Google Scholar]
- 90.de Koning J, van Dorp W T, van Es L A, van't Wout J W, van der Woude F J. Ganciclovir effectively treats cytomegalovirus disease after solid-organ transplantation, even during rejection treatment. Nephrol Dial Transplant. 1992;7:350–356. doi: 10.1093/oxfordjournals.ndt.a092141. [DOI] [PubMed] [Google Scholar]
- 91.Delgado R, Lumbreras C, Alba C, Pedraza M A, Otero J R, Gomez R, Moreno E, Noriega A R, Paya C V. Low predictive value of polymerase chain reaction for diagnosis of CMV disease in liver transplant recipients. J Clin Microbiol. 1992;30:1876–1878. doi: 10.1128/jcm.30.7.1876-1878.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.de Otero J, Gavalda J, Murio E, Vargas V, Calico I, Llopart L, Rossello J, Margarit C, Pahissa A. Cytomegalovirus disease as a risk factor for graft loss and death after orthotopic liver transplantation. Clin Infect Dis. 1998;26:865–870. doi: 10.1086/513949. [DOI] [PubMed] [Google Scholar]
- 93.DesJardin J A, Gibbons L, Cho E H, Supran S E, Falagas M E, Werner B G, Snydman D R. Human herpesvirus 6 reactivation is associated with cytomegalovirus infection and syndromes in kidney transplant recipients at risk for primary cytomegalovirus infection. J Infect Dis. 1998;178:1783–1786. doi: 10.1086/314510. [DOI] [PubMed] [Google Scholar]
- 94.Detwiler R K, Singh H K, Bolin P, Jenette J C. Cytomegalovirus-induced necrotizing and crescentic glomerulonephritis in a renal transplant patient. Am J Kidney Dis. 1998;32:820–824. doi: 10.1016/s0272-6386(98)70139-8. [DOI] [PubMed] [Google Scholar]
- 95.Dickinson B I, Gora-Harper M L, McCraney S A, Gosland M. Studies evaluating high-dose acyclovir, intravenous immune globulin, and cytomegalovirus hyperimmunoglobulin for prophylaxis against cytomegalovirus in kidney transplant recipients. Ann Pharmacother. 1996;30:1452–1464. doi: 10.1177/106002809603001215. [DOI] [PubMed] [Google Scholar]
- 96.DiDomenico N, Link H, Knobel R, Caratsch T, Weschler W, Loewy Z G, Rosenstraus M. COBAS AMPLICOR: fully automated RNA and DNA amplification and detection system for routine diagnostic PCR. Clin Chem. 1996;42:1915–1923. [PubMed] [Google Scholar]
- 97.Dobbins J G, Adler S P, Pass R F, Bale J F, Jr, Grillner L, Stewart J A. The risks and benefits of cytomegalovirus transmission in child day care. Pediatrics. 1994;94:1016–1018. [PubMed] [Google Scholar]
- 98.Dockrell D H, Prada J, Jones M F, Patel R, Badley A D, Harmsen W S, Ilstrup D M, Wiesner R H, Krom R A, Smith T F, Paya C V. Seroconversion to human herpesvirus 6 following liver transplantation is a marker of cytomegalovirus disease. J Infect Dis. 1997;176:1135–1140. doi: 10.1086/514104. [DOI] [PubMed] [Google Scholar]
- 99.Dresdale A R, Kraft P L, Paone G, McFarland T, Levine T B, delBusto R, Lutz S, Drost C, Silverman N A. Reduced incidence and severity of accelerated graft atherosclerosis in cardiac transplant recipients treated with prophylactic antilymphocyte globulin. J Cardiovasc Surg. 1992;33:746–753. [PubMed] [Google Scholar]
- 100.Drew W L, Mintz L, Miner R C, Sands M, Ketterer B. Prevalence of cytomegalovirus infection in homosexual men. J Infect Dis. 1981;143:188–192. doi: 10.1093/infdis/143.2.188. [DOI] [PubMed] [Google Scholar]
- 101.Drouet E, Colimon R, Michelson S, Fourcade N, Niveleau A, Ducerf C, Boibieux A, Chevallier M, Denoyel G. Monitoring levels of human cytomegalovirus DNA in blood after liver transplantation. J Clin Microbiol. 1995;33:389–394. doi: 10.1128/jcm.33.2.389-394.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Drouet E, Michelson S, Denoyel G, Colimon R. Polymerase chain reaction detection of human cytomegalovirus in over 2000 blood specimens correlated with virus isolation and related to urinary virus excretion. J Virol Methods. 1993;45:259–276. doi: 10.1016/0166-0934(93)90112-5. [DOI] [PubMed] [Google Scholar]
- 103.Dummer J S, Ho M, Rabin B, Griffith B P, Hardesty R L, Bahnson H T. The effect of cytomegalovirus and Epstein-Barr virus infection on T lymphocyte subsets in cardiac transplant patients on cyclosporine. Transplantation. 1984;38:433–435. [PubMed] [Google Scholar]
- 104.Duncan S R, Grgurich W F, Iaceno A T, Burckart G J, Yousem S A, Paradis I L, Williams P A, Johnson B A, Griffith B P. A comparison of ganciclovir and acyclovir to prevent cytomegalovirus after lung transplantation. Am J Respir Crit Care Med. 1994;150:146–152. doi: 10.1164/ajrccm.150.1.8025741. [DOI] [PubMed] [Google Scholar]
- 105.Dunn D L, Gillingham K J, Kramer M A, Schmidt W J, Erice A, Balfour H H, Gores P F, Gruessner R W G, Matas A J, Payne W D, Sutherland D E R, Najarian J S. A prospective randomized study of acyclovir versus ganciclovir plus human immune globulin prophylaxis of cytomegalovirus infection after solid organ transplantation. Transplantation. 1994;57:876–884. doi: 10.1097/00007890-199403270-00019. [DOI] [PubMed] [Google Scholar]
- 106.Dunn D L, Mayoral J L, Gillingham K J, Loeffler C M, Brayman K L, Kramer M A, Erice A, Balfour H H, Fletcher C V, Bolman R M, Matas A J, Payne W D, Sutherland D E, Najarian J S. Treatment of invasive cytomegalovirus disease in solid organ transplant patients with ganciclovir. Transplantation. 1991;51:98–106. doi: 10.1097/00007890-199101000-00015. [DOI] [PubMed] [Google Scholar]
- 107.Eckart P, Brouard J, Vabret A, Freymuth F, Guillot M, Ryckelynck J P, Hurault de Ligny B. Detection of human cytomegalovirus in renal transplantation: comparison of four diagnostic methods: DNA in sera by polymerase chain reaction (PCR), DNA in leukocyte by PCR, pp65 leukocytic antigenemia, and viremia. Transplant Proc. 1997;29:2387–2389. doi: 10.1016/s0041-1345(97)00414-4. [DOI] [PubMed] [Google Scholar]
- 108.Eckhoff D E, McGuire B M, Frenette L R, Contreras J L, Hudson S L, Bynon J S. Tacrolimus (FK506) and mycophenolate mofetil combination therapy versus tacrolimus in adult liver transplantation. Transplantation. 1998;65:180–187. doi: 10.1097/00007890-199801270-00006. [DOI] [PubMed] [Google Scholar]
- 109.Egan J J, Barber L, Lomax J, Fox A, Yonan N, Rahman A N, Campbell C S, Deiraniya A K, Carroll K B, Craske J, et al. Detection of human cytomegalovirus antigenaemia: a rapid diagnostic technique for predicting cytomegalovirus infection/pneumonitis in lung and heart transplant recipients. Thorax. 1995;50:9–13. doi: 10.1136/thx.50.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Egan J J, Lomax J, Barber L, Lok S S, Martyszczuk R, Yonan N, Fox A, Deiraniya A K, Turner A J, Woodcock A A. Preemptive treatment for the prevention of cytomegalovirus disease in lung and heart transplant recipients. Transplantation. 1998;65:747–752. doi: 10.1097/00007890-199803150-00026. [DOI] [PubMed] [Google Scholar]
- 111.Ehrnst A. The clinical relevance of different laboratory tests in CMV diagnosis. Scand J Infect Dis Suppl. 1996;100:64–71. [PubMed] [Google Scholar]
- 112.Einsele H, Ehninger G, Steidle M, et al. Polymerase chain reaction to evaluate antiviral therapy for cytomegalovirus disease. Lancet. 1991;338:1170–1172. doi: 10.1016/0140-6736(91)92032-w. [DOI] [PubMed] [Google Scholar]
- 113.Einsele H, Vallbracht A, Jahn G, Kandolf R, Muller C A. Hybridization techniques provide improved sensitivity for HCMV detection and allow quantitation of the virus in clinical samples. J Virol Methods. 1989;26:91–104. doi: 10.1016/0166-0934(89)90077-3. [DOI] [PubMed] [Google Scholar]
- 114.Erice A, Borrell N, Li W Y, Miller W J, Balfour H H. Ganciclovir susceptibilities and analysis of UL97 region in cytomegalovirus (CMV) isolates from bone marrow recipients with CMV disease after antiviral prophylaxis. J Infect Dis. 1998;178:531–534. doi: 10.1086/517467. [DOI] [PubMed] [Google Scholar]
- 115.Erice A, Holm M A, Sanjuan M V, Dunn D L, Gill P C, Balfour H H., Jr Evaluation of CMV-vue antigenemia assay for rapid detection of cytomegalovirus in mixed-leukocyte blood fractions. J Clin Microbiol. 1995;33:1014–1015. doi: 10.1128/jcm.33.4.1014-1015.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Erice A, Jordan M C, Chace B A, Fletcher C, Chinnock B J, Balfour H H. Ganciclovir treatment of cytomegalovirus disease in transplant recipients and other immunocompromised hosts. JAMA. 1987;257:3082–3087. [PubMed] [Google Scholar]
- 117.Eriksson B M, Wirgart B Z, Claesson K, Tufveson G, Magnusson G, Totterman T, Grillner L. A prospective study of rapid methods of detecting cytomegalovirus in the blood of renal transplant recipients in relation to patient and graft survival. Clin Transplant. 1996;10:494–502. [PubMed] [Google Scholar]
- 118.Espy M J, Patel R, Paya C V, Smith T F. Comparison of three methods for extraction of viral nucleic acids from blood cultures. J Clin Microbiol. 1995;33(1):41–44. doi: 10.1128/jcm.33.1.41-44.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Espy M J, Paya C V, Holley K E, Ludwig J, Hermans P F, Wiesner R H, Krom R A, Smith T F. Diagnosis of cytomegalovirus hepatitis by histopathology and in situ hybridization in liver transplantation. Diagn Microbiol Infect Dis. 1991;14:293–296. doi: 10.1016/0732-8893(91)90019-c. [DOI] [PubMed] [Google Scholar]
- 120.Evans M J, Edwards-Spring Y, Myers J, Wendt A, Povinelli D, Amsterdam D, Rittenhouse-Diakun K, Armstrong D, Murray B M, Greenberg S J, Riepenhoff-Talty M. Polymerase chain reaction assays for the detection of cytomegalovirus in organ and bone marrow transplant recipients. Immunol Investig. 1997;26:209–229. doi: 10.3109/08820139709048928. [DOI] [PubMed] [Google Scholar]
- 121.Evans P C, Gray J, Wreghitt T G, Alexander G J M. Optimisation of the polymerase chain reaction and dot-blot hybridisation for detecting cytomegalovirus DNA in urine—comparison with detection of early antigen fluorescent foci and culture. J Virol Methods. 1998;73:41–52. doi: 10.1016/s0166-0934(98)00039-1. [DOI] [PubMed] [Google Scholar]
- 122.Evans P C, Soin A, Wreghitt T G, Alexander G J M. Qualitative and semiquantitative polymerase chain reaction testing for cytomegalovirus DNA in serum allows prediction of CMV related disease in liver transplant recipients. J Clin Pathol. 1998;51:914–921. doi: 10.1136/jcp.51.12.914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Falagas M E, Arbo M, Ruthazer R, Griffith J L, Werner B G, Rohrer R, Freeman R, Lewis W D, Snydman D R. Cytomegalovirus disease is associated with increased cost and hospital length of stay among orthotopic liver transplant recipients. Transplantation. 1997;63:1595–1601. doi: 10.1097/00007890-199706150-00010. [DOI] [PubMed] [Google Scholar]
- 124.Falagas M E, Paya C, Ruthazer R, Badley A, Patel R, Wiesner R, Griffith J, Freeman R, Rohrer R, Werner B G, Snydman D R. Significance of cytomegalovirus for long-term survival after orthotopic liver transplantation—a prospective derivation and validation cohort analysis. Transplantation. 1998;66:1020–1028. doi: 10.1097/00007890-199810270-00010. [DOI] [PubMed] [Google Scholar]
- 125.Falagas M E, Snydman D R. Recurrent cytomegalovirus disease in solid-organ transplant recipients. Transplant Proc. 1995;27(5 Suppl. 1):34–37. [PubMed] [Google Scholar]
- 126.Falagas M E, Snydman D R, Griffith J, Werner B G, Freeman R, Rohrer R. Clinical and epidemiological predictors of recurrent cytomegalovirus disease in orthotopic liver transplant recipients. Boston Center for Liver Transplantation CMVIG Study Group. Clin Infect Dis. 1997;25:314–317. doi: 10.1086/514555. [DOI] [PubMed] [Google Scholar]
- 127.Falagas M E, Snydman D R, Griffith J, Werner B G, Rohrer R, Freeman R, et al. Exposure to cytomegalovirus from the donated organ is a risk factor for bacteremia in orthotopic liver transplant recipients. Clin Infect Dis. 1996;23:468–474. doi: 10.1093/clinids/23.3.468. [DOI] [PubMed] [Google Scholar]
- 128.Falagas M E, Snydman D R, Ruthazer R, Griffith J, Werner B G, Freeman R, Rohrer R. Cytomegalovirus immune globulin (CMVIG) prophylaxis is associated with increased survival after orthotopic liver transplantation. The Boston Center for Liver Transplantation CMVIG Study Group. Clin Transplant. 1997;11:432–437. [PubMed] [Google Scholar]
- 129.Falagas M E, Snydman D R, Ruthazer R, Werner B G, Griffith J. Surveillance cultures of blood, urine, and throat specimens are not valuable for predicting cytomegalovirus disease in liver transplant recipients. Boston Center for Liver Transplantation Cytomegalovirus Immune Globulin Study Group. Clin Infect Dis. 1997;24(5):824–829. doi: 10.1093/clinids/24.5.824. [DOI] [PubMed] [Google Scholar]
- 130.Fassbinder W, Ernst W, Hanke P, Bechstein P B, Scheuermann E H, Schoeppe W. Cytomegalovirus infections after renal transplantation: effect of prophylactic hyperimmunoglobulin. Transplant Proc. 1986;18:1393–1396. [Google Scholar]
- 131.Faulds D, Heel R. Ganciclovir. A review of its antiviral activity, pharmacokinetic properties and therapeutic efficacy in cytomegalovirus infections. Drugs. 1990;39:597–638. doi: 10.2165/00003495-199039040-00008. [DOI] [PubMed] [Google Scholar]
- 132.Fend F, Prior C, Margreiter R, Mikuz G. Cytomegalovirus pneumonitis in heart-lung transplant recipients: histopathology and clinicopathologic considerations. Hum Pathol. 1990;21:918–926. doi: 10.1016/0046-8177(90)90175-5. [DOI] [PubMed] [Google Scholar]
- 133.Fenner T E, Garweg J, Hufert F T, Boehnke M, Scmitz H. Diagnosis of human cytomegalovirus-induced retinitis in human immunodeficiency virus type 1-infected subjects by using the polymerase chain reaction. J Clin Microbiol. 1991;29:2621–2622. doi: 10.1128/jcm.29.11.2621-2622.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Fishburne B C, Mitrani A A, Davis J L. Cytomegalovirus retinitis after cardiac transplantation. Am J Ophthalmol. 1998;125:104–106. doi: 10.1016/s0002-9394(99)80245-1. [DOI] [PubMed] [Google Scholar]
- 135.Fishman J A, Rubin R H. Infection in organ-transplant recipients. N Engl J Med. 1998;338:1741–1751. doi: 10.1056/NEJM199806113382407. [DOI] [PubMed] [Google Scholar]
- 136.Flechner S M, Avery R K, Fisher R, Mastroianni B A, Papajcik D A, O'Malley K J, Goormastic M, Goldfarb D A, Modlin C S, Novick A C. A randomized prospective controlled trial of oral acyclovir versus oral ganciclovir for cytomegalovirus prophylaxis in high-risk kidney transplant recipients. Transplantation. 1998;66:1682–1688. doi: 10.1097/00007890-199812270-00019. [DOI] [PubMed] [Google Scholar]
- 137.Forbes B A. Acquisition of cytomegalovirus infection: an update. Clin Microbiol Rev. 1989;2:204–216. doi: 10.1128/cmr.2.2.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ford-Jones E L, Kitai I, Davis L, Corey M, Farrell H, Petric M, Kyle I, Beach J, Yaffe B, Kelly E, Ryan G, Gold R. Cytomegalovirus infections in Toronto child-care centers: a prospective study of viral excretion in children and seroconversion among day-care providers. Pediatr Infect Dis J. 1996;15:507–514. doi: 10.1097/00006454-199606000-00007. [DOI] [PubMed] [Google Scholar]
- 139.Fox A S, Tolpin M D, Baker A L, Broelsch C E, Whittington P F, Jackson T, Thistlethwaite J R, Stuart F P. Seropositivity in liver transplantation recipients as a predictor of cytomegalovirus disease. J Infect Dis. 1988;157:383–384. doi: 10.1093/infdis/157.2.383. [DOI] [PubMed] [Google Scholar]
- 140.Fox J, Emery V. Quantification of viruses in clinical samples. Rev Med Virol. 1992;2:195–203. [Google Scholar]
- 141.Fox J C, Kidd I M, Griffiths P D, Sweny P, Emery V C. Longitudinal analysis of cytomegalovirus load in renal transplant recipients using a quantitative polymerase chain reaction: correlation with disease. J Gen Virol. 1995;76:309–319. doi: 10.1099/0022-1317-76-2-309. [DOI] [PubMed] [Google Scholar]
- 142.Gaeta A, Nazzari C, Angeletti S, Lazzarini M, Mazzei E, Mancini C. Monitoring for cytomegalovirus infection in organ transplant recipients: analysis of pp65 antigen, DNA and late mRNA in peripheral blood leukocytes. J Med Virol. 1997;53:189–195. doi: 10.1002/(sici)1096-9071(199711)53:3<189::aid-jmv2>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 143.Gane E, Saliba F, Valdecasas G J, J O G, Pescovitz M D, Lyman S, Robinson C A. Randomised trial of efficacy and safety of oral ganciclovir in the prevention of cytomegalovirus disease in liver-transplant recipients. The Oral Ganciclovir International Transplantation Study Group. Lancet. 1997;350:1729–1733. doi: 10.1016/s0140-6736(97)05535-9. [DOI] [PubMed] [Google Scholar]
- 144.Gao S Z, Hunt S A, Schroeder J S, Alderman E L, Hill I R, Stinson E B. Early development of accelerated graft coronary artery disease: risk factors and course. J Am Coll Cardiol. 1996;28:673–679. doi: 10.1016/0735-1097(96)00201-x. [DOI] [PubMed] [Google Scholar]
- 145.Gavalda J, de Otero J, Murio E, Vargas V, Rossello J, Calico I, Margarit C, Pahissa A. Two grams daily of oral acyclovir reduces the incidence of cytomegalovirus disease in CMV-seropositive liver transplant recipients. Transplant Int. 1997;10:462–465. doi: 10.1007/s001470050087. [DOI] [PubMed] [Google Scholar]
- 146.George M J, Snydman D R, Werner B G, Griffith J, Falagas M E, Dougherty N N, Rubin R H. The independent role of cytomegalovirus as a risk factor for invasive fungal disease in orthotopic liver transplant recipients. Boston Center for Liver Transplantation CMVIG-Study Group. Cytogam, MedImmune, Inc. Gaithersburg, Maryland. Am J Med. 1997;103:106–113. doi: 10.1016/s0002-9343(97)80021-6. [DOI] [PubMed] [Google Scholar]
- 147.Georgiev O P, Lal S M, Gupta N, Ross G. Ganciclovir-associated hypercalcemia in a renal transplant patient. Int J Artif Organs. 1998;21:702–704. [PubMed] [Google Scholar]
- 148.Gerdes J C, Spees E K, Fitting K, Hiraki J, Sheehan M, Duda D, Jarvi T, Roehl C, Robertson A D. Prospective study utilizing a quantitative polymerase chain reaction for detection of cytomegalovirus DNA in the blood of renal transplant patients. Transplant Proc. 1993;25:1411–1413. [PubMed] [Google Scholar]
- 149.Gerna G, Baldanti F, Sarasini A, Furione M, Percivalle E, Revello M G, Zipeto D, Zella D. Effect of foscarnet induction treatment on quantitation of human cytomegalovirus (HCMV) DNA in peripheral blood polymorphonuclear leukocytes and aqueous humor of AIDS patients with HCMV retinitis. The Italian Foscarnet Study Group. Antimicrob Agents Chemother. 1994;38:38–44. doi: 10.1128/aac.38.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Gerna G, Baldanti F, Zavattoni M, Sarasini A, Percivalle E, Revello M G. Monitoring of ganciclovir sensitivity of multiple human cytomegalovirus strains coinfecting blood of an AIDS patient by an immediate-early antigen plaque assay. Antiviral Res. 1992;19:333–345. doi: 10.1016/0166-3542(92)90014-v. [DOI] [PubMed] [Google Scholar]
- 151.Gerna G, Furione M, Baldanti F, Sarasini A. Comparative quantitation of human cytomegalovirus DNA in blood leukocytes and plasma of transplant and AIDS patients. J Clin Microbiol. 1994;32:2709–2717. doi: 10.1128/jcm.32.11.2709-2717.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Gerna G, Percivalle E, Baldanti F, Sarasini A, Zavattoni M, Furione M, Torsellini M, Revello M G. Diagnostic significance and clinical impact of quantitative assays for diagnosis of human cytomegalovirus infection/disease in immunocompromised patients. Microbiologica. 1998;21:293–308. [PubMed] [Google Scholar]
- 153.Gerna G, Revello M G, Percivalle E, Morini F. Comparison of different immunostaining techniques and monoclonal antibodies to the lower matrix phosphoprotein (pp65) for optimal quantitation of human cytomegalovirus antigenemia. J Clin Microbiol. 1992;30:1232–1237. doi: 10.1128/jcm.30.5.1232-1237.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Gerna G, Revello M G, Percivalle E, Zavattoni M, Parea M, Battaglia M. Quantification of human cytomegalovirus viremia by using monoclonal antibodies to different viral proteins. J Clin Microbiol. 1990;28:2681–2688. doi: 10.1128/jcm.28.12.2681-2688.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Gerna G, Sarasini A, Percivalle E, Zavattoni M, Baldanti F, Revello M G. Rapid screening for resistance to ganciclovir and foscarnet of primary isolates of human cytomegalovirus from culture-positive blood samples. J Clin Microbiol. 1995;33:738–741. doi: 10.1128/jcm.33.3.738-741.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Gerna G, Zavattoni M, Percivalle E, Grossi P, Torsellini M, Revello M G. Rising levels of human cytomegalovirus (HCMV) antigenemia during initial antiviral treatment of solid-organ transplant recipients with primary HCMV infection. J Clin Microbiol. 1998;36:1113–1116. doi: 10.1128/jcm.36.4.1113-1116.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Gerna G, Zipeto D, Parea M, Revello M G, Silini E, Percivalle E, Zavattoni M, Grossi P, Milanesi G. Monitoring of human cytomegalovirus infections and ganciclovir treatment in heart transplant recipients by determination of viremia, antigenemia, and DNAemia. J Infect Dis. 1991;164:488–498. doi: 10.1093/infdis/164.3.488. [DOI] [PubMed] [Google Scholar]
- 158.Gerna G, Zipeto D, Percivalle E, Parea M, Revello M G, Maccario R, Peri G, Milanesi G. Human cytomegalovirus infection of the major leukocyte subpopulations and evidence for initial viral replication in polymorphonuclear leukocytes from viremic patients. J Infect Dis. 1992;166:1236–1244. doi: 10.1093/infdis/166.6.1236. [DOI] [PubMed] [Google Scholar]
- 159.Giladi M, Lembo A, Johnson B L. Postural epigastric pain—a unique symptom of primary cytomegalovirus gastritis. Infection. 1998;26:234–235. doi: 10.1007/BF02962370. [DOI] [PubMed] [Google Scholar]
- 160.Gleaves C A, Myerson D, Bowden R A, Hackman R C, Meyers J D. Direct detection of cytomegalovirus from bronchoalveolar lavage samples by using a rapid in situ DNA hybridization assay. J Clin Microbiol. 1989;27:2429–2432. doi: 10.1128/jcm.27.11.2429-2432.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Gleaves C A, Smith T F, Shuster E A, Pearson G R. Comparison of standard tube and shell vial cell culture techniques for the detection of cytomegalovirus in clinical specimens. J Clin Microbiol. 1985;21:217–221. doi: 10.1128/jcm.21.2.217-221.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Glenn J. Cytomegalovirus infections following renal transplantation. Rev Infect Dis. 1981;3:1151–1178. doi: 10.1093/clinids/3.6.1151. [DOI] [PubMed] [Google Scholar]
- 163.Gomez E, Aguado S, Melon S, Martinez A, de Ona M, Cimadevilla R, Gorostidi M, Gonzalez E, Alvarez Grande J. A prospective study of the usefulness of rapid diagnostic tests in monitoring cytomegalovirus infection in renal transplants. Transplant Proc. 1992;24:2631–2633. [PubMed] [Google Scholar]
- 164.Gonwa T A. Mycophenolate mofetil for maintenance therapy in kidney transplantation. Clin Transplant. 1996;10:128–130. [PubMed] [Google Scholar]
- 165.Goral S, Ynares C, Dummer S, Helderman J H. Acyclovir prophylaxis for cytomegalovirus disease in high-risk renal transplant recipients: is it effective? Kidney Int Suppl. 1996;57:S62–S65. [PubMed] [Google Scholar]
- 166.Gorensek M, Carey W D, Vogt D, Goormastic M. A multivariate analysis of risk factors for cytomegalovirus infection in liver transplant recipients. Gastroenterology. 1990;98:1326–1332. doi: 10.1016/0016-5085(90)90352-2. [DOI] [PubMed] [Google Scholar]
- 167.Gotti E, Abbate M, Ferrante P, Remuzzi G. Abdominal pain and acute nephritis in a man with a recent renal transplant. J Nephrol. 1998;11:196–198. [PubMed] [Google Scholar]
- 168.Gotti E, Suter F, Baruzzo S, Perani V, Moioli F, Remuzzi G. Early ganciclovir therapy effectively controls viremia and avoids the need for cytomegalovirus (CMV) prophylaxis in renal transplant patients with cytomegalovirus antigenemia. Clin Transplant. 1996;10:550–555. [PubMed] [Google Scholar]
- 169.Gozlan J, Salord J M, Chouaid C, Duvivier C, Picard O, Meyohas M C, Petit J C. Human cytomegalovirus (HCMV) late-mRNA detection in peripheral blood of AIDS patients: diagnostic value for HCMV disease compared with those of viral culture and HCMV DNA detection. J Clin Microbiol. 1993;31:1943–1945. doi: 10.1128/jcm.31.7.1943-1945.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Gozlan J, Salord J M, Roullet E, Baudrimont M, Caburet F, Picard O, Meyohas M C, Duvivier C, Jacomet C, Petit J C. Rapid detection of cytomegalovirus DNA in cerebrospinal fluid of AIDS patients with neurologic disorders. J Infect Dis. 1992;166:1416–1421. doi: 10.1093/infdis/166.6.1416. [DOI] [PubMed] [Google Scholar]
- 171.Grattan M T, Moreno-Cabral C E, Starnes V A, Oyer P E, Stinson E B, Shumway N E. Cytomegalovirus infection is associated with cardiac allograft rejection and atherosclerosis. JAMA. 1989;261:3561–3566. [PubMed] [Google Scholar]
- 172.Green M, Kaufmann M, Wilson J, Reyes J. Comparison of intravenous ganciclovir followed by oral acyclovir with intravenous ganciclovir alone for prevention of cytomegalovirus and Epstein-Barr virus disease after liver transplantation in children. Clin Infect Dis. 1997;25:1344–1349. doi: 10.1086/516139. [DOI] [PubMed] [Google Scholar]
- 173.Grefte A, Van der Giessen M, Van Son W, The T H. Circulating cytomegalovirus (CMV)-infected endothelial cells in patients with an active CMV infection. J Infect Dis. 1993;167:270–277. doi: 10.1093/infdis/167.2.270. [DOI] [PubMed] [Google Scholar]
- 174.Greger B, Vallbracht A, Kurth J, Schareck W D, Muller G H, Hopt U T, Bockhorn H. The clinical value of CMV prophylaxis by CMV hyperimmune serum in the kidney transplant patient. Transplant Proc. 1986;18:1387–1389. [Google Scholar]
- 175.Griffiths P D. Current management of cytomegalovirus disease. J Med Virol. 1993;1993(Suppl. 1):106–111. doi: 10.1002/jmv.1890410521. [DOI] [PubMed] [Google Scholar]
- 176.Griffiths P D. Prophylaxis against CMV infection in transplant patients. J Antimicrob Chemother. 1997;39:299–301. doi: 10.1093/jac/39.3.299. [DOI] [PubMed] [Google Scholar]
- 177.Griffiths P D. Viral complications after transplantation. J Antimicrob Chemother. 1995;36(Suppl. B):91–106. doi: 10.1093/jac/36.suppl_b.91. [DOI] [PubMed] [Google Scholar]
- 178.Griffiths P D, Baboonian C. A prospective study of primary cytomegalovirus infection during pregnancy: final report. Br J Obstet Gynaecol. 1984;91:307–315. doi: 10.1111/j.1471-0528.1984.tb05915.x. [DOI] [PubMed] [Google Scholar]
- 179.Grossi P, Minoli L, Percivalle E, Irish W, Vigano M, Gerna G. Clinical and virological monitoring of human cytomegalovirus infection in 294 heart transplant recipients. Transplantation. 1995;59:847–851. [PubMed] [Google Scholar]
- 180.Grossi P, Revello G, Minoli L, Percivalle E, Zavattoni M, Poma G, Martinelli L, Gerna G. Three-year experience with human cytomegalovirus infections in heart transplant recipients. J Heart Transplant. 1990;9:712–719. [PubMed] [Google Scholar]
- 181.Grundy J E. Virologic and pathogenetic aspects of cytomegalovirus infection. Rev Infect Dis. 1990;12(Suppl. 7):S711–S719. doi: 10.1093/clinids/12.supplement_7.s711. [DOI] [PubMed] [Google Scholar]
- 182.Grundy J E, Ehrnst A, Einsele H, Emery V C, Hebart H, Prentice H G, Ljungman P. A three-center European external quality control study of PCR for detection of cytomegalovirus DNA in blood. J Clin Microbiol. 1996;34:1166–1170. doi: 10.1128/jcm.34.5.1166-1170.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Grundy J E, Lui S F, Super M, Berry N J, Sweny P, Fernando O N, Moorhead J, Griffiths P D. Symptomatic cytomegalovirus infection in seropositive kidney recipients: reinfection with donor virus rather than reactivation of recipient virus. Lancet. 1988;ii:132–135. doi: 10.1016/s0140-6736(88)90685-x. [DOI] [PubMed] [Google Scholar]
- 184.Grundy J E, Shanley J D, Griffiths P D. Is cytomegalovirus interstitial pneumonitis in transplant recipients an immunopathological condition? Lancet. 1987;ii:996–999. doi: 10.1016/s0140-6736(87)92560-8. [DOI] [PubMed] [Google Scholar]
- 185.Gudnason T, Belani K K, Balfour H H. Ganciclovir treatment of cytomegalovirus disease in immunocompromised children. Pediatr Infect Dis J. 1989;8:436–440. doi: 10.1097/00006454-198907000-00006. [DOI] [PubMed] [Google Scholar]
- 186.Guerin C, Pozzetto B, Broyet C, Gaudin O, Berthoux F. Ganciclovir therapy of symptomatic cytomegalovirus infection in renal transplant recipients. Nephrol Dial Transplant. 1989;4:906–910. doi: 10.1093/ndt/4.10.906. [DOI] [PubMed] [Google Scholar]
- 187.Gulizia J M, Kandolf R, Kendall T J, Thieszen S L, Wilson J E, Radio S J, Costanzo M R, Winters G L, Miller L L, McManus B M. Infrequency of cytomegalovirus genome in coronary arteriopathy of human heart allografts. Am J Pathol. 1995;147:461–475. [PMC free article] [PubMed] [Google Scholar]
- 188.Gurevich I, Cunha B A. Non-parenteral transmission of cytomegalovirus in a neonatal intensive care unit. Lancet. 1981;ii:222–224. doi: 10.1016/s0140-6736(81)90473-6. [DOI] [PubMed] [Google Scholar]
- 189.Gutierrez C A, Chaparro C, Krajden M, Winton T, Kesten S. Cytomegalovirus viremia in lung transplant recipients receiving ganciclovir and immune globulin. Chest. 1998;113:924–932. doi: 10.1378/chest.113.4.924. [DOI] [PubMed] [Google Scholar]
- 190.Hamprecht K, Steinmassl M, Einsele H, Jahn G. Discordant detection of human cytomegalovirus DNA from peripheral blood mononuclear cells, granulocytes and plasma—correlation to viremia and HCMV infection. J Clin Virol. 1998;11:125–136. doi: 10.1016/s1386-6532(98)00046-4. [DOI] [PubMed] [Google Scholar]
- 191.Handsfield H H, Chandler S H, Caine V A, Meyers J D, Corey L, Medeiros E, McDougall J K. Cytomegalovirus infection in sex partners: evidence for sexual transmission. J Infect Dis. 1985;151:344–368. doi: 10.1093/infdis/151.2.344. [DOI] [PubMed] [Google Scholar]
- 192.Harbison M A, De-Girolami P C, Jenkins R L, Hammer S M. Ganciclovir therapy of severe cytomegalovirus infections in solid-organ transplant recipients. Transplantation. 1988;46:82–88. doi: 10.1097/00007890-198807000-00015. [DOI] [PubMed] [Google Scholar]
- 193.Heng D, Sharples L D, McNeil K, Stewart S, Wreghitt T, Wallwork J. Bronchiolitis obliterans syndrome: Incidence, natural history, prognosis, and risk factors. J Heart Lung Transplant. 1998;17:1255–1263. [PubMed] [Google Scholar]
- 194.Herbein G, Strasswimmer J, Altieri M, Woehl-Jaegle M L, Wolf P, Obert G. Longitudinal study of human herpesvirus 6 infection in organ transplant recipients. Clin Infect Dis. 1996;22:171–173. doi: 10.1093/clinids/22.1.171. [DOI] [PubMed] [Google Scholar]
- 195.Hertz M I, Jordan C, Savik S K, Fox J M K, Park S, Bolman R M, Doslandmullan B M. Randomized trial of daily versus three-times-weekly prophylactic ganciclovir after lung and heart-lung transplantation. J Heart Lung Transplant. 1998;17:913–920. [PubMed] [Google Scholar]
- 196.Hibberd P L, Snydman D R. Cytomegalovirus infection in organ transplant recipients. Infect Dis Clin North Am. 1995;9:863–877. [PubMed] [Google Scholar]
- 197.Hibberd P L, Tolkoff-Rubin N E, Conti D, Stuart F, Thistlethwaite J R, Neylan J F, Snydman D R, Freeman R, Lorber M I, Rubin R H. Preemptive ganciclovir therapy to prevent cytomegalovirus disease in cytomegalovirus antibody-positive renal transplant recipients. A randomized controlled trial. Ann Intern Med. 1995;123:18–26. doi: 10.7326/0003-4819-123-1-199507010-00002. [DOI] [PubMed] [Google Scholar]
- 198.Hibberd P L, Tolkoff-Rubin N E, Cosimi A B, Schooley R T, Isaacson D, Doran M, Delvecchio A, Delmonico F L, Auchincloss H, Rubin R H. Symptomatic cytomegalovirus disease in the cytomegalovirus antibody seropositive renal transplant recipient treated with OKT3. Transplantation. 1992;53:68–72. doi: 10.1097/00007890-199201000-00013. [DOI] [PubMed] [Google Scholar]
- 199.Hirata M, Terasaki P I, Cho Y W. Cytomegalovirus antibody status and renal transplantation: 1987–1994. Transplantation. 1996;62:34–37. doi: 10.1097/00007890-199607150-00007. [DOI] [PubMed] [Google Scholar]
- 200.Hiyoshi M, Tagawa S, Takubo T, Tanaka K, Nakao T, Higeno Y, Tamura K, Shimaoka M, Fujii A, Higashihata M, Yasui Y, Kim T, Hiraoka A, Tatsumi N. Evaluation of the AMPLICOR CMV test for direct detection of cytomegalovirus in plasma specimens. J Clin Microbiol. 1997;35:2692–2694. doi: 10.1128/jcm.35.10.2692-2694.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ho M. Advances in understanding cytomegalovirus infection after transplantation. Transplant Proc. 1994;26:7–11. [PubMed] [Google Scholar]
- 202.Ho M. Epidemiology of cytomegalovirus infections. Rev Infect Dis. 1990;12(Suppl. 7):S701–S710. doi: 10.1093/clinids/12.supplement_7.s701. [DOI] [PubMed] [Google Scholar]
- 203.Ho S K, Lo C Y, Cheng I K, Chan T M. Rapid cytomegalovirus pp65 antigenemia assay by direct erythrocyte lysis and immunofluorescence staining. J Clin Microbiol. 1998;36:638–640. doi: 10.1128/jcm.36.3.638-640.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Hodge E E. The role of mycophenolate mofetil in clinical renal transplantation. World J Urol. 1996;14:249–255. doi: 10.1007/BF00182076. [DOI] [PubMed] [Google Scholar]
- 205.Hodinka R L. The clinical utility of viral quantitation using molecular methods. Clin Diagn Virol. 1998;10:25–47. doi: 10.1016/s0928-0197(98)00016-6. [DOI] [PubMed] [Google Scholar]
- 206.Hornef M W, Bein G, Fricke L, Steinhoff J, Wagner H J, Hinderer W, Kirchner H. Coincidence of Epstein-Barr virus reactivation, cytomegalovirus infection, and rejection episodes in renal transplant recipients. Transplantation. 1995;60:474–480. doi: 10.1097/00007890-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 207.Hrebinko R, Jordan M L, Dummer J S, Hickey D P, Shapiro R, Vivas C, Starzl T E, Simmons R L, Hakala T R. Ganciclovir for invasive cytomegalovirus infection in renal allograft recipients. Transplant Proc. 1991;23:1346–1347. [PMC free article] [PubMed] [Google Scholar]
- 208.Humar A, Uknis M, Carlone-Jambor C, Gruessner R W, Dunn D L, Matas A. Cytomegalovirus disease recurrence after ganciclovir treatment in kidney and kidney-pancreas transplant recipients. Transplantation. 1999;67:94–97. doi: 10.1097/00007890-199901150-00016. [DOI] [PubMed] [Google Scholar]
- 209.Husni R N, Gordon S M, Longworth D L, Arroliga A, Stillwell P C, Avery R K, Maurer J R, Mehta A, Kirby T. Cytomegalovirus infection is a risk factor for invasive aspergillosis in lung transplant recipients. Clin Infect Dis. 1998;26:753–755. doi: 10.1086/514599. [DOI] [PubMed] [Google Scholar]
- 210.Hutto C, Ricks R, Garvie M, Pass R F. Epidemiology of cytomegalovirus infections in young children: day care vs. home care. Pediatr Infect Dis J. 1985;4:149–152. doi: 10.1097/00006454-198503000-00008. [DOI] [PubMed] [Google Scholar]
- 211.Iberer F, Tscheliessnigg K, Halwachs G, Rehak P, Wasler A, Petutschnigg B, Schreier G, Muller H, Allmayer T, Freigassner M, Prenner G, Hipmair G, Grasser B. Definitions of cytomegalovirus disease after heart transplantation: antigenemia as a marker for antiviral therapy. Transplant Int. 1996;9:236–242. doi: 10.1007/BF00335392. [DOI] [PubMed] [Google Scholar]
- 212.Icenogle T B, Peterson E, Ray G, Minnich L, Copeland J G. DHPG effectively treats CMV infection in heart and heart-lung transplant patients: a preliminary report. J Heart Transplant. 1987;6:199–203. [PubMed] [Google Scholar]
- 213.Imbert-Marcille B M, Cantarovich D, Ferre-Aubineau V, Richet B, Soulillou J P, Billaudel S. Usefulness of DNA viral load quantification for cytomegalovirus disease monitoring in renal and pancreas/renal transplant recipients. Transplantation. 1997;63:1476–1481. doi: 10.1097/00007890-199705270-00018. [DOI] [PubMed] [Google Scholar]
- 214.Jennings R, Green T, Kinghorn G R. Herpesvirus vaccines—an update. Biodrugs. 1998;10:257–264. doi: 10.2165/00063030-199810040-00001. [DOI] [PubMed] [Google Scholar]
- 215.Jensen W A, Rose R M, Hammer S M, Jenkins R L, Bothe A, Benotti P N, Dzik W H, Costello P, Khettry U, Trey C, Eliopoulos G M, Karchmer A W. Pulmonary complications of orthotopic liver transplantation. Transplantation. 1986;42:484–490. doi: 10.1097/00007890-198611000-00008. [DOI] [PubMed] [Google Scholar]
- 216.Jordan M C, Rousseau W E, Noble G R, Steward J A, Chin T D. Association of cervical cytomegaloviruses with venereal disease. N Engl J Med. 1973;288:932–934. doi: 10.1056/NEJM197305032881803. [DOI] [PubMed] [Google Scholar]
- 217.Jordan M L, Hrebinko R L J, Dummer J S, Hickey D P, Shapiro R, Vivas C A, Simmons R L, Starzl T E, Hakala T R. Therapeutic use of ganciclovir for invasive cytomegalovirus infection in cadaveric renal allograft recipients. J Urol. 1992;148:1388–1392. doi: 10.1016/s0022-5347(17)36918-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Jungkind D, Direnzo S, Beavis K G, Silverman N S. Evaluation of automated COBAS AMPLICOR PCR system for detection of several infectious agents and its impact on laboratory management. J Clin Microbiol. 1996;34:2778–2783. doi: 10.1128/jcm.34.11.2778-2783.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Kapasi K, Rice G P. Cytomegalovirus infection of peripheral blood mononuclear cells: effects on interleukin-1 and -2 production and responsiveness. J Virol. 1988;62:3603–3607. doi: 10.1128/jvi.62.10.3603-3607.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Kasdeelen A M, Harmsen M C, Demaar E F, Vanson W J, The T H. A sensitive method for quantifying cytomegalic endothelial cells in peripheral blood from cytomegalovirus-infected patients. Clin Diagn Lab Immunol. 1998;5:622–626. doi: 10.1128/cdli.5.5.622-626.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Kashyap R, Shapiro R, Jordan M, Randhawa P S. The clinical significance of cytomegaloviral inclusions in the allograft kidney. Transplantation. 1999;67:98–103. doi: 10.1097/00007890-199901150-00017. [DOI] [PubMed] [Google Scholar]
- 222.Kasiske B L, Heim-Duthoy K L, Tortorice K L, Ney A L, Odlanc M D, Venkateswara Rao K. Polyvalent immune globulin and cytomegalovirus infection after renal transplantation. Arch Intern Med. 1989;149:2733–2736. [PubMed] [Google Scholar]
- 223.Kathawalla S A, Stillwell P C, Gordon S, Haug M, Perl M, Arroliga A C, Mehta A C, Avery R, Kirby T. Cytomegalovirus infection in seromismatched lung transplant recipients with and without prophylaxis with CMV immunoglobulin. Transplant Proc. 1996;28(6 Suppl. 2):16. [PubMed] [Google Scholar]
- 224.Keating M. Antiviral agents. Mayo Clinic Proc. 1992;67:160–178. doi: 10.1016/s0025-6196(12)61319-6. [DOI] [PubMed] [Google Scholar]
- 225.Reference deleted.
- 226.Keay S, Petersen E, Icenogle T, Zeluff B J, Samo T, Busch D, Newman C L, Buhles W C, Merigan T C. Ganciclovir treatment of serious cytomegalovirus infection in heart and heart-lung transplant recipients. Rev Infect Dis. 1988;10:S563–S572. doi: 10.1093/clinids/10.supplement_3.s563. [DOI] [PubMed] [Google Scholar]
- 227.Keenan R J, Lega M E, Dummer J S, Paradis I L, Dauber J H, Rabinowich H, Yousem S A, Hardesty R L, Griffith B P, Duquesnoy R J, et al. Cytomegalovirus serologic status and postoperative infection correlated with risk of developing chronic rejection after pulmonary transplantation. Transplantation. 1991;51:433–438. doi: 10.1097/00007890-199102000-00032. [DOI] [PubMed] [Google Scholar]
- 228.Kellogg D E, Sninsky J J, Kowk S. Quantitation of HIV-1 proviral DNA relative to cellular DNA by the polymerase chain reaction. Anal Biochem. 1990;189:202–208. doi: 10.1016/0003-2697(90)90108-l. [DOI] [PubMed] [Google Scholar]
- 229.Kendall T J, Wilson J E, Radio S J, Kandolf R, Gulizia J M, Winters G L, Costanzo-Nordin M R, Malcom G T, Thieszen S L, Miller L W, McManus B M. Cytomegalovirus and other herpesvirus: do they have a role in the development of accelerated coronary arterial disease in human heart allografts. J Heart Lung Transplant. 1992;11:S14–S20. [PubMed] [Google Scholar]
- 230.Kendle J B, Fanhavard P. Cidofovir in the treatment of cytomegaloviral disease. Ann Pharmacother. 1998;32:1181–1192. doi: 10.1345/aph.17312. [DOI] [PubMed] [Google Scholar]
- 231.Kidd I M, Fox J C, Pillay D, Charman H, Griffiths P D, Emery V C. Provision of prognostic information in immunocompromised patients by routine application of the polymerase chain reaction for cytomegalovirus. Transplantation. 1993;56:867–871. doi: 10.1097/00007890-199310000-00018. [DOI] [PubMed] [Google Scholar]
- 232.King S M, Superina R, Andrews W, Winston D J, Dunn S, Busuttil R W, Colombani P, Paradis K. Randomized comparison of ganciclovir plus intravenous immune globulin (IVIG) with IVIG alone for prevention of primary cytomegalovirus disease in children receiving liver transplants. Clin Infect Dis. 1997;25:1173–1179. doi: 10.1086/516095. [DOI] [PubMed] [Google Scholar]
- 233.Kini U, Nirmala V. Post-transplantation epididymitis associated with cytomegalovirus. Indian J Pathol Microbiol. 1996;39:151–153. [PubMed] [Google Scholar]
- 234.Kirklin J K, Naftel D C, Levine T B, Bourge R C, Pelletier G B, O'Donnell J, Miller L W, Pritzker M R. Cytomegalovirus after heart transplantation. Risk factors for infection and death: a multi-institutional study. J Heart Lung Transplant. 1994;13:394–404. [PubMed] [Google Scholar]
- 235.Kjellstrom C, Bergstrom T, Martensson G, Ricksten A, Nilsson F, Olofsson S, Collins V P. Relation between polymerase chain reaction findings and morphological changes during cytomegalovirus infection in transplanted lung. Diagn Mol Pathol. 1997;6:267–276. doi: 10.1097/00019606-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 236.Kletzmayr J, Kotzmann H, Popow-Kraupp T, Kovarik J, Klauser R. Impact of high-dose oral acyclovir prophylaxis on cytomegalovirus (CMV) disease in CMV high-risk renal transplant recipients. J Am Soc Nephrol. 1996;7:325–330. doi: 10.1681/ASN.V72325. [DOI] [PubMed] [Google Scholar]
- 237.Klintmalm G, Lonnqvist B, Oberg B, Gahrton G, Lernestedt J-O, Lundgren G, Ringden O, Robert K-H, Wahren B, Groth C-G. Intravenous foscarnet for the treatment of severe cytomegalovirus infection in allograft recipients. Scand J Infect Dis. 1985;17:157–163. doi: 10.3109/inf.1985.17.issue-2.06. [DOI] [PubMed] [Google Scholar]
- 238.Knox K K, Drobyski W R, Carrigan D R. Cytomegalovirus isolate resistant to ganciclovir and foscarnet from a marrow transplant patient. Lancet. 1991;337:1292–1293. doi: 10.1016/0140-6736(91)92965-5. [DOI] [PubMed] [Google Scholar]
- 239.Koskinen P K, Nieminen M S, Marrila S P, Hayry P J, Lautenschlager I T. The correlation between symptomatic CMV infection and CMV antigenemia in heart allograft recipients. Transplantation. 1993;55:547–551. doi: 10.1097/00007890-199303000-00017. [DOI] [PubMed] [Google Scholar]
- 240.Kotsimbos A T, Sinickas V, Glare E M, Esmore D S, Snell G I, Walters E H, Williams T J. Quantitative detection of human cytomegalovirus DNA in lung transplant recipients. Am J Respir Crit Care Med. 1997;156:1241–1246. doi: 10.1164/ajrccm.156.4.96-09106. [DOI] [PubMed] [Google Scholar]
- 241.Kowdley K V, Fawaz K A, Kaplan M M. Extrahepatic biliary stricture associated with cytomegalovirus in a liver transplant recipient. Transplant Int. 1996;9:161–163. doi: 10.1007/BF00336395. [DOI] [PubMed] [Google Scholar]
- 242.Krogsgaard K, Boesgaard S, Aldershvile J, Arendrup H, Mortensen S A, Petterson G. Cytomegalovirus infection rate among heart transplant patients in relation to anti-thymocyte immunoglobulin induction therapy. Copenhagen Heart Transplant Group. Scand J Infect Dis. 1994;26:239–247. doi: 10.3109/00365549409011791. [DOI] [PubMed] [Google Scholar]
- 243.Kroshus T J, Kshettry V R, Savik K, John R, Hertz M I, Bolman R M. Risk factors for the development of bronchiolitis obliterans syndrome after lung transplantation. J Thor Cardiovasc Surg. 1997;114:195–202. doi: 10.1016/S0022-5223(97)70144-2. [DOI] [PubMed] [Google Scholar]
- 244.Kuhn J E, Wendland T, Schafer P, Mohring K, Wieland U, Elgas M, Eggers H J. Monitoring of renal allograft recipients by quantitation of human cytomegalovirus genomes in peripheral blood leukocytes. J Med Virol. 1994;44:398–405. doi: 10.1002/jmv.1890440416. [DOI] [PubMed] [Google Scholar]
- 245.Kulski J K. Quantitation of human cytomegalovirus DNA in leukocytes by end-point titration and duplex polymerase chain reaction. J Virol Methods. 1994;49:195–208. doi: 10.1016/0166-0934(94)90044-2. [DOI] [PubMed] [Google Scholar]
- 246.Kusne S, Manez R, Frye, St B L, George K, Abu-Elmagd K, Tabasco-Menguillon J, Fung J J, Todo S, Rinaldo C, Ehrlich G D. Use of DNA amplification for diagnosis of cytomegalovirus enteritis after intestinal transplantation. Gastroenterology. 1997;112:1121–1128. doi: 10.1016/s0016-5085(97)70122-7. [DOI] [PubMed] [Google Scholar]
- 247.Laifer S A, Ehrlich G D, Huff D S, Balsan M J, Scantlebury V P. Congenital cytomegalovirus infection in offspring of liver transplant recipients. Clin Infect Dis. 1995;20:52–55. doi: 10.1093/clinids/20.1.52. [DOI] [PubMed] [Google Scholar]
- 248.Lam K M, Khan M. Cytomegalovirus in transplantation: new developments. Coronary Artery Dis. 1997;8:305–316. doi: 10.1097/00019501-199705000-00008. [DOI] [PubMed] [Google Scholar]
- 249.Lam K M, Oldenburg N, Khan M A, Gaylore V, Mikhail G W, Strouhal P D, Middeldorp J M, Banner N, Yacoub M. Significance of reverse transcription polymerase chain reaction in the detection of human cytomegalovirus gene transcripts in thoracic organ transplant recipients. J Heart Lung Transplant. 1998;17:555–565. [PubMed] [Google Scholar]
- 250.Landini M P, Mach M. Searching for antibodies specific for human cytomegalovirus: is it diagnostically useful? When and how. Scand J Infect Dis Suppl. 1995;99:18–23. [PubMed] [Google Scholar]
- 251.Landini M P, Michelson S. Human cytomegalovirus proteins. Prog Med Virol. 1988;35:152–185. [PubMed] [Google Scholar]
- 252.Landry M L, Cohen S, Huber K. Comparison of EDTA and acid-citrate-dextrose collection tubes for detection of cytomegalovirus antigenemia and infectivity in leukocytes before and after storage. J Clin Microbiol. 1997;35:305–306. doi: 10.1128/jcm.35.1.305-306.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Landry M L, Ferguson D. Comparison of quantitative cytomegalovirus antigenemia assay with culture methods and correlation with clinical disease. J Clin Microbiol. 1993;31:2851–2856. doi: 10.1128/jcm.31.11.2851-2856.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Lang P, Buisso C, Rostoker G, Ben Maadi A, Fruchaud G, DeForge L, Chopin D, Abbou C, Romano P, Fleury J, Escudier E, Belghiti D, Oncevski A, Duval J, Weil B. DHPG treatment of kidney transplant recipients with severe CMV infection. Transplant Proc. 1989;21:2084–2086. [PubMed] [Google Scholar]
- 255.Lao W C, Lee D, Burroughs A K, Lanzini G, Rolles K, Emery V C, Griffiths P D. Use of polymerase chain reaction to provide prognostic information on human cytomegalovirus disease after liver transplantation. J Med Virol. 1997;51:152–158. [PubMed] [Google Scholar]
- 256.Lautenschlager I, Ahonen J, Eklund B, Hockerstedt K, Salmela K, Isoiemi H, Korsback C, Suni J, Hayry P. Hyperimmune globulin therapy of clinical CMV disease in renal allograft recipients. Transplant Proc. 1989;21:2087–2088. [PubMed] [Google Scholar]
- 257.Lautenschlager I, Hockerstedt K, Linnavuori K, Taskinen E. Human herpesvirus-6 infection after liver transplantation. Clin Infect Dis. 1998;26:702–707. doi: 10.1086/514592. [DOI] [PubMed] [Google Scholar]
- 258.Lee J Y. Cytomegalovirus infection involving the skin in immunocompromised hosts. Am J Clin Pathol. 1989;92:96–100. doi: 10.1093/ajcp/92.1.96. [DOI] [PubMed] [Google Scholar]
- 259.Levy R, Najioullah F, Thouvenot D, Bosshard S, Aymard M, Lina B. Evaluation and comparison of PCR and hybridization methods for rapid detection of cytomegalovirus in clinical samples. J Virol Methods. 1996;62:103–111. doi: 10.1016/s0166-0934(96)02091-5. [DOI] [PubMed] [Google Scholar]
- 260.Lewis R M, Johnson P C, Golden D, Van Buren C T, Kerman R H, Kahan B D. The adverse impact of cytomegalovirus infection on clinical outcome in cyclosporine-prednisone treated renal allograft recipients. Transplantation. 1988;45:353–359. doi: 10.1097/00007890-198802000-00022. [DOI] [PubMed] [Google Scholar]
- 261.Limaye A P, Bowden R A, Myerson D, Boeckh M. Cytomegalovirus disease occurring before engraftment in marrow transplant recipients. Clin Infect Dis. 1997;24:830–835. doi: 10.1093/clinids/24.5.830. [DOI] [PubMed] [Google Scholar]
- 262.Lipson S M, Tseng L F, Kaplan M H, Biondo F X. Antiviral susceptibility testing of cytomegalovirus from primary culture using shell vial assay to detect the late viral antigen. Diagn Microbiol Infect Dis. 1993;17:283–291. doi: 10.1016/0732-8893(93)90037-8. [DOI] [PubMed] [Google Scholar]
- 263.Littler E, Stuart A, Cree M. Human cytomegalovirus UL97 open reading frame encodes a protein that phosphorylates the antiviral analogue ganciclovir. Nature. 1992;358:160–162. doi: 10.1038/358160a0. [DOI] [PubMed] [Google Scholar]
- 264.Ljungman P, Griffiths P. Definitions of cytomegalovirus infection and disease. In: Michelson S, Plotkin S A, editors. Proceedings of the Fourth International Cytomegalovirus Workshop. Multidisciplinary approach to the understanding of cytomegalovirus disease. Paris, France: Elsevier Science Publishers BV; 1993. pp. 233–237. [Google Scholar]
- 265.Ljungman P, Stanley P A. Workshop on cytomegalovirus disease; definitions, clinical severity scores, and new syndromes. Scand J Infect Dis Suppl. 1995;99:87–89. [Google Scholar]
- 266.Lo C Y, Ho K N, Yuen K Y, Lui S L, Li F K, Chan T M, Lo W K, Cheng I K. Diagnosing cytomegalovirus disease in CMV seropositive renal allograft recipients: a comparison between the detection of CMV DNAemia by polymerase chain reaction and antigenemia by CMV pp65 assay. Clin Transplant. 1997;11:286–293. [PubMed] [Google Scholar]
- 267.Locke T J, Odom N J, Tapson J S, Freeman R, McGregor C G A. Successful treatment with trisodium phosphonoformate for primary cytomegalovirus infection after heart transplantation. J Heart Transplant. 1987;6:120–122. [PubMed] [Google Scholar]
- 268.Loning T, Stilo K, Riviere A, Helmchen U. Cytomegalovirus detection in kidney transplants: results obtained from the polymerase chain reaction. Clin Nephrol. 1992;37:78–83. [PubMed] [Google Scholar]
- 269.Lopez-Amado M, Yebra-Pimentel M T, Garcia-Sarandeses A. Cytomegalovirus causing necrotizing laryngitis in a renal and cardiac transplant recipient. Head Neck. 1996;18:455–458. doi: 10.1002/(SICI)1097-0347(199609/10)18:5<455::AID-HED9>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 269a.Lowance D, Neumayer H H, Legendre C M, Squifflet J P, Kovarik J, Brennan P J, Norman D, Mendez R, Keating M R, Coggon G L, Crisp A, Lee I C. Valacyclovir for the prevention of the cytomegalovirus disease after renal transplantation. International Valacyclovir Cytomegalovirus Prophylaxis Transplantation Study Group. N Engl J Med. 1999;340:1462–1470. doi: 10.1056/NEJM199905133401903. [DOI] [PubMed] [Google Scholar]
- 270.Lumbreras C, Otero J R, Herrero J A, Gomez R, Lizasoain M, Aguado J M, Colina F, Garcia I, Moreno E, Noriega A R. Ganciclovir prophylaxis decreases frequency and severity of cytomegalovirus disease in seropositive liver transplant recipients treated with OKT3 monoclonal antibodies. Antimicrob Agents Chemother. 1993;37:2490–2492. doi: 10.1128/aac.37.11.2490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Lurain N S, Ammons H C, Kapell K S, Yeldandi V V, Garrity E R, O'Keefe J P. Molecular analysis of human cytomegalovirus strains from two lung transplant recipients with the same donor. Transplantation. 1996;62:497–502. doi: 10.1097/00007890-199608270-00012. [DOI] [PubMed] [Google Scholar]
- 272.Macartney M, Gane E J, Portmann B, Williams R. Comparison of a new quantitative cytomegalovirus DNA assay with other detection methods. Transplantation. 1997;63:1803–1807. doi: 10.1097/00007890-199706270-00017. [DOI] [PubMed] [Google Scholar]
- 273.MacDonald P A, Keogh A M, Marshman D, Richens D, Harvison A, Kaan A M, Spratt P M. A double-blind placebo-controlled trial of low-dose ganciclovir to prevent cytomegalovirus disease after heart transplantation. J Heart Lung Transplant. 1995;14:32–38. [PubMed] [Google Scholar]
- 274.Madalosso C, de Souza N F, Jr, Ilstrup D M, Wiesner R H, Krom R A. Cytomegalovirus and its association with hepatic artery thrombosis after liver transplantation. Transplantation. 1998;66:294–297. doi: 10.1097/00007890-199808150-00003. [DOI] [PubMed] [Google Scholar]
- 275.Mai M, Nery J, Sutker W, Husberg B, Klintmalm G, Gonwa T. DHPG (ganciclovir) improves survival in CMV pneumonia. Transplant Proc. 1989;21:2263–2265. [PubMed] [Google Scholar]
- 276.Manez R, Breinig M C, Linden P, Wilson J, Torre-Cisneros J, Kusne S, Dummer S, Ho M. Posttransplant lymphoproliferative disease in primary Epstein-Barr virus infection after liver transplantation: the role of cytomegalovirus disease. J Infect Dis. 1997;176:1462–1467. doi: 10.1086/514142. [DOI] [PubMed] [Google Scholar]
- 277.Manez R, Kusne S, Green M, Abu-Elmagd K, Irish W, Reyes J, Furukawa H, Tzakis A, Fung J J, Todo S, et al. Incidence and risk factors associated with the development of cytomegalovirus disease after intestinal transplantation. Transplantation. 1995;59:1010–1014. doi: 10.1097/00007890-199504150-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Manez R, Kusne S, Rinaldo C, Aguado J M, St George K, Grossi P, Frye B, Fung J J, Ehrlich G D. Time to detection of cytomegalovirus (CMV) DNA in blood leukocytes is a predictor for the development of CMV disease in CMV-seronegative recipients of allografts from CMV-seropositive donors following liver transplantation. J Infect Dis. 1996;173:1072–1076. doi: 10.1093/infdis/173.5.1072. [DOI] [PubMed] [Google Scholar]
- 279.Manischewitz J, Quinnan G J, Lane H, Wittek A. Synergistic effect of ganciclovir and foscarnet on cytomegalovirus replication in vitro. Antimicrob Agents Chemother. 1990;34:373–375. doi: 10.1128/aac.34.2.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Marker S C, Simmons R L, Balfour H H J. Cytomegalovirus vaccine in renal allograft recipients. Transplant Proc. 1981;13:117–119. [PubMed] [Google Scholar]
- 281.Markin R S, Langnas A N, Donovan J P, Zetterman R K, Stratta R J. Opportunistic viral hepatitis in liver transplant recipients. Transplant Proc. 1991;23:1520–1521. [PubMed] [Google Scholar]
- 282.Marsano L, Perrillo R P, Flye M W, Hanto D W, Spitzer E D, Thomas J R, Murray P R, Windus D W, Brunt E M, Storch G A. Comparison of culture and serology for the diagnosis of cytomegalovirus infection in kidney and liver transplant recipients. J Infect Dis. 1990;161:454–461. doi: 10.1093/infdis/161.3.454. [DOI] [PubMed] [Google Scholar]
- 283.Marshall G S, Rabalais G P, Stewart J A, Dobbins J G. Cytomegalovirus seroprevalence in women bearing children in Jefferson County, Kentucky. Am J Med Sci. 1993;305:292–296. doi: 10.1097/00000441-199305000-00005. [DOI] [PubMed] [Google Scholar]
- 284.Martin F M, Mañez R, Linden P, Estores D, Torre-Cisneros J, Kusne S, Ondick L, Ptachcinski R, Irish W, Kisor D, Felser I, Rinaldo C, Stieber A, Fung J, Ho M, Simmons R, Starzl T. A prospective randomized trial comparing sequential ganciclovir-high dose acyclovir to high dose acyclovir for prevention of cytomegalovirus disease in adult liver transplant recipients. Transplantation. 1994;58:779–785. doi: 10.1097/00007890-199410150-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Marwick C. First “antisense” drug will treat CMV retinitis. JAMA. 1998;280:871. [PubMed] [Google Scholar]
- 286.Masih A S, Linder J, Shaw B W, Wood R P, Donovan J P, White R, Markin R S. Rapid identification of cytomegalovirus in liver allograft biopsies by in situ hybridization. Am J Surg Pathol. 1988;12:362–367. doi: 10.1097/00000478-198805000-00004. [DOI] [PubMed] [Google Scholar]
- 287.Mathew T H. A blinded, long-term, randomized multicenter study of mycophenolate mofetil in cadaveric renal transplantation—results at three years. Transplantation. 1998;65:1450–1454. doi: 10.1097/00007890-199806150-00007. [DOI] [PubMed] [Google Scholar]
- 288.Mauch T J, Crouch N A, Freese D K, Braunlin E A, Dunn D L, Kashtan C E. Antibody response of pediatric solid organ transplant recipients to immunization against influenza virus. J Pediatr. 1995;127:957–960. doi: 10.1016/s0022-3476(95)70037-4. [DOI] [PubMed] [Google Scholar]
- 289.Mazzulli T, Wood S, Chua R, Walmsley S. Evaluation of the Digene Hybrid Capture System for detection and quantitation of human cytomegalovirus viremia in human immunodeficiency virus-infected patients. J Clin Microbiol. 1996;34:2959–2962. doi: 10.1128/jcm.34.12.2959-2962.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.McCarthy J F, Mccarthy P M, Massad M G, Cook D J, Smedira N G, Kasirajan V, Goormastic M, Hoercher K, Young J B. Risk factors for death after heart transplantation—does a single-center experience correlate with multicenter registries. Ann Thorac Surg. 1998;65:1574–1578. doi: 10.1016/s0003-4975(98)00138-6. [DOI] [PubMed] [Google Scholar]
- 291.McCarthy J M, McLoughlin M G, Shackleton C R, Cameron E C, Yeung C K, Jones E C, Keown P A. Cytomegalovirus epididymitis following renal transplantation. J Urol. 1991;146:417–419. doi: 10.1016/s0022-5347(17)37811-4. [DOI] [PubMed] [Google Scholar]
- 292.McGiffin D C, Savunen T, Kirklin J K, Naftel D C, Bourge R C, Paine T D, White-Williams C, Sisto T, Early L. Cardiac transplant coronary artery disease. A multivariable analysis of pretransplantation risk factors for disease development and morbid events. J Thorac Cardiovasc Surg. 1995;109:1081–1089. doi: 10.1016/S0022-5223(95)70191-5. [DOI] [PubMed] [Google Scholar]
- 293.McNamara D, Di Salvo T, Mathier M, Keck S, Semigran M, Dec G W. Left ventricular dysfunction after heart transplantation: incidence and role of enhanced immunosuppression. J Heart Lung Transplant. 1996;15:506–515. [PubMed] [Google Scholar]
- 294.McSharry J J, Lurain N S, Drusano G L, Landay A L, Notka M, Ogorman M R G, Weinberg A, Shapiro H M, Reichelderfer P S, Crumpacker C S. Rapid ganciclovir susceptibility assay using flow cytometry for human cytomegalovirus clinical isolates. Antimicrob Agents Chemother. 1998;42:2326–2331. doi: 10.1128/aac.42.9.2326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.McSharry J M, Lurain N S, Drusano G L, Landay A, Manischewitz J, Nokta M, M. O G, Shapiro H M, Weinberg A, Reichelderfer P, Crumpacker C. Flow cytometric determination of ganciclovir susceptibilities of human cytomegalovirus clinical isolates. J Clin Microbiol. 1998;36:958–964. doi: 10.1128/jcm.36.4.958-964.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Megison S M, Andrews W S. Combination therapy with ganciclovir and intravenous IgG for cytomegalovirus infections in pediatric liver transplant recipients. Transplantation. 1991;52:151–154. [PubMed] [Google Scholar]
- 297.Mendez J, Espy M, Smith T F, Wilson J, Wiesner R, Paya C V. Clinical significance of viral load in the diagnosis of cytomegalovirus disease after liver transplantation. Transplantation. 1998;65:1477–1481. doi: 10.1097/00007890-199806150-00012. [DOI] [PubMed] [Google Scholar]
- 298.Mendez J C, Espy M J, Smith T F, Wilson J A, Paya C V. Evaluation of PCR primers for early diagnosis of cytomegalovirus infection following liver transplantation. J Clin Microbiol. 1998;36:526–530. doi: 10.1128/jcm.36.2.526-530.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Merigan T C, Renlund D G, Keay S, Bristow M R, Starnes V, O'Connell J B, Resta S, Dunn D, Gamberg P, Ratkovec R M, Richenbacher W E, Millar R C, DuMond C, DeArmond B, Sullivan V, Cheney T, Buhles W, Stinson E B. A controlled trial of ganciclovir to prevent cytomegalovirus disease after heart transplantation. N Engl J Med. 1992;326:1182–1186. doi: 10.1056/NEJM199204303261803. [DOI] [PubMed] [Google Scholar]
- 300.Metselaar H J, Rothbarth P H, Brouwer R M, Wentimg G J, Jeekel J, Weimar W. Prevention of cytomegalovirus-related death by passive immunization. A double-blind placebo-controlled study in kidney transplant recipients treated by rejection. Transplantation. 1989;48:264–266. doi: 10.1097/00007890-198908000-00016. [DOI] [PubMed] [Google Scholar]
- 301.Metselaar H J, Weimar W. Cytomegalovirus infection and renal transplantation. J Antimicrob Chemother. 1989;23(Suppl. E):37–47. doi: 10.1093/jac/23.suppl_e.37. [DOI] [PubMed] [Google Scholar]
- 302.Meyer-Konig U, Serr A, von Laer D, Kirste G, Wolff C, Haller O, Neumann-Haefelin D, Hufert F T. Human cytomegalovirus immediate early and late transcripts in peripheral blood leukocytes: diagnostic value in renal transplant recipients. J Infect Dis. 1995;171:705–709. doi: 10.1093/infdis/171.3.705. [DOI] [PubMed] [Google Scholar]
- 303.Mintz L, Drew W L, Miner R C, Braff E H. Cytomegalovirus infections in homosexual men. An epidemiological study. Ann Intern Med. 1983;99:326–329. doi: 10.7326/0003-4819-99-3-326. [DOI] [PubMed] [Google Scholar]
- 304.Mitchell S M, Fox J D, Tedder R S, Gazzard B G, Lightman S. Vitreous fluid sampling and viral genome detection for the diagnosis of viral retinitis in patients with AIDS. J Med Virol. 1994;43:336–340. doi: 10.1002/jmv.1890430404. [DOI] [PubMed] [Google Scholar]
- 305.Monte P D, Lazzarotto T, Ripalti A, Landini M P. Human cytomegalovirus infection: a complex diagnostic problem in which molecular biology has induced a rapid evolution. Intervirology. 1996;39:193–203. doi: 10.1159/000150495. [DOI] [PubMed] [Google Scholar]
- 306.Moreso F, Seron D, Morales J M, Cruzado J M, Gilvernet S, Perez J L, Fulladosa X, Andres A, Grinyo J M. Incidence of leukopenia and cytomegalovirus disease in kidney transplants treated with mycophenolate mofetil combined with low cyclosporine and steroid doses. Clin Transplant. 1998;12:198–205. [PubMed] [Google Scholar]
- 307.Moudgil A, Germain B M, Nast C C, Toyoda M, Strauss F G, Jordan S C. Ureteritis and cholecystitis: two unusual manifestations of cytomegalovirus disease in renal transplant recipients. Transplantation. 1997;64:1071–1073. doi: 10.1097/00007890-199710150-00021. [DOI] [PubMed] [Google Scholar]
- 308.Muir S W, Murray J, Farquharson M A, Wheatley D J, McPhaden A R. Detection of cytomegalovirus in upper gastrointestinal biopsies from heart transplant recipients—comparison of light microscopy, immunocytochemistry, in situ hybridisation, and nested PCR. J Clin Pathol. 1998;51:807–811. doi: 10.1136/jcp.51.11.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Muldoon J, O'Riordan K, Rao S, Abecassis M. Ischemic colitis secondary to venous thrombosis. A rare presentation of cytomegalovirus vasculitis following renal transplantation. Transplantation. 1996;61:1651–1653. doi: 10.1097/00007890-199606150-00018. [DOI] [PubMed] [Google Scholar]
- 310.Murph J R, Bale J F., Jr The natural history of acquired cytomegalovirus infection among children in group day care. Am J Dis Child. 1988;142:843–846. doi: 10.1001/archpedi.1988.02150080049020. [DOI] [PubMed] [Google Scholar]
- 311.Murray B M, Amsterdam D, Gray V, Myers J, Gerbasi J, Venuto R. Monitoring and diagnosis of cytomegalovirus infection in renal transplantation. J Am Soc Nephrol. 1997;8:1448–1457. doi: 10.1681/ASN.V891448. [DOI] [PubMed] [Google Scholar]
- 312.Musiani M, Roda A, Zerbini M, Pasini P, Gentilomi G, Gallinella G, Venturoli S. Chemiluminescent in situ hybridization for the detection of cytomegalovirus DNA. Am J Pathol. 1996;148:1105–1112. [PMC free article] [PubMed] [Google Scholar]
- 313.Mutimer D. CMV infection of transplant recipients. J Hepatol. 1996;25:259–269. doi: 10.1016/s0168-8278(96)80083-3. [DOI] [PubMed] [Google Scholar]
- 314.Mutimer D, Matyi-Toth A, Elias E, Shaw J, K O D, Kilgariff H, Neuberger J, Gunson B, McMaster P, Stalhandske P. Quantitation of cytomegalovirus in the blood of liver transplant recipients. Liver Transplant Surg. 1995;1:395–400. doi: 10.1002/lt.500010611. [DOI] [PubMed] [Google Scholar]
- 315.Mutimer D, Matyi-Toth A, Shaw J, Elias E, K O D, Stalhandske P. Patterns of viremia in liver transplant recipients with symptomatic cytomegalovirus infection. Transplantation. 1997;63:68–73. doi: 10.1097/00007890-199701150-00013. [DOI] [PubMed] [Google Scholar]
- 316.Mutimer D, Mirza D, Shaw J, K O D, Elias E. Enhanced (cytomegalovirus) viral replication associated with septic bacterial complications in liver transplant recipients. Transplantation. 1997;63:1411–1415. doi: 10.1097/00007890-199705270-00007. [DOI] [PubMed] [Google Scholar]
- 317.Mutimer D J, Shaw J, K O D, Elias E. Enhanced (cytomegalovirus) viral replication after transplantation for fulminant hepatic failure. Liver Transplant Surg. 1997;3:506–512. doi: 10.1002/lt.500030505. [DOI] [PubMed] [Google Scholar]
- 318.Myers J B, Amsterdam D. The laboratory diagnosis of cytomegalovirus infections. Immunol Investig. 1997;26:383–394. doi: 10.3109/08820139709022694. [DOI] [PubMed] [Google Scholar]
- 319.Nakazato P Z, Burns W, Moore P, Garcia-Kennecy R, Cox K, Esquivel C. Viral prophylaxis in hepatic transplantation: preliminary report of a randomized trial of acyclovir and ganciclovir. Transplant Proc. 1993;25:1935–1937. [PubMed] [Google Scholar]
- 320.Nankivel B J, Malouf M A, Russ G R, Barclay P, Glanville A R, Allen R D M, Oconnell P J, Chapman J R. Maintenance therapy with oral ganciclovir after treatment of cytomegalovirus infection. Clin Transplant. 1998;12:270–273. [PubMed] [Google Scholar]
- 321.Neyts J, Andrei G, De Clercq E. The novel immunosuppressive agent mycophenolate mofetil markedly potentiates the antiherpesvirus activities of acyclovir, ganciclovir, and penciclovir in vitro and in vivo. Antimicrob Agents Chemother. 1998;42:216–222. doi: 10.1128/aac.42.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Nicholson M L, Veitch P S, Donnelly P K, Flower A J E, Bell P R F. Treatment of renal transplant-associated cytomegalovirus infection with ganciclovir. Transplant Proc. 1990;22:1811–1812. [PubMed] [Google Scholar]
- 323.Niubo J, Perez J L, Martinez-Lacasa J T, Garcia A, Roca J, Fabregat J, Gil-Vernet S, Martin R. Association of quantitative cytomegalovirus antigenemia with symptomatic infection in solid organ transplant patients. Diagn Microbiol Infect Dis. 1996;24:19–24. doi: 10.1016/0732-8893(95)00248-0. [DOI] [PubMed] [Google Scholar]
- 324.Noble S, Faulds D. Ganciclovir: An update of its use in the prevention of cytomegalovirus infection and disease in transplant recipients. Drugs. 1998;56:115–146. doi: 10.2165/00003495-199856010-00012. [DOI] [PubMed] [Google Scholar]
- 325.O'Hair D P, Johnson C P, Roza A M, Adams M B. Treatment of transplant rejection in the presence of cytomegalovirus viremia. Transplant Proc. 1990;22:1815–1817. [PubMed] [Google Scholar]
- 326.O'Grady J G, Sutherland S, Harvey F, Calne R Y, Alexander G J M, Donaldson P T, Portmann B, Williams R. Cytomegalovirus infection and donor/recipients HLA antigens: interdependent co-factors in pathogenesis of vanishing bile duct syndrome after liver transplantation. Lancet. 1988;ii:302–305. doi: 10.1016/s0140-6736(88)92356-2. [DOI] [PubMed] [Google Scholar]
- 327.Osman H K, Peiris J S, Taylor C E, Warwicker P, Jarrett R F, Madeley C R. “Cytomegalovirus disease” in renal allograft recipients: is human herpesvirus 7 a co-factor for disease progression? J Med Virol. 1996;48:295–301. doi: 10.1002/(SICI)1096-9071(199604)48:4<295::AID-JMV1>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 328.Paar D P, Pollard R B. Immunotherapy of CMV infections. Adv Exp Med Biol. 1996;394:145–151. doi: 10.1007/978-1-4757-9209-6_15. [DOI] [PubMed] [Google Scholar]
- 329.Page M J, Dreese J C, Poritz L S, Koltun W A. Cytomegalovirus enteritis: a highly lethal condition requiring early detection and intervention. Dis Colon Rectum. 1998;41:619–623. doi: 10.1007/BF02235271. [DOI] [PubMed] [Google Scholar]
- 330.Palestine A G. Clinical aspects of cytomegalovirus retinitis. Rev Infect Dis. 1988;10:S515–S521. doi: 10.1093/clinids/10.supplement_3.s515. [DOI] [PubMed] [Google Scholar]
- 331.Pass R F, Hutto C. Group day care and cytomegaloviral infections of mothers and children. Rev Infect Dis. 1986;8:599–605. doi: 10.1093/clinids/8.4.599. [DOI] [PubMed] [Google Scholar]
- 332.Pass R F, Whitley R J, Diethelm A G, Whelchel J D, Reynolds D W, Alford C A. Cytomegalovirus infection in patients with renal transplants: potentiation by antithymocyte globulin and an incompatible graft. J Infect Dis. 1980;142:9–17. doi: 10.1093/infdis/142.1.9. [DOI] [PubMed] [Google Scholar]
- 333.Patel R, Klein D W, Espy M J, Harmsen W S, Ilstrup D M, Paya C V, Smith T F. Optimization of the detection of cytomegalovirus viremia by shell vial in transplantation recipients. J Clin Microbiol. 1995;33:2984–2986. doi: 10.1128/jcm.33.11.2984-2986.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Patel R, Paya C V. Infections in solid-organ transplant recipients. Clin Microbiol Rev. 1997;10:86–124. doi: 10.1128/cmr.10.1.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334a.Patel R, Paya C V. Cytomegalovirus infection and disease in solid organ transplant recipients. In: Bowden R A, Ljungman P, Paya C V, editors. Transplant infections. Philadelphia, Pa: Lippincott-Raven Publishers; 1998. [Google Scholar]
- 335.Patel R, Smith T F, Espy M, Portela D, Wiesner R H, Krom R A F, Paya C V. A prospective comparison of molecular diagnostic techniques for the early detection of cytomegalovirus in liver transplant recipients. J Infect Dis. 1995;171:1010–1014. doi: 10.1093/infdis/171.4.1010. [DOI] [PubMed] [Google Scholar]
- 336.Patel R, Smith T F, Espy M J, Wiesner R H, Krom R A F, Portela D, Paya C V. Detection of cytomegalovirus DNA in sera of liver transplant recipients. J Clin Microbiol. 1994;32:1431–1434. doi: 10.1128/jcm.32.6.1431-1434.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336a.Patel R, Snydman D R, Rubin R H, Ho M, Pescovitz M, Martin M, Paya C V. Cytomegalovirus prophylaxis in solid organ transplant recipients. Transplantation. 1996;61:1279–1289. doi: 10.1097/00007890-199605150-00001. [DOI] [PubMed] [Google Scholar]
- 337.Patterson J W, Broeker A H, Kornstein M J, Mills A S. Cutaneous cytomegalovirus infection in a liver transplant recipient. Am J Dermatopathol. 1988;10:524–530. doi: 10.1097/00000372-198812000-00009. [DOI] [PubMed] [Google Scholar]
- 338.Paya C V, Hermans P E, A. W J, Smith T F, Anhalt J P, Wiesner R H, Krom R A F. Incidence, distribution, and outcome of episodes of infection in 100 orthotopic liver transplantations. Mayo Clin Proc. 1989;64:555–564. doi: 10.1016/s0025-6196(12)65561-x. [DOI] [PubMed] [Google Scholar]
- 339.Paya C V, Hermans P E, Smith T F, Rakela J, Wiesner R H, Krom R A F, Torres V E, Sterioff S, Wilkowske C J. Efficacy of ganciclovir in liver and kidney transplant recipients with severe cytomegalovirus infection. Transplantation. 1988;46:229–234. doi: 10.1097/00007890-198808000-00008. [DOI] [PubMed] [Google Scholar]
- 340.Paya C V, Hermans P E, Wiesner R H, Ludwig J, Smith T F, Rakela J, Krom R A F. Cytomegalovirus hepatitis in liver transplantation: Prospective analysis of 93 consecutive orthotopic liver transplantations. J Infect Dis. 1989;160:752–758. doi: 10.1093/infdis/160.5.752. [DOI] [PubMed] [Google Scholar]
- 341.Paya C V, Holley K E, Wiesner R H, Balasubramaniam K, Smith T F, Espy M J, Ludwig J, Batts K P, Hermans P E, Krom R A. Early diagnosis of cytomegalovirus hepatitis in liver transplant recipients: role of immunostaining, DNA hybridization and culture of hepatic tissue. Hepatology. 1990;12:119–126. doi: 10.1002/hep.1840120119. [DOI] [PubMed] [Google Scholar]
- 342.Paya C V, Marin E, Keating M, Dickson R, Porayko M, Wiesner R. Solid organ transplantation: results and implications of acyclovir use in liver transplants. J Med Virol. 1993;1:123–127. doi: 10.1002/jmv.1890410524. [DOI] [PubMed] [Google Scholar]
- 343.Paya C V, Smith T F, Ludwig J, Hermans P E. Rapid shell vial culture and tissue histology compared with serology for the rapid diagnosis of cytomegalovirus infection in liver transplantation. Mayo Clinic Proc. 1989;64:670–675. doi: 10.1016/s0025-6196(12)65346-4. [DOI] [PubMed] [Google Scholar]
- 344.Paya C V, Wiesner R H, Herman P E, Larson-Keller J J, Ilstrup D M, Krom R A F, Rettke S, Smith T F. Risk factors for cytomegalovirus and severe bacterial infections following liver transplantation: a prospective multivariate time-dependent analysis. J Hepatol. 1993;18:185–195. doi: 10.1016/s0168-8278(05)80245-4. [DOI] [PubMed] [Google Scholar]
- 345.Paya C V, Wold A D, Smith T F. Detection of cytomegalovirus infections in specimens other than urine by the shell vial assay and conventional tube cell cultures. J Clin Microbiol. 1987;25:755–757. doi: 10.1128/jcm.25.5.755-757.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Pehlivanoglu E, Amant M E, Jenkins R L, Bothe A, Benotti P N, Dzik W H, Costello P, Khettry U, Trey C, Eliopoulos G M, Karmel A W. Severe cytomegalovirus infection and immunosuppressive therapy in pediatric liver transplantation. Turk J Pediatr. 1990;32:3–11. [PubMed] [Google Scholar]
- 347.Peiris J S, Taylor C E, Main J, Graham K, Madeley C R. Diagnosis of cytomegalovirus (CMV) disease in renal allograft recipients: the role of semiquantitative polymerase chain reaction (PCR) Nephrol Dial Transplant. 1995;10:1198–1205. [PubMed] [Google Scholar]
- 348.Percivalle E, Revello M G, Vago L, Morini F, Gerna G. Circulating endothelial giant cells permissive for human cytomegalovirus (HCMV) are detected in disseminated HCMV infections with organ involvement. J Clin Investig. 1993;92:663–670. doi: 10.1172/JCI116635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Pescovitz M D, Pruett T L, Gonwa T, Brook B, McGory R, Wicker K, Griffy K, Robinson C A, Jung D. Oral ganciclovir dosing in transplant recipients and dialysis patients based on renal function. Transplantation. 1998;66:1104–1107. doi: 10.1097/00007890-199810270-00023. [DOI] [PubMed] [Google Scholar]
- 350.Petri W A., Jr Infections in heart transplant recipients. Clin Infect Dis. 1994;18:141–148. doi: 10.1093/clinids/18.2.141. [DOI] [PubMed] [Google Scholar]
- 351.Pillay D, Ali A A, Liu S F, Kops E, Sweny P, Griffiths P D. The prognostic significance of positive CMV cultures during surveillance of renal transplant recipients. Transplantation. 1993;56:103–108. doi: 10.1097/00007890-199307000-00019. [DOI] [PubMed] [Google Scholar]
- 352.Pillay D, Charman H, Burroughs A K, Smith M, Rolles K, Griffiths P D. Surveillance for CMV infection in orthotopic liver transplant recipients. Transplantation. 1992;53:1261–1265. doi: 10.1097/00007890-199206000-00018. [DOI] [PubMed] [Google Scholar]
- 353.Plotkin S A, Friedman H M, Fleisher G R, Dafoe D C, Grossman R A, Smiley M L, Starr S E, Wlodaver C, Friedman A D, Barker C F. Towne-vaccine-induced prevention of cytomegalovirus disease after renal transplants. Lancet. 1984;i:528–530. doi: 10.1016/s0140-6736(84)90930-9. [DOI] [PubMed] [Google Scholar]
- 354.Plotkin S A, Higgins R, Kurtz J B, Morris P J, Campbell D A, Jr, Shope T C, Spector S A, Dankner W M. Multicenter trial of Towne strain attenuated virus vaccine in seronegative renal transplant recipients. Transplantation. 1994;58:1176–1178. [PubMed] [Google Scholar]
- 355.Plotkin S A, Starr S E, Friedman H M, Brayman K, Harris S, Jackson S, Tustin N B, Grossman R, Dafoe D, Barker C. Effect of Towne live virus vaccine on cytomegalovirus disease after renal transplant. Ann Intern Med. 1991;114:525–531. doi: 10.7326/0003-4819-114-7-525. [DOI] [PubMed] [Google Scholar]
- 356.Plotkin S A, Starr S E, Friedman H M, Gonczol E, Brayman K. Vaccines for the prevention of human cytomegalovirus infection. Rev Infect Dis. 1990;12(Suppl. 7):S827–S838. doi: 10.1093/clinids/12.supplement_7.s827. [DOI] [PubMed] [Google Scholar]
- 357.Podlech J, Holtappels R, Wirtz N, Steffens H P, Reddehase M J. Reconstitution of CD8 T cells is essential for the prevention of multiple-organ cytomegalovirus histopathology after bone marrow transplantation. J Gen Virol. 1998;79:2099–2104. doi: 10.1099/0022-1317-79-9-2099. [DOI] [PubMed] [Google Scholar]
- 358.Pomerance A, Madden B, Burke M M, Yacoub M H. Clinical significance of viral load in the diagnosis of cytomegalovirus disease after liver transplantation. Transplantation. 1998;65:1477–1481. doi: 10.1097/00007890-199806150-00012. [DOI] [PubMed] [Google Scholar]
- 359.Portela D, Patel R, Larson-Keller J, Ilstrup D, Steers J, Wiesner R, Krom R, Paya C. OKT3 treatment for allograft rejection is a risk factor for cytomegalovirus disease in liver transplantation. J Infect Dis. 1995;171:1014–1018. doi: 10.1093/infdis/171.4.1014. [DOI] [PubMed] [Google Scholar]
- 360.Pouria S, State O I, Wong W, Hendry B M. CMV infection is associated with transplant renal artery stenosis. Q J Med. 1998;91:185–189. doi: 10.1093/qjmed/91.3.185. [DOI] [PubMed] [Google Scholar]
- 361.Pouteil-Noble C, Ecochard R, Landrivon G, Donia-Maged A, Tardy J C, Bosshard S, Colon S, Betuel H, Aymard M, Touraine J L. Cytomegalovirus infection—an etiological factor for rejection? A prospective study in 242 renal transplant patients. Transplantation. 1993;55:851–857. doi: 10.1097/00007890-199304000-00032. [DOI] [PubMed] [Google Scholar]
- 362.Power C, Poland S D, Kassim K H, Kaufman J C E, Rice G P A. Encephalopathy in liver transplantation: neuropathology and CMV infection. Can J Neurol Sci. 1990;17:378–381. doi: 10.1017/s0317167100030912. [DOI] [PubMed] [Google Scholar]
- 363.Prix L, Maierl J, Jahn G, Hamprecht K. A simplified assay for screening of drug resistance of cell-associated cytomegalovirus strains. J Clin Virol. 1998;11:29–37. doi: 10.1016/s0928-0197(98)00043-9. [DOI] [PubMed] [Google Scholar]
- 364.Pucci A, Ghisetti V, Donegani E, Barbui A, David E, Fortunato M, Papandrea C, Pansini S, Zattera G, di Summa M, et al. Histologic and molecular diagnosis of myocardial human cytomegalovirus infection after heart transplantation. J Heart Lung Transplant. 1994;13:1072–1080. [PubMed] [Google Scholar]
- 365.Quinnan G V, Jr, Kirmani N, Rook A H, Manischewitz J F, Jackson L, Moreschi G, Santos G W, Saral R, Burns W H. Cytotoxic t cells in cytomegalovirus infection: HLA-restricted T-lymphocyte and non-T-lymphocyte cytotoxic responses correlate with recovery from cytomegalovirus infection in bone-marrow-transplant recipients. N Engl J Med. 1982;307:7–13. doi: 10.1056/NEJM198207013070102. [DOI] [PubMed] [Google Scholar]
- 366.Rakela J, Wiesner R H, Taswell H F, Smith T F, Perkins J D, Krom R A F. Incidence of cytomegalovirus infection and its relationship to donor-recipient serologic status in liver transplantation. Transplant Proc. 1987;19:2399–2402. [PubMed] [Google Scholar]
- 367.Rancewicz Z, Halama G, Smogorzewski M, Durlik M, Rowinska D, Rao M, Juskow J, Wyzgal J. The usefulness of hyperimmune globulin for treatment of overt cytomegalovirus infection in allograft recipients. Transplant Proc. 1990;22:1818–1819. [PubMed] [Google Scholar]
- 368.Randhawa P S, Manez R, Frye B, Ehrlich G D. Circulating immediate-early mRNA in patients with cytomegalovirus infections after solid organ transplantation. J Infect Dis. 1994;170:1264–1267. doi: 10.1093/infdis/170.5.1264. [DOI] [PubMed] [Google Scholar]
- 369.Ratnamohan V M, Chapman J, Howse H, Bovington K, Robertson P, Byth K, Allen R, Cunningham A L. Cytomegalovirus and human herpesvirus 6 both cause viral disease after renal transplantation. Transplantation. 1998;66:877–882. doi: 10.1097/00007890-199810150-00011. [DOI] [PubMed] [Google Scholar]
- 370.Reed E C, Wolford J L, Kopecky K J, Lilleby K E, Dandliker P S, Todaro J L, McDonald G B, Meyers J D. Ganciclovir for the treatment of cytomegalovirus gastroenteritis in bone marrow transplant patients. Ann Intern Med. 1990;112:505–510. doi: 10.7326/0003-4819-112-7-505. [DOI] [PubMed] [Google Scholar]
- 371.Reina J, Blanco I, Munar M. Determination of the number of blood samples needed for optimal detection of cytomegalovirus viremia in immunocompromised patients using a shell-vial assay. Eur J Clin Microbiol Infect Dis. 1997;16:318–321. doi: 10.1007/BF01695639. [DOI] [PubMed] [Google Scholar]
- 372.Reina J, Saurina J, Fernandezbaca V, Blanco I, Munar M. An increase in the number of polymorphonuclear leukocytes inoculated on shell-vial culture increases the sensitivity of this assay in the detection of cytomegalovirus in the blood of immunocompromised patients. Diagn Microbiol Infect Dis. 1998;31:425–428. doi: 10.1016/s0732-8893(98)00028-5. [DOI] [PubMed] [Google Scholar]
- 373.Reinke P, Fietze E, Ode-Hakim S, Prosch S, Lippert J, Ewert R, Volk H D. Late-acute renal allograft rejection and symptomless cytomegalovirus infection. Lancet. 1994;344:1737–1738. doi: 10.1016/s0140-6736(94)92887-8. [DOI] [PubMed] [Google Scholar]
- 374.Reusser P, Riddell S R, Meyers J D, Greenberg P D. Cytotoxic T-lymphocyte response to cytomegalovirus after human allogeneic bone marrow transplantation: pattern of recovery and correlation with cytomegalovirus infection and disease. Blood. 1991;78:1373–1380. [PubMed] [Google Scholar]
- 375.Richardson W, Colvin R B, Cheeseman S H, Tolkoff-Rubin N E, Herrin J T, Cosimi A B, Collins A B, Hirsch M S, McCluskey R T, Russell P S, Rubin R H. Glomerulopathy associated with cytomegalovirus viremia in renal allografts. N Engl J Med. 1981;305:57–63. doi: 10.1056/NEJM198107093050201. [DOI] [PubMed] [Google Scholar]
- 376.Riddell S R, Greenberg P D. Therapeutic reconstitution of human viral immunity by adoptive transfer of sytotoxic T lymphocyte clones. Curr Top Microbiol Immunol. 1994;189:9–34. doi: 10.1007/978-3-642-78530-6_2. [DOI] [PubMed] [Google Scholar]
- 377.Ringdén O, Lönnqvist B, Paulin T, Ahlmen J, Klintman G, Wahren B, Lernestedt J-O. Pharmacokinetics, safety and preliminary clinical experiences using foscarnet in the treatment of cytomegalovirus infections in bone marrow and renal transplant recipients. J Antimicrob Chemother. 1986;17:373–387. doi: 10.1093/jac/17.3.373. [DOI] [PubMed] [Google Scholar]
- 378.Roberts T C, Brennan D C, Buller R S, Gaudreault-Keener M, Schnitzler M A, Sternhell K E, Garlock K A, Singer G G, Storch G A. Quantitative polymerase chain reaction to predict occurrence of symptomatic cytomegalovirus infection and assess response to ganciclovir therapy in renal transplant recipients. J Infect Dis. 1998;178:626–635. doi: 10.1086/515383. [DOI] [PubMed] [Google Scholar]
- 379.Roberts T C, Brennan D C, Buller R S, Gaudreault-Keener M, Schnitzler M A, Sternhell K E, Garlock K A, Singer G G, Storch G A. Quantitative polymerase chain reaction to predict occurrence of symptomatic cytomegalovirus infection and assess response to ganciclovir therapy in renal transplant recipients. J Infect Dis. 1998;178:626–635. doi: 10.1086/515383. [DOI] [PubMed] [Google Scholar]
- 380.Roberts T C, Buller R S, Gaudreault-Keener M, Sternhell K E, Garlock K, Singer G G, Brennan D C, Storch G A. Effects of storage temperature and time on qualitative and quantitative detection of cytomegalovirus in blood specimens by shell vial culture and PCR. J Clin Microbiol. 1997;35:2224–2228. doi: 10.1128/jcm.35.9.2224-2228.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Rollag H, Sagedal S, Holter E, Degre M, Ariansen S, Nordal K P. Diagnosis of cytomegalovirus infection in kidney transplant recipients by a quantitative RNA-DNA hybrid capture assay for cytomegalovirus DNA in leukocytes. Eur J Clin Microbiol Infect Dis. 1998;17:124–127. doi: 10.1007/BF01682170. [DOI] [PubMed] [Google Scholar]
- 382.Rondeau E, Bourgeon B, Peraldi M N, Lang P, Buisson C, Schulte K M, Weill B, Sraer J D. Effect of prophylactic ganciclovir on cytomegalovirus infection in renal transplant recipients. Nephrol Dial Transplant. 1993;8:858–862. [PubMed] [Google Scholar]
- 383.Rosen H R, Benner K G, Flora K D, Rabkin J M, Orloff S L, Olyaei A, Chou S. Development of ganciclovir resistance during treatment of primary cytomegalovirus infection after liver transplantation. Transplantation. 1997;63:476–478. doi: 10.1097/00007890-199702150-00026. [DOI] [PubMed] [Google Scholar]
- 384.Rosen H R, Chou S, Corless C L, Gretch D R, Flora K D, Boudousquie A, Orloff S L, Rabkin J M, Benner K G. Cytomegalovirus viremia: risk factor for allograft cirrhosis after liver transplantation for hepatitis C. Transplantation. 1997;64:721–726. doi: 10.1097/00007890-199709150-00010. [DOI] [PubMed] [Google Scholar]
- 385.Rosen H R, Corless C L, Rabkin J, Chou S. Association of cytomegalovirus genotype with graft rejection after liver transplantation. Transplantation. 1998;66:1627–1631. doi: 10.1097/00007890-199812270-00010. [DOI] [PubMed] [Google Scholar]
- 386.Ross C, Beynon H, Savill J, Watkins R, Cohen J, Pusey C, Rees A. Ganciclovir treatment for cytomegalovirus infection in immunocompromised patients with renal disease. Q J Med. 1991;81:929–936. [PubMed] [Google Scholar]
- 387.Ross D J, Waters P F, Levine M, Kramer M, Ruzevich S, Kass R M. Mycophenolate mofetil versus azathioprine immunosuppressive regimens after lung transplantation—preliminary experience. J Heart Lung Transplant. 1998;17:768–774. [PubMed] [Google Scholar]
- 388.Rubin R H. Cytomegalovirus disease and allograft loss after organ transplantation. Clin Infect Dis. 1998;26:871–873. doi: 10.1086/513948. [DOI] [PubMed] [Google Scholar]
- 389.Rubin R H. Impact of cytomegalovirus infection on organ transplant recipients. Rev Infect Dis. 1990;12(Suppl. 7):S754–S766. doi: 10.1093/clinids/12.supplement_7.s754. [DOI] [PubMed] [Google Scholar]
- 390.Rubin R H. Infectious disease complications of renal transplantation. Kidney Int. 1993;44:221–236. doi: 10.1038/ki.1993.234. [DOI] [PubMed] [Google Scholar]
- 391.Rubin R H. Preemptive therapy in immunocompromised hosts. N Engl J Med. 1991;324:1057–1059. doi: 10.1056/NEJM199104113241509. [DOI] [PubMed] [Google Scholar]
- 392.Rubin R H, Tolkoff-Rubin N E. Antimicrobial strategies in the care of organ transplant recipients. Antimicrob Agents Chemother. 1993;37:619–624. doi: 10.1128/aac.37.4.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Rubin R H, Tolkoff-Rubin N E, Oliver D, Rota T R, Hamilton J, Betts R F, Pass R F, Hillis W, Szmuness W, Farrell M L, et al. Multicenter seroepidemiologic study of the impact of cytomegalovirus infection on renal transplantation. Transplantation. 1985;40:243–249. doi: 10.1097/00007890-198509000-00004. [DOI] [PubMed] [Google Scholar]
- 394.Rubin R H, Young L S. Infection in the organ transplant recipient. In: Rubin R H, Young L S, editors. Clinical approach to infection in the compromised host. 3rd ed. New York, N.Y: Plenum Publishing Corp.; 1994. pp. 629–705. [Google Scholar]
- 395.Saliba F, Arulnaden J L, Gugenheim J, Serves C, Samuel D, Bismuth A, Mathieu D, Bismuth H. CMV hyperimmune globulin prophylaxis after liver transplantation: a prospective randomized controlled study. Transplant Proc. 1989;21:2260–2262. [PubMed] [Google Scholar]
- 396.Saliba F, Eyraud D, Samuel D, David M F, Arulnaden J L, Dussaiz E, Mathieu D, Bismuth H. Randomized controlled trial of acyclovir for the prevention of cytomegalovirus infection and disease in liver transplant recipients. Transplant Proc. 1993;25:1444–1445. [PubMed] [Google Scholar]
- 397.Salmela K, Hocherstedt K, Lautenschlager I, Eklund B, Isoniemi H, Holmberg C, Ahonen J. Ganciclovir in the treatment of severe cytomegalovirus disease in liver transplant patients. Transplant Proc. 1990;22:238–240. [PubMed] [Google Scholar]
- 398.Saltzman R L, Quirk M R, Jordan M C. Disseminated cytomegalovirus infection. Molecular analysis of virus and leukocyte interactions in viremia. J Clin Investig. 1988;81:75–81. doi: 10.1172/JCI113313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Saltzman R L, Quirk M R, Jordan M C. High levels of circulating cytomegalovirus DNA reflect visceral organ disease in viremic immunosuppressed patients other than marrow recipients. J Clin Investig. 1992;90:1832–1838. doi: 10.1172/JCI116059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Samuel D, Dussaix E. Cytomegalovirus infection, fulminant hepatitis, and liver transplantation: the sides of the triangle. Liver Transplant Surg. 1997;3:547–551. doi: 10.1002/lt.500030513. [DOI] [PubMed] [Google Scholar]
- 401.Sarmiento J M, Munn S R, Paya C V, Velosa J A, Nguyen J H. Is cytomegalovirus infection related to mycophenolate mofetil after kidney transplantation—a case-control study. Clin Transplant. 1998;12:371–374. [PubMed] [Google Scholar]
- 402.Sawyer M D, Mayoral J L, Gillingham K J, Kramer M A, Dunn D L. Treatment of recurrent cytomegalovirus disease in patients receiving solid organ transplants. Arch Surg. 1993;128:165–170. doi: 10.1001/archsurg.1993.01420140042007. [DOI] [PubMed] [Google Scholar]
- 403.Sayage L H, Gonwa T A, Goldstein R M, Husberg B S, Klintmalm G B. Cytomegalovirus infection in orthotopic liver transplantation. Transplant Int. 1989;2:96–101. doi: 10.1007/BF02459327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Sayers M H, Anderson K C, Goodnough L T, Kurtz S R, Lane T A, Piscotto P, Silberstein L E. Reducing the risk for transfusion-transmitted cytomegalovirus infection. Ann Intern Med. 1992;116:55–62. doi: 10.7326/0003-4819-116-1-55. [DOI] [PubMed] [Google Scholar]
- 405.Schafer P, Tenschert W, Cremaschi L, Gutensohn K, Laufs R. Utility of major leukocyte subpopulations for monitoring secondary cytomegalovirus infections in renal-allograft recipients by PCR. J Clin Microbiol. 1998;36:1008–1014. doi: 10.1128/jcm.36.4.1008-1014.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Schafer P, Tenschert W, Gutensohn K, Laufs R. Minimal effect of delayed sample processing on results of quantitative PCR for cytomegalovirus DNA in leukocytes compared to results of an antigenemia assay. J Clin Microbiol. 1997;35:741–744. doi: 10.1128/jcm.35.3.741-744.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Schafers H J, Wahlers T, Jurmann M, Fieguth H G, Milbradt H, Flik J, Haverich A. Hyperimmuneglobulin for cytomegalovirus prophylaxis following heart transplantation. J Hosp Infect. 1988;12(Suppl. D):61–65. doi: 10.1016/0195-6701(88)90031-x. [DOI] [PubMed] [Google Scholar]
- 408.Schirm J, Timmerije W, van der Bij W, The T H, Wilterdink J B, Tegzess A M, van Son W J, Schroder F P. Rapid detection of infectious cytomegalovirus in blood with the aid of monoclonal antibodies. J Med Virol. 1987;23:31–40. doi: 10.1002/jmv.1890230105. [DOI] [PubMed] [Google Scholar]
- 409.Schmidt C A, Oettle H, Peng R, Neuhaus P, Blumhardt G, Lohmann R, Wilborn F, Osthoff K, Oertel J, Timm H, et al. Comparison of polymerase chain reaction from plasma and buffy coat with antigen detection and occurrence of immunoglobulin M for the demonstration of cytomegalovirus infection after liver transplantation. Transplantation. 1995;59:1133–1138. [PubMed] [Google Scholar]
- 410.Schnitzler M A, Woodward R S, Brennan D C, Spitznagel E L, Dunagan W C, Bailey T C. Impact of cytomegalovirus serology on graft survival in living related kidney transplantation: implications for donor selection. Surgery. 1997;121:563–568. doi: 10.1016/s0039-6060(97)90112-4. [DOI] [PubMed] [Google Scholar]
- 411.Schooley R T, Hirsch M S, Colvin R B, Cosimi A B, Tolkoff-Rubin N E, McCluskey R T, Burton R C, Russell P S, Herrin J T, Delmonico F L, Giorgi J V, Henle W, Rubin R H. Association of herpesvirus infections with T-lymphocyte-subset alterations, glomerulopathy, and opportunistic infections after renal transplantation. N Engl J Med. 1983;308:307–313. doi: 10.1056/NEJM198302103080603. [DOI] [PubMed] [Google Scholar]
- 412.Schrier R D, Nelson J A, Oldstone M B A. Detection of human cytomegalovirus in peripheral blood lymphocytes in a natural infection. Science. 1985;230:1048–1051. doi: 10.1126/science.2997930. [DOI] [PubMed] [Google Scholar]
- 413.Schrier R D, Rice G P, Oldstone M B. Suppression of natural killer cell activity and T cell proliferation by fresh isolates of human cytomegalovirus. J Infect Dis. 1986;153:1084–1091. doi: 10.1093/infdis/153.6.1084. [DOI] [PubMed] [Google Scholar]
- 414.Scott J P, Higenbottam T W, Sharples L, Clelland C A, Smyth R L, Stewart S, Wallwork J. Risk factors for obliterative bronchiolitis in heart-lung transplant recipients. Transplantation. 1991;51:813–817. doi: 10.1097/00007890-199104000-00015. [DOI] [PubMed] [Google Scholar]
- 415.Sharples L D, Caine N, Mullins P, Scott J P, Solis E, English T A H, Large S R, Schofield P M, Wallwork J. Risk factor analysis for the major hazards following heart transplantation-rejection, infection, and coronary occlusive disease. Transplantation. 1991;52:244–252. doi: 10.1097/00007890-199108000-00012. [DOI] [PubMed] [Google Scholar]
- 416.Shea B F, Hoffman S, Sesin G P, Hammer S M. Ganciclovir hepatotoxicity. Pharmacotherapy. 1987;7:223–226. doi: 10.1002/j.1875-9114.1987.tb03529.x. [DOI] [PubMed] [Google Scholar]
- 417.Shen G K, Alfrey E J, Knoppel C L, Dafoe D C, Scandling J D. Eradication of cytomegalovirus reactivation disease using high-dose acyclovir and targeted intravenous ganciclovir in kidney and kidney/pancreas transplantation. Transplantation. 1997;64:931–933. doi: 10.1097/00007890-199709270-00026. [DOI] [PubMed] [Google Scholar]
- 418.Shepp D H, Dandliker P S, de Miranda P, Burnette T C, Cederberg D M, Kirk L E, Meyers J D. Activity of 9-[2-hydroxy-1-(hydroxymethyl)ethoxymethyl]guanine in the treatment of cytomegalovirus pneumonia. Ann Intern Med. 1985;103:368–373. doi: 10.7326/0003-4819-103-3-368. [DOI] [PubMed] [Google Scholar]
- 419.Shrestha B M, Parton D, Gray A, Shephard D, Griffith D, Westmoreland D, Griffin P, Lord R, Salaman J R, Moore R H. Cytomegalovirus involving gastrointestinal tract in renal transplant recipients. Clin Transplant. 1996;10:170–175. [PubMed] [Google Scholar]
- 420.Singh N, Dummer J S, Kusne S, Breinig M K, Armstrong J A, Makawoka L, Starzl T E, Ho M. Infections with cytomegalovirus and other herpesvirus in 121 liver transplant recipients: transmission by donated organ and the effect of OKT3 antibodies. J Infect Dis. 1988;158:124–131. doi: 10.1093/infdis/158.1.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Singh N, Gayowski T, Wagener M M, Marino I R. Increased infections in liver transplant recipients with recurrent hepatitis C virus hepatitis. Transplantation. 1996;61:402–406. doi: 10.1097/00007890-199602150-00014. [DOI] [PubMed] [Google Scholar]
- 422.Singh N, Mieles L, Yu V L, Starzl T E. Decreased incidence of viral infections in liver transplant recipients. Possible effects of FK506? Dig Dis Sci. 1994;39:15–18. doi: 10.1007/BF02090054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Singh N, Yu V L, Mietes L, Wagener M W, Miner R C, Gayoski T. High-dose acyclovir compared with short-course preemptive therapy to prevent cytomegalovirus disease in liver transplant recipients. A randomized trial. Ann Intern Med. 1994;120:375–381. doi: 10.7326/0003-4819-120-5-199403010-00004. [DOI] [PubMed] [Google Scholar]
- 424.Singh N, Zeevi A, Gayowski T, Marino I R. Late onset cytomegalovirus disease in liver transplant recipients—de novo reactivation in recurrent hepatitis C virus hepatitis. Transplant Int. 1998;11:308–311. doi: 10.1007/s001470050148. [DOI] [PubMed] [Google Scholar]
- 425.Slusser S O, Boehmer J P, Zurlo J, Ruggiero F, Ouyang A. Questioning the clinical significance of upper gastrointestinal cytomegalovirus disease following heart transplantation. Dig Dis Sci. 1995;40:1824–1830. doi: 10.1007/BF02212708. [DOI] [PubMed] [Google Scholar]
- 426.Smith I L, Cherrington J M, Jiles R E, Fuller M D, Freeman W R, Spector S A. High-level resistance of cytomegalovirus to ganciclovir is associated with alterations in both the UL97 and DNA polymerase genes. J Infect Dis. 1997;176:69–77. doi: 10.1086/514041. [DOI] [PubMed] [Google Scholar]
- 427.Smith M A, Sundaresan S, Mohanakumar T, Trulock E P, Lynch J P, Phelan D L, Cooper J D, Patterson G A. Effect of development of antibodies to HLA and cytomegalovirus mismatch on lung transplantation survival and development of bronchiolitis obliterans syndrome. J Thorac Cardiovasc Surg. 1998;116:812–819. doi: 10.1016/S0022-5223(98)00444-9. [DOI] [PubMed] [Google Scholar]
- 428.Smyth R L, Scott J P, Borysiewicz L K, Sharples L D, Stewart S, Wreghitt T G, Gray J J, Higenbottam T W, Wallwork J. Cytomegalovirus infection in heart-lung transplant recipients: risk factors, clinical associations, and response to treatment. J Infect Dis. 1991;164:1045–1050. doi: 10.1093/infdis/164.6.1045. [DOI] [PubMed] [Google Scholar]
- 429.Snydman D R. Cytomegalovirus immunoglobulins in the prevention and treatment of cytomegalovirus disease. Rev Infect Dis. 1990;12(Suppl. 7):S839–S848. doi: 10.1093/clinids/12.supplement_7.s839. [DOI] [PubMed] [Google Scholar]
- 430.Snydman D R. Ganciclovir therapy for cytomegalovirus disease associated with renal transplants. Rev Infect Dis. 1988;10:S554–S562. doi: 10.1093/clinids/10.supplement_3.s554. [DOI] [PubMed] [Google Scholar]
- 431.Snydman D R, Werner B G, Dougherty N N, Griffith J, Rohrer R H, Freeman R, Jenkins R, Lewis W D, O'Rourke E T. B. C. f. L. T. C.-S. Group. A further analysis of the use of cytomegalovirus immune globulin in orthotopic liver transplant recipients at risk for primary infection. Transplant Proc. 1994;26:23–27. [PubMed] [Google Scholar]
- 432.Snydman D R, Werner B G, Dougherty N N, Griffith J, Rubin R H, Dienstag J L, Rohrer R H, Freeman R, Jenkins R, Lewis D, Hammer S, O'Rourke E, Grady G F, Fawaz K, Kaplan M M, Hoffman M A, Katz A T, Doran M. Cytomegalovirus immune globulin prophylaxis in liver transplantation. A randomized, double blind, placebo-controlled trial. The Boston Center for Liver Transplantation CMVIG Study Group. Ann Intern Med. 1993;10:984–991. doi: 10.7326/0003-4819-119-10-199311150-00004. [DOI] [PubMed] [Google Scholar]
- 433.Snydman D R, Werner B G, Heinze-Lacey B, Bernardi V P, Tilney N L, Kirkman R L, Milford E L, Cho S I, Bush H L, Levey A S, Harmon W E, Carpenter C B, Levey R H, Harmon W E, Zimmerman C E, Shapiro M E, Steinman T, LoGerfo F, Idelson B, Schroter G P J, Levin M J, McIver J, Leszczynski J, Grady G F. Use of cytomegalovirus immune globulin to prevent cytomegalovirus disease in renal-transplant recipients. N Engl J Med. 1987;317:1049–1054. doi: 10.1056/NEJM198710223171703. [DOI] [PubMed] [Google Scholar]
- 434.Soderberg C, Larsson S, Bergstedt-Lindqvist, Moller E. Definition of a subset of human peripheral blood mononuclear cells that are permissive to human cytomegalovirus infection. J Virol. 1993;67:3166–3175. doi: 10.1128/jvi.67.6.3166-3175.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Sohn Y M, Oh M K, Balcarek K B, Cloud G A, Pass R F. Cytomegalovirus infection in sexually active adolescents. J Infect Dis. 1991;163:460–463. doi: 10.1093/infdis/163.3.460. [DOI] [PubMed] [Google Scholar]
- 436.Solans E P, Garrity E R, Jr, McCabe M, Martinez R, Husain A N. Early diagnosis of cytomegalovirus pneumonitis in lung transplant patients. Arch Pathol Lab Med. 1995;119:33–35. [PubMed] [Google Scholar]
- 437.Solans E P, Yong S, Husain A N, Eichorst M, Gattuso P. Bronchioloalveolar lavage in the diagnosis of CMV pneumonitis in lung transplant recipients: an immunocytochemical study. Diagn Cytopathol. 1997;16:350–352. doi: 10.1002/(sici)1097-0339(199704)16:4<350::aid-dc9>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 438.Solez K, Vincenti F, Filo R S. Histopathologic findings from 2-year protocol biopsies from a US multicenter kidney transplant trial comparing tacrolimus versus cyclosporine: A report of the FK506 Kidney Transplant Study Group. Transplantation. 1998;66:1736–1740. doi: 10.1097/00007890-199812270-00029. [DOI] [PubMed] [Google Scholar]
- 439.Spector S A, Hirata K K, Newman T R. Identification of multiple cytomegalovirus strains in homosexual men with acquired immunodeficiency syndrome. J Infect Dis. 1984;150:953–956. doi: 10.1093/infdis/150.6.953. [DOI] [PubMed] [Google Scholar]
- 440.Spector S A, Merrill R, Wolf D, Dankner W M. Detection of human cytomegalovirus in plasma of AIDS patients during acute visceral disease by DNA amplification. J Clin Microbiol. 1992;30:2359–2365. doi: 10.1128/jcm.30.9.2359-2365.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.Spencer G D, Hackman R C, McDonald G B, Arnold D E, Cunningham B A, Meyers J D, Thomas E D. A prospective study of unexplained nausea and vomiting after marrow transplantation. Transplantation. 1986;42:602–607. doi: 10.1097/00007890-198612000-00006. [DOI] [PubMed] [Google Scholar]
- 442.Stagno S, Cloud G A. Working parents: the impact of day care and breast-feeding on cytomegalovirus infections in offspring. Proc Natl Acad Sci USA. 1994;91:2384–2389. doi: 10.1073/pnas.91.7.2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.Stanat S C, Reardon J E, Erice A, Jordan M C, Drew W L, Biron K K. Ganciclovir-resistant cytomegalovirus clinical isolates: mode of resistance to ganciclovir. Antimicrob Agents Chemother. 1991;35:2191–2197. doi: 10.1128/aac.35.11.2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 444.Starzl T, Porter K A, Schroter G, Corman J, Groth C, Sharp H L. Autopsy findings in a long-surviving liver recipient. N Engl J Med. 1973;289:82–84. doi: 10.1056/NEJM197307122890207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445.Steffens H P, Kurz S, Holtappels R, Reddehase M J. Preemptive CD8 T-cell immunotherapy of acute cytomegalovirus infection prevents lethal disease, limits the burden of latent viral genomes, and reduces the risk of virus recurrence. J Virol. 1998;72:1797–1804. doi: 10.1128/jvi.72.3.1797-1804.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 446.Stein D S, Verano A S, Levandowski R A. Successful treatment with ganciclovir of disseminated cytomegalovirus infection after liver transplantation. Am J Gastroenterol. 1988;83:684–686. [PubMed] [Google Scholar]
- 447.Steinmuller D R, Novick A C, Streen S B, Graneto D, Swift C. Intravenous immunoglobulin infusions for the prophylaxis of secondary cytomegalovirus infection. Transplantation. 1990;49:68–70. doi: 10.1097/00007890-199001000-00015. [DOI] [PubMed] [Google Scholar]
- 448.Stephan F, Fajac A, Grenet D, Honderlick P, Ricci S, Frachon I, Friard S, Caubarrere I, Bernaudin J F, Stern M. Predictive value of cytomegalovirus DNA detection by polymerase chain reaction in blood and bronchoalveolar lavage in lung transplant patients. Transplantation. 1997;63:1430–1435. doi: 10.1097/00007890-199705270-00011. [DOI] [PubMed] [Google Scholar]
- 449.Storch G A, Buller R S, Bailey T C, Ettinger N A, Langlois T, Gaudreault-Keener M, Welby P L. Comparison of PCR and pp65 antigenemia assay with quantitative shell vial culture for detection of cytomegalovirus in blood leukocytes from solid-organ transplant recipients. J Clin Microbiol. 1994;32:997–1003. doi: 10.1128/jcm.32.4.997-1003.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Stratta R J. Clinical patterns and treatment of cytomegalovirus infection after solid-organ transplantation. Transplant Proc. 1993;25:15–21. [PubMed] [Google Scholar]
- 451.Stratta R J, Shaefer M S, Markin R S, Wood R P, Kennedy E M, Langnas A N, Reed E C, Woods G L, Donovan J P, Pillen T J, Duckworth R M, Shaw B W. Clinical patterns of cytomegalovirus disease after liver transplantation. Arch Surg. 1989;124:1443–1450. doi: 10.1001/archsurg.1989.01410120093018. [DOI] [PubMed] [Google Scholar]
- 452.Stratta R J, Shaefer M S, Markin R S, Wood R P, Langnas A N, Reed E C, Donovan J P, Woods G L, Bradshaw K A, Pillen T J, Shaw B W. Cytomegalovirus infection and disease after liver transplantation. An overview. Dig Dis Sci. 1992;37:673–688. doi: 10.1007/BF01296422. [DOI] [PubMed] [Google Scholar]
- 453.Stratta R J, Shaeffer M S, Cushing K A, Markin R S, Reed E C, Langnas A N, Pillen T J, Shaw B W. A randomized prospective trial of acyclovir and immune globulin prophylaxis in liver transplant recipients receiving OKT3 therapy. Arch Surg. 1992;127:55–64. doi: 10.1001/archsurg.1992.01420010065009. [DOI] [PubMed] [Google Scholar]
- 454.Sullivan V, Biron K K, Talarico C, Stanat S C, Davis M, Pozzi L M, Coen D M. A point mutation in the human cytomegalovirus DNA polymerase gene confers resistance to ganciclovir and phosphonylmethoxyalkyl derivatives. Antimicrob Agents Chemother. 1993;37:19–25. doi: 10.1128/aac.37.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.Sullivan V, Talarico C, Stanat S, et al. A protein kinase homologue controls phosphorylation of ganciclovir in human cytomegalovirus-infected cells. Nature. 1992;358:162–164. doi: 10.1038/358162a0. [DOI] [PubMed] [Google Scholar]
- 456.Sutherland D E R, Chan F Y, Foucar E. The bleeding cecal ulcer in transplant patients. Surgery. 1979;86:386–398. [PubMed] [Google Scholar]
- 457.Swan S, Munar M, Wigger M, et al. Pharmacokinetics of ganciclovir in a patient undergoing hemodialysis. Am J Kidney Dis. 1991;17:69–72. doi: 10.1016/s0272-6386(12)80253-8. [DOI] [PubMed] [Google Scholar]
- 458.Tanabe K, Tokumoto T, Ishikawa N, Koyama I, Takahashi K, Fuchinoue S, Kawai T, Koga S, Yagisawa T, Toma H, Ota K, Nakajima H. Comparative study of cytomegalovirus (CMV) antigenemia assay, polymerase chain reaction, serology, and shell vial assay in the early diagnosis and monitoring of CMV infection after renal transplantation. Transplantation. 1997;64:1721–1725. doi: 10.1097/00007890-199712270-00016. [DOI] [PubMed] [Google Scholar]
- 459.Tatarowicz W A, Lurain N S, Thompson K D. A ganciclovir-resistant clinical isolate of human cytomegalovirus exhibiting cross-resistance to other DNA polymerase inhibitors. J Infect Dis. 1992;166:904–907. doi: 10.1093/infdis/166.4.904. [DOI] [PubMed] [Google Scholar]
- 460.Telenti A, Smith T F. Screening with a shell vial assay for antiviral activity against cytomegalovirus. Diagn Microbiol Infect Dis. 1989;12:5–8. doi: 10.1016/0732-8893(89)90036-9. [DOI] [PubMed] [Google Scholar]
- 461.Tenney D J, Yamanaka G, Voss S M, Cianci C W, Tuomari A V, Sheaffer A K, Alam M, Colonno R J. Lobucavir is phosphorylated in human cytomegalovirus-infected and -uninfected cells and inhibits the viral DNA polymerase. Antimicrob Agents Chemother. 1997;41:2680–2685. doi: 10.1128/aac.41.12.2680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 462.The T H, Grefte J M, van der Bij W, van Son W J, van den Berg A P. CMV infection after organ transplantation: immunopathological and clinical aspects. Neth J Med. 1994;45:309–318. [PubMed] [Google Scholar]
- 463.The T H, van den Berg A P, Harmsen M C, van der Bij W, van Son W J. The cytomegalovirus antigenemia assay: a plea for standardization. Scand J Infect Dis Suppl. 1995;99:25–29. [PubMed] [Google Scholar]
- 464.The T H, van den Berg A P, van Son W J, Klompmaker I J, Harmsen M C, van der Giessen M, Sloof M J H. Monitoring for cytomegalovirus after organ transplantation: a clinical perspective. Transplant Proc. 1993;25:5–9. [PubMed] [Google Scholar]
- 465.The T H, van der Bij W, van den Berg A P, van der Giessen M, Weits J, Sprenger H G, van Son W J. Cytomegalovirus antigenemia. Rev Infect Dis. 1990;12(Suppl. 7):S734–S744. [PubMed] [Google Scholar]
- 466.The T H, van der Ploeg M, van den Berg A P, Vlieger A M, van der Giessen M, van Son W J. Direct detection of cytomegalovirus in peripheral blood leukocytes—a review of the antigenemia assay and polymerase chain reaction. Transplantation. 1992;54:193–198. doi: 10.1097/00007890-199208000-00001. [DOI] [PubMed] [Google Scholar]
- 467.Todd S, Reyes J, Furukawa H, Abu-Elmagd K, Lee R G, Tzakis A, Rao A S, Starzl T E. Outcome analysis of 71 clinical intestinal transplantations. Ann Surg. 1995;222:270–280. doi: 10.1097/00000658-199509000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 468.Tong C Y. Diagnosis of cytomegalovirus infection and disease. J Med Microbiol. 1997;46:717–719. doi: 10.1099/00222615-46-9-717. [DOI] [PubMed] [Google Scholar]
- 469.Tong C Y W, Cuevas L, Williams H, Bakran A. Use of laboratory assays to predict cytomegalovirus disease in renal transplant recipients. J Clin Microbiol. 1998;36:2681–2685. doi: 10.1128/jcm.36.9.2681-2685.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.Toyoda M, Carlos J B, Galera O A, Galfayan K, Zhang X, Sun Z, Czer L S, Jordan S C. Correlation of cytomegalovirus DNA levels with response to antiviral therapy in cardiac and renal allograft recipients. Transplantation. 1997;63:957–963. doi: 10.1097/00007890-199704150-00009. [DOI] [PubMed] [Google Scholar]
- 471.Turgeon N, Fishman J A, Basgoz N, Tolkoff-Rubin N E, Doran M, Cosimi A B, Rubin R H. Effect of oral acyclovir or ganciclovir therapy after preemptive intravenous ganciclovir therapy to prevent cytomegalovirus disease in cytomegalovirus seropositive renal and liver transplant recipients receiving antilymphocyte antibody therapy. Transplantation. 1998;66:1780–1786. doi: 10.1097/00007890-199812270-00036. [DOI] [PubMed] [Google Scholar]
- 472.Ulrich W, Schlederer M P, Buxbaum P, Stummvoll H, Rockenschaub S, Kovarik J, Krisch I. The histopathologic identification of CMV infected cells in biopsies of human renal allografts. An evaluation of 100 transplant biopsies by in situ hybridization. Pathol Res Pract. 1986;181:739–745. doi: 10.1016/s0344-0338(86)80050-4. [DOI] [PubMed] [Google Scholar]
- 473.Valantine H A. Prevention and treatment of cytomegalovirus disease in thoracic organ transplant patients: evidence for a beneficial effect of hyperimmune globulin. Transplant Proc. 1995;27(5 Suppl. 1):49–57. [PubMed] [Google Scholar]
- 474.van den Berg A P, Klimpmaker I J, Haagsma E B, Scholten-Sampson A, Bijleveld C M A, Schirm J, van der Giessen M, Slooff M J H, The T H. Antigenemia in the diagnosis and monitoring of active cytomegalovirus infection after liver transplantation. J Infect Dis. 1991;164:265–270. doi: 10.1093/infdis/164.2.265. [DOI] [PubMed] [Google Scholar]
- 475.van den Berg A P, Klompmaker I J, Haagsma E B, Peeters P M J G, Meerman L, Verwer R, The T H, Slooff M J H. Evidence for an increased rate of bacterial infections in liver transplant patients with cytomegalovirus infection. Clin Transplant. 1996;10:224–231. [PubMed] [Google Scholar]
- 476.van den Berg A P, Klompmaker I J, Hepkema B G, Gouw A S, Haagsma E B, Lems S P, The T H, Slooff M J. Cytomegalovirus infection does not increase the risk of vanishing bile duct syndrome after liver transplantation. Transplant Int. 1996;9(Suppl. 1):S171–S173. doi: 10.1007/978-3-662-00818-8_42. [DOI] [PubMed] [Google Scholar]
- 477.van den Berg A P, Tegzess A M, Scholten-Sampson A, Schirm J, van der Giessen M, The T H, van Son W J. Monitoring antigenemia is useful in guiding treatment of severe cytomegalovirus disease after organ transplantation. Transplant Int. 1992;5:101–106. doi: 10.1007/BF00339224. [DOI] [PubMed] [Google Scholar]
- 478.van den Berg A P, van Son W J, Haagsma E B, Klompmaker I J, Tegzess A M, Schirm J, Dijkstra G, van der Giessen M, Slooff M J, The T H. Prediction of recurrent cytomegalovirus disease after treatment with ganciclovir in solid-organ transplant recipients. Transplantation. 1993;55:847–851. doi: 10.1097/00007890-199304000-00031. [DOI] [PubMed] [Google Scholar]
- 479.van der Bij W, Schirm J, Torensma R, van Son W J, Tegzess A M, The T H. Comparison between viremia and antigenemia for detection of cytomegalovirus in blood. J Clin Microbiol. 1988;26:2531–2535. doi: 10.1128/jcm.26.12.2531-2535.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 480.van der Meer J T, Drew W L, Bowden R A, Galasso G J, Griffiths P D, Jabs D A, Katlama C, Spector S A, Whitley R J. Summary of the International Consensus Symposium on Advances in the Diagnosis, Treatment and Prophylaxis and Cytomegalovirus Infection. Antiviral Res. 1996;32:119–140. doi: 10.1016/s0166-3542(96)01006-6. [DOI] [PubMed] [Google Scholar]
- 481.Vanrenterghem Y. The use of Mycophenolate Mofetil (Cellcept) in renal transplantation. Nephron. 1997;76:392–399. doi: 10.1159/000190219. [DOI] [PubMed] [Google Scholar]
- 482.van Son W J, The T H. Cytomegalovirus infection after organ transplantation: an update with special emphasis on renal transplantation. Transplant Int. 1989;2:147–164. doi: 10.1007/BF02414602. [DOI] [PubMed] [Google Scholar]
- 483.van Son W J, van der Berg A P, The T H, Tegzess A M. Preemptive therapy with ganciclovir for early high-risk CMV infection allows effective treatment with antithymocyte globulin of steroid-resistant rejection after renal transplantation. Transplant Proc. 1993;25:1436–1438. [PubMed] [Google Scholar]
- 484.van Thiel D H, Gavaler J S, Schade R R, Clien M-C, Starzl T E. Cytomegalovirus infection and gastric emptying. Transplantation. 1992;54:70–73. doi: 10.1097/00007890-199207000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 485.Vogel J-U, Scholz M, Cinatl J J. Treatment of cytomegalovirus diseases. Intervirology. 1997;40:357–367. doi: 10.1159/000150568. [DOI] [PubMed] [Google Scholar]
- 486.Wade J C, Hintz M, McGuffin R W, Springmeyer S C, Connor J D, Meyers J D. Treatment of cytomegalovirus pneumonia with high dose acyclovir. Am J Med. 1982;73:249–256. doi: 10.1016/0002-9343(82)90100-0. [DOI] [PubMed] [Google Scholar]
- 487.Wagner J A, Ross H, Hunt S, Gamberg P, Valantine H, Merigan T C, Stinson E B. Prophylactic ganciclovir treatment reduces fungal as well as cytomegalovirus infections after heart transplantation. Transplantation. 1995;60:1473–1477. doi: 10.1097/00007890-199560120-00018. [DOI] [PubMed] [Google Scholar]
- 488.Walker R C, Paya C V, Marshall W F, Strickler J G, Wiesner R H, Velosa J A, Habermann T M, Daly R C, McGregor C G A. Pretransplantation seronegative Epstein-Barr virus status is the primary risk factor for posttransplantation lymphoproliferative disorder in adult heart, lung, and other solid organ transplantations. J Heart Lung Transplant. 1995;14:214–221. [PubMed] [Google Scholar]
- 489.Walter E A, Greenberg P D, Gilbert M J, Finch R J, Watanabe K S, Thomas E D, Riddell S D. Reconstitution of cellular immunity against cytomegalovirus in recipients of allogeneic bone marrow by transfer of T-cell clones from the donor. N Engl J Med. 1995;333:1038–1044. doi: 10.1056/NEJM199510193331603. [DOI] [PubMed] [Google Scholar]
- 490.Watson F S, O'Connell J B, Amber I J, Renlund D G, Classen D, Johnston J M, Smith C B, Bristow M R, Program T U C T. Treatment of cytomegalovirus pneumonia in heart transplant recipients with 9(1,3-dihydroxy-2-proproxymethyl)-guanine (DHPG) J Heart Transplant. 1988;7:102–105. [PubMed] [Google Scholar]
- 491.Weinberg A, Spiers D, Cai G Y, Long C M, Sun R, Tevere V. Evaluation of a commercial PCR kit for diagnosis of cytomegalovirus infection of the central nervous system. J Clin Microbiol. 1998;36:3382–3384. doi: 10.1128/jcm.36.11.3382-3384.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 492.Weiss L M, Movahed L A, Berry G J, Billingham M E. In situ hybridization studies for viral nucleic acids in heart and lung allograft biopsies. Am J Clin Pathol. 1990;93:675–679. doi: 10.1093/ajcp/93.5.675. [DOI] [PubMed] [Google Scholar]
- 493.Weiss R L, Snow G W, Schumann G B, Hammond M E. Diagnosis of cytomegalovirus pneumonitis on bronchoalveolar lavage fluid: comparison of cytology, immunofluorescence, and in situ hybridization with viral isolation. Diagn Cytopathol. 1991;7:243–247. doi: 10.1002/dc.2840070307. [DOI] [PubMed] [Google Scholar]
- 494.Wiesner R H, Marin E, Porayko M K, Steers J L, Krom R A F, Paya C V. Advances in the diagnosis, treatment, and prevention of cytomegalovirus infections after liver transplantation. Gastroenterol Clin North Am. 1993;22:351–366. [PubMed] [Google Scholar]
- 495.Willmott F E. Cytomegalovirus in female patients attending a VD clinic. Br J Vener Dis. 1975;51:278–280. doi: 10.1136/sti.51.4.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 496.Winston D J, Ho W G, Bartomi K, Holland G N, Mitsuyasu R T, Gale R P, Busuttil R W, Champlin R E. Ganciclovir therapy for cytomegalovirus infections in recipients of bone marrow transplants and other immunosuppressed patients. Rev Infect Dis. 1988;10:S547–S553. doi: 10.1093/clinids/10.supplement_3.s547. [DOI] [PubMed] [Google Scholar]
- 497.Winston D J, Wirin D, Shaked A, Busuttil R W. Randomised comparison of ganciclovir and high-dose acyclovir for long-term cytomegalovirus prophylaxis in liver-transplant recipients. Lancet. 1995;346:69–74. doi: 10.1016/s0140-6736(95)92110-9. [DOI] [PubMed] [Google Scholar]
- 498.Wittes J T, Kelly A, Plante K M. Meta-analysis of CMVIG studies for the prevention and treatment of CMV infection in transplant patients. Transplant Proc. 1996;28(6 Suppl. 2):17–24. [PubMed] [Google Scholar]
- 499.Wolf D G, Spector S A. Diagnosis of human cytomegalovirus central nervous system disease in AIDS patients by DNA amplification from cerebrospinal fluid. J Infect Dis. 1992;166:1412–1415. doi: 10.1093/infdis/166.6.1412. [DOI] [PubMed] [Google Scholar]
- 500.Wolff C, Skourtopoulos M, Hornschemeyer D, Wolff D, Korner M, Huffert F, Korfer R, Kleesier K. Significance of human cytomegalovirus DNA detection in immunocompromised heart transplant patients. Transplantation. 1996;61:750–757. doi: 10.1097/00007890-199603150-00014. [DOI] [PubMed] [Google Scholar]
- 501.Wolff M A, Rand K H, Houck H J, Brunson M E, Howard R J, Langham M R, Davis G L, Mailliard M E, Myers B M, Andres J, et al. Relationship of the polymerase chain reaction for cytomegalovirus to the development of hepatitis in liver transplant recipients. Transplantation. 1993;56:572–576. doi: 10.1097/00007890-199309000-00015. [DOI] [PubMed] [Google Scholar]
- 502.Wright F H, Jr, Banowsky L H. Cytomegalovirus infection and prophylaxis in renal transplantation: financial considerations. Transplant Proc. 1998;30:1318–1319. doi: 10.1016/s0041-1345(98)00258-9. [DOI] [PubMed] [Google Scholar]
- 503.Wu G D, Shintaku I P, Chien K, Geller S A. A comparison of routine light microscopy, immunohistochemistry, and in situ hybridization for the detection of cytomegalovirus in gastrointestinal biopsies. Am J Gastroenterol. 1989;84:1517–1520. [PubMed] [Google Scholar]
- 504.Xiong X, Flores C, Fuller M D, Mendel D B, Mulato A S, Moon K, Chen M S, Cherrington J M. In vitro characterization of the anti-human cytomegalovirus activity of PMEA (Adefovir) Antiviral Res. 1997;36:131–137. doi: 10.1016/s0166-3542(97)00050-8. [DOI] [PubMed] [Google Scholar]
- 505.Yang C W, Kim Y O, Kim Y S, Kim S Y, Moon I S, Ahn H J, Koh Y B, Bang B K. Clinical course of cytomegalovirus (CMV) viremia with and without ganciclovir treatment in CMV-seropositive kidney transplant recipients—longitudinal follow-up of CMV pp65 antigenemia assay. Am J Nephrol. 1998;18:373–378. doi: 10.1159/000013379. [DOI] [PubMed] [Google Scholar]
- 506.Zeevi A, Morel P, Spichty K, Dauber J, Yousem S, Williams P, Grgurich W, Pham S, Iacono A, Keenan R, Duquesnoy R, Griffith B. Clinical significance of CMV-specific T helper responses in lung transplant recipients. Hum Immunol. 1998;59:768–775. doi: 10.1016/s0198-8859(98)00088-3. [DOI] [PubMed] [Google Scholar]
- 507.Zipeto D, Revello M G, Silini E, Parea M, Percivalle E, Zavattoni M, Milanesi G, Gerna G. Development and clinical significance of a diagnostic assay based on the polymerase chain reaction for detection of human cytomegalovirus DNA in blood samples from immunocompromised patients. J Clin Microbiol. 1992;30:527–530. doi: 10.1128/jcm.30.2.527-530.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 508.Zou R, Drach J C, Townsend L B. Design, synthesis, and antiviral evaluation of 2-chloro-5,6-dihalo-1-beta-d-ribofuranosylbenzimidazoles as potential agents for human cytomegalovirus infections. J Med Chem. 1997;40:811–818. doi: 10.1021/jm960462g. [DOI] [PubMed] [Google Scholar]